Babies being sick after feeding
Reflux in babies - NHS
Reflux is when a baby brings up milk, or is sick, during or shortly after feeding. It's very common and usually gets better on its own.
Check if your baby has reflux
Reflux usually starts before a baby is 8 weeks old and gets better by the time they're 1.
Symptoms of reflux in babies include:
- bringing up milk or being sick during or shortly after feeding
- coughing or hiccupping when feeding
- being unsettled during feeding
- swallowing or gulping after burping or feeding
- crying and not settling
- not gaining weight as they're not keeping enough food down
Sometimes babies may have signs of reflux but will not bring up milk or be sick. This is known as silent reflux.
Things you can try to ease reflux in babies
Your baby does not usually need to see a doctor if they have reflux, as long as they're happy, healthy and gaining weight.
Do
-
ask a health visitor for advice and support
-
get advice about your baby's breastfeeding position or how to bottle feed your baby
-
hold your baby upright during feeding and for as long as possible after feeding
-
burp your baby regularly during feeds
-
give formula-fed babies smaller feeds more often
-
make sure your baby sleeps flat on their back (they should not sleep on their side or front)
Non-urgent advice: See a GP if your baby:
- is not improving after trying things to ease reflux
- gets reflux for the first time after they're 6 months old
- is older than 1 and still has reflux
- is not gaining weight or is losing weight
Urgent advice: Ask for an urgent GP appointment or call 111 if your baby:
- has vomit that's green or yellow, or has blood in it
- is projectile vomiting (being sick with more force than usual)
- has blood in their poo
- has a swollen or tender tummy
- has a very high temperature or they feel hot or shivery
- keeps being sick and cannot keep fluid down
- has diarrhoea that lasts for over a week or has signs of dehydration
- will not stop crying and is very distressed
- is refusing to feed
Also call your GP or 111 if you have any other concerns about your baby.
Treatment for reflux in babies
A GP or specialist may sometimes recommend treatments for reflux.
If your baby is formula-fed, you may be given:
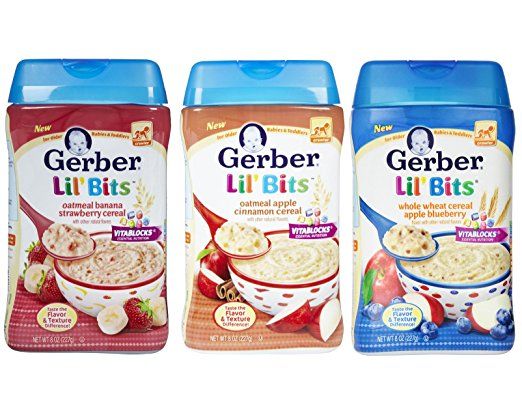
- a powder that's mixed with formula to thicken it
- a pre-thickened formula milk
If the thickening powder does not help or your baby is breastfed, a GP or specialist might recommend medicines that stop your baby's stomach producing as much acid.
Very rarely, surgery might be needed to strengthen the muscles to stop food or milk travelling back up. This is usually only after trying other things or if their reflux is severe.
Causes of reflux
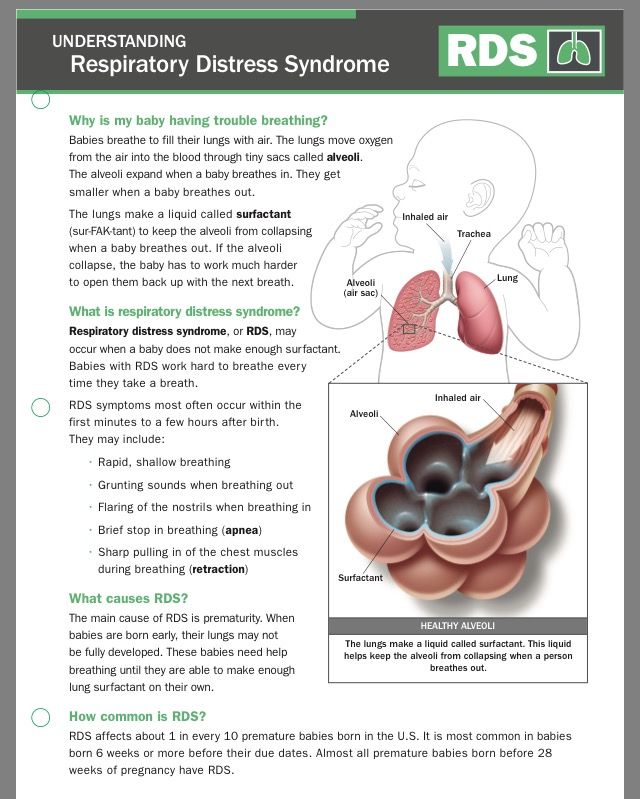
Reflux usually happens because your baby's food pipe (oesophagus) has not fully developed, so milk can come back up easily.
Your baby's oesophagus will develop as they get older and the reflux should stop.
Page last reviewed: 13 December 2021
Next review due: 13 December 2024
Reflux | Breastfeeding Challenges | Start for Life
Breastfeeding challenges
There may be times when breastfeeding is challenging. Never ignore any issues you may have – talk to your health visitor, midwife, GP or breastfeeding specialist as soon as possible, they will be able to help you sort it out quickly.
Here are some common breastfeeding issues, and tips on what to do.
- Colic
- Constipation
- Mastitis
- Milk supply
- Reflux
- Sore nipples
- Thrush
- Tongue-tie
Baby reflux
If your baby brings up milk, or is sick during or after feeding, this is known as reflux.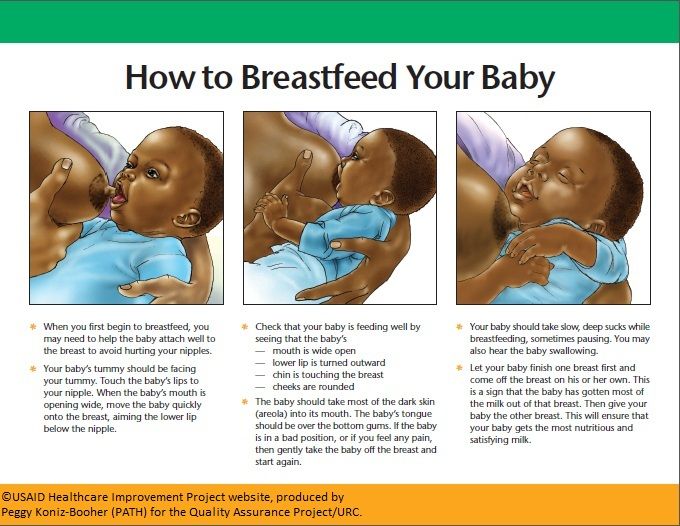 Reflux, also called posseting or spitting up, is quite common and your baby should grow out of it, usually by the time they are 12 months old.
Reflux, also called posseting or spitting up, is quite common and your baby should grow out of it, usually by the time they are 12 months old.
What causes baby reflux?
The muscle at the bottom of the food pipe acts as a kind of door into the stomach – so when food or milk travels down, the muscle opens allowing the food into the stomach.
However, while this muscle is still developing in the first year, it can open when it shouldn't (usually when your baby's tummy is full) allowing some food and stomach acid to travel back up again. Acid in the stomach is normal and a necessary part of the digestion process – it helps break down food.
In most babies, reflux is nothing to worry about as long as they are healthy and gaining weight as expected.
Baby reflux symptoms
- Constant or sudden crying when feeding.
- Bringing up milk during or after feeds (regularly).
- Frequent ear infections.
- Lots of hiccups or coughing.
- Refusing, gagging, or choking during feeds.

- Poor weight gain.
- Waking up at night a lot.
GORD
When reflux becomes painful and it happens frequently, this is known as 'gastro-oesophageal reflux disease' (GORD). GORD is more serious than mild, everyday reflux. The strong stomach acid can irritate and make the food pipe sore and inflamed, which is painful for your baby and may result in them needing medication.
The main signs and symptoms of GORD in your baby are:
- spitting up frequently
- abdominal pain
- feeding difficulties
- seeming unsettled and grizzly after a feed
These symptoms can lead to your baby not gaining weight, or even losing weight.
Silent reflux
Silent reflux can be confusing as there are no obvious signs or clues (such as spitting up). It's when the food travels back up the food pipe – but it's swallowed rather than spat out so is harder to identify. But your baby may display similar symptoms to those of regular reflux.
Breastfeeding Friend from Start for Life
The Breastfeeding Friend, a digital tool from Start for Life, has lots of useful information and expert advice to share with you – and because it's a digital tool, you can access it 24 / 7.
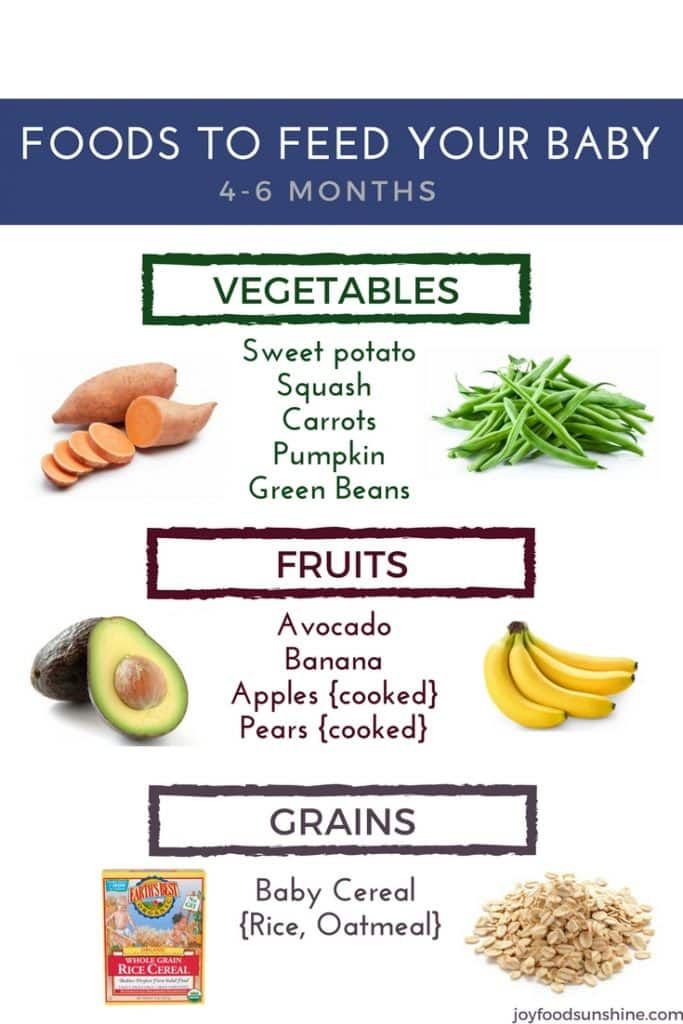
Breastfeeding tips for babies with reflux
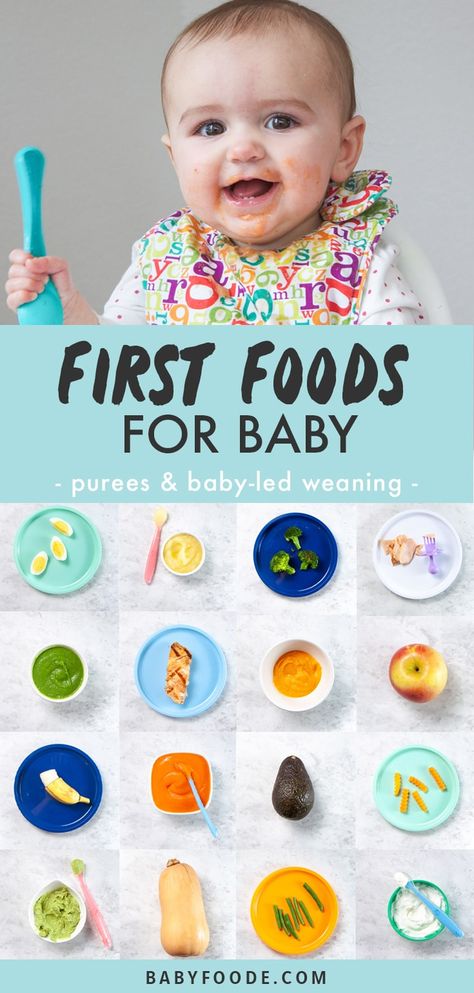
- Feeding little and often (smaller feeds stop their tummy getting too full).
- Burping them requently during feeds – have a look at our guide to burping your baby for techniques.
- Try a different feeding position – check out our our guide to breastfeeding positions.
- Keep your baby upright, for at least an hour after feeding, this should help keep the milk down.
If you are mixed feeding (combining breastmilk and formula feeds), have a look at our advice on bottle feeding and reflux.
When to see the GP
If your baby has difficulty feeding or refuses to feed, regularly brings milk back up and seems uncomfortable after a feed, talk to your pharmacist, GP, or health visitor.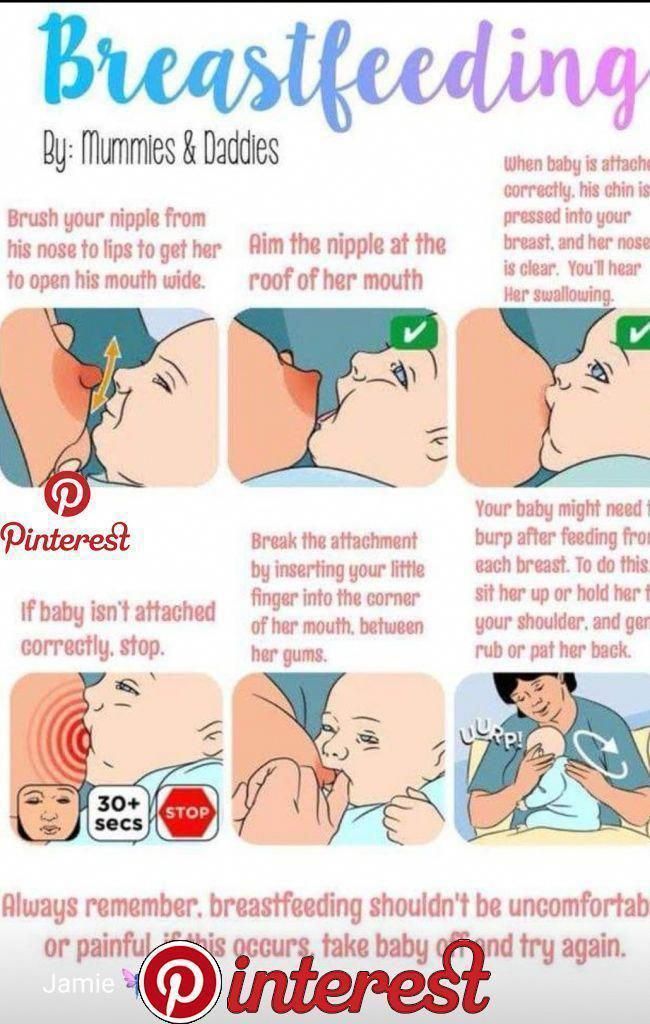 They'll be able to give you practical advice on how to ease the symptoms and manage it – they may also need to rule out other causes (such as cow's milk allergy).
They'll be able to give you practical advice on how to ease the symptoms and manage it – they may also need to rule out other causes (such as cow's milk allergy).
It might be helpful to keep a record of when your baby feeds, with details of how often and how much your baby brings the food back up, and how often your baby cries or seems distressed. This will help your health visitor or GP decide if your baby needs treatment.
Spitting up and vomiting in infants
Spitting up and vomiting in babies is a common reason for visiting a doctor.
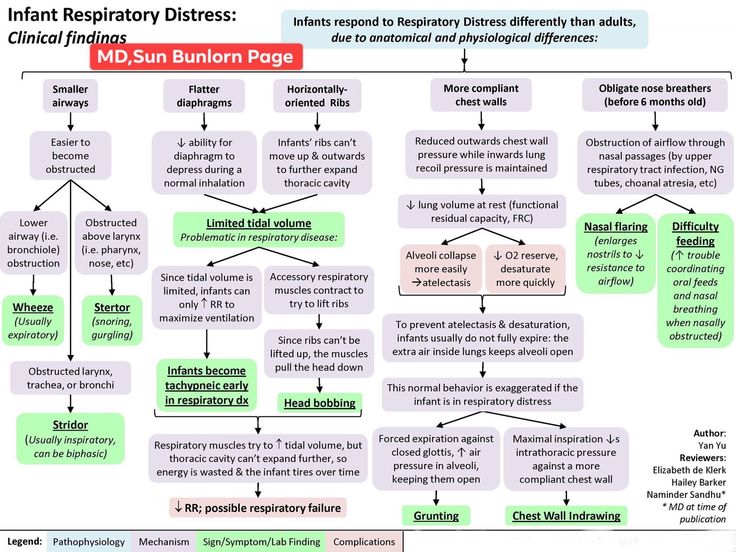
Regurgitation and vomiting is a reflex action that occurs when receptors located in various anatomical zones are irritated, incl. in the stomach, esophagus, pharynx, oral cavity. The signal is transmitted to the vomiting center, which is located in the medulla oblongata and a gag reflex occurs.
What is the difference between regurgitation and vomiting?
The difference lies in the volume and kinetics (movement) of the gastric contents expelled to the outside. When regurgitation occurs, leakage occurs without the participation of the diaphragm and abdominal muscles, i.e. passively. There is little content, up to about 10-15 ml. If the child does not swallow it, it quietly expires from the oral cavity. When vomiting, a wave-like bending of the upper half of the body occurs as a result of contraction of the muscles of the diaphragm and the anterior wall of the abdomen, the volume of vomit is greater, and they are erupted with pressure from the oral cavity with an ejection trajectory of up to 50 cm. In children of the first year of life, this is defined by the term "fountain vomiting" .
When regurgitation occurs, leakage occurs without the participation of the diaphragm and abdominal muscles, i.e. passively. There is little content, up to about 10-15 ml. If the child does not swallow it, it quietly expires from the oral cavity. When vomiting, a wave-like bending of the upper half of the body occurs as a result of contraction of the muscles of the diaphragm and the anterior wall of the abdomen, the volume of vomit is greater, and they are erupted with pressure from the oral cavity with an ejection trajectory of up to 50 cm. In children of the first year of life, this is defined by the term "fountain vomiting" .
Regurgitation is observed only in children of the first year of life and, mainly, up to 6 months. Contribute to this anatomical and physiological features of the esophagus and stomach of the baby. Their esophagus is short and wide, the angle of connection of the esophagus with the stomach is less pronounced, and its obturator function is weak. These regurgitations are physiological.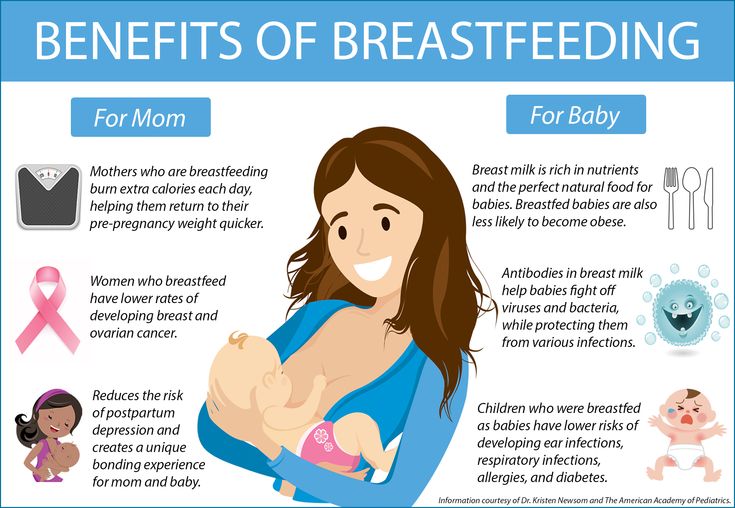 They can be after each feeding, up to 15 ml, do not affect the well-being and weight gain of the baby. They can also be caused by excessive feeding, aerophagia (swallowing air while sucking), straining during intestinal colic. The frequency and volume of such regurgitation decreases with the growth of the child. With the introduction of complementary foods, and this is a thicker food, regurgitation stops or becomes much less frequent.
They can be after each feeding, up to 15 ml, do not affect the well-being and weight gain of the baby. They can also be caused by excessive feeding, aerophagia (swallowing air while sucking), straining during intestinal colic. The frequency and volume of such regurgitation decreases with the growth of the child. With the introduction of complementary foods, and this is a thicker food, regurgitation stops or becomes much less frequent.
If regurgitation persists in a child older than 1 year, then this is a sign of a pathological process.
Vomiting, unlike regurgitation, is accompanied by vegetative symptoms - increased salivation, pallor of the skin, palpitations. This is due to the fact that next to the vomiting center there are additional centers of autonomic regulation, which are reflexively excited, and active biological substances such as serotonin, dopamine, histamine and others are released into the blood.
Regurgitation and vomiting, from the moment of eating, may occur during feeding, after feeding for the first 20-30 minutes or delayed, sometimes after several hours.
Regurgitation and vomiting that occurs immediately after feeding unchanged breast milk or formula may be due to narrowing of the esophagus. If they persist until the next feeding, and the milk / mixture is curdled, has a sour or musty smell, then this is the result of a long standing food in the stomach. The reason for this may be the low tone of the muscle layer of the stomach and, as a result, its peristalsis or narrowing of the output section due to an anomaly in the development or high tone of the sphincter of the lower stomach. With narrowing of the duodenum, bile is present in the regurgitated masses.
Gastroesophageal reflux is a common cause of regurgitation in infants. It is likely that there is a complex problem here, starting with the immaturity of the gastrointestinal tract and disorders of the central nervous system. Perinatal injuries of the central nervous system accompany every second child. Their manifestations are varied. Regurgitation and vomiting can be facilitated by an increase in intracranial pressure, disorders in the segment of the cervical spine, and so on. Therefore, quite often, when carrying out rehabilitation measures for neurological dysfunctions, a positive effect is manifested in the form of a decrease or cessation of regurgitation. A hernia of the esophageal opening of the diaphragm will also manifest itself in a similar way.
Therefore, quite often, when carrying out rehabilitation measures for neurological dysfunctions, a positive effect is manifested in the form of a decrease or cessation of regurgitation. A hernia of the esophageal opening of the diaphragm will also manifest itself in a similar way.
We should not forget about allergic gastrointestinal reactions in the form of regurgitation and vomiting. The most common cause of this is cow's milk protein. With intolerance to cow's milk protein, inflammation of the mucous membrane of the esophagus, stomach and intestines occurs. And, as a result of this, regurgitation and vomiting, pain and increased gas formation, diarrhea or constipation.
Rare endocrine disorders (adrenogenital syndrome) are manifested by vomiting in children from the first weeks of life. In such cases, vomiting is frequent, there may be an admixture of bile, the child loses weight due to loss of fluid and nutrients, and severe metabolic disorders develop.
Vomiting can also be caused by an intestinal infection. Viral gastroenteritis is now common. It must be remembered that the younger the child, the more severe the disease. Within a few hours, the child's condition can go from satisfactory to extremely serious.
Viral gastroenteritis is now common. It must be remembered that the younger the child, the more severe the disease. Within a few hours, the child's condition can go from satisfactory to extremely serious.
As you can see, the causes of regurgitation and vomiting in children of the first year of life are quite diverse, but most often these are transient conditions that disappear with the growth of the child.
Prevention of regurgitation in children of the first months of life is quite simple. Don't overfeed your baby. If he cries, it does not always mean that he is hungry. Excess feeding leads to increased gas formation and colic, during which the child is worried, straining, thereby increasing the likelihood of spitting up. After feeding, hold the baby more upright so that he can burp the swallowed air. This will take 15-20 minutes. If the child is bottle-fed, do not change his formula milk without the recommendation of a pediatrician.
If the child has frequent regurgitation and vomiting, it is necessary to consult a pediatrician or gastroenterologist to diagnose the cause. To make a diagnosis, it is sometimes enough to carry out simple and affordable diagnostic methods in a polyclinic. These include an ultrasound of the stomach and, if necessary, stool tests. However, the approach in each case is individual. Examination and treatment will be assigned to your baby, depending on the diagnosis. Perhaps it will be preventive measures or a certain milk formula, perhaps drug therapy. Rarely, but it happens that it is necessary to examine the child in a hospital and surgical treatment.
To make a diagnosis, it is sometimes enough to carry out simple and affordable diagnostic methods in a polyclinic. These include an ultrasound of the stomach and, if necessary, stool tests. However, the approach in each case is individual. Examination and treatment will be assigned to your baby, depending on the diagnosis. Perhaps it will be preventive measures or a certain milk formula, perhaps drug therapy. Rarely, but it happens that it is necessary to examine the child in a hospital and surgical treatment.
Regurgitation and vomiting in children. When to see a surgeon
The regurgitation syndrome is one of the most common reasons for parents of small children to visit a pediatrician and a surgeon. The causes of regurgitation in children under 1 year old are different: anatomical and functional features, neurological disorders, infectious processes, malformations or other problems. The mechanism that prevents regurgitation and vomiting in children is very complex and depends on the anatomical structure and physiological processes of the child. The formation of this mechanism occurs in the last trimester of pregnancy and continues in the first months of a child's life. Although regurgitation and vomiting can be a symptom of various diseases, in themselves these processes are physiological, i.e. normal. The pathological reflux of stomach contents into the esophagus is called gastroesophageal reflux, and the mechanism that prevents vomiting is called the antireflux mechanism.
The formation of this mechanism occurs in the last trimester of pregnancy and continues in the first months of a child's life. Although regurgitation and vomiting can be a symptom of various diseases, in themselves these processes are physiological, i.e. normal. The pathological reflux of stomach contents into the esophagus is called gastroesophageal reflux, and the mechanism that prevents vomiting is called the antireflux mechanism.
Anti-reflux mechanism in children
In children, the nervous regulation of the antireflux mechanism is very complex and easily disturbed under the influence of external and internal factors. Regurgitation and vomiting easily occur in children with an immature antireflux mechanism, if the mode or volume of feeding is incorrectly selected, as a reaction to artificial mixtures, at the slightest sign of infectious processes. This is especially often observed in children with intrauterine growth retardation and premature babies, as well as in severe pregnancy and toxicosis, caesarean section, complicated childbirth, etc.
When to see a doctor
Despite the fact that moderate spitting up in a child under 6 months is considered a variant of the norm, parents should definitely tell the pediatrician about this during a routine examination. The reason for serious concern and immediate examination of the child is an increase in the frequency or increase in the volume of regurgitation, the appearance of streaks of blood or bile impurities, a lag in recruitment or weight loss, and high temperature. In this case, it is urgent to consult a surgeon to rule out surgical causes.
Diagnostics
In most cases, an ultrasound examination (ultrasound) is necessary to establish an accurate diagnosis and select the correct treatment. An experienced doctor of ultrasound diagnostics helps to establish the correct diagnosis in more than half of the cases. Sometimes, for a more accurate diagnosis, a flexible gastroscopy, X-ray examination, or computed tomography of the abdominal organs is performed.
When surgery is required
Pyloric stenosis, or impaired patency of the gastric outlet, is the cause of the most severe regurgitation syndrome (vomiting "fountain") in children under 2 months, accompanied by severe weight loss and progressive deterioration of the child's condition. This disease requires urgent surgical care. In leading clinics, such operations are performed using a minimally invasive laparoscopic method. The current level of development of surgery and pediatric anesthesiology allows the use of endoscopic surgery techniques even in children in the first weeks of life.
There are also other causes of regurgitation that require surgical intervention, such as hiatal hernia, chalazia (gaping) of the esophagus, and others. These malformations are characterized by a violation of the formation of the antireflux mechanism and lead to constant regurgitation in a child, impaired weight gain, decreased appetite, chronic cough, bronchial asthma, and anemia.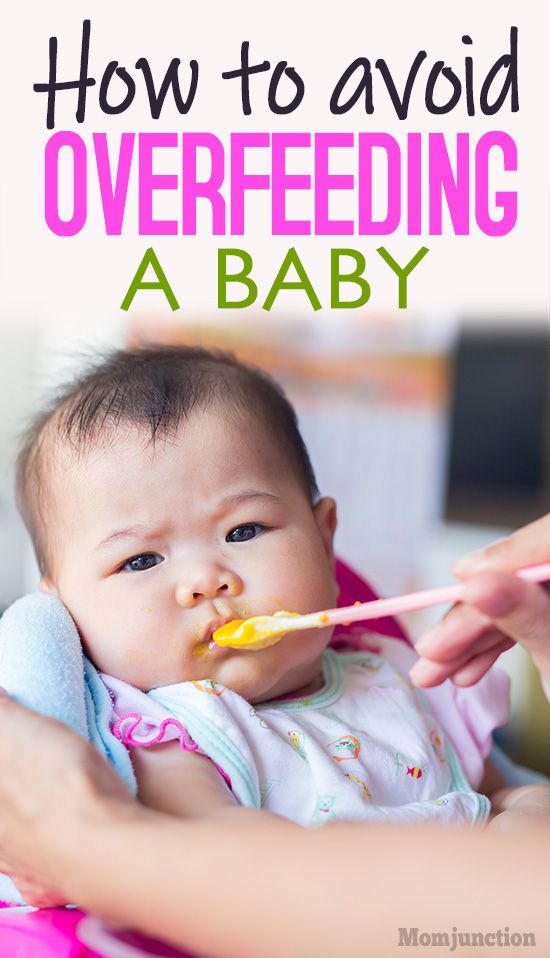 If drug therapy is ineffective, then a gastrofundoplication operation is indicated, in which an artificial antireflux valve is surgically formed. Like many other interventions, in modern children's clinics this operation is performed laparoscopically - with less trauma, minimal blood loss, minimal cosmetic defect and a quick recovery of the child after the operation.
If drug therapy is ineffective, then a gastrofundoplication operation is indicated, in which an artificial antireflux valve is surgically formed. Like many other interventions, in modern children's clinics this operation is performed laparoscopically - with less trauma, minimal blood loss, minimal cosmetic defect and a quick recovery of the child after the operation.
Of course, vomiting and regurgitation can be symptoms of many other diseases and occur at any age of the child. Thus, vomiting is often observed in acute appendicitis and intestinal obstruction, it can be a symptom of an intestinal infection, intoxication, etc. In addition to the disease itself, vomiting and profuse regurgitation are dangerous because the child loses a large amount of water and salts necessary for life, which can lead to dehydration - exsicosis. The younger the child, the faster the disruption of compensatory mechanisms and the worsening of his condition. Therefore, the appearance in a child of symptoms of vomiting or severe regurgitation in young children requires immediate medical attention to identify the causes, establish the correct diagnosis and select the optimal treatment, and, if necessary, surgical.