Baby acne or food allergy
Does my baby have acne or a rash? Diagnosis and treatment
Baby acne is common and usually clears up on its own. Some rashes may need treatment, however, so it is important to know the difference between baby acne, rashes, and other skin problems.
Babies have very sensitive skin, so caregivers may worry that spots or a rash are a sign of an allergic reaction or a health condition.
In this article, we look at how to tell the difference between baby acne and common rashes, plus home remedies and how to prevent baby acne.
Baby acne, or neonatal acne, is common and affects around 20 percent of newborns before they are 6 weeks old. It is most common on the face, but it can present on the neck, upper back, and chest. It is rare elsewhere on the body.
In adults and teenagers, hormonal swings and clogged oil glands commonly cause acne. This might occur due to using makeup, sweating, and applying skin care products.
Maternal hormones cause baby acne. Some babies are born with acne, while others develop it soon after birth.
Baby acne often appears as whiteheads, or closed comedones. Some babies also develop red pimples and mild skin inflammation. In rare cases, a baby may develop serious acne that can leave scars or become infected.
Baby acne does not usually need treatment, but when symptoms are severe, a doctor may choose to prescribe antibiotics or other treatments.
Baby acne typically starts before a baby is 6 weeks old. A rash or spot that appears after 6 weeks could be a result of something else. Babies who develop acne after the age of 6 weeks should see a dermatologist for diagnosis and treatment.
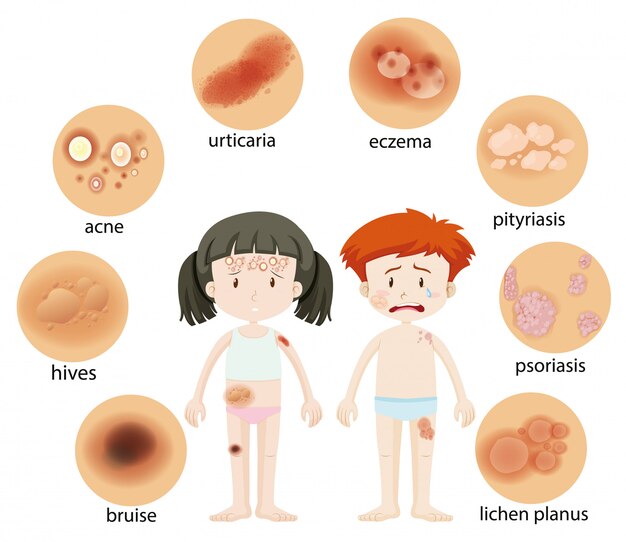
Rashes and other skin conditions are very common in newborns and can arise for many reasons. Some can look similar to acne. A few common skin conditions in babies include:
Contact dermatitis
Contact dermatitis results from coming into contact with something that irritates the skin, such as a lotion, cream, material, or metal. Contact dermatitis can look like red bumps or flattened areas of red irritation.
Allergens, irritating substances such as citrus juice, and wet skin from drooling can all cause contact dermatitis. This type of rash is more common in older babies who have started eating solid foods, and it is most common around the mouth.
It usually clears on its own, but if the rash gets worse, a doctor might prescribe a steroid cream or other treatment.
Heat rash
A heat rash, or miliaria, occurs when sweat glands are blocked. Some common causes include overheating, sitting in front of a space heater, and being held too tightly against a person’s skin.
Keep the baby’s skin cool and dry. Avoid very tight or warm clothes, especially in the summer. Heat rashes usually go away on their own.
Erythema toxicum
Erythema toxicum is a rash that starts a few days after birth. The rash is blotchy and red, with blisters that have a small white or yellow center.
An estimated 48–72 percent of full-term infants will experience erythema toxicum. It is harmless and will go away on its own within a few days.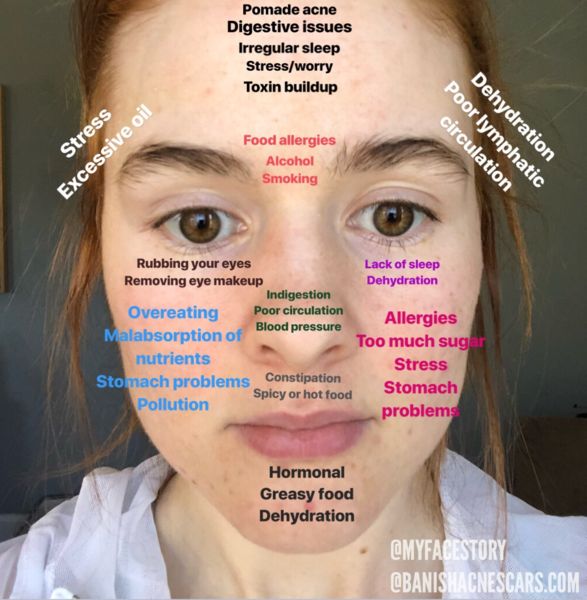
Eczema
Share on PinterestA baby may inherit eczema if a member of their family has it.
Eczema is a skin condition that tends to run in families. Babies with eczema may have small patches of dry or thickened skin. More severe cases can turn the skin red and inflamed. Eczema patches are typically very dry and itchy.
Some babies experience eczema flares due to specific environmental triggers, such as dry weather, a new skin care product, and some food items. Identifying and avoiding these triggers can help.
Use a mild soap for eczema and avoid scrubbing the skin. Some caregivers find that less frequent bathing also helps. Put eczema cream on the affected patches after each bath.
Many infants outgrow eczema by 4 years old.
A number of over-the-counter (OTC) skin creams can make eczema less itchy. Corticosteroid creams, which use a mild steroid to speed healing, can also help. Though these are available over-the-counter, it is safer to talk to a doctor before using them on a baby.
Milia
Milia are small, firm, white bumps on the skin. They are very common, affecting nearly half of newborns. They may be present at birth, or they may develop shortly after.
Milia are harmless and will disappear without treatment. They form when skin flakes or keratin get trapped under the skin.
Transient neonatal pustular melanosis
Transient neonatal pustular melanosis is a common skin condition in newborns. It appears as small pus-filled spots. It is harmless and will go away by itself.
This skin condition is more common in newborns with black skin. The spots usually disappear within 5 days of birth, but they may leave dark marks on the skin for several months.
The spots usually appear on the following body parts:
- forehead
- neck
- upper chest
- chest
- thighs
- small of the back
Is it an allergic reaction?
Allergic reactions can cause raised, swollen bumps, or hives, to appear on the skin. People do not tend to confuse hives with acne. This is because hives is very uncommon under 6 weeks old, does not look like acne, and is usually not confined to the face, neck, and upper chest back as baby acne is.
People do not tend to confuse hives with acne. This is because hives is very uncommon under 6 weeks old, does not look like acne, and is usually not confined to the face, neck, and upper chest back as baby acne is.
Share on PinterestProducts for adult skin can be harmful to babies.
Babies’ skin is thinner than adults’ skin and has fewer oil glands. This makes their skin more vulnerable to injury and irritation.
Adult acne remedies can irritate babies’ sensitive skin. Caregivers should avoid using OTC remedies unless a dermatologist or pediatrician suggests otherwise.
To treat baby acne at home, keep the skin clean but do not overmoisturize it. A gentle cleanser for sensitive skin can help. Avoid touching or picking at acne, which can make it worse and cause infections.
For most young babies, the fewer things that touch their skin, the better. However, if the baby has dry skin and a face moisturizer may work, it is best to use one that manufacturers have specifically designed for use on baby skin.
Though there is no clinical evidence supporting this claim, some caregivers claim that a breast milk remedy can work. Breast milk is rich in antibodies, and some believe that applying it to a baby’s acne can help clear it up more quickly.
Baby acne typically goes away on its own within a few weeks. If it does not go away, or if it gets worse, a person may wish to consider seeing a doctor.
Exposure to certain maternal hormones usually causes baby acne, which means that there is nothing specific that a caregiver can do to prevent it.
However, a few strategies can prevent acne from getting worse and reduce the risk of developing acne between 3 and 6 months:
- Avoid using oily skin care products.
- Monitor how various skin care products affect a baby’s skin. It is important to note that some babies are very sensitive to fragrances.
It can be difficult to tell baby acne from other types of rash, such as contact dermatitis, eczema, and erythema toxicum.
When other symptoms accompany the acne or another skin condition, talk to a doctor. Sometimes, a change to the condition of the skin can warn of a more serious problem, such as an infection or a problem with a baby’s hormonal system.
For most babies, acne is only temporary and will go away on its own. Caregivers who are unsure or who are concerned that their baby’s acne is very severe should see a doctor.
Common Baby Rashes: Eczema, Allergies, Baby Acne
October is Eczema Awareness Month. Here at Ready, Set, Food!, we're dedicating the month to answering common questions about eczema and sharing eczema care tips.
Today, we're covering how to identify whether your baby's rash is eczema, or whether it has another cause.
Is baby's rash eczema? There are many reasons your baby could have a rash. Eczema is one reason, but allergies, viral illnesses, and even heat can cause rashes as well.
How can you tell the difference? Today, we'll cover how to identify 8 common baby rashes.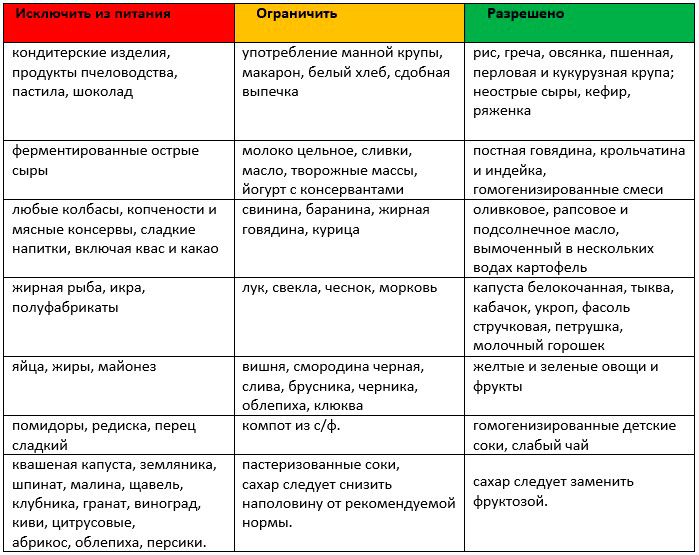
If you're not sure what's causing baby's rash, your pediatrician is your best source of guidance.
Be ready to tell your pediatrician about any other symptoms that came with the rash, as well as any food or environmental triggers that could have caused the rash.
They may refer you to a dermatologist or allergist if the rash is suspected to be from eczema or a food allergy.
How to tell the difference between baby rashes?
1. Eczema rash (atopic dermatitis rash)
What causes it: Eczema is a chronic condition that weakens a child's skin barrier. It causes baby's skin to "flare up," or develop a rash, when exposed to certain irritants.
Some irritants that may cause flare-ups include dry skin, dry air, rough fabrics (like polyester, nylon, or wool), fragrances, dyes, chemicals and metals.
Food allergens and environmental allergens can also cause eczema to flare up.
What the rash looks like: Eczema rash is a dry, rough, flaky, and itchy rash. It can cause patches of rough, itchy skin, dry and inflamed skin, or crusty, scaly bumps that can sometimes leak fluid.
It can cause patches of rough, itchy skin, dry and inflamed skin, or crusty, scaly bumps that can sometimes leak fluid.
On children with lighter skin, eczema rash will be red.
On children with darker skin, eczema rash is usually brown, purple, or gray. The rash may be harder to see, but the skin will still seem dry.
Eczema rashes can appear anywhere on the body. But they will most often appear on the elbows, knees, arm joints, leg joints, forehead, or cheeks.
Eczema rashes are never raised.
Other symptoms of eczema: Eczema will make your child's skin itchy. Mild eczema itching won't interfere with daily life, but moderate eczema may disrupt sleep or other activities, and severe eczema will cause constant itching.
What else to know: There's no cure for eczema, but you can help keep your baby's eczema under control with a daily bath, regular moisturizing, and other parts of an eczema care routine.
2. Contact dermatitis rash
What causes it: Contact dermatitis is another type of eczema.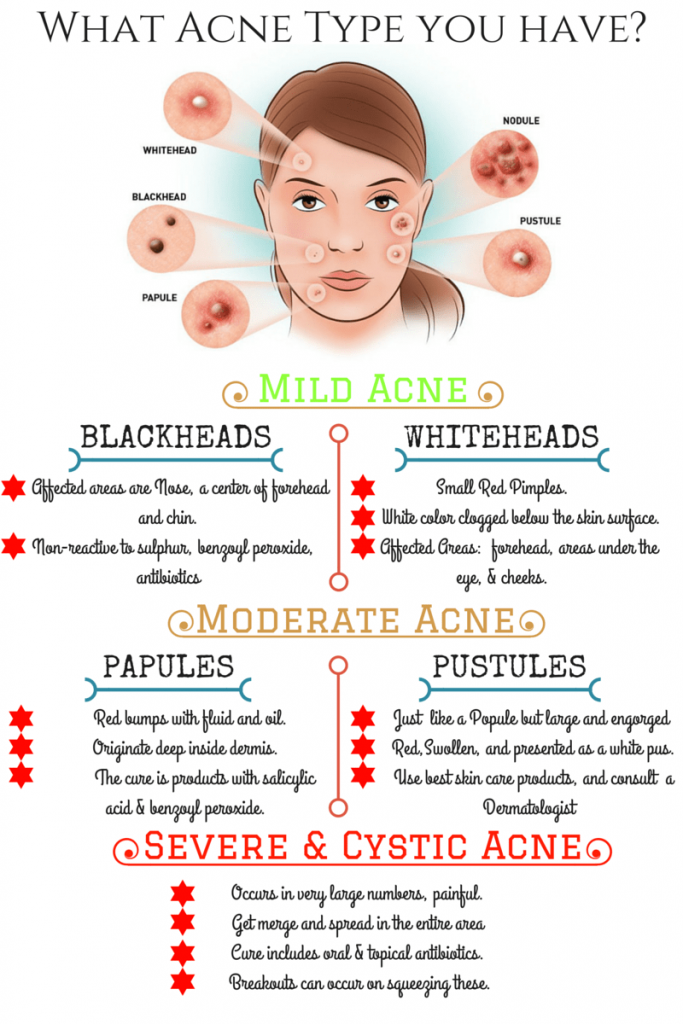 When the skin reacts to certain irritants that come in contact with it, contact dermatitis flares up. Common irritants that can cause these flares include fragrances, soaps, detergents, lotions, spit, urine and feces, and poison ivy.
When the skin reacts to certain irritants that come in contact with it, contact dermatitis flares up. Common irritants that can cause these flares include fragrances, soaps, detergents, lotions, spit, urine and feces, and poison ivy.
(Food will not cause a contact dermatitis flare-up.)
What the rash looks like: Contact dermatitis can show up as an inflamed rash, a blistery rash, or dry skin. It can sometimes swell up, crack, or peel the skin. Sometimes, the blistery rash can ooze, drain, or crust.
The rash will be red on lighter skin, and can be purple, dark brown, or gray on darker skin.
When you remove the irritant, contact dermatitis usually clears up.
Other symptoms of contact dermatitis: Contact dermatitis can cause itchiness, pain, and bleeding in rash areas.
What else to know: Diaper rash is often caused by a type of contact dermatitis, where urine and feces irritate the areas of skin where baby wears their diaper.
Learn more about how to identity rashes in newborns and babies in this video featuring Dr. Richter, a Children's Hospital of Wisconsin pediatrician at Southwest Pediatrics.
3. Food allergy rash (food allergy hives)
What causes it: When someone has a food allergy, their immune system treats the proteins in certain foods like harmful invaders. When someone eats a food they are allergic to, their immune system over-defends the body against that food's proteins, and triggers symptoms of an allergic reaction.
A food allergy rash is one of the most common food allergy symptoms, and is often the first symptom to appear.
What the rash looks like: A food allergy rash is raised, very itchy, and often rounded.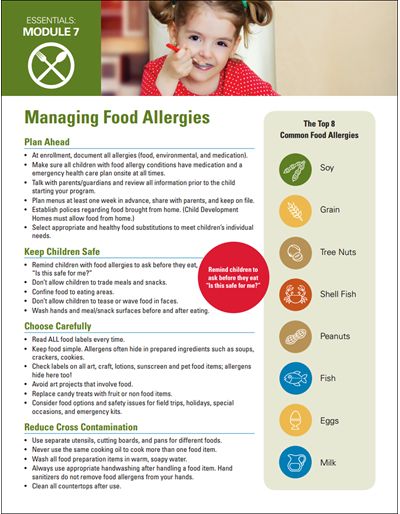 It can appear anywhere on the body.
It can appear anywhere on the body.
On children with lighter skin, the bumps will be red. These raised bumps will often have rash flares around them.
On children with darker skin, the raised bumps will usually be the color of the person's skin, but can sometimes be subtly red or darker red.
A food allergy rash could appear anywhere on the body.
Like other symptoms of a food allergy, it will usually appear seconds to hours after someone eats a food that they are allergic to.
When a food allergy reaction is mild, the rash will be concentrated on one area of the body.
When a food allergy reaction is severe, the rash will spread all over a person's body. Severe food allergy reactions require immediate emergency attention and an Epi-pen injection.
The rash will usually clear up within several hours to a day, and will almost always last no longer than 48 hours.
Other symptoms of food allergies: Besides the raised rash, the most common food allergy symptoms in babies are vomiting and swelling.
Itchy, red, and watery eyes, congestion, coughing, and stomach pain are some of the other food allergy reaction symptoms.
You can find our full breakdown of the mild and severe symptoms food allergies can cause here.
What else to know: Food allergy reactions cause swelling and vomiting, and eczema flares don't cause those symptoms.
Food allergy reactions are also reliable and timely. Someone who is allergic to a food will develop an allergic reaction every time they eat that food. Reaction symptoms may vary, though, and may not always include a rash.
For more on identifying a food allergy rash, don't miss our essential guide.
We also break down all the differences between a food allergy rash and eczema flare-up in another article.
4. Fifth disease
What causes it: Fifth disease is a mild viral infection caused by parvovirus B19.
What the rash looks like: Fifth disease is often called "slapped cheek disease" because it causes a flushed-looking rash to appear on baby's cheeks.
This flushed rash is the rash's first stage. It looks bright red on lighter skin. On darker skin, it looks subtly red, reddish-purple, or slightly lighter than the person’s skin color.
A few days later, a different type of fifth disease rash may appear. This rash will be purplish-red or reddish-brown, and appear laced and flat. It may spread to baby's trunk, arms, and legs. Sometimes, it can get itchy.
This rash may last a few days, but may also come and go for a few weeks. Heat, cold, injury or sunlight could make the rash reappear.
For an example of fifth disease on darker skin, see the image here from Brown Skin Matters.
Other symptoms of fifth disease: Even though the "slapped cheek" rash is the most well-known symptom of fifth disease, other symptoms usually appear first:
- Low fever
- Congestion
- Runny nose
- Sore throat
- Headache
- Nausea
- Fatigue
What else to know: Viral illnesses like fifth disease cause rashes and fever. Food allergies and eczema cause rashes, but don't cause fever.
Food allergies and eczema cause rashes, but don't cause fever.
For our complete guide to fifth disease, please click here.
5. Sixth disease (Roseola)
What causes it: Sixth disease (roseola) is another viral illness that is usually mild. Usually, it’s caused by human herpesvirus 6. Less often, it’s caused by human herpesvirus 7 or another virus.
What the rash looks like: Roseola rash is dotted. It's usually raised, but could be flat. It is usually not itchy.
The rash appears rose-colored on children with lighter skin, and darker red, purple, or the color of the skin on children with darker skin.
It starts out on baby's stomach, then spreads to the torso, neck, back, and other parts of the body.
It usually lasts for a few hours to a few days.
For Roseola on darker skin, see the image here, from Brown Skin Matters.
Other symptoms of roseola: Usually, a baby with roseola will experience a sudden, high fever (102-105 degrees Fahrenheit) before the rash or any other symptoms.
Roseola may also cause congestion, sore throat, coughing, runny nose, swelling of the neck, and other cold-like symptoms.
What else to know:
About 10-15 percent of children with roseola experience seizures from the sudden, high fever. They aren't harmful, but may cause arm and leg twitching and loss of consciousness. Seek medical attention immediately if your baby has a seizure.
For everything else you need to know about sixth disease (roseola), our guide has you covered.
6. Hand, foot and mouth disease
What causes it: Hand, foot, and mouth disease is a mild, common and very contagious viral illness. It is caused by the coxsackievirus.
What the rash looks like: Like the name describes, the illness causes a rash that clusters on the palms of hands and soles of feet. It also causes sores (rashes) inside the mouth.
But sometimes, the rash can also show up on baby's knees, elbows, and behind.
On babies with lighter skin, the rash appears dark red.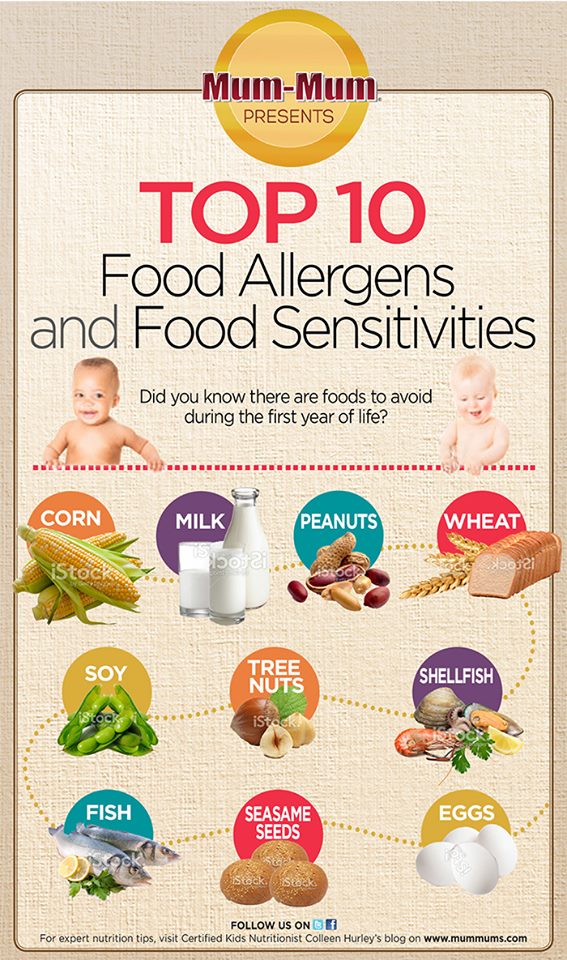 On babies with darker skin, the rash appears skin-colored, reddish-purple, or white.
On babies with darker skin, the rash appears skin-colored, reddish-purple, or white.
It's not an itchy rash, but it often gets blistery.
For Hand, Foot, and Mouth on darker skin, see the image from Brown Skin Matters here.
Other symptoms of hand, foot and mouth disease: With hand, foot and mouth disease, a fever usually starts a few days before the rash.
Hand, foot and mouth disease may also cause a sore throat and a loss of appetite.
What else to know: Viral illnesses like hand, foot and mouth disease cause rashes and fever. Food allergies and eczema cause rashes, but don't cause fever.
For more on identifying and treating viral rashes like hand, foot and mouth disease, please read this guide.
7. Baby acne (neonatal acne)
What causes it: We don't yet know what causes baby acne. But it's thought to be the presence of the mother's hormones in their bloodstream, left over from their time in the womb.
What the rash looks like: Baby acne looks very similar to teen and adult acne. It causes pimples (small, hard, raised, often red bumps) to develop on baby's face, neck, back, and chest. Sometimes, the pimples are surrounded by small inflamed areas, and sometimes, whiteheads appear on the bumps.
Other symptoms of baby acne: There are no other symptoms of baby acne.
What else to know: Baby acne usually appears between 2 and 4 weeks of age, but could develop any time before 6 weeks of age.
For more details about baby acne, please read our guide.
8. Heat rash
What causes it: Heat rashes suddenly appear on baby's skin when it's exposed to heat on hotter days.
What the rash looks like: Heat rash is a prickly rash that looks a lot like acne. It can be red, gray, or white. It usually appears on the face, armpits, wrists, and legs, as these parts of the body heat up most quickly.
Other symptoms: The only other symptom of heat rash is itchiness.
What else to know: Besides causing heat rash, heat can also sometimes be a trigger of eczema rash.
------------------------------
All health-related content on this website is for informational purposes only and does not create a doctor-patient relationship. Always seek the advice of your own pediatrician in connection with any questions regarding your baby’s health.
These statements have not been evaluated by the Food and Drug Administration. Products are not intended to diagnose, treat, cure or prevent any disease.
See the FDA Peanut Allergy Qualified Health Claim at the bottom of our homepage.
How to distinguish acne from allergies
Many mothers face the problem of rashes on the face in the first month of a baby's life. The first thoughts that visit that it is an allergy. Often, unfortunately, a nurse who comes for patronage can also “erroneously” convince that mommy ate forbidden chocolate or oranges. A young mother "sits down" on a diet, leaving only buckwheat and chicken breast, excluding all colored foods.
A young mother "sits down" on a diet, leaving only buckwheat and chicken breast, excluding all colored foods.
In the first three weeks of a baby's life, a rash usually appears that is absolutely not related to the foods consumed by the mother. This is neonatal acne, or newborn acne, is more common than allergies. nine0003
And why do acne occur at such an early age?
In general, acne in children is divided into several groups depending on age.
Newborn acne (neonatal acne) appear in the first three weeks after birth. It occurs quite often, in about 20% of newborns. There are different points of view about the appearance of acne in newborns. The main reason is the increased function of the sebaceous glands in response to androgens ("male" sex hormones) of the mother and the synthesis of own androgens in the newborn. This creates good conditions for the reproduction of microorganisms on the skin Propionbacterium ( Cuibacterium ) acne . The main feature of acne at this age is open and closed comedones (blackheads and whiteheads), papules, pustules (pustules). The usual places of localization are cheeks, forehead, chin, less often the neck and back. There is a variety of neonatal acne - cephalic pustulosis. It is believed that these are not quite classic acne, since usually the rashes are not in the form of comedones, but pustules (pustules) - whiteheads. Their appearance also falls on about the 3rd week of life. And cephalic pustulosis in babies is associated with the colonization of yeast-like fungi Malassezia (malassezia).
The main feature of acne at this age is open and closed comedones (blackheads and whiteheads), papules, pustules (pustules). The usual places of localization are cheeks, forehead, chin, less often the neck and back. There is a variety of neonatal acne - cephalic pustulosis. It is believed that these are not quite classic acne, since usually the rashes are not in the form of comedones, but pustules (pustules) - whiteheads. Their appearance also falls on about the 3rd week of life. And cephalic pustulosis in babies is associated with the colonization of yeast-like fungi Malassezia (malassezia).
Early childhood acne is less common than neonatal acne and may appear as early as 6 weeks during the first year of life. The reasons for their appearance are also associated with "male" hormones. The rash is not as profuse as with neonatal acne. Rash in the form of single comedones, papules, pustules.
What to do about acne in children of the first year of life?
In general, identifying acne in newborns is not a problem.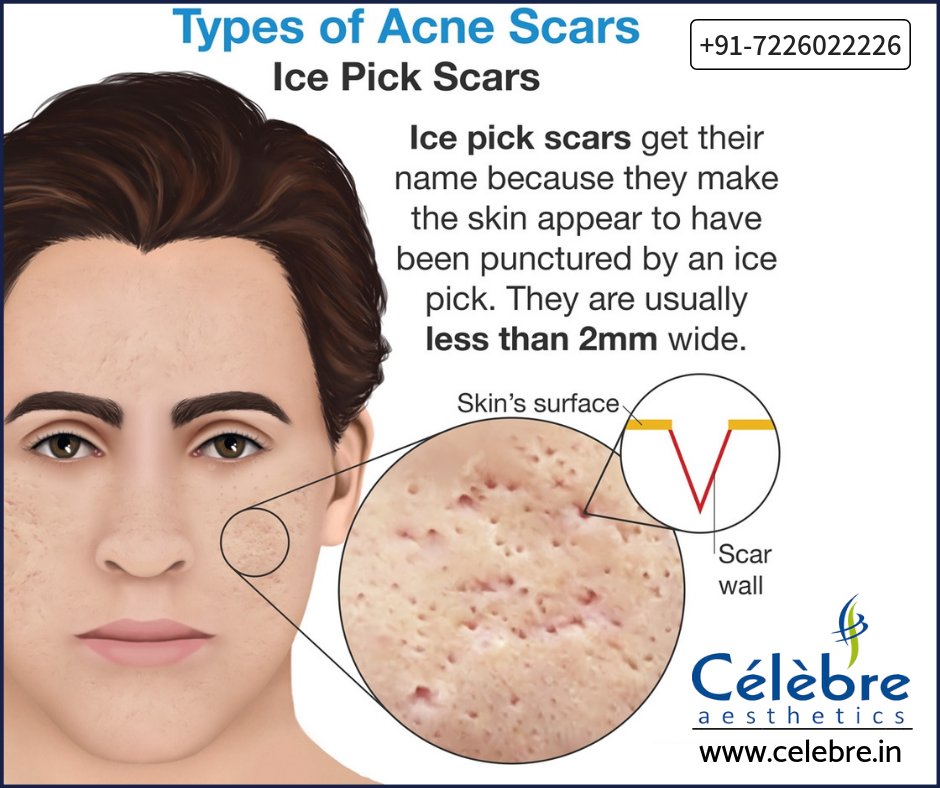 The main problem is the concern of the mother, since in most cases acne at this age does not cause discomfort to the child himself. No special laboratory tests are required. Special treatment too. Neonatal acne refers to one of those child conditions that occur in connection with the birth of a child, in connection with the child's adaptation to extrauterine life, i.e. outside the mother. Therefore, the main thing is the time and patience of the mother. Mommy doesn't need to blame herself for not resisting the "yummy" and start exhausting herself with diets. nine0003
The main problem is the concern of the mother, since in most cases acne at this age does not cause discomfort to the child himself. No special laboratory tests are required. Special treatment too. Neonatal acne refers to one of those child conditions that occur in connection with the birth of a child, in connection with the child's adaptation to extrauterine life, i.e. outside the mother. Therefore, the main thing is the time and patience of the mother. Mommy doesn't need to blame herself for not resisting the "yummy" and start exhausting herself with diets. nine0003
Usually, acne in newborns and early childhood will go away on its own within a few days/weeks, leaving no marks or scars. All that is required is careful but gentle hygiene, and the patience of the mother. Skin cleansing with gentle baby products. Unfortunately, a piece of baby soap will not work for this. It is necessary to use products with neutral ph, without alcohol and irritating components. Non-greasy cosmetics are essential. Avoid herbal decoctions, as they can additionally irritate children's skin. nine0003
Avoid herbal decoctions, as they can additionally irritate children's skin. nine0003
If acne does not go away for a long time, you should consult a doctor. For cephalic pustulosis, usually with a prolonged course, topical antifungal agents may be needed. Although for the most part, it also does not require special treatment.
You should definitely not delay a visit to the doctor if acne appeared at the age of over 1 year to 7 years - this is acne of middle childhood . By the age of one year, androgen synthesis decreases and remains at a low level until about 7 years of age. Therefore, after a year, problems with acne should go away. Otherwise, you need to look for the causes of hyperandrogenism (elevated levels of androgens). This will help the endocrinologist. In such cases, tests are usually prescribed to determine the level of hormones: free and total testosterone, dehydroepiandrosterone, luteinizing and follicle-stimulating hormones (LH and FSH), prolactin and 17-hydroxyprogesterone. nine0003
nine0003
How can you tell baby acne from allergies and other skin conditions?
Unlike acne, true allergies are rarely limited to the face, and the rash spreads throughout the body. The lesions are usually bright red, large, swollen, and may merge. In such cases, the doctor may start looking for the cause of the allergy, if necessary, prescribe allergy tests.
The appearance of acne can also suggest that it is "diathesis," a medical term for atopic dermatitis, which many consider an allergic reaction. But in fact, it is caused by disturbances in the epidermal barrier of the skin. Atopic dermatitis also begins on the face, but later, from 2-3 months of life. The infantile period is characterized by a rash in the form of large red lesions on the cheeks, they are often weeping, there may be crusts. Later, rashes appear on other parts of the body, buttocks. Atopic dermatitis causes discomfort to the child due to itching. nine0003
The main thing, when any rashes appear in a child, is to observe the general condition of the baby, measure the body temperature. Often, a rash of various types, including on the face, can accompany infectious diseases, for example, parvovirus infection, roseola infantum ("sudden exanthema"), bacterial infections. Therefore, if in addition to the rash, the child is lethargic, he has a high temperature, you should consult a doctor!
Often, a rash of various types, including on the face, can accompany infectious diseases, for example, parvovirus infection, roseola infantum ("sudden exanthema"), bacterial infections. Therefore, if in addition to the rash, the child is lethargic, he has a high temperature, you should consult a doctor!
Good to know about ALLERGIC AND NON-ALLERGIC FOOD RESISTANCE (matvareoverfølsomhet)
ALLERGIC AND NON-ALLERGIC FOOD RESISTANCE ( matvareoverf ø lsomhet )
What is food intolerance?
Food immunity is the body's hypersensitivity to certain food components. With food allergies, the body's immune defenses react to the proteins contained in food as dangerous "invaders". Even small particles of an intolerant product can cause an allergic reaction. As a rule, the reaction occurs immediately after the product enters the body and takes, in some cases, serious forms. nine0003
Other types of food hypersensitivity are not a reaction of the body's immune defense, but the symptoms may be similar to allergic symptoms.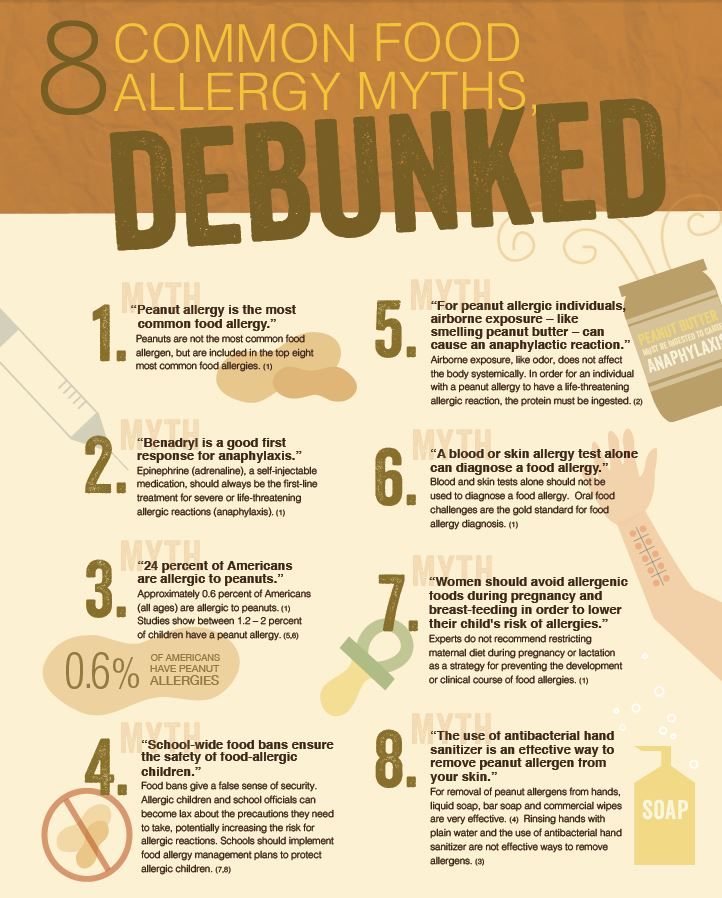 They depend on the amount of food eaten, occur a little more slowly and are less serious. The concept of "immunity" is used in cases where there is a reaction of the body to food, but the test results are normal. (There are many types of food hypersensitivity or, as it is often called, "food intolerance"). nine0003
They depend on the amount of food eaten, occur a little more slowly and are less serious. The concept of "immunity" is used in cases where there is a reaction of the body to food, but the test results are normal. (There are many types of food hypersensitivity or, as it is often called, "food intolerance"). nine0003
Prevalence of food allergy
About 5-8% of young children aged one to three years react to certain foods. Nationwide, about 5% of the population suffers from food allergies or sensitivities, including allergies that cross with pollen allergies. In addition, the problem affects many others due to the additional practical concerns for relatives and friends.
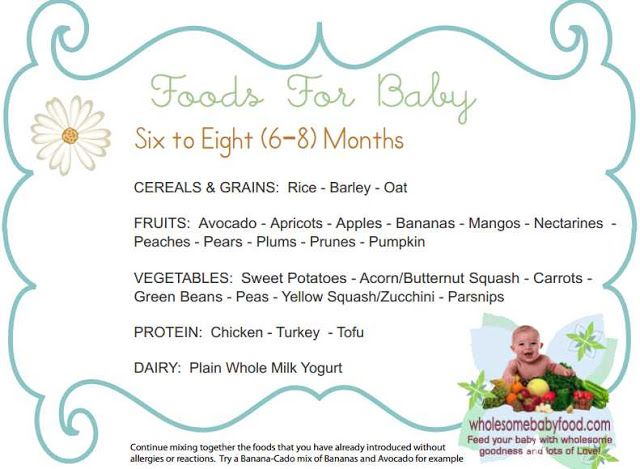
Common forms of food intolerance
In young children, the most common allergies are to milk, eggs, fish, nuts, shellfish and legumes (peas, peanuts, beans, soybeans, lupins and lentils). Children suffering from atopic eczema are characterized by an allergic reaction to citrus fruits, strawberries and tomatoes. The intensity of the reaction depends on the amount of the allergen received and, most often, consists in the appearance of itching and an eczema rash.
The intensity of the reaction depends on the amount of the allergen received and, most often, consists in the appearance of itching and an eczema rash.
In adolescents and adults, allergies to nuts (peanuts and hazelnuts) and shellfish and shellfish are common. In addition, there may be cross-reactions associated with pollen allergy to certain raw fruits and vegetables. nine0003
Allergy to wheat flour is less common, but can lead to a serious allergic reaction in children. This type of allergy rarely occurs in adults. Children and adults suffering from intestinal disorders may complain of difficulty breathing, as well as increased pain in the stomach, after eating large amounts of foods containing flour, rye and barley.
There is also the possibility of an allergic reaction to wheat and other foods only in cases where the body is subjected to physical activity after eating. This type of allergic reaction can be difficult to identify. nine0003
Celiac disease is a disease of the small intestine, often referred to as gluten intolerance, in which proteins found in barley, rye, and wheat lead to intestinal inflammation. The treatment for celiac disease is a lifelong gluten-free diet.
The treatment for celiac disease is a lifelong gluten-free diet.
Lactose intolerance is the inadequate ability of the intestinal mucosa to process lactose (the sugar found in milk and dairy products). The symptom of lactose intolerance usually does not appear at an early age, until the age of 4-10 years. Lactose intolerance is not dangerous, but it is accompanied by abdominal pain, bloating, and diarrhea after taking large amounts of milk sugar. nine0003
Symptoms
The reaction can be moderate and short-term, or severe, sometimes life-threatening. Itching in the mouth and larynx with swelling of the mucous membrane is called oral allergic syndrome, which is typical of a cross-reaction to food and often occurs in individuals suffering from pollen allergies.
Common symptoms of a gastrointestinal reaction are bloating, pain, diarrhea, nausea and vomiting. Also common, especially in young children, are skin reactions such as hives, increased eczema, and itching. Anaphylactic shock is rare but requires emergency medical attention. Its symptoms are swelling of the larynx, breathing problems, often vomiting, with a possible drop in blood pressure and loss of consciousness. nine0003
Anaphylactic shock is rare but requires emergency medical attention. Its symptoms are swelling of the larynx, breathing problems, often vomiting, with a possible drop in blood pressure and loss of consciousness. nine0003
Diagnosis
Diagnosis is usually based on Pirquet and blood tests. These tests alone are not sufficient for an accurate diagnosis and in most cases must be combined with food control. Without an accurate diagnosis, foods important to the body should not be excluded from the diet. This is especially important in cases of suspected celiac disease, where the diagnosis is almost impossible to make without a gluten-free diet. During the control period, you can exclude suspicious foods from the diet for a certain period, and then gradually introduce them back into the diet. nine0003
There are good methods for diagnosing celiac disease and lactose intolerance. However, in conventional medicine there is no single test that can establish general food hypersensitivity. In the field of alternative medicine, such tests are offered, but their correctness is not documented.
In the field of alternative medicine, such tests are offered, but their correctness is not documented.
The Children's Clinic in Voksentoppen (Barneklinikken Voksentoppen) at the State Hospital (Rikshospitalet HF) is a specialized hospital for children with allergies. There are no such specialized medical institutions for adults. They should first contact their local doctor, who can then make a referral to a specialist. For example, to a specialist in diseases of the gastrointestinal tract, lungs or an otolaryngologist. nine0003
The Regional Centers for Asthma, Allergy and Hypersensitivity handle complex case histories.
Treatment
The only treatment for food allergies is to avoid food intolerances. Most often, the most reliable way is self-cooking. Read the list of ingredients carefully when using prepared products. When visiting restaurants and catering places, it is important to clarify the content of dishes, as well as to inform in advance about allergies or hypersensitivity to certain products.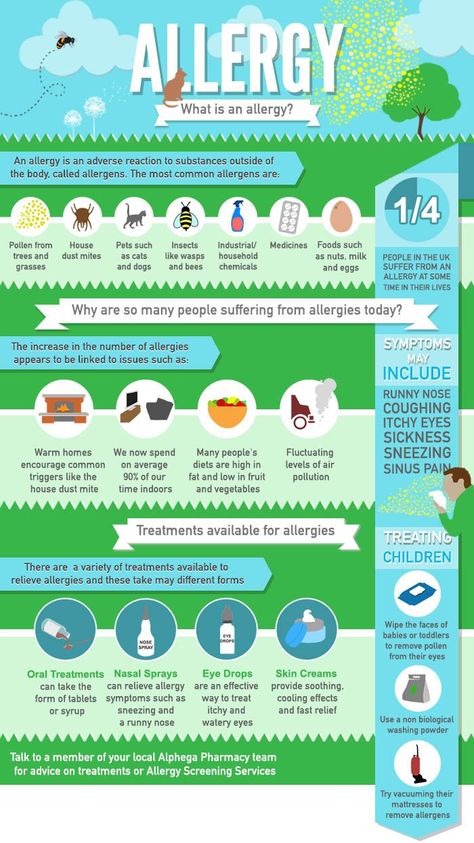 nine0003
nine0003
Proper selection of nutrition is very important, especially in childhood. Nutrients found in excluded foods need to be replaced. With milk allergy, care must be taken to ensure sufficient intake of calcium, iodine and vitamins B. It should be ensured that young children receive sufficient amounts of protein.
Children (under 3 years of age) who are allergic to cow's milk should be given a complete cow's milk substitute (available from a pharmacy with a prescription). When following a diet with the exclusion of wheat flour from the diet, it is necessary to monitor the receipt of a sufficient amount of proteins, fibers and minerals. Avoiding many fruits and vegetables can lead to a lack of vitamin C in the body. Your doctor may refer you to a specialist physiologist for individual nutritional advice. nine0003
Medications
People with severe, life-threatening allergic reactions should carry an epinephrine syringe (Epipen or Jext). Adrenaline is administered as an "antidote" if a person has inadvertently taken an intolerable product.