Baby nystagmus when feeding
Nystagmus in Babies - All About Vision
By Anna Barden; reviewed by Gary Heiting, OD
Babies move their eyes to follow objects such as toys and people around them — this is a normal part of the vision development in an infant. However, if your child’s eyes appear to be moving at a constant, erratic rate, it could be an indicator of something else: nystagmus.
Nystagmus in infants is estimated to occur in one in 5,000 births, and is typically onset between 6 weeks and 6 months of age, although the condition can also develop later in babyhood and childhood, due to other causes, including trauma, cataracts and more.
There are two main classifications of infantile nystagmus: congenital (present at birth or occurring within 6 months of age) and acquired (occurring at age 6 months or older). Depending on individual development, each type may appear and/or be treated differently.
Types of infantile nystagmus
Infants with this condition typically experience one of two main types of nystagmus: jerk nystagmus (eyes quickly move in one direction, followed by slow movement in the opposite direction) or pendular nystagmus (eyes move at equal velocity in each direction).
There are two “types” of congenital nystagmus: nystagmus with abnormal vision and nystagmus with normal vision. There is one main category for acquired infantile nystagmus, though it can occur for a variety of reasons.
Congenital sensory nystagmus
Congenital sensory nystagmus occurs when the child has abnormal vision, due to something interfering with visual information reaching the brain. This is called an afferent sensory defect because it involves incoming sensory (in this case, visual) information on its way to the brain.
Causes include congenital cataracts, problems with the retina or optic nerve, and severe refractive errors.
Congenital sensory nystagmus usually occurs at around 2 to 3 months of age and continues throughout life, according to the American Academy of Pediatric Ophthalmology and Strabismus (AAPOS).
Congenital motor nystagmus
Congenital motor nystagmus is more common than congenital sensory nystagmus, says AAPOS. Infants with congenital motor nystagmus have no underlying conditions and experience basically normal vision, but the brain lacks steady control or “motor” skills when it comes to eye movement.
Infants with congenital motor nystagmus have no underlying conditions and experience basically normal vision, but the brain lacks steady control or “motor” skills when it comes to eye movement.
If a child shows general symptoms of nystagmus in their first few months of development, they should be medically evaluated to determine the reason.
If medical testing rules out the underlying conditions associated with congenital sensory nystagmus, and the brain and vision system prove to be otherwise healthy, it can then be determined that the child has congenital motor nystagmus.
Acquired infantile nystagmus
Acquired nystagmus in babies occurs at least several months after birth, with some cases occurring as early as 6 months old. There are a number of causes for acquired infantile nystagmus, from eye and head trauma to brain abnormalities and even reactions to certain medications.
The most efficient way to determine the underlying cause of acquired infantile nystagmus is through medical testing, including bloodwork and/or an MRI scan.
Symptoms of infantile nystagmus
What does nystagmus look like in babies? The primary symptom that could indicate nystagmus in an infant is jerky or random eye movement.
It’s important to note that the frequency and intensity of these movements can vary in each individual infant, and movements are typically absent when the infant is asleep.
In addition to constantly moving or jerking eyes, some key symptoms of infantile nystagmus can include:
Holding the head in a tilted position
Sensitivity to light
Trouble using the eyes to follow an object
Some nystagmus symptoms may not appear until several months into childhood development. If symptoms occur after infancy, it could be the result of an underlying condition.
Causes of infantile nystagmus
Nystagmus in infants can be congenital (occurring at birth) or acquired, though congenital nystagmus occurs more often than acquired nystagmus
Congenital nystagmus generally occurs sporadically in infants, but multiple members of the same family have been known to share the condition, and some studies have been able to link the condition to genetics.
Some of the most prominent conditions that can be associated with nystagmus in babies include:
Eye or head trauma
Improper brain or eye development
Cataracts
Albinism
Aniridia
Strabismus
Fetal alcohol syndrome
Vitamin deficiency
Severe refractive error
Reactions to certain medications
Amblyopia
Retina coloboma
Optic nerve hypoplasia
Stroke (rare)
SEE RELATED: Nystagmus causes
Diagnosis of infantile nystagmus
When is nystagmus diagnosed in babies? Though infantile nystagmus cases are often considered congenital (present at birth), it is typically not diagnosed at the time of birth. More often, congenital nystagmus is diagnosed between 6 weeks and 6 months of age.
Depending on the degree of the symptoms and the age when they start showing, an eye doctor may recommend testing beyond a comprehensive eye exam, such as blood work or an MRI brain scan. This will help the doctor further investigate the cause of nystagmus, and the severity of any underlying cause that may be present.
This will help the doctor further investigate the cause of nystagmus, and the severity of any underlying cause that may be present.
SEE RELATED: How eye twitching may be a sign of a brain disorder
Treatment for infantile nystagmus
How is nystagmus treated in babies? Treatment may vary depending on the type of nystagmus that is diagnosed. If nystagmus is due to a refractive error, corrective lenses may be prescribed for your young child. Vision therapy also may be helpful.
If nystagmus occurs due to a serious underlying condition, treatment is primarily reserved for the said condition, and will vary accordingly.
Surgical treatment is possible under circumstances in which head tilting has severely impaired the child, or for other major conditions.
In any case, it is best to consult an eye care professional to confirm a diagnosis and determine what the best treatment options are for your child. Children should have their first comprehensive eye exam at 6 months of age, but if conditions such as nystagmus are present, vision may need to be evaluated sooner.
READ NEXT: What Are Setting Sun Eyes (Setting Sun Sign)?
Page published on Tuesday, September 15, 2020
Nystagmus | Great Ormond Street Hospital
Nystagmus is a rhythmical, repetitive and involuntary movement of the eyes. It is usually from side to side, but sometimes up and down or in a circular motion. Both eyes can move together or independently of each other. A person with nystagmus has no control over this movement of the eyes.
What causes nystagmus?
Early onset nystagmus will appear in very young babies. It can also be called congenital nystagmus. Acquired nystagmus is when the condition appears later in childhood.
The condition might be caused by a developmental problem of the eye or brain, or the pathway between the two. Sometimes the condition can be caused by a stroke or head injury. The majority of children with the condition do not have any other health problems. When the cause is unknown it is called idiopathic. Some forms of nystagmus can be inherited.
When the cause is unknown it is called idiopathic. Some forms of nystagmus can be inherited.
The most obvious sign that a child has nystagmus is their eye or eyes will be moving randomly. The child may not be aware of this.
Children with nystagmus often have poorer vision and problems with balance. They will also find it more difficult to follow fast movements.
How is nystagmus normally diagnosed?
The condition can be diagnosed by various eye tests. These will include a normal sight test and monitoring their eye movements.
Nystagmus is defined according to the direction of movement of the eyes, how far they move and how often. Both eyes can move together or independently of each other.
How is nystagmus normally treated?
There is no cure for nystagmus.
Sight problems, such as long or short sightedness are common in people with nystagmus. Glasses will not cure the condition, but can help with reduced vision.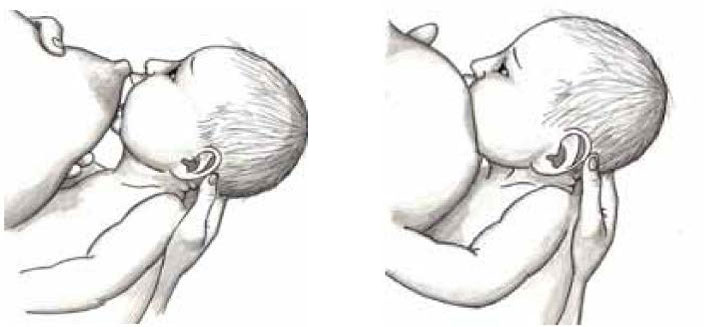
Large print books can help and will be especially useful for children learning to read. Extra time in school tests may be needed as reading the questions may take a little longer.
There is often a ‘null point’ where the eye movement is reduced. This can sometimes involve holding the head at an awkward angle, but it will help improve vision. Sometimes the eyes can be operated upon to reduce the awkward head posture (angle).
There are some authorities who advise operating on certain types of nystagmus to improve the quality of vision. Certain strict criteria must be met by eye movement recording before such procedures can be undertaken.
What happens next?
Each case of nystagmus will vary in severity and symptoms and reduced vision is common.
Children with nystagmus will need extra support and time to read. But this does not mean that they are unable or have learning difficulties. They simply have a challenge to overcome and it will take extra effort.
Children with nystagmus may feel self-conscious. This means it is important to build up their confidence.
Last review date:
August 2011
Ref:
2012F1269
N_stagm: faces, yak_ prescribe for liking
Faces that are used for juicing:
Goods: 7
Sorting: RatingCheapest Expensive
Type:
Evrizam Items: 1 Analogue: no
Go to box
Go to box
Phezam Items: 1 Analogue: NEMA
Go to the cat
Go to the cat
Rent to the cat
Go to the cat
Go to Koshik
NOOZEM Goods: No Analogues: no
Editorial team
Creation date: 04/27/2021 Update date: 12/20/2022
Nistagm - an important form of okorukhovyh porushen, which appears in the fleeting piercing eyes and is accompanied by a significant decrease in the severity of the dawn - a weak view.
Overhead views
Nystagmus - repeated mimic pendulum-like eye twitching, which may be physiological and pathological. So, nystagmus, which is normal for the wrapping of an opto-netic drum or body in space, is normal and serves to preserve a good dawn. Ruhi eyes, yakі zdіysnyuyut fixation on ob'єktі, are called foveous, and those, yakі vіdsuvayut fovea vіd ob'єkta, - defovuchimi. In case of pathological nystagmus of the skin, the cycle of derangement begins to sound like a fleeting respiration of the eyes at the object with the onset of recurrent reflux stribkopodibnym derangement. In a straight line, nystagmus can be horizontal, vertical, torsion, or nonspecific. The amplitude of nystagmus can be small-caliber or large-caliber (the amplitude of nystagmus is determined by the degree of respiration of the eyes), and the frequency of nystagmus can be high, medium, and low (the frequency of nystagmus is determined by the frequency of the eyes). nine0003
Causes of nystagmus
The development of nystagmus can be influx of central or mental factors.
Nystagmus is blamed for congenital or early reduced vision in connection with various eye diseases (clouding of the optic media, atrophy of the optic nerve, albinism, dystrophy of the eyes, etc.). As a result, the mechanism of oral fixation is destroyed.
Symptoms
The cream of the fleeting eyes of an ailment shows itself light-sensitivity, lowered eyesight, awareness of the fact that the visual picture is shifting, spreading and trembling. Likewise, you can feel a little inconsistency, confusion. In case of any ailment itself, it is possible to commemorate the pathology not in the first place, but only after concentration on this defect. nine0003
Acts of various illnesses do not lead to a severe deterioration of the dawn.
What can you do about nystagmus? With the manifestation of similar symptoms, one should turn to the doctor.
What can a healer do?
Respect! The symptom chart is for educational purposes only. Do not self-medicate; For all questions regarding the definition of the disease and how to treat it, contact your doctor. Our site is not responsible for the consequences caused by the use of the information posted on it. nine0003
Do not self-medicate; For all questions regarding the definition of the disease and how to treat it, contact your doctor. Our site is not responsible for the consequences caused by the use of the information posted on it. nine0003
Nervous system of an infant
The problem of children's health has always been one of the main priorities in the state system. Its versatility consists not only in the birth of a healthy child, but also in the creation of favorable conditions for its growth and development. Great importance is attached to the development of a system for the prevention and treatment of sick children, including children with congenital pathology.
In this regard, special attention is paid to disorders that occur in the antenatal and perinatal periods of development. It should be noted that the technical capabilities of diagnostic medicine (including DNA diagnostics), fetal imaging methods have significantly expanded, and therefore early diagnosis of diseases and malformations has become possible.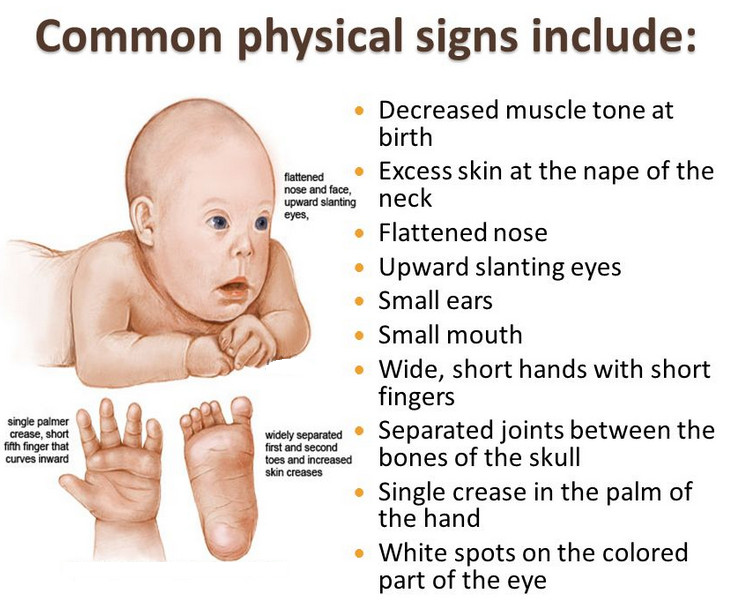 The pathology of early childhood and especially newborns is an increased complexity for the diagnostic process. To a greater extent, this applies to neurological examination. At this age, the general symptoms associated with the immaturity of the central nervous system come to the fore. Morphological immaturity of the central nervous system is manifested by the peculiarity of its functioning, which is characterized by an undifferentiated response to various stimuli, the lack of stability of neurological reactions and their rapid exhaustion. nine0003
The pathology of early childhood and especially newborns is an increased complexity for the diagnostic process. To a greater extent, this applies to neurological examination. At this age, the general symptoms associated with the immaturity of the central nervous system come to the fore. Morphological immaturity of the central nervous system is manifested by the peculiarity of its functioning, which is characterized by an undifferentiated response to various stimuli, the lack of stability of neurological reactions and their rapid exhaustion. nine0003
When evaluating the data obtained, it is necessary to take into account the state of the mother both during pregnancy and during childbirth.
Violations in the health of the mother can lead to depression of the general condition of the child, weakening of motor activity, inhibition or weakening of conditioned or unconditioned reflexes.
The state of the newborn can change significantly with intrauterine growth retardation. In addition, when examining a child, it is necessary to take into account the state of the environment: lighting, noise, room air temperature, etc. For the final diagnosis, a repeated examination is carried out, since the neurological symptoms detected for the first time may disappear during a second examination, or, symptoms , regarded for the first time as mild signs of a CNS disorder, may become more significant in the future. Assessment of the neurological status of children in the first year of life, including newborns, has a number of features. Thus, there is a predominance of general reactions, regardless of the nature of the irritating factors, and some symptoms, regarded in older children and adults as unconditionally pathological, are the norm in newborns and infants, reflecting the degree of maturity of certain structures of the nervous system and the stages of functional morphogenesis. The examination begins with visual observation of the child. Pay attention to the position of the head, torso, limbs.
In addition, when examining a child, it is necessary to take into account the state of the environment: lighting, noise, room air temperature, etc. For the final diagnosis, a repeated examination is carried out, since the neurological symptoms detected for the first time may disappear during a second examination, or, symptoms , regarded for the first time as mild signs of a CNS disorder, may become more significant in the future. Assessment of the neurological status of children in the first year of life, including newborns, has a number of features. Thus, there is a predominance of general reactions, regardless of the nature of the irritating factors, and some symptoms, regarded in older children and adults as unconditionally pathological, are the norm in newborns and infants, reflecting the degree of maturity of certain structures of the nervous system and the stages of functional morphogenesis. The examination begins with visual observation of the child. Pay attention to the position of the head, torso, limbs. Spontaneous movements of the arms and legs are assessed, the child's posture is determined, and the volume of active and passive movements is analyzed. A newborn baby's arms and legs are in constant motion. Spontaneous locomotor activity and crying increase before feeding and weaken after it. The newborn sucks and swallows well. nine0003
Spontaneous movements of the arms and legs are assessed, the child's posture is determined, and the volume of active and passive movements is analyzed. A newborn baby's arms and legs are in constant motion. Spontaneous locomotor activity and crying increase before feeding and weaken after it. The newborn sucks and swallows well. nine0003
With cerebral disorders, there is a sharp decrease in spontaneous motor activity. Sucking and swallowing reflexes are sharply reduced or absent. Low-amplitude high-frequency tremor of the chin, arms during a cry or an excited state of a newborn refers to physiological manifestations. A newborn full-term baby and an infant of the first months of life holds a predominantly flexor posture of the limbs, i.e. muscle tone in the flexors of the limbs prevails over the tone in the extensors, and the tone in the arms is higher than in the legs and it is symmetrical. Changes in muscle tone are manifested by muscle hypotension, dystonia, and hypertension. nine0003
Muscular hypotension is one of the most commonly diagnosed syndromes in newborns. It can be expressed from birth and be diffuse or limited, depending on the nature of the pathological process. It occurs in: congenital forms of neuromuscular diseases, asphyxia, intracranial and spinal birth trauma, damage to the peripheral nervous system, chromosomal syndromes, hereditary metabolic disorders, as well as in preterm infants. Since muscle hypotension is often combined with other neurological disorders (convulsions, hydrocephalus, cranial nerve paresis, etc.), the latter can modify the nature of developmental delay. It should also be noted that the quality of the hypotension syndrome itself and its impact on developmental delay will vary depending on the disease. Children with reduced excitability, with hypotension syndrome, suck sluggishly, often spit up. nine0003
It can be expressed from birth and be diffuse or limited, depending on the nature of the pathological process. It occurs in: congenital forms of neuromuscular diseases, asphyxia, intracranial and spinal birth trauma, damage to the peripheral nervous system, chromosomal syndromes, hereditary metabolic disorders, as well as in preterm infants. Since muscle hypotension is often combined with other neurological disorders (convulsions, hydrocephalus, cranial nerve paresis, etc.), the latter can modify the nature of developmental delay. It should also be noted that the quality of the hypotension syndrome itself and its impact on developmental delay will vary depending on the disease. Children with reduced excitability, with hypotension syndrome, suck sluggishly, often spit up. nine0003
Muscular hypertension syndrome is characterized by increased resistance to passive movements, limitation of spontaneous and voluntary motor activity. With the syndrome of muscular hypertension, some effort should be made to open the fists or straighten the limbs. Moreover, children quite often react to this by crying. Hypertonicity syndrome occurs with: increased intracranial pressure, purulent meningitis, biliary encephalopathy, intrauterine infection with CNS damage, after intracranial hemorrhage. Children with hypertonicity often have difficulty feeding, as the acts of sucking and swallowing are uncoordinated. Regurgitation and aerophagia are noted. However, it should be noted that physiological hypertension is observed in children during the first months of life. It arises due to the absence of the inhibitory effect of the pyramidal system on the spinal reflex arcs. But, if, as the baby grows older, there is an increase in muscle hypertension and the appearance of unilateral symptoms, then this should alert in terms of the possible development of cerebral palsy. The syndrome of movement disorders in newborns may be accompanied by muscular dystonia (a state of alternating tones - muscular hypotension alternates with muscular hypertension). Dystonia - a passing increase in muscle tone in the flexors, then in the extensor.
Moreover, children quite often react to this by crying. Hypertonicity syndrome occurs with: increased intracranial pressure, purulent meningitis, biliary encephalopathy, intrauterine infection with CNS damage, after intracranial hemorrhage. Children with hypertonicity often have difficulty feeding, as the acts of sucking and swallowing are uncoordinated. Regurgitation and aerophagia are noted. However, it should be noted that physiological hypertension is observed in children during the first months of life. It arises due to the absence of the inhibitory effect of the pyramidal system on the spinal reflex arcs. But, if, as the baby grows older, there is an increase in muscle hypertension and the appearance of unilateral symptoms, then this should alert in terms of the possible development of cerebral palsy. The syndrome of movement disorders in newborns may be accompanied by muscular dystonia (a state of alternating tones - muscular hypotension alternates with muscular hypertension). Dystonia - a passing increase in muscle tone in the flexors, then in the extensor. At rest, these children with passive movements expressed general muscular dystonia. When you try to perform any movement, with positive or emotional reactions, muscle tone increases dramatically. Such conditions are called dystonic attacks. The syndrome of mild transient muscular dystonia does not significantly affect the age-related motor development of the child. Only a doctor, a pediatrician and a neuropathologist can assess the state of muscle tone, so parents should remember that timely access to a doctor, dynamic observation of a child by specialists, necessary examinations carried out on time, and compliance with the appointments of the attending physician can prevent the development of any serious disorders from the side of CNS. When assessing the neurological status in children after examining muscle tone, it is necessary to examine the head, measure its circumference and compare its size with the size of the chest. nine0003
At rest, these children with passive movements expressed general muscular dystonia. When you try to perform any movement, with positive or emotional reactions, muscle tone increases dramatically. Such conditions are called dystonic attacks. The syndrome of mild transient muscular dystonia does not significantly affect the age-related motor development of the child. Only a doctor, a pediatrician and a neuropathologist can assess the state of muscle tone, so parents should remember that timely access to a doctor, dynamic observation of a child by specialists, necessary examinations carried out on time, and compliance with the appointments of the attending physician can prevent the development of any serious disorders from the side of CNS. When assessing the neurological status in children after examining muscle tone, it is necessary to examine the head, measure its circumference and compare its size with the size of the chest. nine0003
Hydrocephalus is characterized by an increase in the size of the head, which is associated with the expansion of the ventricular systems of the brain and subarochnoid spaces due to an excess amount of cerebrospinal fluid.
Macrocephaly is an increase in the size of the head, accompanied by an increase in the mass and size of the brain. May be a congenital malformation of the brain, occurs in children with famacoses, storage diseases, may be a family feature. Microcephaly is a reduction in the size of the head due to the small size of the brain. Congenital microcephaly is observed in genetic diseases, occurs with intrauterine neuroinfection, alcoholic fetopathy, brain malformations and other diseases. nine0003
Microcrania - reduction in the size of the head due to slow growth of the skull bones and their rapid ossification, with early closure of the sutures and fontanelles. Often, microcrania is a hereditary-constitutional feature. Craniostenosis is a congenital malformation of the skull, which leads to the formation of an irregular shape of the head with a change in its size, characterized by fusion of the sutures, a violation of the growth of individual bones of the skull. Craniostenosis is detected already in the first year of life and is manifested by various deformities of the skull - tower, scaphoid, triangular, etc. It is very important to assess the condition of the fontanelles. At birth, the anterior (large) and posterior (small) fontanelles are determined. The size of the fontanel is individual and ranges from 1 to 3 cm. A large fontanel closes, as a rule, by 1.5 years. The delay in the closure of the fontanel may be associated with high intracranial pressure, features of the ontogeny of the skull. Pay attention also to the presence of hematomas, swelling of the tissues of the head, the state of the subcutaneous venous network. Often, in children of the first day of life, palpation reveals swelling of the soft tissues of the head (birth tumor), which is not limited to one bone and reflects the physiological trauma of the skin and subcutaneous tissue during childbirth. nine0003
It is very important to assess the condition of the fontanelles. At birth, the anterior (large) and posterior (small) fontanelles are determined. The size of the fontanel is individual and ranges from 1 to 3 cm. A large fontanel closes, as a rule, by 1.5 years. The delay in the closure of the fontanel may be associated with high intracranial pressure, features of the ontogeny of the skull. Pay attention also to the presence of hematomas, swelling of the tissues of the head, the state of the subcutaneous venous network. Often, in children of the first day of life, palpation reveals swelling of the soft tissues of the head (birth tumor), which is not limited to one bone and reflects the physiological trauma of the skin and subcutaneous tissue during childbirth. nine0003
Cephalohematoma - hemorrhage under the periosteum, which is always located within one bone. Large cephalohematomas are removed, small ones resolve themselves.
Expanded subcutaneous venous network on the head indicates increased intracranial pressure both due to the CSF component and due to impaired venous outflow. The presence or absence of the above symptoms can only be assessed by a doctor (pediatrician or neuropathologist), after a thorough examination. In case of changes found by him, the child may be prescribed the necessary examination (NSG, EEG, Doppler examination of cerebral vessels, etc.), as well as treatment. After a general examination of a newborn child, an assessment of his consciousness, motor activity, muscle tone, the condition of the bones of the skull and soft tissues of the head, the pediatrician and neuropathologist assess the condition of the cranial nerves, unconditioned and tendon reflexes. The state of the cranial nerves in a newborn can be judged by the peculiarities of his facial expressions, crying, the act of sucking and swallowing, and the reaction to sound. Particular attention is paid to the organ of vision, since external changes in the eyes in some cases make it possible to suspect the presence of a congenital or hereditary disease, hypoxic or traumatic damage to the central nervous system.
The presence or absence of the above symptoms can only be assessed by a doctor (pediatrician or neuropathologist), after a thorough examination. In case of changes found by him, the child may be prescribed the necessary examination (NSG, EEG, Doppler examination of cerebral vessels, etc.), as well as treatment. After a general examination of a newborn child, an assessment of his consciousness, motor activity, muscle tone, the condition of the bones of the skull and soft tissues of the head, the pediatrician and neuropathologist assess the condition of the cranial nerves, unconditioned and tendon reflexes. The state of the cranial nerves in a newborn can be judged by the peculiarities of his facial expressions, crying, the act of sucking and swallowing, and the reaction to sound. Particular attention is paid to the organ of vision, since external changes in the eyes in some cases make it possible to suspect the presence of a congenital or hereditary disease, hypoxic or traumatic damage to the central nervous system. Specialist doctors (pediatrician, neurologist, ophthalmologist), when assessing the organ of vision, pay attention to the size and symmetry of the palpebral fissures, the condition of the iris, the presence of hemorrhage, the shape of the pupil, the presence of exophthalmos, nystagmus, ptosis and strabismus. The condition of the deeper structures of the eye (crystalline lens, vitreous body, retina) can only be assessed by an ophthalmologist. Therefore, it is so important that already in the first month of life the child be examined not only by a pediatrician and a neurologist, but also by an ophthalmologist. nine0003
Specialist doctors (pediatrician, neurologist, ophthalmologist), when assessing the organ of vision, pay attention to the size and symmetry of the palpebral fissures, the condition of the iris, the presence of hemorrhage, the shape of the pupil, the presence of exophthalmos, nystagmus, ptosis and strabismus. The condition of the deeper structures of the eye (crystalline lens, vitreous body, retina) can only be assessed by an ophthalmologist. Therefore, it is so important that already in the first month of life the child be examined not only by a pediatrician and a neurologist, but also by an ophthalmologist. nine0003
Thus, in order to diagnose in time and prevent serious disorders of the central nervous system in the future, parents must follow a number of rules: regular examinations by a neurologist: at 1 month, 3 months and a year; if the need arises, then more often. Consultations with an ophthalmologist at 1 month, 3 months and 1 year, if necessary, more often. Carrying out a screening study of the central nervous system (neurosonography) and other studies, if there is an indication for this.