Baby milk protein allergy foods to avoid
Milk Allergy Diet | Johns Hopkins Medicine
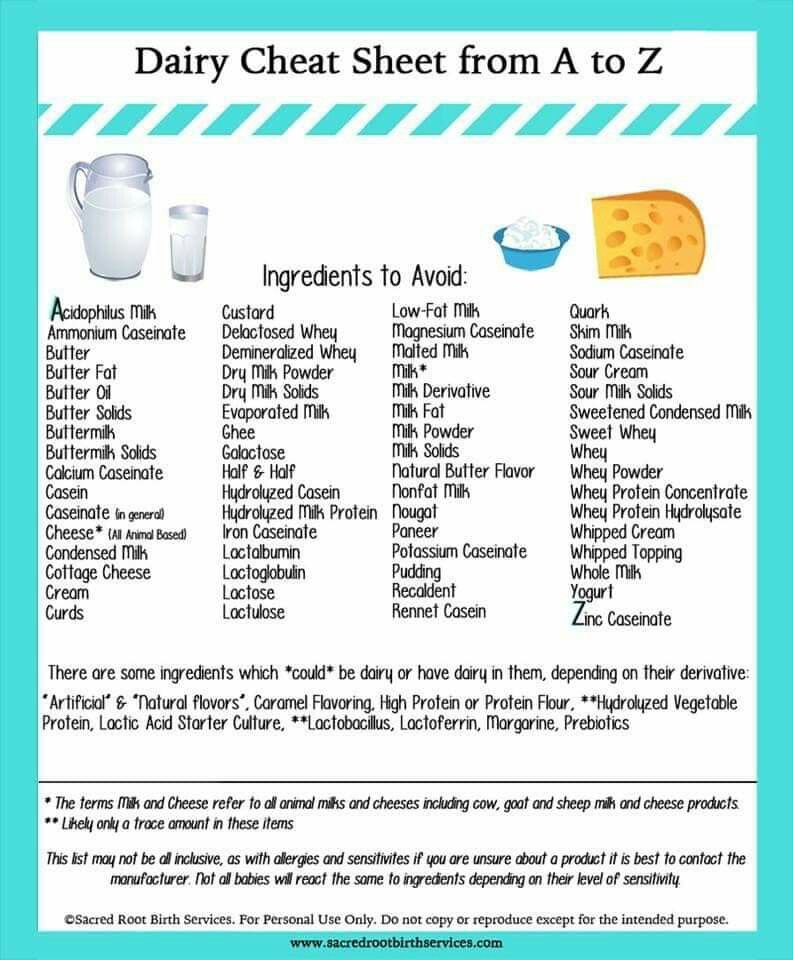
The key to an allergy-free diet is to avoid foods or products containing the food to which you are allergic. The items that you are allergic to are called allergens. Milk allergy is most common among infants and young children. Obvious forms of milk are cream, cheese, butter, ice cream, and yogurt. Milk and milk products may also be used as ingredients in many other foods. To avoid foods that contain milk and milk products, it is necessary to read food labels.
| Foods | Allowed | Not allowed |
|---|---|---|
| Beverages |
|
|
| Breads |
|
|
| Cereals |
|
|
| Desserts |
|
|
| Eggs |
|
|
| Fats |
|
|
| Fruits |
|
|
| Meats, fish, poultry, and cheese |
|
|
| Potatoes |
|
|
| Soups |
|
|
| Sweets |
|
|
| Vegetables |
|
|
| Miscellaneous |
|
|
Artificial butter flavor
Butter, butter fat, butter oil
Casein, casein hydrolysates
Caseinates (ammonium, calcium, magnesium, potassium, sodium)
Cheese, cottage cheese
Cream
Custard, pudding
Ghee
Half and Half
Hydrolysates (casein, milk protein, protein, whey, whey protein)
Lactalbumin, lactalbumin phosphate
Lactoglobulin, lactoferrin
Lactose, lactulose
Milk
-
Derivative, protein, solids, malted, condensed, evaporated, or dry
-
Whole, low-fat, nonfat, skim
-
Goat's milk and milk from other animals
Nisin
Nougat
Recaldent
Rennet casein
Sour cream or sour cream solids
Whey (delactosed, demineralized, protein concentrate)
Yogurt
Cow’s Milk Alternatives: Parent FAQs
By: Anthony Porto, MD, MPH, FAAP & Rachel Drake, MS, RD, CSO, CSP, CDN
Milk is a grocery list staple for many families. But some avoid it because of milk protein allergies or other health concerns. Some kids simply don't like the taste. These families may choose from a growing array of cow's milk alternatives that now fill the dairy aisle.
But some avoid it because of milk protein allergies or other health concerns. Some kids simply don't like the taste. These families may choose from a growing array of cow's milk alternatives that now fill the dairy aisle.
The nutritional content in the various dairy alternative products is important for parents to be aware of when shopping. Choices range from other animal-based beverages (such as goat's milk) to products made from nuts (such as almond milk), beans (such as soy milk), grains (such as oat) and other plants.
The American Academy of Pediatrics (AAP) knows that deciding what's best for your family can be confusing. To help you sort it all out, here are frequently asked questions from parents about cow's milk alternatives.
When do I introduce cow's milk into my baby's diet?
The AAP recommends
breast milk as the sole source of nutrition for your baby for about the first 6 months. If a baby is breastfed by a mother who is drinking cow's milk, or is formula fed with traditional infant formula, they have already been exposed to cow's milk protein. Most babies can begin consuming dairy foods around 6 months of age—after a few first
solid foods have been introduced. Plain, whole-fat or whole Greek yogurt is a good first form of cow's milk protein for babies to try. Avoid the added sugar commonly found in yogurt marketed to babies and toddlers.
If a baby is breastfed by a mother who is drinking cow's milk, or is formula fed with traditional infant formula, they have already been exposed to cow's milk protein. Most babies can begin consuming dairy foods around 6 months of age—after a few first
solid foods have been introduced. Plain, whole-fat or whole Greek yogurt is a good first form of cow's milk protein for babies to try. Avoid the added sugar commonly found in yogurt marketed to babies and toddlers.
Once a baby is developmentally able to eat finger foods, other dairy—such as pieces of cheese—can be added. The AAP recommends that whole cow's milk and low-iron formulas not be used during the first year of life, because babies' digestive systems under age one year old may not tolerate the cow's milk protein in large quantities. Low-iron formulas can also lead to anemia. Note: Low-iron formulas are no longer marketed routinely in the United States.
What if my baby is allergic to cow's milk?
If your formula-fed baby has a cow's milk allergy, ask your pediatrician about switching to a non-cow's milk, protein-based formula. Hypoallergenic formulas are cow's milk based; only soy formulas are not. Discuss these options with your child's pediatrician before switching.
Hypoallergenic formulas are cow's milk based; only soy formulas are not. Discuss these options with your child's pediatrician before switching.
According to a study published in Pediatrics, there is not enough evidence for breastfeeding mothers to routinely avoid allergenic foods—like cow's milk—while breastfeeding.
If your pediatrician diagnoses your baby with a cow's milk protein allergy, then they may recommend you remove cow's milk from your diet while breastfeeding. Be aware that it can take several weeks for the milk protein to disappear entirely. The AAP does not currently have an official recommendation on this issue.
After your baby's first birthday, they may begin using cow's milk alternatives or occasionally change to a toddler version of the formulas mentioned above. Many infants diagnosed with allergic colitis caused by cow's milk protein, including healthy babies with rectal bleeding, may safely begin cow's milk at a year or so of age.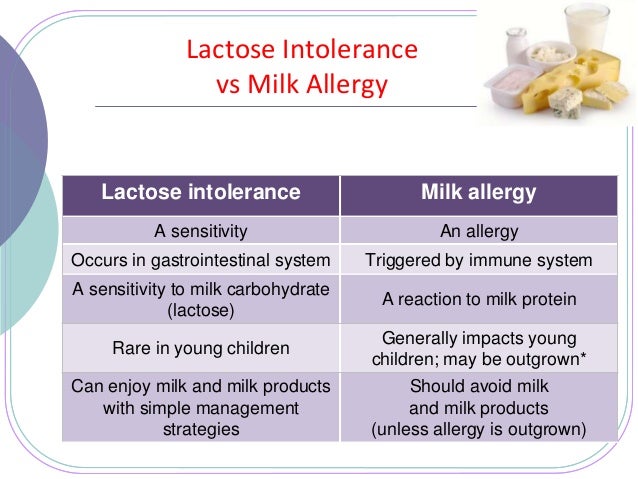 Your pediatrician can help you make this decision.
Your pediatrician can help you make this decision.
What kinds of cow's milk alternatives are available?
While soy milk has traditionally been the most commonly used cow's milk alternative, there are many options available. In addition, soy protein should also be avoided if your child is diagnosed with an allergy to cow's milk protein. This is because 50% of infants with cow's milk protein allergy may also have cross reactivity with the soy protein.
Use of tree nut milk, including almond and cashew milks, have become increasingly popular. Rice and oat milk, as well as hemp milk, are also possible alternatives. Some of these alternatives are flavored, for example with chocolate and vanilla. Keep in mind that these often contain added sugar and calories. It is best to avoid sugar-sweetened beverages for children under 2 years of age, and also limit them for older children as much as possible.
What are the differences among cow's milk alternatives?
Cow's milk alternatives often contain less protein and less calories in comparison to cow's milk. Most are fortified with vitamin D and calcium. It is important to
check labels since protein and vitamin content may differ among brands.
See the chart for a comparison of common unflavored milk alternatives.
Most are fortified with vitamin D and calcium. It is important to
check labels since protein and vitamin content may differ among brands.
See the chart for a comparison of common unflavored milk alternatives.
Comparison of common unflavored milk alternatives | ||||||||
|
Whole Milk (1 cup) |
Rice Milk (1 cup) |
Soy Milk (1 cup) |
Coconut Milk (1 cup) |
Almond Milk (1 cup) |
Oat Milk (1 cup) |
Hemp Milk (1 cup) | Pea Milk (1 cup) | |
Energy (kcal) | 149 | 115 | 105 | 76 | 37 | 130 | 70 | 80 |
Protein (g) | 7. | 0.68 | 6.34 | 0.51 | 1.44 | 4 | 3 | 8 |
Total fat (g) | 7.93 | 2.37 | 3.59 | 5.08 | 2.68 | 2.5 | 5 | 4.5 |
Saturated fat (g) | 4.55 | 0 | 0.5 | 5.083 | 0 | 0 | 0.5 | 0.5 |
Cholesterol (mg) | 24 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
Carbohydrate (g) | 11. | 22.37 | 12 | 7.12 | 1.42 | 24 | 1 | < 1 |
Calcium (mg) | 276 | 288 | 300 | 459 | 481 | 350 | 300 | 440 |
Iron (mg) | 0.07 | 0.49 | 1.02 | 0.73 | 0.85 | 1.8 | 1.8 | 0 |
Vitamin D (IU) | 128 | 96 | 108 | 96 | 96 | 100 | 100 | 110 |
Note: Homemade almond milk or other homemade milk alternatives do not contain the same number of vitamins, because they are not fortified. | ||||||||
How much dairy is recommended for my child?
Infants' diets primarily consist of dairy to help them meet their caloric needs for growth. In addition, dairy provides enough fat needed for brain and eye development.
At one year, babies should consume approximately 2 servings of dairy per day, or about 16 to a maximum of 24 ounces of whole milk per day. Whole-fat milk is recommended for children at this age, unless there is a family history or risk for obesity or heart disease. Talk with your child's pediatrician about which milk they recommend for your one-year-old child.
Between two and three years old, children should consume 2.5 servings of dairy per day. The AAP recommends that children stay on whole milk until they are two years of age—unless there is a reason to switch to low-fat milk sooner. Whole milk contains approximately 4% milk fat. It may help to gradually switch your child from whole milk to a lower-fat milk.
 Therefore, many pediatricians recommend that children get reduced fat (2%) milk for a few weeks before switching them to low fat (1%) or no fat (skim) milk. If your child cannot drink cow's milk, they can meet their dairy requirements by eating yogurt and cheese. However, they may need a vitamin D supplement since not all yogurts are fully supplemented with vitamin D. Talk with your child pediatrician before giving your child any supplements.
Therefore, many pediatricians recommend that children get reduced fat (2%) milk for a few weeks before switching them to low fat (1%) or no fat (skim) milk. If your child cannot drink cow's milk, they can meet their dairy requirements by eating yogurt and cheese. However, they may need a vitamin D supplement since not all yogurts are fully supplemented with vitamin D. Talk with your child pediatrician before giving your child any supplements.
How much calcium and vitamin D are recommended for my child to eat each day?
The specific amount is based on your child's age. Here is a breakdown of the recommended dietary allowances (RDA) for calcium and
vitamin D.
Recommended Dietary Allowances for Calcium and Vitamin D | ||
| Age |
Amount of Calcium Per Day |
Amount of Vitamin D Per Day |
0 to 6 months | 200 mg | 400 IU |
7 to 12 months | 260 mg | 400 IU |
1 to 3 years | 700 mg | 600 IU |
4 to 8 years | 1000 mg | 600 IU |
9 to 18 year | 1300 mg | 600 IU |
More information
-
Infant Allergies and Food Sensitivities
- Why Formula Instead of Cow's Milk?
- Where We Stand: Soy Formulas
- Choosing a Formula
- Lactose Intolerance in Infants & Children: Parent FAQs
- Ask the Pediatrician:
My preschooler refuses to drink milk.
 What should we do?
What should we do? - The Use of Soy Protein-Based Formulas in Infant Feeding (AAP Policy Statement)
About Dr. Porto:
Anthony Porto, MD, MPH, FAAP is a board-certified pediatrician and board-certified pediatric gastroenterologist. He is an Associate Professor of Pediatrics and Associate Clinical Chief of Pediatric Gastroenterology at Yale University and Director, Pediatric Gastroenterology at Greenwich Hospital in Greenwich, CT. He is also the medical director of the Yale Pediatric Celiac Program. Within the American Academy of Pediatrics, Dr. Porto sits on the PREP Gastroenterology Advisory Board and is a member of the Section on Gastroenterology, Hepatology and Nutrition. He is also a member of the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition's Public Education Committee, a pediatric expert on nutrition for The Bump's
Real Answers, and is the co-author of
The Pediatrician's Guide to Feeding Babies and Toddlers. |
About Ms. Drake:Rachel Drake, MS, RD, CSO, CSP, CDN is a is a registered dietitian-nutritionist practicing in Connecticut. She is a board-certified specialist in pediatric nutrition through the Academy of Nutrition and Dietetics and the former Chair of the Failure to Thrive, Gastroenterology & Allergy specialty group within the
Pediatric Nutrition Practice Group of the Academy of Nutrition and Dietetics. In 2015, Ms. Drake was honored by the Academy of Nutrition and Dietetics as the
Recognized Young Dietitian of the Year for the state of Connecticut. She lives in Connecticut with her husband and young daughter. |
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Diet for milk allergy
Cow's milk and products containing it are excluded from the diet. Although cow's milk and goat's milk are similar in antigenic composition, some patients with cow's milk allergy tolerate goat's milk. In order to avoid the use of ready-made products containing cow's milk, you should always study their composition on the packaging.
Some products containing milk:
- Skimmed milk powder
- Powdered milk
- Oil
- Whey
- Curd
- Lactose
- Margarine
- Casein
- Casein hydrolyzate
- Ice cream
- Cheese
Since the composition of any product is subject to change, it is necessary to study the packaging even of previously consumed products.
Dishes excluded from the diet:
1. Soups - Puree soups and other soups based on or containing milk.
2. High protein foods - Cheese, cottage cheese, sausages (e.g. sausages, smoked sausage) containing milk and milk components, beef, fish, poultry (breaded or with white sauce), egg dishes with the addition of dairy products.
3. Potatoes and other side dishes - Any food containing milk and its components (eg mashed potatoes, macaroni and cheese).
4. Vegetables - Any vegetable products with the addition of milk and its components (for example spinach puree).
5. Bakery products - Any bakery products with the addition of milk and its components:
- donuts
- pancakes
- pancakes
- wafers
- dry biscuits
- biscuit rolls
- biscuits
6. Cereal dishes — Dishes prepared with milk, prepared foods with the addition of milk or its components.
Cereal dishes — Dishes prepared with milk, prepared foods with the addition of milk or its components.
7. Fats - Butter, cream, salad dressings, mayonnaise and margarine containing milk or milk components.
8. Sweet dishes — Any sweet dishes containing milk or its components, ready-made pies, cakes, biscuits, puddings, ice cream, sherbets, yoghurts, dry mixes.
9. Milk Whole cow's milk, skimmed milk, skimmed milk powder, sweetened or unsweetened condensed milk, yoghurt, cow's milk infant formula, cocoa with milk.
10. Beverages — Beverages with added milk:
- cocoa
- milkshakes
- alcoholic drinks with cream
11. Other products — Milk chocolate, cream sauce, whey, cottage cheese, products fried in butter, fried in breadcrumbs, cheese, dough, low quality chocolate.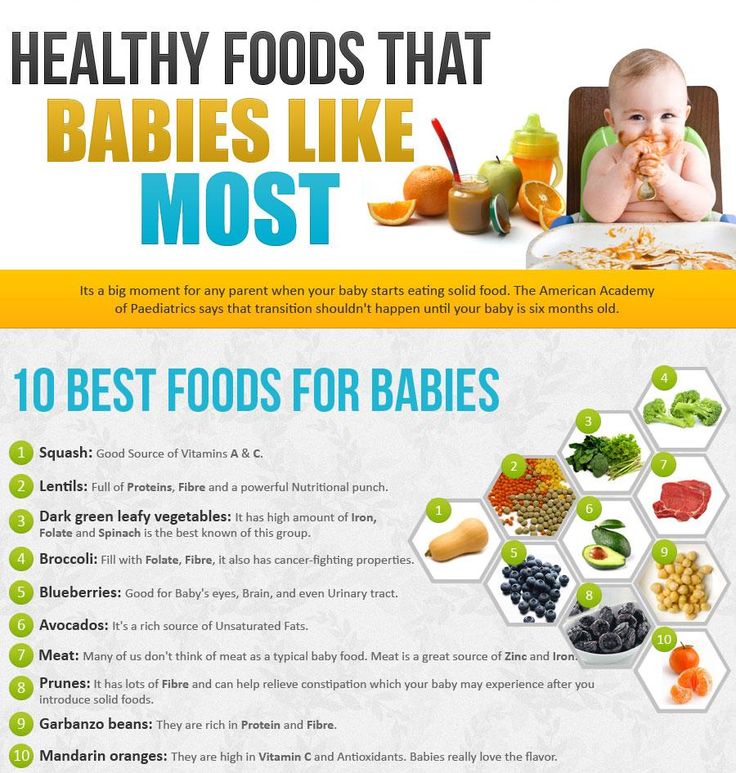 ⠀
⠀
Features of food allergy to milk and egg
It is not the whole product (milk, egg, chicken, etc.) that is responsible for the development of an allergic reaction, but the individual proteins that make up its composition. Some proteins are destroyed by heating or fermentation and lose their allergenic properties, so sometimes the cooked product becomes safe for an allergic person.
If, having learned that you are allergic to some products (milk, eggs, chicken, etc.), you immediately decided that everything that contains this product is impossible for you, then we recommend that you contact an allergist again and draw up the optimal plan for diagnosing at the molecular level of previously identified allergic reactions to food and other allergens. Perhaps this will allow you to significantly enrich your diet with foods that are safe for you, which you previously avoided for fear of an allergic reaction.
Milk allergy
There are over 40 different proteins in milk, and each of them contributes to allergies. In general, allergenic proteins come in two fractions - caseins (80% of milk proteins, insoluble, form clots - "curdle") and whey proteins (20%, soluble in whey).
In general, allergenic proteins come in two fractions - caseins (80% of milk proteins, insoluble, form clots - "curdle") and whey proteins (20%, soluble in whey).
The most important allergen in milk is casein . The casein fraction (allergen Bos d 8) consists of four types of caseins: alpha-S1-caseins (Bos d 9), alpha-S2-caseins (Bos d 10), beta-caseins (Bos d 11) and kappa-caseins (Bos d 12).
Being a thermostable protein, it is able to cause a reaction in sensitized patients when consuming products, both raw and cooked, thermally processed. If you are allergic to this particular protein, all dairy and sour-milk products are excluded from the diet. If you are allergic to Casein, absolutely all milk-containing products must be excluded from the diet, including pastries, ice cream, some sauces, etc. Casein and caseinates are used as fillers for sausages, long loaves, soups and stews.
If it is caseins that cause an allergic reaction, then milk and products containing it will have to be completely excluded.
The remaining components of milk (alpha-lactalbumin, beta-lactoglobulin, whey proteins) lose their allergenic properties during frying / boiling / baking, etc.
Alpha-lactalbumin (Bos d 4, α-lactalbumin) is approximately 25% whey and 5% cow's milk proteins. It is a calcium-binding protein involved in the synthesis of lactose in the mammary glands and in the formation of immunity. It is important that the protein is thermolabile, that is, during heat treatment it loses its allergenic properties. Cross-reactivity between bovine protein and protein from other animals is quite possible, but scientists have not yet been able to fully answer this question.
Beta-lactoglobulin (b-lactoglobulin) in whey is twice as much as α-lactalbumin. However, in human milk it is not at all, even analogues. But this protein can cause cross-reactions with milk proteins of mice / rats, cats, dogs, horses. Fortunately, this protein is also thermolabile and loses its allergenic properties already at 90*C. Another great news is the fact that in yoghurts and other fermented milk products, under the action of fermentation, b-lactoglobulin also loses its allergenic properties and becomes safe.
Another great news is the fact that in yoghurts and other fermented milk products, under the action of fermentation, b-lactoglobulin also loses its allergenic properties and becomes safe.
Bovine serum albumin (Bos d 6, BSA) is the main protein in cow's milk, which is found not only in milk, but also in beef, cow plasma. Fortunately, the protein is thermolabile. It is a minor cow's milk allergen that is physically and immunologically very similar to human serum albumin. It carries small molecules and protects against free radicals. When heated, this allergen is destroyed. BSA is used in cosmetology (as an additive in anti-wrinkle creams) and even as a nutrient medium for cells in the field of artificial insemination.
component diagnostics of milk allergy ImmunoCap (ImmunoCAP) will allow you to check which of the dairy products you can. The study makes it possible to differentiate sensitization to thermostable and thermolabile fractions of milk proteins and to resolve the issue of the possibility of eating some dairy and sour-milk products by patients with milk allergy.
Book an appointment with an allergist
Egg allergy
The cause of an allergic reaction to an egg can be not only the eggs themselves in raw or cooked form, but also products that contain eggs:
- bread, biscuits, cakes and other baked goods,
- desserts: cakes and cakes with cream, marshmallows, ice cream,
- mayonnaises, sauces and salad dressings,
- ready-made soups and drinks,
- semi-finished products, e.g. sausages,
- chick embryo vaccines,
- contact lens cleaning fluids.
Egg white contains the main allergens of a chicken egg - ovalbumin (44% of all protein proteins), ovomucoid (11%), ovotransferrin (12%), ovomucin (3.5%) and lysozyme (3.4%). Despite the prevailing concentration of ovalbumin, ovotransferrin and ovomucoid are considered more allergenic. The pronounced allergenic properties of ovomucoid are associated with the resistance of the protein to heat treatment, the effects of digestive tract enzymes.
Allergen ovalbumin Gald2 - ovalbumin is one of the main (major) allergens of chicken protein. Its content in the egg is 5 times higher than the amount of ovomucoid. Previously, ovalbumin was considered the most significant chicken protein allergen until the more allergenic properties of ovomucoid were discovered. Although ovalbumin is a thermostable protein, its allergenicity is reduced by heat treatment. Ovalbumin molecules are able to cross the placenta and into breast milk and interact with the cells of the child's immune system, and the concentration of protein in milk depends on the number of eggs eaten. It is assumed that during feeding, egg white proteins can cause sensitization of an infant, since the digestive system and enzyme activity in the child's body are not sufficiently developed.
Allergen Gald3 (conalbumin, or ovotransferrin) is present in egg white, yolk and plasma and shares a gene with chicken serum transferrin, but only partial cross-reactivity of these proteins has been noted.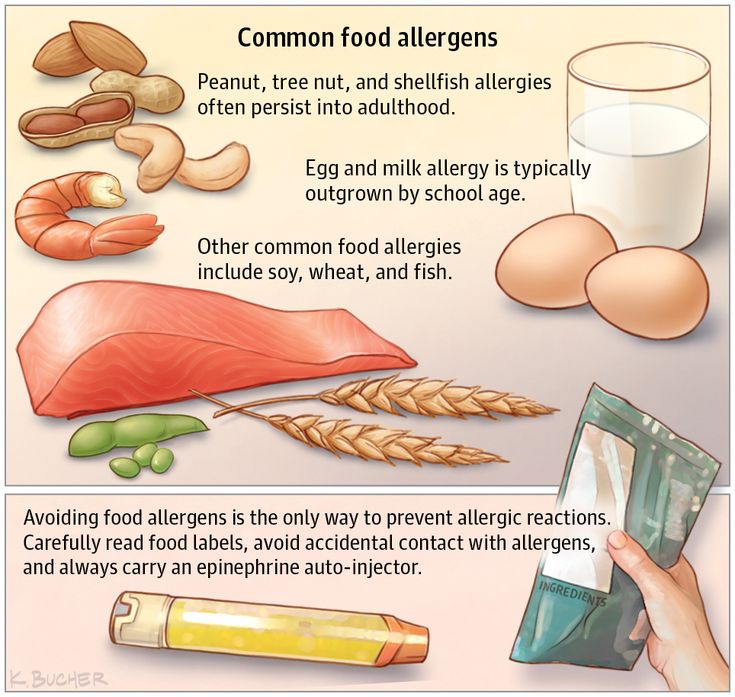 The physiological significance of conalbumin is associated with the binding and transport of iron. It belongs to thermolabile proteins, its allergenic properties are reduced by heat treatment and under the influence of digestive enzymes.
The physiological significance of conalbumin is associated with the binding and transport of iron. It belongs to thermolabile proteins, its allergenic properties are reduced by heat treatment and under the influence of digestive enzymes.
Allergen lysozyme Gal d4 refers to globular peptides distributed in various tissues and organs of animals. It has antibacterial properties and is present in serum, saliva and other secretions, and its structure differs in different species of living organisms. Lysozyme is used in the food industry as a food additive E1105, a biological catalyst in the production of hard cheeses, as a preservative in the pharmaceutical industry, it is also part of medicines for the treatment of respiratory diseases and is used as a local antiseptic. Mostly, lysozyme is biotechnologically obtained from the protein of chicken eggs.
People sensitized to chicken protein lysozyme should pay attention to the composition and avoid the use of foods and drugs in which this allergenic protein may be added.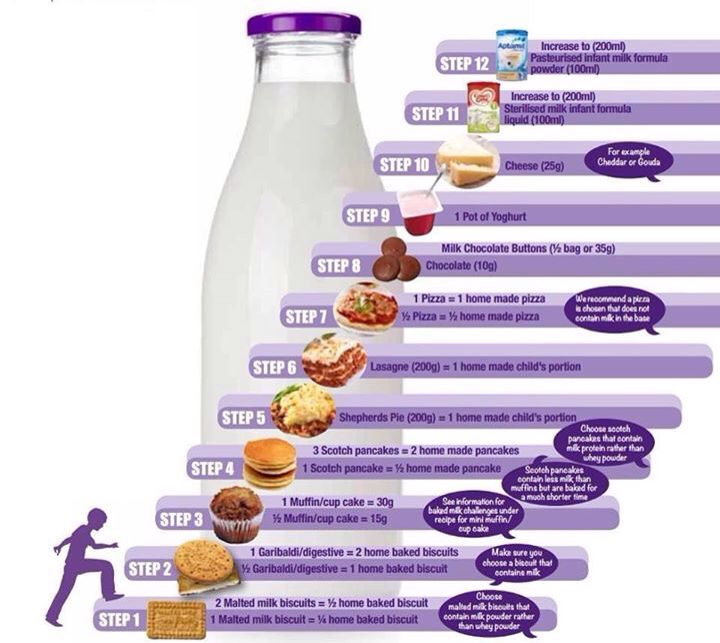

 69
69 71
71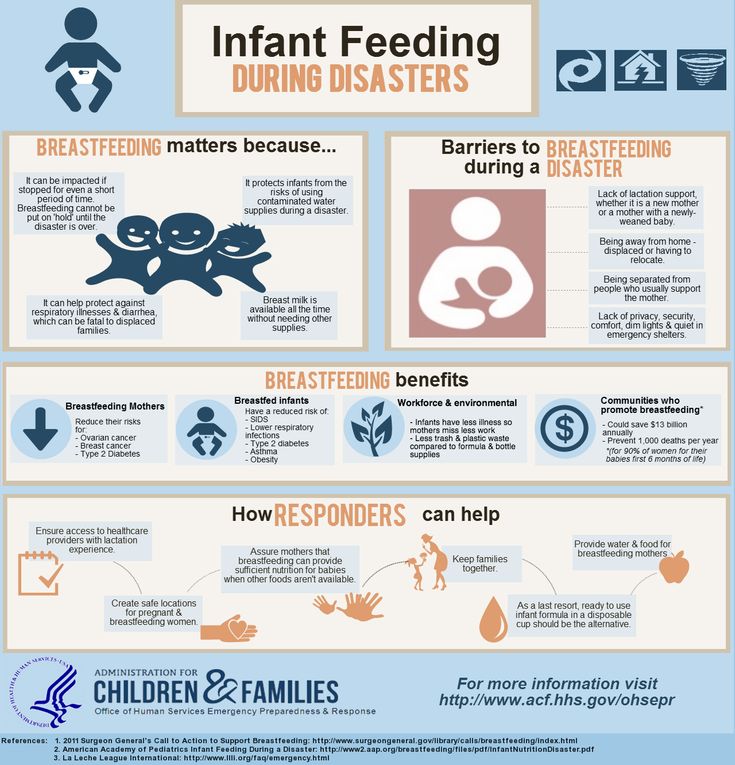
 Follow him on Instagram
@Pediatriciansguide.
Follow him on Instagram
@Pediatriciansguide.