Baby food poisoning breastfeeding
What to Do and How to Treat It
It can seem like there’s nothing worse than food poisoning — except maybe getting food poisoning while parenting. Not only do you feel terrible, but it can feel like you can’t catch a break. The parenting must go on, multiple trips to the bathroom and all.
And if you’re a nursing parent, you may face an added stress: the uncertainty of whether you can continue.
That’s a valid worry — after all, you don’t want your child somehow catching a food-borne illness through your milk. But thankfully, having food poisoning while breastfeeding is generally not a problem, according to 2017 research.
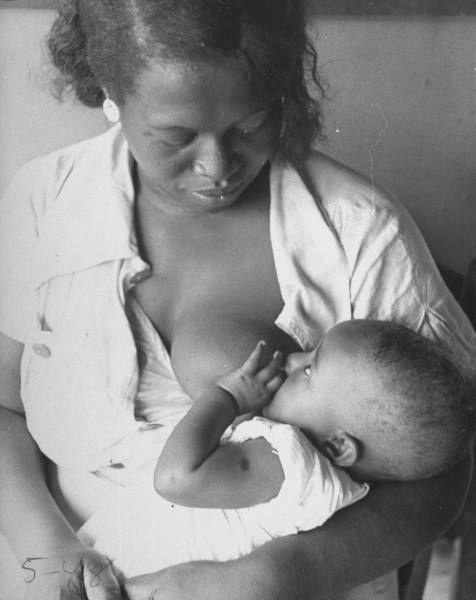
So you can (and should) keep nursing your baby.
As the Centers for Disease Control and Prevention (CDC) explains, you don’t have to stop breastfeeding when you have food poisoning, which is a non-medical term for a food-borne disease or infection.
In fact, the CDC actually recommends that you should continue breastfeeding.
But wait, there’s more: The CDC also encourages you to nurse even more frequently, while also increasing your own fluids.
Why? Because breastfeeding more frequently while you have food poisoning helps protect your baby from contracting the illness, too. It’s also excellent rehydration therapy if your baby has diarrhea.
No one wants their baby to be exposed to a pathogen that causes uncomfortable and potentially worrisome symptoms. So it makes sense to want to know about the potential risks of breastfeeding while you have a bout of food poisoning, despite expert assurance that you should continue.
Here’s what to know about the potential (but unlikely) risks of breastfeeding with food poisoning:
Danger to breastfeeding parent
Although food poisoning certainly isn’t a comfortable experience, most adults fare well and are back to health after a couple of days. However, adults who are older, immunocompromised, or pregnant may have a tougher time and may require medical attention if the situation becomes severe.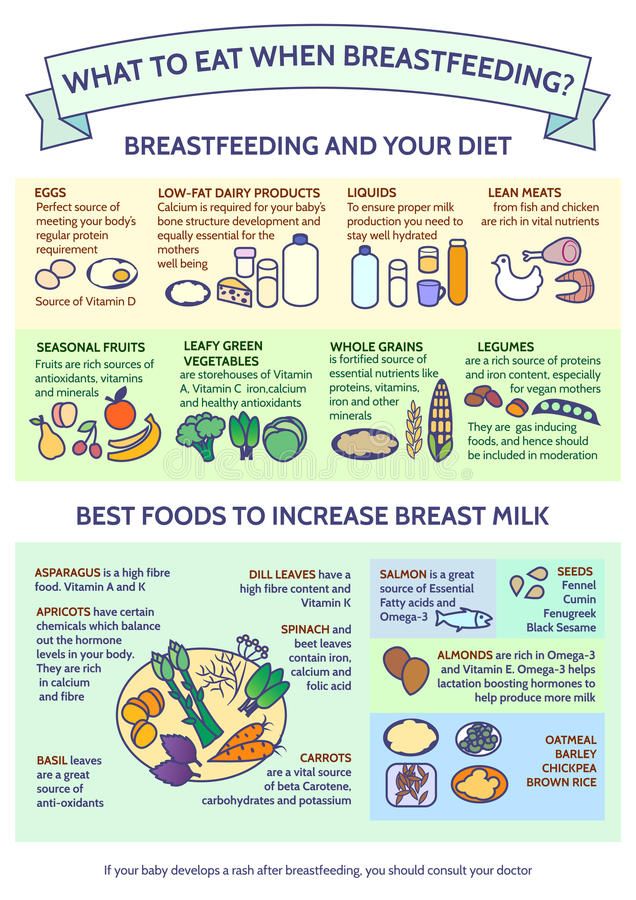
But it’s important to remember that even moderate cases of food poisoning can cause dehydration. Some breastfeeding parents notice drops in their milk supply after illnesses like food poisoning. That’s why it’s important that you stay well hydrated.
If you do notice a drop in your milk supply, it should be temporary. Nursing more frequently and replenishing your fluids should resolve things.
Danger to breastfed baby
As the CDC notes, almost all the organisms that cause food poisoning don’t get into breast milk, so there’s virtually no danger of your baby getting food poisoning from breastfeeding.
However, it’s possible that your baby could pick up the germ that made you sick from another source outside of your breast milk — for example, if baby had a taste of whatever food contained the pathogen.
Regardless, your breast milk can help protect your little one from infection. And if they do get sick, your milk will keep them properly hydrated and nourished.
It can be easy to try to just push yourself through when you’re parenting with food poisoning. But it’s important to take care of yourself, too.
Additionally, you’ll want to be sure to take some steps to minimize passing an infection onto your baby or other children.
Here are some tips for getting through food poisoning while breastfeeding:
- Stay hydrated. Dehydration is the biggest concern when it comes to food poisoning. Even if you can’t keep food down, it’s important to continue drinking plenty of water. Consider adding some fluids meant to replenish and balance your electrolytes, too.
- Avoid Pepto Bismol. Products with oral rehydration salts are compatible with breastfeeding. However, products containing bismuth subsalicylate compounds, like Pepto Bismol, may not be safe.
- Seek medical attention. If your symptoms are lasting more than 1 or 2 days, you have a persistent fever, or you’re severely dehydrated, seek medical attention.
 In some cases, your doctor may prescribe medication to help your symptoms or to treat the infection.
In some cases, your doctor may prescribe medication to help your symptoms or to treat the infection. - Ask a doctor about medication. If you’re unsure whether a product, medication, or antibiotic used to treat food poisoning is compatible with breastfeeding, talk with your doctor. You can also check the LactMed database, where you can find information about different substances and medications as well as their impact on breastfeeding.
- Wash your hands frequently. Over the course of your illness, wash your hands frequently with soap and water after using the toilet and after vomiting. Give your hands an extra wash before holding or nursing your baby.
- Minimize risk to others. Consider sanitizing any high touch surfaces like door handles, light switches, and toilet handles. Clean food prep areas well. Additionally, make sure that anything your baby touches or puts into their mouth — such as pacifiers, nipples, and teethers — have been thoroughly cleaned.

Remember, it’s important to take care of you so you can take care of your baby.
Most food poisoning symptoms — which can include nausea, vomiting, diarrhea, and stomachache — resolve within 1 or 2 days and don’t require medical attention.
However, visit a healthcare professional if you experience any of the following symptoms:
- bloody diarrhea
- high fever of over 102°F (38.8°C)
- inability to keep fluids down
- dehydration
- diarrhea that lasts for 3 or more days
Food poisoning is linked to a food or drink you ingested that was contaminated. The main symptoms of food poisoning are gastrointestinal — such as vomiting, diarrhea, and upset stomach.
Respiratory symptoms such as coughing, sneezing, or congestion are usually not caused by food poisoning.
However, food poisoning can sometimes cause fever. If you’re unsure if you’re experiencing food poisoning or something else, consult with your doctor.
It’s never fun getting sick, and you might worry about what food poisoning in particular means for you as a breastfeeding or chestfeeding parent.
The good news is, you can — and should — continue breastfeeding your baby even if you get food poisoning.
Your breast milk should not give your baby food poisoning, and in fact, it can help protect them from contracting the germ that caused the food poisoning.
If you have any questions about a food-borne illness while breastfeeding, talk with your child’s pediatrician. And if you or your baby have severe symptoms or become severely dehydrated, seek emergency medical care.
6 tips for breastfeeding when you have food poisoning
Photo by Dave ClubbWe traveled to Phuket, Thailand, when baby was 7 months old and unfortunately on that trip I managed to pick up food poisoning from a meal or water we ate or drank somewhere. I narrowed it down to two places that I ate at but, as is often the case, it was hard to tell for sure where exactly the poisoning came from. Having food poisoning while taking care of a 7 month old baby presented three main challenges in terms of breastfeeding: two of which passed quickly and the other having seemingly slightly longer term implications.
Having food poisoning while taking care of a 7 month old baby presented three main challenges in terms of breastfeeding: two of which passed quickly and the other having seemingly slightly longer term implications.
Challenge #1:
The first challenge was finding out whether I could pass on the infection to the baby through the breast-milk. Some people in the know may think this sounds crazy but, for me, I knew that so many other viruses and substances that the mother ingests (medicines, alcohol etc.) can be passed through breast-milk, and so I wanted to be sure that I wouldn’t pass any harmful infection on to the baby. In terms of food poisoning, the one thing worse than having horrible symptoms of your own, would be having to watch your baby suffer through those horrible symptoms. It turns out that breastfeeding after food poisoning is fine in most cases. I found this article on kellymom about breastfeeding when sick to be helpful. Additional useful information from the CDC on breastfeeding with food-borne and waterborne illnesses like travelers diarrhea.
What the experts say:
A nursing mother with diarrhea believed to have been caused by food or water sources should be encouraged to increase the frequency of breastfeeding while significantly increasing her own fluid intake… The organisms that cause travelers’ diarrhea do not pass through breast milk. Use of oral rehydration salts by breastfeeding mothers and their children is fully compatible with breastfeeding. Breastfeeding mothers should carefully check the labels of over-the-counter antidiarrheal medications to avoid using bismuth subsalicylate compounds, which can lead to the transfer of salicylate to the child via breast milk… Most experts consider the use of short-term azithromycin [antibiotic] compatible with breastfeeding.
Centers for Disease Control and Prevention
As long as the symptoms are confined to the gastrointestinal tract (vomiting, diarrhea, stomach cramps), breastfeeding should continue without interruption as there is no risk to the baby.
Kellymom.com
Challenge #2:
The second challenge was getting through the 2 – 3 days where I was feeling very sick – the first 24 hours being the worst. Without getting into too much undesirable information here, I could barely make it to the bathroom, did not leave the hotel room for at least 36 hours, was not able to drink very much and was able to eat only dry, plain crackers.
Needless to say, taking care of a crying, pooping, hungry baby was not easy. I had barely any energy to lift a glass of water, never mind lift the baby to breastfeed her, and it was so hard to be patient when she was crying. It is no fun trying to care for the baby when you can barely even take care of yourself, but we did because there is no alternative! I do think she sensed that something was wrong though, and was calmer for us.
Challenge #3:
3. The third challenge was the implications on our breastfeeding quantity, which I was not aware of until after it had happened.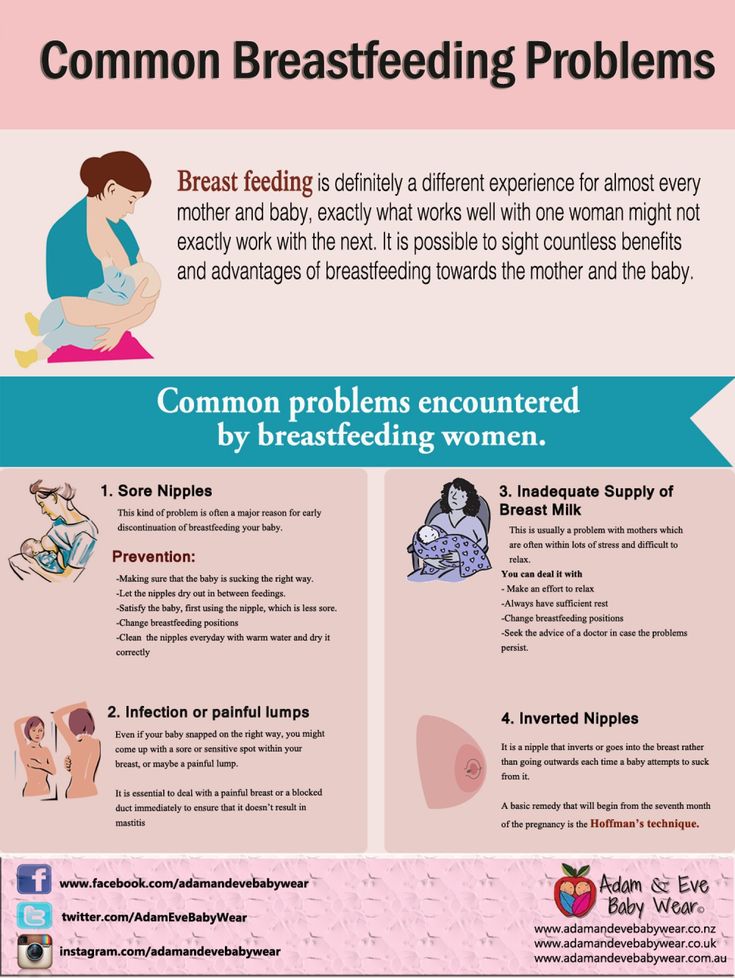 Normally, her most filling breastfeed was first thing in the morning when we would wake up, and then each feed later in the day was a little smaller than. On the first morning after being awake all night with the food poisoning symptoms, I could tell my breasts were not as full as they normally would be at that time in the morning, after not having fed her for about 9 hours or so.
Normally, her most filling breastfeed was first thing in the morning when we would wake up, and then each feed later in the day was a little smaller than. On the first morning after being awake all night with the food poisoning symptoms, I could tell my breasts were not as full as they normally would be at that time in the morning, after not having fed her for about 9 hours or so.
I could barely lift the baby and I decided not to breastfeed her that morning so I asked my partner to feed her the solid food breakfast earlier than usual. I knew I had lost a lot of liquids through diarrhea and sweating, and not being able to keep up my usual water intake. And I knew that dehydration could have a detrimental effect on breastfeeding.
I figured that by the next day I would be better hydrated and the milk supply would be back to normal. Although I had been drinking some oral rehydration salts in my water, I unfortunately had not been able to consume as much liquids that first daytime as I had hoped and I was still very dehydrated.
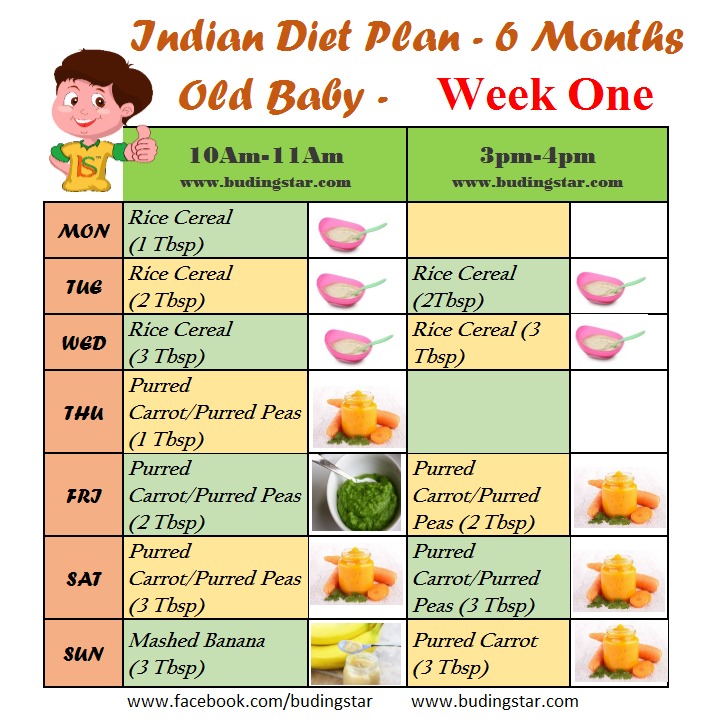
On the second day after the food poisoning, I woke up again with my breasts not as full as they usually would be first thing in the morning. This time, I was strong enough to hold the baby and I fed her, but I knew it would not be enough to fill her and so straight after that I gave her some solids (whereas normally we would wait an hour or two until ‘solid food breakfast’).
The same thing happened on the third morning. And by the fourth morning, I began to wonder if we had entered a ‘new normal’ in that my body was producing less in the morning now as standard, rather than because I was sick.
After recovery…
Unfortunately, my ‘normal’ milk supply and full-feeling in my breasts never returned after that bout of food poisoning, even two months later as I write this.
Now, if the baby was still under 6 months old and exclusively breastfeeding this whole scenario would have been much more challenging and stressful, but we were fortunate in the timing since she was already used to eating solid food and had been doing so for just over a month. It was therefore easy to supplement more of the solids to compensate for the reduced amount of breast-milk. Had we not been able to add more of the solids, we would have struggled more as she would have been hungry and crying more. In that scenario, it would have been good to be able to use some previously expressed milk stored in a fridge or freezer, however, when you’re traveling you may not have access to a pump or to a fridge or freezer or facilities to sterilize all the necessary equipment for expressing milk.
It was therefore easy to supplement more of the solids to compensate for the reduced amount of breast-milk. Had we not been able to add more of the solids, we would have struggled more as she would have been hungry and crying more. In that scenario, it would have been good to be able to use some previously expressed milk stored in a fridge or freezer, however, when you’re traveling you may not have access to a pump or to a fridge or freezer or facilities to sterilize all the necessary equipment for expressing milk.
Medical advice in this scenario is to increase the frequency of the breastfeeding sessions and increase intake of liquids. However, having been in the position of being very sick and unable to even lift or barely hold my baby, I’m not sure this will work in every situation. If your baby is not on solids yet and/or is not used to drinking milk or formula from a bottle, food poisoning could potentially be a concern for you on your travels to consider how you would ensure baby gets enough to feed on.
6 practical tips on breastfeeding when you have food poisoning…
- try to avoid or minimize consumption of foods that are known to increase the chances of contracting food poisoning (for example, shell fish, raw foods like salads, unpasteurized dairy, ice cubes, meat not thoroughly cooked) and to eat at places that look busy and/or are well reviewed by many others;
- carry a supply of oral re-hydration salts with you when you travel to help re-hydrate more quickly;
- carry a supply of loperamide (Imodium) anti-diarrheals, which are considered compatible and safe with breastfeeding;
- wash your hands often – after going to the bathroom and before touching baby – to minimize risk of passing any germs;
- try to consume as much water as possible, even if you don’t feel like it and it’s difficult to swallow down: you need the liquids for re-hydrating your own body so that you can keep producing milk for baby;
- if you feel that your milk supply has decreased, as mine did, increase the frequency of the feedings so that your body gets the message to keep producing more for baby (according to the body’s supply and demand mechanisms of breast-milk production).

Wishing you safe and healthy travels with no food-borne or waterborne illnesses!
Breastfeeding when the mother is ill.
home
Articles
Nutrition
Stulova Maria Alexandrovna Breastfeeding consultant
09.10.2013
Mom got sick! Nightmare! Grandmothers rush to the rescue, trying to protect the baby from infection and let the patient recover in peace.
However, good intentions and ignorance of physiology often lead to negative results. nine0003
Very important: if a nursing mother falls ill, it is necessary to choose medications that are compatible with breastfeeding*, and continue breastfeeding!!!
Contraindications to breastfeeding are the following diseases of the mother:
- eclampsia, severe bleeding during childbirth and in the postpartum period,
- open tuberculosis,
- a state of severe decompensation in chronic diseases of the heart, lungs, kidneys, liver,
- and hyperthyroidism,
- acute mental illness,
- especially dangerous infections (typhus, cholera, etc.
 ),
), - herpetic eruptions on the nipple of the mammary gland (before their follow-up treatment),
- HIV infection.
With such diseases of a nursing mother as rubella, chickenpox, measles, mumps, cytomegalovirus infection, herpes simplex, acute intestinal and acute respiratory viral infections, if they occur without severe intoxication, breastfeeding, subject to the rules of general hygiene, is not contraindicated. nine0003
The presence of hepatitis B and C in women is currently not a contraindication to breastfeeding, however, feeding is carried out through special silicone pads. In acute hepatitis A in the mother, breastfeeding is prohibited.
And if we are dealing with banal colds, flu or mastitis, then interrupting breastfeeding for the duration of the illness is NOT good for either the mother or the child.
Why? nine0003
Because by the time the mother has symptoms of the disease, the child may already be infected. He is in a state of “pre-disease”, but has the opportunity not to get sick or to suffer the disease in a mild / latent form.
He is in a state of “pre-disease”, but has the opportunity not to get sick or to suffer the disease in a mild / latent form.
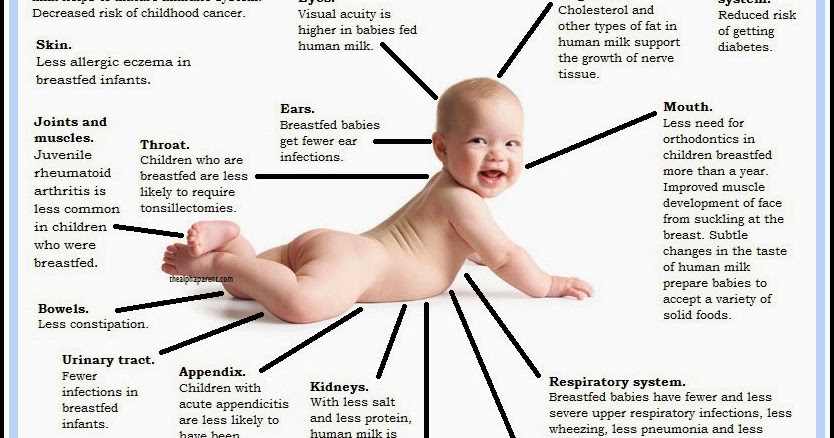
To do this, it is necessary to help the baby's immune system and save the body's resources to fight infection. What can help the immune system are breast milk immunoglobulins, as well as a huge amount of vitamins and other biologically active substances from milk. nine0003
How to preserve the resources of the body - provide the child with the most easily digestible food (this is breast milk), which will save energy, reduce stressful situations (absence of a mother nearby, inability to habitually suckle the breast, the appearance of a new person in the house to care for the baby), save heat (avoid long walks in the cold season). Conclusion: the main help for the child's body is the preservation of the usual rhythm of breastfeeding and the usual contact with the mother. nine0003
If we decide to interrupt breastfeeding for the duration of the illness, then the child has to be transferred to artificial formula. What is NOT good for the child:
What is NOT good for the child:
- The child is deprived of mother's milk immunoglobulins and many bioactive substances
- The load on the gastrointestinal tract increases, because the mixture is an indigestible product to which the body must adapt
- The risk of allergies increases and, accordingly, the body's resistance to infections decreases
- The child is deprived of habitual sucking and nutrition, and with it the necessary contact with the mother - this is a psychological stress for the baby, weakening the body's resources
- Often, when suckling the nipple, a child develops a mechanism of improper suckling, which prevents a further return to breastfeeding
What is NOT useful for a mother to interrupt breastfeeding during illness:
A change in the rhythm and quality of breast emptying, which in turn can provoke lactostasis, and then mastitis (especially if the mother has a bacterial infection). nine0003
During illness, the breast must be emptied very efficiently, sometimes giving the child to suck even more often than usual and from different positions. At the same time, many children themselves increase the rhythm of attachments during illnesses (mother's and / or their own) - they seem to “hang” on their chest for a couple of days. And grandmothers at this time can help mom around the house, take care of hygiene and the baby.
At the same time, many children themselves increase the rhythm of attachments during illnesses (mother's and / or their own) - they seem to “hang” on their chest for a couple of days. And grandmothers at this time can help mom around the house, take care of hygiene and the baby.
Usually safe, used in medium doses, are short courses of paracetamol, ibuprofen; most cough medicines; antibiotics - ampicillin and other penicillins, erythromycin. However, in the instructions for these drugs, you will most likely find a contraindication - breastfeeding. This is due to the fact that the manufacturer must conduct studies on the effect of the drug on the child through breast milk. Since it is very expensive and not every pharmaceutical company can conduct such studies, manufacturers are forced to write a warning. Studies by foreign companies show that the above drugs practically do not penetrate into breast milk (either due to the very large size of the molecules, or due to strong binding to blood proteins) and cannot harm the child. nine0003
nine0003
There are specialized guides on the compatibility of drugs with breastfeeding. These are foreign publications that indicate the degree of risk for a child when taking a particular drug by a nursing mother, indicate what the risk may be, and offer safe alternatives. The most convenient is the directory of the Marina Alta Hospital (address http://www.e-lactancia.org/ingles/inicio.asp).
In most cases, when the mother is ill, breastfeeding should continue. And in each specific situation, the mother must assess the risks of transferring the child to artificial feeding and compare them with the risks of taking the drug. nine0003
At the same time, while taking medications by a nursing mother, careful monitoring of the child is necessary in order to detect possible side effects in a timely manner.
Be healthy.
Your lactation consultant Maria Stulova
The role of nutrition in maintaining health
Breastfeeding (video).
Return to list
Treatment of food poisoning in a child
Food poisoning is an acute infectious-toxic pathology. It occurs when eating poor-quality products that contain pathogens, toxic substances and poisons. The main manifestations are diarrhea, vomiting, fever, signs of dehydration and severe intoxication. The task of treatment is to quickly stop the symptoms of poisoning, replenish fluid deficiency, and prevent the development of complications.
Classification
Food poisoning is classified as toxic infection or intoxication. Pathology develops after the use of low-quality food, water, plant, chemical or medicinal toxic substances. nine0003
There are two types of food poisoning in children:
- Infectious. The causative agents are microbes and their toxic waste products.
- Non-infectious. Caused by toxic substances of plant, animal origin, toxic impurities.
The asymptomatic or latent stage of food poisoning begins from the moment the toxins enter the body until the first symptoms appear. The duration depends on the individual characteristics and age of the child, the amount and rate of absorption of poisons. This stage is most favorable for therapy, since toxic substances have not yet penetrated into the blood. nine0003
The duration depends on the individual characteristics and age of the child, the amount and rate of absorption of poisons. This stage is most favorable for therapy, since toxic substances have not yet penetrated into the blood. nine0003
The toxicogenic stage begins with the appearance of the first symptoms of poisoning and lasts until bacteria and poisons are completely eliminated from the body. This period is characterized by the manifestation of all symptoms of poisoning. In order for the treatment to be effective, it is necessary to identify toxins and accelerate the process of elimination.
At the last stage of convalescence, the disturbed functions of the organs of the digestive, excretory, and immune systems are restored.
Causes
Food poisoning is one of the most common problems in pediatrics. In children, intoxication is more severe than in adults. This is due to the characteristics of the child's body: low acidity of gastric juice, incompletely formed intestinal microflora, rapid absorption of poisons and the spread of toxins throughout the body. nine0003
nine0003
The main causative agents of food poisoning in children are staphylococci, proteus, klebsiella, enterotoxigenic strains of E. coli, clostridia. Pathogens enter the body only with food, in which they multiply, release toxins.
Causes of violation of food quality:
- non-compliance with sanitary and hygienic standards;
- violation of the rules of storage, preparation and sale of food products;
- contamination of food by people with intestinal infections, purulent pathologies - tonsillitis, furunculosis, panaritium, mastitis, streptoderma; nine0030
- contamination of soil and plants with animal feces.
Spoiled products may have an unpleasant taste, smell, uncharacteristic texture, but often organoleptic indicators remain within the normal range.
Non-infectious poisoning - a consequence of accidental consumption of poisonous berries or plants, mushrooms. Intoxication can occur after eating agricultural products that are contaminated with poisonous fungicides, insecticides.
Which products are classified as potentially hazardous? nine0113
In children, food poisoning often occurs after drinking unboiled water, missing milk or dairy products.
Dangerous products include:
- eggs;
- cream confectionery;
- fish and seafood;
- sausages;
- meat, vegetable preserves;
- mushrooms.
Food poisoning is most often diagnosed in summer and autumn. During this period, the conditions for the reproduction of microbial pathogens are the most favorable. nine0003
Symptoms of food poisoning in a child
Despite the variety of toxic infections, clinical manifestations are largely similar. The latent stage lasts an average of 2-6 hours, sometimes no more than 30 minutes or more than a day. Signs of poisoning are manifested by symptoms of gastroenteritis, intoxication, dehydration.
Poisoning always begins acutely - nausea, repeated vomiting with particles of undigested food.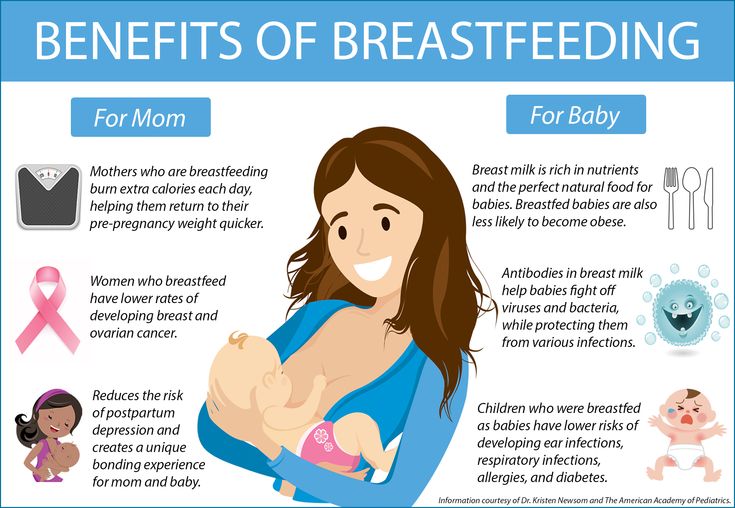 The child complains of abdominal pain, watery stools, mucous membranes, green impurities, blood streaks. Bowel emptying occurs up to 5-10 times a day. nine0003
The child complains of abdominal pain, watery stools, mucous membranes, green impurities, blood streaks. Bowel emptying occurs up to 5-10 times a day. nine0003
Simultaneously with dyspeptic disorders, the temperature rises to 38–39 degrees. Signs of intoxication quickly increase: refusal to eat, headache and muscle pain. Symptoms of dehydration appear: the skin is pale and dry, facial features are sharpened, the number of urination decreases, the mucous membranes dry out. In infants, the fontanel sinks. With food poisoning, convulsions often occur, acidosis develops.
In most cases, signs of poisoning gradually disappear after 2-3 days, but weakness and abdominal pain may persist for several weeks. nine0003
Severe forms of food poisoning are predominantly observed in young children with weakened immunity. The risk of developing complications against the background of intoxication increases with prematurity, malnutrition and dysbacteriosis in history.
If a child is poisoned by poisonous plants, berries, lesions of the central nervous system are observed:
- retardation of reactions;
- euphoria;
- hallucinations;
- impaired speech, vision; nine0030
- convulsions.
If the cardiovascular system is damaged by toxins, the heart rate speeds up or slows down, blood pressure decreases.
Mushroom poisoning is very dangerous for children. After eating a pale toadstool, indomitable vomiting, cholera-like diarrhea with impurities of blood in the feces begins. Other symptoms are intestinal colic, respiratory disorders, convulsions. Toxins adversely affect the liver, which leads to the development of toxic hepatitis. AT 90% of cases are fatal due to acute liver failure.
Signs of fly agaric poisoning are increased salivation, shortness of breath, severe vomiting, convulsions, bronchospasm, hallucinations, nystagmus or strabismus. But the mortality rate is less than 1%.
Botulism develops when poor-quality canned food is consumed. The toxin affects the nervous system, which manifests itself in the form of paralysis and paresis. Poisoning in children can cause the development of acute respiratory failure, heart rhythm disturbances.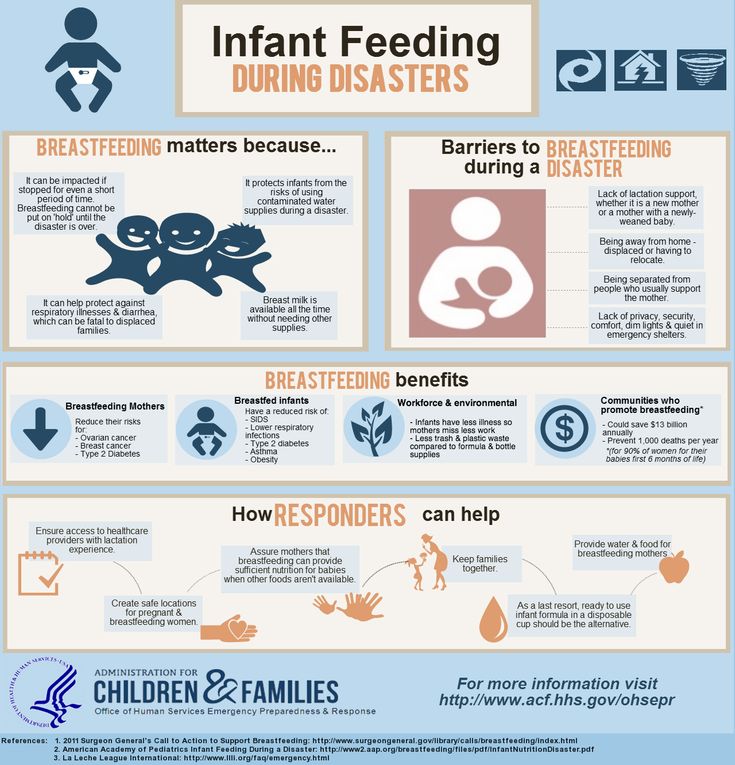 The first symptoms appear after 4-6 hours. Worries about pain in the epigastric region, nausea, vomiting, diarrhea. Sometimes there are problems with vision. When the respiratory system is affected, shortness of breath begins, the skin in the region of the nasolabial triangle turns blue, and arrhythmia develops. nine0003
The first symptoms appear after 4-6 hours. Worries about pain in the epigastric region, nausea, vomiting, diarrhea. Sometimes there are problems with vision. When the respiratory system is affected, shortness of breath begins, the skin in the region of the nasolabial triangle turns blue, and arrhythmia develops. nine0003
First aid for child poisoning
Act immediately. Rules for first aid:
- In case of poisoning with mushrooms, berries, medicines, induce vomiting.
- Gastric lavage with clean water to remove toxins from the intestines. Babies should not do the washing themselves, as the child can inhale the vomit. Instead, you can do a cleansing enema. The volume of water for gastric lavage - 16 ml / kg for children 3-6 years old, over 7 years old - 14 ml / kg. nine0030
- Taking enterosorbents - these drugs collect toxins in the intestinal lumen, remove them with feces.
- More to drink. You need to drink in small portions, but often. You can give your child water with a weak saline solution, weak tea, mineral water without gas.

- Call a doctor.
Timely first aid will help to avoid the development of complications of poisoning.
In case of poisoning, children should not:
- give painkillers, drugs, drugs for vomiting and diarrhea; nine0030
- apply hot or cold compresses to the abdomen;
- use soda to induce vomiting, potassium permanganate to wash the stomach;
- give milk and dairy products.
Diagnosis of food poisoning in a child
A pediatrician or an infectious disease specialist can diagnose food poisoning in a child. The examination begins with the collection of anamnesis, examination of the patient.
Specific diagnostic tests are prescribed to isolate the pathogen. Biomaterial - feces and vomit, gastric lavage, the remains of contaminated food. With a generalized form of infection, a blood culture is prescribed. Auxiliary methods - RIF, PCR, ELISA. Additionally, you may need to consult a neurologist, gastroenterologist, surgeon. nine0003
nine0003
Be sure to carry out differential diagnosis to exclude acute gastritis, cholecystitis, pancreatitis, giardiasis, acute intestinal infection, inflammation of the appendix, meningitis. A blood test is prescribed to rule out a viral, bacterial infection, a stool test to detect infections caused by pathological bacteria.
How to treat
Treatment of poisoning in a child begins with the elimination of signs of dehydration. Apply oral, parenteral rehydration therapy. nine0003
Auxiliaries:
- enzymes;
- sorbents;
- prebiotics to restore the balance of intestinal microflora;
- antimicrobials are necessary for severe toxic infections.
In case of toadstool poisoning, emergency hemosorption is performed to cleanse the blood of toxins.
Child poisoning diet
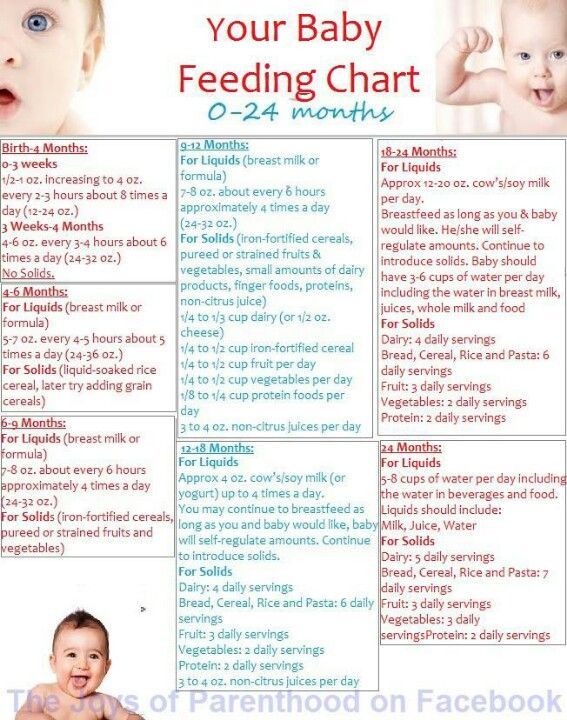
It is best not to feed the child for 12-24 hours after poisoning. When vomiting stops, a sparing diet is indicated. Breastfed babies under one year of age need to skip a few feedings. nine0003
nine0003
How to feed a child after poisoning:
- liquid porridge - rice, buckwheat, cooked in a mixture of equal amounts of water and milk;
- slimy soups;
- crackers;
- kefir;
- compotes;
- after a few days - vegetable puree, children's cottage cheese or kefir, yogurt without additives;
- gradually introduce meat and fish soufflé into the menu.
List of prohibited foods - pastries, whole milk, black bread, fresh white bread. You can not give your child pasta, chocolate, ice cream, chips, sweet carbonated drinks, wheat and barley porridge. From vegetables, cucumbers, tomatoes, cabbage are contraindicated. nine0003
The duration of the diet is 14 days.
Possible consequences of food poisoning in a child
Complications occur in case of severe poisoning, lack of correct and timely therapy.
Possible effects:
- dysbacteriosis;
- renal and hepatic insufficiency;
- disturbances in the functioning of the nervous and immune systems;
- chronic diseases of the gastrointestinal tract.
Prognosis and prevention
Poisoning in a child of mild and moderate severity ends in complete recovery.
Methods of prevention:
- properly store food, observe the temperature regime and other storage conditions;
- observe the rules of heat treatment, children should absolutely not be given raw fish, poorly fried meat;
- drink only boiled, purified water, do not swallow water when swimming in reservoirs;
- wash hands, vegetables and fruits thoroughly; nine0030
- store medicines, chemicals out of the reach of children;
- to tell children about poisonous mushrooms, berries, plants, the dangers of their use.
People who work in the kitchen in children's institutions should have regular medical check-ups. In the presence of pustular skin pathologies, respiratory diseases, signs of an intestinal infection, the worker is not allowed into the catering unit.
Treatment of food poisoning in Moscow
Food poisoning in a child is a dangerous condition, you should not self-medicate, you should immediately consult a doctor. Call our clinic, describe the symptoms, the patient's condition, the possible cause of the poisoning. The administrator of the "Miracle Doctor" center will write you to the doctor in the near future.
Call our clinic, describe the symptoms, the patient's condition, the possible cause of the poisoning. The administrator of the "Miracle Doctor" center will write you to the doctor in the near future.
Q&A
Why is acute poisoning dangerous for a child?
Fever, vomiting more often 3–5 times, diarrhea in a child is a reason to immediately call an ambulance. nine0003
Poisoning in a child at any age leads to a breakdown of the immune system. Dehydration is very dangerous for babies. In children under 4 years of age with profuse vomiting and loose stools, the critical phase of dehydration can occur within a few hours.
How to drink a baby if he vomits very often?
Even if the vomiting is severe and persistent, the child must be given water. The consequences of dehydration are extremely dangerous for the child's body. You need to water the child in small portions - 1 tsp each.