Baby leaks milk from mouth while bottle feeding
Bottle-feeding babies: giving the bottle
About bottle-feeding
If your baby can’t always feed directly from your breast, you might choose to bottle-feed with expressed breastmilk. Or you might need to feed your baby infant formula, which is the only safe alternative to breastmilk.
Before you bottle-feed your baby, it’s important to know how to clean and sterilise bottle-feeding equipment, as well as how to prepare, store and warm bottles of formula. This will help to keep your baby safe from infection and make sure baby is getting the right nutrition.
Getting the right flow when bottle-feeding
To test the flow of the formula or breastmilk, hold the bottle upside down when it’s filled with liquid at room temperature. The liquid should drip steadily from the teat but not pour out.
If you have to shake the bottle vigorously to see the drip, the flow is too slow. Your baby might go to sleep before drinking what they need.
When you feed your baby, you might see a little leakage at the corners of your baby’s mouth. This doesn’t mean the flow is too fast. It’s nothing to worry about. It will stop as your baby gets older.
If you have trouble finding a teat with a flow to suit your baby, try a faster teat rather than a slower one. You might need to try a few different teats before you find one that suits.
Giving baby the bottle
Make yourself comfortable and cuddle your baby close to you, holding baby gently but firmly. It’s better for your baby to be on a slight incline so any air bubbles rise to the top, making burping easier.
Put the teat against your baby’s lips. Your baby will open their mouth and start to suck. Keep the neck of the bottle at an angle so it’s filled with formula or breastmilk.
When your baby stops sucking strongly or when about half of the formula or breastmilk has gone, gently remove the bottle and see whether baby wants to burp. Once you’ve tried burping your baby, you can offer the bottle again.
Paced bottle-feeding
Babies who are normally breastfed might find it hard to pace themselves when bottle-feeding, particularly if they’re premature. This is because they’re used to controlling the flow of breastmilk. Sometimes these babies can drink too much too quickly.
This is because they’re used to controlling the flow of breastmilk. Sometimes these babies can drink too much too quickly.
Paced feeding can sometimes help. This involves holding your baby in an upright position and letting them rest every few minutes. If you’re interested in paced bottle-feeding, it’s best to get help from your child and family health nurse or a lactation consultant.
Holding, cuddling and talking to your baby during feeding will help baby develop and grow. It’s also a great opportunity to bond with your baby.
When baby doesn’t finish the bottle or goes to sleep while feeding
Don’t worry if your baby doesn’t finish the bottle. Babies are very good at judging how much they need, so you can let your baby decide when they’ve had enough formula or breastmilk.
If your baby goes to sleep during a feed, put baby over your shoulder, rub their back, and stroke their head, legs and tummy. This can help your baby to wake up. A nappy change is a good way to wake up your baby if that doesn’t work.
Wait until your baby is properly awake before offering the rest of the formula or breastmilk.
If there’s any formula or breastmilk left in the bottle, throw it away after one hour. When your baby drinks from a bottle of formula or breastmilk, bacteria from their mouth get into the milk. The bacteria can grow and make your baby sick if you give your the baby the half-finished bottle later.
When baby refuses the bottle
Babies sometimes refuse a bottle altogether. Here are things to try if this happens:
- Try a new feeding position or change the feeding environment. For example, move around while you’re feeding, find a quieter place to feed, or play some relaxing background music.
- Try again later when your baby is more settled. For example, give your baby a bath and then try again.
- Ask your partner or another family member to give your baby the bottle.
- Try using a different teat. If the flow of formula or breastmilk is too slow, it might frustrate your baby.

- Let your baby open their mouth for the bottle when they’re ready, rather than putting the teat into their mouth.
- Offer the formula or breastmilk from a small cup or spoon. To do this, sit your baby up and offer them small sips.
If your baby is regularly refusing the bottle, you could try adjusting your routine.
If you think your baby is refusing the bottle because they’re unwell, treat your baby’s symptoms or take your baby to see your GP.
How much do bottle-feeding babies drink?
Newborn babies commonly have 6-8 feeds every 24 hours, but there’s no set amount of food or number of feeds your baby should have. Different babies drink different amounts of formula or breastmilk. Some might have feeds close together and others further apart. And it can change from day to day.
Just feed your baby whenever they’re hungry. You’ll see baby cues that say ‘I’m hungry’ – for example, your baby will make sucking noises or start turning towards the breast or bottle. If your baby stops sucking or turns their head away from the bottle, you’ll know they’ve had enough.
If your baby stops sucking or turns their head away from the bottle, you’ll know they’ve had enough.
As your baby eats more and more solid food, the total amount of breastmilk or formula they take in a day will decrease. The amount of breastmilk or formula will also decrease as your baby starts to drink from a cup instead of a bottle.
Some babies never drink the ‘recommended amount’ for their age and size, and others need more. Plenty of wet nappies, consistent healthy weight gains, and a thriving, active baby mean all is well. If you’re concerned about how much breastmilk or formula your baby is taking, talk to your child and family health nurse or GP.
Bottle-feeding in bed: issues and risks
Sleep associations
If your baby gets used to falling asleep with a bottle in bed, they might depend on it to get to sleep. This can make it more difficult for your child to fall asleep or settle for sleep independently.
Bottle-feeding in bed also has several risks for your baby.
Choking
Babies who fall asleep while bottle-feeding can draw liquid into their lungs. They might then choke on it or inhale it.
Tooth decay
Babies have less saliva in their mouths to protect their teeth during sleep. If your baby falls asleep with a bottle, the lactose in the milk can build up on your baby’s teeth, putting your baby at risk of tooth decay.
Ear infections
If your baby drinks while lying flat, milk can flow into the ear cavity, which can cause ear infections.
It’s best to put your baby to bed without a bottle or to take the bottle away after your baby has finished feeding.
Using a feeding cup
When your baby is around 6 months old, you can help your baby start leaning to drink from a cup. It’s best to stop using bottles by the time your baby is 12 months old.
You should continue to thoroughly wash and sterilise feeding cups containing infant formula or breastmilk until your baby is 12 months old.
Correctly bottle feeding your baby
Correctly bottle feeding your baby can promote breast to bottle and back as well as prevent ear infections.
Before becoming a NICU nurse, I didn’t even know there were different “ways” to hold your baby while feeding. I had only ever seen – and done – the “crook of the arm” feeding. This is the way babies, in my mind, were always fed!
Well, the NICU quickly changed that!
Did you know that the instinct to feed is not generally seen in babies less than 36 weeks gestation? This means that babies born before 36 weeks (also known as late preterm) may not show signs that they are ready to take a feeding by mouth (bottle or breast).
For this reason, it’s not uncommon to see premature + late preterm babies with a nasogastric (NG) tube. This tube allows baby to be fed breastmilk or formula straight into their tummy without the actual act of eating.
As babies approach their due date and become “term” (36-37 weeks+, sometimes a bit earlier), we test their readiness to feed by bottle.
We give them little tastes of milk on a pacifier to help them learn how to suck, swallow, and breathe correctly (we even give preemies a swab of breastmilk very early on to get them familiar with the taste!).
But giving tastes does more than just familiarize them with the taste and smell of milk – it actually tells us A LOT of information!
We can gather baby’s interest in feeding, neurological readiness (sleepy preemies can’t take a bottle!), and read their cues. Have they developed a negative association with oral stimulus (paci, bottle) from having a breathing tube for so long?
Is their reflux so painful that they associate feedings with pain? Are they overwhelmed while feeding (sleepy at the bottle, breathing fast, dropping their heart rate low, sticking their tongue out and pushing the bottle out?)
Suck, swallow, breathe is a coordination skill that some babies need a little help in mastering.
I say this all the time to my clients, but LOOK at your baby and LISTEN to cues as you feed! We can gather SO MUCH information by looking at our baby feed – including signs of hunger, satiety, oral aversion, reflux, etc.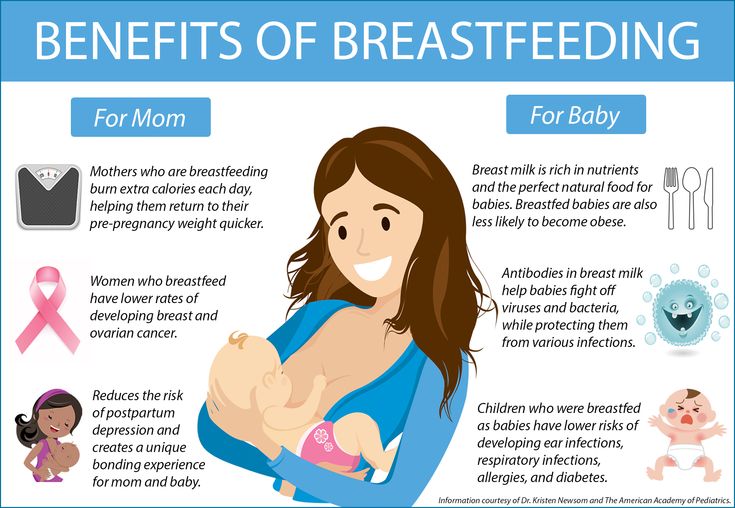
We understand that bottle feeding can be challenging! We are here to help you! Click here to learn more about the supportive services we offer!
My baby isn’t a preemie. Do I still need to watch them closely while they feed?
Yes! Bottle feeding should still be to your term baby’s cues. Feeding and taking a bottle is a skill that baby needs to learn how to do.
And bottle feeding positioning is important for many reasons which we will get into below.
Why is it so important to know your baby’s feeding cues while bottle feeding?
It tells us a lot about how baby is feeling during a feed:
- It tells us if baby needs to slow down the pace (size down on a nipple) or speed up the pace (upsize the nipple). See below.
- It tells us if baby is full. We often try to feed all the contents of the bottle – but baby may not want all the contents. It’s MORE important for baby to control the amount they take in and have a positive experience, than accidentally force feeding.

- It tells us if baby is still hungry BUT prevents overfeeding. If a bottle is completely finished, and baby is rooting or sucking, they may want more. We will talk about side lying feeding in a bit, but basically by following baby’s cues with side lying, baby is controlling the pace of the bottle.
- So if baby does want more, it is available to take at their pace, rather than dripping out of the bottle due to gravity. Signs of being done with the bottle include yawning, sneezing, pushing out of the tongue, pushing the bottle out with the tongue, arching back away from the bottle, gazing up and away from the bottle.
- It tells us if baby is overwhelmed. Persistent hiccuping, sneezing, yawning, gagging, or pushing out of the tongue all are signs of being “done” or overwhelmed with the bottle.
- It prevents oral aversion. You wouldn’t like it either if someone was forcefully sticking food in your mouth! Repetitive accidental force feeding creates an oral aversion, refusal of the bottle, fussiness, and refusal to eat by bottle.
- Try allowing baby to open BEFORE you place the bottle in baby’s mouth by gently tickling their upper lip with the bottle. Once baby opens, they are ready to latch and feed.
But who CARES?! My baby hasn’t shown any of these things and feeds just fine the way I feed her.
YOU are the parent! You have every right to make the decision for your baby! I am here to inform and help you prevent or reverse some possible negative symptoms of gravity-lead bottle feeding positioning.
Does it matter if the contents in the bottle are formula or breastmilk?
No! Anytime you are bottle feeding, no matter the contents, side-lying is the way to go.
Correctly bottle feeding
SIDE LYING POSITIONING + INCLINED!
What is side lying + inclined positioning?
Side lying positioning is when baby is laying on their side (ear, shoulder, and hip should all be aligned). Then, incline their head slightly with your hand or a pillow (I even just cross my legs!).
Why is side lying + inclined feeding important?
Side lying + inclined feeding mimics breastfeeding – both in position and flow. It allows baby to control the flow of the bottle, leading to a positive experience with the bottle, less choking and coughing, less flooding, and LESS EAR INFECTIONS!
A bottle has an opening at the nipple. This opening is consistently open, whether baby is sucking or not. Test by holding a bottle upside down – it drips!
This dripping also happens in baby’s mouth when we hold the bottle in a downward position where gravity is pulling the milk out of the bottle, not baby, such as in the “crook of the arm” feeding position.
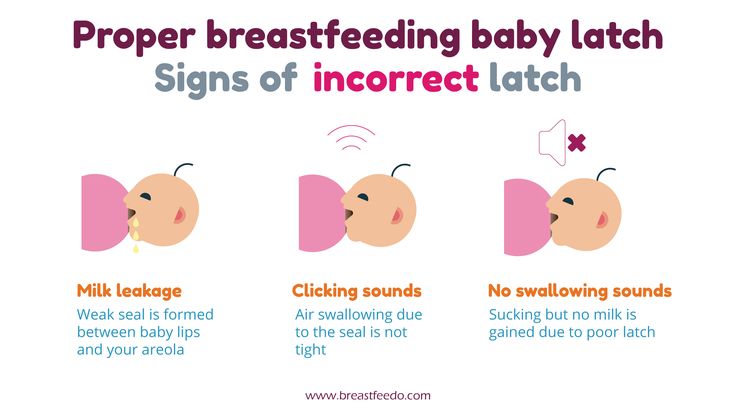
When gravity pulls out the milk (aka dripping of the bottle), baby is actually getting more milk flow than they are sucking out. This causes baby to get flooded – meaning there is too much milk in baby’s mouth.
This makes it hard to baby to keep up with the amount of milk in their mouth – leading to gulping, choking, coughing, milk dripping out of the side of their mouth.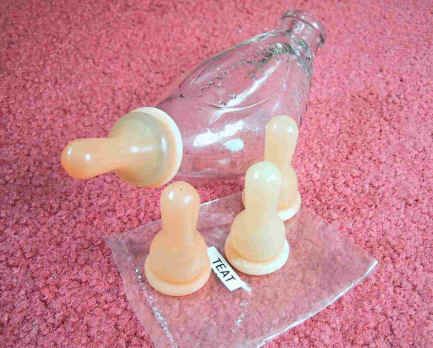
This can happen with a “crook of the arm” positioning because the nipple is angling down, allowing gravity to do the work.
Think about if you were trying to drink something using a straw. Then, someone was simultaneously pushing more liquid in your mouth.
It would be really hard for us to keep up! If this was consistently happening, we would pretty soon say, “I’m not drinking out a straw anymore!”
This same thing happens to baby – they simply can’t keep up and may start to associate the feeds negatively.
How do I feed baby in side lying position?
- Bend your knees and elevate your legs on a coffee table or ottoman. If you don’t have those available, cross your legs or place a pillow on your lap.
- Place baby in side lying position on your lap with their head closest to your knees.
- Support baby’s head and neck with your non-dominant hand.
- Hold the bottle parallel to the floor.
- Feed baby.
Tip: Watch my reels on how to correctly bottle feed your baby and how to burp your baby!
Ear infections + how they related to feeding positionEar infections are also called otitis media. They are very common, especially in infants. Side note – ear infections are NOT contagious.
They are very common, especially in infants. Side note – ear infections are NOT contagious.
The eustachian tube in the ear connects the middle ear with the back of the throat. If formula or breastmilk continually is entering the eustachian tubes, this causes bacteria from the mouth (naturally occurring bacteria) to enter the middle ear, causing ear infections.
Bacteria feed on the nutrients in breastmilk and formula, making easy for them to multiply, causing and infection.
“Crook of the arm” is gravity lead, which leads to flooding, making the risk of formula or breastmilk entering the eustachian tubes much higher (and therefore the middle ear), which in turn increases the risk for ear infections.
Side lying feeding is baby lead, meaning baby is pulling the amount they can handle from the bottle. This prevents flooding, and therefore, the risk of ear infections is much lower.
I heard that breastfeeding lowers the chance of ear infections. Is that true?
Is that true?
To an extent. Breastmilk does contain antibodies that can help prevent infections, including ear infections. However, bottle-fed breastmilk poses basically the same risk as formula since the positioning is actually what causes the ear infections.
Breastfeeding from the breast does help reduce the risk for ear infections due to proper positioning and flow, however, it does not eliminate the risk.
I see air in the nipple. Should I be concerned?
No. Air at the top of the nipple is normal – the milk still fills the tip of the nipple so baby won’t suck in air.
My baby is gulping and chokes on the bottle. What can I do?
Your baby may need a smaller size nipple. If you’re already using the smallest size, try paced feedings. Paced feedings allow baby to “catch up” and swallow the milk in their mouth, then breathe, then suck.
Too much milk will cause them to gulp, not be able to take a breath, etc. Click here for a demonstration.
Click here for a demonstration.
My baby gets frustrated at the bottle and when I take the bottle out, the nipple is completely flat and collapsed.
Time to move up to the next size nipple! Baby is sucking harder than the nipple flow allows.
It takes FOREVER for my baby to feed from the bottle, more than 45 minutes. What can I do?
Try upsizing the nipple! If baby is dripping, gagging or choking, the flow is too fast and move down a nipple size. Or try paced feedings with the larger nipple.
My breastfed baby WILL NOT take a bottle. HELP!
Your wish is my command! We offer 1:1 virtual consults from the comfort of your own home to introduce the bottle to your breastfed baby in a way that promotes a positive association with the bottle.
We also offer in home bottle feeding consultations for the Chicagoland area!
Click here to view the consultations we offer!
Watch our workshop!
Watch our recorded workshop, “Bottle Refusal and Tips. ” Join Lauren, NICU RN and mother of 2, discuss tips for bottle refusal in infants. She discusses different strategies for avoiding bottle refusal along with tips and tricks for reversing bottle aversions. She also goes over alternative methods for giving breast milk/formula to babies who have ongoing issues with bottle refusal. Are you exclusively pumping or offering pumped milk in a bottle? You may have high lipase which could be causing bottle refusal. Read more here in our high lipase and ways to battle it blog post.
” Join Lauren, NICU RN and mother of 2, discuss tips for bottle refusal in infants. She discusses different strategies for avoiding bottle refusal along with tips and tricks for reversing bottle aversions. She also goes over alternative methods for giving breast milk/formula to babies who have ongoing issues with bottle refusal. Are you exclusively pumping or offering pumped milk in a bottle? You may have high lipase which could be causing bottle refusal. Read more here in our high lipase and ways to battle it blog post.
WATCH BOTTLE WORKSHOP NOW
Have more questions? Schedule a text or video chat consult with Kate, Lauren or Natalie (NICU RNs) and they can help answer any questions that you have!
BOOK CONSULT NOW
PRO TIP: I highly recommend these Lansinoh bottles (I use them all the time in consultations). I also really like these Evenflo bottles for newborns too!
Other helpful blog posts:
- High lipase breastmilk and how it relates to bottle refusal
- How to supplement with formula
- Everything you need to know about acid reflux
- Transitioning from formula to milk
- Everything you need to know about formula
- Diaper bag essentials
- How to travel with kids
**This post is educational and not meant to take the place of your provider. Bumblebaby makes a small commission on some of the items listed above
Bumblebaby makes a small commission on some of the items listed above
Bottle feeding | Canpolbabies.com
Find out how to bottle feed your baby safely, how to help your baby feel safe while feeding, and how to set feeding times based on your baby's needs.
The most important thing is to choose the right position when feeding
When bottle feeding, avoid lying down as the milk flows out of the bottle under the force of gravity (at a constant rate controlled by alternating pressure on the nipple).
An infant may choke on milk if fed in a horizontal position. Therefore, it is very important to choose the right - more upright - position for feeding (the baby's head should always be slightly higher than the rest of the body).
Your baby's head should be in the crook of your arm, in line with his spine. The bottle feeding position should resemble the natural feeding position - especially when you feed him with two different feeding methods.
Remember:
- Never leave your baby alone with a bottle as they may choke
- Never let your baby sleep with a bottle in his mouth
How to give your baby a bottle
Put the bottle in your baby's mouth so that it forms a right angle with his face. Your baby should not encircle the entire nipple with his lips, but only its oblong part, while the lips should rest against the rounded part. The oblong part should always be full of milk. Otherwise, the baby will swallow a lot of air during feeding, which can cause colic. Air bubbles in the bottle mean your baby is suckling properly.
Emotional connection
Young children need parental love and affection. Your closeness helps him feel safe. Therefore, it is very important to talk affectionately with the baby as often as possible, hug and stroke him. Feeding is the best time to build an emotional relationship with your baby.
This is very easy to do when you are breastfeeding because you are already in physical contact with each other.![]() However, bottle feeding also allows you to be closer to your baby as he feels the warmth of your body. Bottle feeding also allows other family members - the father, brothers and sisters to get closer to the child, since not only the mother can feed the baby in this way.
However, bottle feeding also allows you to be closer to your baby as he feels the warmth of your body. Bottle feeding also allows other family members - the father, brothers and sisters to get closer to the child, since not only the mother can feed the baby in this way.
Calm emotional background
Never feed your baby when you are irritated or tense. Take time for yourself first, take a deep breath and try to relax. When you have calmed down, sit in a comfortable chair, place a pillow under your arm, place your baby on the pillow, and start feeding while speaking gently to your baby. Your child feels your emotions. If you are tense, he will also feel restless. Also, never feed your baby when he is excited, crying or screaming. When he is in this state, his airways are not protected and food can enter his larynx instead of his esophagus.
Feeding by the hour
Formula milk is not as easily digested by the baby's stomach as breast milk, so according to generally accepted rules, it should be given every 3 hours.
Some pediatricians say it's best to give your baby formula on demand, that is, when the baby is hungry. In their opinion, it is better to feed the child than to wait another hour and keep him in suspense because he wants to eat. However, you still need to control the number of feedings and your baby's weight gain.
During the first month of life, the baby should eat > 7-8 times a day, 90-100 ml for each feeding, in the second month of life: 6-7 times a day, 100-120 ml for each feeding. During the first six months, the baby should gain approximately 150-200 g per week.
Feeding breaks
When your baby suckles milk from a bottle, he also swallows air. Therefore, he may feel full even before he drinks half the bottle. When feeding a child, breaks should be taken every few minutes to allow the baby to take in air - after such a break, he should ask for food again. During feeding, hold the baby in an upright or semi-recumbent position for a while (sometimes even for several minutes) to give him the opportunity to release air accumulated during feeding from the digestive tract. Help the child by holding him on your shoulder, putting his hands on your back. Bend and spread his legs a little. You can also massage his back or pat him gently from the bottom up. Remember to protect your clothes with a diaper or towel. You can also help your baby burp out excess air when he is in your lap. The child should lie on his tummy, leaning on your hip, and his arms should hang freely on the other side. Its bottom should rest on your foot, slightly lower than the other foot.
Help the child by holding him on your shoulder, putting his hands on your back. Bend and spread his legs a little. You can also massage his back or pat him gently from the bottom up. Remember to protect your clothes with a diaper or towel. You can also help your baby burp out excess air when he is in your lap. The child should lie on his tummy, leaning on your hip, and his arms should hang freely on the other side. Its bottom should rest on your foot, slightly lower than the other foot.
Remember:
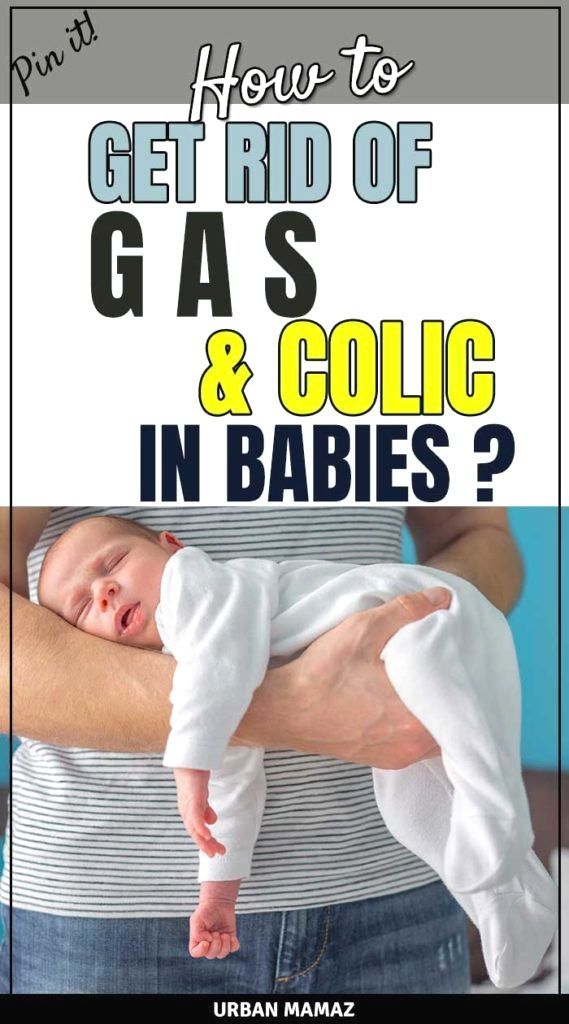
If you don't help your baby clear the air that has accumulated in his stomach, this can cause painful gas.
Preventive measures against regurgitation in children
08.03.2017
Regurgitation is the spontaneous reflux of gastric contents into the esophagus and mouth. This condition is not uncommon in infants and is often a cause for concern for parents. The frequency of regurgitation syndrome in children of the first year of life is 18-50%: up to 4 months - 67%, up to 6 months 24%, up to 1 year 5%.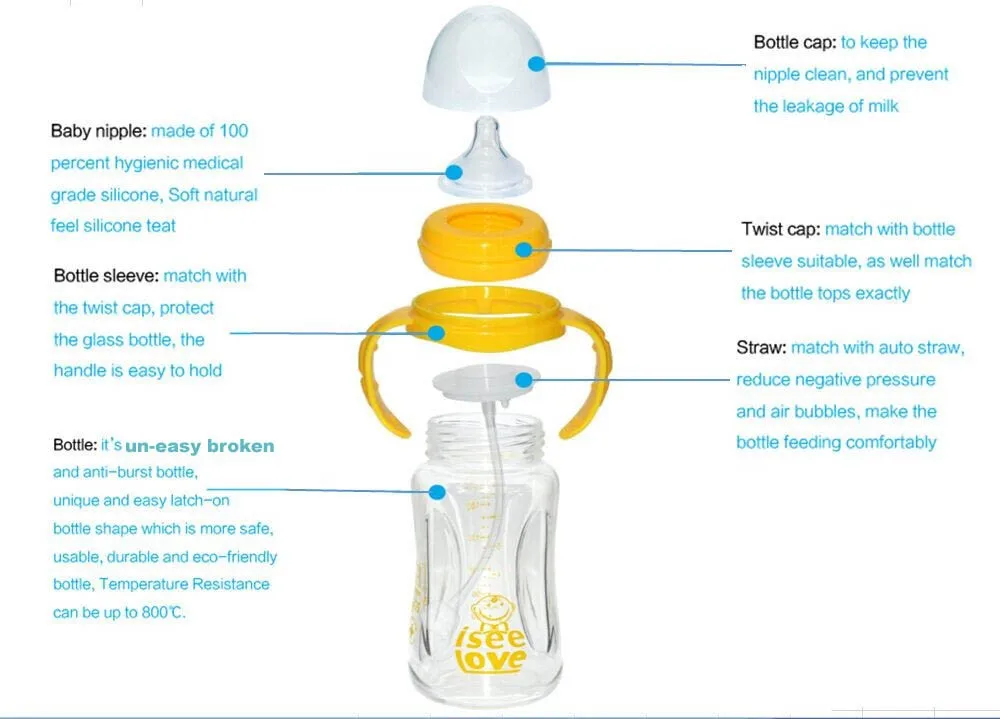 In most cases, regurgitation is "benign" and disappears on its own after 12-18 months. At the same time, “benign” or physiological regurgitation characterizes:
In most cases, regurgitation is "benign" and disappears on its own after 12-18 months. At the same time, “benign” or physiological regurgitation characterizes:
-
the age of the child is up to 12 months;
-
spitting up 2 or more times a day for 3 or more weeks;
-
sufficient weight gain;
The child has no signs of metabolic disorders, diseases of the gastrointestinal tract or the central nervous system. The child does not experience difficulty in swallowing or feeding, there is no forced position of the body.
Do not confuse regurgitation with vomiting. When a child burps, the abdominal muscles do not tense up. With vomiting, on the contrary, muscle tension occurs and food is ejected by pressure not only through the mouth, but also through the nose. In some cases, there may be general anxiety, pallor, cold extremities. Often with vomiting, the temperature rises, loose stools appear, which is a sign of an infectious disease. Vomit may contain unchanged milk, mucus, blood or bile.
Vomit may contain unchanged milk, mucus, blood or bile.
What causes physiological regurgitation
What is the tendency of babies to spit up? This phenomenon is explained by the peculiarity of the structure of the gastrointestinal tract of young children. At the age of one year, the esophagus is shorter and wider, physiological narrowing is weakly expressed. The stomach is located horizontally, its capacity is small, and the muscles that close the entrance to the stomach and prevent the contents from being thrown back into the esophagus are poorly developed. As the child begins to walk, the axis of the stomach becomes more vertical. The capacity of the stomach increases by the year from 30-35 ml to 250-300 ml. The secretory apparatus matures, the work of the closing muscles (sphincters) improves, which leads to a gradual decrease in the frequency and disappearance of regurgitation. These features explain the predisposition of young children to regurgitation and even the inevitability of this condition.![]() However, there are measures to help reduce the frequency of regurgitation.
However, there are measures to help reduce the frequency of regurgitation.
Factors contributing to physiological regurgitation include:
-
Overfeeding. As a rule, actively sucking babies begin to suffer from overfeeding, with abundant milk secretion, as well as when switching to artificial or mixed feeding with an incorrect calculation of the required amount of milk formula. Regurgitation appears immediately or some time after feeding in the amount of 5-10 ml. Milk can flow out unchanged or curdled.
-
Swallowing air during feeding (aerophagia). A similar situation arises if the child suckles greedily at the breast, and the mother's milk is not very plentiful; due to the retracted, flat nipple of the mother's breast, since the child fails to fully capture the nipple and areola; with artificial feeding, if the hole at the nipple of the bottle is large enough or the nipple is not completely filled with milk. Babies with aerophagia often experience anxiety after feeding, bulging of the abdominal wall (belly inflates).
 After 10-15 minutes, the swallowed milk flows out unchanged, which is accompanied by a loud sound of air eructation.
After 10-15 minutes, the swallowed milk flows out unchanged, which is accompanied by a loud sound of air eructation. -
Intestinal colic or constipation. These conditions lead to an increase in pressure in the abdominal cavity and a violation of the movement of food through the gastrointestinal tract, causing regurgitation.
Until the child is four months old, spitting up up to two teaspoons of milk after feeding, or one spitting up of more than three spoons during the day, is considered the norm. You can check the amount of spitting up in the following way: take a diaper, pour one teaspoon of water on its surface, and then compare this spot with the spot formed after the next spitting up.
Abnormal regurgitation may be due to:
-
surgical diseases and malformations of the digestive system;
-
diaphragmatic hernia;
-
pathology of the central nervous system, trauma of the cervical spine during childbirth;
-
food intolerance, lactase deficiency;
-
increased intracranial pressure.
Such regurgitation is characterized by intensity, systematicity, the child spits up a large amount of milk. At the same time, there is a violation of the general condition of the baby - the child is whiny, loses or does not gain weight, cannot eat the amount of food necessary for his age. In such a situation, a pediatrician, gastroenterologist, surgeon, allergist, neurologist should be examined. It also requires examination and exclusion of anomalies in the structure of the upper gastrointestinal tract, the preservation of regurgitation for more than 1 year.
Scale for assessing the intensity of regurgitation:
-
Less than 5 regurgitations per day with a volume of not more than 3 ml - 1 point.
-
More than 5 regurgitations per day with a volume of more than 3 ml - 2 points.
-
More than 5 regurgitations per day up to half the amount of formula or breast milk, not more often than in half of the feedings - 3 points.
-
Spitting up a small amount of milk for 30 minutes or more after each feeding - 4 points.
-
Regurgitation from half to full volume of formula or breast milk in at least half of the feedings - 5 points.
Regurgitation with an intensity of 3 or more points requires a visit to a doctor.
Preventive measures against regurgitation in children
If regurgitation is physiological in nature, then it is not worth treating or correcting in this case. It is necessary to deal with the elimination of the cause, if possible, and carry out prevention.
Prevention of regurgitation in children includes the following measures:
-
Postural therapy: when feeding, it is necessary to hold the baby at an angle of 45 °, make sure that he completely grasps the nipple with the areola; after feeding, hold the baby in an upright position ("column") for 20 minutes - to drain the swallowed air.
Due to this, the air that has entered the stomach will be able to go out. If nothing happened, then put the baby down and after a minute or two, lift him upright again.
-
Make sure that the opening in the bottle is not too large and that the nipple is filled with milk. Experiment with nipples - perhaps the other will be better. Milk should come out in drops, not a trickle.
-
Before you start feeding your baby, lay him belly down on a solid base.
-
After feeding, try to minimize the baby's physical activity, do not disturb him unnecessarily, and change clothes only if there is an emergency.
-
Avoid squeezing diapers or clothes on the abdomen of the child.
-
If the baby's appetite is good, then it is better to feed him often, but in small portions, otherwise, due to the large amount of food, the stomach may overflow, and this, as a result, leads to regurgitation of excess food.