Feeding medicine to baby
How to Give by Mouth
Nationwide Children’s Hospital
Giving medicine to infants and young children can be hard. Here are some suggestions and safety tips that may make giving medicine easier.
- Read the label each time before you give the medicine.
- If the medicine is a liquid, use a pediatric measuring device or syringe (Picture 1). You can get these at the pharmacy. Never measure liquid medicines in kitchen spoons.
- Give the exact amount of medicine ordered.
- Ask your child's doctor, health care provider, or pharmacist if the medicine can be mixed with foods and drinks. Some foods or drinks make the medicine not work well.
- Stay with your child until they swallow all of the medicine.
- This medicine is only for your child. Do not give it to anyone else.
- Never call medicine "candy." Call it medicine.
A Positive Approach
The way you give medicine to your child is very important. A direct approach is usually best. This means you expect your child to take the medicine just as you expect them to put on their coat before going out in cold weather.
How to Give to Infants (Newborn to One Year Old)
Here are the ways to give medicine to an infant. Choose the one that you think will work with your baby. If one method does not work, try another one.
- Draw up the correct amount of medicine into an oral syringe (a syringe without a needle). Let your infant suck the medicine out of the syringe. Do not squirt medicine directly at the back of the baby's throat. This may cause them to choke.
- Give small amounts of medicine at a time to avoid choking (Picture 2).
- Let your baby swallow all the medicine before you give more.
- Give the medicine right before a feeding unless your doctor tells you not to.
 Your baby is hungry and more likely to swallow the medicine. You know that your baby may be hungry by watching for their sucking reflex.
Your baby is hungry and more likely to swallow the medicine. You know that your baby may be hungry by watching for their sucking reflex. - Avoid mixing medicine with foods your child must have. They may begin to dislike the foods they need.
- Some medicines may be crushed and mixed in soft food. Check with your doctor, nurse, or pharmacist first. To crush a pill, place it between two spoons and press the spoons together. Mix the medicine with a small amount (1 to 2 teaspoons) of applesauce or pears and give it with a spoon.
- Some medicines can be put in a small amount of juice or sugar water. Do not put medicine in a full bottle or cup in case the infant does not drink very much.
How to Give to a Child 1 Year and Older
Your attitude toward giving medicine is especially important with young children. These are some ways to give medicine. Try one that you think will work with your child. If one method does not work, try another one.
- Give the medicine straight from a pediatric measuring device (Picture 1, page 1).

- Check with your doctor, health care provider, or pharmacist before crushing medicines and mixing them in soft food, like ice cream, pudding, or applesauce. Do not use foods your child must have, such as meat or vegetables.
- Try mixing the medicine with small amounts of food that have a strong flavor. This helps hide the taste of the medicine. Mixing with sweet or cold foods may also help.
- Some medicines can be put in a small amount of juice or sugar water. Mix the medicine with a small amount (1 to 2 teaspoons) or juice or sweetened water. Give with a spoon or let your child drink it. Do not put medicine in a full cup in case your child does not drink very much. Follow the instructions from your child's doctor, health care provider, or pharmacist.
- If your child doesn't like the taste of the medicine, offer a popsicle before giving it. The popsicle will freeze the taste buds, so the medicine doesn't taste as bad.
- Explain to your child why they need to take the medicine in words they can understand.
 For example, "This medicine will make your tummy stop hurting."
For example, "This medicine will make your tummy stop hurting." - When possible let the child choose how and when to take the medicine (or which one to take first). Let him hold the spoon, cup, or syringe and take it themselves.
- Praise your child every time they take the medicine without a struggle. Giving a special sticker works well for some children.
- Try to ignore your child's behavior when they do not cooperate.
- Never give medicine right after disciplining your child. They may think the medicine is punishment.
- Never threaten your child with a "shot" if they do not take the medicine.
- Give your child a drink of water after they take the medicine.
- If you do not have a medicine spoon or syringe from a pharmacist, use a measuring spoon made for cooking (Picture 3).
Measuring Spoons Conversion Table
Measuring Spoon Metric (1 mL = 1 cc)
1/4 teaspoon = 1. 25 mL
25 mL
1/2 teaspoon = 2.5 mL
3/4 teaspoon = 3.75 mL
1 teaspoon = 5 mL
1 ½ teaspoons = 7.5 mL
2 teaspoons = 10 mL
1 tablespoon = 15 mL
1 ounce = 30 mL
Medicine: How to Give by Mouth (PDF), Somali (PDF), Spanish (PDF)
HH-V-28 8/84, Revised 6/22 | Copyright 1984, Nationwide Children’s Hospital
How to Get Babies to Take Medicine
When your child is sick, you want to do whatever you can to make them feel better—like lots of cuddles, snuggles and cartoons. But when medicine is involved in helping them feel better, it can be a struggle.
“Issues taking medication is a common scenario we face in the pediatric office,” said Meghan Fels, DO, a pediatrician with Banner Health Clinic in Greeley, CO.
Whether it’s an over-the-counter (OTC) pain reliever or a prescribed antibiotic, sometimes it’s impossible to get the medicine to go down. Dr. Fels shared some stress-free ways to help you make it go down in the most delightful way (hopefully!).
Improve the flavor
As it can go with food, the smell, taste, consistency and sight of some medications can be a turnoff to children of all ages. “The good news is that most medications do have a good enough flavor or a flavor that is easily masked,” Dr. Fels said.
Whenever possible, look for medications that are flavored or tailored to your child’s palate. Many OTC medicines come in both liquid and chewable forms in a variety of fun flavors—from watermelon to berry-flavored.
For prescriptions, check with your child’s health care provider or pharmacy to see if they can help improve the taste. Many traditional pharmacies offer a service called FLAVORx. “But check with your child’s doctor or pharmacist, because not all medications can be flavored due to how they are constituted,” Dr. Fels said.
Trick their taste buds
Get creative! If your child isn’t having it, try mixing the dose of medicine with a strong, sweet flavor of your child’s choice (that is, if they’re old enough to verbalize). “My go-to is typically chocolate or strawberry syrup,” Dr. Fels said. “Typically, 5ml of sweetener mixed in is enough for a single dose.” Pancake syrup or ice cream are alternative options to try with the medication dose. If your child is under the age of 1, however, steer clear of honey due to a botulism risk.
“My go-to is typically chocolate or strawberry syrup,” Dr. Fels said. “Typically, 5ml of sweetener mixed in is enough for a single dose.” Pancake syrup or ice cream are alternative options to try with the medication dose. If your child is under the age of 1, however, steer clear of honey due to a botulism risk.
This being said: Some medications can’t be given during meals or with particular foods, so remember to check with your pharmacist or child’s health care provider regarding any restrictions. And refrain from diluting medicine in a large cup of liquid. You want to make sure they take all the medicine, which can be difficult in a large quantity.
Focus on remaining calm
“It’s always better to focus on a good, calm technique for giving medicine,” Dr. Fels said. “Forcing a child to take medication can be a struggle, struggling can cause resistance as well as vomiting or choking.”
Children can pick up on what you’re putting down—especially if you’re frustrated or nervous. If you remain calm and positive, it’ll help your child stay calm as well. “For older children who will understand, explain why the medication will help their body and will help them feel better or to heal,” Dr. Fels said.
If you remain calm and positive, it’ll help your child stay calm as well. “For older children who will understand, explain why the medication will help their body and will help them feel better or to heal,” Dr. Fels said.
Try a different delivery
If you at first don’t succeed, try a different method.
- Difficulty swallowing pills? If your child has difficulty swallowing pills, check to see if there are other formulations for the medication. Sometimes medications come in a chewable form or in capsules that can be opened and more easily swallowed. You can also try drinking quickly through a straw or using thicker fluid—such as a smoothie—to help the pill go down. Call your child’s doctor if you aren’t successful.
- Difficulty swallowing liquid? Try a plastic medication syringe or dropper and slowly push the medicine into your child’s mouth. “I typically recommend a syringe or medication dropper, so you know you’re delivering the proper amount,” Dr.
 Fels said.
Fels said.
Reward and celebrate
After giving them their medicine, end with positive reinforcement. This can be as simple as a sticker and a hug. Let them know they are helping themselves feel better.
Helpful reminders about giving medicine
Whether OTC or prescribed by their health care provider, medicine can still be dangerous if not handled appropriately. Dr. Fels shared some important reminders for all parents and caregivers:
- Keep your child/baby upright when dispensing medication—never give to them while lying down. This will help prevent choking or vomiting up the medicine.
- Don’t squirt medicine to the back of the throat. Instead, aim for the back of the cheek and slowly dispense the medicine, so your child can easily swallow.
- Only give medication when needed.
- Always read the labels for appropriate dosing and if your child is old enough for the medication. That’s because some medications are not safe for babies/infants.
 If you have any questions, always check with your child’s health care provider for dosage, timing and appropriate medication.
If you have any questions, always check with your child’s health care provider for dosage, timing and appropriate medication. - Cough suppressants are not recommended for those under age 6.
- Honey medications are not recommended for those under age 1.
- Infant drops (i.e., Motrin) are stronger (more concentrated) than the children's formulation so always read labels for proper dosage.
- Always remember to store medication out of reach and out of sight, stored up high and in a locked cabinet.
- Never refer to medicine as candy or as a treat. For children who will understand, explain to them why the medication will help their body, will help them feel better or to heal.
- Get rid of any old medications and prescriptions you aren’t using or that have expired, plus outdated products.
Call your child’s health care provider
Helping an uncooperative baby or child take medicine is never easy—especially if you are frustrated.![]() If you’re both struggling to get the medicine to go down, don’t hesitate to reach out to your child’s health care provider.
If you’re both struggling to get the medicine to go down, don’t hesitate to reach out to your child’s health care provider.
“There are always other options, such as different medication forms, we can try instead,” Dr. Fels said. “And, if they aren’t getting any better or their symptoms are worsening, always reach out to your child’s doctor or call 911 if your child is showing signs of any emergency.”
Similar articles
- Baby Poop: What’s Normal and What’s Not
- 6 Common Contagious Childhood Conditions
- Rashes on Children: When Should You Worry?
- How to Treat Your Child’s Flu Symptoms
Children's Health Parenting
Join the Conversation
Breastfeeding and drug use
And now the birth is behind, the labor pain has been forgotten, lactation has been established, and at any moment a new problem may arise in front of the young mother: how the medicine will affect the newborn baby when breastfeeding. Unfortunately, not every mother can boast of excellent health and there is a need to take medication.
Unfortunately, not every mother can boast of excellent health and there is a need to take medication.
The degree of adverse effect of the drug on the body of the newborn is determined by the following factors:
- drug toxicity;
- the true amount of the drug that entered the child's body;
- a feature of the effect of the drug on the immature organs of the child;
- the duration of the drug excretion from the child's body;
- the duration of taking the medicine by a nursing mother;
- individual sensitivity of the child to this drug;
- the risk of developing allergic reactions.
Of the most commonly used drugs, most are not very toxic drugs that cause significant toxic effects on organs and tissues. Therefore, it is believed that in many cases, with medical treatment, breastfeeding can be continued.
If a woman combines breastfeeding and treatment, then it may be useful to select the optimal scheme for alternating the drug and feeding. It is necessary to take the medicine in such a way that the time of feeding does not fall on the period of its maximum concentration in the blood.
It is necessary to take the medicine in such a way that the time of feeding does not fall on the period of its maximum concentration in the blood.
When using the medicine, a woman during breastfeeding should be aware that the side effects caused by this drug may also occur in a child.
If the risk of adverse effects of the drug on the child's body is high, then for the duration of treatment you need to stop breastfeeding, but continue pumping milk to maintain lactation. After the end of the course of treatment, it is necessary to resume breastfeeding. It is believed that after a course of antibiotics incompatible with breastfeeding, you can feed 24 hours after the last dose of the drug. And when using a number of radioactive agents, the radioactivity of milk can persist from 3 days to 2 weeks.
Features of the use of various groups of drugs during breastfeeding
Medicines contraindicated while breastfeeding:
Cytostatics and radioactive preparations (drugs used to treat tumors and autoimmune diseases, rheumatoid arthritis). These drugs significantly suppress immunity and cell division. If necessary, these drugs stop breastfeeding.
These drugs significantly suppress immunity and cell division. If necessary, these drugs stop breastfeeding.
Antibiotics is used to treat various infectious and inflammatory diseases. Penicillins, cephalosporins, macrolides, aminoglycosides are usually not contraindicated in breastfeeding. These antibiotics pass into milk in small amounts, so their toxicity to the child is low.
Macrolides (erythromycin, sumamed, vilprofen, etc.) penetrate milk well, but their use during breastfeeding is possible. There is a potential risk of developing complications associated with the occurrence of allergic reactions, disruption of the normal intestinal flora (diarrhea), reproduction of fungi (candidiasis - thrush). For the prevention of dysbacteriosis, it is recommended that the child be given probiotics (Bifidum Bacterin, Linex). If an allergic reaction occurs in a child, you should stop taking this antibiotic or temporarily stop breastfeeding.
Tetracyclines, sulfonamides (Bactrim, Biseptol, etc. ), Metronidazole, Clindamycin, Lincomycin, Ciprofloxacin penetrate into milk, and the likelihood of negative reactions is high. Therefore, the use of these drugs during breastfeeding is contraindicated.
), Metronidazole, Clindamycin, Lincomycin, Ciprofloxacin penetrate into milk, and the likelihood of negative reactions is high. Therefore, the use of these drugs during breastfeeding is contraindicated.
Side effects of tetracyclines - growth retardation of the child, a violation of the development of bone tissue and tooth enamel of the child. Side effect of Clindamycin - risk of gastrointestinal bleeding; and Levomycetin - toxic damage to the bone marrow, the effect on the cardiovascular system.
Antihypertensive agents are used in hypertension.
When breastfeeding, the following drugs can be used with caution: Dibazol, Dopegit, Verapamil.
Contraindicated in breastfeeding: Cordaflex, ACE inhibitors (Enap, Kapoten), Diazoxide, Reserpine.
The use of antihistamines for allergies during breastfeeding is possible. It is advisable to use Cetirizine, Loratadine. It is not desirable to use 1st generation drugs (Suprastin, Tavegil), which can cause drowsiness in a child.![]() Erius is contraindicated in breastfeeding.
Erius is contraindicated in breastfeeding.
Antithyroid drugs for breastfeeding
Antithyroid drugs are used in diseases of the thyroid gland, occurring with an increase in its function. These drugs are used when breastfeeding with caution, controlling the condition of the child. They suppress the function of the child's thyroid gland.
Salbutamol, terbutaline, fenoterol are approved for use during breastfeeding. It is necessary to monitor the condition of the child, since their side effect is excitement, increased heart rate.
Hormones (prednisolone, dexamethasone, hydrocortisone) are used for autoimmune diseases (rheumatoid arthritis, systemic connective tissue diseases, autoimmune hepatitis, etc., with adrenal insufficiency) are usually not contraindicated in breastfeeding.
However, if it is necessary to treat them for more than 10 days, the issue of continuing breastfeeding is decided individually. If a woman needs long-term hormonal treatment at a high dose, breastfeeding should be stopped.
Paracetamol is not contraindicated during breastfeeding if used in the usual dose (1 tablet up to 3-4 times a day, no more than 2-3 days). Exceeding the dose and long-term use of paracetamol should be avoided, since the side effect of the drug is a toxic effect on the liver and blood.
Contraceptives for breastfeeding
When breastfeeding, drugs containing progesterone are allowed. Other medicines are contraindicated during breastfeeding.
Expectorants during breastfeeding
- Ambroxol, Bromhexine, ACC can be used during breastfeeding.
- Pre- and probiotics (Linex, Hilak forte, etc.) are compatible with breastfeeding.
It should be noted that in our Center for Mother and Child, all medications used are safe for the health of the baby and mother. We try to minimize the prescription of drugs, only in the most extreme cases are prescribed drugs that are contraindicated during breastfeeding. And the most important recommendation is not to prescribe medications on your own, especially to nursing mothers! Health to you and your Babies!
Obstetrician-gynecologist Nugmanova M. K .
K .
Checked the head. genus. house number 2 Markashova M. Yu.
Medicines and breastfeeding | Medela
Breastfeeding mothers can safely use most prescribed medications. It is well known that most of the drugs pass into milk, however, as a rule, we are talking about such small amounts that they do not pose a danger to the child. However, doctors and pharmacists should be warned that a woman is breastfeeding before any drug is prescribed.
Share this information
Drugs can pass into milk if they reach high plasma concentrations in the mother's blood, have a low molecular weight (< 800 Da), have little protein binding, and are easily transported to the brain. Other factors are also very important, such as the oral bioavailability of the drug to the child. Many drugs, for example, can be destroyed in the baby's intestines or accumulate in the mother's liver and never get into her blood plasma.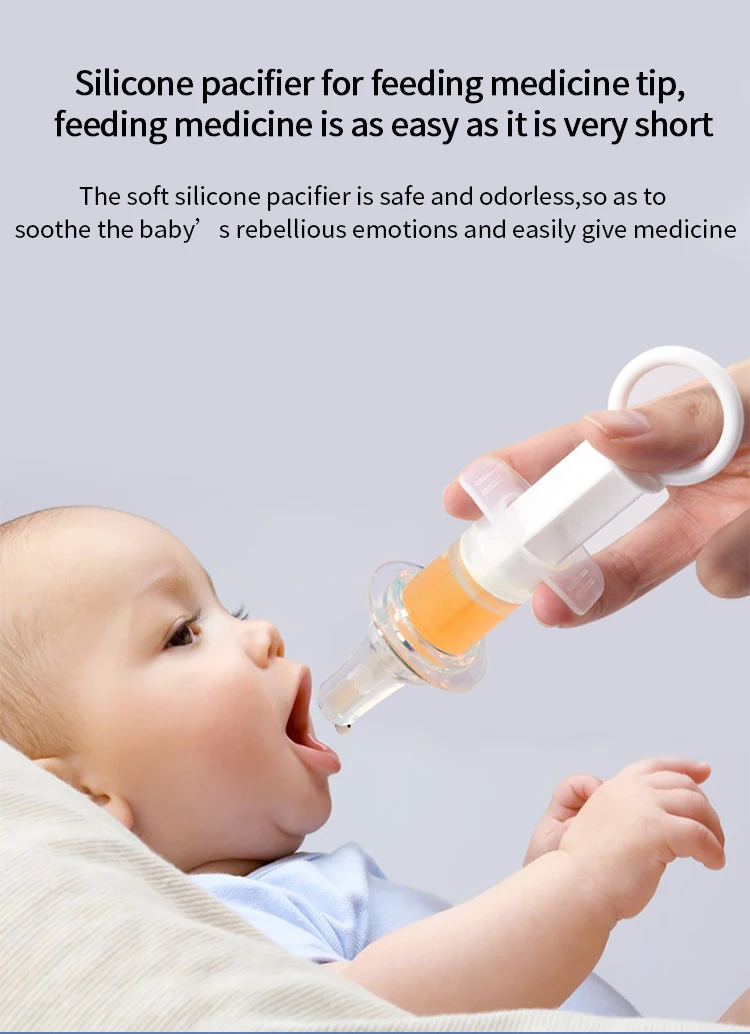
Drugs can pass into milk through passive transfer from the mother's blood plasma. Drugs normally pass from maternal plasma to lactocytes, but in order to reach milk, they must pass through both lactocyte lipid bilayer membranes. However, in the first three days after birth, the tight junctions between lactocytes may be open, allowing the drug to more easily pass into milk.
Drugs that inhibit milk production
Suppression of milk production due to medication may be due to suppression of prolactin production in the pituitary gland, difficulty in the release of oxytocin and a direct effect on lactocytes. For a complete list of medications and medications that can inhibit milk production, see http://toxnet.nlm.nih.gov/newtoxnet/lactmed.htm.
General recommendations for most drugs and medications while breastfeeding
- Avoid medications, including herbal preparations, unless absolutely necessary.
- Most medicines can be used if the relative dose for a child is less than 10 percent, but it is still recommended to seek medical advice.

Learn more











