Foods to avoid while breastfeeding baby with eczema
Breastfeeding and maternal diet in atopic dermatitis
Can Fam Physician. 2011 Dec; 57(12): 1403–1405.
Language: English | French
Author information Copyright and License information Disclaimer
Question Many children are affected by atopic dermatitis (AD) at a very young age. I often consider whether nonpharmacologic interventions could prevent or mitigate the development of AD. Do breastfeeding or changes to the maternal diet help prevent the development of childhood AD?
Answer The American Academy of Pediatrics suggests that lactating mothers with infants at high risk of developing AD should avoid peanuts and tree nuts, and should consider eliminating eggs, cow’s milk, and fish from their diets. The World Health Organization also recommends breastfeeding infants up to 2 years of age. Studies have shown that breastfeeding can have a protective effect for AD in children; however, other studies have found insignificant or reversal effects. More research in this area is required.
Question De nombreux enfants sont affectés par la dermatite atopique (DA) en très bas âge. Je me demande souvent si des interventions non pharmacologiques pourraient prévenir ou atténuer le développement d’une DA. L’allaitement ou des changements dans l’alimentation maternelle aideraient-ils à prévenir le développement d’une DA infantile?
Réponse L’American Academy of Pediatrics fait valoir que les femmes qui allaitent des nourrissons à risque élevé de développer une DA devraient éviter les arachides et les noix, et envisager d’éliminer les œufs, le lait de vache et le poisson de leur alimentation. L’Organisation mondiale de la Santé recommande aussi d’allaiter les enfants jusqu’à l’âge de 2 ans. Des études ont démontré que l’allaitement pouvait avoir un effet de protection contre la DA chez l’enfant; toutefois, d’autres études ont trouvé des effets non significatifs ou inverses. Il faudrait plus de recherche à ce sujet.
Eczema, a common, chronic, relapsing inflammation of the skin, is often seen in young children.1 Over the past 3 decades, the rate of eczema among children has increased, including the rate of atopic dermatitis (AD), one type of eczema.2 Some 20% of school-aged children in North America and 10% of children in Western Europe suffer from eczema.2 Similarly, incidence in other industrialized nations is about 20%.1
There is mounting evidence that genetic linkage and family history are risk factors for developing eczema,3 and it is essential to be able to provide sound advice to families. Although food has long been thought to cause or aggravate eczema, research on prevention of AD through early nutritional intervention is lacking.
For many years, food has been considered a trigger for eczema, resulting in elimination diets, on occasion at the cost of malnutrition and emotional stress for children. 1 According to the American Academy of Pediatrics, the timing of introducing solid food can also affect the development of AD.4 It is recommended that initiating solid food be delayed until 4 to 6 months of age, and whole cow’s milk be delayed until 12 months of age.4
1 According to the American Academy of Pediatrics, the timing of introducing solid food can also affect the development of AD.4 It is recommended that initiating solid food be delayed until 4 to 6 months of age, and whole cow’s milk be delayed until 12 months of age.4
Several studies have evaluated the potential for hydrolyzed formula to reduce the risk of allergies compared with cow’s milk. In a randomized double-blind trial from the German Infant Nutritional Intervention study, among more than 2000 children offered hydrolyzed formulas from birth to 1 year of age, those offered extensively hydrolyzed casein formula (odds ratio [OR] 0.42, 95% confidence interval [CI] 0.22 to 0.79) and partially hydrolyzed whey formula (OR 0.56, 95% CI 0.32 to 0.99) had significantly reduced incidence of AD compared with those offered cow’s milk formula.5
In a Cochrane review comparing soy formula and cow’s milk formula, Osborn and Sinn6 included 3 studies with 875 infants 0 to 6 months of age without clinical evidence of allergy or food intolerance.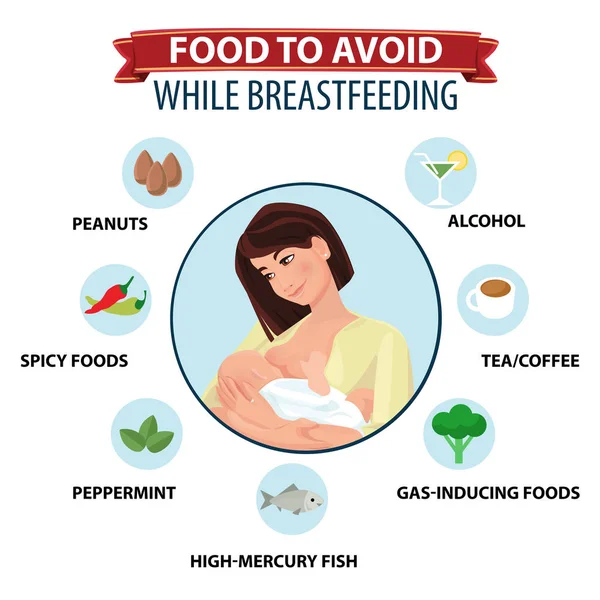 After comparing the effect of adapted soy formula with human milk, cow’s milk formula, and hydrolyzed protein formula on the development of atopy, they found that soy formula offered no significant benefit in preventing infant eczema (relative risk 1.20, 95% CI 0.95 to 1.52).6
After comparing the effect of adapted soy formula with human milk, cow’s milk formula, and hydrolyzed protein formula on the development of atopy, they found that soy formula offered no significant benefit in preventing infant eczema (relative risk 1.20, 95% CI 0.95 to 1.52).6
The World Health Organization currently recommends exclusive breastfeeding for the first 6 months and continuing to breastfeed, as well as introducing other foods, until 2 years of age.7 Breast milk contains compounds such as α-tocopherol, β-tocopherol, and prolactin—all help degrade inflammatory compounds, increase immune function, and decrease sensitivity of infants.8 In a meta-analysis of 18 prospective studies from 1966 to 2002, exclusive breastfeeding during the first 3 months of life was found to reduce the incidence of AD in children with a family history of atopy (OR 0.58, CI 0.41 to 0.92) and in those without a family history of atopy (OR 0. 84 for combined populations, CI 0.59 to 1.19).9 In another study, more than 2700 infants in the Netherlands were enrolled in a KOALA (Child, Parent, Health, Focus on Lifestyle and Predisposition) birth cohort study, in which it was found that breastfeeding could prevent atopic eczema in children.10 This study included repeated questionnaires at 34 weeks of gestation and at 3, 7, 12, and 24 months after birth, with immunoglobulin E levels measured at 2 years of age. Breastfeeding was found to prevent AD in the first 2 years of life among children of mothers without allergies and asthma.10 For mothers with allergies but no asthma, the results were not significant (P = .14) compared with mothers without allergies and asthma (P = .01), and there were no preventive effects when mothers had asthma (P = .87).10 Thus, it was concluded that breastfeeding had only negligible effects in children without first-order relatives who had atopy.
84 for combined populations, CI 0.59 to 1.19).9 In another study, more than 2700 infants in the Netherlands were enrolled in a KOALA (Child, Parent, Health, Focus on Lifestyle and Predisposition) birth cohort study, in which it was found that breastfeeding could prevent atopic eczema in children.10 This study included repeated questionnaires at 34 weeks of gestation and at 3, 7, 12, and 24 months after birth, with immunoglobulin E levels measured at 2 years of age. Breastfeeding was found to prevent AD in the first 2 years of life among children of mothers without allergies and asthma.10 For mothers with allergies but no asthma, the results were not significant (P = .14) compared with mothers without allergies and asthma (P = .01), and there were no preventive effects when mothers had asthma (P = .87).10 Thus, it was concluded that breastfeeding had only negligible effects in children without first-order relatives who had atopy. 10 In a birth cohort study conducted in Germany between 1995 and 1998, 3903 children were recruited, and exclusive breastfeeding was found to have a significant protective effect on AD prevention compared with cow’s milk formula (OR 0.64, 95% CI 0.45 to 0.90).11 In another prospective cohort study of healthy newborns at risk of atopy, 865 infants were exclusively breastfed and 256 infants were partially or exclusively formula fed, and were then followed for signs of AD or sensitization to milk or eggs for a year.12 The exclusively breastfed group had a lower incidence of AD (OR 0.47, 95% CI 0.30 to 0.74). The recommendation for children with AD in the family was exclusive breastfeeding for at least 4 months to prevent AD in the first year of life.12
10 In a birth cohort study conducted in Germany between 1995 and 1998, 3903 children were recruited, and exclusive breastfeeding was found to have a significant protective effect on AD prevention compared with cow’s milk formula (OR 0.64, 95% CI 0.45 to 0.90).11 In another prospective cohort study of healthy newborns at risk of atopy, 865 infants were exclusively breastfed and 256 infants were partially or exclusively formula fed, and were then followed for signs of AD or sensitization to milk or eggs for a year.12 The exclusively breastfed group had a lower incidence of AD (OR 0.47, 95% CI 0.30 to 0.74). The recommendation for children with AD in the family was exclusive breastfeeding for at least 4 months to prevent AD in the first year of life.12
However, breastfeeding effects on AD are still controversial. In a large population-based telephone cohort study in Denmark, Benn et al reported that exclusive breastfeeding for the first 4 months actually led to an increased incidence of AD in children with parents without allergies. 13 The association between breastfeeding and risk of AD seemed to increase with each month of exclusive breastfeeding.13 However, there was no dose-response effect found when comparing exclusive breastfeeding for 6 months and 4 months.13 Another cross-sectional study from Japan among junior high-school students reported an increased AD incidence if children were fed breast milk in their first 3 months of infancy compared with formula (P = .03).14 This result was not significant among children with no parental history of allergy.14
13 The association between breastfeeding and risk of AD seemed to increase with each month of exclusive breastfeeding.13 However, there was no dose-response effect found when comparing exclusive breastfeeding for 6 months and 4 months.13 Another cross-sectional study from Japan among junior high-school students reported an increased AD incidence if children were fed breast milk in their first 3 months of infancy compared with formula (P = .03).14 This result was not significant among children with no parental history of allergy.14
There are 2 possible ways to explain these findings. One possible reason is maternal awareness of the risk of developing AD, thus the increased risk of AD comes from atopic heredity as opposed to the effect of breast-feeding.13 Another explanation is the hygiene hypothesis.14 Early infection can promote maturation of the immune system and prevent further allergies, including eczema. 14 Because breastfeeding decreases the chance for children to be exposed to common allergens found in solid food or formulas, their immune systems will not be able to function properly to protect them from antigens, which might be the cause of more eczema cases found in the previous 2 studies. Although these hypotheses explain the increased incidence of AD seen in children with first-order parents with allergies, they cannot explain the increased risk of AD in children with parents without allergies.13
14 Because breastfeeding decreases the chance for children to be exposed to common allergens found in solid food or formulas, their immune systems will not be able to function properly to protect them from antigens, which might be the cause of more eczema cases found in the previous 2 studies. Although these hypotheses explain the increased incidence of AD seen in children with first-order parents with allergies, they cannot explain the increased risk of AD in children with parents without allergies.13
Can maternal dietary changes help infants avoid the risk of developing AD? In 2000, the American Academy of Pediatrics suggested that lactating mothers with infants at high risk of developing AD should avoid peanuts and tree nuts, and should consider eliminating eggs, cow’s milk, and fish from their diets.15 Food allergens such as peanuts have been detected in breast milk.14 However, in a cohort study of almost 14 000 preschool children, no association was demonstrated between breastfeeding and peanut allergy. 16 A Cochrane review of 4 trials with 334 pregnant women did not show adequate evidence that avoidance of eggs, milk, and other antigenic food in women during lactation prevented AD in children.17 The combined evidence from these trials does not show a strong correlation between maternal antigen avoidance and the incidence of AD in the first 18 months of life (relative risk 1.01, CI 0.39 to 12.67).17 A larger sample size and a longer follow-up study are needed to determine potential outcome benefits.17
16 A Cochrane review of 4 trials with 334 pregnant women did not show adequate evidence that avoidance of eggs, milk, and other antigenic food in women during lactation prevented AD in children.17 The combined evidence from these trials does not show a strong correlation between maternal antigen avoidance and the incidence of AD in the first 18 months of life (relative risk 1.01, CI 0.39 to 12.67).17 A larger sample size and a longer follow-up study are needed to determine potential outcome benefits.17
Other than focusing on antigenic foods, there has been increasing interest in the effects of probiotics as a maternal dietary supplement for preventing AD in children.18 In a Norwegian study, women received probiotic supplements during the last 4 weeks of pregnancy and until 3 months after birth.18 The results showed that the administration of probiotic bacteria significantly reduced the incidence of AD among children (OR 0. 51, 95% CI 0.30 to 0.87; P = .013).18 However, the results were not statistically significant in children with a positive family history.18 It was suggested that maternal supplementation with probiotics might influence the composition of the infant’s intestinal microbial flora and that such supplementation might be a potential mechanism for increasing anti-inflammatory immunoregulatory factors in breast milk.18 Other dietary supplements undergoing research are vitamin C19 and essential fatty acids.20 While there have been promising results for maternal intake of vitamin C,19 increasing the supplementation of omega-320 has not been found to reduce the incidence of AD among children.19,20 Further large-scale studies are required to explore these issues.19,20
51, 95% CI 0.30 to 0.87; P = .013).18 However, the results were not statistically significant in children with a positive family history.18 It was suggested that maternal supplementation with probiotics might influence the composition of the infant’s intestinal microbial flora and that such supplementation might be a potential mechanism for increasing anti-inflammatory immunoregulatory factors in breast milk.18 Other dietary supplements undergoing research are vitamin C19 and essential fatty acids.20 While there have been promising results for maternal intake of vitamin C,19 increasing the supplementation of omega-320 has not been found to reduce the incidence of AD among children.19,20 Further large-scale studies are required to explore these issues.19,20
The effects of breastfeeding and maternal diet on the development of AD in children are still controversial. While some reports suggest positive effects in preventing AD by breastfeeding or changing the maternal diet, other studies show insignificant or reverse effects. Further research is needed to determine sound recommendations for families.
While some reports suggest positive effects in preventing AD by breastfeeding or changing the maternal diet, other studies show insignificant or reverse effects. Further research is needed to determine sound recommendations for families.
PRETx
Child Health Update is produced by the Pediatric Research in Emergency Therapeutics (PRETx) program (www.pretx.org) at the BC Children’s Hospital in Vancouver, BC. Ms Lien is a member and Dr Goldman is Director of the PRETx program. The mission of the PRETx program is to promote child health through evidence-based research in therapeutics in pediatric emergency medicine.
Do you have questions about the effects of drugs, chemicals, radiation, or infections in children? We invite you to submit them to the PRETx program by fax at 604 875-2414; they will be addressed in future Child Health Updates. Published Child Health Updates are available on the Canadian Family Physician website (www.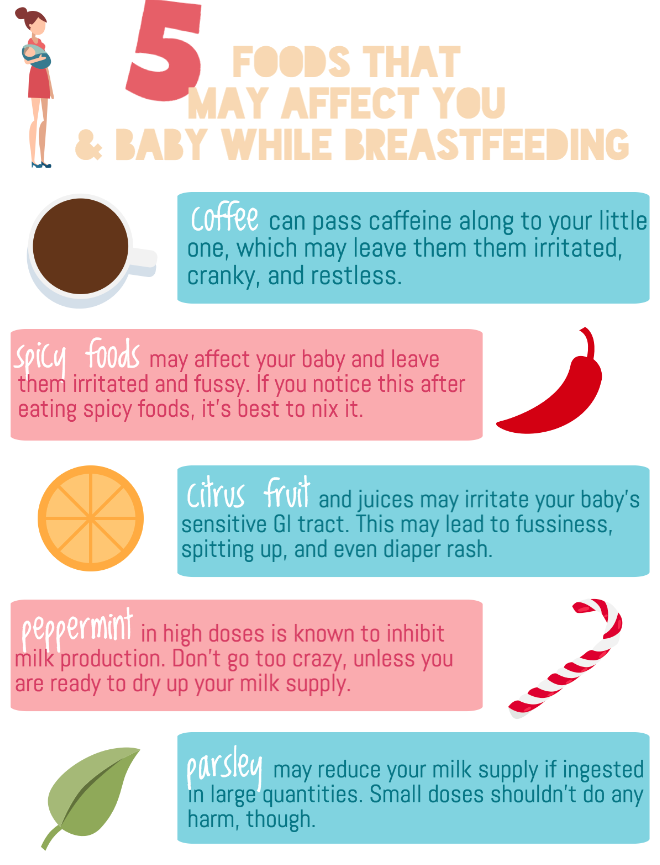 cfp.ca).
cfp.ca).
Competing interests
None declared
1. Finch J, Munhutu MN, Whitaker-Worth DL. Atopic dermatitis and nutrition. Clin Dermatol. 2010;28(6):605–14. [PubMed] [Google Scholar]
2. Eichenfield LF, Hanifin JM, Beck LA, Lemanske RF, Jr, Sampson HA, Weiss ST, et al. Atopic dermatitis and asthma: parallels in the evolution of treatment. Pediatrics. 2003;111(3):608–16. [PubMed] [Google Scholar]
3. Snijders BEP, Stelma FF, Reijmerink NE, Thijs C, van der Steege G, Damoiseaux JGMC, et al. CD14 polymorphisms in mother and infant, soluble CD14 in breast milk and atopy development in the infant (KOALA study) Pediatr Allergy Immunol. 2010;21(3):541–9. Epub 2009 Sep 15. [PubMed] [Google Scholar]
4. Greer FR, Sicherer SH, Burks AW, Committee on Nutrition and Section on Allergy and Immunology Effects of early nutritional interventions on the development of atopic disease in infants and children: the role of maternal dietary restriction, breastfeeding, timing of introduction of complementary foods, and hydrolyzed formulas. Pediatrics. 2008;121(1):183–91. [PubMed] [Google Scholar]
Pediatrics. 2008;121(1):183–91. [PubMed] [Google Scholar]
5. Von Berg A, Koletzko S, Grübl A, Filipiak-Pittroff B, Wichmann HE, Bauer CP, et al. The effect of hydrolyzed cow’s milk formula for allergy prevention in the first year of life: the German Infant Nutritional Intervention study, a randomized double-blind trial. J Allergy Clin Immunol. 2003;111(3):533–40. [PubMed] [Google Scholar]
6. Osborn DA, Sinn J. Soy formula for prevention of allergy and food intolerance in infants. Cochrane Database Syst Rev. 2004;(3):CD003741. [PubMed] [Google Scholar]
7. World Health Organization [website] Exclusive breastfeeding. Geneva, Switz: World Health Organization; 2011. Available from: www.who.int/nutrition/topics/exclusive_breastfeeding/en/. Accessed 2011 Jul 30. [Google Scholar]
8. Oddy WH. The long-term effects of breast-feeding on asthma and atopic disease. Adv Exp Med Biol. 2009;639:237–51. [PubMed] [Google Scholar]
9. Gdalevich M, Mimouni D, David M, Mimouni M. Breast-feeding and the onset of atopic dermatitis in childhood: a systematic review and meta-analysis of prospective studies. J Am Acad Dermatol. 2001;45(4):520–7. [PubMed] [Google Scholar]
Breast-feeding and the onset of atopic dermatitis in childhood: a systematic review and meta-analysis of prospective studies. J Am Acad Dermatol. 2001;45(4):520–7. [PubMed] [Google Scholar]
10. Snijders BE, Thijs C, Dagnelie PC, Stelma FF, Mommers M, Kummeling I, et al. Breast-feeding duration and infant atopic manifestations, by maternal allergic status, in the first 2 years of life (KOALA study) J Pediatr. 2007;151(4):347–51. 351.e1–2. Epub 2007 Jul 12. [PubMed] [Google Scholar]
11. Laubereau B, Brockow I, Zirngibl A, Koletzko S, Gruebl A, von Berg A, et al. Effect of breast-feeding on the development of atopic dermatitis during the first 3 years of life: results from the GINI-birth cohort study. J Pediatr. 2004;144(5):602–7. [PubMed] [Google Scholar]
12. Schoetzau A, Filipiak-Pittroff B, Franke K, Koletzko S, von Berg A, Gruebl A, et al. Effect of exclusive breast-feeding and early solid food avoidance on the incidence of atopic dermatitis in high-risk infants at 1 year of age. Pediatr Allergy Immunol. 2002;13(4):234–42. [PubMed] [Google Scholar]
Pediatr Allergy Immunol. 2002;13(4):234–42. [PubMed] [Google Scholar]
13. Benn CS, Wohlfahrt J, Aaby P, Westergaard T, Benfeldt E, Michaelsen KF, et al. Breastfeeding and risk of atopic dermatitis, by parental history of allergy during the first 18 months of life. Am J Epidemiol. 2004;160(3):217–23. [PubMed] [Google Scholar]
14. Miyake Y, Yura A, Iki M. Breastfeeding and the prevalence of symptoms of allergic disorders in Japanese adolescents. Clin Exp Allergy. 2003;33(3):312–6. [PubMed] [Google Scholar]
15. American Academy of Pediatrics, Committee on Nutrition Hypoallergenic infant formulas. Pediatrics. 2000;106(2 Pt 1):346–9. [PubMed] [Google Scholar]
16. Lack G, Fox D, Northstone K, Golding J, Avon Longitudinal Study of Parents and Children Study Team Factors associated with the development of peanut allergy in childhood. N Engl J Med. 2003;348(11):977–85. Epub 2003 Mar 10. [PubMed] [Google Scholar]
17. Kramer MS, Kakuma R. Maternal dietary antigen avoidance during pregnancy or lactation, or both, for preventing or treating atopic disease in the child. Cochrane Database Syst Rev. 2006;(3):CD000133. [PubMed] [Google Scholar]
Cochrane Database Syst Rev. 2006;(3):CD000133. [PubMed] [Google Scholar]
18. Dotterud CK, Storrø O, Johnsen R, Oien T. Probiotics in pregnant women to prevent allergic disease: a randomized, double-blind trial. Br J Dermatol. 2010;163(3):616–23. doi: 10.1111/j.1365-2133.2010.09889.x. Epub 2010 Jun 9. [PubMed] [CrossRef] [Google Scholar]
19. Hoppu U, Rinne M, Salo-Väänänen P, Lampi AM. Piironen, Isolauri E. Vitamin C in breast milk may reduce the risk of atopy in the infant. Eur J Clin Nutr. 2005;59(1):123–8. [PubMed] [Google Scholar]
20. Dunstan JA, Mori TA, Barden A, Beilin LJ, Taylor AL, Holt PG, et al. Maternal fish oil supplementation in pregnancy reduces interleukin-13 levels in cord blood of infants at high risk of atopy. Clin Exp Allergy. 2003;33(4):442–8. [PubMed] [Google Scholar]
Your Baby's Diet and Eczema: Breastfeeding and Bottle-Feeding
Written by Stephanie Watson
Medically Reviewed by Dan Brennan, MD on December 17, 2018
When your baby has eczema, you may wonder if that itchy rash is related to your feeding style. Is breastfeeding to blame? Or is it the solid foods you just introduced?
Is breastfeeding to blame? Or is it the solid foods you just introduced?
Some simple tips can help you get your baby off to a healthy start.
Breast Milk or Formula?
Breast milk is always best. It gives your little one the perfect balance of fat, protein, and other nutrients. It's also good for your baby's growing immune system.
"Breastfed infants will get some of the mom's immune system, so it actually helps boost their immunity," says Cindy Gellner, MD, a pediatrician at the University of Utah Community Clinics.
Breastfeeding also helps make the immune system less sensitive. That's important for eczema, which is triggered by overactive defenses.
Can a Breastfeeding Mom's Diet Affect Their Baby's Eczema?
Certain foods in a mom's diet could cause problems for their baby with eczema. If you’re breastfeeding, you may want to avoid common triggers like:
- Cow's milk
- Peanuts
- Tree nuts
- Shellfish
Signs that your baby is having a reaction to something you ate include an itchy red rash on the chest and cheeks, and hives. If you see these, stay away from whatever you think may be causing the problem for a couple of weeks.
If you see these, stay away from whatever you think may be causing the problem for a couple of weeks.
If things get better, brings foods back one at a time, says Robert Roberts, MD, PhD, a professor of pediatrics at UCLA.
Get some help from your doctor so you'll know when it's safe to start eating those foods again.
Which Formula Is Best for Bottle-Feeding?
"All babies will start off on milk-based formula," Gellner says. "If the baby has a lot of eczema and it's really problematic, then we'll try switching them to a formula made with hydrolyzed proteins."
Hydrolyzed means that the milk proteins are already broken down, so they're less likely to trigger an allergic reaction.
When Should You Introduce Solid Foods?
Experts say you can start your baby on solids between 4 and 6 months old. Ask your pediatrician what age is best for your child.
Which Foods Should You Give Your Baby First?
Many parents start their babies with iron-fortified rice or oatmeal cereals, and then graduate them to fruits and vegetables. Still, it's perfectly fine to start your kid on stage 1 fruits and vegetables or puree a veggie or fruit yourself.
Still, it's perfectly fine to start your kid on stage 1 fruits and vegetables or puree a veggie or fruit yourself.
"The biggest issue for parents of children with eczema is they need to introduce one food at a time so they can know what is causing a problem," says Chris Adigun, MD, a clinical assistant professor of dermatology at the New York University School of Medicine. "Stick with that food for at least 4 or 5 days before you move on to the next food."
After each new one, watch out for signs of an allergy, like:
- Diarrhea, sometimes with blood
- Hives
- Rash
- Swelling of the lips or tongue
- Vomiting
If you see any of these, call your child's doctor.
When Can Your Child Start on Cow's Milk?
Around 1 year old, you can try giving your child whole milk. If you notice any skin problems, then ask your doctor if you should switch to soy milk.
5 foods to limit or avoid while breastfeeding
Breast milk is incredibly nutritious. It provides most of the nutrients your baby needs during the first 6 months of life.
It provides most of the nutrients your baby needs during the first 6 months of life.
Although the composition of breast milk is highly regulated by your body, studies have shown that what you eat has some effect on the composition of breast milk.
In general, prohibited foods are prohibited. Instead, women are encouraged to eat a balanced and varied diet. However, there are some foods and drinks that you can limit while breastfeeding.
Here are 5 foods to limit or avoid while breastfeeding and tips on how to determine if your diet is affecting your baby.
1. High Mercury Fish
Fish is an excellent source of docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA), two types of omega-3 fatty acids that are important for brain development in infants but are difficult to find in other foods .
However, some types of fish and seafood can also contain high amounts of mercury, a metal that can be toxic, especially to infants and children who are more sensitive to mercury poisoning.
Acute exposure to high levels of mercury can permanently affect your child's central nervous system. As a result, they may have delays or impairments in:
- cognition
- fine motor skills
- speech and language development
- visual-spatial perception
Therefore, when breastfeeding, fish with a high mercury content should be avoided. Examples include:
- bigeye tuna
- Royal macrel
- Marlin
- Orange rough
- shark
- Fish-sword
- Tile fish
To ensure adequate consumption of omega-3 while reducing the risk of mercury poisoning, feeding mothers, it is recommended to avoid fish with a high content of ghosts and fish instead, consume 8–12 ounces (225–340 grams) of low-mercury fish per week.
Summary: Due to concerns about mercury poisoning in infants, breastfeeding women should avoid high mercury fish such as shark, swordfish and bigeye tuna.
2. Some herbal supplements.
The use of herbs and spices such as cumin or basil in food while breastfeeding is considered safe.
We offer you: The Anti-Inflammatory Diet: How to Reduce Inflammation Naturally
However, there are some safety concerns when it comes to herbal supplements and teas, as research on breastfeeding women is lacking.
In addition, because herbal supplements are not regulated by the US Food and Drug Administration (FDA), these supplements can also be contaminated with potentially harmful heavy metals.
Although many women try supplements to increase milk production, overall data on their effectiveness are limited, and most studies find no difference in breast milk production compared to placebo.
It's best to talk to your doctor before trying a supplement.
Summary: Because most herbal supplements have not been tested for safety while breastfeeding, it is recommended that you consult with your health care provider before using any supplements or herbal teas.

3. Alcohol
According to the Centers for Disease Control and Prevention (CDC), abstaining from alcohol is the safest option while breastfeeding. However, drinking from time to time is probably safe if you're careful with the amount and timing.
How much alcohol your baby can get from breast milk depends on how much alcohol you drink and when you drink it. Studies show that the amount of alcohol in breast milk peaks 30 to 60 minutes after the last drink.
We offer you: FODMAP: a complete guide for beginners
In addition, alcohol can stay in the body for up to 2-3 hours. This is for one serving only - the more alcohol you have, the longer it will take to get it out of your system.
As a result, the CDC recommends limiting alcohol to one standard drink per day and waiting at least 2 hours after that drink before breastfeeding.
One standard drink is equivalent to:
- 12 oz (355 ml) beer
- 5 oz (125 ml) wine
- 1.
 5 oz (45 ml) spirits
5 oz (45 ml) spirits
High alcohol consumption has been shown to reduce breast milk production by 20%. %.
Moreover, frequent heavy drinking during breastfeeding has been associated with an increased risk of sleep disturbance, delayed psychomotor skills, and even cognitive delay later in life.
Summary: women who are breastfeeding are advised to limit their alcohol intake to one drink or less per day and wait at least 2 hours before breastfeeding. Frequent and excessive drinking of alcohol can reduce milk production and have serious consequences for your baby.
4. Caffeine.
Coffee, sodas, tea and chocolate are common sources of caffeine. When you consume them, some of this caffeine may end up in your breast milk.
This can be problematic as babies have difficulty getting upset and getting rid of caffeine. As a result, large amounts of caffeine can accumulate in the child's body over time, causing irritability and sleep problems.
According to the CDC, breastfeeding mothers are advised to consume no more than 300 mg of caffeine per day, equivalent to two or three cups of coffee.
Because energy drinks often contain added vitamins and herbs, in addition to high amounts of caffeine, breastfeeding women are advised to avoid these products unless otherwise approved by a trusted health care provider.
Here are 11 foods and drinks to avoid during pregnancy
Summary: While breastfeeding, women are advised to limit their caffeine intake to 300 mg per day or less to prevent irritability and sleep disturbance in their infant.
5. Highly processed products.
To meet the increased nutritional needs of breastfeeding, it is extremely important to eat a healthy and balanced diet.
Because highly processed foods tend to be high in calories, unhealthy fats, and added sugars, but low in fiber, vitamins, and minerals, it is recommended that you limit your intake as much as possible.
Early research has also shown that a mother's diet during breastfeeding can affect her baby's diet later in life.
In particular, animal studies have shown that odors to which infants are exposed through breast milk may affect their food preferences as they grow older.
One study found that rats born to mothers high in unhealthy foods were significantly more likely to prefer foods high in fat and sugar than those whose mothers had a balanced and healthy diet.
Although more human studies are needed, there are concerns that frequent consumption of fatty and sugary foods during infancy may lead to less healthy eating habits and obesity as the child matures.
Summary: Because highly processed foods tend to be low in essential nutrients and may affect your baby's eating habits later in life, breastfeeding moms are advised to limit their intake of foods high in added sugar and processed fats.
Other considerations
When odors from foods and drinks pass into breast milk, some mothers find that strong flavors such as onions, garlic or spices cause their babies to refuse to eat or become fussy after eating.
While there is no evidence that all mothers should avoid strong tasting foods, if you notice changes in your baby's feeding it is important to talk to a dietitian or pediatrician about eliminating certain foods or spices from your diet.
Other potential food groups to avoid while breastfeeding include cow's milk and soy products.
We offer you: A keto diet plan and menu that can change your body
Approximately 0.5-2% of breastfed infants may be allergic to cow's milk protein from mother's milk, while 0.25% may be allergic to soy protein.
If your pediatrician suspects that your child may have a milk or soy allergy, it is recommended that you eliminate all cow's milk or soy protein from your diet for 2 to 4 weeks if you wish to continue breastfeeding.
Summary: Some children may be more sensitive to strong flavored foods or allergic to cow's milk or soy protein. In these cases, it's important to talk to your pediatrician before eliminating foods from your diet.
How to know if your diet is affecting your child
Every child is different. However, there are some general signs that your diet may be affecting your child, including:
- eczema
- Blood chair
- vomiting
- Dono
- Utnitsa
- Card
- wheezing
- Accumulation
- Excessive gas
- anaphylaxia - albeit rarely, it is important to immediately seek medical care 9,000 9000 9,000 9000 If your child shows any of these symptoms, this may be a sign that they have an allergy or intolerance to food from your diet. It's important to make an appointment with your pediatrician, as they can help you identify problem foods.
For some food allergies, you may be asked to rule out any suspected allergens for 2 to 4 weeks to see if symptoms go away.
Be aware that although your baby may have had an intolerance or allergy as an infant, they may still be able to tolerate these foods as they get older.
 Check with your pediatrician before adding foods to your or your child's diet again.
Check with your pediatrician before adding foods to your or your child's diet again. Summary: Symptoms such as eczema, bloody stools, diarrhea, and nasal congestion may indicate a food allergy or intolerance in your child. It is very important to work with your pediatrician to determine which foods may affect your child.
Summary
Breastfeeding provides your growing baby with essential nutrients.
We bring you: Acidic foods: what foods to limit or avoid
While most of the foods that should not have been consumed during pregnancy are back on the menu, there are some foods and drinks that may be intolerable or have negative consequences for your child.
While it is recommended to completely avoid high-mercury fish and some herbal supplements, foods such as alcohol, caffeine, and highly processed foods can still be consumed, but in limited amounts.
If your child has symptoms such as eczema or bloody stools, it may be related to something in your diet.
 It's important to share your concerns with your pediatrician before making drastic dietary changes.
It's important to share your concerns with your pediatrician before making drastic dietary changes. Topics
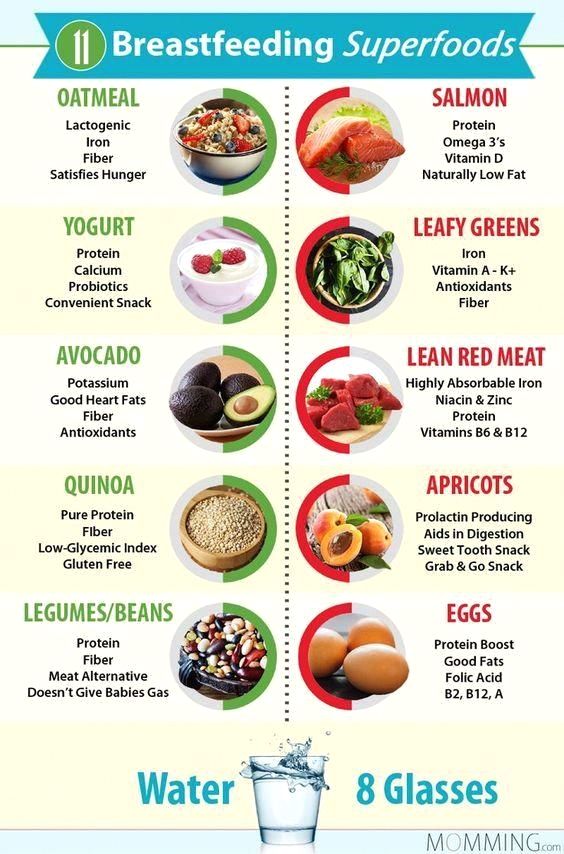
What to eat while breastfeeding | Breastfeeding Diet
You know that breast milk is the best food for your baby. What about your own nutrition while breastfeeding? We asked the nutritionist a few questions about the nutrition of a nursing mother.
Share this information
Priya Tew, UK-based registered dietitian :
Priya is a nutritionist, M.D., multi-award winning member of the British Dietetic Association and the Health Professions Council. She has three children, and she breastfed each of them for up to 18 months.There is no need to follow a special diet while breastfeeding, as long as your diet is balanced. It should include plenty of fruits and vegetables, whole grains such as oats, brown rice, various cereals, and breads labeled "whole grain", "wholemeal" or "wholemeal". These foods, along with potatoes, pasta, and couscous, are high in starch, an important source of energy.

In addition, you need lean proteins found in chicken, eggs, legumes, lentils, fish, and lean beef, as well as healthy fats found in olive oil, nuts, seeds, avocados, and fatty fish such as salmon and mackerel. Oily fish is very good for your health and development of your baby, but you should not eat more than two servings per week (about 140 g), as it may contain harmful impurities. 1
Should I take vitamins while breastfeeding?
The most important is vitamin D. It is essential for healthy bones, yours and your baby's. We get most of this vitamin from the sun. If you live in a region with insufficient solar activity, especially in winter, your body may lack it. In this case, the doctor may advise taking vitamin D supplements. 2
You also need to get enough calcium, as it is excreted from the body during breastfeeding. 3 Try to eat four servings of foods rich in this mineral a day. These can be dairy products such as milk, yogurt, and cheese, or non-dairy products such as nuts, tofu, sesame seeds, and leafy vegetables.
 One serving may consist of, for example, half a cup of green vegetables or a small piece of cheese (50 g).
One serving may consist of, for example, half a cup of green vegetables or a small piece of cheese (50 g). What foods should I avoid while breastfeeding?
The good news is that you can eat almost anything while breastfeeding. Only the consumption of oily fish should be limited. In small quantities, even caffeine is acceptable - more on this below.
If you are not allergic to peanuts, there is no reason to deny yourself products that contain peanuts. Recent studies show that if you eat peanuts while breastfeeding and gradually introduce them into your baby's diet during the first year, your baby will be less likely to become allergic to them in the future. 4
Do I need extra calories while breastfeeding?
Breastfeeding mothers need about 500 more calories per day. 5 But every mother is unique and your energy needs will change throughout your breastfeeding period. The number of calories you need depends on your baby's age, appetite, height, and weight, as well as your body mass index (BMI), your activity, and factors such as whether you are exclusively breastfeeding or not, and whether you are breastfeeding twins or multiple babies.
Can I go on a diet while breastfeeding?
Trying to lose weight while breastfeeding is not a good idea because you need to get enough nutrients for you and your baby. The fat accumulated during pregnancy is used to produce milk, so breastfeeding in itself will help you shed those extra pounds.
If your weight changes by more than 1 kg per week, check if you are eating a healthy and balanced diet and adjust if necessary. You can also ask your doctor for advice.
How can I find time to prepare healthy meals?
Having devoted yourself to feeding a child, you can forget about your own nutrition. However, it is important to ensure that your diet does not consist only of sweets and cookies. Of course, sweet snacks are easy and quick, but they do not bring any benefit to your body.
Opt for quick yet nutritious meals like scrambled eggs with spinach or fried chicken with brown rice. Oatmeal is great for breakfast, as it provides a slow release of energy from grains and soluble dietary fiber, which is what you need to restore strength in the morning after a night of breastfeeding.

Store pre-cut fruits and vegetables in the refrigerator for light snacks, or carry unsalted nuts in your bag. It's much easier than peeling tangerines with one hand while holding a baby with the other.
Should I drink more water while breastfeeding?
Breastfeeding can make you thirsty, so it's important to drink enough water. A person needs six to eight glasses of fluid a day, and even more if breastfeeding. 6 Make it a habit to drink a glass of water, milk or fruit juice without sugar every time you feed your baby.
I love coffee. Do I need to quit caffeine?
Coffee, like everything you eat or drink, passes into breast milk, so it is advisable to limit your intake while breastfeeding. Legal coffee limits vary by country, but the average recommendation is not to exceed 200-300 mg of caffeine per day (300 mg is equivalent to two cups of filtered coffee or four cups of tea). Talk to your doctor about the acceptable amount of coffee consumption for you.
 Also, don't forget that caffeine is found in colas and energy drinks, and a small bar of dark chocolate can contain up to 50 mg. 7
Also, don't forget that caffeine is found in colas and energy drinks, and a small bar of dark chocolate can contain up to 50 mg. 7 If I eat a varied diet, will my baby be less picky about food?
Breast milk has the flavor of everything you eat. 8 Therefore, if you eat a variety of foods while breastfeeding, giving your baby a chance to taste different flavors, he may like them in the future.
If you like spicy and spicy foods, there is no reason to refuse them while breastfeeding. When my first child was born, I ate a lot of spicy food. When my daughter was two years old, we went to Sri Lanka, coincidence or not, but she ate absolutely everything.
Is there anything in my diet that is not suitable for a child?
Babies often suffer from colic or are picky eaters at an early age, so mothers naturally wonder if their diet is causing this. Probably not. Studies show that the proportion of children who are allergic to any component of breast milk is only slightly more than 1%.
 9 Cow's milk, eggs, corn, and soy proteins in moms' diets are much more likely to cause allergic reactions than spicy foods, hot sauces, or cruciferous vegetables, which moms usually worry about.
9 Cow's milk, eggs, corn, and soy proteins in moms' diets are much more likely to cause allergic reactions than spicy foods, hot sauces, or cruciferous vegetables, which moms usually worry about. If your baby is allergic to substances in your milk, it can cause profuse vomiting, rash, bloody stools, or prolonged constipation. If your baby has an intolerance to any food, you will notice symptoms such as moodiness and crying after feeding, burping, diarrhea, or the baby will press his knees to his chest. Contact your doctor if something is bothering you. He may suggest eliminating certain foods for a couple of weeks, and then see if the child's behavior changes after eating them again.
You can also keep a food diary: write down everything you eat and drink, as well as your child's symptoms, and you may notice some patterns. However, before cutting out any foods, such as dairy, always check with your doctor, as it's important to know that you're getting the nutrients you need from other sources.
 Depending on where you live, you will be referred to a nutritionist or other specialist.
Depending on where you live, you will be referred to a nutritionist or other specialist. Does a vegetarian diet affect breast milk?
If you are getting enough calories and all the nutrients your body needs (carbohydrates, proteins, fats, vitamins and minerals), then you have nothing to worry about. A vegetarian or vegan diet requires plenty of vitamin B12, vitamin D, calcium, and omega-3 fatty acids while breastfeeding, so opt for foods and supplements that provide you with these essential nutrients.
If you are on a vegetarian, vegan, macrobiotic, or other special diet, you may need additional medical advice to make sure you are getting all the nutrients your baby needs.
Literature
1 National Health Service (NHS) [Internet]. Burnley, UK: Department of Health; 2018. Should pregnant and breastfeeding women avoid some types of fish?; 2015 Jul 06 [cited 2018 Apr 12]; Available from: https://www.nhs.uk/chq/Pages/should-pregnant-and-breastfeeding-women-avoid-some-types-of-fish.
 aspx - National Health Service (NHS) [Internet]. Burnley, UK: Department of Health; 2018. "Should a pregnant and lactating woman refrain from eating certain types of fish?"; July 6, 2015 [cited April 12, 2018]; See article on site https://www.nhs.uk/chq/Pages/should-pregnant-and-breastfeeding-women-avoid-some-types-of-fish.aspx
aspx - National Health Service (NHS) [Internet]. Burnley, UK: Department of Health; 2018. "Should a pregnant and lactating woman refrain from eating certain types of fish?"; July 6, 2015 [cited April 12, 2018]; See article on site https://www.nhs.uk/chq/Pages/should-pregnant-and-breastfeeding-women-avoid-some-types-of-fish.aspx 2 Oberhelman SS et al. Maternal vitamin D supplementation to improve the vitamin D status of breast-fed infants: a randomized controlled trial. Mayo Clin Proc. 2013;88(12):1378–1387. - Oberhelman S.S. et al., Introduction of Vitamin D to the Diet of Nursing Mothers to Increase Vitamin D in children: a randomized controlled trial. Mayo Clean Proc. 2013;88(12):1378–1387. : effects on the mother and the fetus. Am J Obstet Gynecol. 2006;194(4):937-945. - Thomas M., Weisman S.M., "Calcium intake during pregnancy and lactation: effects on the mother and on the fetus".
 Am J Obstet Ginekol (American Journal of Obstetrics and Gynecology). 2006;194(4):937-945.
Am J Obstet Ginekol (American Journal of Obstetrics and Gynecology). 2006;194(4):937-945. 4 Pitt et al . Reduced risk of peanut sensitization following exposure through breast-feeding and early peanut introduction. J Allergy Clinic Immunol. 2018;141(2):620-625. e 1 - Pitt et al., "Reducing the Risk of Peanut Allergy by Introducing Peanuts into the Breastfeeding Mother's Diet and as a Baby's First Food." J Allergy Clean Immunol. 2018;141(2):620-625.e1
5 Dewey KG. Energy and protein requirements during lactation. Annu Rev Nutr. 1997 Jul;17(1):19-36. - Dewey K. J., "Energy and Protein Requirements During Lactation". Anna Rev Nutr . 1997 Jul;17(1):19-36.
6 Food Standards Agency (FSA) [Internet]. London, UK: Crown copyright 2002.
 Eating for breastfeeding; [cited 2018 Apr 13]; Available from: https://www.food.gov.uk - Food Standards Agency (FSA) [Internet]. London, UK: State Copyright 2002. "Eat to feed" [cited April 13, 2018]. See article on https://www.food.gov.uk
Eating for breastfeeding; [cited 2018 Apr 13]; Available from: https://www.food.gov.uk - Food Standards Agency (FSA) [Internet]. London, UK: State Copyright 2002. "Eat to feed" [cited April 13, 2018]. See article on https://www.food.gov.uk 7 National Health Service (NHS) [Internet]. Burnley, UK: Department of Health; 2018. Breastfeeding and diet; 2016 Jan 29 [cited 2018 Apr 12]; Available from: https://www.nhs.uk/conditions/pregnancy-and-baby/breastfeeding-diet - National Health Service (NHS) [Internet]. Burnley, UK: Department of Health 2018. Breastfeeding and Diet; 29 January 2016 [cited 12 April 2018] See article at https://www.nhs.uk/conditions/pregnancy -and-baby/breastfeeding-diet
8 Mennella JA et al. Prenatal and postnatal flavor learning by human infants. Pediatrics. A. et al., Prenatal and postnatal recognition of odors in children. Pediatrix (Pediatrics). 2001;107(6):e88.