Baby gulping while bottle feeding
How to Have a Calm-Gulp Free Feeding
Free Shipping on Orders $60+ (US Only)
Learn More
Start typing and hit Enter
Shopping Cart
Register
Back to login
How to Have a Calm-Gulp Free Feeding
By :Amy Peterson 13 May 2019
Babies feed many times each day. As moms, we want this to be a happy experience for our babies. Helping your baby have a gulp-free feeding is one way to make the feeding calm. Sometimes a mom may hear her baby gulp during a feeding, but sometimes gulping can be more subtle and quiet.
If your baby is struggling with gulping during bottle-feeding, you will be able to see it in your baby’s feeding behaviors even if you can’t hear it. A baby’s face will look worried with a furrowed brow when she feels overwhelmed. You might even notice your baby’s arms move up to block the bottle, or hos hands shift from a closed position to fingers that are spread apart. These are signs that the feeding doesn’t feel right for your baby. If your baby is struggling with some gulping during a feeding, here are some tips that may help.
LOOK AT YOUR BABY’S LIPS
Your baby’s lips need to form a complete seal on the nipple. If there are gaps between your baby’s lips and the nipple, chances are your baby is swallowing extra air which can sound like gulping. Using a nipple that gradually widens at the base and has a place for your baby’s lips to rest is helpful for many babies. You may need to try more than one nipple to see which works best for your baby.
CHECK THE BOTTLE FLOW
Most babies start with a slow flow nipple. Keep in mind that brands flow differently from one another, so a slow nipple from one brand might flow faster than a slow nipple from a different brand. Use a nipple, such as the Evenflo Feeding Balance + Nipple, that allows your baby to swallow after every one or two sucks without gulping.
FEED IN A SEMI-UPRIGHT POSITION
Bottle-feeding your baby a slightly upright position allows the milk to collect in the mouth, rather than the at the throat, so your baby can have a controlled swallow. For example, think of drinking from a cup while sitting up versus lying down. When lying down, gravity causes the milk to rush to the back of the throat which can result in gulping. A more upright position can prevent the need to gulp.
For example, think of drinking from a cup while sitting up versus lying down. When lying down, gravity causes the milk to rush to the back of the throat which can result in gulping. A more upright position can prevent the need to gulp.
ALLOW YOUR BABY TO REST BRIEFLY DURING A FEEDING
When a baby breastfeeds, milk stops flowing periodically between letdowns. This is nature’s way of allowing the baby a brief rest to catch his/her breath. Many babies will stop sucking and rest during bottle-feeding on their own. But if your baby tends to continuously swallow which can lead to gulping, help you baby rest by leaving the nipple in the mouth and tipping it down slightly so the milk doesn’t reach the nipple tip. When your baby starts sucking again, let the milk flow again.
Previous Post
Next Post
Correctly bottle feeding your baby
Correctly bottle feeding your baby can promote breast to bottle and back as well as prevent ear infections.
Before becoming a NICU nurse, I didn’t even know there were different “ways” to hold your baby while feeding. I had only ever seen – and done – the “crook of the arm” feeding. This is the way babies, in my mind, were always fed!
I had only ever seen – and done – the “crook of the arm” feeding. This is the way babies, in my mind, were always fed!
Well, the NICU quickly changed that!
Did you know that the instinct to feed is not generally seen in babies less than 36 weeks gestation? This means that babies born before 36 weeks (also known as late preterm) may not show signs that they are ready to take a feeding by mouth (bottle or breast).
For this reason, it’s not uncommon to see premature + late preterm babies with a nasogastric (NG) tube. This tube allows baby to be fed breastmilk or formula straight into their tummy without the actual act of eating.
As babies approach their due date and become “term” (36-37 weeks+, sometimes a bit earlier), we test their readiness to feed by bottle.
We give them little tastes of milk on a pacifier to help them learn how to suck, swallow, and breathe correctly (we even give preemies a swab of breastmilk very early on to get them familiar with the taste!).
But giving tastes does more than just familiarize them with the taste and smell of milk – it actually tells us A LOT of information!
We can gather baby’s interest in feeding, neurological readiness (sleepy preemies can’t take a bottle!), and read their cues. Have they developed a negative association with oral stimulus (paci, bottle) from having a breathing tube for so long?
Is their reflux so painful that they associate feedings with pain? Are they overwhelmed while feeding (sleepy at the bottle, breathing fast, dropping their heart rate low, sticking their tongue out and pushing the bottle out?)
Suck, swallow, breathe is a coordination skill that some babies need a little help in mastering.
I say this all the time to my clients, but LOOK at your baby and LISTEN to cues as you feed! We can gather SO MUCH information by looking at our baby feed – including signs of hunger, satiety, oral aversion, reflux, etc.
We understand that bottle feeding can be challenging! We are here to help you! Click here to learn more about the supportive services we offer!
My baby isn’t a preemie. Do I still need to watch them closely while they feed?
Do I still need to watch them closely while they feed?
Yes! Bottle feeding should still be to your term baby’s cues. Feeding and taking a bottle is a skill that baby needs to learn how to do.
And bottle feeding positioning is important for many reasons which we will get into below.
Why is it so important to know your baby’s feeding cues while bottle feeding?
It tells us a lot about how baby is feeling during a feed:
- It tells us if baby needs to slow down the pace (size down on a nipple) or speed up the pace (upsize the nipple). See below.
- It tells us if baby is full. We often try to feed all the contents of the bottle – but baby may not want all the contents. It’s MORE important for baby to control the amount they take in and have a positive experience, than accidentally force feeding.
- It tells us if baby is still hungry BUT prevents overfeeding. If a bottle is completely finished, and baby is rooting or sucking, they may want more.
 We will talk about side lying feeding in a bit, but basically by following baby’s cues with side lying, baby is controlling the pace of the bottle.
We will talk about side lying feeding in a bit, but basically by following baby’s cues with side lying, baby is controlling the pace of the bottle. - So if baby does want more, it is available to take at their pace, rather than dripping out of the bottle due to gravity. Signs of being done with the bottle include yawning, sneezing, pushing out of the tongue, pushing the bottle out with the tongue, arching back away from the bottle, gazing up and away from the bottle.
- It tells us if baby is overwhelmed. Persistent hiccuping, sneezing, yawning, gagging, or pushing out of the tongue all are signs of being “done” or overwhelmed with the bottle.
- It prevents oral aversion. You wouldn’t like it either if someone was forcefully sticking food in your mouth! Repetitive accidental force feeding creates an oral aversion, refusal of the bottle, fussiness, and refusal to eat by bottle.
- Try allowing baby to open BEFORE you place the bottle in baby’s mouth by gently tickling their upper lip with the bottle.
 Once baby opens, they are ready to latch and feed.
Once baby opens, they are ready to latch and feed.
But who CARES?! My baby hasn’t shown any of these things and feeds just fine the way I feed her.
YOU are the parent! You have every right to make the decision for your baby! I am here to inform and help you prevent or reverse some possible negative symptoms of gravity-lead bottle feeding positioning.
Does it matter if the contents in the bottle are formula or breastmilk?
No! Anytime you are bottle feeding, no matter the contents, side-lying is the way to go.
Correctly bottle feeding
SIDE LYING POSITIONING + INCLINED!
What is side lying + inclined positioning?
Side lying positioning is when baby is laying on their side (ear, shoulder, and hip should all be aligned). Then, incline their head slightly with your hand or a pillow (I even just cross my legs!).
Why is side lying + inclined feeding important?
Side lying + inclined feeding mimics breastfeeding – both in position and flow. It allows baby to control the flow of the bottle, leading to a positive experience with the bottle, less choking and coughing, less flooding, and LESS EAR INFECTIONS!
It allows baby to control the flow of the bottle, leading to a positive experience with the bottle, less choking and coughing, less flooding, and LESS EAR INFECTIONS!
A bottle has an opening at the nipple. This opening is consistently open, whether baby is sucking or not. Test by holding a bottle upside down – it drips!
This dripping also happens in baby’s mouth when we hold the bottle in a downward position where gravity is pulling the milk out of the bottle, not baby, such as in the “crook of the arm” feeding position.
When gravity pulls out the milk (aka dripping of the bottle), baby is actually getting more milk flow than they are sucking out. This causes baby to get flooded – meaning there is too much milk in baby’s mouth.
This makes it hard to baby to keep up with the amount of milk in their mouth – leading to gulping, choking, coughing, milk dripping out of the side of their mouth.
This can happen with a “crook of the arm” positioning because the nipple is angling down, allowing gravity to do the work.
Think about if you were trying to drink something using a straw. Then, someone was simultaneously pushing more liquid in your mouth.
It would be really hard for us to keep up! If this was consistently happening, we would pretty soon say, “I’m not drinking out a straw anymore!”
This same thing happens to baby – they simply can’t keep up and may start to associate the feeds negatively.
How do I feed baby in side lying position?
- Bend your knees and elevate your legs on a coffee table or ottoman. If you don’t have those available, cross your legs or place a pillow on your lap.
- Place baby in side lying position on your lap with their head closest to your knees.
- Support baby’s head and neck with your non-dominant hand.
- Hold the bottle parallel to the floor.
- Feed baby.
Tip: Watch my reels on how to correctly bottle feed your baby and how to burp your baby!
Ear infections + how they related to feeding positionEar infections are also called otitis media. They are very common, especially in infants. Side note – ear infections are NOT contagious.
They are very common, especially in infants. Side note – ear infections are NOT contagious.
The eustachian tube in the ear connects the middle ear with the back of the throat. If formula or breastmilk continually is entering the eustachian tubes, this causes bacteria from the mouth (naturally occurring bacteria) to enter the middle ear, causing ear infections.
Bacteria feed on the nutrients in breastmilk and formula, making easy for them to multiply, causing and infection.
“Crook of the arm” is gravity lead, which leads to flooding, making the risk of formula or breastmilk entering the eustachian tubes much higher (and therefore the middle ear), which in turn increases the risk for ear infections.
Side lying feeding is baby lead, meaning baby is pulling the amount they can handle from the bottle. This prevents flooding, and therefore, the risk of ear infections is much lower.
I heard that breastfeeding lowers the chance of ear infections.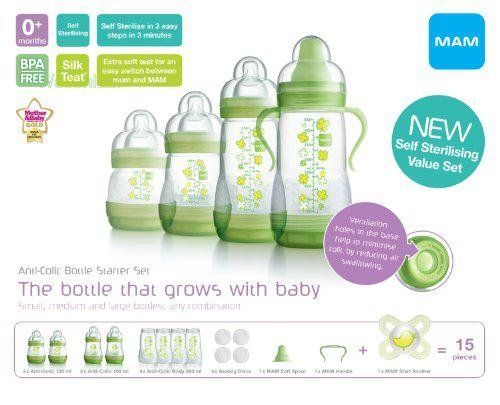 Is that true?
Is that true?
To an extent. Breastmilk does contain antibodies that can help prevent infections, including ear infections. However, bottle-fed breastmilk poses basically the same risk as formula since the positioning is actually what causes the ear infections.
Breastfeeding from the breast does help reduce the risk for ear infections due to proper positioning and flow, however, it does not eliminate the risk.
I see air in the nipple. Should I be concerned?
No. Air at the top of the nipple is normal – the milk still fills the tip of the nipple so baby won’t suck in air.
My baby is gulping and chokes on the bottle. What can I do?
Your baby may need a smaller size nipple. If you’re already using the smallest size, try paced feedings. Paced feedings allow baby to “catch up” and swallow the milk in their mouth, then breathe, then suck.
Too much milk will cause them to gulp, not be able to take a breath, etc. Click here for a demonstration.
Click here for a demonstration.
My baby gets frustrated at the bottle and when I take the bottle out, the nipple is completely flat and collapsed.
Time to move up to the next size nipple! Baby is sucking harder than the nipple flow allows.
It takes FOREVER for my baby to feed from the bottle, more than 45 minutes. What can I do?
Try upsizing the nipple! If baby is dripping, gagging or choking, the flow is too fast and move down a nipple size. Or try paced feedings with the larger nipple.
My breastfed baby WILL NOT take a bottle. HELP!
Your wish is my command! We offer 1:1 virtual consults from the comfort of your own home to introduce the bottle to your breastfed baby in a way that promotes a positive association with the bottle.
We also offer in home bottle feeding consultations for the Chicagoland area!
Click here to view the consultations we offer!
Watch our workshop!
Watch our recorded workshop, “Bottle Refusal and Tips. ” Join Lauren, NICU RN and mother of 2, discuss tips for bottle refusal in infants. She discusses different strategies for avoiding bottle refusal along with tips and tricks for reversing bottle aversions. She also goes over alternative methods for giving breast milk/formula to babies who have ongoing issues with bottle refusal. Are you exclusively pumping or offering pumped milk in a bottle? You may have high lipase which could be causing bottle refusal. Read more here in our high lipase and ways to battle it blog post.
” Join Lauren, NICU RN and mother of 2, discuss tips for bottle refusal in infants. She discusses different strategies for avoiding bottle refusal along with tips and tricks for reversing bottle aversions. She also goes over alternative methods for giving breast milk/formula to babies who have ongoing issues with bottle refusal. Are you exclusively pumping or offering pumped milk in a bottle? You may have high lipase which could be causing bottle refusal. Read more here in our high lipase and ways to battle it blog post.
WATCH BOTTLE WORKSHOP NOW
Have more questions? Schedule a text or video chat consult with Kate, Lauren or Natalie (NICU RNs) and they can help answer any questions that you have!
BOOK CONSULT NOW
PRO TIP: I highly recommend these Lansinoh bottles (I use them all the time in consultations). I also really like these Evenflo bottles for newborns too!
Other helpful blog posts:
- High lipase breastmilk and how it relates to bottle refusal
- How to supplement with formula
- Everything you need to know about acid reflux
- Transitioning from formula to milk
- Everything you need to know about formula
- Diaper bag essentials
- How to travel with kids
**This post is educational and not meant to take the place of your provider. Bumblebaby makes a small commission on some of the items listed above
Bumblebaby makes a small commission on some of the items listed above
How to help the baby when regulating
Support icon ofKeywords for searching
Home ›!! How to help a child in sprinkling
Home Home ›!! How to help a child in regurgitation
↑ Verki
Breastal feeding - completely special time for mom and her newborn baby. Together with the feeling of closeness and affection that feeding brings, understanding its nuances cannot but raise many questions, including the question of how to help an infant spit up. Regurgitation in a newborn is by no means always the result of a simple pat on his back. nine0015
In this article, we'll talk about the basics of helping a newborn spit up, as well as other questions you may have about spitting up.
Why do babies spit up?
Let's get it straight: why do newborns need to burp in the first place? During feeding, children usually swallow extra air - this is called aerophagy. Spitting up helps prevent this air from entering the intestines, as well as vomiting, gas, and crankiness in the baby. To avoid the return of milk after feeding, you should give the baby the opportunity to burp more often. nine0003
Spitting up helps prevent this air from entering the intestines, as well as vomiting, gas, and crankiness in the baby. To avoid the return of milk after feeding, you should give the baby the opportunity to burp more often. nine0003
How to help a newborn spit up?
During the first six months, the baby should be kept upright in a column for 10-15 minutes after each feed. This will help keep the milk in his stomach, but if the baby occasionally burps anyway, parents need not worry. While carrying your baby in an upright position, you can put a baby diaper or wipes on your shoulder to keep your clothes clean.
We've already seen why spitting up is important, now let's find out how to help your baby spit up. Parents should gently pat the baby on the back with a hand folded in a handful until he burps. Folding your hand into a handful is important because clapping with a flat palm may be too strong for an infant.
Every baby is different and there is no one right position for spitting up.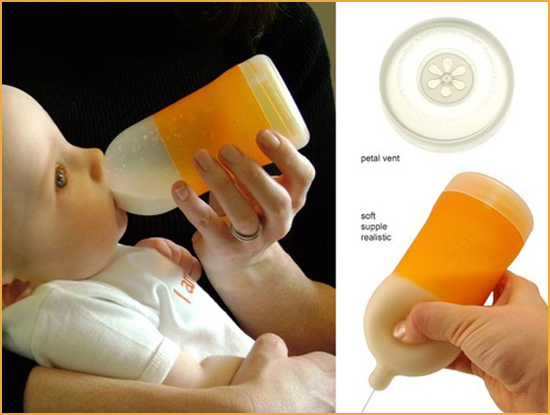 To get started, you can try the following options:
To get started, you can try the following options:
- Sitting position with the baby on the chest. In this position, the parent puts the baby's head with his chin on his shoulder and with one hand supports the baby under the back. With the other hand, you can gently pat the baby on the back. This method is most effective in a rocking chair or when the baby is gently rocking. nine0044
- Holding the child upright on your legs. With one hand, parents can hold the baby by the back and head, supporting his chin and placing his palm on the baby’s chest, with the other hand, you can gently pat him on the back. At the same time, it is important to be careful: do not press the child on the throat, but only gently support his chin.
- Holding a baby on your lap while lying on your tummy. Make sure his head is above his chest and gently pat your baby on the back until he burps. nine0015
Here are some tips on how best to help your newborn spit up:
- Let your baby spit up during feeding.
 If the baby is restless or has swallowed air, it is worth giving him the opportunity to burp during feeding, and not just after.
If the baby is restless or has swallowed air, it is worth giving him the opportunity to burp during feeding, and not just after. - When bottle feeding, let the newborn burp after every 50-60 ml.
- When breastfeeding, let the baby burp at every breast change. nine0015
It is important to let your baby spit up after eating, even if he spit up during feeding!
If your baby is gassy, spit up more often. Also, if he vomits frequently or suffers from gastroesophageal reflux disease (GERD), have him spit up after every 30 ml bottle-feeding or every five minutes while breastfeeding.
How long should a baby be held for it to burp? It's different for everyone, but generally keeping a newborn upright for 15 to 20 minutes after a feed helps the milk stay in the baby's stomach. nine0003
Minimize the amount of air you swallow. Gas production and regurgitation result from aerophagia during feeding. The baby will inevitably swallow air, but there are ways to prevent it from swallowing too much. Whether you bottle feed your baby or combine breastfeeding with bottle feeding, the Philips Avent anti-colic bottle with AirFree valve is designed so that the nipple is always filled with milk without excess air, even in a horizontal position, thus preventing the baby from swallowing excess air during feeding. nine0015
Whether you bottle feed your baby or combine breastfeeding with bottle feeding, the Philips Avent anti-colic bottle with AirFree valve is designed so that the nipple is always filled with milk without excess air, even in a horizontal position, thus preventing the baby from swallowing excess air during feeding. nine0015
Reducing the amount of air your baby swallows can help reduce your baby's risk of colic, gas, and spitting up.
Breastfeeding is a wonderful time to strengthen the bond between parent and baby. Every mom and every baby is different, so learning to help your newborn burp properly can take time and practice.
Articles and tips from Philips Avent
Baby+ app
Download the app and track your child's development and growth with trackers, and keep those special moments forever.
Download app:
You are leaving the Philips Healthcare (“Philips”) official website. Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain. nine0003
Philips makes no warranties regarding any third party websites or the information they contain. nine0003
I understand
You are about to visit a Philips global content page
Continue
You are about to visit the Philips USA website.
I understand
Infant Reflux: Symptoms and Treatment
Search Support IconSearch Keywords
Home ›› What is Reflux in Infants?
Home ›› What is reflux in babies?
↑ Top
Signs and what to do
Post-feed spitting up is common in the first few months of life. This is usually harmless and completely normal, but parents should read about gastroesophageal reflux (GER) and laryngopharyngeal reflux (LPR) in infants and how long it lasts to give them peace of mind.
We look at signs of reflux in babies, symptoms of different types of reflux, and how to help a child with signs of reflux. If you require further information, always contact your healthcare provider. nine0003
If you require further information, always contact your healthcare provider. nine0003
What is reflux in babies?
So we know reflux is common, but what causes reflux in babies? Because young children have not yet fully developed the lower esophageal sphincter (LES), that is, the muscle at the bottom of the esophagus that opens and closes to let food into the stomach and keep it there, food can easily pass back up the esophagus.
Acid reflux, also known as gastroesophageal reflux (GER), is a normal reflux that occurs in babies. This type of reflux is considered normal and occurs in 40-65% of babies. nine0003
How do I know if my child has acid (gastroesophageal) reflux?
If a baby is spitting up milk after a feed, it is most likely acid reflux. As babies get older, GER usually goes away on its own without any intervention. If a baby has complications beyond just spitting up a small amount of milk (such as feeding difficulties and discomfort), they may have gastroesophageal reflux disease (GERD). nine0015
nine0015
Symptoms of GERD include:
- baby arching during or after feeding;
- crying more than three hours a day for no apparent reason;
- cough;
- gag reflex or difficulty swallowing;
- irritability, restlessness after eating;
- eating little or not eating;
- poor weight gain or loss;
- difficult breathing;
- severe or frequent vomiting. nine0015
GERD usually occurs when the muscle tone of the LES is not weakened in time, causing stomach contents to back up into the esophagus.
How do I know if my child has Laryngopharyngeal Reflux?
Another type of reflux, laryngopharyngeal reflux (LPR), also called silent reflux, is when the contents of the baby's stomach leak back into the larynx, the back of the nasopharynx. This type of reflux does not always cause external symptoms, which is why it is called "silent". Babies can have GERD and silent reflux at the same time, but their symptoms are somewhat different. nine0015
nine0015
The following are some of the symptoms of laryngopharyngeal reflux:
- trouble breathing;
- gag reflex;
- chronic cough;
- swallowing problems;
- hoarseness;
- regurgitation;
- poor weight gain or weight loss.
We have looked at the signs of reflux in infants, now we will move on to the treatment and duration of silent reflux in children, as well as the treatment of GERD. nine0003
How to deal with laryngopharyngeal reflux in babies while breastfeeding?
Breastfeeding mothers may need to review their diet if their babies show signs of reflux. The American Academy of Pediatrics (AAP) recommends breastfeeding mothers cut eggs and milk from their diet for two to four weeks to see if their baby's reflux symptoms improve or disappear. It may be worth eliminating acidic foods from your diet. nine0015
In most cases, GER and laryngopharyngeal reflux go away on their own. Typically, children outgrow reflux in the first year of life. If a child has persistent symptoms of laryngopharyngeal reflux, parents should consult a doctor. If your baby is vomiting heavily, has blood in the stool, or has any of the symptoms of GERD listed above, parents should contact their pediatrician as soon as possible.
Typically, children outgrow reflux in the first year of life. If a child has persistent symptoms of laryngopharyngeal reflux, parents should consult a doctor. If your baby is vomiting heavily, has blood in the stool, or has any of the symptoms of GERD listed above, parents should contact their pediatrician as soon as possible.
How can I help my child with reflux or GERD? nine0008
Reflux symptoms in babies usually go away on their own, but the following tips can help relieve symptoms:
- Thicken your food with rice or a special milk thickener.
- Hold the bottle at an angle that fills the nipple completely with milk to reduce the amount of air your baby swallows. This can help prevent colic, gas, and reflux.
- Try the AirFree anti-colic bottle, designed to reduce air swallowing during feeding. nine0044
4. Let your baby burp during and after feeding. If the baby is bottle fed, parents can let him burp after every 30-60 ml. If the mother is breastfeeding, she may let the baby burp when changing breasts.
If the mother is breastfeeding, she may let the baby burp when changing breasts.
5. Hold baby upright after feeding. As a rule, in order for the milk to remain in the stomach, after feeding the baby, it is necessary to hold it in an upright position for 10-15 minutes. But, if the child has reflux, parents should keep him upright a little longer. nine0003
These tips may help relieve symptoms, but they do not replace a doctor's advice.
Parents should not change their infant formula without first talking to their healthcare provider.
Don't panic! Reflux is very common in babies during the first three months of life, and most babies outgrow it without any consequences. Although GERD is a slightly more serious condition, there are many treatments, ways to manage it, and help newborns. Feel free to contact your doctor with any questions or concerns you may have. nine0003
4 Seattle Children’s Hospital
5 The National Institute of Diabetes and Digestive and Kidney Diseases - Treatment for GER & GERD in Infants
Any links to third party websites that may be included on this site are provided solely as a convenience to you.![]()