Baby food allergy test
Allergy testing for babies and children
About 6 million children in the U.S. have food allergies.
A food allergy is a condition that causes your child’s immune system to react to harmless proteins found in foods as if they were a dangerous virus, bacteria or other infectious agent. The reaction usually happens shortly after a food is eaten and can range from mild rashes to more serious complications.
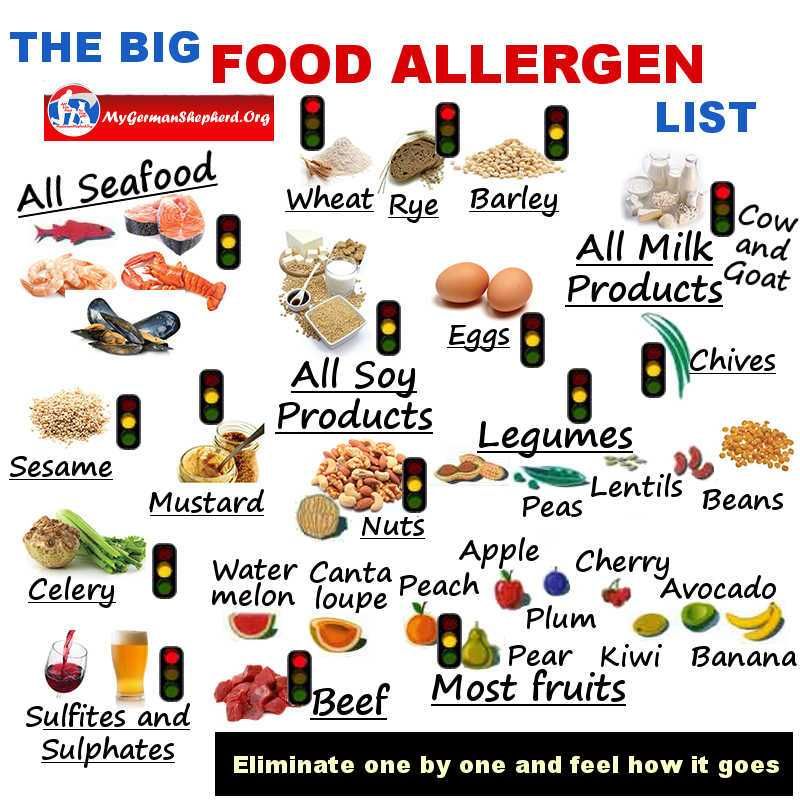
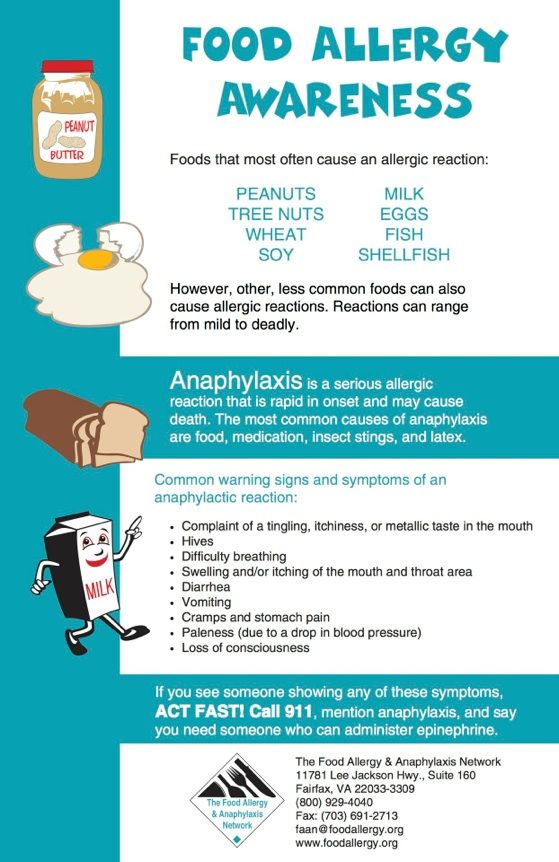
Children most often have allergies to peanuts and cow's milk. Other common allergens include eggs, soy, tree nuts (such as almonds, walnuts, pistachios, pecans and cashews), wheat, fish and shellfish (such as shrimp and lobster). Children can have symptoms when they're exposed to or eat the allergen. Breastfed infants and young children can even have allergic reactions to foods their mothers eat. Here we'll discuss signs of food allergies and how they're diagnosed in babies and children.
Signs of food allergies
Food allergies can cause symptoms, including:
- Skin problems, such as hives, itchy rashes or swelling
- Digestive issues, such as upset stomach, nausea, vomiting or diarrhea
- Respiratory problems, such as trouble breathing, wheezing, sneezing or throat tightness
- Circulatory issues, such as lightheadedness, pale skin or loss of consciousness
If your child has signs of a food allergy, see their healthcare provider. They may refer you to an allergist.
When several systems of the body are affected, the reaction may be severe or even life-threatening. This type of allergic reaction is called anaphylaxis and requires immediate medical attention.
Food allergy testing
Kids' allergy testing is similar to allergy testing in adults. Your child's allergist will ask you about your child's and your family’s health history and allergy symptoms. They'll likely want to know the following:
- The food you believe your child may be allergic to
- How much of the food they ate before they had a reaction
- Whether the reaction occurs every time your child eats the food
- The specific symptoms they experienced
- How long it took for symptoms to start after eating the food
- How long symptoms lasted
Your child's allergist will decide if your child needs allergy testing and which tests to perform.
Skin allergy tests
For a skin allergy test, your child will have a small amount of liquid food extract placed onto the skin of their back or forearm.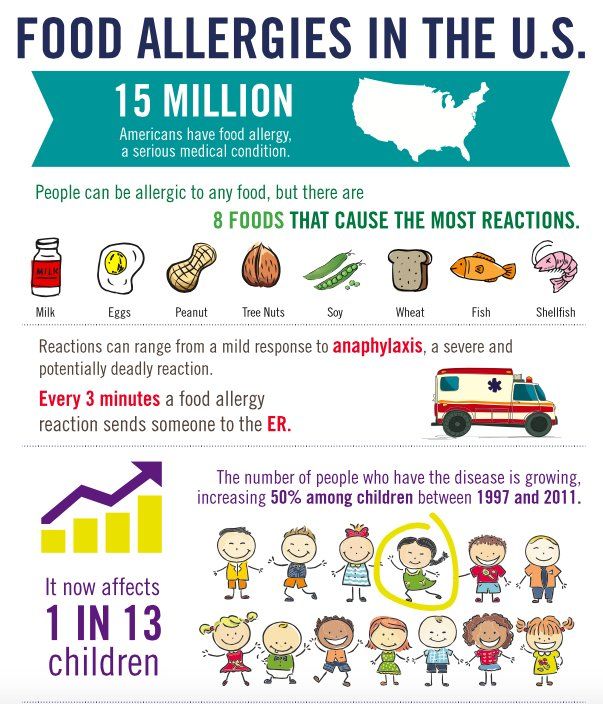 They'll receive one drop for each food they're being tested for. Next, the healthcare provider will use a needle to gently prick the areas of skin that have the liquid. This lets a small amount of the liquid food extract to get beneath their skin. If a small, red and raised bump appears 15–20 minutes later, it probably means your child is allergic to that food.
They'll receive one drop for each food they're being tested for. Next, the healthcare provider will use a needle to gently prick the areas of skin that have the liquid. This lets a small amount of the liquid food extract to get beneath their skin. If a small, red and raised bump appears 15–20 minutes later, it probably means your child is allergic to that food.
Allergy blood tests
In allergies, the immune system overreacts to an allergen and produces immunoglobulin E (IgE) antibodies. Food allergy blood tests measure the amount of IgE antibodies that develop in your child's blood after eating certain foods. For this test, a healthcare provider will take a small sample of blood from a vein in your child's arm. If the blood test is positive for IgE antibodies to a specific food, your child is likely allergic to that food.
Oral food challenge tests
Positive results on skin tests or blood tests often mean your child has an allergy to the food tested, but results aren't always conclusive. In these cases, your child's allergist may recommend an oral food challenge test to confirm their results. The challenge involves eating or drinking a small amount of the food in increasing amounts over time to see if your child has a reaction. The test is done in a doctor's office or hospital under a healthcare provider's supervision. This way, your child can receive immediate treatment if they have an allergic reaction. Oral food challenges may also be done to figure out if a child has outgrown a food allergy.
In these cases, your child's allergist may recommend an oral food challenge test to confirm their results. The challenge involves eating or drinking a small amount of the food in increasing amounts over time to see if your child has a reaction. The test is done in a doctor's office or hospital under a healthcare provider's supervision. This way, your child can receive immediate treatment if they have an allergic reaction. Oral food challenges may also be done to figure out if a child has outgrown a food allergy.
Elimination diet
To narrow the search for foods causing allergies, your child's allergist may suggest trying an elimination diet if they have mild symptoms. This involves removing all suspect foods from their diet for one to two weeks, reintroducing them one at a time and noting their symptoms. If they react to a specific food, your child may be allergic to that food. If your child is breastfed, you may need to do an elimination diet and note your child's symptoms when you remove foods from your diet and reintroduce them.
Know that food allergies can only be diagnosed by a qualified healthcare provider. While there are several at-home allergy tests available that measure IgG antibodies to foods (not IgE), according to the American College of Allergy, Asthma and Immunology, these at-home allergy tests aren't useful or effective.
Is there a gluten allergy test?
Gluten is a protein naturally found in wheat, barley and rye. It can also be found in other products, like medicines, vitamins and supplements. "Gluten allergy" is actually an incorrect term. It's often misused to describe gluten-related conditions, such as an allergy to wheat, a sensitivity to gluten or celiac disease (an autoimmune disorder where the intestinal lining can't absorb gluten and is harmed by foods that contain it). Testing for wheat allergies is the same as testing for other food allergies. To see if your child has a gluten sensitivity, their healthcare provider may suggest trying an elimination diet. For celiac disease testing, your child may need a blood test and a biopsy of their small intestine.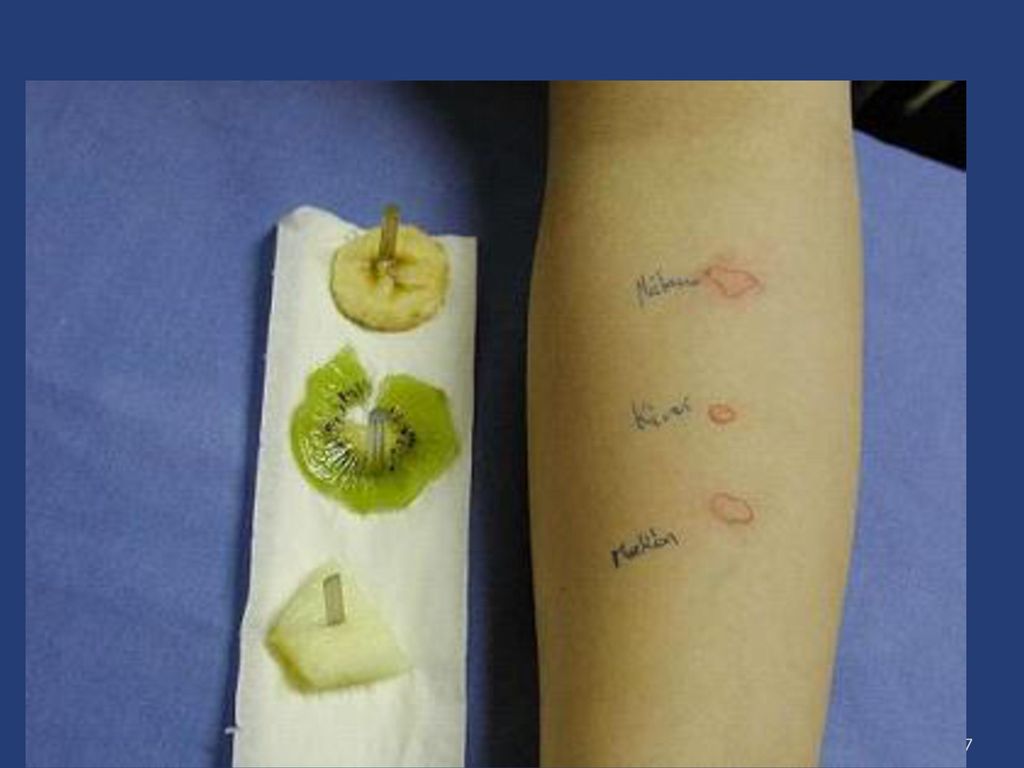
Non-food-related allergy testing
Note that children can be allergic to other things besides food. Testing for other allergens, such as pollen and mold, may be done using a blood or skin test, or with a patch test. A patch test will show if a substance, such as latex, fragrances or medications, is causing contact dermatitis or allergic skin irritation. For this test, a suspected allergen is placed onto a patch, and then the patch is placed onto your child's skin. They'll wear the patch for about 48 hours, and then their provider removes it. Irritation at the site of the patch can indicate an allergy.
Allergy testing cost
Blood tests tend to cost more than other allergy tests. In general, skin tests combined with a physical exam and information about your child's symptoms is the most cost-effective way to diagnose food allergies. To learn how much allergy testing costs, contact your health insurance provider and allergist.
If your child is diagnosed with an allergy, take heart in knowing that your child's symptoms can be managed. Work with your child's allergist to learn how to avoid their allergens and what to do if your child has an allergic reaction. Also, about 80% to 90% of egg, milk, wheat and soy allergies resolve by age 5. Your child’s allergist can perform tests to monitor their allergies and watch to see if they are going away.
Work with your child's allergist to learn how to avoid their allergens and what to do if your child has an allergic reaction. Also, about 80% to 90% of egg, milk, wheat and soy allergies resolve by age 5. Your child’s allergist can perform tests to monitor their allergies and watch to see if they are going away.
Clinically reviewed and updated March 2022.
Sources:
1. https://acaai.org/allergies/testing-diagnosis/food-allergy-testing-and-diagnosis/
2. https://medlineplus.gov/lab-tests/food-allergy-testing/
3. https://www.nationwidechildrens.org/family-resources-education/700childrens/2018/07/at-home-allergy-tests
4. https://www.healthychildren.org/English/healthy-living/nutrition/Pages/Food-Allergies-in-Children.aspx
5. https://acaai.org/allergies/allergies-101/who-gets-allergies/children/
6. https://www.aaaai.org/Tools-for-the-Public/Conditions-Library/Allergies/all-about-allergy-testing
7. https://medlineplus.gov/glutensensitivity. html
html
8. https://celiac.org/about-celiac-disease/screening-and-diagnosis/screening/
9. https://celiac.org/about-celiac-disease/screening-and-diagnosis/diagnosis/
10. https://www.mayoclinic.org/tests-procedures/allergy-tests/about/pac-20392895
When Should I Get a Food Allergy Test for My Kid? – Cleveland Clinic
Raising kids can sometimes feel like you’re in a constant state of low-level panic. What if they break an arm on the playground? Are they getting enough sleep? How much screen time is just too much?
And then there’s the fear of allergic reactions, specifically around what they eat. The Centers for Disease Control and Prevention (CDC) says that about 8% of children (1 in 13) have a food allergy.
“Can’t I just get my child tested for food allergies and take one worry off my plate (and out of my fridge)?”
Unfortunately, says pediatric allergy specialist Jackie Bjelac, MD, allergy tests don’t work that way.
“The allergy tests performed in a doctor’s office are imperfect,” Dr.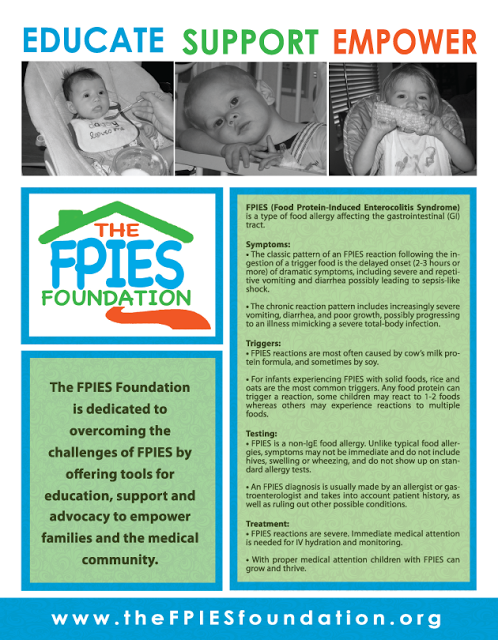 Bjelac says. “The absolute best test for food allergies is your history of reaction after you were exposed. Allergy tests should be used to confirm an allergy, not discover it.”
Bjelac says. “The absolute best test for food allergies is your history of reaction after you were exposed. Allergy tests should be used to confirm an allergy, not discover it.”
Dr. Bjelac explains when and how doctors test kids for food allergies and what to do if you suspect your child has one.
When to test your child for a food allergyThere’s no right age to test your child for allergies. The best time to consider an allergy test is after your child has eaten a food and shows signs of a food allergy.
“If you are exposed to something and don’t have symptoms, you are not allergic. There is no test that would convince me otherwise,” Dr. Bjelac states. “The opposite is also true. If a child clearly reacts to a food, but their allergy test is negative, I don’t believe the test. Exposure history trumps everything.”
Common food allergies and symptomsThese eight foods account for about 90% of all food allergies:
- Eggs.

- Fish.
- Milk.
- Peanuts.
- Shellfish.
- Soy.
- Tree nuts.
- Wheat.
Common symptoms of a food allergy in a child can include:
- A rash or hives.
- Difficulty swallowing.
- Swelling of the lips, tongue or throat.
- Wheezing or trouble breathing.
If your child is experiencing a severe allergic reaction, contact your healthcare provider immediately or get medical help right away. In rare cases, an allergic reaction can lead to anaphylaxis, a severe condition that requires quick medical attention.
Advertising Policy
Dr. Bjelac says if your child is having an allergic reaction to a food, the symptoms should be obvious.
“Allergic reactions to food are not subtle,” she continues. “If you’re thinking, ‘Well, maybe Junior isn’t sleeping well because of a food allergy.’ That’s not a thing. That can be really hard for parents, though, because sometimes, we go down rabbit holes when we’re looking out for what’s best for our kids. It’s normal to worry.”
It’s normal to worry.”
Studies call a history of allergic reactions the “cornerstone of diagnosis of food allergy.”
But why is it that we have to subject children to possible allergens and then hope they don’t break out in hives?
Research shows that current allergy tests just aren’t up to the task of reliably diagnosing food allergies for people who don’t have a history of an allergic reaction to that food. Without a history, the tests are too difficult to interpret accurately.
And inaccurate results can have a detrimental impact on your child’s well-being.
“If an allergy test indicates that your child has a wheat allergy, or an egg allergy or any food allergy, suddenly your life changes to avoid allergen-containing foods, and kids can be picky eaters as it is,” Dr. Bjelac says. “So, if that test is wrong, you’re putting them on a restricted diet when they don’t need to be. You’re avoiding nutritionally dense food that is important for their growing body and mind. ”
”
Further, labeling a child as having food allergies can come with significant effects on your child’s mental health and social life. Studies show that the fear and vigilance that comes with living with a food allergy can negatively affect a child’s quality of life.
Food is a common bonding experience among friends and family. Kids with food allergies may need to sit at a special table in the school lunchroom or miss out on cake and ice cream at a friend’s birthday party, which can be socially isolating.
“If we’re diagnosing someone with a food allergy, there are big implications for their life and their family’s lives,” Dr. Bjelac notes. “Families need to know that there is a dangerous situation if the child eats the food, not just assume there will be a problem.”
Advertising Policy
How are kids tested for food allergies?Allergy tests can be performed for kids who have a history of allergic reactions to:
- Food.
- Medication.
- Environmental allergens, like cats, dogs and pollen.
- Venoms, like bee stings.
When testing children for food allergies, Dr. Bjelac says your healthcare provider will likely use a skin test or blood test. Other kinds of allergy tests are better suited for other kinds of allergies. Patch tests, for example, are used to diagnose allergies that affect the skin, like nickel or certain ingredients in skin care products. Intradermal injections — which use a needle to inject a small amount of an allergen into the skin — are suitable for confirming allergies to medications or pollen, for example. Neither of those is used for testing food allergies.
Allergy skin testIn an allergy skin test, your healthcare provider will use a thin needle to prick the skin on your child’s forearm or back with several different potential allergens. Or your provider may place droplets of potential allergens onto their skin and use a device to scratch and lightly puncture the area.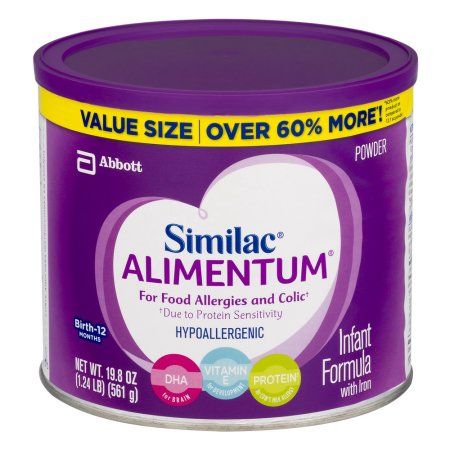 If an allergy is detected, your child’s skin will show redness, a rash or raised, round spots at the site of the allergen.
If an allergy is detected, your child’s skin will show redness, a rash or raised, round spots at the site of the allergen.
In an allergy blood test (IgE test), your provider will take a small vial of blood and test it against suspected allergens. The test measures levels of Immunoglobin E (IgE) antibodies, which are proteins your body sends out to get rid of germs. If you have an allergy, your body produces IgE in response to the allergen, even if it’s harmless. Allergy blood tests can deliver false positive results more than half of the time.
Allergy food challenge testOne of the most effective ways to test for allergies is by taking part in a food challenge test. The Food Allergy and Research organization, or FARE, calls it the “gold standard” for diagnosing allergies effectively.
In a food challenge, a child with a suspected or confirmed food allergy goes to a medical facility to be introduced to foods and monitored closely for a reaction by medical staff, who can provide treatment quickly in the case of a reaction.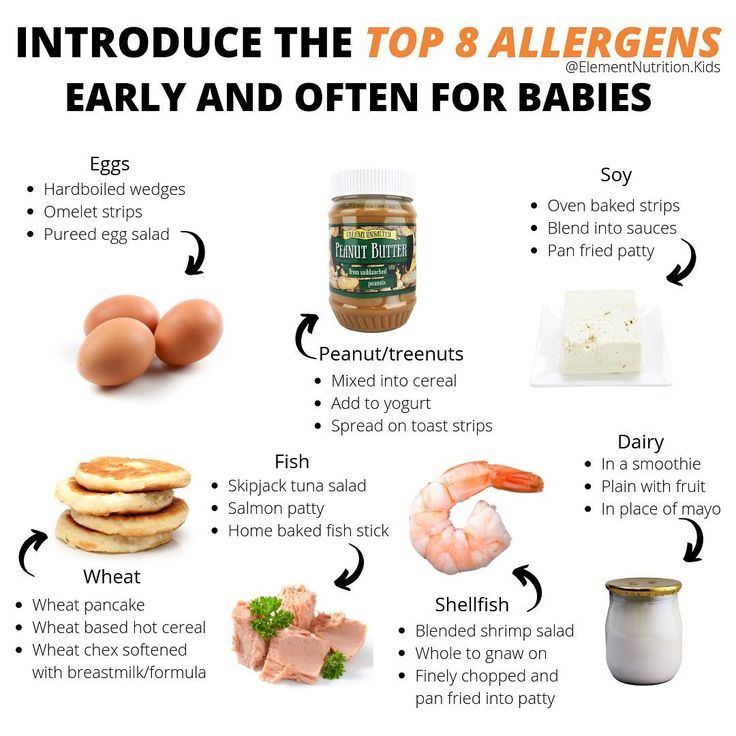 Food challenges are lengthy (usually several hours long) and usually are reserved for children at the highest risk for severe allergic reactions.
Food challenges are lengthy (usually several hours long) and usually are reserved for children at the highest risk for severe allergic reactions.
“Food challenge is a really powerful tool, especially when used in situations where we think it’s too risky to try at home,” Dr. Bjelac says.
Food challenges may also be considered in some cases where a child is suspected to have outgrown an allergy.
Talking with a healthcare providerFood allergies can be dangerous and scary for kids and their families. Monitor your child after they eat a new food, particularly ones that are common allergens. If your child has an allergic reaction, or if you suspect an allergy, don’t hesitate to contact a healthcare provider.
“If your child had an allergic reaction, reach out to a board-certified allergist to talk about what testing is appropriate based on what those possible triggers could have been,” Dr. Bjelac says.
Infant Food Allergen IgE mix fx5: Egg white, Milk, Fish, Wheat, Peanut, Soybean - f1, f2 , f3, f4, f13, f14)
Description
Method of determination Immunofluorescence assay (ImmunoCAP).
Test material Blood serum
Home visit available
Online check-in
Determination of specific IgE to six food allergens, which can most often cause the development of allergies in children. Used for laboratory confirmation of IgE sensitization in skin/food allergy symptoms. The answer is general for the mixture.
Food allergies and atopic dermatitis/eczema are most common among young children. Sometimes the causal dependence of allergic-like manifestations on certain food allergens can be established by excluding the suspected product and assessing the patient's condition after cessation of contact with him. For the same purposes, skin allergy tests and / or blood tests are used to detect specific IgE antibodies, confirming the presence of allergic sensitization to the corresponding allergens.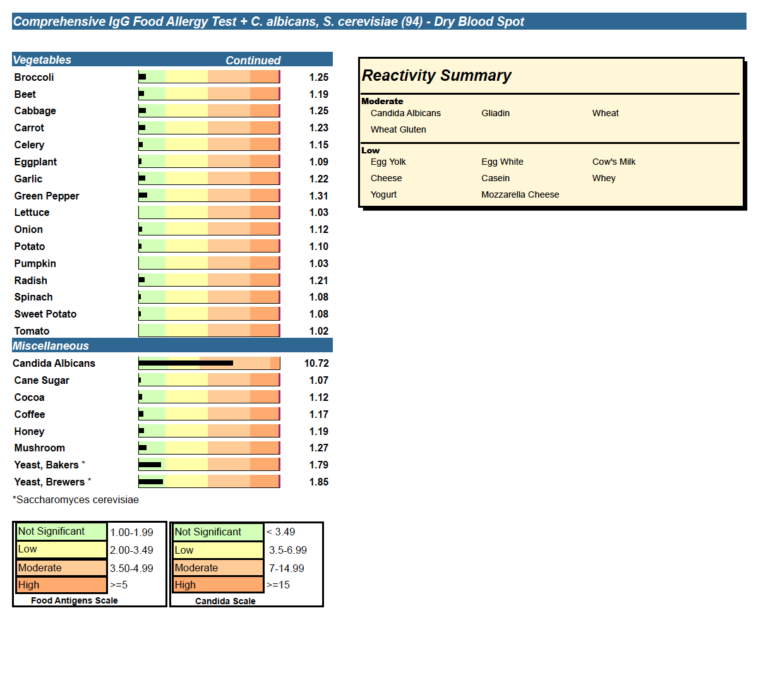 This is important for making the right recommendations for monitoring the child's condition, determining (if necessary) appropriate treatment, and timely referral to an allergist for follow-up. Food allergies and atopic dermatitis in the first years of life and familial predisposition are considered risk factors for the subsequent development of allergy to inhalant allergens ("allergic march").
This is important for making the right recommendations for monitoring the child's condition, determining (if necessary) appropriate treatment, and timely referral to an allergist for follow-up. Food allergies and atopic dermatitis in the first years of life and familial predisposition are considered risk factors for the subsequent development of allergy to inhalant allergens ("allergic march").
A test that detects the presence of specific IgE to a mixture of six common food allergens can be used in addition to clinical assessment to screen for suspected food allergies in children. If the result of this study is positive, subsequent testing should be aimed at identifying specific causative allergens and based on the patient's history, taking into account the allergens with which he comes into contact.
Preparation
Preferably 4 hours after the last meal, no requirement. Antihistamines do not affect the result. It is undesirable to conduct a study against the background of the use of glucocorticoid hormone preparations (you should consult with your allergist about the advisability of conducting a study or the conditions for canceling the corresponding drug).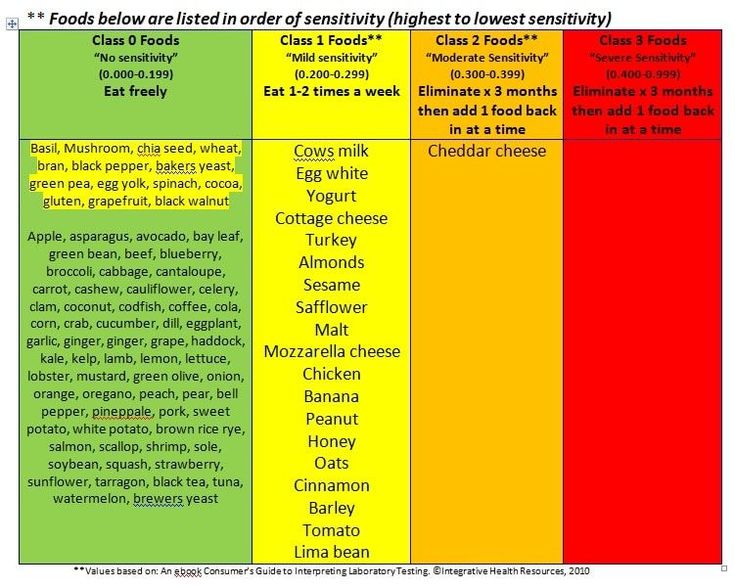
Indications for use
in the presence of allergic-like symptoms (including skin, gastrointestinal) for the purpose of screening to confirm / exclude sensitization to common food allergens listed in the mixture, which most often cause food allergies in children.
Interpretation of results
Interpretation of test results contains information for the attending physician and is not a diagnosis. The information in this section should not be used for self-diagnosis or self-treatment. An accurate diagnosis is made by the doctor, using both the results of this examination and the necessary information from other sources: history, results of other examinations, etc.
Units: kU/l.
Limits of detection: 0.1-100 kU/l.
Reference values:
Interpretation of results
Increasing levels
- A result above the specified threshold confirms the presence of sensitization to one or more food allergens in the mixture, higher values indicate the level of sensitization.
 The causative allergen should be clarified by further testing. The diagnosis of allergy is established on the basis of clinical symptoms, taking into account the patient's history and examination results.
The causative allergen should be clarified by further testing. The diagnosis of allergy is established on the basis of clinical symptoms, taking into account the patient's history and examination results. - False positive due to very high levels of total IgE.
Decreased levels
No sensitization to food allergens included in the mixture.
In this section you can find out how much it costs to perform this study in your city, read the description of the test and the table of interpretation of the results. Choosing where to take the test "Infant Food Allergen IgE, mix fx5: Egg white, Milk, Fish, Wheat, Peanut, Egg white, Milk, Fish, Wheat, Peanut, Soybean - f1, f2, f3, f4, f13, f14)" in Moscow and other cities of Russia, do not forget that the price of analysis, the cost of the procedure for taking biomaterial, the methods and terms of research in regional medical offices may differ.
Allergy in infants treatment, allergy in newborns, allergy in infants, food allergy in infants, allergic rash in infants › Outpost Clinic
(044) 502-22-62
(multichannel)62
093 / 068 / 066 / 502-22-62
info@forpost. ua
ua
License of the Ministry of Health of Ukraine
(093) 502-22-62
(068) 502-22-62
- en
- en
- UK
What is the risk of developing allergies in an infant
One of the most common causes of allergy in infants is formula milk. Despite the fact that manufacturers try to adapt milk formulas as much as possible, they still cannot be fully adapted to the child.
If the parents or relatives of the baby have allergies, asthma, allergic rhinitis, urticaria or atopic dermatitis, then through the genes they can "reward" him with a predisposition to allergies. The risk of developing an allergy in a baby to milk formula depends on the degree of predisposition of the child, the more allergies in the family, the higher the likelihood of developing an allergy:
- 10-20% - family without allergies;
- 20-40% - 1 parent is allergic;
- 50-80% - both parents suffer from allergic diseases.

For children with a predisposition to allergies, it is very important not to get cow's milk, which is very high in casein (mother's milk is much less). Therefore, attention should be paid to the fact that children prone to allergies are not supplemented in maternity hospitals with conventional mixtures, as this leads to allergization of the child from the first days, while there is a breakdown in adaptation, and further such children are more likely to develop allergies.
Manifestations of allergy in infants to milk formulas
Signs of allergy to milk protein can manifest both in the immediate type (IgE-dependent, the reaction manifests itself after the use of the milk formula during the first 30 min-2 hours), and the delayed type (IgG4 dependent) - does not appear immediately, but within one or two days. Allergy in infants to formula milk is manifested by:
- rash on the skin in the form of various dermatitis, urticaria, rash around the mouth;
- inflammation on the cheeks, buttocks, legs, back, vulva in the form of redness, papules, accompanied by itching;
- gastrointestinal manifestations in the form of vomiting, hiccups, regurgitation, stool disorders (constipation, diarrhea, bloating, intestinal colic).

What components of milk formula cause allergies in a child? 80% of milk formulas are made on the basis of cow's milk, because cow's milk in its composition is the most identical to human milk and contains the necessary proteins and trace elements for the growth and development of the child. 20% of mixtures are made on the basis of soy or goat milk.
Food allergies in infants. Allergy of children under one year to milk
Cow's milk contains proteins such as casein, lactalbumin and lactoglobulin. All three proteins can cause allergies in a child, either individually or all at the same time. Lactalbumin and lactoglobulin are thermolabile, which means that they are destroyed by boiling and can no longer cause allergies in a child. Casein, on the other hand, is thermostable (that is, it does not break down when boiled and can cause an allergic reaction). Unfortunately, most children are allergic to casein.
Diagnosis of allergy in infants you can check for allergies in infants to all the main protein components of milk. This is possible only with the help of molecular allergy diagnostics, which determines the allergy not to the entire product, but to its individual components.
This is possible only with the help of molecular allergy diagnostics, which determines the allergy not to the entire product, but to its individual components.
Allergic rash in infants. Allergy to cereals
Sometimes milk formulas may contain various cereals (buckwheat, oats, rice), then the child may be allergic to these cereals. Such mixtures are usually intended for older children - after 6 months. Accordingly, tests are made for the respective components of the cereals. You can just separately make IgE for wheat, rye and others. But it is best to do molecular component diagnostics → on the main (major) proteins of cereals (rPhl p1, rPhl p5b), which are included in buckwheat, wheat, rye, fescue and many other cereals, as well as minor (rPhl p7, rPhl p12) proteins, due to which cross-reactions with other foods and plants often occur.
What are hypoallergenic formulas and are they prescribed for allergies in infants? If initially we know that the parents are allergic and the likelihood of developing allergies in the child is high, then it is recommended to immediately start feeding with hypoallergenic mixtures, preventing the development of allergies in the child.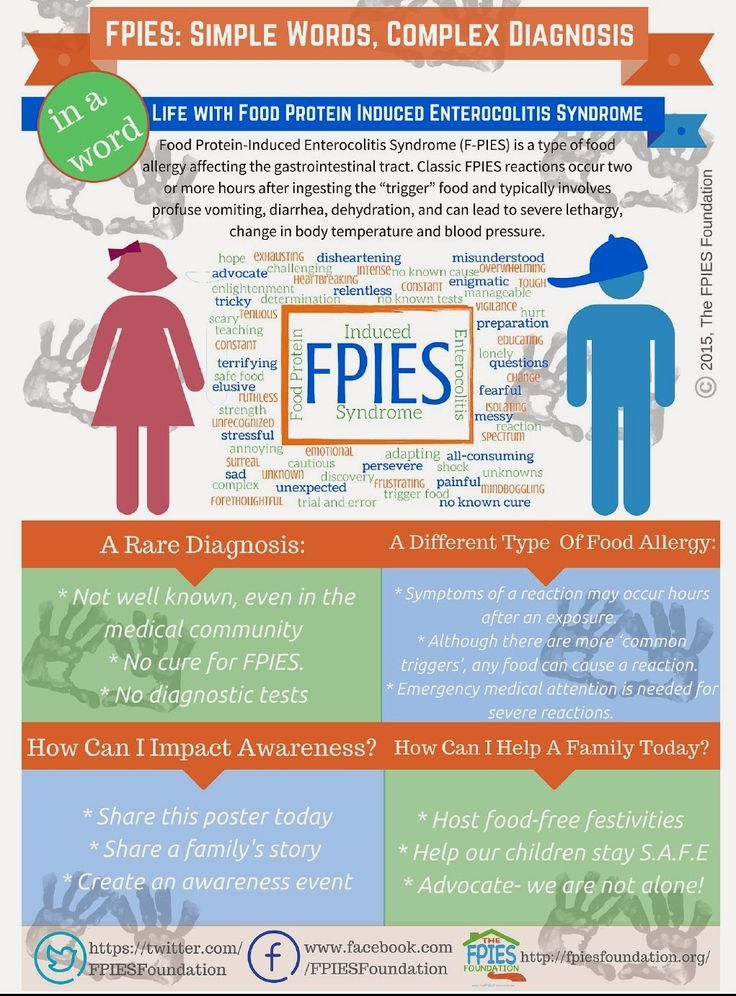
Hypoallergenic mixtures are hydrolysates of cow's milk proteins (i.e. the protein is broken down into amino acids). As a rule, there is no allergic reaction to these mixtures. But hydrolysates, due to the split protein, become bitter in taste. Therefore, at the beginning it happens that the child does not want to eat, and although his taste buds are not as developed as in an adult, he still feels a bitter taste, especially since mother's milk is sweet. Therefore, it is necessary to gradually accustom the child to the hydrolyzate, at first, in the first 3-5 days, he may refuse, and then he gets used to it. It is important that parents do not rush to cancel the mixture, as a mixture that cannot be fed to the child.
Types of hypoallergenic mixtures for allergy in an infant
There are hydrolysates depending on the degree of milk protein hydrolysis: moderate and high hydrolysates. If the baby’s allergy is not severe, then moderate hydrolysates are recommended, since they have small amounts of allergens and thus “train” and “accustom” the baby’s immune system.
Does your child have skin rashes, gastro-intestinal problems?! This is a minimally traumatic tactic for examining infants and older children. Search for the cause of problems, taking into account possible allergies.
Stages:
- Fecal analysis for a coprogram, which looks at the degree of digestion of food, signs of inflammation in the intestine, the presence of pathogenic (iodophilic) flora, etc.
- Ultrasound of the abdominal cavity, which allows you to identify possible developmental anomalies (atresia, underdevelopment of the bile ducts, deformation of the gallbladder, etc.)
- Blood test to determine the level of total immunoglobulin E and/or Phadiatop Infant. Fadiatop Infant is an allergy screening test that contains all the main foods - milk, eggs, wheat, etc., as well as inhaled allergens. If this test is positive, then component allergy diagnostics is necessary. If negative, then go to step
- Component diagnosis of allergy to casein, lactalbumin, lactoglobulin (if the child consumes only milk formula).