At what age do you stop burping your baby after a feeding
How and When to Burp a Newborn
NewbornPediatricsLactation Consultation
Reviewed By Melinda L. Winterscheid, M.D.
While it might not be the most glamorous of tasks, burping your baby is important for his or her comfort. When babies are feeding, they take in air, which can build up and make them uncomfortable, causing you to find yourself with a fussy, squirmy child.
When to Burp Your Baby
How much a baby needs to burp will vary from baby to baby. If you're burping a newborn after breastfeeding, the baby will typically burp less because they swallow less air. Most babies will outgrow the need to be burped by 4-6 months of age.
You can often tell that a baby needs to be burped if he or she is squirmy or pulling away while being fed. This being said, the American Academy of Pediatrics recommends that parents try to burp their baby:
- When a nursing mother switches breasts or
- Every 2-3 oz.
if being bottle-fed (60 – 90 mL)
Pausing to burp frequently slows feeding and reduces air intake. However, if your baby has not successfully burped after a few minutes of trying, switch methods or give up and continue with the feeding. It is possible that your baby doesn’t actually have to burp. The best method for burping will generally differ for babies and parents – use the method that works best for you.
Burping Methods
There are three popular methods for burping newborns and babies. All will require a burping cloth to protect from spit up or wet burps and a gentle patting motion across a baby’s back to coax out the burp. The main difference is how the baby is held. Take care to support the baby’s head and neck safely and move the baby slowly and gently.
- Leaning
- Place a burping cloth or towel on your shoulder and/or back.
- Rest your baby’s chin or belly on your shoulder. (If opting for the belly, make sure that your baby can breathe easily.
 Parents may benefit from trying this option after their baby has better head/neck control.)
Parents may benefit from trying this option after their baby has better head/neck control.) - Support and hold your baby in place with one hand, while using the other to gently pat your baby on the back.
- Sitting
- Place a burping cloth or towel across your lap and put a bib on your baby.
- Using your palm to support your baby’s chest and your fingers to support his or her jaw (not throat), place your baby sitting on your lap, facing away from you.
- With your free hand, gently pat your baby on the back.
- Laying
- Place a burping cloth or towel across your lap.
- Lay your baby across your knees, perpendicular to your body.
- Use one hand to support your baby’s head so that it is higher than the chest. This will prevent blood from rushing to the head.
- With your free hand, gently pat your baby on the back.
More information about feeding and burping your newborn:
When to be Concerned About Spit Up
Feeding Your Newborn
Is My Baby Eating Enough?
Newborn Pediatrics;Lactation Consultation
It looks like your browser does not have JavaScript enabled. Please turn on JavaScript and try again.
It looks like your browser does not have JavaScript enabled. Please turn on JavaScript and try again.
Please turn on JavaScript and try again.
When Do You Stop Burping A Baby?
Our editorial team personally selects each featured product. If you buy something through our links, we may earn an affiliate commission, at no cost to you.
Wouldn’t it be great if there was a perfect guide for burping your baby? Like a recipe it would read: Add twelve firm pats, plus a smidge of back rubs, and after six and a half minutes you’ll have a perfect burp and a happy baby! While a clear-cut formula doesn’t really exist to spell out when your baby needs to be burped, there are burping tricks that can help you out. We’ve put together a plan that supports you in how to burp, find the best burping position, and when to stop burping your baby.
Table of Contents
- When to burp your baby
- When do you stop burping a baby
- How long do you have to burp a baby
- Signs a baby needs to burp
- What if my baby won’t burp after feeding
- Burping methods
- What if burping isn’t effective
- Baby Burping Tricks
- How to burp a baby with reflux
- When can you stop burping a baby with reflux
- When can I stop burping my baby at night?
- At what age do I stop burping my baby completely
When to burp your baby
Dr. Amna Husain, Pediatrician and Bobbie Medical Advisor, says burping is the most helpful during the first two to three months of your baby’s life. There’s not an exact manual for burping a newborn but there are moments when burping is most effective. For breastfed babies, Dr. Husain suggests burping your little one when switching breasts, and if you’re bottle-feeding your baby, squeeze in (or out) a burping session during the first few ounces of feeding. Dr Amna created a video about burping babies to share her advice and baby burping positions pictures.
Amna Husain, Pediatrician and Bobbie Medical Advisor, says burping is the most helpful during the first two to three months of your baby’s life. There’s not an exact manual for burping a newborn but there are moments when burping is most effective. For breastfed babies, Dr. Husain suggests burping your little one when switching breasts, and if you’re bottle-feeding your baby, squeeze in (or out) a burping session during the first few ounces of feeding. Dr Amna created a video about burping babies to share her advice and baby burping positions pictures.
When do you stop burping a baby
There’s no set age to stop burping your baby, but four to six months seems to be the general time frame. “Once your baby is able to move (sit up, rollover) they may not need to be burped,” Dr. Husain begins, “they may even burp themselves as mobilization of air occurs with movement.”
How long do you have to burp a baby
Throughout the first two to three months of your newborn’s life, they’ll need to be burped. Dr. Husain says when your baby is swallowing formula or milk they’re also potentially taking in air. “A baby’s stomach is pretty small in the first couple of days to weeks. When your baby takes in lots of air, it can impact the way they feel. This can cause an uncomfortable feeling of distention in the tummy area and influence how well and how much milk/formula they’re able to drink,” Dr. Husain says. So, in the first days, weeks, and months of your baby’s life burping is super helpful.
Dr. Husain says when your baby is swallowing formula or milk they’re also potentially taking in air. “A baby’s stomach is pretty small in the first couple of days to weeks. When your baby takes in lots of air, it can impact the way they feel. This can cause an uncomfortable feeling of distention in the tummy area and influence how well and how much milk/formula they’re able to drink,” Dr. Husain says. So, in the first days, weeks, and months of your baby’s life burping is super helpful.
When can you stop burping a baby
All babies are different, so their needs will vary. But you can start listening for the soothing sounds of your baby belching all by themselves around the four-month mark.
As your baby grows, you’ll begin to notice signs all your baby’s own that they need to burp. Some babies grow fidgety, move their legs closer to their chest, or even make odd facial expressions. Then there are some signals babies have in common. Dr. Husain suggests looking out for these four universal hints your baby is ready to assume their favorite burping position:
- Crying or fussy
- Not feeding comfortably
- Difficulty latching
- Pulling away from the bottle and/or breast
What if my baby won’t burp after feeding
There’s no reason to force a burp— especially after 10 to 15 minutes of trying, Dr.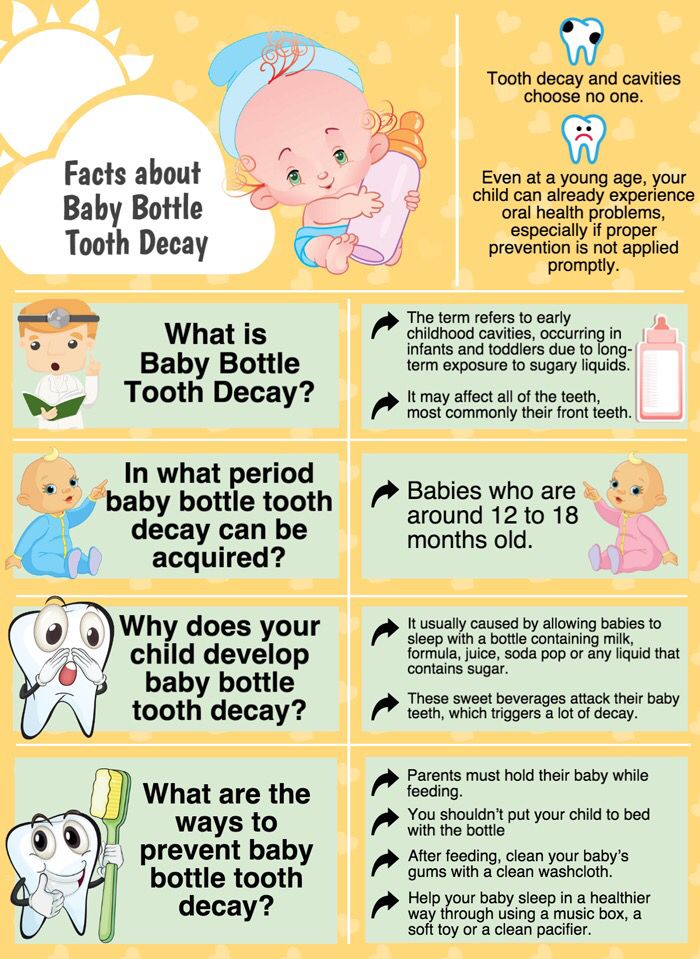 Husain says. If your baby is having a tough time burping, you can always try different burping positions/methods to see if this change will coax out that additional air.
Husain says. If your baby is having a tough time burping, you can always try different burping positions/methods to see if this change will coax out that additional air.
Burping methods
1. Over the shoulder: This is the most popular method and you start by sitting up and placing your infant on their tummy against your chest. This provides a comfortable “counter-pressure” on your baby’s belly. For a newborn who can’t support their head (or if you have a slightly sleeping baby), let their chin rest on your shoulder— but grab your burp cloth for unexpected spit-ups! For infants who can raise their heads, Dr. Husain suggests placing the baby so their head is over your shoulder. “If your baby spits up a lot, the spit-up will go over your shoulder rather than on your clothes,” she says.
2. Sitting Up: This is Dr. Husain’s preferred position because “it’s easy to do and not so tough on the body.” With your baby sitting upright on your lap, find a good “c-hold” with your hand around their jaw and underneath their ears (this supports a newborn’s head. ) Lean your infant forward slightly and to pat your baby, Dr. Husain encourages firm pats (versus gentle patting) higher on the baby’s back for better burping results.
) Lean your infant forward slightly and to pat your baby, Dr. Husain encourages firm pats (versus gentle patting) higher on the baby’s back for better burping results.
3. Laying on lap: Lay your baby on their stomach across your lap and let the back-patting begin. You can give your baby’s head a little extra support with your free hand if needed. You should know, Dr. Husain says, that this isn’t her favorite position because it can lead to more vomiting and she finds many babies aren’t a fan of this position.
What if burping isn’t effective
There are times when you’ve tried all the burping positions and even sung a few choruses of Bon Jovi’s Livin’ On A Prayer for good measure and still your baby cries loud enough for your neighbors to hear. Dr. Husain reassures us that if your baby is resisting a burp, there are baby burping tricks you can try and it’s good to note breastfed babies require less burping than bottle-fed babies.
Baby Burping Tricks
1. Baby massage: Dr. Husain says baby massage is a way to encourage some big ol’ burps. Baby massage can help calm and soothe your little one.
2. Walk around: Dr. Husain advises to get in your steps with your baby before (or during) burping. “The change of pace and change of scenery allows them to relax,” she says.
3. Feed more: If your baby is still fussy after burping, Dr. Husain suggests feeding your infant a little more so they have a fuller stomach. “I’ve seen this work!” she says.
How to burp a baby with reflux
If your baby has been diagnosed with infant reflux, you’ll notice them spitting up frequently, being cranky after eating, and possibly projectile vomiting. The Mayo Clinic reassures reflux generally isn’t cause for concern— only for investing in many more burp cloths. When burping a baby with reflux, the same rules apply although Dr. Husain suggests burping more frequently.
When can you stop burping a baby with reflux
Babies with reflux also begin to burp on their own as they move into their fourth month, Dr. Husain says.
When can I stop burping my baby at night?
Ending your middle-of-the-night burping sessions can occur around two to three months. Dr. Husain does mention that if you’re dream feeding (a practice where a caregiver/parent wakes baby to feed them when not fully awake) you should know it isn’t always necessary to burp. “Your baby may be more relaxed and take in less air in general during the feed,” Dr. Husain says.
At what age do I stop burping my baby completely
While all babies will grow and develop at their own pace, the general rule is that anywhere from four to six months, your baby will outgrow the need to be burped. Once your baby is able to roll over which is around four months, and then sit up which happens close to six months, your baby will more than likely burp themselves.
Now that you have all the tricks of the burping trade, you can discover which ones work best for your little one–until then don’t forget to stock up on the best burp cloths!
The content on this site is for informational purposes only and not intended to be a substitute for professional medical advice, diagnosis or treatment. Discuss any health or feeding concerns with your infant's pediatrician. Never disregard professional medical advice or delay it based on the content on this page.
Discuss any health or feeding concerns with your infant's pediatrician. Never disregard professional medical advice or delay it based on the content on this page.
Preventive measures against regurgitation in children
08.03.2017
Regurgitation is the spontaneous reflux of gastric contents into the esophagus and mouth. This condition is not uncommon in infants and is often a cause for concern for parents. The frequency of regurgitation syndrome in children of the first year of life is 18-50%: up to 4 months - 67%, up to 6 months 24%, up to 1 year 5%. In most cases, regurgitation is "benign" and disappears on its own after 12-18 months. At the same time, “benign” or physiological regurgitation characterizes:
-
the age of the child is up to 12 months;
-
spitting up 2 or more times a day for 3 or more weeks;
-
sufficient weight gain;
The child has no signs of metabolic disorders, diseases of the gastrointestinal tract or the central nervous system. The child does not experience difficulty in swallowing or feeding, there is no forced position of the body.
The child does not experience difficulty in swallowing or feeding, there is no forced position of the body.
Do not confuse regurgitation with vomiting. When a child burps, the abdominal muscles do not tense up. With vomiting, on the contrary, muscle tension occurs and food is ejected by pressure not only through the mouth, but also through the nose. In some cases, there may be general anxiety, pallor, cold extremities. Often with vomiting, the temperature rises, loose stools appear, which is a sign of an infectious disease. Vomit may contain unchanged milk, mucus, blood or bile.
What explains physiological regurgitation
What is the tendency of babies to spit up? This phenomenon is explained by the peculiarity of the structure of the gastrointestinal tract of young children. At the age of one year, the esophagus is shorter and wider, physiological narrowing is weakly expressed. The stomach is located horizontally, its capacity is small, and the muscles that close the entrance to the stomach and prevent the contents from being thrown back into the esophagus are poorly developed. As the child begins to walk, the axis of the stomach becomes more vertical. The capacity of the stomach increases by the year from 30-35 ml to 250-300 ml. The secretory apparatus matures, the work of the closing muscles (sphincters) improves, which leads to a gradual decrease in the frequency and disappearance of regurgitation. These features explain the predisposition of young children to regurgitation and even the inevitability of this condition. However, there are measures to help reduce the frequency of regurgitation.
As the child begins to walk, the axis of the stomach becomes more vertical. The capacity of the stomach increases by the year from 30-35 ml to 250-300 ml. The secretory apparatus matures, the work of the closing muscles (sphincters) improves, which leads to a gradual decrease in the frequency and disappearance of regurgitation. These features explain the predisposition of young children to regurgitation and even the inevitability of this condition. However, there are measures to help reduce the frequency of regurgitation.
Factors contributing to physiological regurgitation include:
-
Overfeeding. As a rule, actively sucking babies begin to suffer from overfeeding, with abundant milk secretion, as well as when switching to artificial or mixed feeding with an incorrect calculation of the required amount of milk formula. Regurgitation appears immediately or some time after feeding in the amount of 5-10 ml. Milk can flow out unchanged or curdled.
-
Swallowing air during feeding (aerophagia).
 A similar situation arises if the child suckles greedily at the breast, and the mother's milk is not very plentiful; due to the retracted, flat nipple of the mother's breast, since the child fails to fully capture the nipple and areola; with artificial feeding, if the hole at the nipple of the bottle is large enough or the nipple is not completely filled with milk. Babies with aerophagia often experience anxiety after feeding, bulging of the abdominal wall (belly inflates). After 10-15 minutes, the swallowed milk flows out unchanged, which is accompanied by a loud sound of air eructation.
A similar situation arises if the child suckles greedily at the breast, and the mother's milk is not very plentiful; due to the retracted, flat nipple of the mother's breast, since the child fails to fully capture the nipple and areola; with artificial feeding, if the hole at the nipple of the bottle is large enough or the nipple is not completely filled with milk. Babies with aerophagia often experience anxiety after feeding, bulging of the abdominal wall (belly inflates). After 10-15 minutes, the swallowed milk flows out unchanged, which is accompanied by a loud sound of air eructation. -
Intestinal colic or constipation. These conditions lead to an increase in pressure in the abdominal cavity and a violation of the movement of food through the gastrointestinal tract, causing regurgitation.
Until the child is four months old, spitting up up to two teaspoons of milk after feeding, or one spitting up of more than three spoons during the day, is considered the norm. You can check the amount of spitting up in the following way: take a diaper, pour one teaspoon of water on its surface, and then compare this spot with the spot formed after the next spitting up.
You can check the amount of spitting up in the following way: take a diaper, pour one teaspoon of water on its surface, and then compare this spot with the spot formed after the next spitting up.
Pathological regurgitation may be due to:
-
surgical diseases and malformations of the digestive system;
-
diaphragmatic hernia;
-
pathology of the central nervous system, trauma of the cervical spine during childbirth;
-
food intolerance, lactase deficiency;
-
increased intracranial pressure.
Such regurgitation is characterized by intensity, systematicity, the child spits up a large amount of milk. At the same time, there is a violation of the general condition of the baby - the child is whiny, loses or does not gain weight, cannot eat the amount of food necessary for his age. In such a situation, a pediatrician, gastroenterologist, surgeon, allergist, neurologist should be examined. It also requires examination and exclusion of anomalies in the structure of the upper gastrointestinal tract, the preservation of regurgitation for more than 1 year.
It also requires examination and exclusion of anomalies in the structure of the upper gastrointestinal tract, the preservation of regurgitation for more than 1 year.
Scale for assessing the intensity of regurgitation:
-
Less than 5 regurgitations per day with a volume of not more than 3 ml - 1 point.
-
More than 5 regurgitations per day with a volume of more than 3 ml - 2 points.
-
More than 5 regurgitations per day up to half the amount of formula or breast milk, not more often than in half of the feedings - 3 points.
-
Spitting up a small amount of milk for 30 minutes or more after each feeding - 4 points.
-
Regurgitation from half to full volume of formula or breast milk in at least half of the feedings - 5 points.
Regurgitation with an intensity of 3 or more points requires a visit to a doctor.
Preventive measures against regurgitation in children
If regurgitation is physiological in nature, then it is not worth treating or correcting in this case. It is necessary to deal with the elimination of the cause, if possible, and carry out prevention.
It is necessary to deal with the elimination of the cause, if possible, and carry out prevention.
Prevention of regurgitation in children includes the following measures:
-
Postural therapy: when feeding, it is necessary to hold the baby at an angle of 45 °, make sure that he completely grasps the nipple with the areola; after feeding, hold the baby in an upright position ("column") for 20 minutes - to drain the swallowed air. Due to this, the air that has entered the stomach will be able to go out. If nothing happened, then put the baby down and after a minute or two, lift him upright again.
-
Make sure that the opening in the bottle is not too large and that the nipple is filled with milk. Experiment with nipples - perhaps the other will be better. Milk should come out in drops, not a trickle.
-
Before you start feeding your baby, lay him belly down on a solid base.
-
After feeding, try to minimize the baby's physical activity, do not disturb him unnecessarily, and change clothes only if there is an emergency.
-
Avoid squeezing diapers or clothes on the abdomen of the child.
-
If the baby's appetite is good, then it is better to feed him often, but in small portions, otherwise, due to the large amount of food, the stomach may overflow, and this, as a result, leads to regurgitation of excess food.
-
The surface in the bed on which the baby lies should rise 10 cm at the head.
-
In addition, it is possible to use special "thickeners" of milk or anti-reflux mixtures, which the doctor will help you choose.
In the event that regurgitation begins to become more frequent or becomes abundant, or first began after six months of the baby's life, or does not subside by one and a half to two years of life, the child should be consulted by a pediatrician. With a high probability, additional help from a gastroenterologist will be needed.
In our Family Medical Center you can always find highly professional help.
← Back to the list of articles
How to help the baby when regulating
Support Support iconKeywords for searching
Home Home ›!! How to help a child in sprinkling
HOW HOLIDAY ›› How to help a child in spitting 9000 a very special time for a mother and her newborn baby. Together with the feeling of closeness and affection that feeding brings, understanding its nuances cannot but raise many questions, including the question of how to help an infant spit up. Regurgitation in a newborn is by no means always the result of a simple pat on his back.
In this article, we'll talk about the basics of helping a newborn spit up, as well as other questions you may have about spitting up.
Why do babies spit up?
Let's get it straight: Why do newborns need to burp in the first place? During feeding, children usually swallow extra air - this is called aerophagia. Spitting up helps prevent this air from entering the intestines, as well as vomiting, gas, and crankiness in the baby. To avoid the return of milk after feeding, you should give the baby the opportunity to burp more often.
To avoid the return of milk after feeding, you should give the baby the opportunity to burp more often.
How to help a newborn spit up?
During the first six months, the baby should be kept upright in a column for 10-15 minutes after each feed. This will help keep the milk in his stomach, but if the baby occasionally burps anyway, parents need not worry. While carrying your baby in an upright position, you can put a baby diaper or wipes on your shoulder to keep your clothes clean.
We've already seen why spitting up is important, now let's find out how to help your baby spit up. Parents should gently pat the baby on the back with a hand folded in a handful until he burps. Folding your hand into a handful is important because clapping with a flat palm may be too strong for an infant.
Every baby is different and there is no one right position for spitting up. To get started, you can try the following options:
- Sitting position with the baby on the chest.
 In this position, the parent puts the baby's head with his chin on his shoulder and with one hand supports the baby under the back. With the other hand, you can gently pat the baby on the back. This method is most effective in a rocking chair or when the baby is gently rocking.
In this position, the parent puts the baby's head with his chin on his shoulder and with one hand supports the baby under the back. With the other hand, you can gently pat the baby on the back. This method is most effective in a rocking chair or when the baby is gently rocking. - Holding a child upright on one's legs. With one hand, parents can hold the baby by the back and head, supporting his chin and placing his palm on the baby’s chest, with the other hand, you can gently pat him on the back. At the same time, it is important to be careful: do not press the child on the throat, but only gently support his chin.
- Holding a baby on your lap while lying on your tummy. Make sure his head is above his chest and gently pat your baby on the back until he burps.
Here are some tips on how best to help your newborn spit up:
- Let your baby spit up while feeding. If the baby is restless or has swallowed air, it is worth giving him the opportunity to burp during feeding, and not just after.

- When bottle feeding, let the newborn burp after every 50-60 ml.
- When breastfeeding, let the baby burp at every breast change.
It is important to let your baby spit up after eating, even if he spit up during feeding!
If your baby is gassy, spit up more often. Also, if he vomits frequently or suffers from gastroesophageal reflux disease (GERD), have him spit up after every 30 ml bottle-feeding or every five minutes while breastfeeding.
How long should a baby be held for it to burp? It's different for everyone, but generally keeping a newborn upright for 15 to 20 minutes after a feed helps the milk stay in the baby's stomach.
Minimize the amount of air you swallow. Gas production and regurgitation result from aerophagia during feeding. The baby will inevitably swallow air, but there are ways to prevent it from swallowing too much. Whether you bottle feed your baby or combine breastfeeding with bottle feeding, the Philips Avent anti-colic bottle with AirFree valve is designed so that the nipple is always filled with milk without excess air, even in a horizontal position, thus preventing the baby from swallowing excess air during feeding.