Feed training baby
Why feeding "on cue" benefits babies
© 2009 – 2021 Gwen Dewar, Ph.D., all rights reserved
The infant feeding schedule reconsidered
In the past, Western “baby experts” often instructed parents to feed their babies at regularly-spaced intervals of 3- or 4-hours. Today, official medical recommendations have shifted in favor of letting babies decide. Why the change?
There are a number of reasons, but the simple answer is this: When we let babies determine the timing and the length of their own feeds, they are more likely to get what they need: Not too little, and not too much.
It begins in the newborn period. If newborn babies aren’t fed frequently enough, they are at higher risk for dehydration and underfeeding. So the American Academy of Pediatrics (AAP) advises parents to feed infants at least once every 2-3 hours — whenever babies show signs of hunger (AAP 2015).
During the subsequent months, babies may be able to go longer between meals. But feeding responsively — on cue — remains the ideal approach.
- It can help breastfed babies adjust to natural variations in milk quality (Institute of Medicine, National Academy of Sciences 1991).
- It can help bottle-bed babies avoid overfeeding.
- And it can help any infant cope with the challenges of getting enough to eat during a growth spurt.
All babies experience fluctuations in their energy requirements. Feeding on cue makes it easier for infants to increase or decrease their intake as needed (Tylka et al 2015).
That’s probably why responsive feeding is associated with healthier growth trajectories in babies (Chen et al 2020; Fuglestad et al 2017).
And that’s not all. Research hints that responsive feeding benefits babies in additional ways. It might affect an infant’s emotional functioning. It might support better cognitive outcomes.
So it seems that the best infant feeding schedule is the one that babies devise for themselves.
But what is the evidence? Let’s take more detailed look.
The infant feeding schedule in evolutionary perspective
Mammal babies everywhere begin life on a diet of milk. But they don’t all time their feedings in the same way. In some species, mothers “park” or “cache” their young in nests, and leave them there.
It’s a strategy that allows the mother to go foraging without the fuss of a tag-along infant. But it only works if there’s a way to keep the babies from starving during those long separations. How do they cope?
The solution is two-fold.
1. Mothers produce milk that is high in fat, and high in protein — what we might call super-fuel.
2. Infants have the ability to suckle very fast and efficiently when they finally get to feed.
Together, these elements permit babies to “tank up” on a highly-concentrated food–enough to last them for many hours.
Mammals that follow this strategy are called “spaced feeders,” and their milk is very rich indeed.
A good example of a spaced feeder is the rabbit, which produces milk that is 18.3% fat and 13.9% protein (Jenness 1974).
By contrast, other mammals keep their babies with them as they forage. Exactly how they do this varies from species to species. Some, like monkeys, carry their babies. Others, like cows, have their infants follow them around on foot.
But regardless, the babies stay close, and along with proximity comes frequent meals. Babies tend to initiate feedings, and suckle at a more leisurely rate. They don’t need to tank up on a super-fuel, and so their mothers don’t make one. The milk is less caloric, more dilute.
A good example of a continual feeder is a cow, which produces milk that is typically 3.7% fat and 3.4% protein (Jenness 1974).
What about humans?
In some modern, industrial societies, humans act like spaced feeders. Babies are “parked” in cribs or cradles and get fed after intervals of 3-4 hours.
But were we designed for this strategy?
Does the biology of human breastfeeding have the earmarks of spaced feeding?
The answer is no because
- human milk is relatively low in fat (3.
 8%) and protein (1%), and
8%) and protein (1%), and - human infants suckle at the slow pace typical of continual feeders.
So our basic physiology gives us away. We don’t produce super-fuel, and our infants lack the spaced-feeder’s knack for super-fast milk extraction. And that’s consistent with the behavior of other members of our family tree. Continual feeding is the strategy of choice among all of our close relatives — including bonobos, chimpanzees, and gorillas.
It is also the strategy observed among human beings living in traditional societies.
In hunter-gatherer societies, babies aren’t just nursed on cue. They are also nursed very frequently — about 2-4 times an hour (Konner 2006).
In other traditional societies, parents don’t match this extreme pace, but feedings are nonetheless initiated by the infants.
In a survey of non-industrial societies (which included nomadic pastoralists and settled agricultural peoples) anthropologists found that “on demand” feeding was the rule. In every society for which information about the infant feeding schedule was available (25 out of 25), people fed their infants on cue (Severn Nelson et al 2000).
In every society for which information about the infant feeding schedule was available (25 out of 25), people fed their infants on cue (Severn Nelson et al 2000).
This, then, is our basic physiology and our evolutionary heritage. But how much does it matter? Is this something we can work around?
Mightn’t we be able to keep babies equally happy and healthy using a strict infant feeding schedule? Perhaps it’s just a matter of tweaking the timing of feeds.
It sounds straightforward, but there are stumbling blocks.
Babies vary in their needs — from individual to individual, and from day to day
Different babies have different needs, and the same baby experiences fluctuations in energy requirements over time.
What if your baby has the urge to be more active, and needs more food to fuel her activities?
What if your infant needs more fluids because it’s hot, or because he’s coming down with a virus?
What if your baby is in the middle of a growth spurt?
It isn’t merely that you need to adopt a schedule that is individualized to your baby’s current needs. You also need a schedule that keeps changing in response his or her future needs.
You also need a schedule that keeps changing in response his or her future needs.
That’s pretty hard to do unless you are paying attention to your baby, offering meals when you observe signs of hunger. And if you are doing that, you aren’t imposing a strictly-timed infant feeding schedule. By definition, you are feeding on cue.
Moreover, the baby’s need for food and fluids is only one side of the equation — the demand side. There is also the supply side of the equation. If your baby is on formula, it’s easy to figure out what your baby is being supplied with. You can read the label, and know your baby is getting the same formulation from one feed to the next.
But breast milk doesn’t work that way. Human breast milk is roughly similar in composition from one woman to the next, but there are significant differences. Not only does breast milk vary between individuals. It also varies between milk samples produced by the same woman at different points in time.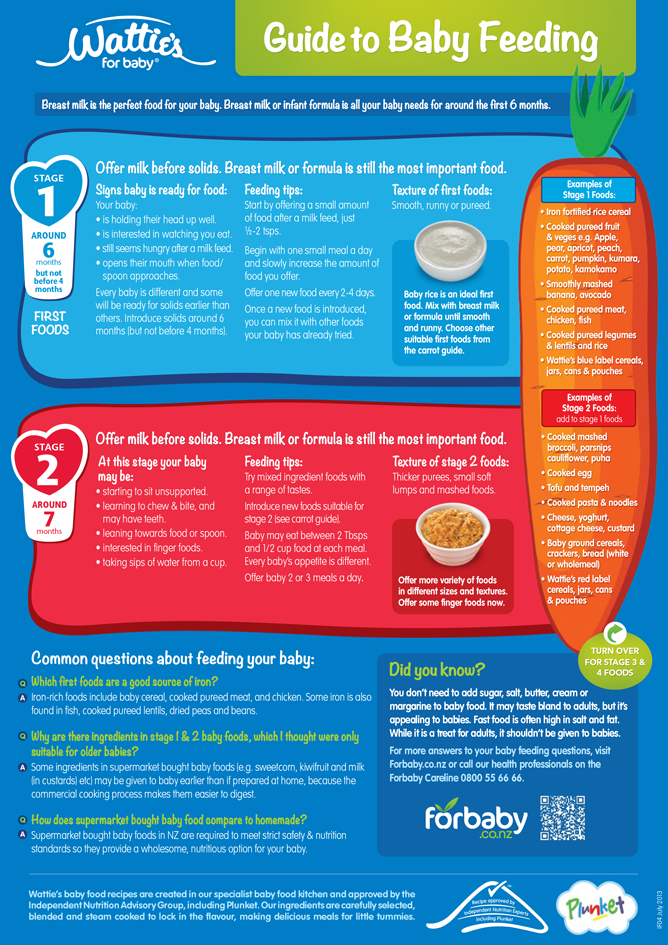
Breast milk varies in caloric content
When Shelly Hester and her colleagues analyzed 22 published studies on the metabolizable energy content of breast milk, the researchers were able to estimate the calories found per serving: About 65 calories per 100 milliliters (mL) of breast milk.
But hang on. That estimate is the average for milk expressed between 2 weeks and 6 weeks postpartum (Hester et al 2012).
Milk produced earlier is substantially less caloric. Colostrum, the milk produced during the first few days, has only about 53 calories per 100 mL. Then, between approximately 6 and 14 days postpartum, the caloric density increases slightly, averaging 58 calories per 100 mL (Hester et al 2012).
And milk produced later — after the 6 weeks postpartum — becomes increasingly caloric as time goes by. That’s because the fat content of breast milk tends to increase the longer a woman continues to nurse.
When researchers have tracked lactating mothers over time, they’ve found that the fat content in milk produced at 6 months is higher than it is at 3 months (Szabó et al 2010).
That’s a lot of variation already, but we’ve only scratched the surface because individual mothers vary substantially in the energy content of their milk. Studies indicate that individual woman may range widely in the fat content of their milk — from 2 grams per 100mL to 5 grams per mL (Institute of Medicine, National Academy of Sciences 1991).
And other research has identified some of the causes of this variation: Diet, body mass index, maternal age, socioeconomic status, and even smoking habits have been linked with differences in the amount of fat in breast milk (Daniel et al 2021; Innis 2014; Rocquelin et al 1998; Argov-Argaman et al 2017; Al-Tamer et al 2006; Agostoni et al 2003).
So it shouldn’t surprise us if there is no “one size fits all” infant feeding schedule that’s going to serve every baby equally well. Babies vary in their needs, and different breastfed babies may be receiving very different types of breast milk. Some get milk that is richer than average. Others get milk that is much lighter.
Others get milk that is much lighter.
And since babies can only drink so much before their stomachs are full, the fat content of milk is going to make a substantial difference in the calories they obtain from any given feeding session. Some babies will need more frequent feedings than other babies do, simply because their milk has fewer calories per serving.
Just as important, milk from the same mother can fluctuate in quality from day to day, and even from hour to hour (Khan et al 2013). So it’s possible that an infant feeding schedule that works pretty well one day might leave a baby dissatisfied on another.
Finally, it’s worth noting that the quality of breast milk changes during the course of a feed.
At the beginning of a feeding session, when the breast appears full, the milk that is released is relatively diluted and low in fat. Then, as the session continues, the breast takes on a softer, emptier appearance, and the milk changes.
The earlier “foremilk” gives way to a more concentrated, fattier “hindmilk” (Woolridge 1995), and you can see the difference in this photo.
The foremilk looks watery and bluish. The hindmilk — produced by the same breast, but later in the session — is ivory in color, and thicker.
Thus, if the adult terminates the breastfeeding session too soon, or forces a baby to switch breasts too soon, the baby will miss out on hindmilk (Woolridge and Fisher 1988).
Babies in this situation will fill up on a low calorie meal, and require more frequent feedings to obtain the energy they need.
In addition, they may be at higher risk for symptoms associated with consuming low quality milk. As breastfeeding expert Michael Woolridge (MD and PhD) has pointed out, low-fat milk can contribute to colic, vomiting, diarrhea, and flatulence in infants (Woolridge 1995).
What about formula-fed babies? Don’t they need us to impose restrictions — so they won’t overfeed?
You may have heard about research linking formula-feeding with rapid infant growth and an increased risk of childhood obesity. The links have been replicated in many studies, have prompted concern. Why are formula-fed babies more likely to become overweight?
The links have been replicated in many studies, have prompted concern. Why are formula-fed babies more likely to become overweight?
One answer is that formula might be too energy-dense for some babies (Hester et al 2012). But it also appears that the delivery system — drinking from a bottle — is a contributing factor.
For example, in one study of 1250 American infants, researchers found that bottle-feeding in early infancy was associated with a tendency to eat everything on offer, regardless of whether the babies consumed formula or breast milk.
The more frequently babies drank from bottles during their first 6 months, the more likely they were to become big eaters later. As toddlers, they were more likely to completely drain any bottle or cup given to them (Li et al 2010).
A smaller study conducted in the United Kingdom reports similar results (Brown and Lee 2012).
It’s not clear what this means, but we know that infants can extract milk more quickly from a bottle than they can from a breast.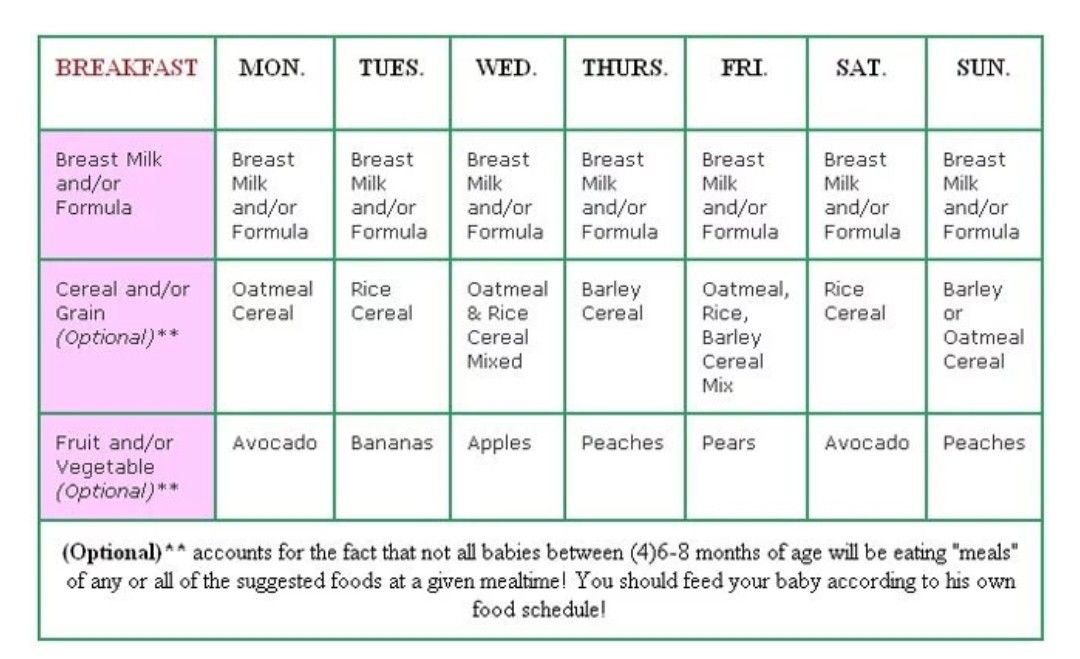
Perhaps the fast pace leads to consuming more during a feed, so babies become accustomed to taking in bigger meals.
Whatever the underlying cause, it invites the obvious question: Isn’t this a good reason to impose an infant feeding schedule? Aren’t bottle-fed babies better off if we restrict the timing of their meals?
The evidence suggests not.
For instance, experimental research indicates that babies are sensitive to internal cues of hunger and satiety. When allowed to feed on demand, both breastfed (Woolridge and Baum 1992) and formula-fed (Fomon et al 1975) infants adjust their intakes in response to the caloric content of their milk or formula.
And when researchers have tracked infant development over time, they haven’t found that feeding restrictions — including timed feeding schedules — reduce the risk of a child becoming overweight. On the contrary.
In one study, researchers found that scheduled feeding was a risk factor for rapid weight gain (Mihrshahi et al 2011). And — overall — research suggests that restrictive feeding is more likely than responsive feeding to lead to high weight gain (Gubbels et al 2011; DiSantis et al 2011b; Dinkevich et al 2015; Gross et 2014; Spill et al 2019).
And — overall — research suggests that restrictive feeding is more likely than responsive feeding to lead to high weight gain (Gubbels et al 2011; DiSantis et al 2011b; Dinkevich et al 2015; Gross et 2014; Spill et al 2019).
Surprising? Perhaps it shouldn’t be. These observations are consistent with studies of older children.
It appears that intrusive, restrictive rules about eating may interfere with the development of self-regulation. They may actually increase a child’s tendency to engage in emotional overeating (Jani et al 2015; Rodgers et al 2013), and lead to excessive weight gain (Tylka et al 2015).
So researchers suspect that imposing restrictions — like a strict infant feeding schedule — are counterproductive for preventing obesity.
Kids might learn to ignore their own hunger cues, and eat in response to social cues (“it’s time!”) or emotions (“I’ve been denied — now it’s time to make up for that”). By allowing infants to initiate feedings, we may be helping them develop a more healthy relationship with food.![]()
Other considerations: Do the effects of an infant schedule extend beyond matters of nutrition and energy regulation?
That’s an interesting question.
From birth, infants get distressed when their signals to nurse are ignored. And studies indicate brief, token acts of feeding can help newborns bounce back from stress.
Newborns cry less and show signs of reduced pain when they receive small amounts of milk, formula, or sucrose (see review by Shaw et al 2007; also Blass 1997a; Blass 1997b; Blass and Watt 1999; Barr et al 1999). The act of suckling is itself an analgesic (Blass and Watt 1999). And breastfeeding may be a painkiller and stress-reducer.
In one study, newborns subjected to a painful blood collection procedure cried much less if they were permitted to breastfeed (Gray et al 2002). They cried just 4% of time total procedure time, versus 43% for infants in a control group.
Babies who fed during the procedure also showed markedly reduced rates of grimacing (8% v. 50%), and their heart rates increased less (6 beats per minute v. 29 beats per minute).
50%), and their heart rates increased less (6 beats per minute v. 29 beats per minute).
Some of these differences may be attributable to the extra skin-to-skin contact that the breastfed babies got. But in a follow-up study, the researchers confirmed that breastfeeding was more soothing than skin-to-skin contact alone (Gray et al 2000; Gray et al 2002). And the authors noted that babies who were held without being fed tended to get frustrated, and required much more time to settle down (Gray et al 2002).
So what might happen to a baby who finds that her signals for quick comfort are routinely ignored?
While I’ve found no studies that bear directly on this question, responsive care has been linked with development of better stress regulation skills — even among highly irritable, “at risk” babies.
Moreover, a variety of studies suggest that sensitive, responsive parenting contributes to secure attachment relationships and better child outcomes.
And there is intriguing research regarding cognitive development.
In what is perhaps the largest study yet to investigate the effects of an infant feeding schedule, Maria Iacovou and Almudena Sevilla (2013) tracked the development of more than 10,000 British children — breastfed and bottle-fed alike — from birth to age 14.
There were no experimental manipulations. The researchers merely noted whether babies had been fed on schedule or “on demand”, and then followed their cognitive and academic progress. And the results? They favored feeding “on demand”.
At every age, kids who’d been subjected to an infant feeding schedule performed more poorly on standardized tests. Moreover, their IQs were, on average, 4.5 points lower.
Correlation doesn’t prove causation, of course, and this is just one study. It needs to be replicated.
But it’s interesting to note that the study’s results remained much the same even after researchers controlled for a variety of potential confounds, like parents’ education levels, economic factors, health, breastfeeding, maternal smoking, and the children’s exposure to negative discipline tactics.
There wasn’t any obvious reason for the difference between groups. Just the distinction between feeding on cue and following an infant feeding schedule.
Summing up: What do we really know?
As with most science, we still have a lot left to learn.
We don’t yet understand all the determinants of breast milk quality, or why the composition of breast milk changes over time.
We don’t yet understand all the causes of increased obesity risk in formula-fed and bottle-fed infants.
And it isn’t yet clear how much impact an infant feeding schedule might have over the long-term. In particular, we need more research on the possible effects an infant feeding schedule might have on stress regulation and cognitive development.
Meanwhile, what we do know is that human beings exhibit the characteristics of continual feeders, and it’s a sure bet that relatively frequent, “on demand” feedings have been the historic and evolutionary norm for our species.
It’s also clear that breast milk can vary substantially in fat composition and caloric density, so that babies will benefit from being able to schedule the timing of their own feeds.![]()
And all babies — whether they consume breast milk or formula — experience fluctuations in their needs for fluids and energy. When we are responsive to their cues of hunger and thirst, we’re more likely to meet these needs.
More reading
How can you tell if a newborn is hungry? Find answers to this and other questions in my article, “The newborn infant feeding schedule: A review of the evidence against regimented feedings.”
In addition, you can read more about this topic in “Breastfeeding on demand: A cross-cultural perspective.” And for more information about the composition of breast milk, read this Parenting Science article.
Wondering if you can time your baby’s meals to optimize sleep at night? Check out my article, “Dream feeding: An evidence-based guide to helping babies sleep longer.”
What about solid foods? When and how should you introduce your baby to solids? This Parenting Science article will guide you through the process, and answer interesting questions about infant behavior, adding spices to foods, and more.
And are some other Parenting Science articles that might interest you:
- Baby sleep patterns for the science-minded
- The newborn senses: What can babies feel, see, hear, smell, and taste
- Stress in babies: How to keep babies calm, happy, and healthy
- Motor milestones: How do babies develop during the first two years?
References: The best infant feeding schedule
Agostoni C, Marangoni F, Grandi F, Lammardo AM, Giovannini M, Riva E, Galli C. 2003. Earlier smoking habits are associated with higher serum lipids and lower milk fat and polyunsaturated fatty acid content in the first 6 months of lactation. Eur J Clin Nutr. 57(11):1466-72.
Al-Tamer YY and Mahmood AA.2006. The influence of Iraqi mothers’ socioeconomic status on their milk-lipid content. Eur J Clin Nutr. 60(12):1400-5.
American Academy of Pediatrics. 2015. Caring for your baby and young child: Birth to age 5. 7th Edition. T. Altmann (ed). Bantam.
Argov-Argaman N, Mandel D, Lubetzky R, Hausman Kedem M, Cohen BC, Berkovitz Z, Reifen R. 2017. Human milk fatty acids composition is affected by maternal age. J Matern Fetal Neonatal Med 30(1):34-37.
2017. Human milk fatty acids composition is affected by maternal age. J Matern Fetal Neonatal Med 30(1):34-37.
Barr RG, Pantel MS, Young SN, Wright JH, Hendricks LA, Gravel R. 1999. The response of crying newborns to sucrose: is it a “sweetness” effect? Physiol. Behav 66: 409-417.
Bergmeier HJ, Skouteris H, Haycraft E, Haines J, Hooley M. 2015. Reported and observed controlling feeding practices predict child eating behavior after 12 months. J Nutr. 145(6):1311-6.
Blass EM. 1997a Milk-induced hypoanalgesia in human newborns. Pediatrics 99: 825-829.
Blass EM. 1997b. Infant formula quiets crying newborns. Journal of Dev Behavioral Pediatrics. 18:162-165.
Brown A and Lee M. 2012. Breastfeeding during the first year promotes satiety responsiveness in children aged 18-24 months. Pediatr Obes. 7(5):382-90.
Chen TL, Chen YY, Lin CL, Peng FS, Chien LY. 2020. Responsive Feeding, Infant Growth, and Postpartum Depressive Symptoms During 3 Months Postpartum. Nutrients. 12(6):1766.
12(6):1766.
Daly SE, DiRosso A, Owens RA and Hartmann PE. 1993. Degree of breast emptying explains fat content, but not fatty acid composition, of human milk. Exp Physiol 78: 741-755.
Daniel AI, Shama S, Ismail S, Bourdon C, Kiss A, Mwangome M, Bandsma RHJ, O’Connor DL. 2021. Maternal BMI is positively associated with human milk fat: a systematic review and meta-regression analysis. Am J Clin Nutr. 113(4):1009-1022.
Dinkevich E, Leid L, Pryor K, Wei Y, Huberman H, Carnell S. 2015. Mothers’ feeding behaviors in infancy: Do they predict child weight trajectories? Obesity (Silver Spring). 23(12):2470-6.
Disantis KI, Collins BN, Fisher JO, and Davey A. 2011a. Do infants fed directly from the breast have improved appetite regulation and slower growth during early childhood compared with infants fed from a bottle? Int J Behav Nutr Phys Act. 8:89.
Disantis KI, Hodges EA, Johnson SL, and Fisher JO. 2011b. The role of responsive feeding in overweight during infancy and toddlerhood: a systematic review. International Journal of Obesity 35: 480–492
International Journal of Obesity 35: 480–492
Fomon SJ, Filmer, Jr., JA, Thomas LN, Anderson TA and Nelson SE. 1975. Influence of formula concentration on caloric intake and growth of normal infants. Acta Pediatrica Scandinavica 64: 172-181.
Fuglestad AJ, Demerath EW, Finsaas MC, Moore CJ, Georgieff MK, Carlson SM. 2017. Maternal executive function, infant feeding responsiveness and infant growth during the first 3 months. Pediatr Obes. 12 Suppl 1:102-110.
Gubbels JS, Thijs C, Stafleu A, van Buuren S, Kremers SP. 2011. Association of breast-feeding and feeding on demand with child weight status up to 4 years. Int J Pediatr Obes. 6(2-2):e515-22.
Gray L, Miller LW, Philipp BL, Blass EM. 2002. Breastfeeding is analgesic in healthy newborns. Pediatrics 109: 590-593.
Gray L, Watt L, Blass EM. Skin-to-skin contact is analgesic in healthy newborns. Pediatrics 105(1).
Gross RS, Mendelsohn AL, Fierman AH, Hauser NR, Messito MJ. 2014. Maternal infant feeding behaviors and disparities in early child obesity. Child Obes. 10(2):145-52.
Child Obes. 10(2):145-52.
Hausman Kedem M, Mandel D, Domani KA, Mimouni FB, Shay V, Marom R, Dollberg S, Herman L, Lubetzky R. 2013. The effect of advanced maternal age upon human milk fat content. Breastfeed Med. 8(1):116-9.
Hester SN, Hustead DS, Mackey AD, Singhal A, and Marriage BJ. 2012. Is the macronutrient intake of formula-fed infants greater than breast-fed infants in early infancy? Journal of Nutrition and Metabolism: 891201.
Iacovou M and Sevilla A. 2013. Infant feeding: the effects of scheduled vs. on-demand feeding on mothers’ wellbeing and children’s cognitive development. Eur J Public Health. 23(1):13-9.
Illingworth RS, Stone DHG, Jowett JH and Scott JF. 1952. Self-demand feeding in a maternity unit. Lancet 1: 683-687.
Innis SM. 2014. Impact of maternal diet on human milk composition and neurological development of infants. Am J Clin Nutr. 99(3):734S-41S.
Institute of Medicine, National Academy of Sciences. 1991. Nutrition during lactation. Washington, DC: National Academy Press.
Washington, DC: National Academy Press.
Jackson DA, Imong SM, Silpraset A, Preunglumpoo Ruckphaopunt S, Williams AF, Woolridge MW, Baum JD, and Amatayakul K. 1988. Circadian variation in fat concentration of breastmilk in rural Northern Thailand. British Journal of Nutrition 59: 365-371.
Jani R, Mallan KM, Daniels L.2015. Association between Australian-Indian mothers’ controlling feeding practices and children’s appetite traits. Appetite 84:188-95
Jenness 1974. Biosynthesis and composition of milk. Journal of investigative dermatology. 63: 109-118.
Kersting M and Dulon M. 2001. Assessment of breastfeeding promotion in hospitals and follow up survey of mother-infant pairs in Germany: The Su-Se study. Public Health Nutrition 5(4): 547-552.
Khan S, Hepworth AR, Prime DK, Lai CT, Trengove NJ, Hartmann PE. 2013. Variation in fat, lactose, and protein composition in breast milk over 24 hours: associations with infant feeding patterns. J Hum Lact. 29(1):81-9
Konner M. 2005. Hunter-gatherer infancy and childhood: The !Kung and others. In: Hunter-gatherer childhoods: Evolutionary, developmental and cultural perpectives. BS Hewlett and ME Lamb (eds). New Brunswick: Transaction Publishers.
2005. Hunter-gatherer infancy and childhood: The !Kung and others. In: Hunter-gatherer childhoods: Evolutionary, developmental and cultural perpectives. BS Hewlett and ME Lamb (eds). New Brunswick: Transaction Publishers.
Li R, Fein SB, Grummer-Strawn LM. 2010. Do infants fed from bottles lack self-regulation of milk intake compared with directly breastfed infants? Pediatrics. 125(6):e1386-93.
Mandel D, Lubetzky R, Dollberg S, Barak S, Mimouni FB. 2005. Fat and energy contents of expressed human breast milk in prolonged lactation. Pediatrics. 116(3):e432-5.
Mihrshahi S, Battistutta D, Magarey A, Daniels LA. 2011. Determinants of rapid weight gain during infancy: baseline results from the NOURISH randomised controlled trial. BMC Pediatr. 11:99.
Prentice AM and Prentice A. 1988. Energy costs of lactation. Annual review of nutrition 8: 63-79.
Prentice A, Prentice AM and Whitehead RG. 1981. Breast-milk concentrations of rural African women I. Short-term variations within individuals. British Journal of Nutrition 45: 483-494.
British Journal of Nutrition 45: 483-494.
Rocquelin G, Tapsoba S, Dop MC, Mbemba F, Traissac P, Martin-Prével Y. 1998. Lipid content and essential fatty acid (EFA) composition of mature Congolese breast milk are influenced by mothers’ nutritional status: impact on infants’ EFA supply. Eur J Clin Nutr. 52(3):164-71
Rodgers RF, Paxton SJ, Massey R, Campbell KJ, Wertheim EH, Skouteris H, Gibbons K. 2013. Maternal feeding practices predict weight gain and obesogenic eating behaviors in young children: a prospective study. Int J Behav Nutr Phys Act. 10:24
Saxon TF, Gollapalli A, Mitchell MW, and Stanko S. 2002. Demand feeding or schedule feeding: infant growth from birth to 6 months. Journal of reproductive and infant psychology 20(2): 89-99.
Severn Nelson EA, Schiefenhoevel W, and Haimerl F. 2000. Child care practices in nonindustrial societies. Pediatrics 105: 75-79.
Shah PS, Aliwalas L, and Shah V. 2007. Breastfeeding or breast milk to alleviate procedural pain in neonates: a systematic review.![]() Breastfeeding medicine 2:74-82.
Breastfeeding medicine 2:74-82.
Spill MK, Callahan EH, Shapiro MJ, Spahn JM, Wong YP, Benjamin-Neelon SE, Birch L, Black MM, Cook JT, Faith MS, Mennella JA, Casavale KO. 2019. Caregiver feeding practices and child weight outcomes: a systematic review. Am J Clin Nutr. 109(Suppl_7):990S-1002S.
Szabó E, Boehm G, Beermann C, Weyermann M, Brenner H, Rothenbacher D, Decsi T. 2010. Fatty acid profile comparisons in human milk sampled from the same mothers at the sixth week and the sixth month of lactation. J Pediatr Gastroenterol Nutr. 50(3):316-20.
Tilden CD and Oftedal OT. 1997. Milk composition reflects pattern of maternal care in prosimian primates. American Journal of Primatology 41: 195-211.
Tylka TL, Lumeng JC, Eneli IU. 2015. Maternal intuitive eating as a moderator of the association between concern about child weight and restrictive child feeding. Appetite 95:158-65.
Ventura AK, Inamdar LB, Mennella JA. 2015. Consistency in infants’ behavioural signalling of satiation during bottle-feeding. Pediatr Obes. 10(3):180-7.
Pediatr Obes. 10(3):180-7.
Wojcik KY, Rechtman DJ, Lee ML, Montoya A, Medo ET. 2009. Macronutrient analysis of a nationwide sample of donor breast milk. J Am Diet Assoc. 109(1):137-40.
Woolridge MW. 1995. Baby-controlled breastfeeding: Biocultural implications. In: Breastfeeding: Biocultural perspectives. P. Stuart-Macadam and KA Dettwyler (eds). New York: Aldine deGruyter.
Woolridge MW and Baum JD. 1992. Infant appetite-control and the regulation of breast milk supply. Children’s hospital quarterly 3:133-119.
Woolridge MW and Fisher C. 1988. Colic, ‘Overfeeding,’ and Symptoms of Lactose Malabsorption in the Breast-Fed Baby: A Possible Artifact of Feed Management. Lancet 13: 382-384.
Note: Portions of this article, “Jettisoning the infant feeding schedule: Why babies are better off feeding on cue,” are taken from an earlier Parenting Science article, “The infant feeding schedule: Why babies benefit from feeding on demand.” The material here has been updated and substantially revised.
For more references pertaining to the infant feeding schedule, see my article on breastfeeding on demand.
Image credits for “The best infant feeding schedule”
image of infant breastfeeding by istock / Jomkwan
Content of “The best infant feeding schedule” last modified 5/2021
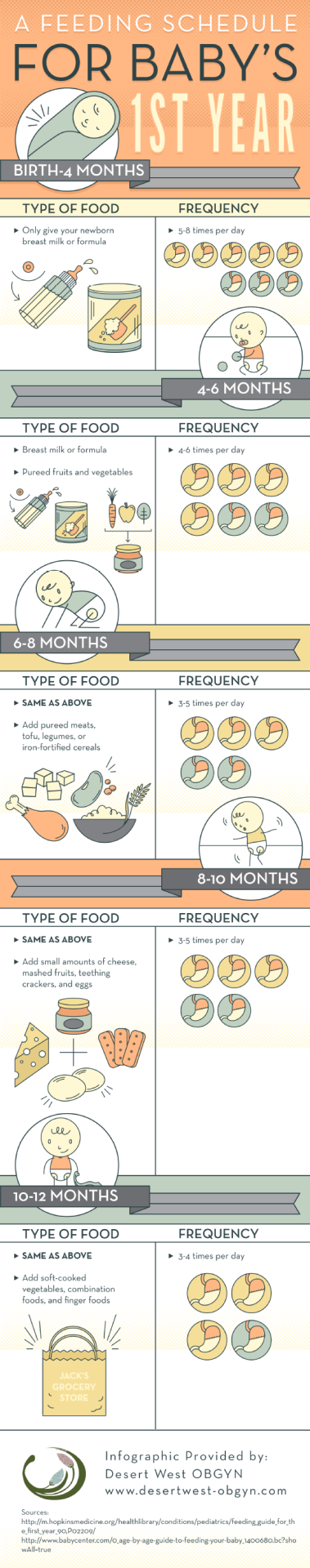
Tips for the First Year
Every baby may get hungry on their own unique schedule. That said, most infants in the first months of life will eat every 2-4 hours, depending if they are nursing or drinking formula. Once they eat solids, they’ll gradually drink less.
Eat, sleep, pee, poop, repeat. Those are the highlights of a day of the life of a brand-new baby.
And if you’re a new parent, it’s the eating part that may be the source of many of your questions and worries. How many ounces should your baby take? Do you wake a sleeping baby to eat? Why do they seem hungry all the time? When can your child start solids?
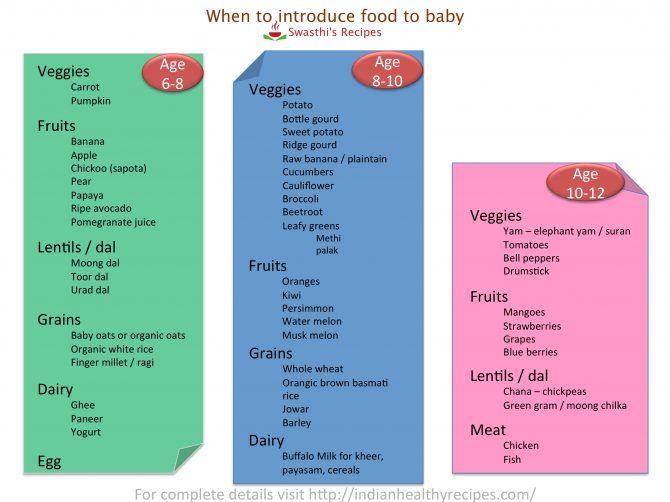
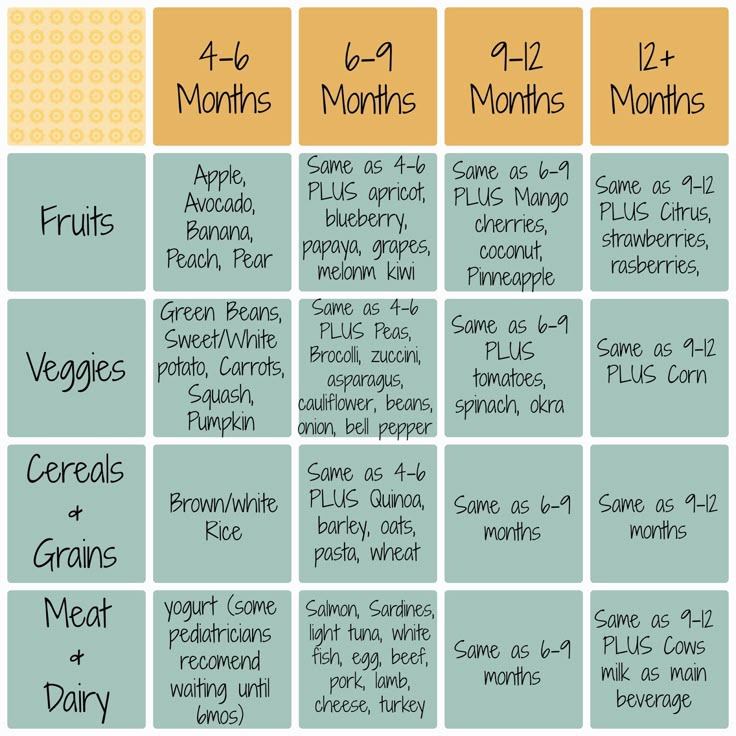
Questions abound — despite Grandma’s insistence, the answers have changed since you were a tot. It’s now recommended that newborns, even formula-fed ones, eat on demand (consider it good preparation for the teenage years) and that babies wait to start solid foods until they’re 4 to 6 months old.
It’s now recommended that newborns, even formula-fed ones, eat on demand (consider it good preparation for the teenage years) and that babies wait to start solid foods until they’re 4 to 6 months old.
On day one of life, your baby’s stomach is the size of a marble and can only hold 1 to 1.4 teaspoons of liquid at a time. As your baby gets older, their stomach stretches and grows.
It’s hard (or impossible, really) to know how much milk your baby is taking in while breastfeeding. But if you’re bottle feeding due to any number of valid reasons, it’s a bit easier to measure.
Here, from the American Academy of Pediatrics (AAP), a typical feeding schedule for bottle-fed babies.
| Age | Ounces per feeding | Solid foods |
|---|---|---|
| Up to 2 weeks of life | .5 oz. in the first days, then 1–3 oz. | No |
| 2 weeks to 2 months | 2–4 oz. | No |
| 2–4 months | 4-6 oz. | No |
| 4–6 months | 4–8 oz. | Possibly, if your baby can hold their head up and is at least 13 pounds. But you don’t need to introduce solid foods yet. |
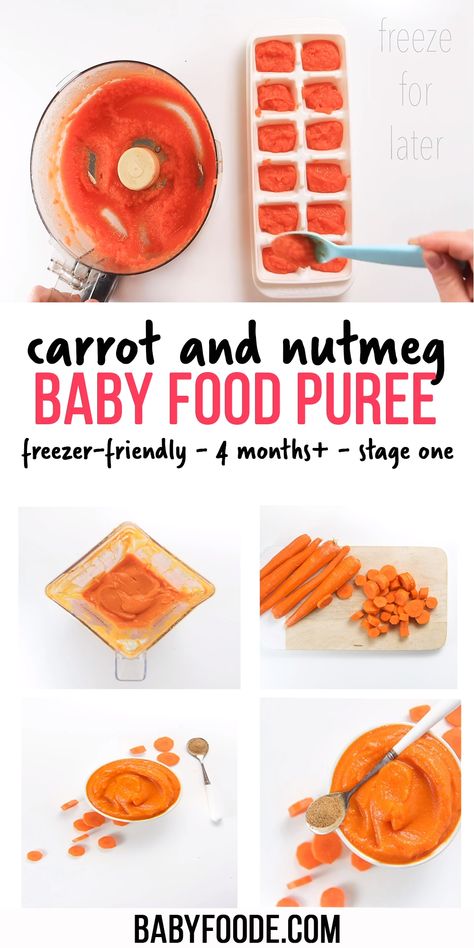
| 6–12 months | 8 oz. | Yes. Start with soft foods, like one-grain cereals and pureed vegetables, meats, and fruits, progressing to mashed and well-chopped finger foods. Give your baby one new food at a time. Continue supplementing with breast or formula feedings. |
Every baby is unique — but one thing that’s pretty consistent is that breastfed babies eat more frequently than bottle-fed ones. That’s because breast milk is easily digested and empties from the stomach a lot quicker than formula.
Breastfed babies
There’s no rest for the weary. According to La Leche League International, you should begin nursing your baby within 1 hour of birth and provide about 8 to 12 feedings daily in the first few weeks of life (yeah, we’re exhausted for you).
At first, it’s important not to let your baby go more than 4 hours without feeding. You’ll likely need to wake them up if necessary, at least until breastfeeding is well established and they’re gaining weight appropriately.
As your baby grows and your milk supply amps up, your baby will be able to take in more milk in less time at one feeding. That’s when you might start to notice a more predictable pattern.
- 1 to 3 months: Your baby will feed 7 to 9 times per 24 hours.
- 3 months: Feedings take place 6 to 8 times in 24 hours.
- 6 months: Your baby will feed around 6 times a day.
- 12 months: Nursing may drop to about 4 times a day. The introduction of solids at about 6 months helps to fuel your baby’s additional nutritional needs.
Keep in mind that this pattern is just one example. Different babies have different paces and preferences, along with other factors that influence the frequency of feedings.
Bottle-fed babies
Like breastfed babies, bottle-fed newborns should eat on demand. On average, that’s about every 2 to 3 hours. A typical feeding schedule may look like this:
On average, that’s about every 2 to 3 hours. A typical feeding schedule may look like this:
- Newborn: every 2 to 3 hours
- At 2 months: every 3 to 4 hours
- At 4 to 6 months: every 4 to 5 hours
- At 6+ months: every 4 to 5 hours
For both breastfed and bottle-fed babies
- Don’t give liquids other than formula or breast milk to babies under a year old. That includes juices and cow’s milk. They don’t provide the right (if any) nutrients and can be upsetting to your baby’s tummy. Water can be introduced around 6 months when you start offering a cup.
- Don’t add baby cereal to a bottle.
- It can create a choking hazard.
- A baby’s digestive system isn’t mature enough to handle cereal until about 4 to 6 months of age.
- You could overfeed your baby.
- Don’t give your baby any form of honey until after their first birthday. Honey can be dangerous for a baby, occasionally causing what’s called infant botulism.

- Do adjust your expectations based on your baby and their unique needs. Premature babies are likely to follow feeding patterns according to their adjusted age. If your baby has challenges like reflux or failure to thrive, you may need to work with your doctor on the appropriate feeding schedule and amount they should be eating.
Schedules are the holy grail of every parent. Your child will naturally start to fall into a feeding pattern as their tummy grows and they can take in more breast milk or formula at one sitting. This may begin to happen between 2 and 4 months of age.
For now, though, focus on learning your baby’s hunger cues, such as:
- rooting around your chest, looking for a nipple.
- putting their fist in their mouth
- smacking or licking their lips
- fussing that can escalate quickly (don’t wait until your baby’s hangry to feed them)
Once your baby is a few months old, you may be able to introduce a sleep/feed schedule that works for you.
Let’s say, for example, your 4-month-old wakes every 5 hours for a feeding. That means if you feed at 9 p.m., your baby wakes around 2 a.m. But if you wake and feed the baby at 11 p.m., just before you go to bed, they may not rouse until 4 a.m., giving you a decent chunk of nighttime winks.
In general, if your baby seems hungry, feed them. Your baby will naturally eat more frequently during growth spurts, which typically occur around 3 weeks, 3 months, and 6 months of age.
Some babies will also “cluster feed,” meaning they’ll feed more frequently during certain periods and less at others. For example, your baby may cluster feed during the late afternoon and evening and then sleep longer at night (yay!). This is more common in breastfed babies than bottle fed babies.
Worried about overfeeding? While this isn’t really possible to do with an exclusively breastfed baby, you can overfeed a baby who’s taking a bottle — especially if they’re sucking on the bottle for comfort. Follow their hunger cues, but talk to your pediatrician if you’re worried your little one may be overeating.
Follow their hunger cues, but talk to your pediatrician if you’re worried your little one may be overeating.
Your baby is probably ready for solids if they’re 4 to 6 months old and:
- have good head control
- seem interested in what you’re eating
- reach for food
- weigh 13 or more pounds
Which food to start with? The AAP now says it doesn’t really matter much in what order you introduce foods. The only real rule: Stick with one food for 3 to 5 days before offering another. If there’s an allergic reaction (rash, diarrhea, vomiting are common first signs), you’ll know which food is causing it.
As your baby grows, move from pureed baby food to ones that have more texture (for example, mashed banana, scrambled egg, or well-cooked, chopped pasta). This generally happens around 8 to 10 months of age.
Your supermarket offers a variety of baby food products, but if you want to make your own, keep it sugar and salt free. Additionally, at this stage, don’t feed your baby anything that could be a choking hazard, including:
- hard foods, such as popcorn or nuts
- hard, fresh fruits, like apples; cook to soften or chop into very small pieces
- any meat that isn’t well cooked and very well chopped (this includes hot dogs)
- cheese cubes
- peanut butter (though talk to your pediatrician about this one — and the benefits of introducing diluted peanut butter before the age of 1)
As your baby nears their first birthday, they should be eating a variety of foods and taking in about 4 ounces of solids at each meal.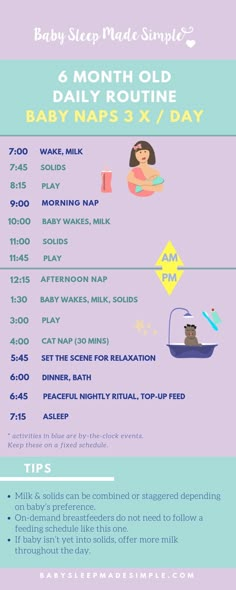 Continue to offer breast milk or formula. By 8 months, babies are drinking about 30 ounces a day.
Continue to offer breast milk or formula. By 8 months, babies are drinking about 30 ounces a day.
Oh yeah, and buy some stock in a company that makes stain-fighting laundry detergent. It’ll pay for college.
Babies aren’t cookie cutter. Some will gain weight easily, while others will have problems. Things that can affect a baby’s weight gain include:
- having a birth defect like a cleft lip or palate, which creates problems feeding
- having a milk protein intolerance
- being premature
- being fed with a bottle versus the breast
A 2012 study of more than 1,800 babies found that the infants who were fed with a bottle — regardless of whether the bottle contained breast milk or formula — gained more weight in the first year than babies who nursed exclusively.
Your baby’s doctor is the best one to advise you on a healthy weight range for your baby.
How, when, and what to feed a baby are top worries of every parent — but there’s good news: Most babies are pretty good judges of when they’re hungry and when they’re full — and they’ll let you know it.
You just need to present them with the right choices at the right time and pay attention to their cues. If you have any questions or concerns, your pediatrician is there to help you along the way.
Breastfeeding on demand
You can often hear from a nursing mother: "I feed on demand, my baby requires a breast every 3.5 hours." Or: “I have always fed on demand. In a year, we already had 1 feeding in the evening, and my child calmly refused to breastfeed. Before talking about the demand of the child, it is necessary to find out what modern women mean when they say - "I breastfeed."
Modern mothers consider breastfeeding necessary for feeding their baby. Just for feeding. Breast milk is food, the mother supplies the baby with the nutrients necessary for growth and development. When a baby suckles at the breast, he eats. Breastfeeding makes sense only as a process of supplying proteins, fats, carbohydrates, vitamins and microelements.
During suckling, the baby receives the nutrients it needs with mother's milk. This is the absolute truth. There is another unconditional truth, which is not given any importance in modern society, it is not taken into account and is not considered. Breastfeeding for a child is communication with the mother. We need to figure out how the child understands feeding on demand? Can he understand anything at all? Is there any difference for him how he is fed, for 15-20 minutes after 3.5 hours or in some other way?
What is on-demand feeding
On-demand feeding of a newborn baby means putting it to the breast for every squeak or search. Squeak and search movements in newborns, even as early as the second or third day of life, begin to appear much more often than after 3.5 or 2.5 hours. The need for attachments increases rapidly, and by the 10-12th day of life, the need to attach to a child may occur 15-16 or more times a day. Applications vary in duration. The baby can fall asleep and sleep while sucking for, for example, 1. 5-2 hours. Can release the breast after 1-2 minutes. And then ask her again. Why does a child need such frequent contact with his mother's breast?
5-2 hours. Can release the breast after 1-2 minutes. And then ask her again. Why does a child need such frequent contact with his mother's breast?
That's why. Being in the mother's belly, in a calm, familiar environment, listening to the noises of the mother's body, being in a warm, cramped, confined space, the baby sucked his fist, fingers, loops of the umbilical cord, swallowed amniotic fluid. Learned to suck and swallow. After birth, experiencing discomfort for any, the most insignificant reason, the baby tries to get rid of it. You can get rid of discomfort by getting into the usual conditions of a comfortable stay. The only place where the baby after birth can feel the sensations familiar to him is in the arms of the mother. The only familiar action is sucking. The only familiar taste and smell is the taste and smell of milk and lube in the areola. Milk and lubricant have an odor and taste similar to the taste and smell of amniotic fluid. Therefore, experiencing discomfort, the baby squeaks, or begins to look for an object to suck with his mouth. Ideally, it is immediately applied to the chest. The baby becomes warm, cramped, he hears the beating of his mother's heart, breathing, grumbling in the intestines, he sucks and feels the familiar taste and smell. If such an action happens constantly, the baby gains confidence, no matter what happens, he will solve all his problems with his mother. The place of comfort is now under the breast, and you can suck on the breast.
Ideally, it is immediately applied to the chest. The baby becomes warm, cramped, he hears the beating of his mother's heart, breathing, grumbling in the intestines, he sucks and feels the familiar taste and smell. If such an action happens constantly, the baby gains confidence, no matter what happens, he will solve all his problems with his mother. The place of comfort is now under the breast, and you can suck on the breast.
This whole process is biologically justified. A newborn child does not feel the feeling of hunger, this feeling is not formed in him. It will begin to form at about two months of age. How to feed a creature that does not experience hunger ?! How to encourage him to take some action to get food? This can be done only at the expense of some other incentives. This stimulus for the newborn is constant bodily discomfort, thanks to which he wants to suckle all the time! The most intense, frequent and prolonged sucking in infants is observed in the first two or three months of life. It is in these first months that the main weight gain of the baby occurs.
It is in these first months that the main weight gain of the baby occurs.
Feeding in the first month
Baby falls asleep with breast in mouth, sleeps sucking for a while. Falling asleep deeply, lets go of the chest. After sleeping for a while, he wakes up, and is applied on waking. After sleep, he can stay awake for some time, for example, an hour and a half. During wakefulness, he may feel discomfort 2-3 times, for example, from a completely natural desire to pee, and having called his mother for help, having kissed for a couple of minutes, he will do his deeds. Then he will want to sleep, feel discomfort and, kissing his chest, will again fall asleep sucking. After some time, he will wake up and attach again. Then again a little "walk". And after some time, he will fall asleep at the chest again.
The daytime naps of a one-month-old infant feeding on demand vary in duration and number. There can be 4-6 dreams during the day, and they can last from 5-15 minutes to 2-2. 5 sometimes 3 hours. "Around" each dream, the baby is applied to the chest, and applied between dreams several times. At night, the child falls asleep at the breast. Usually in the early morning hours, he begins to fuss and apply. In the morning, he almost never fully wakes up. The baby sleeps, from time to time, sucking on his mother's breast. Waking up in the morning, the baby is again applied to the chest. If you count all the attachments that have happened in a baby of one month of age, then approximately 16-20 attachments are obtained. This is how a newborn human cub behaves if it is given the opportunity to behave in accordance with physiological and psychological needs, which, by the way, are genetically determined. The child of the first months of life does not separate his personality from the personality of the mother and from her breast. Mom and her breasts, and everything connected with them, are the universe of the baby and himself.
In most cases, a modern woman, being afraid to “accustom a child to hands”, strives to limit his requests for suckling. A pacifier and a bottle of tea or water come to her aid in this matter. They, too, can be sucked ... The need for sucking seems to be satisfied. But only the need for communication with the mother during suckling is not satisfied, the peculiar chain of mutual assistance and cooperation between mother and baby is destroyed, the formation of maternal affection and concentration is disrupted. Is the difference in the two actions noticeable to the reader: the baby cried, the mother took him, put him to her chest and started rocking him, or gave him a pacifier and started rocking the stroller, even with the words “Why are you crying, my sun?”
The modern woman who gives a pacifier and pumps a stroller is not a bad person deliberately harming an infant. She is simply in captivity of prejudices regarding the relationship between mother and baby. She does not know how to behave correctly, does not know what to do in accordance with the natural needs of the child. If you tell her what the child really needs, she will exclaim in horror: “What is it, don’t let him get away with?!” Indeed, the child of the first months of life must not be let off the hook. For a woman who does not know how to comfortably carry a baby, and who does not know how to feed him in various positions (sitting, lying, standing and even moving), this can be very difficult. Especially if she is not sure of the correctness of her actions.
An action that should become automatic for the mother of a newborn: when the baby cries or shows other signs of anxiety, put the baby to the breast.
What's next?
The baby is growing. A fairly stable rhythm of daytime sleep begins to form in him, and a 3-4-month-old baby behaves quite differently from a newborn. Feeding on demand at this age looks something like this...
- At three months, the baby has 10-12 feeds during the day and 2-4 at night. There are frequent applications for a short time, but their number is reduced. There may be a long night break in feedings, about 5 hours, but this is very rare. Much more often the night break is 2.5-3.5 hours. By this age, the baby's body is noticeably rounded.
- At four months, the baby begins to breastfeed noticeably less frequently. The main feedings are associated with sleep: the baby suckles before bedtime, during awakening and during sleep, both daytime and nighttime. In this regard, he has a fairly accurate feeding regimen. And many babies stop breastfeeding when they wake up after daytime sleep, sometimes as early as 2.5-3 months.
- At five months, the baby has 8-10 daytime feedings and 2-3 nighttime, attachments as well as in the fourth month of life, are organized around dreams - the baby eats when going to bed and some babies suck during awakening.
- At six months, the feeding regimen changes. The most active sucking shifts to the last 2-3 hours before waking up from a night's sleep. The period of daytime wakefulness can be divided into two periods: in the morning, when the baby sucked during the night is rarely applied to the breast, and in the evening, when attachments become very frequent. In total, there can be 7-10 day applications and 3-4 night applications.
At this age, the baby begins a period of acquaintance with new food - pedagogical complementary foods. Sometimes there are attachments associated with the introduction of complementary foods, the baby “washes down” samples of new food with mother's milk. But many children do not want to drink complementary foods. When complementary foods are introduced to an on-demand baby, it is never meant to replace feedings with complementary foods. This is practically impossible, because the main feedings of the baby are associated with sleep, and mother's breakfasts, lunches and dinners, during which the baby gets acquainted with new food, are located between the baby's dreams, during his wakefulness.
- At seven months, the frequency of application is about the same.
- At eight months, the feeding regimen changes. Since the baby shows high motor activity and is very busy exploring the surrounding space, in the daytime he forgets to breastfeed. In this regard, the number of daily feedings can be reduced to 6-8 times.
The baby compensates for the reduction in daytime feedings by increasing the frequency and duration of nighttime feedings up to 6 times.
- In the second half of the year, babies who stopped breastfeeding when waking up after daytime naps recall this habit again. The baby’s daytime sleep in the second half of life, as well as in the region of a year and older, looks something like this: the baby falls asleep sucking, sleeps quietly for a while, for example 1-1.5 hours, then starts tossing and turning, fiddling, worrying, at this moment the mother lies down next to , gives him a breast and the baby can fill up 10-15-30 minutes sucking. Mom may well use this time for her own rest - lie down, read, while the baby sleeps while sucking. I know my mother, a lover of embroidery, who used this time specifically for embroidery ...
- Breastfeeding becomes more frequent at nine to ten months. In the daytime, this is 4-6 full feedings and about the same number of attachments for various reasons.
The baby has new reasons for attachment. If, during active actions to explore the world, the baby stuffs a bump or gets scared, he calms down with his mother's breast. There may be situations when you can comfort the baby by sitting next to him and hugging him. At night, 4-6 feedings remain, the baby begins to suckle more actively in the morning between 3 and 8 hours.
- At eleven months, a baby can already have 2-3 complete complementary foods. Initiation to adult food in the mind of a child is not associated with breastfeeding: attachment to the mother's breast is something other than the desire to get enough of the product they like. As a rule, after the baby has eaten, he feels the need to attach himself to the breast. The number of daily feedings remains the same in the child, but the number of short-term attachments increases. There are active mid-morning feedings between 4 and 8 o'clock in the morning.
- At ten or twelve months, the baby, if he is already walking, can sometimes breastfeed every time he comes to his mother, i.
e. about every 15-30 minutes. Attachments around dreams and night sucking persist. Therefore, if a mother says that a child suckles once or twice a day, this means that there is no feeding at the request of the child. There are restrictions imposed by the mother, with which the baby has come to terms. He treats breast sucking like food, sucks on a pacifier or a finger to fall asleep or soothe, or falls asleep just like that, without calming down.
- At twelve months, the baby is applied in about the same way.
- At the age of one and a half years, there may already be one daytime nap, so there are fewer attachments associated with sleep. Preserved for morning sucking. The baby is very free with his mother's breasts. Sometimes it happens that he comes up to suck just for pleasure. For example, like this: he comes up, climbs on his knees, looks into his mother’s face, smiles, starts to swarm in his shirt, gets breasts, smiles at his breasts, sucks for 30 seconds and leaves.
As for the number of feedings per day when feeding a child on demand, their number is almost never less than 12. A newborn has 12 or more attachments, mostly they are all associated with dreams. And a child, say 1.5-2 years old, can also have about 12 attachments, only 3-4 are associated with sleep, and the rest are short-term attachments for various reasons. I suggest to all mothers reading this text - do not count the application, do not notice their duration. Breastfeed your baby as often as he asks, when you feel the need to.
Moms who don't think about breastfeeding without looking at the clock may get the impression that when breastfeeding on demand, the mother can do nothing but feed the baby. This is wrong. After the birth of a baby, a mother begins another life, she is called life with a baby. That's all. The child is with the mother, not the mother with the child! Feel the difference! You need to be able to organize your life in a different way, in the first months, of course, the help of loved ones is very necessary. In the tradition of many peoples, it was customary for the first 40 days after childbirth to remove a woman from any housework and household chores, she was engaged only in a child. In some nations, objects that the mother of a newborn touched were considered “unclean”, therefore, they preferred to protect the mother from the rest of the household, allocating her a separate “corner” of the house, where no one bothered her and she did not interfere with anyone. Among the Slavs, such a restrictive custom was called a six-week. By 1.5-2 months, the rhythm of daytime dreams begins to form, and the baby has a kind of “regime”, the mother becomes more free.
For a mother who can't imagine breastfeeding without looking back at the clock, and who is sure that the “right” baby is the baby lying quietly in her crib all the time, feeding on demand will be a complete hassle. It will be much easier for such a mother if she stops looking at the clock and ties the baby to herself with a large scarf or uses a patchwork holder (sling). It will become easier for her if she stops running between the nursery and the kitchen, but takes the baby with her to the kitchen and carries him around the house with her, doing housework, in a box, a cradle, a special chair, if she tries not to put him off often, and pick up as soon as possible, postponing the baby only in case of emergency and not for long.
Breastfeeding is not the same as house arrest. In the conditions of modern society, it is possible to organize the exit of a nursing mother to work from about 6 months of age of the baby. If necessary, you can start working from the age of 4 months, but, of course, it is better not every day of the week and not full time. It is the responsibility of a breastfeeding consultant to help a mother organize her return to work.
Sometimes, when I advise mothers on breastfeeding, I suggest that they forget for a second that they are already living in the 21st century. I propose to return, for example, to the cave and ask what they will do if the child woke up at night, how to calm him down? If you are walking through the forest and trying not to attract the attention of predators, how to make the baby silent? If the child is thirsty, what will you give him? What is the baby used to, for thousands of years of its existence? To the fact that he sleeps on his mother while she wanders through the forest with a digging stick in search of roots, and wakes up when mother stops. Since mom stopped, then there is time to wake up and suck. Therefore, even now the child sleeps well, tied to the mother with a patchwork holder, wakes up when the mother, having done a few household chores, sits in a chair to take care of the baby.
Some mother, reading about the cave, will be offended, saying that she is a civilized creature. But please think. Man, mother's breast and mother's milk have been created by evolution over millions of years. They are made for each other. Baby food has created progress and more recently. The skills of motherhood and breastfeeding have also been lost by our society quite recently. A person is not physiologically adapted to artificial feeding and a pacifier. The mother's breast will not produce enough milk at 6-7 feedings per day. Nature did not know, when creating man as a mammal, that the time would come when the need for breastfeeding would be satisfied by some kind of pacifiers and nipples.
Changes that occur during the formation of the personality of a child who did not have full contact with the mother during prolonged breastfeeding are noted by modern research by psychologists and sociologists. These are changes with a minus sign. It would be better if they were not, these changes.
Breastfeeding is important not only for the baby, it is also important for the mother. During on-demand feeding, the woman's feelings change, a stronger attachment to the baby is formed, the woman becomes more sensitive to the needs of the baby. Deeper affection and understanding are not only preserved in infancy. They persist for life. For clarity, imagine what happens to a woman’s feelings if she tries to “withstand” a child, endures his crying, anxiety. What happens to a woman if she uses the recommendation from one very popular book for parents: "Come to the child if he cries for more than 15 minutes"? Speaking in abstract terms, humanity is interested in reviving the practice of breastfeeding. The revival of this practice is impossible without mothers realizing the true reasons for the child's need for attachment to the breast.
Lilia Kazakova, pediatrician,
breastfeeding and child care counselor leader
First month breastfeeding: what to expect
Not sure how to establish lactation and increase milk production? If you need help, support, or just want to know what to expect, read our first month breastfeeding advice
Share this information
The first few weeks of breastfeeding are stressful. If at times you feel like you can't handle it, know that you are not alone. Feeding your baby all day long is completely natural and helps produce breast milk, but can be quite tiring at times. Be patient, think about yourself and remember: after the first month, when milk production stabilizes, it will become easier.
How often should a baby be breastfed?
Babies are born with a small stomach that grows rapidly as milk production increases: in the first week it is no larger than an apricot, and after two weeks it is already the size of a large hen's egg. 1.2 Let the child eat as much as he wants and when he wants. This will help him quickly regain the weight lost after birth and grow and develop further.
“Be prepared to feed every two to three hours throughout the day. At night, the intervals between feedings can be longer: three to four or even five hours, says Cathy Garbin, a recognized international expert on breastfeeding. Some eat quickly and are satiated in 15 minutes, while others take an entire hour to feed. Do not compare your breastfeeding regimen with that of other mothers - it is very likely that there will be nothing in common between them.
At each feed, give your baby a full meal from one breast and then offer a second one, but don't worry if the baby doesn't take it. When the baby is full, he lets go of his chest and at the same time looks relaxed and satisfied - so much so that he can immediately fall asleep. The next time you feed, start on the other breast. You can monitor the order of the mammary glands during feeding using a special application.
Why does the child always ask for a breast?
The first month is usually the hardest time to breastfeed. But do not think that because the baby is constantly hungry and asks for a breast almost every 45 minutes, then you do not have enough milk.
In the first month, the baby needs to eat frequently to start and stimulate the mother's milk production. It lays the foundation for a stable milk supply in the future. 3
In addition, we must not forget that the child needs almost constant contact with the mother. The bright light and noise of the surrounding world at first frighten the baby, and only by clinging to his mother, he can calm down.
Sarah, mother of three from the UK, confirms: “Crying is not always a sign of hunger. Sometimes my kids just wanted me to be around and begged for breasts to calm them down. Use a sling. Place the cradle next to the bed. Don't look at the clock. Take advantage of every opportunity to relax. Forget about cleaning. Let those around you take care of you. And not three days, but six weeks at least! Hug your baby, enjoy the comfort - and trust your body."
Do I need to feed my baby on a schedule?
Your baby is still too young for a strict daily routine, so
forget about breastfeeding schedules and focus on his needs.
“Volumes have been written about how to feed your baby on a schedule, but babies don't read or understand books,” Cathy says. - All children are different. Some people can eat on a schedule, but most can't. Most often, over time, the child develops his own schedule.
Some mothers report that their babies are fine with scheduled feedings, but they are probably just the few babies who would eat every four hours anyway. Adults rarely eat and drink the same foods at the same time of day - so why do we expect this from toddlers?
Offer your baby the breast at the first sign of hunger. Crying is already the last stage, so be attentive to early signs: the baby licks his lips, opens his mouth, sucks his fist, turns his head with his mouth open - looking for the breast. 4
What is a “milk flush”?
At the beginning of each feed, a hungry baby actively suckles the nipple,
thereby stimulating the milk flow reflex - the movement of milk through the milk ducts. 5
“Nipple stimulation triggers the release of the hormone oxytocin,” explains Cathy. “Oxytocin is distributed throughout the body and causes the muscles around the milk-producing glands to contract and the milk ducts to dilate. This stimulates the flow of milk.
If the flushing reflex fails, milk will not come out. This is a hormonal response, and under stress it may not work at all or work poorly. Therefore, it is so important that you feel comfortable and calm when feeding.
“Studies show that each mother has a different rhythm of hot flashes during one feed,” Kathy continues, “Oxytocin is a short-acting hormone, it breaks down in just 30-40 seconds after formation. Milk begins to flow, the baby eats, the effect of oxytocin ends, but then a new rush of milk occurs, the baby continues to suckle the breast, and this process is repeated cyclically. That is why, during feeding, the child periodically stops and rests - this is how nature intended.
The flow of milk may be accompanied by a strong sensation of movement or tingling in the chest, although 21% of mothers, according to surveys, do not feel anything at all. 5 Cathy explains: “Many women only feel the first rush of milk. If you do not feel hot flashes, do not worry: since the child eats normally, most likely, you simply do not understand that they are.
How do you know if a baby is getting enough milk?
Since it is impossible to track how much milk a baby eats while breastfeeding, mothers sometimes worry that the baby is malnourished. Trust your child and your body.
After a rush of milk, the baby usually begins to suckle more slowly. Some mothers clearly hear how the baby swallows, others do not notice it. But one way or another, the child himself will show when he is full - just watch carefully. Many babies make two or three approaches to the breast at one feeding. 6
“When a child has eaten, it is noticeable almost immediately: a kind of “milk intoxication” sets in. The baby is relaxed and makes it clear with his whole body that he is completely full, says Katie, “Diapers are another great way to assess whether the baby is getting enough milk. During this period, a breastfed baby should have at least five wet diapers a day and at least two portions of soft yellow stool, and often more. ”
From one month until weaning at six months of age, a baby's stool (if exclusively breastfed) should look the same every day: yellow, grainy, loose, and watery.
When is the child's birth weight restored?
Most newborns lose weight in the first few days of life. This is normal and should not be cause for concern. As a rule, weight is reduced by 5-7%, although some may lose up to 10%. One way or another, by 10–14 days, almost all newborns regain their birth weight. In the first three to four months, the minimum expected weight gain is an average of 150 grams per week. But one week the child may gain weight faster, and the next slower, so it is necessary that the attending physician monitor the health and growth of the baby constantly. 7.8
At the slightest doubt or signs of dehydration, such as
dark urine, no stool for more than 24 hours, retraction of the fontanel (soft spot on the head), yellowing of the skin, drowsiness, lethargy, lack of appetite (ability to four to six hours without feeding), you should immediately consult a doctor. 7
What is "cluster feeding"?
When a baby asks for a breast very often for several hours, this is called cluster feeding. 6 The peak often occurs in the evening between 18:00 and 22:00, when many babies are especially restless and need close contact with their mother. Most often, mothers complain about this in the period from two to nine weeks after childbirth. This is perfectly normal and common behavior as long as the baby is otherwise healthy, eating well, gaining weight normally, and appears content throughout the day. 9
Cluster feeding can be caused by a sharp jump in the development of the body - during this period the baby especially needs love, comfort and a sense of security. The growing brain of a child is so excited that it can be difficult for him to turn off, or it just scares the baby. 9 If a child is overworked, it is often difficult for him or her to calm down on his own, and adult help is needed. And breastfeeding is the best way to calm the baby, because breast milk is not only food, but also pain reliever and a source of happiness hormones. 10
“Nobody told me about cluster feeding, so for the first 10 days I just went crazy with worry - I was sure that my milk was not enough for the baby,” recalls Camilla, a mother from Australia, “It was a very difficult period . I was advised to pump and supplement until I finally contacted the Australian Breastfeeding Association. There they explained to me what was happening: it turned out that it was not about milk at all.
Remember, this is temporary. Try to prepare dinner for yourself in the afternoon, when the baby is fast asleep, so that in the evening, when he begins to often breastfeed, you have the opportunity to quickly warm up the food and have a snack. If you are not alone, arrange to carry and rock the baby in turns so that you have the opportunity to rest. If you have no one to turn to for help and you feel that your strength is leaving you, put the baby in the crib and rest for a few minutes, and then pick it up again.
Ask your partner, family and friends to help you with household chores, cooking and caring for older children if you have any. If possible, hire an au pair. Get as much rest as possible, eat well and drink plenty of water.
“My daughter slept a lot during the day, but from 23:00 to 5:00 the cluster feeding period began, which was very tiring,” recalls Jenal, a mother from the USA, “My husband tried his best to make life easier for me - washed, cleaned, cooked, changed diapers, let me sleep at every opportunity and never tired of assuring me that we were doing well.
If you are concerned about the frequency of breastfeeding, it is worth contacting a specialist. “Check with a lactation consultant or doctor to see if this is indicative of any problems,” recommends Cathy. “Resist the temptation to supplement your baby with formula (unless recommended by your doctor) until you find the cause. It may not be a matter of limited milk production at all - it may be that the child is inefficiently sucking it.
When will breastfeeding become easier?
This early stage is very special and does not last long. Although sometimes it seems that there will be no end to it, rest assured: it will get easier soon! By the end of the first month, breast milk production will stabilize, and the baby will become stronger and learn to suckle better. 2.3 Any problems with latch on by this time will most likely be resolved and the body will be able to produce milk more efficiently so inflammation and leakage of milk will begin to subside.
“The first four to six weeks are the hardest, but then things start to get better,” Cathy assures. It just needs to be experienced!”
The longer breastfeeding continues, the more benefits it brings, from saving on formula and improving sleep quality 11-13 to boosting your baby's immune system 14 and reducing your risk of developing certain types of cancer. 15
“When you feel like you're pushing yourself, try to go from feed to feed and day to day,” says Hannah, a UK mom. “I was sure I wouldn’t make it to eight weeks. And now I have been breastfeeding for almost 17 weeks, and I dare say it is very easy.”
Read the resource Breastfeeding beyond the first month: what to expect
Readings
1 Naveed M et al. An autopsy study of relationship between perinatal stomach capacity and birth weight. Indian J Gastroenterol .1992;11(4):156-158. - Navid M. et al., Association between prenatal gastric volume and birth weight. Autopsy. Indian J Gastroenterol. 1992;11(4):156-158.
2 Neville MC et al. Studies in human lactation: milk volumes in lactating women during the onset of lactation and full lactation .Am J Clinl Nutr .1988;48(6):1375-1386.-Neville M.S. at the beginning and at the peak of lactation." Am F Clean Nutr. 1988;48(6):1375-1386.
3 Kent JC et al. Principles for maintaining or increasing breast milk production. 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
4 Australian Breastfeeding Feeding cues ; 2017 Sep [ cited 2018 Feb ]. - Australian Breastfeeding Association [Internet], Feed Ready Signals; September 2017 [cited February 2018]
5 Kent JC et al. Response of breasts to different stimulation patterns of an electric breast pump. J Human Lact . 2003;19(2):179-186. - Kent J.S. et al., Breast Response to Different Types of Electric Breast Pump Stimulation. J Human Lact (Journal of the International Association of Lactation Consultants). 2003;19(2):179-186.
6) Kent JC et al . Volume and frequency of breastfeedings and fat content of breast milk throughout the day. Pediatrics. 2006;117(3): e 387-395. — Kent J.S. et al., "Amount and frequency of breastfeeding and fat content of breast milk during the day." Pediatrix (Pediatrics). 2006;117(3):e387-95.
7 Lawrence RA, Lawrence RM. Breastfeeding: A guide for the medical profession. 7th ed. Maryland Heights MO, USA: Elsevier Mosby; 2010. 1128 p . - Lawrence R.A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." Seventh edition. Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2010. P. 1128.
8 World Health Organization. [Internet]. Child growth standards; 2018 [cited 2018 Feb] - World Health Organization. [Internet]. Child Growth Standards 2018 [cited February 2018].
9 Australian Breastfeeding Association [ Internet ]. Cluster feeding and fussing babies ; Dec 2017 [ cited 2018 Feb ] - Australian Breastfeeding Association [Internet], Cluster Feeding and Screaming Babies; December 2017 [cited February 2018].
10 Moberg KU, Prime DK. Oxytocin effects in mothers and infants during breastfeeding. Infant . 2013;9(6):201-206.- Moberg K, Prime DK, "Oxytocin effects on mother and child during breastfeeding". Infant. 2013;9(6):201-206.
11 U.S. Department of Health & Human Services [Internet]. Surgeon General Breastfeeding factsheet; 2011 Jan 20 [cited 2017 Feb] - Department of Health and Human Services [Internet], "Breastfeeding Facts from the Chief Medical Officer", Jan 20, 2011 [cited Feb 2017]
12 Kendall-Tackett K et al. The effect of feeding method on sleep duration, maternal well-being, and postpartum depression. clinical lactation. 2011;1;2(2):22-26. - Kendall-Tuckett, K. et al., "Influence of feeding pattern on sleep duration, maternal well-being and the development of postpartum depression." Clinical Lactation. 2011;2(2):22-26.
13 Brown A, Harries V. Infant sleep and night feeding patterns during later infancy: Association with breastfeeding frequency, daytime complementary food intake, and infant weight. Breast Med . 2015;10(5):246-252. - Brown A., Harris W., "Night feedings and infant sleep in the first year of life and their association with feeding frequency, daytime supplementation, and infant weight." Brest Med (Breastfeeding Medicine). 2015;10(5):246-252.
14 Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk.