Babies and breast feeding
Breastfeeding FAQs: How Much and How Often (for Parents)
Breastfeeding is a natural thing to do, but it still comes with its fair share of questions. Here's what you need to know about how often and how long to breastfeed your baby.
How Often Should I Breastfeed?
Newborn babies should breastfeed 8–12 times per day for about the first month. Breast milk is easily digested, so newborns are hungry often. Frequent feedings helps stimulate your milk production during the first few weeks.
By the time your baby is 1–2 months old, he or she probably will nurse 7–9 times a day.
In the first few weeks of life, breastfeeding should be "on demand" (when your baby is hungry), which is about every 1-1/2 to 3 hours. As newborns get older, they'll nurse less often, and may have a more predictable schedule. Some might feed every 90 minutes, whereas others might go 2–3 hours between feedings.
Newborns should not go more than about 4 hours without feeding, even overnight.
How Do I Count the Time Between Feedings?
Count the length of time between feedings from the time your baby begins to nurse (rather than at the end) to when your little one starts nursing again. In other words, when your doctor asks how often your baby is feeding, you can say "about every 2 hours" if your first feeding started at 6 a.m., the next feeding was around 8 a.m., then 10 a.m., and so on.
Especially at first, you might feel like you're nursing around the clock, which is normal. Soon enough, your baby will go longer between feedings.
How Long Does Nursing Take?
Newborns may nurse for up to 20 minutes or longer on one or both breasts. As babies get older and more skilled at breastfeeding, they may take about 5–10 minutes on each side.
How long it takes to breastfeed depends on you, your baby, and other things, such as whether:
- your milk supply has come in (this usually happens 2–5 days after birth)
- your let-down reflex (which causes milk to flow from the nipple) happens right away or after a few minutes into a feeding
- your milk flow is slow or fast
- the baby has a good latch, taking in as much as possible of your areola (the dark circle of skin around your nipple)
- your baby begins gulping right away or takes it slow
- your baby is sleepy or distracted
Call your doctor if you're worried that your baby's feedings seem too short or too long.
When Should I Alternate Breasts?
Alternate breasts and try to give each one the same amount of nursing time throughout the day. This helps to keep up your milk supply in both breasts and prevents painful engorgement (when your breasts overfill with milk).
You may switch breasts in the middle of each feeding and then alternate which breast you offer first for each feeding. Can't remember where your baby last nursed? It can help to attach a reminder — like a safety pin or small ribbon — to your bra strap so you'll know which breast your baby last nursed on. Then, start with that breast at the next feeding. Or, keep a notebook handy or use a breastfeeding app to keep track of how your baby feeds.
Your baby may like switching breasts at each feeding or prefer to nurse just on one side. If so, then offer the other breast at the next feeding. Do whatever works best and is the most comfortable for you and your baby.
How Often Should I Burp My Baby During Feedings?
After your baby finishes on one side, try burping before switching breasts. Sometimes, the movement alone can be enough to cause a baby to burp.
Sometimes, the movement alone can be enough to cause a baby to burp.
Some infants need more burping, others less, and it can vary from feeding to feeding.
If your baby spits up a lot, try burping more often. While it's normal for infants to "spit up" a small amount after eating or during burping, a baby should not vomit after feeding. If your baby throws up all or most of a feeding, there could be a problem that needs medical care. If you're worried that your baby is spitting up too much, call your doctor.
Why Is My Baby Hungrier Than Usual?
When babies go through a period of rapid growth (called a growth spurt), they want to eat more than usual. These can happen at any time. But in the early months, growth spurts often happen when a baby is:
- 7–14 days old
- 2 months old
- 4 months old
- 6 months old
During these times and whenever your baby seems extra hungry, follow your little one's hunger cues. You may need to breastfeed more often for a while.
How Long Should I Breastfeed My Baby?
That's a personal choice. Experts recommend that babies be breastfed exclusively (without formula, water, juice, non–breast milk, or food) for the first 6 months. Then, breastfeeding can continue until 12 months (and beyond) if it's working for you and your baby.
Breastfeeding has many benefits for mom and baby both. Studies show that breastfeeding can lessen a baby's chances of diarrhea, ear infections, and bacterial meningitis, or make symptoms less severe. Breastfeeding also may protect children from sudden infant death syndrome (SIDS), diabetes, obesity, and asthma.
For moms, breastfeeding burns calories and helps shrink the uterus. In fact, breastfeeding moms might return to their pre–pregnancy shape and weight quicker. Breastfeeding also helps lower a woman's risk of diseases like:
- breast cancer
- high blood pressure
- diabetes
- heart disease
It also might help protect moms from uterine cancer and ovarian cancer.
The Benefits of Breastfeeding for Both Mother and Baby
Written by Rebecca Buffum Taylor
Reviewed by Dan Brennan, MD on July 05, 2022
In this Article
- What is Breastfeeding?
- Signs Your Baby is Hungry
- Benefits of Breastfeeding for the Baby
- Breastfeeding Benefits for the Mother
- Will You Make Enough Milk to Breastfeed?
- What's the Best Position for Breastfeeding?
- How to Get Your Baby to 'Latch on' During Breastfeeding
- Tips for New Breastfeeding Moms
- Are There Medical Considerations With Breastfeeding?
- What Are Some Common Challenges With Breastfeeding?
- Where Can I Get Help With Breastfeeding?
What is Breastfeeding?
Breastfeeding is when you feed your baby breast milk, usually directly from your breast. It’s also called nursing. Making the decision to breastfeed is a personal matter. It's also one that's likely to draw opinions from friends and family.
Many medical experts, including the American Academy of Pediatrics (AAP) and the American College of Obstetricians and Gynecologists, strongly recommend breastfeeding exclusively (no formula, juice, or water) for 6 months. After the introduction of other foods, it recommends continuing to breastfeed through the baby’s first year of life.
How often you should breastfeed your baby depends on whether your baby prefers small, frequent meals or longer feedings. This will change as your baby grows. Newborns often want to feed every 2-3 hours. By 2 months, feeding every 3-4 hours is common, and by six months, most babies feed every 4-5 hours.
You and your baby are unique, and the decision to breastfeed is up to you.
Signs Your Baby is Hungry
One of the most common ways your baby will let you know they're hungry is to cry. Other signs your baby is ready to be fed include:
- Licking their lips or sticking out their tongue
- Rooting, which is moving their jaw, mouth, or head to look for your breast
- Putting their hand in their mouth
- Opening their mouth
- Fussiness
- Sucking on things
Benefits of Breastfeeding for the Baby
Breast milk provides the ideal nutrition for infants. It has a nearly perfect mix of vitamins, protein, and fat -- everything your baby needs to grow. And it's all provided in a form more easily digested than infant formula. Breast milk contains antibodies that help your baby fight off viruses and bacteria. Breastfeeding lowers your baby's risk of having asthma or allergies. Plus, babies who are breastfed exclusively for the first 6 months, without any formula, have fewer ear infections, respiratory illnesses, and bouts of diarrhea. They also have fewer hospitalizations and trips to the doctor.
It has a nearly perfect mix of vitamins, protein, and fat -- everything your baby needs to grow. And it's all provided in a form more easily digested than infant formula. Breast milk contains antibodies that help your baby fight off viruses and bacteria. Breastfeeding lowers your baby's risk of having asthma or allergies. Plus, babies who are breastfed exclusively for the first 6 months, without any formula, have fewer ear infections, respiratory illnesses, and bouts of diarrhea. They also have fewer hospitalizations and trips to the doctor.
Breastfeeding has been linked to higher IQ scores in later childhood in some studies. What's more, the physical closeness, skin-to-skin touching, and eye contact all help your baby bond with you and feel secure. Breastfed infants are more likely to gain the right amount of weight as they grow rather than become overweight children. The AAP says breastfeeding also plays a role in the prevention of SIDS (sudden infant death syndrome). It's been thought to lower the risk of diabetes, obesity, and certain cancers as well, but more research is needed.
The AAP says breastfeeding also plays a role in the prevention of SIDS (sudden infant death syndrome). It's been thought to lower the risk of diabetes, obesity, and certain cancers as well, but more research is needed.
Breastfeeding Benefits for the Mother
Breastfeeding burns extra calories, so it can help you lose pregnancy weight faster. It releases the hormone oxytocin, which helps your uterus return to its pre-pregnancy size and may reduce uterine bleeding after birth. There are continued benefits from breastfeeding beyond 1 year, and up to 2 years especially in the mother.Breastfeeding also lowers your risk of breast and ovarian cancer. It may lower your risk of osteoporosis, too.
Since you don't have to buy and measure formula, sterilize nipples, or warm bottles, it saves you time and money. It also gives you regular time to relax quietly with your newborn as you bond.
Will You Make Enough Milk to Breastfeed?
The first few days after birth, your breasts make an ideal "first milk." It's called colostrum. Colostrum is thick, yellowish, and there’s not a lot of it, but there's plenty to meet your baby's nutritional needs. Colostrum helps a newborn's digestive tract develop and prepare itself to digest breast milk.
Colostrum is the first phase of breast milk, which changes over time to give your baby the nutrition they need as they grow. The second phase is called transitional milk. You make this as your colostrum is gradually replaced with the third phase of breast milk, called mature milk.
You’ll start to make transitional milk a few days after birth. By 10 to 15 days after birth, you’ll make mature milk, which gives your baby all the nutrition they need.
Most babies lose a small amount of weight in the first 3 to 5 days after birth. This is unrelated to breastfeeding.
As your baby needs more milk and nurses more, your breasts respond by making more milk. Experts recommend trying to breastfeed exclusively (no formula, juice, or water) for 6 months. If you supplement with formula, your breasts might make less milk.
Experts recommend trying to breastfeed exclusively (no formula, juice, or water) for 6 months. If you supplement with formula, your breasts might make less milk.
Even if you breastfeed less than the recommended 6 months, it's better to breastfeed for a short time than no time at all. You can add solid food at 6 months but also continue to breastfeed if you want to keep producing milk.
Is your baby getting enough milk?
Many breastfeeding moms wonder whether their babies get enough milk for good nutrition. If your baby is getting enough breastmilk they should:
- Not lose more than 7% of their birth weight in the first few days after delivery
- Seem content for about 1-3 hours between feedings
- Have at least 6 diapers a day wet with very pale or clear pee by the time they are 7-10 days old
What's the Best Position for Breastfeeding?
The best position for you is the one where you and your baby are both comfortable and relaxed, and you don't have to strain to hold the position or keep nursing. Here are some common positions for breastfeeding your baby:
Here are some common positions for breastfeeding your baby:
- Cradle position. Rest the side of your baby's head in the crook of your elbow with their whole body facing you. Position your baby's belly against your body so they feel fully supported. Your other, "free" arm can wrap around to support your baby's head and neck -- or reach through your baby's legs to support the lower back.
- Football position. Line your baby's back along your forearm to hold your baby like a football, supporting the head and neck in your palm. This works best with newborns and small babies. It's also a good position if you're recovering from a cesarean birth and need to protect your belly from the pressure or weight of your baby.
- Side-lying position. This position is great for night feedings in bed. Side-lying also works well if you're recovering from an episiotomy, an incision to widen the vaginal opening during delivery. Use pillows under your head to get comfortable.
 Then snuggle close to your baby and use your free hand to lift your breast and nipple into your baby's mouth. Once your baby is correctly "latched on," support the head and neck with your free hand so there's no twisting or straining to keep nursing.
Then snuggle close to your baby and use your free hand to lift your breast and nipple into your baby's mouth. Once your baby is correctly "latched on," support the head and neck with your free hand so there's no twisting or straining to keep nursing. - Cross-cradle hold. Sit straight in a comfortable chair that has armrests. Hold your baby in the crook of your arm that's opposite the breast you will use to feed them. Support their head with your hand. Bring your baby across your body so your tummies face each other. Use your other hand to cup your breast in a U-shaped hold. Bring your baby's mouth to your breast and cradle them close, and don't lean forward.
- Laid-back position. This position, also called biological nurturing, is a lot like it sounds. It's meant to tap into the natural breastfeeding instincts you and your baby have. Lean back, but not flat, on a couch or bed. Have good support for your head and shoulders. Hold your baby so your entire fronts touch.
 Let your baby take any position they're comfortable in as long as their cheek rests near your breast. Help your baby latch on if they need it.
Let your baby take any position they're comfortable in as long as their cheek rests near your breast. Help your baby latch on if they need it.
How to Get Your Baby to 'Latch on' During Breastfeeding
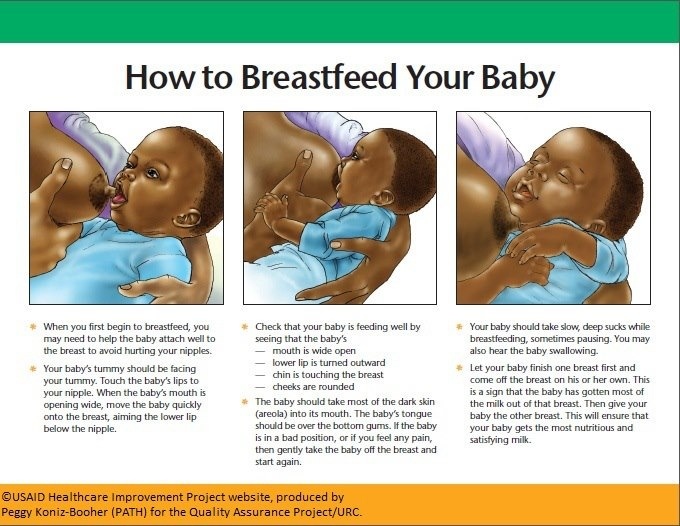
Position your baby facing you, so your baby is comfortable and doesn't have to twist their neck to feed. With one hand, cup your breast and gently stroke your baby's lower lip with your nipple. Your baby's instinctive reflex will be to open the mouth wide. With your hand supporting your baby's neck, bring the mouth closer around your nipple, trying to center your nipple in the mouth above the tongue.
You'll know your baby is "latched on" correctly when both lips are pursed outward around your nipple. Your infant should have all of your nipple and most of the areola, which is the darker skin around your nipple, in their mouth. While you may feel a slight tingling or tugging, breastfeeding should not be painful. If your baby isn't latched on correctly and nursing with a smooth, comfortable rhythm, gently nudge your pinky between your baby's gums to break the suction, remove your nipple, and try again. Good "latching on" helps prevent sore nipples.
Tips for New Breastfeeding Moms
Some things help you prepare for breastfeeding:
- Get regular prenatal care to help you avoid preterm birth.
- Tell your doctor you plan to breastfeed and ask what support the facility you plan to deliver in offers to help you breastfeed after birth.
- Take a breastfeeding class.
- Ask your doctor to connect you with a lactation consultant, who can teach you breastfeeding basics and help you if have issues.
- Talk to your doctor about any health conditions you have or medications you take that could interfere with breastfeeding.
- Tell your doctor and hospital health care providers that you want to breastfeed as soon as possible after delivery.
- Talk to friends who breastfeed or join a support group for breastfeeding.
- Stock up on the supplies you need for breastfeeding, such as nursing bras and other items.
These tips, called the ABCs of breastfeeding, will help you and your baby get comfortable with the process:
- Awareness.
 Watch for your baby's signs of hunger, and breastfeed whenever your baby is hungry. This is called "on demand" feeding. The first few weeks, you may be nursing eight to 12 times every 24 hours. Hungry infants move their hands toward their mouths, make sucking noises or mouth movements, or move toward your breast. Don't wait for your baby to cry. That's a sign their too hungry.
Watch for your baby's signs of hunger, and breastfeed whenever your baby is hungry. This is called "on demand" feeding. The first few weeks, you may be nursing eight to 12 times every 24 hours. Hungry infants move their hands toward their mouths, make sucking noises or mouth movements, or move toward your breast. Don't wait for your baby to cry. That's a sign their too hungry. - Be patient. Breastfeed as long as your baby wants to nurse each time. Don't hurry your infant through feedings. Infants typically breastfeed for 10 to 20 minutes on each breast.
- Comfort. This is key. Relax while breastfeeding, and your milk is more likely to "let down" and flow. Get yourself comfortable with pillows as needed to support your arms, head, and neck, and a footrest to support your feet and legs before you begin to breastfeed.
Are There Medical Considerations With Breastfeeding?
In a few situations, breastfeeding could cause a baby harm. Here are some reasons you should not breastfeed:
Here are some reasons you should not breastfeed:
- You are HIV positive. You can pass the HIV virus to your infant through breast milk.
- You have active, untreated tuberculosis.
- You're receiving chemotherapy for cancer.
- You're using an illegal drug, such as cocaine or marijuana.
- Your baby has a rare condition called galactosemia and cannot tolerate the natural sugar, called galactose, in breast milk.
- You're taking certain prescription medications, such as some drugs for migraine headaches, Parkinson's disease, or arthritis.
Talk with your doctor before starting to breastfeed if you're taking prescription drugs of any kind. Your doctor can help you make an informed decision based on your particular medication.
Having a cold or flu should not prevent you from breastfeeding. Breast milk won't give your baby the illness and may even give antibodies to your baby to help fight off the illness.
Breast milk won't give your baby the illness and may even give antibodies to your baby to help fight off the illness.
Also, the AAP suggests that -- starting at 4 months of age -- exclusively breastfed infants, and infants who are partially breastfed and receive more than half of their daily feedings as human milk, should be supplemented with oral iron. This should continue until foods with iron, such as iron-fortified cereals, are introduced in the diet. The AAP recommends checking iron levels in all children at age 1.
Discuss supplementation of both iron and vitamin D with your pediatrician. Your doctor can guide you on recommendations about the proper amounts for both your baby and you, when to start, and how often the supplements should be taken.
What Are Some Common Challenges With Breastfeeding?
- Sore nipples. You can expect some soreness in the first weeks of breastfeeding. Make sure your baby latches on correctly, and use one finger to break the suction of your baby's mouth after each feeding.
 That will help prevent sore nipples. If you still get sore, be sure you nurse with each breast fully enough to empty the milk ducts. If you don't, your breasts can become engorged, swollen, and painful. Holding ice or a bag of frozen peas against sore nipples can temporarily ease discomfort. Keeping your nipples dry and letting them "air dry" between feedings helps, too. Your baby tends to suck more actively at the start. So begin feedings with the less-sore nipple.
That will help prevent sore nipples. If you still get sore, be sure you nurse with each breast fully enough to empty the milk ducts. If you don't, your breasts can become engorged, swollen, and painful. Holding ice or a bag of frozen peas against sore nipples can temporarily ease discomfort. Keeping your nipples dry and letting them "air dry" between feedings helps, too. Your baby tends to suck more actively at the start. So begin feedings with the less-sore nipple. - Dry, cracked nipples. Avoid soaps, perfumed creams, or lotions with alcohol in them, which can make nipples even more dry and cracked. You can gently apply pure lanolin to your nipples after a feeding, but be sure you gently wash the lanolin off before breastfeeding again. Changing your bra pads often will help your nipples stay dry. And you should use only cotton bra pads.
- Worries about producing enough milk. A general rule of thumb is that a baby who's wetting six to eight diapers a day is most likely getting enough milk.
 It's best not to supplement your breast milk with formula, and never give your infant plain water. Your body needs the frequent, regular demand of your baby's nursing to keep producing milk. Some women mistakenly think they can't breastfeed if they have small breasts. But small-breasted women can make milk just as well as large-breasted women. Good nutrition, plenty of rest, and staying well hydrated all help, too.
It's best not to supplement your breast milk with formula, and never give your infant plain water. Your body needs the frequent, regular demand of your baby's nursing to keep producing milk. Some women mistakenly think they can't breastfeed if they have small breasts. But small-breasted women can make milk just as well as large-breasted women. Good nutrition, plenty of rest, and staying well hydrated all help, too. - Pumping and storing milk. You can get breast milk by hand or pump it with a breast pump. It may take a few days or weeks for your baby to get used to breast milk in a bottle. So begin practicing early if you're going back to work. Breast milk can be safely used within 2 days if it's stored in a refrigerator. You can freeze breast milk for up to 6 months. Don't warm up or thaw frozen breast milk in a microwave. That will destroy some of its immune-boosting qualities, and it can cause fatty portions of the breast milk to become super hot.
 Thaw breast milk in the refrigerator or in a bowl of warm water instead.
Thaw breast milk in the refrigerator or in a bowl of warm water instead. - Inverted nipples. An inverted nipple doesn't poke forward when you pinch the areola, the dark skin around the nipple. A lactation consultant -- a specialist in breastfeeding education -- can give you tips that allow women with inverted nipples to breastfeed successfully.
- Breast engorgement. Breast fullness is natural and healthy. It happens as your breasts become full of milk, staying soft and pliable. But breast engorgement means the blood vessels in your breast have become congested. This traps fluid in your breasts and makes them feel hard, painful, and swollen. Alternate heat and cold, for instance using ice packs and hot showers, to relieve mild symptoms. It can also help to release your milk by hand or use a breast pump.
- Blocked ducts. A single sore spot on your breast, which may be red and hot, can signal a plugged milk duct.
 This can often be relieved by warm compresses and gentle massage over the area to release the blockage. More frequent nursing can also help.
This can often be relieved by warm compresses and gentle massage over the area to release the blockage. More frequent nursing can also help. - Breast infection (mastitis). This occasionally results when bacteria enter the breast, often through a cracked nipple after breastfeeding. If you have a sore area on your breast along with flu-like symptoms, fever, and fatigue, call your doctor. Antibiotics are usually needed to clear up a breast infection, but you can most likely continue to breastfeed while you have the infection and take antibiotics. To relieve breast tenderness, apply moist heat to the sore area four times a day for 15 to 20 minutes each time.
- Stress. Being overly anxious or stressed can interfere with your let-down reflex. That's your body's natural release of milk into the milk ducts. It's triggered by hormones released when your baby nurses.
 It can also be triggered just by hearing your baby cry or thinking about your baby. Stay as relaxed and calm as possible before and during nursing -- it can help your milk let down and flow more easily. That, in turn, can help calm and relax your infant.
It can also be triggered just by hearing your baby cry or thinking about your baby. Stay as relaxed and calm as possible before and during nursing -- it can help your milk let down and flow more easily. That, in turn, can help calm and relax your infant. - Premature babies may not be able to breastfeed right away. In some cases, mothers can release breast milk and feed it through a bottle or feeding tube.
- Warning signs. Breastfeeding is a natural, healthy process. But call your doctor if:
- Your breasts become unusually red, swollen, hard, or sore.
- You have an unusual discharge or bleeding from your nipples.
- You're concerned your baby isn't gaining weight or getting enough milk.
Where Can I Get Help With Breastfeeding?
Images of mothers breastfeeding their babies make it look simple -- but some women need some help and coaching. It can come from a nurse, doctor, family member, or friend, and it helps mothers get over possible bumps in the road.
Reach out to friends, family, and your doctor with any questions you may have. Most likely, the women in your life have had those same questions.
Breastfeeding a newborn | What to Expect in the First Week
The first week of a baby's life is a wonderful but hectic time, especially if you haven't breastfed before. Our breastfeeding tips will help you settle in as quickly as possible
Share this information
The first time after childbirth, mothers are often confused. The body is still recovering, and you are already starting to get to know your newborn baby. The emotional state during this period can be unstable, especially between the second and fifth day, when many women have milk 1 and at the same time postpartum depression begins 2 . In addition, people around often expect (and demand) that a woman come to her senses as soon as possible and become a “super mom”. But the best thing to do this first week is just to be with your baby and get breastfeeding going.
When should I start breastfeeding my newborn?
Try to breastfeed your baby within the first hour after birth. When the baby latch onto the breast and begins sucking rhythmically, it stimulates the mammary gland cells and starts milk production. nine0009 1 It is not for nothing that this time is called the “magic hour”!
“Ideally, the baby should be placed on the mother's stomach immediately after birth so that it can immediately attach to the breast. He won't necessarily eat, but he should be able to,” explains Cathy Garbin, an internationally recognized expert on breastfeeding.
“Hold your baby and let him find the breast on his own and put the nipple in his mouth. This is called the breast-seeking reflex. On the Internet you can watch videos that show what this process looks like. If the baby does not latch onto the nipple on its own, the midwife will help to properly attach it to the breast. But for starters, it’s good to give the baby the opportunity to do it on their own. In this case, the optimal position for the mother is reclining. ” nine0003
In this case, the optimal position for the mother is reclining. ” nine0003
Don't spend that special first hour of your baby's life weighing and swaddling—or at least wait until he's suckling for the first time. Enjoy hugs and close skin-to-skin contact. This promotes the production of oxytocin, the hormone of love, in you and your baby, and oxytocin plays a key role in the supply of the first breast milk - colostrum. 3
“As soon as the obstetricians were convinced that our son was healthy, the three of us — me, my husband and our baby — were left to give us the opportunity to get to know each other. It was a very special hour - an hour of awkwardness, turbulent emotions and bliss. During this time, I breastfed my son twice, ”recalls Ellie, a mother of two from the UK. nine0003
Did you know that breastfeeding helps to recover after childbirth? This is because oxytocin stimulates uterine contractions. In the first hours after childbirth, this contributes to the natural release of the placenta and reduces blood loss. 4
4
What if the birth did not go according to plan?
If you had a cesarean section or other complications during childbirth,
You can still make skin-to-skin contact with your baby and breastfeed him in the first hours after birth. nine0003
“If you can't hold your baby, have your partner do it for you and make skin-to-skin contact with the baby. This will give the baby a sense of security, care and warmth so that he can hold on until you recover, ”Katie advises.
If the baby is unable to breastfeed, it is advisable to start expressing milk as early as possible and do so as often as possible until the baby is able to feed on its own. “While breastfeeding in the first hours after birth lays an excellent foundation for the future, it is not so important,” Cathy reassures. “It is much more important to start lactation so that in the future, if necessary, you can start breastfeeding.” nine0003
To start milk production, you can express milk manually or use a breast pump that can be given to you at the hospital. 5 And with expressed precious colostrum, it will be possible to feed the child. This is especially important if the baby was born premature or weak, since breast milk is extremely healthy.
5 And with expressed precious colostrum, it will be possible to feed the child. This is especially important if the baby was born premature or weak, since breast milk is extremely healthy.
If a baby was born prematurely or has a medical condition and cannot be breastfed immediately, this is no reason not to continue breastfeeding. “I have worked with many new mothers who were unable to breastfeed their baby for the first six weeks due to preterm labor or other reasons. Nevertheless, all of them later successfully switched to breastfeeding,” says Kathy. nine0003
Does the baby latch on correctly?
Correct breastfeeding is essential for successful breastfeeding 6 , as it determines how effectively the baby will suckle milk and hence grow and develop. Latching on the breast incorrectly can cause sore or damaged nipples, so don't hesitate to ask your doctor to check that your baby is properly attached to the breast, even if you are told that everything is fine and you do not see obvious problems - especially while you are in the hospital. nine0003
nine0003
“While I was in the hospital, I called the doctor at every feed and asked me to check if I was breastfeeding correctly,” says Emma, mother of two from Australia. - There were several cases when it seemed to me that everything seemed to be right, but it was painful to feed, and the doctor helped me take the baby off the breast and attach it correctly. By the time I was discharged, I had already learned to do it confidently.”
When applying to the breast, point the nipple towards the palate. This will allow the baby to take the nipple and part of the areola under it into their mouth. It will be easier for him to suck if he has both the nipple and part of the areola around in his mouth. nine0009 6
“When a baby latch on properly, it doesn't cause discomfort and it causes a pulling sensation, not pain,” Cathy explains. - The baby's mouth is wide open, the lower lip may be slightly turned outward, and the upper one lies comfortably on the chest. The body language of the child indicates that he is comfortable. There isn't much milk at this early stage, so you probably won't notice your baby swallowing, but he will suckle a lot and nurse frequently."
There isn't much milk at this early stage, so you probably won't notice your baby swallowing, but he will suckle a lot and nurse frequently."
How often should a newborn be fed? nine0015
The frequency and duration of breastfeeding in the first week can vary greatly. “The first 24 hours of life are completely different for different children. Someone sleeps a lot (after all, childbirth is tiring!), And someone often eats, says Katie. - Such a variety greatly confuses young mothers. Everyone gives different advice, so it's important to remember that every mother and child is different."
“Colostrum is thicker than mature breast milk and is produced in smaller amounts, but has many benefits. When the baby eats colostrum, he learns to suck, swallow and breathe until milk begins to flow in more volume, ”explains Cathy. nine0003
Milk usually arrives on the second or fourth day after birth. Until this time, the baby is applied to the breast 8-12 times a day (and sometimes more often!), including at night. 7 Feeding may last 10-15 minutes at this stage, or 45 minutes or even an hour, as the baby is just beginning to develop the muscles and coordination needed to suckle effectively.
7 Feeding may last 10-15 minutes at this stage, or 45 minutes or even an hour, as the baby is just beginning to develop the muscles and coordination needed to suckle effectively.
“At first, the intensity of feeding is very high, often higher than many people realize, and this is shocking to most new mothers,” says Cathy. - Sometimes mom has no time to go to the toilet, take a shower and have a snack. It usually comes as a surprise." nine0003
Camille, a mother from Australia, experienced this. “The first week, Frankie ate every two hours, day and night, and each time it took half an hour to an hour to feed,” she recalls. “My husband and I were completely exhausted!”
Do I need to feed my newborn on a schedule?
The good news is that frequent feeding promotes lactation and stimulates milk production. 7 The more your baby eats, the more milk you will have. Therefore, forget about feeding your newborn on a schedule - this way he will have less chance of feeding. Try to feed your baby when he signals that he is hungry 8 :
Try to feed your baby when he signals that he is hungry 8 :
- tossing and turning in her sleep;
- opens eyes;
- turns his head if he feels a touch on his cheek;
- sticks out tongue;
- groans;
- licks lips;
- sucks fingers;
- is naughty;
- whimpers;
- is crying.
Crying is the last sign of hunger, so when in doubt, just offer your baby the breast. If he bursts into tears, it will be more difficult to feed him, especially at first, when both of you are just learning how to do it. As your baby grows, he will likely eat less frequently and take less time to feed, so breastfeeding will seem more predictable. nine0003
Does breastfeeding hurt?
You may have heard that breastfeeding is not painful at all, but in fact, in the first days, many new mothers experience discomfort. And this is not at all surprising, given that the nipples are not used to such frequent and strong sucking.
“Breastfeeding can be uncomfortable for the first couple of days – your body and your baby are just getting used to it. If a baby eats for too long and does not latch well, the sensations are almost the same as from unworn new shoes, Cathy compares. Just as tight shoes can rub your feet, improper suckling can damage your nipples. Prevention is always better than cure, so if the pain persists after a few days of feeding, contact a lactation consultant or healthcare professional.” nine0003
Maria, a mother from Canada, agrees: “Although my son seemed to latch onto the breast well, he damaged his nipples while feeding, and I was in pain. As it turned out, the reason was a shortened frenulum of the tongue. The breastfeeding specialists at our city clinic have been of great help in diagnosis and treatment.”
In addition, you may experience period cramps during the first few days after breastfeeding, especially if this is not your first baby. This is the so-called postpartum pain. The fact is that oxytocin, which is released during breastfeeding, contributes to further contraction of the uterus to restore its normal size. nine0009 4
The fact is that oxytocin, which is released during breastfeeding, contributes to further contraction of the uterus to restore its normal size. nine0009 4
When milk arrives, the breasts usually become fuller, firmer and larger than before delivery. In some women, the breasts swell, harden and become very sensitive - swelling of the mammary glands occurs. 10 Frequent breastfeeding relieves these symptoms. For more breast care tips, read our article What is Breast Swelling?
How often does the newborn urinate and defecate?
What goes into the body must go back out. Colostrum
has a laxative effect, helping to eliminate meconium - the original feces. It looks a little scary - black and sticky, like tar. 11 But don't worry, it won't always be like this. Breastfed babies usually have a slightly sweet smell of stool.
How many times a day you will need to change diapers and how the contents should look like, see below.
Day one
- Frequency: once or more.

- Colour: greenish black. nine0087
- Texture: sticky like tar.
Day two
- Frequency: twice or more.
- Colour: dark greenish brown.
- Texture: less sticky.
Day three
- Frequency: twice or more.
- Colour: greenish brown to brownish yellow.
- Texture: non-sticky.
Fourth day and then the entire first month
- Frequency: twice or more.
- Color: yellow (feces should turn yellow no later than by the end of the fourth day).
- Texture: grainy (like mustard with grains interspersed). Leaky and watery.
The baby's urine should be light yellow. On average, babies urinate once a day for the first two days. Starting around the third day, the number of wet diapers increases to three, and from the fifth day onwards, diapers have to be changed five times a day or more often. In addition, during the first few days, the weight of wet diapers increases.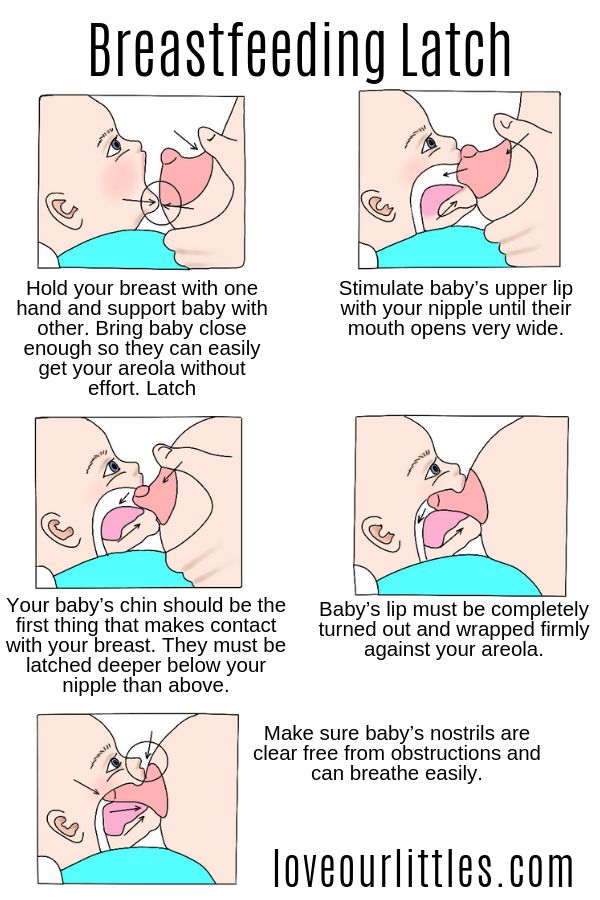 nine0009 11
nine0009 11
Is the baby getting enough breast milk?
Since very little milk is produced at first,
You may feel that this is not enough for your baby. But if you feed your baby on demand, you will produce exactly as much milk as he needs. If you want to keep the process under control, be guided by the frequency of diaper changes above. If your baby soils less diapers, check with your doctor.
“For the first three or four weeks, most babies just eat and sleep. If the child is worried and constantly asks for a breast, you should consult with your doctor, ”Katie recommends. nine0003
Sometimes the baby may vomit after feeding. If the vomit is the color of milk, this is not a cause for concern. But if there are orange, red, green, brown or black blotches in it, or the child vomits with a "fountain", consult a doctor. You should also consult a doctor if the baby has a high temperature, the fontanel (soft spot on the head) has sunk, blood is found in the stool, and also if the weight recorded at birth has not recovered within two weeks. 11
11
But if there are no frightening symptoms and the baby is growing at a normal pace, it means that he has enough milk. Soon you will both get used to breastfeeding and establish a more stable routine.
For the next step in breastfeeding, see Breastfeeding in the First Month: What to Expect.
Literature
1 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
2 Shashi R et al. Postpartum psychiatric disorders: Early diagnosis and management. Indian J Psychiatry . 2015; 57( Suppl 2): S 216– S 221. - Shashi R. et al., Postnatal mental disorders: early diagnosis and treatment. Indian J Saikiatri. 2015; 57(App 2):S216-S221.
2015; 57( Suppl 2): S 216– S 221. - Shashi R. et al., Postnatal mental disorders: early diagnosis and treatment. Indian J Saikiatri. 2015; 57(App 2):S216-S221.
3 Moberg KU, Prime DK. Oxytocin effects in mothers and infants during breastfeeding. Infant . 2013;9(6):201-206. - Moberg K, Prime DK, "The effects of oxytocin on mother and child during breastfeeding." nine0201 Infant. 2013;9(6):201-206.
4 Sobhy SI, Mohame NA. The effect of early initiation of breast feeding on the amount of vaginal blood loss during the fourth stage of labor. J Egypt Public Health Assoc . 2004;79(1-2):1-12. - Sobhi SI, Moham NA, "Early initiation of breastfeeding and its effect on vaginal bleeding in the fourth stage of labor." nine0201 G Egypt Public Health Assoc. 2004;79(1-2):1-2.
2004;79(1-2):1-2.
5 Meier PP et al. Which breast pump for which mother: an evidence-based approach to individualizing breast pump technology. J Perinatol . 2016;36(7):493. - Meyer P.P. et al., Breastpump Selection: A Scientific Approach to Customizing Pumping Technology. J Perinatol (Journal of Perinatology). 2016;36(7):493-499.
6 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women ’ s 2007;52(6):638-642. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." W Midwifery Women Health. 2007;52(6):638-642.
7 Kent JC et al. Principles for maintaining or increasing breast milk production. 2012;41(1):114-121. - Kent J.S. et al. , "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
, "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
8 Australian Breastfeeding Association [ Internet ]. Feeding cues ; 2017 Sep [ cited 2018 Feb ]. - Australian Breastfeeding Association [Internet], Feed Ready Signals; September 2017 [cited February 2018]
9 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe Frauenheilkd . 2013;73(12):1202-1208. - Jacobs A. et al., "Guidelines S -3 for the management of inflammatory breast disease during breastfeeding." Geburtskhilfe und Frauenheilkünde. 2013;73(12):1202-1208.
10 Lawrence RA, Lawrence RM. Breastfeeding: A guide for the medical profession. 7th ed. Maryland Heights MO, USA: Elsevier Mosby; 2010. 1128 p . - Lawrence R.A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." Seventh edition. Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2010. P. 1128.
Breastfeeding: A guide for the medical profession. 7th ed. Maryland Heights MO, USA: Elsevier Mosby; 2010. 1128 p . - Lawrence R.A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." Seventh edition. Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2010. P. 1128.
Breastfeeding in the first month: what to expect
Not sure how to establish lactation and increase milk production? If you need help, support, or just want to know what to expect, read our First Month Breastfeeding Recommendations
Share this information
The first weeks of breastfeeding are a very stressful period. If at times you feel like you can't handle it, know that you are not alone. Feeding your baby all day long is completely natural and helps produce breast milk, but can be quite tiring at times. Be patient, think about yourself and remember: after the first month, when milk production stabilizes, it will become easier. nine0003
nine0003
How often should a baby be breastfed?
Babies are born with a small stomach that grows rapidly with increasing milk production: in the first week it is no larger than an apricot, and after two weeks it is already the size of a large chicken egg. 1.2 Let the child eat as much as he wants and when he wants. This will help him quickly regain the weight lost after birth and grow and develop further.
“Be prepared to feed every two to three hours throughout the day. At night, the intervals between feedings can be longer: three to four or even five hours, says Cathy Garbin, a recognized international expert on breastfeeding. Some eat quickly and are satiated in 15 minutes, while others take an entire hour to feed. Do not compare your breastfeeding regimen with that of other mothers - it is very likely that there will be nothing in common between them. nine0003
At each feed, give your baby a full meal from one breast and then offer a second one, but don't worry if the baby doesn't take it. When the baby is full, he lets go of his chest and at the same time looks relaxed and satisfied - so much so that he can immediately fall asleep. The next time you feed, start on the other breast. You can monitor the order of the mammary glands during feeding using a special application.
When the baby is full, he lets go of his chest and at the same time looks relaxed and satisfied - so much so that he can immediately fall asleep. The next time you feed, start on the other breast. You can monitor the order of the mammary glands during feeding using a special application.
Why does the child always ask for a breast?
The first month is usually the hardest time to breastfeed. But do not think that because the baby is constantly hungry and asks for a breast almost every 45 minutes, then you do not have enough milk. nine0003
In the first month, the baby needs to eat frequently to start and stimulate the mother's milk production. It lays the foundation for a stable milk supply in the future. 3
In addition, we must not forget that the child needs almost constant contact with the mother. The bright light and noise of the surrounding world at first frighten the baby, and only by clinging to his mother, he can calm down.
Sarah, mother of three from the UK, confirms: “Crying is not always a sign of hunger. Sometimes my kids just wanted me to be around and begged for breasts to calm them down. Use a sling. Place the cradle next to the bed. Don't look at the clock. Take advantage of every opportunity to relax. Forget about cleaning. Let those around you take care of you. And not three days, but six weeks at least! Hug your baby, enjoy the comfort - and trust your body." nine0003
Sometimes my kids just wanted me to be around and begged for breasts to calm them down. Use a sling. Place the cradle next to the bed. Don't look at the clock. Take advantage of every opportunity to relax. Forget about cleaning. Let those around you take care of you. And not three days, but six weeks at least! Hug your baby, enjoy the comfort - and trust your body." nine0003
Do I need to feed my baby on a schedule?
Your baby is still too young for a strict daily routine, so
forget about breastfeeding schedules and focus on his needs.
“Volumes have been written about how to feed a baby on a schedule, but babies don't read or understand books,” Cathy says. - All children are different. Some people can eat on a schedule, but most can't. Most often, over time, the child develops his own schedule.
Some mothers report that their babies are fine with scheduled feedings, but they are probably just the few babies who would eat every four hours anyway. Adults rarely eat and drink the same foods at the same time of day - so why do we expect this from toddlers?
Offer your baby the breast at the first sign of hunger. Crying is already the last stage, so be attentive to early signs: the baby licks his lips, opens his mouth, sucks his fist, turns his head with his mouth open - looking for the breast. nine0009 4
Crying is already the last stage, so be attentive to early signs: the baby licks his lips, opens his mouth, sucks his fist, turns his head with his mouth open - looking for the breast. nine0009 4
What is a "milk flush"?
At the beginning of each feeding, a hungry baby actively sucks on the nipple,
thereby stimulating the milk flow reflex - the movement of milk through the milk ducts. 5
“Nipple stimulation triggers the release of the hormone oxytocin,” Cathy explains. “Oxytocin is distributed throughout the body and causes the muscles around the milk-producing glands to contract and the milk ducts to dilate. This stimulates the flow of milk. nine0003
If the flushing reflex fails, milk will not come out. This is a hormonal response, and under stress it may not work at all or work poorly. Therefore, it is so important that you feel comfortable and calm when feeding.
“Studies show that each mother has a different rhythm of hot flashes during one feed,” Kathy continues, “Oxytocin is a short-acting hormone, it breaks down in just 30-40 seconds after formation. Milk begins to flow, the baby eats, the effect of oxytocin ends, but then a new rush of milk occurs, the baby continues to suckle the breast, and this process is repeated cyclically. That is why, during feeding, the child periodically stops and rests - this is how nature intended. nine0003
Milk begins to flow, the baby eats, the effect of oxytocin ends, but then a new rush of milk occurs, the baby continues to suckle the breast, and this process is repeated cyclically. That is why, during feeding, the child periodically stops and rests - this is how nature intended. nine0003
The flow of milk may be accompanied by a strong sensation of movement or tingling in the chest, although 21% of mothers, according to surveys, do not feel anything at all. 5 Cathy explains: “Many women only feel the first rush of milk. If you do not feel hot flashes, do not worry: since the child eats normally, most likely, you simply do not understand that they are.
How can you tell if your baby is getting enough milk?
Since it is impossible to track how much milk a baby eats while breastfeeding, mothers sometimes worry that the baby is malnourished. Trust your child and your body. nine0003
After a rush of milk, the baby usually begins to suckle more slowly. Some mothers clearly hear how the baby swallows, others do not notice it.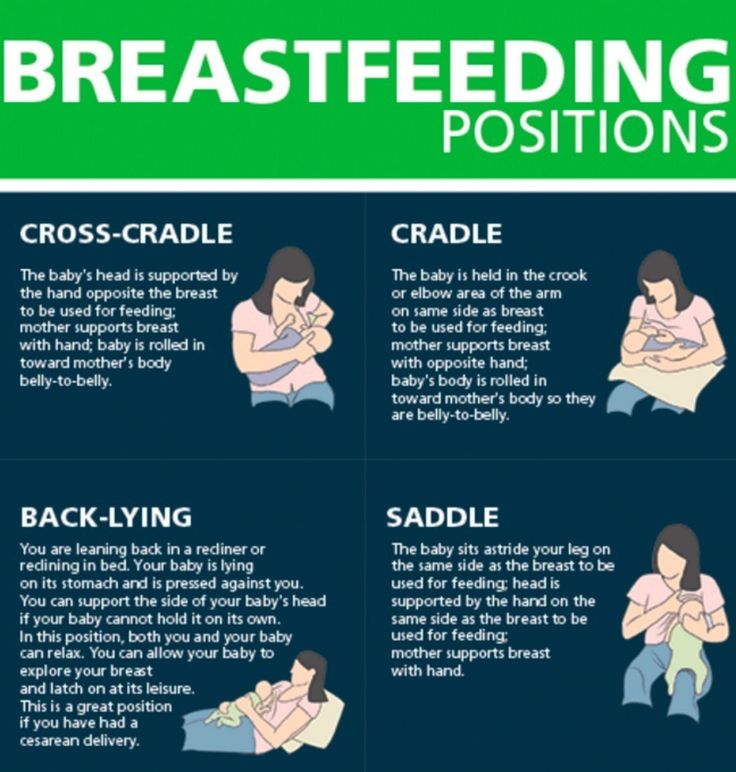 But one way or another, the child himself will show when he is full - just watch carefully. Many babies make two or three approaches to the breast at one feeding. 6
But one way or another, the child himself will show when he is full - just watch carefully. Many babies make two or three approaches to the breast at one feeding. 6
“When a child has eaten, it is noticeable almost immediately: a kind of “milk intoxication” sets in. The baby is relaxed and makes it clear with his whole body that he is completely full, says Katie, “Diapers are another great way to assess whether the baby is getting enough milk. During this period, a breastfed baby should have at least five wet diapers a day and at least two portions of soft yellow stool, and often more.” nine0003
From one month until weaning at six months of age, a baby's stool (if exclusively breastfed) should look the same every day: yellow, grainy, loose, and watery.
When is the child's birth weight restored?
Most newborns lose weight in the first few days of life. This is normal and should not be cause for concern. As a rule, weight is reduced by 5-7%, although some may lose up to 10%. One way or another, by 10–14 days, almost all newborns regain their birth weight. In the first three to four months, the minimum expected weight gain is an average of 150 grams per week. But one week the child may gain weight faster, and the next slower, so it is necessary that the attending physician monitor the health and growth of the baby constantly. nine0009 7.8
One way or another, by 10–14 days, almost all newborns regain their birth weight. In the first three to four months, the minimum expected weight gain is an average of 150 grams per week. But one week the child may gain weight faster, and the next slower, so it is necessary that the attending physician monitor the health and growth of the baby constantly. nine0009 7.8
At the slightest doubt or signs of dehydration, such as
dark urine, no stool for more than 24 hours, retraction of the fontanel (soft spot on the head), yellowing of the skin, drowsiness, lethargy, lack of appetite (ability to four to six hours without feeding), you should immediately consult a doctor. 7
What is "cluster feeding"?
When a baby asks to breastfeed very often for several hours, this is called cluster feeding. nine0009 6 The peak often occurs in the evening between 18:00 and 22:00, just when many babies are especially restless and need close contact with their mother. Most often, mothers complain about this in the period from two to nine weeks after childbirth. This is perfectly normal and common behavior as long as the baby is otherwise healthy, eating well, gaining weight normally, and appears content throughout the day. 9
Most often, mothers complain about this in the period from two to nine weeks after childbirth. This is perfectly normal and common behavior as long as the baby is otherwise healthy, eating well, gaining weight normally, and appears content throughout the day. 9
Cluster feeding can be caused by a sharp jump in the development of the body - during this period the baby especially needs love, comfort and a sense of security. The growing brain of a child is so excited that it can be difficult for him to turn off, or it just scares the baby. nine0009 9 If a child is overworked, it is often difficult for him or her to calm down on his own, and adult help is needed. And breastfeeding is the best way to calm the baby, because breast milk is not only food, but also pain reliever and a source of happiness hormones. 10
“No one told me about cluster feeding, so for the first 10 days I just went crazy with worry - I was sure that my milk was not enough for the baby,” recalls Camille, a mother from Australia, “It was a very difficult period . I was advised to pump and supplement until I finally contacted the Australian Breastfeeding Association. There they explained to me what was happening: it turned out that it was not about milk at all. nine0003
I was advised to pump and supplement until I finally contacted the Australian Breastfeeding Association. There they explained to me what was happening: it turned out that it was not about milk at all. nine0003
Remember, this is temporary. Try to prepare dinner for yourself in the afternoon, when the baby is fast asleep, so that in the evening, when he begins to often breastfeed, you have the opportunity to quickly warm up the food and have a snack. If you are not alone, arrange to carry and rock the baby in turns so that you have the opportunity to rest. If you have no one to turn to for help and you feel that your strength is leaving you, put the baby in the crib and rest for a few minutes, and then pick it up again. nine0003
Ask your partner, family and friends to help you with household chores, cooking and caring for older children if you have any. If possible, hire an au pair. Get as much rest as possible, eat well and drink plenty of water.
“My daughter slept a lot during the day, but from 23:00 to 5:00 the cluster feeding period began, which was very tiring,” recalls Jenal, a mother from the USA, “My husband tried his best to make life easier for me - washed, cleaned, cooked, changed diapers, let me sleep at every opportunity and never tired of assuring me that we were doing well. nine0003
nine0003
If you are concerned about the frequency of breastfeeding, it is worth contacting a specialist. “Check with a lactation consultant or doctor to see if this is indicative of any problems,” recommends Cathy. “Resist the temptation to supplement your baby with formula (unless recommended by your doctor) until you find the cause. It may not be a matter of limited milk production at all - it may be that the child is inefficiently sucking it.
When will breastfeeding become easier? nine0015
This early stage is very special and does not last long. Although sometimes it seems that there will be no end to it, rest assured: it will get easier soon! By the end of the first month, breast milk production will stabilize, and the baby will become stronger and learn to suckle better. 2.3 Any problems with latch on by this time will most likely be resolved and the body will be able to produce milk more efficiently so inflammation and leakage of milk will begin to subside.
“The first four to six weeks are the hardest, but then things start to get better,” Cathy assures. It just needs to be experienced!” nine0003
The longer breastfeeding continues, the more benefits it brings, from saving on formula and improving sleep quality 11–13 to boosting your baby's immune system 14 and reducing your risk of certain cancers. 15
“When you feel like you're pushing yourself, try to go from feed to feed and day to day,” advises Hannah, a UK mom. “I was sure I wouldn’t make it to eight weeks. And now I have been breastfeeding for almost 17 weeks, and I dare say it is very easy.” nine0003
Read the resource Breastfeeding Beyond the First Month: What to Expect
Literature
1 Naveed M et al. An autopsy study of relationship between perinatal stomach capacity and birth weight. Indian J Gastroenterol .1992;11(4):156-158. - Navid M. et al., Association between prenatal gastric volume and birth weight. Autopsy. Indian J Gastroenterol. 1992;11(4):156-158.
et al., Association between prenatal gastric volume and birth weight. Autopsy. Indian J Gastroenterol. 1992;11(4):156-158.
2 Neville MC et al. Studies in human lactation: milk volumes in lactating women during the onset of lactation and full lactation .Am J Clinl Nutr .1988;48(6):1375-1386. at the beginning and at the peak of lactation." Am F Clean Nutr. 1988;48(6):1375-1386.
3 Kent JC et al. Principles for maintaining or increasing breast milk production. 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121. nine0201
4 Australian Breastfeeding Feeding cues ; 2017 Sep [ cited 2018 Feb ]. - Australian Breastfeeding Association [Internet], Feed Ready Signals; September 2017 [cited February 2018]
- Australian Breastfeeding Association [Internet], Feed Ready Signals; September 2017 [cited February 2018]
5 Kent JC et al. Response of breasts to different stimulation patterns of an electric breast pump. J Human Lact . 2003;19(2):179-186. - Kent J.S. et al., Breast Response to Different Types of Electric Breast Pump Stimulation. J Human Lact (Journal of the International Association of Lactation Consultants). 2003;19(2):179-186.
6) Kent JC et al . Volume and frequency of breastfeedings and fat content of breast milk throughout the day. Pediatrics. 2006;117(3): e 387-395. - Kent J.S. et al., "Amount and frequency of breastfeeding and fat content of breast milk during the day." Pediatrix (Pediatrics). 2006;117(3):e387-95.
7 Lawrence RA, Lawrence RM. Breastfeeding: A guide for the medical profession. 7th ed. Maryland Heights MO, USA: Elsevier Mosby; 2010. 1128 p . - Lawrence R.A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." Seventh edition. Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2010. P. 1128.
Breastfeeding: A guide for the medical profession. 7th ed. Maryland Heights MO, USA: Elsevier Mosby; 2010. 1128 p . - Lawrence R.A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." Seventh edition. Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2010. P. 1128.
8 World Health Organization. [Internet]. Child growth standards; 2018 [cited 2018 Feb] - World Health Organization. [Internet]. Child Growth Standards 2018 [cited February 2018]. nine0201
9 Australian Breastfeeding Association . [ Internet ]. Cluster feeding and fussing babies ; Dec 2017 [ cited 2018 Feb ] - Australian Breastfeeding Association [Internet], "Cluster feeding and screaming babies"; December 2017 [cited February 2018]. nine0201
nine0201
10 Moberg KU, Prime DK. Oxytocin effects in mothers and infants during breastfeeding. Infant . 2013;9(6):201-206.- Moberg K, Prime DK, "Oxytocin effects on mother and child during breastfeeding". Infant. 2013;9(6):201-206.
11 U.S. Department of Health & Human Services [Internet]. Surgeon General Breastfeeding factsheet; 2011 Jan 20 [cited 2017 Feb] - Department of Health and Human Services [Internet], "Breastfeeding Facts from the Chief Medical Officer", Jan 20, 2011 [cited Feb 2017]
12 Kendall-Tackett K et al. The effect of feeding method on sleep duration, maternal well-being, and postpartum depression. clinical lactation. 2011;1;2(2):22-26. - Kendall-Tuckett, K. et al., "Influence of feeding pattern on sleep duration, maternal well-being and the development of postpartum depression." Clinical Lactation. 2011;2(2):22-26.
13 Brown A, Harries V. Infant sleep and night feeding patterns during later infancy: Association with breastfeeding frequency, daytime complementary food intake, and infant weight. Breast Med . 2015;10(5):246-252. - Brown A., Harris W., "Night feedings and infant sleep in the first year of life and their association with feeding frequency, daytime supplementation, and infant weight." Brest Med (Breastfeeding Medicine). 2015;10(5):246-252.
Infant sleep and night feeding patterns during later infancy: Association with breastfeeding frequency, daytime complementary food intake, and infant weight. Breast Med . 2015;10(5):246-252. - Brown A., Harris W., "Night feedings and infant sleep in the first year of life and their association with feeding frequency, daytime supplementation, and infant weight." Brest Med (Breastfeeding Medicine). 2015;10(5):246-252.
14 Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin Transl immunology. 2013;2(4). - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." nine0201 Clean Transl Immunology. 2013;2(4):e3.
15 Li DP et al. Breastfeeding and ovarian cancer risk: a systematic review and meta-analysis of 40 epidemiological studies. Asian Pac J Cancer Prev .