Do babies burp every time they feed
How and When to Burp Your Baby
A key part of your baby's feeding routine is burping him. Your baby may swallow lots of air while feeding, and burping can help remove some of that gassiness and ease his fussiness. It may also help prevent him from spitting up.
Find out how to burp your baby, and pick up some tips on making burping more effective.
How to Burp Your Baby: Positions to Try
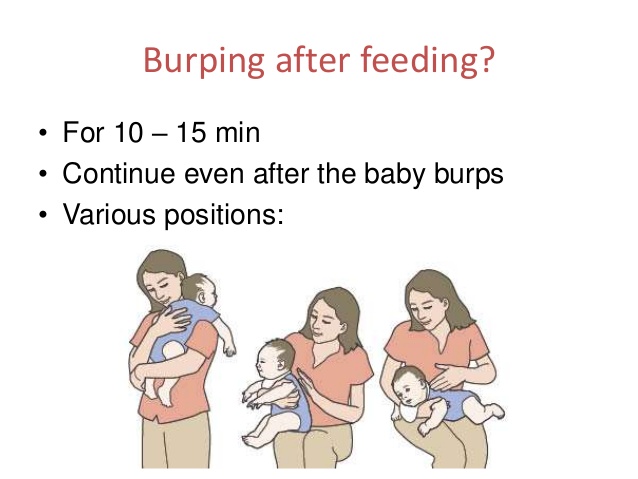
Here are three burping techniques that have stood the test of time. After trying each of them out, you’ll probably settle on one that works best for you and your baby:
Hold your baby upright against your chest with his chin on your shoulder, all the while supporting him with one hand as you gently pat his back with your other hand.
Place your baby on your lap with him sitting up, all the while supporting his head and chest with one hand while you softly pat his back with your other hand.
Lay your baby on your lap with his belly faced down, all the while supporting his head so it’s higher than his chest, and pat his back.
Tips for Burping Your Baby
Try these tips the next time you need to burp your baby:
Use repeated, gentle pats on her back.
Cup your hand slightly as you pat her, as this is gentler than using a flattened palm.
Drape a towel or bib over your lap or shoulder to protect your clothing as you burp your baby, in case your baby spits up (sometimes called “wet burps”).
Now that you know how to burp your baby, and these tips help you do so effectively, here’s a helpful visual guide:
How Long Should You Burp Your Baby?
There is no specific length of time needed for burping your baby. The more important factor is how often you burp him. With that in mind, burp your baby frequently throughout feeds, even when it looks like he doesn’t need to be burped.
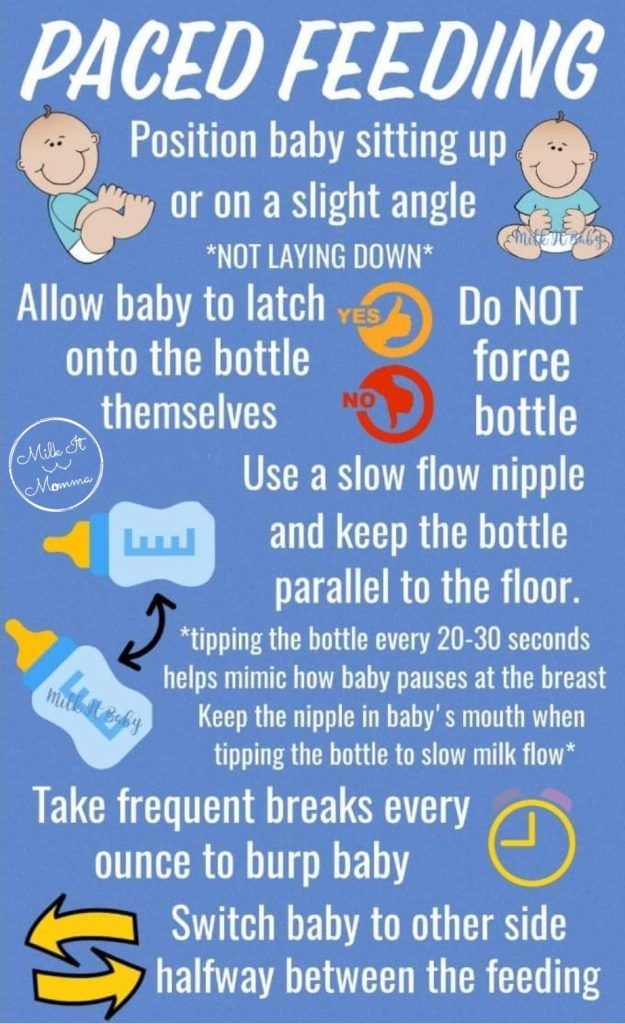
Waiting until after a feeding to burp your baby may mean your little one has swallowed too much air and may be fussier, so it’s better to stop feeding every so often and try to burp your little one. You could also try paced bottle feeding, which slows the flow of breast milk or formula from the bottle, which could help prevent gas.
You could also try paced bottle feeding, which slows the flow of breast milk or formula from the bottle, which could help prevent gas.
Here are some tips for burping your baby during a feeding:
If you’re bottle feeding (which can include formula feeding or offering expressed breast milk), you’ll want to burp him after every two to three ounces of milk.
If you’re breastfeeding, burp your baby each time he switches breasts. Some breastfed babies may not need to burp as often, as they may not swallow as much air.
If your baby hasn’t burped after some time, go back to feeding. Not every baby burps every time you want him to burp.
If your baby shows any of the following signs, you may want to burp him more regularly — for example, after every ounce of milk during bottle feeding or every five minutes during breastfeeding:
He is gassy
He spits up frequently
He has Gastroesophageal Reflux Disease (GERD)
He seems very fussy.

After a feeding is over, keep your baby in an upright position for 10 to 15 minutes. This can help prevent him from spitting up. You may need to burp him longer if he does spit up or has been diagnosed with GERD.
Other Instances When Burping Your Baby Might Be Beneficial
If your sleeping baby wakes suddenly and you suspect it may be because of gas, burping her might help relieve the pressure and help her fall back asleep.
A colicky baby, who may cry for three or more hours per day, might have gas from all the air she’s swallowed during one of these crying spells. You may consider burping her to see if it helps comfort her.
We hope these tips can help you burp your baby during feeding time to ensure she’s more comfortable.
Don’t forget to stock up on plenty of diapers, which you will surely need after all these feedings and burpings. Get rewarded for your Pampers purchases by using the Pampers Club app to earn rewards like coupons, gifts, and gift cards.
How to burp a sleeping baby: Effective methods
When a baby falls asleep without burping, parents and caregivers can try a few methods to help them relieve wind while staying asleep.
The act of breastfeeding or feeding from a bottle often has a calming effect. As a result, it can make many infants fall asleep during or after their meal.
This can pose a problem if the baby has swallowed air during their feed. They may need to release air through a burp, which is more difficult to do when asleep. Their body may be too relaxed to get into a burping position, or the parent or caregiver may not wish to risk waking the baby from their slumber.
However, many people find that they must burp their baby after every feed — sleeping or not. If the baby does not release air through a burp after feeding, they may have discomfort later as it moves through the intestines and causes gas.
In addition, some babies are so sleepy at the breast or bottle that they fail to take in enough calories at their meals. It may sometimes be necessary to wake the baby during feeding to help them eat more. Burping the baby may help by eliminating some feelings of fullness and helping them stay awake longer.
It may sometimes be necessary to wake the baby during feeding to help them eat more. Burping the baby may help by eliminating some feelings of fullness and helping them stay awake longer.
A parent or caregiver will often need to decide on a case-by-case basis whether they should try to burp their sleeping baby or simply let them sleep.
Share on PinterestBurping a baby may help relieve discomfort after feedings.As air travels upward, burping positions usually require the baby to be at least partially upright. This position encourages any air bubbles to move upward, passing through the throat and out of the mouth.
It is possible to burp a sleeping baby, often without waking them completely. Each baby is different, so people may need to try various techniques to find one that works.
Method 1: Shoulder
This method is suitable for babies who are sound sleepers. It can also be useful if a person needs to wake a baby up to continue their feeding.
- Turn the baby upright and lean them against the upper chest.
 Put one hand under their buttocks for support. The baby’s head should be on top of the shoulder.
Put one hand under their buttocks for support. The baby’s head should be on top of the shoulder. - Gently pat the baby’s back between their shoulder blades. Use an open palm to pat, being firm but gentle.
- If patting does not work, try rubbing their upper back in circular motions with the palm.
If the aim is to keep the baby awake, lightly bouncing them while they are on the shoulder may help wake them while also bringing up a burp.
Method 2: Chest
If a shoulder burp tends to wake the baby up, try a chest burp instead. Placing the baby on the chest can feel more comforting for them than the shoulder, so this position can often allow them to stay asleep after feeding.
- Gently lift the baby to the chest, putting one hand on their back and one under their buttocks.
- Avoid stretching their legs out. Allow their body to stay in a curled up position, which may make them less likely to wake up.
- Use the hand that is on their back to rub it, making circular motions first.
- If rubbing does not produce a burp, try gentle pats between their shoulders.
Method 3: Hip
The hip method works well for people who prefer to breastfeed their baby while lying down. It may help keep the baby asleep because the parent or caregiver does not have to sit up, and the baby is not fully upright.
- Gently place the baby’s tummy down over the hip or belly. Make sure that the baby’s head remains elevated above their body.
- Gently pat their back between the shoulder blades.
- Alternatively, rub their back in an upward circular motion.
Method 4: Arm hold
For smaller babies, the arm hold method can be useful. However, it is not always practical for older or larger babies.
- Place one arm under the baby’s back, allowing them to rest their body on the forearm. The baby may already be in this position for feeding.
- Carefully turn the baby’s body so that they are resting belly down on the parent’s or caregiver’s forearm with their head in the crook of the elbow.
 Place the hand between the baby’s legs, holding the baby for stability.
Place the hand between the baby’s legs, holding the baby for stability. - Rub or pat the baby’s upper back with the other hand.
- When finished, gently roll the baby toward the body. They will then be face up to continue feeding or to go to sleep.
Method 5: Lap
If the parent or caregiver is already sitting in a chair or on a couch, the lap method may work well to keep the baby asleep. It does not require the baby to be upright, which may be more soothing for them.
- While in a sitting position, gently turn the baby over onto their tummy and allow them to rest on the parent’s or caregiver’s thighs.
- Place one arm under the baby’s chin and chest to raise their upper body slightly.
- Use the other hand to pat their back or rub it in circular motions.
- When finished, turn the baby back over onto their back.
The baby may not always burp during or after feeding. In some cases, this may be because the baby did not swallow much air.
Sometimes, however, it takes a little persistence to get a burp out. Here are some helpful tips for parents and caregivers in these instances:
- Burp the baby during the feed. When a baby has finished feeding, they may be especially drowsy and may have swallowed more air. Try burping them before switching breasts or when they are halfway through their bottle.
- If the baby does not burp after 5 minutes of trying, gently lie them down on their back, either in their crib or on another safe surface, such as a playpen. After a few minutes, carefully pick the baby up and try burping them again. Sometimes, lying down helps move the air bubbles around, making them easier to release.
- Keep the baby upright after their feed. Using a baby wrap or sling can be a good way to let the baby sleep in a semi-upright position, allowing the air bubble to escape without any work from the parent or caregiver.
- There is no need to stress if the baby does not burp. There are times when a baby will not burp or has no air to release.
 If the baby does not burp despite using the methods above, do not worry. One study found that burping does not significantly reduce colic episodes.
If the baby does not burp despite using the methods above, do not worry. One study found that burping does not significantly reduce colic episodes.
The best way to help prevent excess gas in a baby is to try to prevent them from swallowing too much air. Swallowing air is often the result of the baby eating too quickly.
When bottle feeding, follow these tips to help prevent gas:
- Use a slow flow nipple on bottles, especially for newborns. Fast flow nipples may cause the baby to swallow more air.
- Angle the bottle so that air is not getting into the milk or formula while feeding. Doing this usually means tipping the bottle upward at an angle and keeping it tipped as the baby finishes the bottle.
- Test the flow of a bottle’s nipple before giving it to the baby. Tip it upside down and allow a few drops to come out. If the liquid comes out quickly, the nipple may have become worn out.
- Replace bottle nipples if the hole gets bigger, or the nipple shows signs of wear.

When breastfeeding, follow these tips to help prevent gas in the baby:
- Watch for signs of a fast letdown of milk from the breast. If the milk comes out too quickly at the beginning, and the baby is gulping or gasping, take the baby off the breast for a few seconds. Catch the excess milk in a towel or cloth if necessary. Once the milk flow has slowed down, put the baby back on the breast.
- Experiment with different breastfeeding positions. Different babies and women find that certain positions allow them both to breastfeed comfortably. It may help to ask a lactation consultant for tips.
- Make sure that the baby has latched on correctly. The baby’s lips should be sealed and spread out around the nipple. Their lips should not turn inward.
There are ways to burp a sleeping baby without waking them, but no method is foolproof. Parents and caregivers may need to experiment with different burping methods to find which ones work best for them and the baby.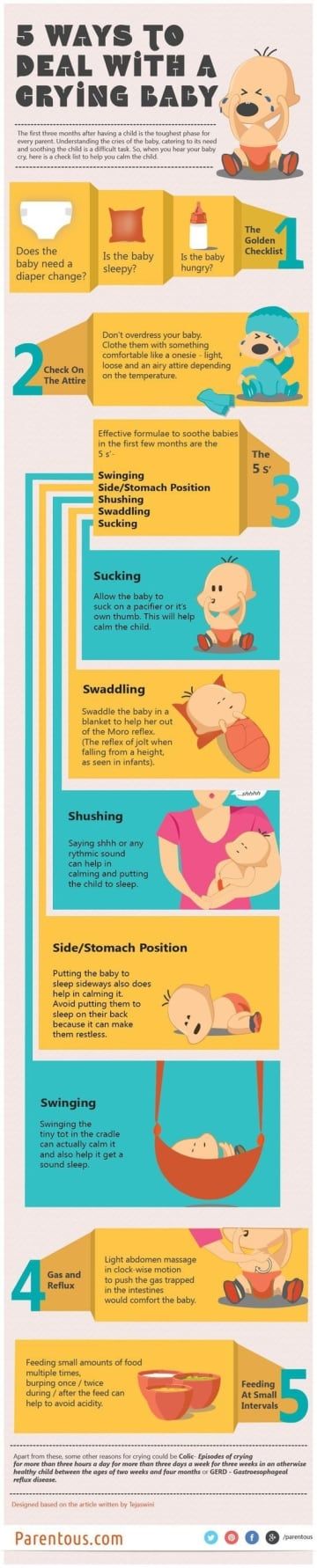
While many babies fall asleep while breastfeeding or bottle feeding, it is important to follow the American Academy of Pediatrics‘ safe sleep guidelines for babies. Following these guidelines may help prevent sudden infant death syndrome (SIDS) and sleep-related infant deaths.
Babies should have regular checkups with a pediatrician to be sure that they are feeding and gaining weight as necessary.
Why do newborns spit up? | Philips Avent
search support iconSearch Keywords
Home ›› Why is my baby spitting up and how can I help him?
Home ›› Why does my baby spit up and how can I help him?
↑ Top
Whether it's your first or third baby, you're bound to have questions about feeding. Reflux (spitting up) is a common topic among frequently discussed feeding topics, so you are not alone in finding the answer to the question “Why does my baby spit up so often?”.
So why do babies spit up? And is spitting up normal for babies? You have probably thought about this many times.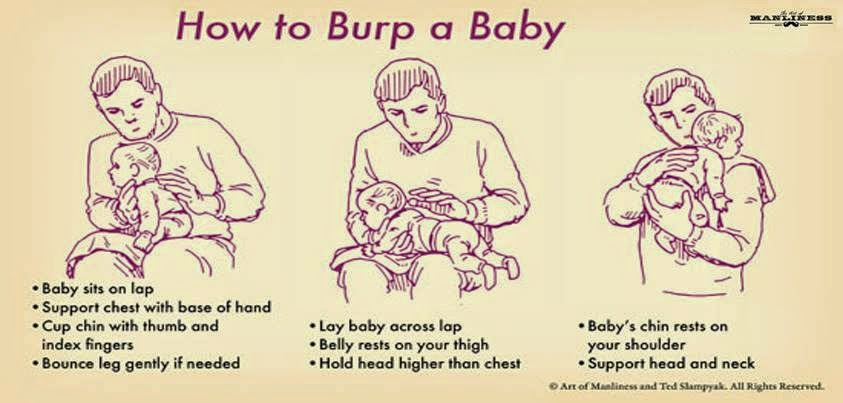 After reading this article, you will receive important information that will explain the causes of infant spitting up, and you will learn how to act to help the child.
After reading this article, you will receive important information that will explain the causes of infant spitting up, and you will learn how to act to help the child.
If you have any questions or your child has other symptoms, be sure to contact your doctor.
Why do babies spit up and when is it normal?
Let's look at why babies spit up and answer the frequently asked question "Why does my baby spit up so much?". Many newborns spit up after feedings or when burping because their digestive tract is not yet fully developed. However, in some situations, the likelihood of regurgitation in infants increases.
So what causes reflux in babies? The following are some of the main causes of regurgitation in infants: 1
- The child has moved.
- The child was eating too fast.
- You help your baby spit up air, and with the air, the baby spit up part of the food.
- The child has too much air in the stomach.
- The child has excessive salivation.
So is spitting up normal in infants? In simple words: spitting up after some feeds, or even after each, is absolutely normal for a growing baby. However, there are points that need to be noted in order to distinguish ordinary regurgitation from vomiting. The two processes are very different, so you should check with your doctor if your baby is vomiting heavily after every or most feeds.
Also seek medical attention if your child has any of the following symptoms that a doctor can help identify: 2
- The child vomits frequently, does not gain enough height or weight.
- Judging by external signs, he is in pain, cries a lot or arches his back.
- Coughing or difficulty breathing, which may be a symptom of gastroesophageal reflux disease.
- Regurgitates even if he hasn't eaten anything.

- There is severe vomiting.
- Fever or diarrhea, which may be a sign of an intestinal infection and lead to dehydration.
If your baby spit up a small amount of milk after a feed and continues to grow and stay healthy, rest assured that this is normal and nothing to worry about. If you have any questions about reflux in infants, check out this article to learn about the symptoms of reflux and how to deal with it!
What to do
Now that you know that spitting up is a normal physiological process and what causes it, you are probably wondering what you can do to help your baby. After you have consulted with your pediatrician and he has determined that spitting up is not a cause for concern, there are a few things you can do to help you when you are confused: 1
1. Regular belching of air.
In addition to burping after feedings, try helping your baby burp when changing breasts. And when feeding from a bottle, try to have the child spit up air every 30-60 ml of the mixture. Consider using an anti-colic bottle with an AirFree valve. The AirFree valve prevents air from entering the nipple even when the bottle is in a horizontal position and the nipple remains completely filled with milk. The use of such a bottle will allow your baby to drink in an upright position, which will reduce the frequency of reflux, improve the digestion process and make the feeding process more comfortable for both you and the baby. Find out more about Philips Avent anti-colic bottles with AirFree valve here.
And when feeding from a bottle, try to have the child spit up air every 30-60 ml of the mixture. Consider using an anti-colic bottle with an AirFree valve. The AirFree valve prevents air from entering the nipple even when the bottle is in a horizontal position and the nipple remains completely filled with milk. The use of such a bottle will allow your baby to drink in an upright position, which will reduce the frequency of reflux, improve the digestion process and make the feeding process more comfortable for both you and the baby. Find out more about Philips Avent anti-colic bottles with AirFree valve here.
3. Avoid vigorous movement after feeding.
To avoid spitting up after a feed, it is best to refrain from any bouncing, rocking or active play until the milk has been digested better.
4. Keep your baby's head up while feeding.
When you're trying to find the right feeding position that's comfortable for both your baby and you, try to avoid a position where your baby's head is down. In other words, it is necessary to ensure that in the process of feeding the head of the child is above the level of his legs.
In other words, it is necessary to ensure that in the process of feeding the head of the child is above the level of his legs.
5. Raise the mattress at the head of the bed
It is a good idea to roll up some towels or blankets and put them under the mattress (but not on top of the mattress) in the crib. Make sure that only the headboard is raised and that there are no creases in the middle of the mattress. There should be a very slight slope from which the baby will not slip.
It's a natural process
If you ever ask yourself the question "Why is my baby spitting up?" just remember that spitting up is a completely natural, sometimes troublesome process that is part of parenthood. There are various reasons for spitting up in babies, but if your baby looks calm after a feed and is actively developing, you have nothing to worry about. In truth, spitting up is more of a problem for the parents than for the child himself, who may not even notice it.
Philips Avent Articles & Tips
New Anti-colic Bottle with AirFree Valve
Designed to reduce colic, gas and spitting up 1
9005 that the baby is not getting enough milk, do not postpone the visit to the doctor. If the doctor confirms that the baby's spitting up is normal, all you have to do is keep a clean bib ready!
Baby+ app
Download the app and track your child's development and growth with trackers and save those special moments forever.
Download App:
1 kidshealth.org - Breastfeeding FAQs: Some Common Concerns Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain.
I understand
You are about to visit a Philips global content page
You are about to visit the Philips USA website.
Why does the baby spit up after feeding?
search support iconSearch Keywords
Regurgitation is a common condition in newborns and infants and is most often a normal variant. However, it is not uncommon for parents to worry if their baby is spitting up frequently, believing that it is due to nutritional or health problems in general. Sometimes these fears are not unfounded, and regurgitation really has a pathological origin. What is its cause and when should you really consult a doctor about this?
Regurgitation - Return of a small amount of food (uncurdled or partially curdled milk) from the stomach up the digestive tract: into the esophagus and further into the oral cavity. According to statistics, at least 1 time during the day, at least 50% of babies from 0 to 3 months can spit up, more than 60% of children 3-4 months old, and in 5% of children spit up continues up to the year 1 .
Regurgitation in newborns is considered a physiological process. It is caused by a number of factors, including:
It is caused by a number of factors, including:
- Features of the structure of the upper digestive tract in babies
- In newborns and infants up to a year of age, the stomach has a spherical shape. It holds a small amount of food, besides, the release from it into the duodenum is slower in comparison with children after the year 2 .
- Weakness of the lower esophageal sphincter that separates the esophagus from the stomach
- Normally, the lower esophageal sphincter should tightly "close" the esophagus, allowing food to pass into the stomach and not allowing it to enter back into the upper digestive tract. However, in young children (up to a year), the muscles of the esophageal sphincter are poorly developed, and it does not do its job very well 2 .
- Slow movement of food through the gastrointestinal tract
- The neuromuscular apparatus of newborns is immature. It does not ensure the proper movement of food through the esophagus, causing regurgitation.

One of the important risk factors contributing to the appearance of regurgitation in newborns is aerophagia. This is the swallowing of large amounts of air during feedings. This happens when the baby is not properly attached to the breast, the mother has a lack of breast milk, or the bottle is in the wrong position in the child who receives the mixture. The size of the opening in the nipple also matters - if it is too large, the newborn swallows a lot of air 3 .
With aerophagia, the baby becomes capricious, restless immediately after feeding. Noticeable bloating. If the baby burps immediately after a feed, the milk (or formula) remains practically fresh, uncurdled 3 .
Promotes post-feeding regurgitation and predominantly horizontal position of the baby during the day, combined with relatively high intra-abdominal pressure 4 . Therefore, the correct position of the baby after feeding is so important. To avoid regurgitation of an excessive amount of stomach contents, after feeding, it is necessary to hold the baby in an upright “column” position for some time (10-20 minutes), lightly patting on the back and allowing excess air to “exit”.
To avoid regurgitation of an excessive amount of stomach contents, after feeding, it is necessary to hold the baby in an upright “column” position for some time (10-20 minutes), lightly patting on the back and allowing excess air to “exit”.
Regurgitation in many newborns can be provoked by other situations in which pressure in the abdominal cavity increases and stomach contents are thrown into the esophagus, in particular 3 :
- tight swaddling;
- stool disorder, in particular constipation;
- long, forced cry and some others.
Want to avoid common feeding problems?
Start with a baby bottle with an anti-colic system that helps avoid common feeding problems such as colic, gas and spitting up*
How can you tell the difference between normal spitting up and vomiting?
Sometimes regurgitation is considered a manifestation of disorders in the digestive tract of children. Due to the constant reflux of acidic stomach contents into the upper sections, inflammation and other complications may develop, including growth retardation, a decrease in hemoglobin levels, and others. Therefore, it is important for parents to understand where the line is between physiological and pathological regurgitation 1 .
Due to the constant reflux of acidic stomach contents into the upper sections, inflammation and other complications may develop, including growth retardation, a decrease in hemoglobin levels, and others. Therefore, it is important for parents to understand where the line is between physiological and pathological regurgitation 1 .
If the mother is worried that her baby is spitting up, keep track of when this happens and count the total number of spit ups per day. Normally, regurgitation usually occurs after eating (the child burps after each feeding), lasts no more than 20 seconds and repeats no more than 20-30 times a day. With pathology, the problem manifests itself at any time of the day, regardless of when the baby was fed. Their number can reach 50 per day, and sometimes more 1 .
The amount of discharge during regurgitation also matters. With normal, physiological regurgitation, it is approximately 5 - 30 ml. If this volume fluctuates between 50 and 100 ml, it is already defined as profuse vomiting. When the range of the jet of vomit is up to 50 cm, doctors talk about "vomiting a fountain." A variant of atonic vomiting is possible, when the contents of the stomach flow "sluggishly". It occurs with atony of the stomach (decrease in muscle tone of the stomach wall) and disruption of the esophagus 1 .
When the range of the jet of vomit is up to 50 cm, doctors talk about "vomiting a fountain." A variant of atonic vomiting is possible, when the contents of the stomach flow "sluggishly". It occurs with atony of the stomach (decrease in muscle tone of the stomach wall) and disruption of the esophagus 1 .
Vomiting in babies is a warning sign. Doctors are especially alarmed by repeated vomiting, a fountain, with an admixture of bile, in combination with constipation. Vomiting can lead to the development of dehydration, acid-base imbalance and other consequences, therefore, if it occurs, you should urgently contact a pediatrician to find out the cause and begin treatment. A doctor's consultation is necessary if the child is spitting up a lot (more than 15-30 ml at a time), with a frequency of more than 50 episodes per day 1.3 .
Physiological regurgitation: symptoms
Regurgitation in newborns, which is considered normal and not of concern to pediatricians 3 :
- usually continues for a certain period of time;
- is characterized by slow, "passive" leakage; if the baby spits up a fountain, it is better to consult a doctor;
- has a sour smell of curdled milk;
- occurs without the participation of muscles - the baby does not strain during regurgitation;
- does not affect the general well-being of the baby.
How can I help a newborn who vomits frequently?
If the baby is healthy, no medication is prescribed for spitting up. To help the child allow simple measures based on lifestyle changes and feeding.
- Frequent feeding of the baby
It is known that babies are more prone to spit up if their stomach is full. To improve the situation, it is recommended to feed the baby more often, avoiding oversaturation, best of all - on demand 5 .
- Correct feeding technique
Every feeding, the mother must ensure that the baby does not swallow too much air during suckling. When sucking, there should be no loud, smacking, clicking sounds. You also need to control that the baby captures the nipple along with the areola.
- Choosing the right bottle and nipple
If the newborn is bottle-fed and receiving formula, it is important to choose the right bottle and nipple. The hole in it should be such that the milk flows out in drops, and not in a stream. The nipple must not be filled with air
The hole in it should be such that the milk flows out in drops, and not in a stream. The nipple must not be filled with air New Anti-colic bottle with AirFree valve
The AirFree valve prevents air from entering the baby's stomach.
- Baby standing upright after eating
To allow air that has entered the digestive tract during meals to escape, it is important to keep the newborn upright for 10-20 minutes after feeding 4 .
- Ensure the correct position of the baby during sleep
To reduce the negative impact of the acidic contents of the stomach on the esophagus, it is necessary to put the baby to sleep in the supine position. The side or prone position, which many pediatricians used to recommend, is no longer recommended. It was found to be associated with an increased risk of sudden infant death syndrome 5 .
If parents notice alarming symptoms, such as spitting up too often or large volume, etc.
 , it is important to consult a pediatrician without delay. This will allow you to identify the real problem in time and help the baby grow up healthy and happy.
, it is important to consult a pediatrician without delay. This will allow you to identify the real problem in time and help the baby grow up healthy and happy.
References1 Zakharova I. N., Andryukhina E. N. Regurgitation and vomiting syndrome in young children // Pediatric pharmacology, 2010. V. 7. No. 4.
Nagornaya 2903 V., Limarenko M. P., Logvinenko N. G. Experience with the use of domperidone in suspension in young children with regurgitation syndrome // Child Health, 2013. No. 5 (48).3 Zakharova IN Regurgitation and vomiting in children: what to do? //Pediatrics. Supplement to Consilium Medicum, 2009. No. 3. S. 58-67.
4 Zakharova I. N., Sugyan N. G., Pykov M. I. Regurgitation syndrome in young children: diagnosis and correction // Effective pharmacotherapy, 2014. No. 3. P. 18-28.
5 Vandenplas Y. et al. Pediatric gastroesophageal reflux clinical practice guidelines: joint recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) //Journal of pediatric gastroenterology and nutrition.