Foods for baby with stomach bug
Gastroenteritis (Stomach Flu) (for Parents)
What Is Gastroenteritis?
Gastroenteritis, often called the stomach flu, is a common illness that causes nausea, vomiting, diarrhea, and belly cramps. It usually lasts a few days and isn't serious. Most kids get better at home by resting and drinking plenty of liquids.
What Causes Gastroenteritis?
Gastroenteritis (gass-troh-en-teh-RYE-tis) happens when germs (viruses, bacteria, or parasites) infect the stomach or intestines, causing inflammation.
In kids, viruses are the most common cause of gastroenteritis. Rotavirus causes many cases of stomach flu in children, but the rotavirus vaccine can help prevent them.
Many of the germs that cause gastroenteritis spread easily. So someone can get sick if they:
- Touch something contaminated and then touch food or their mouth.
- Share food or drinks with someone who is sick.
- Live with someone who’s infected, even if that person isn’t sick.
What Are the Signs & Symptoms of Gastroenteritis?
The most common signs of gastroenteritis are vomiting and diarrhea. Many children also have a fever.
When kids have diarrhea or vomiting, they lose lots of fluid in their poop or vomit. This can lead to dehydration (not having enough water in the body). If that happens, the body can have trouble working as it should.
How Is Gastroenteritis Diagnosed?
Doctors usually can tell if someone has stomach flu by hearing about the symptoms. Usually, no tests are needed. If a child is very sick or has blood or mucus in the poop, doctors might order a stool (poop) test, urine (pee) test, or blood test to check for dehydration and to see what’s causing it.
How Is Gastroenteritis Treated?
There is no specific treatment for gastroenteritis, and most kids can be treated at home. Keep your child hydrated by offering plenty of liquids. Kids with more severe dehydration may need treatment in the ER or hospital.
Mild dehydration is treated with oral (by mouth) rehydration. This usually includes giving oral rehydration solution (such as Pedialyte, Enfalyte, or a store brand). It has the right amounts of water, sugar, and salt to help with dehydration. You can buy it without a prescription at drugstores or supermarkets. If you can’t get oral rehydration solution, talk to your doctor.
If your child has mild dehydration and your doctor says it’s OK to start treatment at home:
- Give your child an oral electrolyte solution as often as possible. If your child throws up, start with small sips, about 1 or 2 teaspoons every few minutes.
- Babies can continue to breastfeed or take formula as long as they are not throwing up repeatedly.
- Don't give babies plain water instead of oral rehydration solution. It doesn't have the right nutrients for babies with dehydration.
- Older children can have frozen electrolyte popsicles.
- Do not give your child full-strength juice (undiluted), soda, or sports drinks.
 These have a lot of sugar, which can make diarrhea worse.
These have a lot of sugar, which can make diarrhea worse.
When your child stops vomiting, you can offer small amounts of solid foods, such as toast, crackers, rice, or mashed potatoes. Yogurt, fruits, vegetables, and lean meat, like chicken, are also OK.
A child who isn’t throwing up can eat a regular diet, if they feel up to it. It may take time for them to feel like eating. There's no need to avoid dairy unless it makes the vomiting or diarrhea worse. Avoid fatty foods, which can make diarrhea worse.
To help your child feel better, let your child rest as needed. You can give medicine for fever or pain, like acetaminophen or ibuprofen (do not give ibuprofen to babies under 6 months old), if your doctor says it’s OK. Follow the package directions for how much medicine to give and how often. Don't give aspirin to your child or teen. It's linked to a rare but serious illness called Reye syndrome.
Don't give medicines for diarrhea or vomiting unless your doctor tells you to.
Keep your child out of school or childcare until 24 hours without vomiting or fever and diarrhea has improved. Your child also should stay out of swimming pools until all symptoms have stopped.
When Should I Call the Doctor?
Call the doctor if your child:
- can’t drink for several hours
- is peeing less often (more than 4–6 hours for babies and 6-8 hours for older children)
- has signs of dehydration, such as crying with few or no tears, having a dry mouth or cracked lips, feeling dizzy or lightheaded, acting very sleepy or less alert
- has a high fever
- has blood in their poop or vomit
- is vomiting for more than 24 hours or the diarrhea doesn’t get better after several days
Can Gastroenteritis Be Prevented?
Germs that cause gastroenteritis are contagious. The best way to avoid the illness is to keep the germs from spreading:
- Teach all family members to wash their hands well and often.
 They should wash for at least 20 seconds with soap and water. This is especially important after using the bathroom and before preparing or eating food.
They should wash for at least 20 seconds with soap and water. This is especially important after using the bathroom and before preparing or eating food. - Clean tabletops, doorknobs, and other surfaces that get touched a lot with a cleaner that kills viruses.
- Follow food safety guidelines to prevent bacteria and viruses from getting into food and drinks (food poisoning).
- Make sure your kids get all recommended immunizations on time.
Reviewed by: Mary L. Gavin, MD
Date reviewed: September 2021
Symptoms and Treatment for Stomach Flu
What causes vomiting and diarrhea?
Vomiting (throwing up) and diarrhea (frequent, watery bowel movements) can be caused by viruses, bacteria and parasites. Foods that are hard to digest (such as too many sweets) and undercooked (still partially raw) meat or fish can also cause vomiting and diarrhea.
Can vomiting and diarrhea be dangerous for children?
Vomiting and diarrhea can be harmful because they can cause dehydration. Dehydration occurs when you lose too much fluid. Young children can become dehydrated quickly, but dehydration can occur at any age.
Dehydration occurs when you lose too much fluid. Young children can become dehydrated quickly, but dehydration can occur at any age.
Schedule a telehealth appointment
Stomach flu and dehydration
How can I prevent dehydration?
If your baby or child has had several bouts of vomiting or diarrhea, he or she will need to replace lost fluids and electrolytes.
If you are breastfeeding, continue to give your baby breastmilk. Breastmilk has fluids and electrolytes needed to prevent dehydration. Your doctor may also want you to give your baby an oral rehydration solution (ORS).
If you feed your baby formula, try switching to one that is lactose free while your baby is sick. Lactose can make diarrhea worse. Your doctor may also suggest switching from formula to an ORS for 12 to 24 hours, and then switching back.
For toddlers and young children, use an ORS, which contains the right mix of salt, sugar, potassium and other nutrients to help replace lost body fluids.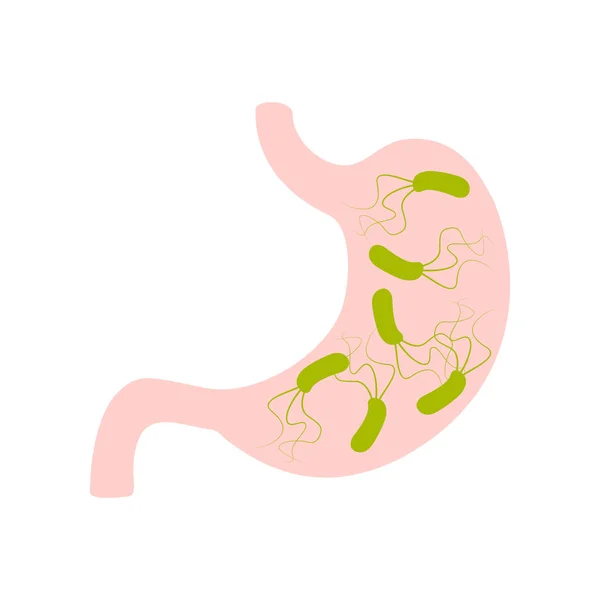 Children older than 1 year may also have clear soups, clear sodas or juice mixed with water to help prevent dehydration. You should avoid giving your child plain water and dark sodas. Water alone does not contain enough salt and nutrients to help with dehydration. Dark sodas are typically very high in sugar and can irritate your child’s stomach.
Children older than 1 year may also have clear soups, clear sodas or juice mixed with water to help prevent dehydration. You should avoid giving your child plain water and dark sodas. Water alone does not contain enough salt and nutrients to help with dehydration. Dark sodas are typically very high in sugar and can irritate your child’s stomach.
- Little or lack of urine, or urine that is darker than usual
- Urinating less frequently than usual (fewer than 6 wet diapers a day for infants and 8 hours or more without urinating for children)
- Thirst (babies may show thirst by crying, being irritable and eager to drink when something is offered)
- Irritability
- Not eating as well as usual
- Weight loss
- Dry mouth
- No tears when crying
- In babies who are younger than 18 months old, sunken soft spots on the top of their heads
- Skin that isn’t as springy or elastic as usual
- Sleepiness
An oral rehydration solution, or ORS, is a great way to replace fluids and nutrients lost through vomiting and diarrhea. An ORS is safe for babies and older children. An ORS can come in several forms, including a powder that you mix with water, a liquid that is already mixed and as frozen popsicle
An ORS is safe for babies and older children. An ORS can come in several forms, including a powder that you mix with water, a liquid that is already mixed and as frozen popsicle
Brands of ORS include Pedialyte, Ricelyte, Rehydralyte and the World Health Organization’s Oral Rehydration Solution (WHO-ORS). You can purchase these at most grocery stores and drugstores. If you don’t have access to store-bought ORS, you can mix 8 teaspoons of sugar and 1 teaspoon of salt in a quart (4 cups) of water. This mixture lacks potassium but is otherwise a good ORS. You can supply some potassium by adding a cup of orange juice to your homemade ORS or feeding your child some banana.
If your child is vomiting, try giving him or her small amounts of an ORS often, such as 1 teaspoonful every minute. When your child is able to keep the drink down, slowly increase how much you give.
If your child keeps vomiting, wait 30 to 60 minutes after the last time he or she vomited, and then give him or her a few sips of an ORS. Small amounts every few minutes may stay down better than a large amount all at once.
Small amounts every few minutes may stay down better than a large amount all at once.
When your child stops vomiting, you may increase how much of the ORS you give each time and add clear broths or clear sodas. Remember, small amounts are less likely to upset your child’s stomach.
If your child has diarrhea and isn’t vomiting, give him or her an ORS and other liquids. Your doctor may ask you to keep track of how much your child drinks. You can use a dropper, a spoon or a measuring cup to help you keep track.
Should I feed my child when he or she has diarrhea?Yes. Older children should begin eating within 12 to 24 hours after starting to take an ORS. Avoid foods with a lot of sugar and fat, such as ice cream, gelatin, pudding and fried foods. These may irritate your child’s stomach and digestive tract. It’s best to avoid dairy products for 3 to 7 days.
Your doctor may recommend that you give your child bland foods for the first 24 hours. Bland foods include bananas, rice, applesauce, toast, saltine crackers and unsweetened cereals. If your child does well with these foods, you can add other foods over the next 48 hours.
Bland foods include bananas, rice, applesauce, toast, saltine crackers and unsweetened cereals. If your child does well with these foods, you can add other foods over the next 48 hours.
Most children can return to their usual diet about 3 days after the diarrhea stops. If your child has been vomiting, wait 6 hours after the last time he or she vomited before offering food. Try offering small amounts of bland foods. Do not force your child to eat. Your child may not feel very hungry for a few days after vomiting.
Should I give my child medicine to stop diarrhea?Probably not. Diarrhea usually doesn’t last long. If it’s caused by an infection, diarrhea is a way for the body to get rid of the infection. Giving medicines that stop diarrhea may actually interfere with the body’s efforts to heal. Antibiotics are usually not necessary either. Talk to your family doctor if you think your child needs medicine.
Will my child need to go to the hospital?Probably not, unless dehydration becomes severe. In this case, your child may need to be given fluids intravenously (through an IV) to replace fluids lost through vomiting or diarrhea. Call your doctor if you notice any of the signs in the box below.
In this case, your child may need to be given fluids intravenously (through an IV) to replace fluids lost through vomiting or diarrhea. Call your doctor if you notice any of the signs in the box below.
Call your doctor if your child is vomiting or has diarrhea and:
- Is younger than 6 months old.
- Is older than 6 months old and has a fever higher than 101.4°F.
- Has signs of dehydration (see box above).
- Has been vomiting longer than 8 hours or is vomiting with great force.
- Has blood in his or her stools.
- Has blood in his or her vomit.
- Has not urinated in 8 hours.
- Might have swallowed something that could be poisonous.
- Has a stiff neck.
- Is listless or unusually sleepy.
- Has had abdominal pain for more than 2 hours.
Vomiting and diarrhea may be caused by foods that are hard for your child to digest (such as sugar or by bacteria in undercooked meat). Make sure your child eats a healthy diet.
Make sure your child eats a healthy diet.
Most infections that cause diarrhea are caused by a virus found in feces. Help prevent infection by disposing of dirty diapers properly and by washing your hands after changing a diaper or going to the bathroom. Make sure your child washes his or her hands frequently, especially after going to the bathroom.
Schedule a telehealth appointment
Source
Written by familydoctor.org editorial staff. American Academy of Family Physicians
Memo for parents: nutrition after an intestinal infection G.N. Speransky, within two weeks after suffering an intestinal infection, it is recommended to adhere to a certain diet.
Water porridge . Well boiled are allowed - rice, corn, buckwheat. With frequent and loose stools in a child, it is better to cook rice. When the stool improves (it resembles thick porridge in consistency), buckwheat can be gradually introduced, starting with the replacement of 1/3-1/2 of the feeding volume, once a day.![]() If the stool has not worsened, the next day one feeding can be completely replaced with buckwheat. For children with a tendency to constipation, it is better to include corn or buckwheat porridge in the diet, it is preferable to introduce oatmeal gradually, starting with the replacement of 1/2 -1/3 of the feeding volume.
If the stool has not worsened, the next day one feeding can be completely replaced with buckwheat. For children with a tendency to constipation, it is better to include corn or buckwheat porridge in the diet, it is preferable to introduce oatmeal gradually, starting with the replacement of 1/2 -1/3 of the feeding volume.
Lean meat. Recommended beef, veal, turkey, rabbit, chicken breast. The meat is cooked in the form of mashed potatoes, cutlets, steamed. For children of the first year of life, meat in jars is preferable. We introduce meat into the diet gradually, starting with half a teaspoon once a day for children under one year old and 1-2 teaspoons for children 2-3 years old. If the child tolerated the introduction of meat into the diet well (there is no vomiting, the stool has become more frequent and thinner), each next day the volume of meat can be doubled from the previous one with a gradual achievement of the age norm.
Dairy products. For children of the first year of life we introduce into the diet gradually, starting with half a teaspoon. Cottage cheese for baby food (without fillers - fruits and berries). If the child learns well cottage cheese for baby food, then after a week you can give cottage cheese with an apple, pear and banana. Curds with berries and exotic fruits are introduced last - after 3-4 weeks. For older children, cottage cheese with a minimum percentage of fat content of 0-5% without fillers is suitable for food.
For children of the first year of life we introduce into the diet gradually, starting with half a teaspoon. Cottage cheese for baby food (without fillers - fruits and berries). If the child learns well cottage cheese for baby food, then after a week you can give cottage cheese with an apple, pear and banana. Curds with berries and exotic fruits are introduced last - after 3-4 weeks. For older children, cottage cheese with a minimum percentage of fat content of 0-5% without fillers is suitable for food.
Fruit: mashed bananas, starting with 1-2 teaspoons per day. Apples during the first week after infection are preferably consumed in the form of industrial or home-made applesauce - you can bake an apple in the oven or microwave, rub through a sieve), also starting with one teaspoon. Examine purchased jars carefully so that there is no cream in them. After 5-7 days, if applesauce is well tolerated, you can offer your child a piece of fresh apple without peel. After two weeks, give your child plums, apricots, kiwi, and lastly - after 3-4 weeks - pineapple, mango.
After two weeks, give your child plums, apricots, kiwi, and lastly - after 3-4 weeks - pineapple, mango.
Vegetables. Zucchini, cauliflower, broccoli, pumpkin, potatoes are allowed boiled and pureed. It is desirable that potatoes in the child's diet during this period should not exceed 1/3-1/2 of the volume of all vegetables.
Eggs. Best prepared as steam omelettes in water and administered 1-2 weeks after an intestinal infection. And no more than 1-2 times a week for 2-3 weeks.
Bakery products: dried white bread, dryers and crackers without raisins, poppy seeds, sugar. And also - simple crackers and dry cookies.
Nutrition for intestinal infections in children
Parents of small children are especially afraid of intestinal infections. After all, it is important for a mother that her baby is full and healthy. And the presence of an intestinal infection in the body does not even allow to feed the child properly. Any meal is accompanied by vomiting, diarrhea, and in severe forms of the disease, children cannot eat at all.
Any meal is accompanied by vomiting, diarrhea, and in severe forms of the disease, children cannot eat at all.
Experienced grandmothers advise to keep the child on dry rations (ie, to eat crackers, dryers, biscuit cookies), others offer to treat immediately with herbal decoctions. Feeding children with an intestinal infection is a very important and delicate issue, so you should know not only how and what to feed a child, but also other important principles, for example, combating dehydration, drinking regimen, and so on. You can read about all this in the materials of this article.
What is an intestinal infection
Intestinal infections rank second among childhood diseases and are more common in young children (under 3 years of age). In the morning, the child was healthy and cheerful, as after a couple of hours the baby abruptly begins to vomit, the stool is upset and the temperature rises. All these symptoms indicate the presence of an intestinal infection in the body.![]()
Intestinal infection can be either viral or bacterial. From the names themselves it becomes clear what the difference between their pathogens is. In childhood, it is the rotovirus causative agent of intestinal infection that is more common.
As a type of intestinal infection, one can name:
- dysentery;
- salmonellosis;
- enterovirus.
At the first signs of an intestinal infection in a child, parents should not despair and become depressed. Doctors say that in 90% of cases, medical care is not needed and parents can cope with the disease on their own at home, you just need to follow the rules that will prevent dehydration.
But, in the remaining 10%, the situation is more complicated and at home you can only aggravate the situation. This requires urgent medical intervention and qualified assistance. It is worth remembering that in acute forms of intestinal infection, rapid dehydration of the body occurs and if slowed down with treatment, it can be fatal.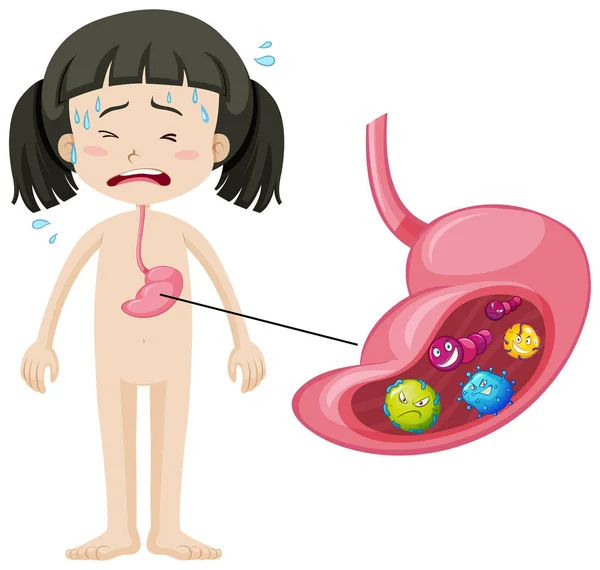
An ambulance must be called if:
- Bloody manifestations have been noticed in the child's vomit or stool.
- If you cannot get your child to drink (the child cannot swallow liquid or the water comes out immediately with vomit).
- The first signs of dehydration begin to appear, such as: dry skin, "dry" tongue, lack of sweat, tears, urination (the child has not gone to the toilet in the last few hours).
- In case of upset stool or vomiting, symptoms such as a sharp increase in temperature (in severe forms more than 38.5 C), lethargy, drowsiness, complete or partial refusal to eat, vomiting or diarrhea can be observed.
How can you get an intestinal infection?
The very moment of infection with an intestinal infection occurs when a bacterium or virus enters the body, namely, it settles in the gastrointestinal tract.
There are several ways to become infected with an intestinal infection:
- Through food - when eating poor-quality, contaminated food.

- By water - by bathing in contaminated water, swallowing water, or using poor-quality water at home.
- Contact-household - dirty hands and non-compliance with the rules of personal hygiene.
Treatment of intestinal infection
In the treatment of acute intestinal infection, special attention is paid to replenishing fluid in the body, as well as the use of a number of antibiotics. There is an opinion that antibiotics should be used in moderate and severe forms of the disease. Indeed, against the background of inhibition of the viability of microbes, antibiotics weaken the body's immunity, which leads to the development of dysbacteriosis, and hence the removal of all useful substances.
Prescribe antibiotics strictly after passing a series of tests, identifying the causes of the disease and monitoring by medical personnel.
Indications for prescribing therapeutic nutrition
One of the important factors in the treatment of children who have had an intestinal infection is proper nutrition or diet therapy. With improper nutrition, prolonged diarrhea, a sharp weight loss and lactose intolerance (milk is not absorbed by the body) can be seen.
With improper nutrition, prolonged diarrhea, a sharp weight loss and lactose intolerance (milk is not absorbed by the body) can be seen.
The main function of diet therapy is the ability to adjust the diet, nutrition of the child and make timely adjustments based on the form of the disease, the state of the body and the rate of recovery. Scientists have proven that even in severe forms of the disease, the gastrointestinal tract retains the function of eating and absorbing nutrients, but if food does not enter the child’s body for a long time (water-tea diets), then the body loses its recovery function, which and leads to dramatic weight loss.
Principles of nutrition in intestinal infections
The main principle of the modern approach to the nutrition of children who have had acute intestinal infections is the rejection of water-tea diets and the correct selection of products that contributed to an increase in the level of body resistance.
The type of food, the amount of servings and the amount of food consumed per day will be determined by a number of factors:
- the age of the child;
- form of the disease;
- the presence of other diseases;
- feeding form.
There are several principles that should be applied to all forms of the disease. There must be a break at night, there should not be overfeeding and force-feeding. We should not forget that in feeding you must always adhere to the regimen. In older children, the urge to vomit is associated with overeating. It is necessary to adhere to the generally accepted principle: it is better to eat more often, but in smaller portions.
If a child suffers a mild form of intestinal infection, without severe intoxication of the body, doctors advise reducing the amount of food consumed in the first days, the lack of food can be filled with liquid. It can be unsweetened teas, compotes, decoctions of chamomile, purified non-carbonated water. P
P
I'm looking for better to use in a pureed form (soup-puree, cereals and scrambled eggs), so it will be easier for the body to perceive it. All cooked food should be boiled or steamed. And already for 5-6 days it will be possible to return to normal life. In mild forms of diarrhea, it is recommended to reduce the amount of food by 15-20% and increase the number of meals by 1-2. By the fourth day after the onset of the disease state, the volume of food becomes the same and the diet is restored. With medium forms, it is necessary to divide meals into 5-6 approaches, the amount of food received per day is reduced by 30%. On the 6-7th day, there is a complete restoration of the volume of portions, and the number of meals.
In severe forms of intestinal infections, the patient is transferred to fractional food intake, and the daily volume is reduced by half - 45-50%. On the fourth day, the volume is gradually increased and only on the 8th day the diet is resumed.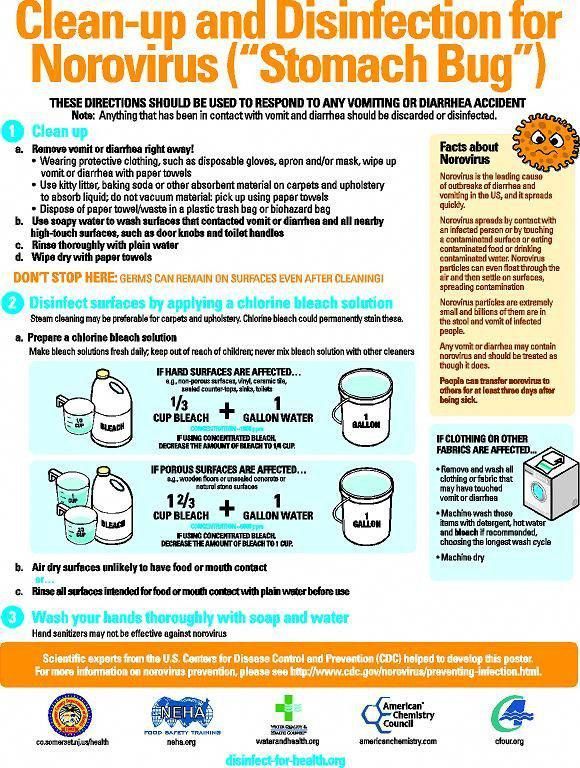
Drinking regimen
First of all, in case of an intestinal infection, doctors try to restore the body's water balance. The patient is recommended to drink 1 teaspoon of pure water every 5 minutes. Water allows you to remove all toxins from the body. You can also drink decoctions of chamomile, compotes, teas. It is important to take liquid in small portions. Too much fluid taken at one time can cause repeated vomiting and severe dehydration. Instead of water, it is mono to give the child a solution of rehydron, a slightly sweet compote of dried fruits, non-carbonated mineral water.
With diarrhea and vomiting, the water-salt balance of the body is disturbed. To restore it, it is recommended to drink Regidron. This drug can be purchased at a pharmacy or prepared at home. For a liter of water, you need to take 2 tbsp. spoons of sugar, 1 tbsp. a spoonful of coarse salt (fine you need to take 0.5 tablespoons) and 0.5 teaspoons of soda. It is not worth drinking such a drink in large doses, it is necessary to alternate. A teenager will need 50 ml 1 time in 1.5-2 hours, a child no more than 1 spoon at the same intervals. If there is a shortage of food, it must be supplemented with liquid.
A teenager will need 50 ml 1 time in 1.5-2 hours, a child no more than 1 spoon at the same intervals. If there is a shortage of food, it must be supplemented with liquid.
Do's and don'ts for children with intestinal infection
In case of intestinal infection, remember that all food should be steamed or boiled, in the form of puree, rarely soup, soufflé or scrambled eggs. The less often and lighter the food used, the faster it is absorbed by the body. If, after eating one portion, the patient did not eat and wants more, this is a sure sign that he is on the mend. But do not rush, but rather take care of the body. In this case, try to maintain an interval of at least 30 minutes and then offer the child another meal.
If an intestinal infection is transferred to the diet, you can use:
- Kissels from natural berries, preferably blueberries and dried fruits.
- Kashi on the water.
- Baked apples.
- Mashed potatoes.

- Vegetable puree.
Do not eat if you have an intestinal infection:
- Whole milk.
- Milk porridge.
- Dairy products: fermented baked milk, cream.
- Rye crackers and bread.
- Vegetables, fruits rich in fiber: radish, cabbage, beets, cucumbers, radishes, lettuce, grapes, apricots and plums.
- Nuts, mushrooms and legumes.
- Bakery and confectionery products.
- Salted, smoked and pickled foodstuffs.
- Carbonated drinks and water.
- Fatty varieties of poultry and meat.
- Fatty fish.
- Rich broths and soups.
The first few days the child's diet will be as scarce as possible, but already on the 4th day you can gradually introduce meatballs, steam cutlets, low-fat soups, boiled or steamed fish, eggs, bananas and peeled apples. On the recommendation of a doctor, you can enter milk porridge in a ratio of 1: 1.
Later you can add bakery products: dry biscuits, biscuits, breadcrumbs from dark types of bread, prepared by yourself. By the end of the third week, you can gradually drive rich pastries.
By the end of the third week, you can gradually drive rich pastries.
Peculiarities of breastfeeding in case of intestinal infection
If the child is infancy, then you should not refuse breastfeeding, but you can increase the number of feedings, if the baby needs it, switch to feeding on demand.
The only food at this age is mother's milk. After all, it is believed that children with severe diarrhea tolerate lactose in human milk more easily, so there is no need to refuse it at all. In addition, lactose retains a large amount of useful substances and those that promote growth. All of them affect the speedy recovery of the intestine.
But it should be remembered that for children who are bottle-fed, on the contrary, doctors recommend reducing the dose of the resulting mixture and increasing the number of meals (more often, but in smaller portions). But more detailed recommendations on nutrition can only be obtained from the attending pediatrician.