Baby heaving after feed
Reflux | Breastfeeding Challenges | Start for Life
Breastfeeding challenges
There may be times when breastfeeding is challenging. Never ignore any issues you may have – talk to your health visitor, midwife, GP or breastfeeding specialist as soon as possible, they will be able to help you sort it out quickly.
Here are some common breastfeeding issues, and tips on what to do.
- Colic
- Constipation
- Mastitis
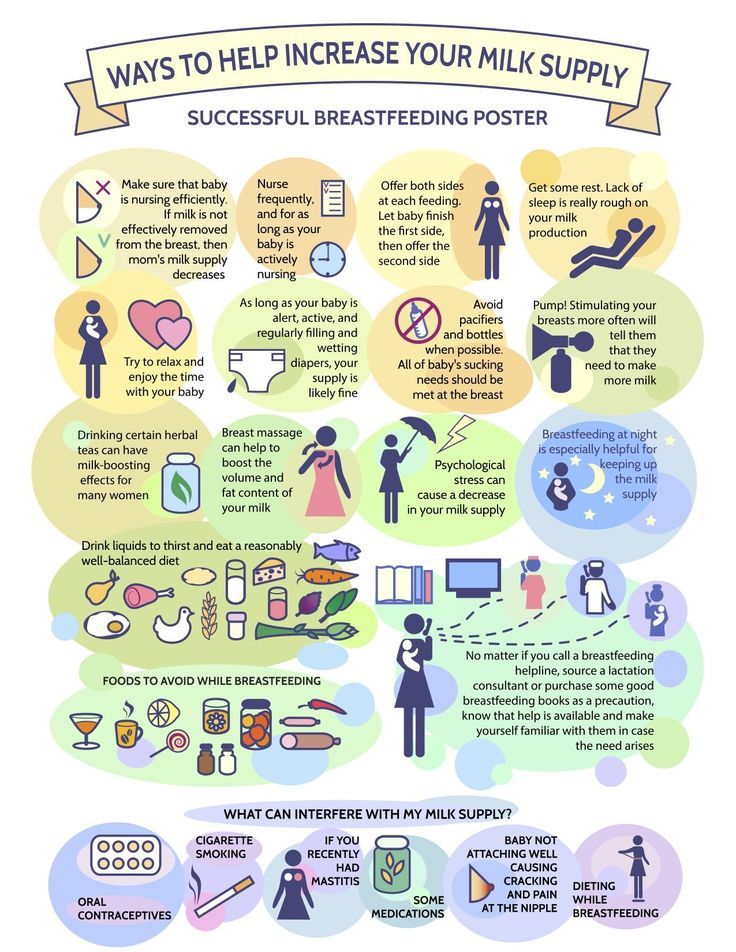
- Milk supply
- Reflux
- Sore nipples
- Thrush
- Tongue-tie
Baby reflux
If your baby brings up milk, or is sick during or after feeding, this is known as reflux. Reflux, also called posseting or spitting up, is quite common and your baby should grow out of it, usually by the time they are 12 months old.
What causes baby reflux?
The muscle at the bottom of the food pipe acts as a kind of door into the stomach – so when food or milk travels down, the muscle opens allowing the food into the stomach.
However, while this muscle is still developing in the first year, it can open when it shouldn't (usually when your baby's tummy is full) allowing some food and stomach acid to travel back up again. Acid in the stomach is normal and a necessary part of the digestion process – it helps break down food.
In most babies, reflux is nothing to worry about as long as they are healthy and gaining weight as expected.
Baby reflux symptoms
- Constant or sudden crying when feeding.
- Bringing up milk during or after feeds (regularly).
- Frequent ear infections.
- Lots of hiccups or coughing.
- Refusing, gagging, or choking during feeds.
- Poor weight gain.
- Waking up at night a lot.
GORD
When reflux becomes painful and it happens frequently, this is known as 'gastro-oesophageal reflux disease' (GORD). GORD is more serious than mild, everyday reflux. The strong stomach acid can irritate and make the food pipe sore and inflamed, which is painful for your baby and may result in them needing medication.
The main signs and symptoms of GORD in your baby are:
- spitting up frequently
- abdominal pain
- feeding difficulties
- seeming unsettled and grizzly after a feed
These symptoms can lead to your baby not gaining weight, or even losing weight.
Silent reflux
Silent reflux can be confusing as there are no obvious signs or clues (such as spitting up). It's when the food travels back up the food pipe – but it's swallowed rather than spat out so is harder to identify. But your baby may display similar symptoms to those of regular reflux.
Breastfeeding Friend from Start for Life
The Breastfeeding Friend, a digital tool from Start for Life, has lots of useful information and expert advice to share with you – and because it's a digital tool, you can access it 24 / 7.
Breastfeeding tips for babies with reflux
- Feeding little and often (smaller feeds stop their tummy getting too full).
- Burping them requently during feeds – have a look at our guide to burping your baby for techniques.
- Try a different feeding position – check out our our guide to breastfeeding positions.
- Keep your baby upright, for at least an hour after feeding, this should help keep the milk down.
If you are mixed feeding (combining breastmilk and formula feeds), have a look at our advice on bottle feeding and reflux.
When to see the GP
If your baby has difficulty feeding or refuses to feed, regularly brings milk back up and seems uncomfortable after a feed, talk to your pharmacist, GP, or health visitor. They'll be able to give you practical advice on how to ease the symptoms and manage it – they may also need to rule out other causes (such as cow's milk allergy).
It might be helpful to keep a record of when your baby feeds, with details of how often and how much your baby brings the food back up, and how often your baby cries or seems distressed. This will help your health visitor or GP decide if your baby needs treatment.
Signs, symptoms and how to help
Reflux and regurgitationReflux and regurgitation are when your baby brings up small amounts of milk after a feed. It’s perfectly normal. In fact, around 30% of healthy babies experience regurgitation during their first year, while their digestive system is still maturing1.
Read on to learn about the signs and symptoms to look out, what causes reflux and regurgitation, and how to relieve it.
What is reflux or acid reflux in babies?Reflux (or acid reflux) in babies is when milk goes into your baby’s stomach, but then comes back up into their oesophagus – or food pipe2. This is referred to as gastro-oesophageal reflux. If it becomes painful and happens frequently it’s known as gastro-oesophageal reflux disease (GORD)2.
Regurgitation (also known as ‘posseting’ or ‘spitting up’) is when milk goes into your baby’s stomach, but then comes back up into, or out of, their mouth. Unlike vomiting there’s no straining involved; it’s effortless, more like a hiccup2.
Reflux and regurgitation are both very common and completely normal. You may worry that your little one isn’t getting enough nutrients, but as long as they aren’t showing signs of discomfort or losing weight, there shouldn’t be a problem.
Gastro-oesophageal reflux disease in babies (GORD/GERD)
Gastro-oesophageal reflux disease, (GORD, or GERD in the US), is when your baby experiences prolonged symptoms of acid reflux, which can become troublesome or begin to cause complications.
Silent reflux in babies
Confusingly, some babies suffer from silent reflux3. This is much harder to diagnose because they only bring up a small amount of milk, or don’t spit out what comes back up but swallow it instead. While babies with silent reflux might not appear to bring up their milk, and may even continue to gain weight normally, they may show some of the other symptoms of reflux.
Signs and symptoms of reflux in babies
Symptoms of reflux include3:
- Bringing up small or large amounts of milk during and after feeding on a regular basis, with no other obvious signs of illness.
- Coughing or spluttering during feeding and having trouble swallowing milk.
- Crying during and after feeds.
- An arched back during and after feeds.
- Crying suddenly and/or constantly.
- Recurrent hiccups.
- Irritability and unsettled sleep.
What causes reflux in babies?
It makes no difference if your baby is breast- or bottle-fed. Reflux can affect any baby from shortly after birth until their first birthday.
When your baby is born, the oesophagus (the pipe leading from your baby’s mouth to their stomach) isn’t always fully developed. The oesophagus has a valve which closes over the stomach, helping food to stay down and be digested. In newborn babies, this valve may not be quite ready to fully function, meaning that milk and stomach acid occasionally come back up. The good news is that this valve gets stronger during your baby’s first year of life. As this happens, the chances of your baby developing reflux get much, much lower4.
Feeding is new to your baby and their tiny tummy is still getting used to the sensation and process of eating and feeling full.
Lying down after feedsIf your baby spends a lot of time lying down, with a lot of milk in their tummy it may be harder for them to digest.
Your baby drinking too much at onceThis can cause discomfort in their tummy.
How long does reflux last in babies?
Reflux usually starts before a baby is 8 weeks old and usually resolves itself before their first birthday4. If baby gets reflux for the first time after they’re 6 months old, or is older than 12 months and still has reflux, make an appointment with your GP4.
Baby reflux management: how to help
While reflux is usually nothing to worry about and generally resolves itself,
there are plenty of things you can do to help:
- Feed your baby little and often – smaller amounts of milk are more manageable for tiny tummies.
- Take your time – babies with reflux don’t cope well if feeding happens too quickly.
- Try to keep your baby upright during and after feeding.
- Try winding your baby before and after feeds.
- Avoid bouncing your baby up and down after a feed.
- Avoid dressing your baby in outfits that are tight around the waist.
- If you’re bottle-feeding, try a slow-flowing teat to stop your baby guzzling their milk and taking in too much in one go.
- You might also want to speak with your GP or pharmacist about the special infant formulas available for babies with reflux.
Taking care of you: Happy mum, happy baby
Coping with reflux is hard. You may feel as though you don’t want to feed your baby anywhere other than at home, where there’s an abundance of muslin cloths and a change of clothes at hand. You may also feel that all you do is feed your baby, because the moment you’re finished they bring it all back up and you have to start all over again. Or you may find yourself worrying that your baby isn’t getting enough nutrients - but rest assured that this is highly unlikely.
It’s completely normal to feel a bit helpless or anxious about your baby’s next feed if your baby is suffering from with reflux. We also know that trusting your instincts is the right thing to do; after all, you know your baby better than anyone else. If you’re concerned about your baby’s weight, or your baby is often bringing up large amounts of milk and appears to be distressed or in pain, talk with your Health Visitor and GP. Together you can look at ways to make feeding time more manageable for you and your little one.
References
- Vandenplas Y et al. J Pediartr Gastroenterol Nutr 2015;61(5) 531-7
- NHS Start 4 Life. Breastfeeding challenges. [Online]. Available at: https://www.nhs.uk/start4life/baby/breastfeeding/breastfeeding-challenges/reflux/ [Accessed October 2020].
- Vandenplas Y et al.
J Pediartr Gastroenterol Nutr 2009;49:498-547.
- NICE. NG1. Gastro-oesophageal reflux disease: recognition, diagnosis and management in children and young people. 2015. Available at: https://www.nice.org.uk/guidance/ng1/resources/gastrooesophageal-reflux-disease-recognition-diagnosis-and-management-in-children-and- young-people-51035086789 [Accessed October 2020].
- NHS. Reflux in babies. [Online]. 2019. Available at: https://www.nhs.uk/conditions/reflux-in-babies/ [Accessed October 2020]
Last reviewed: 18th October 2020
Reviewed by Nutricia’s Medical and Scientific Affairs Team
Related Articles
Join the club
Ready to stop worrying about what other people think and do what feels right to you? We’ll give you the support you need to follow your instincts and enjoy parenthood to the max:
*Weaning is recommended at around 6 months. Please speak with a healthcare professional before introducing solid foods.
Join the club
Ready to stop worrying about what other people think and do what feels right to you? We’ll give you the support you need to follow your instincts and enjoy parenthood to the max:
Helpful emails
Non-judgemental support
Free weaning plan*
Tips from real parents
Join now
*Weaning is recommended at around 6 months. Please speak with a healthcare professional before introducing solid foods.
Why the infant is shuddering in a dream
09/17/2015
82809
57
Calm Sleep conditions
0-6 months
Article
Tatyana Chkhikvishvili
Tatyana Chkhikvishvili
Head of the ONLINE- programs, psychologist, sleep and breastfeeding consultant
Mom of two children
Have you ever noticed how a child who is falling asleep or already sleeping suddenly shudders? Why the child is twitching, should parents worry, how to help the child - our article tells.
0–4 months. Improve sleep in 3 weeks
Why do babies startle in their sleep?
REM sleep
A month-old baby's sleep consists almost half of REM sleep (also called REM sleep). It is believed to be necessary for the growth and development of the brain. As the child grows older, the proportion of REM sleep gradually decreases. By the age of 3-5, it is already about a third.
In this phase, the newborn often twitches, moves his arms and legs rather strongly, grimaces, makes sounds, reproduces sucking movements with his mouth, actively moves his pupils. Sometimes it is even difficult for parents to understand whether he is sleeping at all or not.
REM sleep is not strong, and when the newborn twitches, he can wake himself up with his arms. In this case, swaddling helps very well - it “extinguishes” twitches when the baby shudders. The sling performs the same function.
Gradually, the child's nervous system matures, he shudders less and less, and the need for swaddling disappears. This usually happens after 4-6 months, but some parents find that swaddling works well later.
Why else can a newborn start in his sleep?
Sleep structure
At 1-3 months of life, infants develop slow-wave sleep. Now sleep begins precisely with the phase of non-REM sleep, which is divided into three stages:
- Falling asleep itself, or falling asleep.
- Superficial sleep.
- Deep sleep.
When the phase of non-REM sleep ends, it is the turn of fast sleep. And then a new cycle begins. Often between these cycles, the baby wakes up.
During falling asleep and light sleep, children often startle. They are associated with a change in nervous excitability in transitional states - from wakefulness to falling asleep and between different stages.
Moro reflex and startle
As you know, babies are born with a whole set of reflexes. One of them is the Moro reflex. What it is: the baby takes the arms to the sides, fingers spread out, and then presses them to him. The Moro reflex is another reason why newborns startle so often. It is quite clearly expressed up to 4 months, and by about 6 months it gradually fades away.
Throwing up due to noise and unsuitable temperature
The newborn may startle due to sharp sounds. The reason may be a phone call, a car signal, the sound of a fallen object. Throwing up in a dream can also be if the child is cold or hot.
Pediatrician's comment
Natalya Trofimova
Senior sleep consultant, pediatrician
Newborn reflexes are unconditioned, that is, congenital. The severity of reflexes depends on the condition of the child, the gestational age at birth, the weight of the baby, and how long he was fed. In the first days after birth, reflexes can be reduced even in healthy newborns. Reflexes fade at different rates, most by 3–4 months.
The Moro reflex occurs in response to auditory (clapping), tactile and vestibular stimuli (patting on the changing table, on the child's buttocks, moving the position of the body, sharp straightening of the legs).
This reflex has 2 phases:
- Pulling the arms to the sides and opening the hands.
- Return to starting position.
In full-term children, the second phase is more pronounced, in premature babies, on the contrary. The Moro reflex fades by 6 months of age.
Spontaneous Moro reflex is a symptom of increased neuro-reflex excitability. Latent hyperexcitability is detected if the Moro reflex is also caused by tapping a finger on the sternum.
As regards sleep twitches in infants, they are normally much more common than in adults, especially those born prematurely. The earlier the baby was born, the more different movements he has in sleep and when falling asleep.
These jerks are not random or purposeless. Research shows that proprioceptive feedback from a twitching limb triggers bursts of electrical activity in the appropriate areas of the developing cortex.
How to help a baby who starts in his sleep
Swaddling
Swaddling allows the child to reduce the number of throwing up in a dream and increase the duration of restful sleep. Swaddling helps to recreate intrauterine sensations that reduce stress in a child, soothe him.
Regular swaddling and traditional swaddling can be used. And you can use Australian swaddling or a special modern convenient envelope with Velcro or zippers.
Remember the rules of safe swaddling!
White Noise
If a child throws up his hands because of a sharp noise, white noise will become an indispensable assistant. White noise not only reminds the baby of the sounds that he is used to hearing in his mother's stomach, he is able to veil, smooth out extraneous sounds. Read the rules for the safe use of white noise.
Optimum temperature
The optimal conditions for sleep are considered to be a temperature of 18-22 about C and a relative humidity of 40-60%. Before laying, ventilate the room even in winter. If necessary, use a humidifier. Do not dress your baby too warmly and do not cover with a blanket. It is better to put the crib away from the battery.
Call your doctor if you see any of the following symptoms while raising your baby's arms:
- The baby's start during sleep occurs throughout the duration of sleep and is accompanied by crying.
- The child begins to shudder in his sleep, if he has not shuddered before.
- The baby flinches too often.
- The shuddering continues even if the child is picked up.
- Startles are accompanied by tilting the head, trembling of the chin, frequent regurgitation.
In the first months of life, it is normal for a baby to shudder quite a lot in a dream, gradually such shudders become less. Try to help your child sleep peacefully, create the right conditions in the bedroom.
If you need counseling help, come to BabySleep for an individual consultation. It can be a short one-time consultation or an escorted package.
', nextArrow: '', responsive: [{breakpoint: 1199, settings: {arrows: !1, infinite: !1, slidesToShow: 1}}] }) })Elena Muradova
Founder of BabySleep, the first sleep consultant in Russia and the CIS
Consulting center specialists | Children's Clinical Diagnostic Center in Domodedovo
Alexander Savich General Director
Kharitonova Marina Alekseevna Chief physician, pediatrician, member of the Union of Pediatricians of Russia
Badamshina Liliya Mikhailovna Radiologist of the highest category, doctor of ultrasound diagnostics of the highest category, Doctor of Medical Sciences
Tarasova Irina Viktorovna Candidate of Medical Sciences, Associate Professor
Allergist-Immunologist
Laletin Evgeny Viktorovich Pediatrician
Nikolsky Grigory Nikolaevich Otolaryngologist
Tatyana Yurievna Krylova Ophthalmologist
Andrey Karpov Orthopedic surgeon, doctor of the highest category
Strelnikova Maria Vladimirovna Ophthalmologist
Kazantseva Marina Anatolyevna Candidate of Medical Sciences, Doctor of Ultrasound Diagnostics
Pozdnyakov Boris Aleksandrovich Orthopedic surgeon
Kotova Anastasia Sergeevna Dermatologist
Danilycheva Lyubov Ivanovna Pediatric endocrinologist, pediatrician
Slesareva Olga Valerianovna Children's massage therapist
Shubin Vladimir Gennadievich Vertebroneurologist, chiropractor
Silenko Oksana Nikolaevna Pediatric gynecologist, candidate of medical sciences
Ermolaev Sergey Sergeevich Candidate of Medical Sciences, neurologist, doctor of functional diagnostics
Prodan (Stepanchikova) Olga Viktorovna Neurologist
Kiseleva Lyudmila Ivanovna Pediatrician, doctor of functional diagnostics
Salimova Kristina Salimovna Ophthalmologist
Usova Olga Yurievna Medical (clinical) psychologist
Lazebnaya Elena Vasilievna Pediatric cardiologist, ultrasound diagnostician
Krylova Olga Yurievna Neurologist
Guseva Anna Andreevna Senior Administrator, Contract Curator
Andrey Unanov Pediatrician, Nephrologist
Golikov Vladimir Alekseevich Dermatologist
Elena Mamontova Doctor - pediatric cardiologist
Arkhipova Irina Vitalievna Otolaryngologist
Bagirov Elchin Safailevich Pediatrician
Azbukina Olga Aleksandrovna Neurologist-epileptologist
Danilyuk Natalya Vitalievna Nurse
Yulia Lokteva Nurse
Lusine V.