Baby milk feeding video
Breastfeeding & baby-led attachment | Raising Children Network
Renee Kam (lactation consultant): Baby-led attachment is where a baby uses their own instincts to find the mother’s breast on their own accord. Baby-led attachment really helps to lay down the foundation for breastfeeding. A baby who has had many opportunities, particularly in the early weeks, to do baby-led attachment becomes a lot more orientated towards the breast.
Adele (mother of Charlie, 5 years, Noah, 3 years, and Holly, 4 weeks): I did baby-led attachment because I had a lot of trouble feeding my first baby and getting him to attach and when I saw a video of baby-led attachment it just looked like a natural way to do it, so I thought I would try it to see if that meant that I didn’t have attachment issues with the children I had after my first one.
Miranda (mother of Mattie, 8 years, Tacy, 6 years, Sedna, 7 months): When I had my second baby, when she was born at home and she was lying on me, she all of a sudden attached by herself, which was a wonderful feeling but I never followed-up on it because I didn’t know anything about it. So then when we moved to Australia I so wanted to try it so we tried it with this one. It really started at home, so when we got home we started doing it. You don’t have to do it straight away – baby-led attachment – it’s something that they can do for quite a few weeks after they’re born. It’s imprinted in their being, I guess.
Renee Kam: If a mother wants to do baby-led attachment the tips that I would give her would be the timing of it. So a baby will be able to follow through on their instincts best when they’re calm. So it would be when the baby’s showing early feeding cues such as turning their head from side to side with mouth open, sticking their tongue out, sucking on their hands, or it might be as soon as their baby wakes up from a sleep. So in those situations baby is typically calm and then if the baby is then placed skin-to-skin contact with the mum and the mum, say, is in a semi-reclined position, then that will help a baby to follow through on their instincts to find their mother’s breast.
Narrator: Find a comfortable position. Many mothers find that a semi-reclined position with pillows behind them for support works well. A partially laid-back position allows gravity to assist the baby in moving to the breast. With as much skin-to-skin as possible between you and your baby, place your baby on your chest facing you between your breasts with her head just above your breasts. Start when your baby is calm, such as when she is showing early feeding cues like turning her head from side to side with her mouth open.
As your baby starts to instinctively move towards a breast, she will start to lift her head and bob it around. As she moves towards a breast, you may find it helpful to hug her bottom in close to you and to support her neck and shoulders with your hand and wrist. It is important to avoid putting pressure on her head as she needs her head free to instinctively move it into an extended position to help her attach and feed well.
When her head nears your nipple, she may nuzzle around to find your nipple and bring her tongue toward it. When she finds the right position, she will anchor with her chin, open her mouth wide, attach and begin sucking.
When she finds the right position, she will anchor with her chin, open her mouth wide, attach and begin sucking.
Renee Kam: Straight after a baby is born for the first 1 to 2 hours after they’re born, they’re typically alert and eager and ready to receive their first breastfeed. So when placed into skin-to-skin contact with their mother straight after birth, then that can allow the baby to do baby-led attachment, find the mother’s breasts on their own accord and receive their first breastfeed.
Adele: I did skin-to-skin with all of my children in hospital. So with the baby it probably took a few minutes before like they would kind of just be laying there for a little while and it was a few minutes before they kind of started moving around. But they did the bopping around and choosing a side and finding the nipple and all of that themselves.
Renee Kam: The great news is even if you don’t get to do baby-led attachment straight after a baby is born, babies’ instincts to find a mother’s breasts are easily reproducible for at least the first few months. When a mother and baby are in skin-to-skin contact, there are many benefits of it such as the baby’s heart rate and temperature, blood sugar levels, breathing rate are all kept stable and also when a mother and baby are in skin-to-skin contact it also helps a mother to be able to learn her baby’s feeding cues.
When a mother and baby are in skin-to-skin contact, there are many benefits of it such as the baby’s heart rate and temperature, blood sugar levels, breathing rate are all kept stable and also when a mother and baby are in skin-to-skin contact it also helps a mother to be able to learn her baby’s feeding cues.
Miranda: As with the baby-led attachment, I also did try the mother-led attachment, attachment and feeding and it was quite painful. I went to see a lactation consultant a couple of times for her to help as well. Of course, they have told me to use the baby-led attachment, which was great.
Renee Kam: Even if the mother doesn’t have any breastfeeding problems, by using baby-led attachment frequently, particularly in the early weeks, it can help to reduce the risk of developing any breastfeeding problems such as the baby simply not attaching at all or sore nipples.
Miranda: Persevering with the baby-led attachment actually did help to heal the wounds and I think it was around 3 weeks that we had a happy breastfeeding relationship.
Renee Kam: A mother can do baby-led attachment whenever it’s right for her and her baby to do so. By having done baby-led attachment whenever she feels comfortable to do so, then it means that when she is breastfeeding in public, it makes it easier because baby knows what they’re doing and baby attaches easier to the mum’s breast.
Adele: So I think the baby-led attachment improved my confidence by I was able to see them feeding well, when I could look at them and I could see that they were attached really well and I could hear the swallowing and I knew we were having a good feed and so I didn’t have to really think about what I was doing with them.
Miranda: It helps to know about the fact that everyone is different. With baby-led attachment, it doesn’t matter because babies just go for the breast; they know what to look for.
Renee Kam: Baby-led attachment – it helps a mum and baby get breastfeeding off to a really good start. Then, it may help a mum to be able to breastfeed for as long as she wanted to and reach her own breastfeeding goals.
Then, it may help a mum to be able to breastfeed for as long as she wanted to and reach her own breastfeeding goals.
Breastfeeding: Mini Parenting Master Class
Transcript of 'Breastfeeding: Mini Parenting Master Class' video
"Did you know that your nipples have good bacteria? So you don’t need to wash them before breastfeeding.
My name is Dr. Michele Griswald, and this is my Mini Parenting Master Class on breastfeeding."
Is breastfeeding easy?
"Sometimes mothers get messages that breastfeeding is natural and it’s easy. Sometimes breastfeeding can be easy with the first baby, and hard with the second baby for the same mother. So it really just depends."
Does breastfeeding hurt?
"You shouldn’t stop breastfeeding if your nipples hurt. You should keep breastfeeding but you should get help to see why it’s hurting."
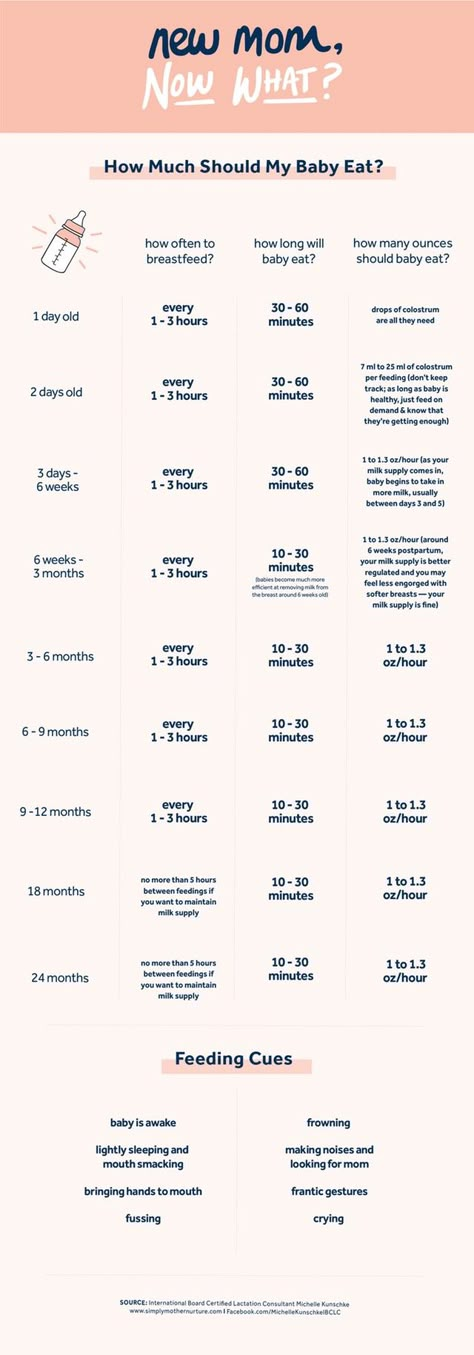
How much should my baby eat?
"They should see signs of hunger about 8 to 12 times in 24 hours. Newborn babies need to eat a lot because they’re growing rapidly. They double their birth weight in the first six months of life, or before. So you can imagine how much you would need to eat if you had to double your weight."
Newborn babies need to eat a lot because they’re growing rapidly. They double their birth weight in the first six months of life, or before. So you can imagine how much you would need to eat if you had to double your weight."
Should I wash my nipples before breastfeeding?
"It’s not necessary to wash your nipples before you breastfeed, because the breasts and the skin around the nipple actually produces good bacteria. And it’s that good bacteria that helps to prevent infections on the mother’s breast."
When should I start breastfeeding?
"The first hour after birth is a very important time for the mother and the baby. Breastfeeding is a very organized, neurological behavior. And so right after birth, keeping them against the mother’s skin can help them to be calm enough to start to seek the breast. And if we do just leave mothers and babies like that after birth, then they will usually start to go towards the breast on their own. Within about 30 minutes to one hour. "
"
What should I eat while breastfeeding?
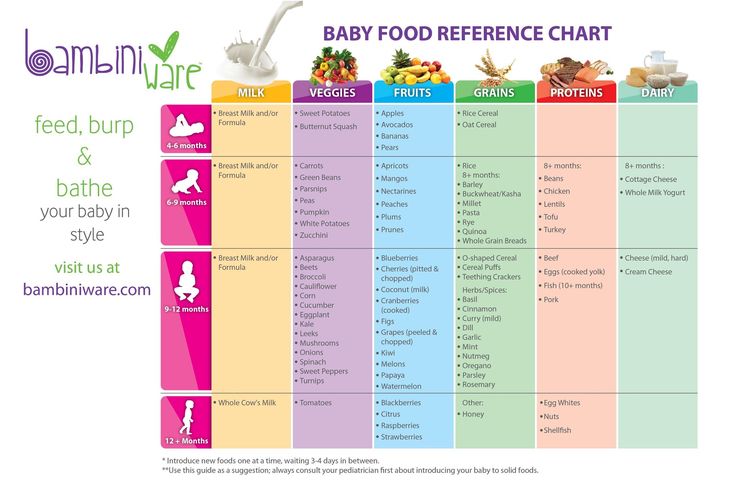
"Most mothers can eat anything they want when they breastfeed. They can follow their normal diet. And the interesting thing is whatever they eat, the babies will taste through their milk and start to get them ready for table foods when they’re about 6 months old."
When should I wean my baby?
"Babies will naturally wean starting around one year of age or so because developmentally, they’re changing so much. They’re becoming less focused on their mother, and more focused on learning about the world around them."
Will I have to wean my baby when I got back to work?
"We would hope that mothers who return to work do not have to wean their babies. Mothers need time and they need support to continue to breastfeed their babies. They need the support of their family, they need the support of their workplace, their employers, they need the support of their entire community.
Breastfeeding not just about food.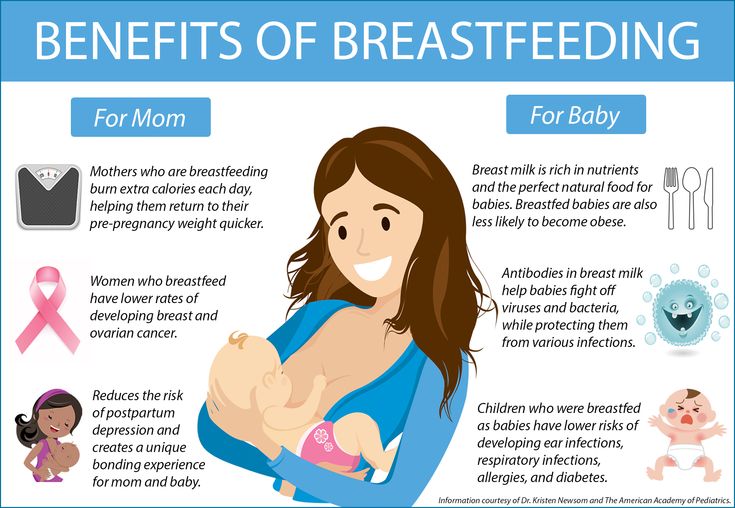 It’s part a nurturing care package that helps children to grow and thrive throughout their entire life."
It’s part a nurturing care package that helps children to grow and thrive throughout their entire life."
UNICEF Mini Parenting Master Class with Dr. Michele Griswold PhD, MPH, RN, IBCLC. Dr Griswold is a lactation consultant, registered nurse, breastfeeding researcher and advocate. She represents the International Lactation Consultant Association to the WHO/UNICEF Global Breastfeeding Collective, which calls on governments and society as a whole to provide mothers the support they need to breastfeed.
Understanding tongue movement in infants
2 min.
Sept. 2021
This resource is for healthcare professionals
Researchers have used video recording for the first time to see differences in tongue movements between breastfed infants and adults when swallowing.
The tongue is an active muscle and a miracle of coordination. When we drink, the tongue prepares for swallowing by collecting liquid in the mouth, taking the shape of a bowl. It then quickly pushes the liquid back where it is swallowed, while still allowing us to continue breathing.
It then quickly pushes the liquid back where it is swallowed, while still allowing us to continue breathing.
When we eat, the tongue works by holding the food in the mouth, moving it with saliva and turning it into a lump, which is then pushed back for swallowing. Both adults and infants use a peristaltic type of movement when swallowing.
Language training before birth
Teaching our tongue to do all this work begins in the womb. Before birth, the tongue begins to work by swallowing the amniotic fluid. After the birth of a child, the tongue plays a key role - it helps to squeeze milk out of the mother's breasts, working in conjunction with the jaws and lips.
When the baby is suckled to the mother's breast, the nipple and areola are retracted into the mouth so that the nipple reaches the junction of the hard and soft palate. After the baby has sucked well, the tongue begins to work, rhythmically squeezing the nipple with peristaltic movements that squeeze the milk from the mammary gland into the back of the throat, where it is swallowed. Babies naturally coordinate sucking, swallowing, and breathing.
Babies naturally coordinate sucking, swallowing, and breathing.
Bottle feeding
This process changes slightly when a baby is bottle fed. The stiffness of the artificial material does not allow the nipple to stretch and take the shape of the baby's mouth. Peristaltic movements of the tongue are difficult and milk can flow almost without effort on the part of the child.
Parents should remember that during breastfeeding, babies make an effort to get milk. When bottle-feeding, milk often flows very easily and babies can drink the same amount of milk much faster (compared to breastfeeding). This may seem like a good way to save time, but as with many other things in life, slower is often better. If you choose a bottle that works more like a breast, with a slower flow, it allows the baby to stop and pause, the baby enjoys comfortable feeding, and the corresponding satiety signals are developed more slowly.
Research task
Usually everything goes smoothly. But from time to time, babies have difficulty swallowing. This may be due to various problems and they are not always easy to learn and understand.
But from time to time, babies have difficulty swallowing. This may be due to various problems and they are not always easy to learn and understand.
At the beginning of the atomic era, diagnostics were carried out with the help of X-ray cinematography (filming of X-ray images). For the first time in history, people could see the amazing internal processes in the mouth and observe how the tongue helps to swallow. When concerns arose about the effects of radiation on technicians and patients, the practice was discontinued. Currently, video recording using ultrasound and MRI is often used. However, even with the use of less invasive methods or technologies, scientists still have to find ways to study babies while breastfeeding that do not affect their actions.
Tongue Movement Study
The 2020 study "Quantifying Tongue Movement During Feeding in Infants and Swallowing in Adults" shows patterns. The scientists used ultrasound video to study tongue movements.
“We observed the most organized and rhythmic tongue movements in exclusively breastfed infants, less mobility in those who had conditions that interfere with normal feeding, such as tongue tie, and more “disorganized” movements with bottle feeding than breastfeeding,” the researchers report. “This highlights the key role of tongue movements in breast or bottle sucking.”
Disorganized movements with bottle feeding than with breastfeeding,” researchers report. “This highlights the key role of tongue movements in breast or bottle sucking.” They could also observe differences in tongue mobility before and after treatment in infants with tongue and lip frenulum. And for the first time, pictures of a baby with torticollis during breastfeeding and bottle feeding were obtained. The results showed "slightly less rhythmic sucking than usual during breastfeeding and irregular sucking during bottle feeding".
Although this study was limited, the use of ultrasound video was effective in obtaining objective information about tongue movements. As more scientists use this technique, we'll get more information about how language works and we'll be able to get more accurate information about natural feeding and how to deal with it.
As more scientists use this technique, we'll get more information about how language works and we'll be able to get more accurate information about natural feeding and how to deal with it.
Share this article:
Similar articles
Are you not a healthcare professional?
References
Genna CW, Saperstein Y, Siegel SA, Laine AF, Elad D. Quantitative imaging of tongue kinematics during infant feeding and adult swallowing reveals highly conserved patterns. Physiol Rep. 2021;9:e14685. doi.org/10.14814/phy2.14685
You are leaving the Philips Healthcare (“Philips”) official website. Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain.
I understand
You are about to visit a Philips global content page
Continue
You are about to visit the Philips USA website.
I understand
Myths about breastfeeding
Ani Gazoyan
medical journalist
Author profile
There are a lot of requirements for new mothers, but they are not always justified.
While breastfeeding, a woman is expected to follow a strict diet, pump regularly, and avoid medication. These and other restrictions greatly complicate the life of a young mother and do not always benefit the child.
This article contains the most popular misconceptions about breastfeeding. We tell you why you should not believe in them.
What myths we checked
- Breasts need to be washed before each feeding
- The baby on breastfeeding should be given water
- It is important to express it after each feeding
- during lactostasis, with breasts 9010 breastfeeding medicines must not be taken
- Cannot get pregnant during lactation
- Breastfeeding during pregnancy increases the risk of miscarriage
See a doctor
Our articles are written with love for evidence-based medicine. We refer to authoritative sources and go to doctors with a good reputation for comments. But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you.
We refer to authoritative sources and go to doctors with a good reputation for comments. But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you.
MYTH No. 1
Breasts should be washed before each feedBreast milk is not sterile by itself. It contains lactic acid bacteria such as B. infantis, L. gasseri and L. fermentum, which form the intestinal microbiota.
Up to 80% of immune cells live in the intestine, so if the microflora is out of balance, the whole organism suffers. And vice versa, "tincture" of beneficial bacteria strengthens the immune system - and the child does not need additional protection measures. Breast milk also contains nucleotides, antibodies, immune complexes, active leukocytes, macrophages and other biologically active substances. They are involved in the formation of the child's immune system.
The role of the microbiota in immunity and inflammation - National Institutes of Health
Breastfeeding: composition and properties of breast milk - Cyberleninka
In addition, the newborn may want to eat every 1-3 hours. As the baby gets older, the breastfed baby drinks more milk and the interval between feedings gradually increases. However, in the first months of life, a child needs to be fed 8-12 times daily, and sometimes up to 20 times.
As the baby gets older, the breastfed baby drinks more milk and the interval between feedings gradually increases. However, in the first months of life, a child needs to be fed 8-12 times daily, and sometimes up to 20 times.
How much and how often to breastfeed - CDC
Washing the breasts and nipples before each feeding will cause dryness and irritation of the skin. At the same time, there is no benefit in frequent washing of the mother's breast for the child. It is enough to wash the chest twice a day during the shower. If you treat your nipples with anti-crack cream or ointment, check the instructions for use to see if you need to rinse off the product before feeding.
MYTH No. 2
A breastfed child should be given water While the child is exclusively breastfed, without complementary foods, it is not necessary to supplement him with water. The composition of milk varies depending on the needs of the child. How this happens is not yet clear, but scientists suggest that a woman’s body “reads” the signals of the baby during feeding, “adjusts” milk to his needs, and even in the heat, a breast-fed baby does not need additional liquid. Moreover, supplementation can be harmful: water will fill the child's stomach, the child will drink less milk and it will be worse to gain weight.
Moreover, supplementation can be harmful: water will fill the child's stomach, the child will drink less milk and it will be worse to gain weight.
But a mother, in order to avoid dehydration, needs to monitor her drinking regime, because her body turns part of the liquid into breast milk. There is no need to calculate a certain rate of drinking, it is enough to drink when you want. If you notice that your urine has become dark in color, urination has become rare, dry mouth has appeared, then you do not have enough fluid.
Patient Education: Health and Nutrition During Breastfeeding - UpToDate
MYTH No. 3
It is important to pump after each feed The Academy of Breastfeeding Medicine recommends avoiding unnecessary pumping. The fact is that breast milk contains a feedback lactation inhibitor that controls milk production. In order for milk to begin to be produced, you need to empty your chest, and the more often and more carefully you do this, the more milk comes.
How Breast Milk Production Works - La Leche League GB
Treatment of Hyperlactation - Clinical Protocol of the Academy of Breastfeeding Medicine No. 32
Due to frequent pumping, hyperlactation can occur - when more milk is produced than the baby needs. Hyperlactation often leads to stagnation of milk - lactostasis - and inflammation of the mammary gland - mastitis.
Milk does not need to be expressed when feeding on demand, not by the clock. If you feed a child when he is hungry, the amount of milk will correspond to the needs and appetite of the baby: the more milk he sucks, the more it is produced for the next feeding. However, if after feeding you feel that the breast is not completely emptied, and this gives you discomfort, you can express milk a little - until you feel relief.
/pluggedduct/
How I survived 10 lactose and 2 mastitis but kept breastfeeding
Pumping may be necessary, for example, if the baby was specifically woken up to feed. A sleepy baby will suckle sluggishly at the breast and eat less. In response to this, the mother's body will produce less milk for the next feeding - and the child will not eat enough. In this case, pumping after the first feeding will help to avoid a shortage of milk in the future.
A sleepy baby will suckle sluggishly at the breast and eat less. In response to this, the mother's body will produce less milk for the next feeding - and the child will not eat enough. In this case, pumping after the first feeding will help to avoid a shortage of milk in the future.
MYTH No. 4
With lactostasis, you can not breastfeedLaktostasis occurs when the breast is not completely emptied: part of the milk remains in the ducts of the mammary gland and forms stagnation. This is a painful condition, but the quality of milk in the breast does not change with lactostasis, and feeding is not dangerous for the baby - you can breastfeed him as usual.
Moreover, breastfeeding will speed up recovery, because the main treatment for lactostasis is to empty the breast. If feeding during lactostasis is very painful or the child has eaten without having time to eliminate the stagnation, you can additionally express with your hands or with the help of a breast pump until the condition improves.
MYTH No. 5
A woman must follow a strict dietHighly allergenic foods such as seafood, nuts, red berries and citrus fruits should be avoided while breastfeeding. However, there is no evidence that following a hypoallergenic diet by a pregnant or breastfeeding woman will prevent the development of allergies in a child. Moreover, babies whose mothers eat a balanced and varied diet are less likely to suffer from food allergies.
Rarely, a baby may be allergic to cow's milk or soy. It can be indicated by vomiting, diarrhea, and blood in the stool. If these symptoms appear, you should contact your pediatrician: he may recommend that these foods be excluded from the woman's diet until she finishes breastfeeding.
Many women gain weight during pregnancy and want to lose weight as soon as possible after giving birth. Even if a young mother is on a strict diet and loses weight quickly, lactation will most likely not be affected. Under conditions of negative energy balance, the concentration of prolactin, the hormone that is responsible for the production of breast milk, increases, protecting the baby from milk deficiency.
But mom will definitely lack energy, macronutrients, vitamins and microelements to feel good and stay healthy. Therefore, during breastfeeding, it is recommended to eat 300-400 kcal more than usual. At the same time, the diet should be balanced and include:
Community 06/22/21
How to eat properly while breastfeeding?
- Protein found in lean meats, dairy, fish, seafood, and legumes.
- Healthy fats, such as those from unrefined oils and nuts.
- Complex carbohydrates found in berries and fruits, vegetables, whole grains, and pasta.
Occasionally, a woman who is breastfeeding can drink one serving of a low-alcohol drink, such as 350 ml of beer or 150 ml of wine. The main thing is to wait at least two hours before breastfeeding in order to completely avoid getting alcohol into the baby's body. If a woman drank more, she should refrain from breastfeeding for an additional two hours for each serving of alcohol. There is no need to express yourself.
There is no need to express yourself.
MYTH No. 6
Medicines must not be taken while breastfeedingMany medicines are labeled not to be taken while breastfeeding. Often this ban is due to the fact that pregnant and breastfeeding women do not participate in most clinical drug trials. It is unprofitable for manufacturers to include them in studies and register the drug as safe during breastfeeding. Pharmaceutical companies simply do not know how a particular drug will affect this category of patients, and do not recommend it in order to play it safe.
The active ingredients of medicines can pass into breast milk, causing adverse effects, poisoning or an allergic reaction in the baby, but more often their concentration is too low and does not harm. At the same time, even within the same pharmacological group there are drugs with low and high risk. For example, among antipyretic drugs, paracetamol is safe during lactation, the risks are slightly higher when taking aspirin, but it is better to refuse propyphenazone.
Breastfeeding and drugs: what is safe? - Mayo Clinic
To check if a specific drug or active ingredient is compatible with breastfeeding, visit e-lactacia.org or the LactMed knowledge base. It is better to do this together with your doctor: he will tell you if it is possible to replace the drug with analogues.
If a woman still needs to take medications that are incompatible with lactation, it is recommended to stop breastfeeding for the duration of treatment and pump so that the milk does not disappear completely. When the drug needs to be taken constantly, breastfeeding is stopped.
MYTH No. 7
It is impossible to get pregnant during lactation Indeed, for some time, lactating women cannot become pregnant. This happens because the hormone prolactin, necessary for lactation, blocks ovulation. But over time, when feedings become less frequent, complementary foods are added, the intervals between feedings are lengthened, the menstrual cycle is restored - and a woman can become pregnant again.
The menstrual cycle can be restored at any time: a month after the baby is born, and two years later, when the woman stopped breastfeeding. In most women, menstruation resumes after 9-18 months postpartum. In addition, ovulation occurs before menstruation and a woman can become pregnant without knowing that her reproductive function has already recovered.
If a woman is not planning a pregnancy, contraception must be used during the entire period of breastfeeding. Here are some contraceptives that are allowed for breastfeeding women and do not affect the composition of breast milk:
- Condoms.
- Diaphragms and intrauterine devices.
- Certain birth control pills: Doctors usually recommend progestin-only pills.
MYTH No. 8
Breastfeeding during pregnancy increases the risk of miscarriage This myth is prevalent because a woman's body releases the hormone oxytocin during breastfeeding. It causes the uterus to contract, and it seems that feeding can lead to miscarriage or preterm labor.