Baby crying in pain when feeding
My baby fusses or cries when breastfeeding
By Kelly Bonyata, BS, IBCLC
© Lsantilli - Fotolia.com
Some babies will fuss, cry or pull off the breast during breastfeeding. There are a number of reasons why this might be happening. It’s pretty common to see this type of behavior at around 6-8 weeks, though it can occur at any time. If your baby is generally fussy (not just when nursing) see My baby is fussy! Is something wrong?
Determining the problem
Here are some of the problem-solving steps I go through when my baby is fussy at the breast or a mother asks me why her baby is fussing while breastfeeding:
.
How old is baby? Most babies go through growth spurts during the first few days at home and around 7-10 days, 2-3 weeks, 4-6 weeks, 3 months, 4 months, 6 months, 9 months, etc. Many babies are fussy during growth spurts.
Is baby working on anything new developmentally? Babies who are starting to notice the world around them can be notoriously distractible. Any kind of new developmental step that baby is working on can affect nursing temporarily, whether it be fussy nursing behavior or simply more frequent nursing.
When is baby fussing? To figure out the cause it’s helpful to pay attention to when the fussy behavior happens, both during the nursing session and during the day.
If baby is fussy right when your milk is letting down (or immediately after), there’s a good chance that the fussy nursing is related to a fast let-down. If baby is fussy before let-down, or a few minutes into nursing (and a while after let-down), then baby may be impatient for the fast flow of milk that comes with let-down. Fussing at the end of a nursing session (or what seems to be the end) may mean that baby needs to burp, or is ready to finish nursing, or just wants to suck (and doesn’t want to deal with a new let-down at this point), or wants to continue nursing on the other side or with a faster flow of milk.
If the fussy behavior is mainly in the mornings, it might be due to a faster than usual let-down if baby has just had a longer sleep period and mom’s breasts are fuller than usual. If baby is fussier during evening nursings, it may be due to the normal fussy time that most babies have during the evening. Although most babies don’t react to foods that mom eats, some do. If you eat a particular food at about the same time each day (or most days) and baby has a regular time where she fusses during nursing, try not eating that food for a week or two to see if things improve.
If baby is fussier during evening nursings, it may be due to the normal fussy time that most babies have during the evening. Although most babies don’t react to foods that mom eats, some do. If you eat a particular food at about the same time each day (or most days) and baby has a regular time where she fusses during nursing, try not eating that food for a week or two to see if things improve.
Does fussing occur on both sides equally or only on one side? Most moms have a faster let-down and/or a more abundant milk supply on one side than the other, so if your baby fusses more on one side, it may be due to these differences.
What else is going on with baby? Is she sick or teething? Is something new or different going on in her environment? Has she started solids or is she trying a new food? Is she exhibiting other symptoms besides the fussy nursing?
Below are discussions of some of the different things that can lead to fussy nursing behavior. Keep in mind that the problem may also be a combination of several things.
Keep in mind that the problem may also be a combination of several things.
Does baby need to burp?
Many babies will cry, fuss, pull off the breast, etc. if they need to burp. Try to burp between breasts and after a feeding, but don’t worry if baby does not burp and is content. Breastfed babies overall don’t take in as much air during a feeding as bottle-fed babies do, so usually don’t need to burp as often. If baby has been crying before she nurses, or is so hungry that she nurses “frantically” or if mom has a fast let-down, baby could be taking in more air and may need to be burped more often.
Burping is usually only necessary during the first few months, though it may extend longer. Once your baby is moving more freely, she will be able to relieve the gastric gas herself. This usually will occur between the 4th and 6th month, but may be shorter in some children and longer in others.
If baby has a hard time burping, try burping more often during a feeding. The best burping position is one that applies firm pressure to the baby’s tummy. Placing baby over the shoulder way up so that there is pressure on baby’s abdomen often works well. Walking around while doing this might distract her long enough to get a good burp. You may even want to lie baby down on her stomach and burp her that way.
The best burping position is one that applies firm pressure to the baby’s tummy. Placing baby over the shoulder way up so that there is pressure on baby’s abdomen often works well. Walking around while doing this might distract her long enough to get a good burp. You may even want to lie baby down on her stomach and burp her that way.
Growth spurt
Babies often pull off and fuss during growth spurts. Most babies go through growth spurts, sometimes called frequency days, during the first few days at home and around 7-10 days, 2-3 weeks, 4-6 weeks, 3 months, 4 months, 6 months and 9 months (more or less). More growth spurt information in this link.
Distractible baby
If baby seems to be pulling off the breast at any distraction (real or imaginary), then see The Distractible Baby.
Forceful let-down
Some babies will pull off the breast soon after let-down if mom has a forceful let-down. Baby may be frustrated by the too-fast flow of milk with let-down. A too-forceful let-down can also cause excessive gas or spitting up/vomiting. There is more information here on symptoms of and how to deal with a fast let-down reflex.
A too-forceful let-down can also cause excessive gas or spitting up/vomiting. There is more information here on symptoms of and how to deal with a fast let-down reflex.
Slow let-down
Some babies get very impatient if mom has a slow let-down. There is more information here on speeding up a slow let-down reflex.
Baby wants a faster milk flow
Even very young babies can be quick to notice that pulling off, kneading the breast, etc. can cause an additional let-down, and can facilitate a faster, easier milk flow. Some babies become impatient with the slower milk flow following the initial fast flow at let-down. This may or may not be related to a slow let-down.
When a feeding begins at the breast there are drops of milk. Then when the initial let-down occurs (several seconds to a minute into the feeding), the milk flow speeds up quite a bit. At that time it may drip very quickly, squirt, or even spray. Some minutes later it slows again and the baby must continue to suck vigorously in order to elicit further let-downs. This pattern can continue through successive, multiple let-downs as long as the baby is continuing to nurse vigorously. Eventually, baby will learn that the flow will pick back up again if she’ll only continue to vigorously suck/swallow.
This pattern can continue through successive, multiple let-downs as long as the baby is continuing to nurse vigorously. Eventually, baby will learn that the flow will pick back up again if she’ll only continue to vigorously suck/swallow.
With bottle feeding, the flow is instant and continuous. The baby is required to work very little. Once a baby has had a bottle, especially a lot of bottles, she may begin to prefer the ease of bottle-feeding over the work of breastfeeding. She may become frustrated at the breast after the first let-down occurs and the flow of milk begins to slow.
If baby is getting bottles you might consider putting them away, at least for a while. When you must use a bottle, only use a newborn nipple for as long as baby will tolerate it so that she never gets a really fast flow of milk from the bottle, but has to work a little more to get the milk.
Sometimes babies of moms with oversupply or fast let-down will also get very used to the fast flow and object when it normally slows somewhere between 3 weeks to 3 months.
It can be helpful to do some breast compression when this fussiness starts or right before you expect it to. This will help speed up the milk flow again. Once compression stops helping, try switching baby to the other side when she begins to fuss and back and forth again (after using compression) as you need to.
Baby is done nursing for the moment
If baby is fussing after she’s been nursing for a while, and you’ve ruled out other causes, she may be in the process of changing her nursing pattern. Babies become very efficient at the breast with growth and maturity. They can milk the breast in a lot less time per feeding session than they required before. Baby’s frustration may just be a sign that she’s finished and wants to move on.
On a similar note, an occasional baby will just want to suck at the end of a nursing session and the flow of milk with let-down frustrates her. You might see if offering her a finger or pacifier (if baby is older than 4-6 weeks) to suck on during these times seems to help.
Baby prefers one side
Sometimes babies will refuse or fuss at a breast when the let-down is slower or too forceful, or the supply a bit lower. They in turn will prefer the side which lets down more/less quickly and in which the supply is more bountiful. See also: Lopsided! What can I do?
Fussy in the evening
Many young babies tend to pull off and fuss at the breast in the evening. See the article Cluster Feeding and Fussy Evenings.
Teething
Teething can cause fussy nursing behavior, as some babies experience gum discomfort with sucking. Baby might start to nurse, but then pull off and cry or fuss and not want to nurse anymore. See Teething for more information and tips.
Thrush
Frequent pulling off the breast can be a symptom of thrush.
Stuffy nose
A stuffy nose can cause fussy nursing behavior. If your baby has a stuffy nose and is having a hard time breathing and nursing at the same time, see colds & congestion.
Allergy or food sensitivity
Some babies with allergies or food sensitivities exhibit fussy nursing behavior. Often when there is a sensitivity to something in mom’s diet, baby will come to the breast hungry but when she tastes/smells something in the milk that will cause her GI distress, she pulls off, bats her head back and forth, etc. Sensitivities to foods in mom’s diet are rare. If this is the problem, you will most likely notice other symptoms, such as excessive spitting up or vomiting, colic, diarrhea, rash, persistent congestion or runny nose, or excessive gas. More information on food sensitivities in babies and links to more allergy information can be found in my article Dairy and other Food Sensitivities in Breastfed Babies.
Low milk supply
Low milk supply can cause baby to be fussy at the breast. If you feel that your milk supply may be low, see this page for more info: Increasing low milk supply.
Reflux
Reflux can result in baby being fussy at the breast. See Reflux and Breastfeeding for more information.
See Reflux and Breastfeeding for more information.
Tongue-Tie
Tongue-Tie can result in baby being fussy at the breast. See Breastfeeding a Baby with Tongue-Tie (Resources) for more information.
The Distractible Baby • KellyMom.com
By Kelly Bonyata, BS, IBCLC
- Is my baby distractible?
- What can I do about it?
- Additional Information
Is my baby distractible?
Latch on, suck a moment, pull off… latch on, suck a moment, pull off. Nurse a minute, pull away to smile at mom. Nurse a minute, pull away to see who just walked in the room. Nurse a minute, pull away to listen to the TV. Nurse a moment, pull away because the dog wagged his tail.
Sound familiar?? Baby starts to nurse and just as soon as your milk starts to let-down, baby pulls off and wiggles around in your lap. Babies aged two to six months are notorious for pulling off the breast at any distraction (real or imaginary) and tend to forget to let go before they turn around (ouch!).
.
This is a passing developmental stage that can be quite a nuisance – it’s usually at it’s worst between four and five months. At around 2 months, your baby will become able to see things clearly across the room. At around 3 months, he’ll start to stay awake longer and take a greater interest in the world around him. Your baby is also beginning to recognize that he is separate from mom. All of these things can result in a distractible baby. When baby first becomes aware of the rest of the world, he will have a hard time concentrating on nursing. In effect, he will be unable to “walk and chew gum at the same time.” Once he gets a little older, he’ll find it easier to both nurse and take in the world around him at the same time.
Distractibility is also common around 8-10 months, and can lead mom to think that her baby is trying to wean. If your baby is younger than a year, it’s highly unlikely that this temporary disinterest is self-weaning. It’s very rare for a baby younger than 12 months to self-wean.
What can I do about it?
Many moms find it more and more difficult to nurse a distractible baby, and sometimes even interpret it personally (“I don’t want mom any more” or “I don’t want to nurse any more”). At the very least, it’s frustrating to deal with a distractible baby. Less frequent/shorter nursing during this distractible stage can lead to a low milk supply, so do your best to get in a few decent feedings during the day.
Until this stage has passed, baby may need a quiet place to nurse and/or more night nursing until he’s figured out how to deal with distraction. Do take advantage of night nursing during this time – it doesn’t matter when baby takes in his calories during a 24-hour period. One study showed that older babies can consume as much as 25% of their total daily intake of mother’s milk during the night, probably partly because of daytime distractibility.
Nursing in a quiet, darkened, boring room often helps. Talk in quiet, soothing tones (if you talk at all). Nurse while lying down; nap nurse. Cover baby with a shawl or put him in a sling to nurse. Nursing while in motion (walking, rocking) can also help baby to focus better on nursing. Try to catch your baby when he’s more willing, such as when he’s just waking up, already a little sleepy, or actually asleep. Baby’s initial pulling off is probably not an indication that he is finished – just an indication that he saw/heard something interesting across the room. When he pulls off, try to coax him back to the breast a few more times before giving up.
Nurse while lying down; nap nurse. Cover baby with a shawl or put him in a sling to nurse. Nursing while in motion (walking, rocking) can also help baby to focus better on nursing. Try to catch your baby when he’s more willing, such as when he’s just waking up, already a little sleepy, or actually asleep. Baby’s initial pulling off is probably not an indication that he is finished – just an indication that he saw/heard something interesting across the room. When he pulls off, try to coax him back to the breast a few more times before giving up.
If baby pulls away without letting go, keep a finger ready to break the suction as soon as he starts to pull away. You can also nurse baby in the football (clutch) hold so you have better control of his head, or nurse him in the cradle hold in a sling. This type of behavior sometimes leads to biting; if your baby bites, see When Baby Bites.
If baby is not nursing as much because of distractibility, offer the breast often (even when he doesn’t “ask” to nurse). Make up for lost time by nursing more often during the night. Older babies may nurse better if you try different and novel nursing positions in which they have more control – baby standing up, sitting on your lap facing you, etc.
Make up for lost time by nursing more often during the night. Older babies may nurse better if you try different and novel nursing positions in which they have more control – baby standing up, sitting on your lap facing you, etc.
Additional information
Wakeful 4 Month Olds by Jan Barger, RN, MA, IBCLC @
Breastfeeding as Baby Grows. This article, by Becky Flora, IBCLC, talks about baby’s different developmental stages during the first year and how they affect breastfeeding.
What is Normal? by Paula Yount discusses the variations of normal that you can expect throughout your breastfeeding experience.
My baby fusses or cries during nursing – what’s the problem? This article discusses some possible reasons for fussy nursing behavior. If you’re looking for the rest of the info that used to be on this page, it’s in this article (with more added).
Is my older baby getting enough milk? If you feel that your baby is not nursing enough, this page may be helpful.
Why does the baby cry during breastfeeding
Yakovleva Ekaterina Andreevna
pediatrician, breastfeeding consultant
Why does baby cry while breastfeeding? The answer may lie on the surface and depend on the situation. Some mothers themselves begin to put forward theories that are often incorrect - “I don’t have milk”, “I ate something wrong”, “The milk became tasteless and bitter”, “I shouldn’t have bought silicone pads” ... Consider the most frequent causes of crying at the breast and options for helping the baby together with Ekaterina Andreevna Yakovleva, pediatrician, breastfeeding consultant and mother of two babies. She knows about the tears of babies not only from professional, but also from maternal experience.
WHY A CHILD CRYS DURING FOOD
— Ekaterina Andreevna, is crying during feeding dangerous?
— Crying during feeding is a normal way for a baby to communicate with the outside world. So he calls his mother, shows that he wants to eat or something bothers him. The only thing that crying can affect is that the baby will come off the chest and take in air. This will lead to more abundant regurgitation, increased pain in the tummy.
The only thing that crying can affect is that the baby will come off the chest and take in air. This will lead to more abundant regurgitation, increased pain in the tummy.
Table. Newborn cries during feeding - 9 reasons0018
— Can a change in priorities of a child affect his behavior at the breast?
- Up to three months, babies have one priority - they need to either eat and sleep or change a wet diaper. After the children become more active, they are already interested in the world around them. Therefore, when feeding in public places, and also when the mother combines the process with talking on the phone or watching TV, the child can be distracted: suck - turn away - suck, ask for different breasts in turn, indulge.
After three or four months, the baby should not be on the breast very often, but mothers find it difficult to readjust and continue to breastfeed constantly to soothe him. But in fact, the child’s needs are already different - he wants to be vilified on the handles, paid attention to him, played with him, showed him toys.
- Let's discuss misattachment in more detail. What can a mother do wrong if the child does not eat well and cries?
- A very common symptom of improper attachment or refusal of the breast is trouble-free feeding only in sleep. When the child sleeps, he eats calmly, and when he is awake, he begins to twist at the chest, cry. Mom can get tired of this, and in order to calm and feed the baby, during the day she gives him a bottle. In such a situation, it makes sense to talk about breastfeeding and work to restore normal feeding.
Problems may arise from awkward or repetitive posture during feeding. By trial and error, the mother should choose the position that will be most convenient for her and the child. However, if a baby is fed only lying down from birth, at an older age he may refuse to eat in his arms, break out and cry.
A CHILD CRYING WHEN FEEDING - HOW TO HELP
- Ekaterina Andreevna, everything is very individual for small children. How to understand why a child eats and cries?
How to understand why a child eats and cries?
— If the baby cries during feeding, the mother should examine the possible reasons for this behavior step by step and:
- Eliminate the reasons related to the child's well-being, which she can deal with herself.
- Work on breastfeeding techniques.
- Seek medical attention if all else fails - child continues to cry and has additional questionable symptoms.
A triad of symptoms that are always alarming
You should also consult a doctor if, during feeding, the child wriggles and cries from constant acute pain, cannot calm down, vomiting, blood and mucus in the stool, rashes in the mouth, stuffy nose are observed. Fever is an acute condition that is not associated with constant (for example, for a month) baby crying during feeding.
— What should I do if my baby refuses to breastfeed?
— The main thing for a mother is to remain calm and adequate. For a breastfed baby, one break can last an hour, and another five to six hours if the baby has slept long and well. Taking long breaks during the day, the child will still finish his daily allowance in order to develop normally. For example, if he has not eaten for six hours during the daytime, he will breastfeed more often at night. Therefore, in feeding children in the first half of life during the day, it is better not to take breaks for more than 3-3.5 hours. With the introduction of complementary foods, the intervals may be slightly longer.
For a breastfed baby, one break can last an hour, and another five to six hours if the baby has slept long and well. Taking long breaks during the day, the child will still finish his daily allowance in order to develop normally. For example, if he has not eaten for six hours during the daytime, he will breastfeed more often at night. Therefore, in feeding children in the first half of life during the day, it is better not to take breaks for more than 3-3.5 hours. With the introduction of complementary foods, the intervals may be slightly longer.
Night breaks are individual and depend only on the child - some children are born with a 6-8 hour interval, and some sleep at night for eight to twelve hours or eat every hour.
Read also
- About the reasons why a child refuses breast milk and whether it is necessary to switch to mixed or artificial feeding in such cases.
— Is it necessary to stop feeding if the baby is naughty?
- Depends on age. Mom should feel what exactly the child needs at this moment. If a newborn cries and refuses to breastfeed, you can calm him down, vilify him with a column, shake him, and then attach him to the breast again. If, having calmed down, the child turns away from the chest, then he has eaten.
Mom should feel what exactly the child needs at this moment. If a newborn cries and refuses to breastfeed, you can calm him down, vilify him with a column, shake him, and then attach him to the breast again. If, having calmed down, the child turns away from the chest, then he has eaten.
An older child is distracted from the breast, becoming interested in something else. Do not force feed him. We must try to remove all irritants - feed in isolation in a separate room, not be distracted by gadgets, sounds, or give the child the opportunity to satisfy his interests, and then offer the breast again.
— What else can help calm the baby?
- Since most causes of crying are not related to medical problems, medication is not needed. It is necessary to relax, set up the baby, pump him, try to competently organize breastfeeding - apply correctly, do not give a dummy, nipple, supplement from a cup or syringe without a needle. As a rule, this is how most feeding problems go away.
— In what situations can a breast be replaced with a bottle?
— It is not worth replacing breastfeeding with formula feeding without acute vital signs. When a baby is not accepting the breast well, it is worth removing all bottles, continuing to supplement with “non-sucking” items, and contacting a breastfeeding specialist to try to establish attachment and breastfeeding. This is done by a lot of people.
- Does changing the feeding regimen help to get rid of crying?
- Rather, these are unrelated things. It is not worth forcibly adjusting the feeding regimen, you need to listen to the child - in the first three months, the children constantly hang on their chest, after they begin to form a regimen and the intervals between meals increase. It is important to feel the needs of the child, because not only hunger, but also other things can disturb him, and if he constantly poke his chest, he will not be very pleased.
Table.
 Mistakes during breastfeeding
Mistakes during breastfeeding The baby cries during breastfeeding for many reasons. It can be improper attachment to the breast, "tangled nipples", inflammatory diseases of the oral cavity, runny nose, colic, teething, lactase deficiency, or a very nervous state of the mother. It is possible to understand what the problem is only by eliminating the organic and psychological causes of crying. With prolonged ongoing anxiety, the child should be shown to a specialist.
* Breast milk is the best food for babies. WHO recommends exclusive breastfeeding for the first 6 months of a child's life and continued breastfeeding after complementary foods are introduced until the age of 2 years. Before introducing new products into the baby's diet, you should consult with a specialist. The material is for informational purposes and cannot replace the advice of a healthcare professional. For feeding children from birth. The product is certified.
#advice for mom #breastfeeding
See also
The baby is not full of breast milk: how to determine it and what to do
#Food #breast-feeding #supplementing formula while breastfeeding
Shcherbakova Alla Anatolyevna
Candidate of Medical Sciences, pediatrician, gastroenterologist
Infant feeding patterns - what to choose
#Tips for Mom #breastfeeding
Kizino Polina Alexandrovna
pediatrician, perinatal psychologist
Why does the baby not sleep after feeding?
#Tips for Mom #breast-feeding #colic #gaziki 7-12
Nikulina Anastasia Anatolyevna
pediatrician
See all
View all
Why does the baby not sleep after feeding?
# Tips for mom # grudnoe-vskarmlivanie # breast-feeding # colic #koliki # gaziki 7-12
Nikulina Anastasia Anatolyevna
pediatrician
The baby is not full of breast milk: how to determine it and what to do
# Lure # breast-feeding # grudnoe-vskarmlivanie # formula supplementation while breastfeeding
Shcherbakova Alla Anatolyevna
Candidate of Medical Sciences, pediatrician, gastroenterologist
Infant feeding patterns - what to choose
# Tips for mom # breast-feeding #grudnoe-vskarmlivanie
Kizino Polina Alexandrovna
pediatrician, perinatal psychologist
See all
View all
View all
View all
Solutions to six breastfeeding problems in the first week
Are you having difficulty breastfeeding your newborn baby? Read on for expert advice on tackling the main challenges of the first week of breastfeeding.
Share this information
Cathy Garbin, child health nurse, midwife and lactation consultant:
Cathy, a mother of two, was a seven-year research fellow at the renowned Human Lactation Research Institute, founded by Peter Hartmann, providing support to breastfeeding mothers in clinics and at home. Today, she still works as a family counselor, and also conducts seminars for attending physicians and speaks at international conferences.
Breastfeeding is not always easy, so if
You are having difficulties, know that you are not alone. A US study found that out of 500 new mothers surveyed, 92% experienced breastfeeding problems by the third day. 1 Fortunately, most early breastfeeding problems are easy to resolve. Below you can read recommendations for solving the main problems that mothers often face in the first week of feeding.
Problem #1. Breastfeeding hurts!
Pain during feeding is usually associated with tenderness or inflammation of the nipples, especially when milk "comes" on the second to fourth day after birth.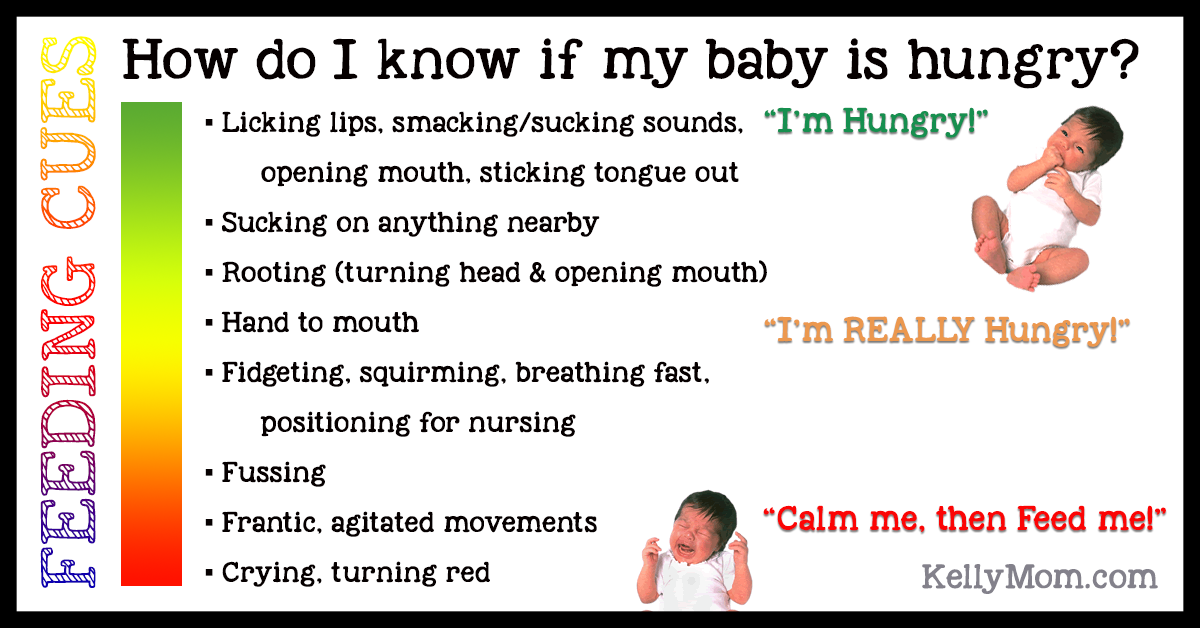 2 The baby will beg for a breast every couple of hours and this can quickly aggravate the problem: some mothers have cracked, bleeding or blistering nipples. This is, of course, very annoying.
2 The baby will beg for a breast every couple of hours and this can quickly aggravate the problem: some mothers have cracked, bleeding or blistering nipples. This is, of course, very annoying.
Solutions 3
- Check baby's latch on. An incorrect latch is one of the most common causes of pain during breastfeeding. A newborn baby should take most of the lower half of the areola (dark skin around the nipple) into his mouth, and your nipple should rest against his palate, supported from below by the tongue.
- Contact a lactation consultant or healthcare professional to make sure your baby's mouth and torso are properly positioned during feeding and there are no other latch-on problems. The doctor may also examine the baby's mouth for physical abnormalities.
- Try other feeding positions. Reclining, cross cradle, under-arm, or lying positions can relieve pressure on the most painful areas of your breasts.

- Gently wipe soaked nipples with water-dampened cotton swabs after each feed to remove milk residues that can cause infection.
- Air dry nipples or pat them dry with a clean, soft muslin or flannel cloth to prevent bacterial growth in a humid environment. Use disposable or reusable bra pads to absorb leaking milk and remember to change them regularly.
- Soften your nipples. An ultra-pure lanolin treatment will help relieve inflammation and dry skin. You can also apply a few drops of your own breast milk to your nipples. In both cases, you do not have to wash your breasts before the next feeding. You can also apply refrigerated hydrogel pads* to your nipples. They soothe the nipples and help relieve pain during feeding, as well as speed up healing.
- Protect your nipples. Nipple shields* protect the sore area from rubbing against clothing.
- Be patient. Inflammation usually resolves after a few days as your body adjusts to breastfeeding and your baby learns to suckle.
- Seek medical attention, if pain during feeding does not improve after a few days. Constant inflammation of the nipples may indicate an infection that requires prompt treatment.
Problem #2. Baby doesn't latch on properly
Some newborns do not latch on properly right away. Maybe both of you just need more time to learn how to breastfeed, or maybe the baby was born prematurely, feels unwell after a difficult birth, or mom has flat or inverted nipples.
Solutions
- Contact a lactation consultant or healthcare professional, , who can help identify the cause of the problem and suggest solutions.
- Flat or inverted nipples must be pulled out. Nipple formers* fit comfortably in the bra and apply gentle pressure to the nipples to help them come out for easier feeding.
- Try different positions and ways to support the newborn. The baby needs to feel supported.
 He needs to be comfortable and breathe freely in order to suckle properly. Do not hold the child by the head and do not put pressure on it. Lean back and let your child take the lead. This stimulates his natural reflexes and helps him find and latch on to his breasts. 4
He needs to be comfortable and breathe freely in order to suckle properly. Do not hold the child by the head and do not put pressure on it. Lean back and let your child take the lead. This stimulates his natural reflexes and helps him find and latch on to his breasts. 4 - When feeding, try to find the optimal position. Instead of putting your baby on and off, stressing both of you, try positioning your baby in a way that is easy and comfortable. Hold the torso and legs of the baby close to you, support him by the shoulders and hold him firmly so that he feels safe. Let the baby's head rest freely on your arm so that he can tilt it back slightly and breathe freely. The chin should be pressed against your chest. If these small adjustments don't make feeding more comfortable for your baby, seek help from a lactation consultant or healthcare professional.
- Use nursing pads. If your baby is having difficulty latch-on, a lactation consultant or healthcare professional may suggest trying nursing pads*.
 A nipple with an overlay is more convenient to take in the mouth, so it is larger and more rigid. Do not use nursing pads for a long time.
A nipple with an overlay is more convenient to take in the mouth, so it is larger and more rigid. Do not use nursing pads for a long time.
Problem #3. Not enough breast milk
You will not produce much breast milk at the very beginning, because the hormonal changes that trigger milk production are slow and do not end until the second or fourth day after birth. 2 You may be worried that your baby is not getting enough milk, but in the early days his stomach is still too small and feedings are frequent, so don't worry. The only things to worry about these days are excessive weight loss, too few wet and soiled diapers, or signs of dehydration in the baby. For more information on how often a newborn should urinate and void, see Breastfeeding Newborns: What to Expect in the First Week.
Solutions
- Contact a Lactation Consultant or your healthcare provider who can determine if you have problems with milk production.
 The sooner you do this, the better.
The sooner you do this, the better. - Feed your baby on demand, not on a schedule. In the first week after birth, your baby will ask to breastfeed every two to three hours (or even more often!), Both day and night. Such frequent feeding helps to establish the production of breast milk.
- Take care of yourself. It's not always easy with a newborn, but try to rest whenever you can, eat right, and accept any help around the house or with older children that your loved ones can give you to fully focus on breastfeeding.
- Try expressing milk. If a baby is feeding frequently but not gaining any weight, a lactation consultant or doctor may recommend pumping to increase breast milk production. If milk is not coming out at all, you can try the Medela Symphony Dual Electric Clinical Breast Pump**. It features an Initiate program that mimics a baby's natural sucking rhythm for the first few days.
Problem #4.
 Breast full and heavy
Breast full and heavy Your breasts will become fuller and heavier as milk comes in.
If the baby suckles well and often, this should not cause any problems. However, in some women, the breasts become so full that they become hard and painful. This condition, called breast swelling, can cause discomfort. The swollen chest seems to be “burning”, now all the activity of your body is concentrated in it, resembling a busy traffic at rush hour. Fortunately, this condition usually resolves within 24 to 48 hours. However, due to the swelling of the mammary glands, the nipples can become flat and the baby may have difficulty latch-on. 5
Solutions
- Feed your baby often. Aim to breastfeed at least 8-12 times per day. This is the main way to alleviate this condition. For more tips and tricks, see the article on Breast Swelling. 6.7
- Call your healthcare provider, if symptoms persist for more than 48 hours, you have a fever, or your baby is unable to breastfeed due to swelling.

Problem #5. Milk is leaking
Breast leakage is very common in the early days of breastfeeding when milk production begins. Milk may leak from one breast while you are feeding the other, when you sleep on your stomach, or when something accidentally triggers the milk flow reflex, such as when you hear a baby crying in a store. The leakage usually stops after about six weeks.
Solutions
- Protect clothes from stains will help disposable or reusable bra pads to be used day and night.
- Don't waste precious drops! Breast milk collection pads* fit inside the bra and collect any leaking milk. This is a very useful thing when there is too much milk and the pads are not absorbing well, or when one breast is leaking while you are feeding the other. If you want to save the collected milk, use only the milk collected at the feeding. Place it in a sterile container and refrigerate immediately if you are not supplementing with it right away.
 Collected milk must be used within 24 hours. The breast milk collection sleeves should not be worn for more than two to three hours at a time.
Collected milk must be used within 24 hours. The breast milk collection sleeves should not be worn for more than two to three hours at a time.
Problem #6. There seems to be too much milk
Sometimes when milk comes in, too much is produced! In the first few weeks there may be an overabundance of milk, but usually everything returns to normal soon. 7 Up to this point, the breasts may be heavy and sore almost all the time, even immediately after a feed, and a lot of milk may leak. A strong flush can cause a baby to cough or choke, vomit immediately after a feed, have tummy discomfort, or have hard, frothy, greenish stools. These are all signs that you are having too much milk, but the problem may resolve itself as your breasts get used to the new function.
Solutions
- Express some milk by hand at the beginning of each feed to ease the force of the flush.
- Try to feed while leaning back: to help your baby control milk flow.
 The "cradle" position is also good: hold the baby obliquely by the shoulders so that the head can lean back slightly while on your arm. The torso of the baby will be located diagonally on you.
The "cradle" position is also good: hold the baby obliquely by the shoulders so that the head can lean back slightly while on your arm. The torso of the baby will be located diagonally on you. - Be kind and patient. Let your baby rest and absorb milk both during and after feeding. Don't move your baby too much or too fast, as this can make him nauseous. As the baby grows, he will learn to better cope with the rush of milk, which is likely to weaken anyway.
- Use the towel or swaddle to soak up spilled milk if the baby can't handle the flush, and place the breast milk collection pad on the other breast to catch any spilled milk.
- Contact a lactation consultant or doctor if problems persist after a few weeks . He will examine you and may suggest one-sided feedings or hourly breast changes (“breast duty”) to reduce your milk supply.
Related materials: Difficulties in breastfeeding in the next few weeks and problems with breastfeeding after the first month
Literature
1 Wagner EA et al.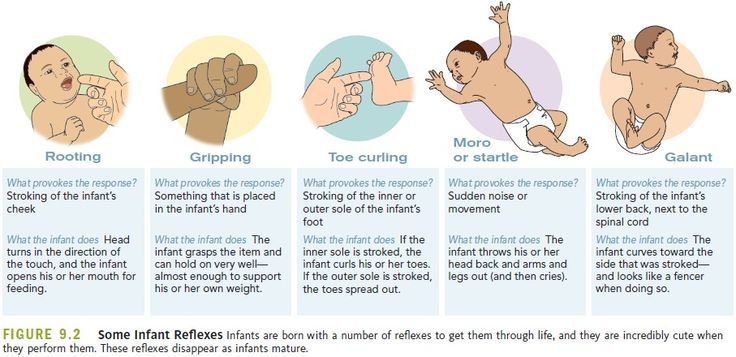 Breastfeeding concerns at 3 and 7 days postpartum and feeding status at 2 months. Pediatrics . 2013: peds -2013. - Wagner I.A. et al., "Breastfeeding Problems at Days 3 and 7 of a Child's Life and Type of Feeding at 2 Months". Pediatrix (Pediatrics). 2013:e865–e875.
Breastfeeding concerns at 3 and 7 days postpartum and feeding status at 2 months. Pediatrics . 2013: peds -2013. - Wagner I.A. et al., "Breastfeeding Problems at Days 3 and 7 of a Child's Life and Type of Feeding at 2 Months". Pediatrix (Pediatrics). 2013:e865–e875.
2 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
3 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women ’ s 2007;52(6):638-642. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
— Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
4 Colson SD et al. Optimal positions for the release of primitive neonatal reflexes stimulating breastfeeding. Early Hum Dev . 2008;84(7):441-449. - Colson S.D. et al., "Optimal Positions for Provoking Primitive Innate Reflexes to Induce Breastfeeding." Airlie Hume Dev. 2008;84(7):441-449.
5 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe Frauenheilkd. 2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations S -3 for the treatment of inflammatory diseases of the breast during breastfeeding. Geburtskhilfe und Frauenheilkünde. Med6 2014;9(5):239-243 - Amir L. H., Academy of Breastfeeding Protocol Committee, AVM Clinical Protocol #4: Mastitis, March 2014 edition of Brestfeed Med (Breastfeeding Medicine).