Baby rapid breathing after feeding
Transient tachypnea - newborn: MedlinePlus Medical Encyclopedia
URL of this page: //medlineplus.gov/ency/article/007233.htm
To use the sharing features on this page, please enable JavaScript.
Transient tachypnea of the newborn (TTN) is a breathing disorder seen shortly after delivery, most often in early term or late preterm babies.
- Transient means it is short-lived (most often less than 48 hours).
- Tachypnea means rapid breathing (faster than most newborns, who normally breathe 40 to 60 times per minute).
As the baby grows in the womb, the lungs make a special fluid. This fluid fills the baby's lungs and helps them grow. When the baby is born at term, hormones released during labor tell the lungs to stop making this special fluid. The baby's lungs start removing or reabsorbing it.
The first few breaths a baby takes after delivery fill the lungs with air and help to clear most of the remaining lung fluid.
Leftover fluid in the lungs causes the baby to breathe rapidly. It is harder for the small air sacs of the lungs to stay open.
TTN is more likely to occur in babies who are:
- Born before 38 completed weeks gestation (preterm, or early term)
- Delivered by C-section, especially if labor has not already started
- Born to a mother with diabetes or asthma
- Twins
Newborns with TTN have breathing problems soon after birth, usually starting within 1 to 2 hours.
Symptoms include:
- Bluish skin color (cyanosis)
- Rapid breathing, which may occur with noises such as grunting
- Flaring nostrils or movements between the ribs or breastbone known as retractions
The mother's pregnancy and labor history are important to make the diagnosis.
Tests performed on the baby may include:
- Blood count and blood culture to rule out infection
- Chest x-ray to rule out other causes of breathing problems
- Blood gas to check levels of carbon dioxide and oxygen
- Continuous monitoring of the baby's oxygen levels, breathing, and heart rate
The diagnosis of TTN is most often made after the baby is monitored for 2 or 3 days. If the condition goes away in that time, it is considered to be transient.
If the condition goes away in that time, it is considered to be transient.
Your baby will be given oxygen, and sometimes CPAP (continuous positive airway pressure) as well, to keep the blood oxygen level and breathing rate stable. Your baby will often need the most support within a few hours after birth and will usually begin to improve after that. Most infants with TTN improve in less than 24 to 48 hours, but some will need help for a few days.
Very rapid breathing usually means a baby is unable to eat. Fluids and nutrients will be given through a vein until your baby improves. Your baby may also receive antibiotics until the health care team is sure there is no infection. Sometimes, babies with TTN will need help with breathing or feeding for a week or more, usually if they are premature.
The condition most often goes away within 48 to 72 hours after delivery. In most cases, babies who have had TTN have no further problems from the condition. They will not need special care or follow-up other than their routine checkups. However, there is some evidence that babies with TTN may be at a higher risk for wheezing problems later in infancy.
However, there is some evidence that babies with TTN may be at a higher risk for wheezing problems later in infancy.
Late preterm or early term babies (born more than 2 to 6 weeks before their due date) who have been delivered by C-section without labor may be at risk for a more severe form known as "malignant TTN."
TTN; Wet lungs - newborns; Retained fetal lung fluid; Transient RDS; Prolonged transition; Neonatal - transient tachypnea
Ahlfeld SK. Respiratory tract disorders. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 122.
Crowley MA. Neonatal respiratory disorders. In: Martin RJ, Fanaroff AA, Walsh MC, eds. Fanaroff and Martin's Neonatal-Perinatal Medicine: Diseases of the Fetus and Infant. 11th ed. Philadelphia, PA: Elsevier; 2020:chap 66.
Greenberg JM, Haberman BE, Narendran V, Nathan AT, Schibler K. Neonatal morbidities of prenatal and perinatal origin. In: Creasy RK, Lockwood CJ, Moore TR, Greene MF, Copel JA, Silver RM, eds. Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2019:chap 73.
In: Creasy RK, Lockwood CJ, Moore TR, Greene MF, Copel JA, Silver RM, eds. Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2019:chap 73.
Updated by: Kimberly G. Lee, MD, MSc, IBCLC, Clinical Professor of Pediatrics, Division of Neonatology, Medical University of South Carolina, Charleston, SC. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
What’s Normal and When You Should See a Doctor
Because newborns have developing lungs and weaker muscles, their typical breathing pattern may appear fast. Heavy breathing, coughing, and whistling sounds may be signs of a breathing problem.
You might notice your newborn breathing fast, even while sleeping. Babies can also take long pauses between each breath or make noises while breathing.
Most of these come down to a baby’s physiology. Babies have smaller lungs, weaker muscles, and breathe mostly through their noses. As newborns, babies are just learning to breathe, since the umbilical cord delivered all of their oxygen straight to their body by way of their blood while in the womb.
Babies have smaller lungs, weaker muscles, and breathe mostly through their noses. As newborns, babies are just learning to breathe, since the umbilical cord delivered all of their oxygen straight to their body by way of their blood while in the womb.
A child’s lungs are not fully developed until they are around 8 years old.
Newborns breathe a lot faster than older babies, kids, and adults. They may initially breathe irregularly before developing a regular breathing pattern.
Newborns younger than 6 months take about 40-60 breaths per minute. That looks pretty fast if you’re watching them.
Breathing may slow down to 30 breaths per minute while newborns sleep. In periodic breathing, a newborn’s breathing may stop for 5 to 10 seconds and then begin again more rapidly — around 40 to 60 breaths per minute — for 10 to 15 seconds. They shouldn’t pause more than 10 seconds between breaths, even when resting.
Familiarize yourself with your newborn’s typical breathing pattern while they’re healthy and relaxed. This can help you notice if things ever change.
This can help you notice if things ever change.
Fast breathing by itself may not be a cause for concern, but there are a few things to pay attention to. Once you have a sense of your newborn’s usual breathing pattern, you can watch closely for signs of change.
A sick newborn will look and act differently than they usually do. But it can be difficult to know what’s typical when you’ve only known your baby for a few weeks. Over time, as you get to know your baby better, your confidence may grow.
You can call a doctor whenever you have questions or concerns. Most offices have an on-call nurse who can offer tips and guidance.
Call a doctor or go for a walk-in appointment for any of the following:
- trouble sleeping or eating
- extreme fussiness
- deep cough
- barking cough
- fever above 100.4°F or 38°C (seek immediate care if your baby is under 3 months)
If your newborn has any of the following signs, seek immediate care:
- trouble catching their breath
- breathing faster than 60 breaths per minute
- grunting at the end of each breath
- nostrils flaring
- breathing with difficulty, such as the muscles pulling in under the ribs or around the neck
- blue or grayish tinge to the skin, especially around the mouth, head, and central body
- trouble crying
- dehydration from lack of eating
Recognizing an emergency
If a newborn is having significant difficulty breathing or has a blue or gray tinge to the skin, you should seek emergency medical care by calling 911 or your local emergency services.
Newborns may experience breathing difficulties due to a heart condition, infection, or another health condition.
Newborn breathing problems can include:
- deep cough, which may be a sign of mucus or infection in the lungs
- whistling noise or snoring, which may require suctioning mucus from the nose
- barking and hoarse cry that could indicate croup
- fast, heavy breathing which could potentially be fluid in the airways from pneumonia or transient tachypnea
- wheezing which could stem from bronchiolitis
- persistent dry cough, which may signal an allergy
- when a newborn stops breathing for at least 20 seconds, which can be a sign of apnea
Premature newborns may have underdeveloped lungs and be more likely to have problems breathing.
According to the National Heart, Lung, and Blood Institute (NHLBI), newborns delivered before 32 weeks of pregnancy may develop neonatal respiratory distress syndrome.
Full-term babies delivered by cesarean are at increased risk for other breathing issues right after birth, such as transient tachypnea of the newborn. This condition typically resolves within 3 days after birth, the NHLBI notes.
This condition typically resolves within 3 days after birth, the NHLBI notes.
If your newborn has been diagnosed with either condition, a doctor can discuss what signs you need to monitor.
Remember that coughing is a natural reflex that protects your baby’s airways and keeps germs out. If you’re concerned about your newborn’s breathing, monitor them over a few hours. You’ll soon be able to tell if it’s a mild cold or something more serious.
If your newborn is sick, you may want to contact a doctor. It can be difficult to tell how sick a newborn is.
Take a video of any worrisome behavior to show a doctor. You may be able to communicate with a doctor or pediatrician online or through an app for faster communication.
In a medical emergency, you should call 911 or your local emergency services or take your newborn to the nearest emergency room.
If a doctor advises home care for a mild cold, the follow tips may help:
- keep them hydrated
- use saline drops to help clear mucus
- prepare a warm bath or run a hot shower and sit in the steamy bathroom
- play calming music
- rock your baby in their favorite position
- ensure your baby gets enough sleep
If your newborn does not improve or their condition worsens, contact a doctor.
You should not use vapor rub as a treatment for children younger than age 2.
The American Academy of Pediatrics recommends putting babies to sleep flat on their backs for the best breathing support.
It might be difficult to settle your baby down on their back when they’re sick, but it remains the safest sleeping position.
Takeaway
Any irregular breathing in your child can be very alarming. Watch your baby and learn about their typical behavior so that you can act quickly if you notice that they’re having trouble breathing.
If you have concerns about your newborn’s breathing, it may be best to contact a doctor or visit an immediate care facility or emergency room, depending on the severity.
The baby gets tired quickly when feeding and breathes often: symptoms, diagnosis
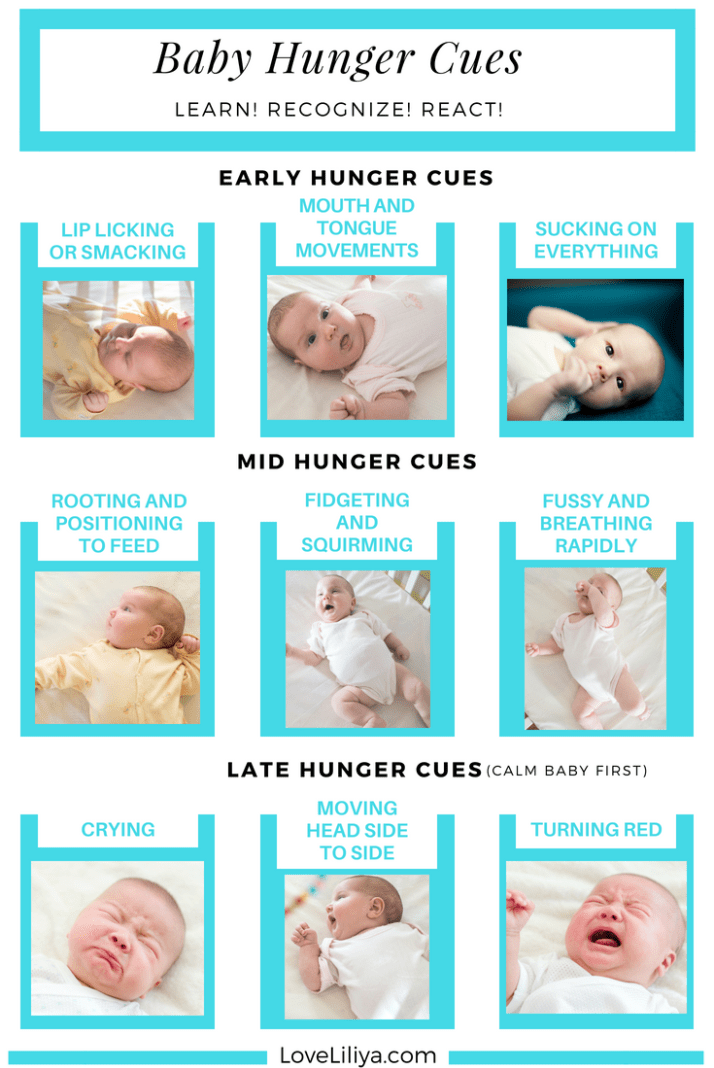
With the advent of the baby, all the mother's attention is focused on feeding the baby. After all, I really want the baby to gain weight well. But often during feeding, a woman notices that the baby gets tired quickly. In such a situation, the baby's breathing quickens, which prevents him from eating the prescribed norm. If such a picture is observed with frightening frequency, it is necessary to find out the cause of the problem.
But often during feeding, a woman notices that the baby gets tired quickly. In such a situation, the baby's breathing quickens, which prevents him from eating the prescribed norm. If such a picture is observed with frightening frequency, it is necessary to find out the cause of the problem.
In pediatric cardiology, there are several important signs that indicate heart problems in a young patient. The children's cardiologist of the multidisciplinary center "Edkarik" will be able to figure out what caused the difficulties in feeding. At the first negative symptoms in the baby, parents should contact us to exclude the presence of a serious heart pathology in the crumbs.
Features of breathing in infants
It should be noted right away that difficulty breathing during feeding is not always an indicator of an existing heart pathology. Such a symptom is typical for respiratory diseases, breathing difficulties may be associated with structural features of the nasal septum.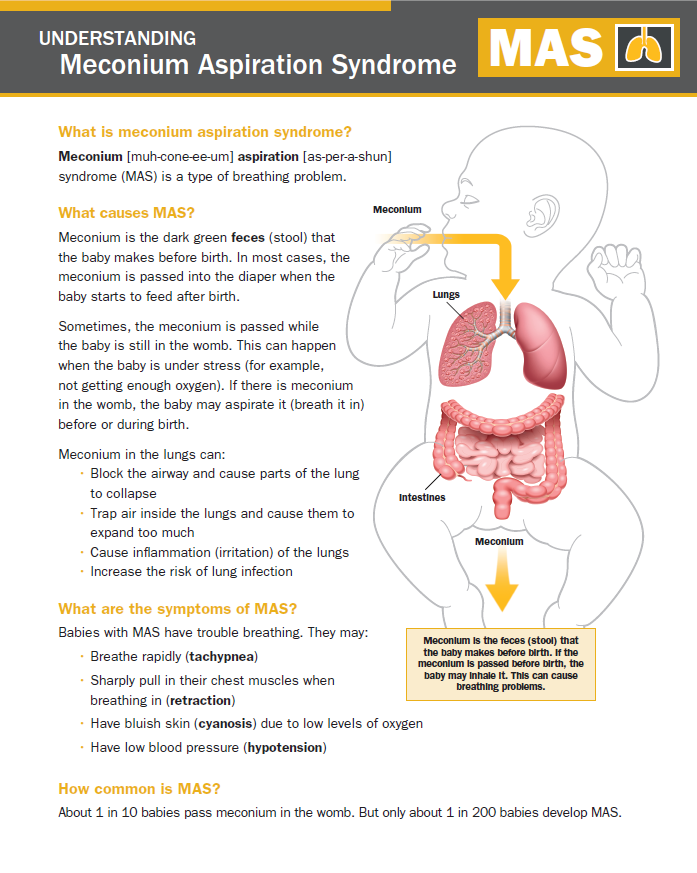 This problem is often observed in the first weeks due to undeveloped breasts in the mother. The child has to make every effort to get the right portion of food. Therefore, he quickly gets tired, and his breathing goes astray from the normal rhythm.
This problem is often observed in the first weeks due to undeveloped breasts in the mother. The child has to make every effort to get the right portion of food. Therefore, he quickly gets tired, and his breathing goes astray from the normal rhythm.
The breathing of children in the first months of life has its own characteristics. Babies need twice the amount of oxygen, but their respiratory system is not yet completely formed. Certain difficulties in the respiratory function are imposed by narrow nasal passages and weakness of the pectoral muscles. Therefore, breathing in children up to a year is uneven. The child often takes quick breaths, so his breathing is shallow and intermittent.
The norm of respiratory movements in babies of the first month of life is 40-60, from the end of the fourth week and up to 3 months - up to 45, in the period of 4-6 months - 35-40. By the year, the baby is already taking about 30-35 breaths per minute, which is considered the norm.
Mom can determine the respiratory rate on her own.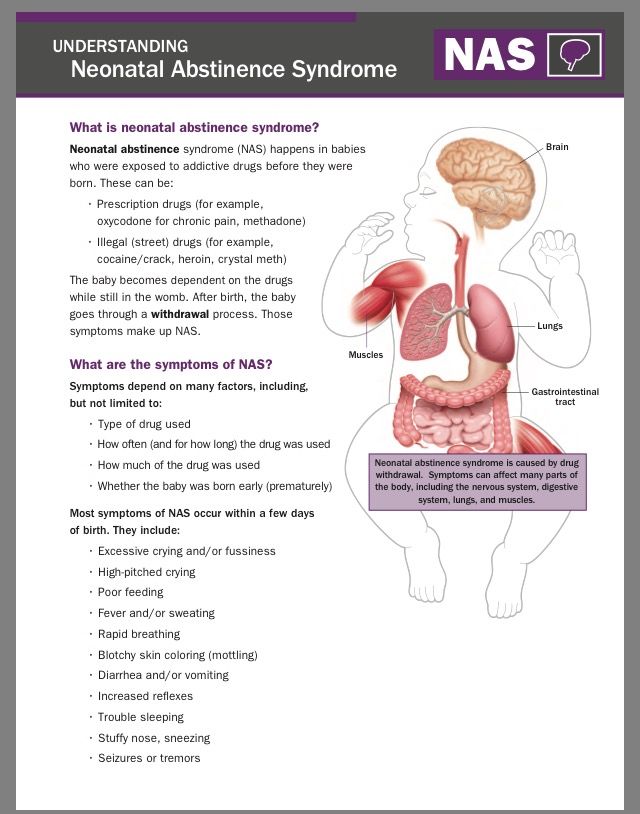 To do this, put the baby on his back, and use a stopwatch to count the number of breaths. Since babies "breathe" with their tummies, such a calculation is easy to make. The main condition for performing this procedure is that the child must be calm.
To do this, put the baby on his back, and use a stopwatch to count the number of breaths. Since babies "breathe" with their tummies, such a calculation is easy to make. The main condition for performing this procedure is that the child must be calm.
When there is no reason to worry
The nervous system of young children is still imperfect, so they cannot control their breathing. During active games and crying, the frequency of respiratory movements increases, and in a dream they often sniffle. If such features are observed sporadically, you should not worry. The sniffing nose can be washed with boiled water, and then carefully remove the dried mucus.
What should cause alarm
You need to see a doctor if the baby:
- holds his breath for a long time;
- exhales noisily;
- if breathing is accompanied by wheezing and wheezing.
Typically, such symptoms can be traced against the background of an acute period of respiratory diseases.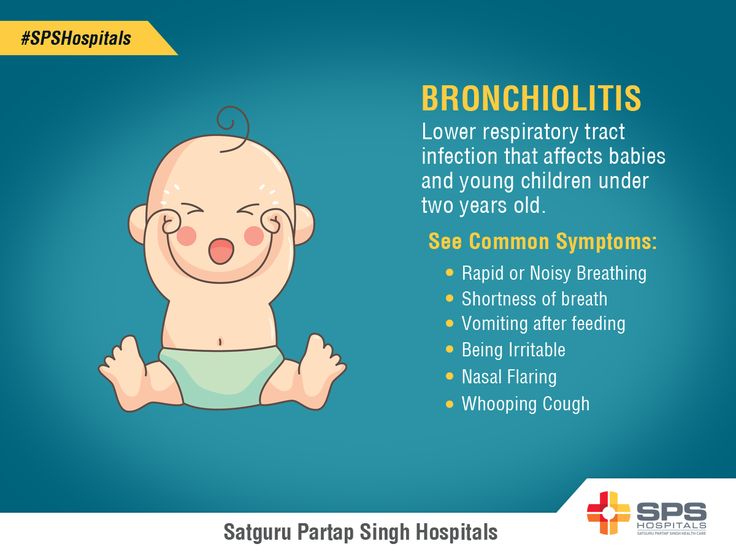 Timely treatment will help to quickly eliminate these negative signs, after which the child will be able to breastfeed normally again.
Timely treatment will help to quickly eliminate these negative signs, after which the child will be able to breastfeed normally again.
Which symptoms require special attention
We have listed physiological breathing problems. But sometimes the situation is much more serious than the usual runny nose. We list the signs that should be a strong argument for parents to urgently visit a pediatric cardiologist.
- Cyanosis
If holding the breath during feeding is accompanied by a blue nasolabial triangle, this sign indicates a lack of oxygen. In severe forms of cardiac pathologies, the chin and fingers of the baby turn blue. This symptom is characteristic of congenital malformations of both the heart and vascular anomalies.
- Shortness of breath
This symptom also indicates a lack of oxygen. Since the child has to expend more energy during sucking, this symptom is more pronounced than at rest.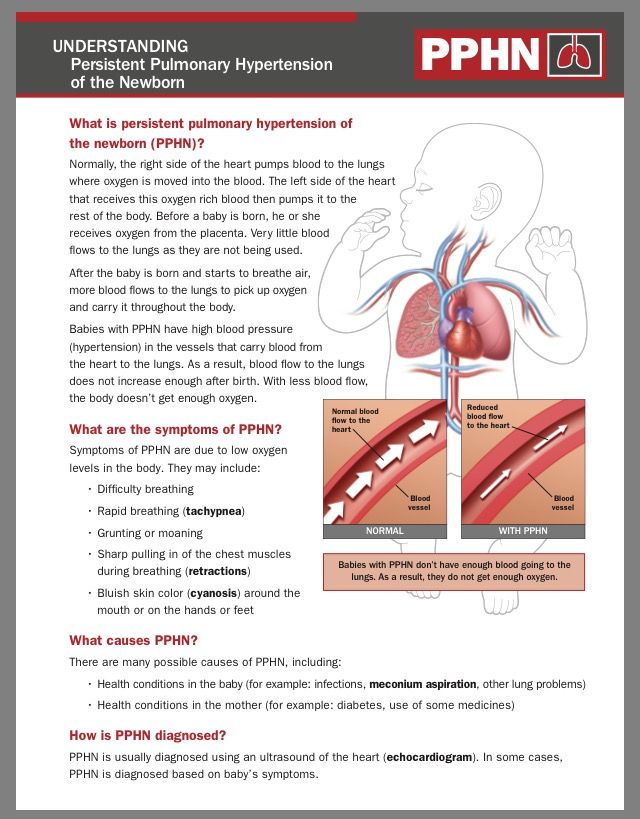 A cause for concern can be considered frequent breaks for rest during suckling. Normally, there are no more than two such pauses, and a child with heart disease takes breaks after 2-3 sips.
A cause for concern can be considered frequent breaks for rest during suckling. Normally, there are no more than two such pauses, and a child with heart disease takes breaks after 2-3 sips.
- Fatigue
Infants with congenital heart defects are much less active than healthy children. They are not able to suck out the norm during feeding, so they lose weight. The problem is aggravated by frequent breathing. The child simply suffocates under tension.
- Chest pain
Infants may not complain of such a symptom, but an observant mother will notice under what circumstances and how often the child begins to worry.
If all the described signs are repeated from the baby during feeding regularly, it is urgent to consult a pediatric cardiologist. A full-scale examination will determine the cause of the problem, and an experienced pediatric cardiologist will prescribe adequate therapy for the child.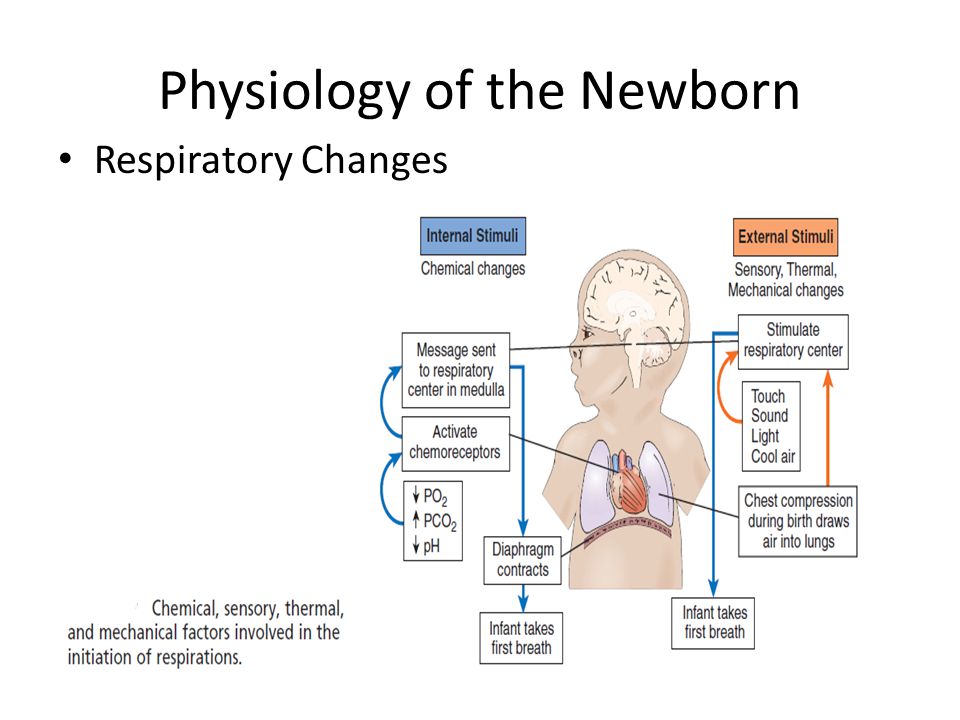
Peculiarities of diagnosing infants
Babies under one year old cannot describe the symptoms that prevent them from developing normally. Therefore, all hope for an objective examination. During the initial examination of the infant, a pediatric cardiologist:
- evaluates the general condition;
- notes the color of the skin;
- listens to the baby's heart;
- performs heart rate monitoring and saturation level measurement.
The doctor pays special attention to taking an anamnesis, since such information can indicate the cause of the problem. For example, an infection transmitted by a woman during her mother's pregnancy can provoke the development of congenital heart defects. An important factor is heredity, especially if there were cases of premature death (up to 50 years) among close relatives in the family. After collecting the data, the pediatric cardiologist will definitely prescribe the following types of diagnostic procedures:
- ECG with daily monitoring;
- ultrasound of the heart;
- Chest x-ray;
- Laboratory tests.
Instrumental methods of examination with the use of modern devices will clarify the parameters of the baby's heart and the features of its anatomical structure. Ultrasound diagnostics helps to identify defects in the heart chambers and great vessels. Having the data of all studies at hand, the pediatric cardiologist will draw up an individual treatment program, or prescribe additional procedures. In severe cardiac pathologies and rhythm disturbances, the question of a surgical way to eliminate the problem can be decided.
Examination and treatment in the center "Edkarik"
Among our guarantees:
- professionalism of doctors;
- high quality service;
- comfortable conditions in the clinic;
- individual approach;
- a wide range of services;
- accompanying patients during the rehabilitation period.
Our clinic is known not only in Kaliningrad, but also in other regions of the country. Parents and their kids will feel comfortable in our center, because there is everything you need to make sick children feel at home with us. You can make an appointment with a pediatric cardiologist on the official website of our center. There are also contact numbers where parents can consult on issues of concern to them.
Parents and their kids will feel comfortable in our center, because there is everything you need to make sick children feel at home with us. You can make an appointment with a pediatric cardiologist on the official website of our center. There are also contact numbers where parents can consult on issues of concern to them.
Breathing of a newborn. What parents should know
Breathing to breathing is different. How newborns breathe
When a baby appears in the house, many questions arise with him: what is the norm for a newborn, and what is a deviation from it, when you need to worry and worry, and when everything is in perfect order. Especially often young mothers are concerned about the baby's breathing. This is not surprising, because the breath of babies is very different from the breath of an adult.
1. The breathing of a newborn baby is very light, literally shallow. Sometimes it can be difficult to understand whether the baby is breathing at all, especially in a dream. This is the norm for newborns.
This is the norm for newborns.
2. For the first few weeks of life, the infant breathes unevenly, the breathing rhythm is constantly changing, any activity or external stimulus can affect the rhythm change. After a couple of months, the baby's breathing will become smoother, more stable.
3. The breathing of a newborn is much more rapid than in adults. The average frequency of breaths in a dream in an infant in the first year of life is about 35-40 per minute; during wakefulness, this figure will be even higher. This is also completely normal.
4. Nasal passages in newborns are very narrow, so any speck is enough to provoke a sneeze. In this case, the main task of parents is not to overdo it with care. If, apart from periodic sneezing, the child has no other signs of a cold, then, most likely, everything is in perfect order with him.
5. But such an interesting feature of newborn babies as the inability to breathe through the mouth requires the close attention of parents. The fact is that in the first weeks, and sometimes months of life, the baby simply does not know how to inhale air through the mouth, which means that any nasal congestion - due to a cold or simply due to the accumulation of mucus - becomes a real problem. In order not to provoke breathing difficulties, you should closely monitor the hygiene of the baby's nose. An important rule: you can clean the nose only with a cotton flagellum, in no case with cotton swabs.
The fact is that in the first weeks, and sometimes months of life, the baby simply does not know how to inhale air through the mouth, which means that any nasal congestion - due to a cold or simply due to the accumulation of mucus - becomes a real problem. In order not to provoke breathing difficulties, you should closely monitor the hygiene of the baby's nose. An important rule: you can clean the nose only with a cotton flagellum, in no case with cotton swabs.
6. Another common problem is the sound of the breathing of newborn babies. The structure of the muscles of the baby's larynx is such that when exhaling air, he often makes an accompanying noise: the baby sniffs, or even snores. In this case, it makes sense to worry only if the child's sniffling is accompanied by additional syndromes: the baby chokes in a dream, hoarseness of voice is observed, and general well-being worsens. If no additional symptoms are observed, sonorous breathing will disappear gradually, as the laryngeal muscles develop.











