How long after drinking can i feed my baby
Alcohol | Breastfeeding | CDC
What is “moderate consumption”?
The Dietary Guidelines for Americans defines moderate consumption for women of legal drinking age as up to 1 standard drink per day.
What is a “drink”?
The Dietary Guidelines for Americans defines a standard “drink” as 12 ounces of 5% beer; 8 ounces of 7% malt liquor; 5 ounces of 12% wine; or 1.5 ounces of 40% (80 proof) liquor. All of these drinks contain the same amount (i.e., 14 grams, or 0.6 ounces) of pure alcohol. However, many common drinks contain much more alcohol than this. For example, 12 ounces of 9% beer contains nearly the same amount of alcohol as two (1.8) standard drinks. Consuming one of these drinks would be the equivalent of two standard drinks.
Is it safe for mothers to breastfeed their infant if they have consumed alcohol?
Not drinking alcohol is the safest option for breastfeeding mothers. Generally, moderate alcohol consumption by a breastfeeding mother (up to 1 standard drink per day) is not known to be harmful to the infant, especially if the mother waits at least 2 hours after a single drink before nursing. However, exposure to alcohol above moderate levels through breast milk could be damaging to an infant’s development, growth, and sleep patterns. Alcohol consumption above moderate levels may also impair a mother’s judgment and ability to safely care for her child.
Drinking alcoholic beverages is not an indication to stop breastfeeding; however, consuming more than one drink per day is not recommended.
Can alcohol be found in breast milk?
Yes. Alcohol levels are usually highest in breast milk 30-60 minutes after an alcoholic beverage is consumed, and can be generally detected in breast milk for about 2-3 hours per drink after it is consumed. However, the length of time alcohol can be detected in breast milk will increase the more alcohol a mother consumes. For example, alcohol from 1 drink can be detected in breast milk for about 2-3 hours, alcohol from 2 drinks can be detected for about 4-5 hours, and alcohol from 3 drinks can be detected for about 6-8 hours, and so on.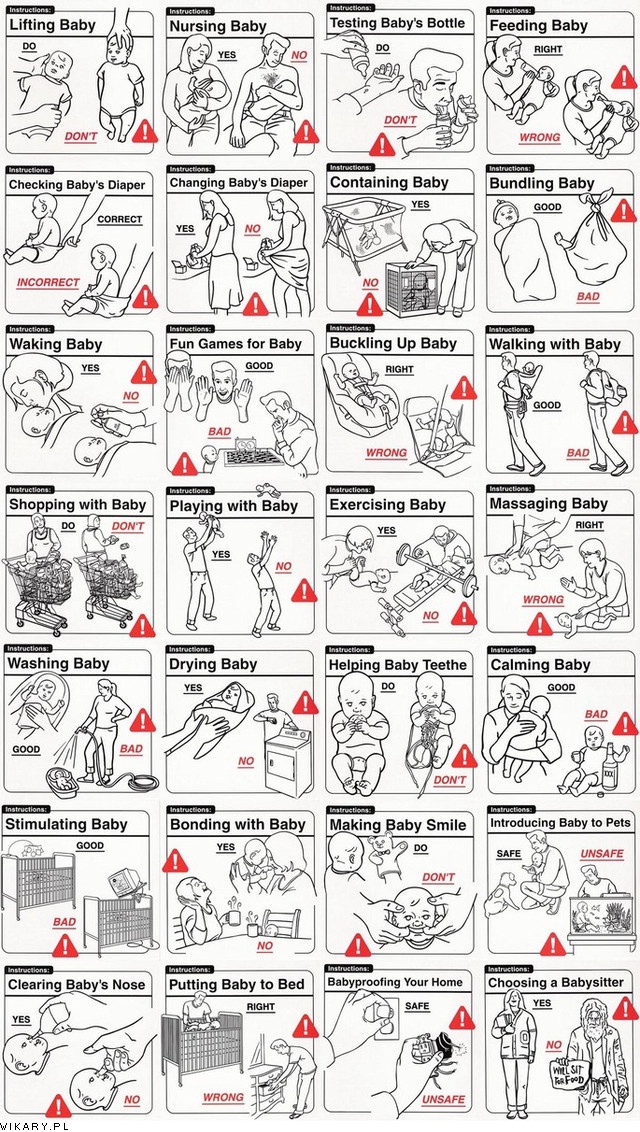 However, blood alcohol levels and the length of time alcohol can be detected in breast milk after drinking will depend on a number of factors, including the amount of alcohol consumed, how fast the alcohol is consumed, whether it is consumed with food, how much a mother weighs, and how fast alcohol is broken down in a mother’s body.
However, blood alcohol levels and the length of time alcohol can be detected in breast milk after drinking will depend on a number of factors, including the amount of alcohol consumed, how fast the alcohol is consumed, whether it is consumed with food, how much a mother weighs, and how fast alcohol is broken down in a mother’s body.
What effect does alcohol have on a breastfeeding infant?
Moderate alcohol consumption by a breastfeeding mother (up to 1 standard drink per day) is not known to be harmful to the infant, especially if the mother waits at least 2 hours before nursing. However, higher levels of alcohol consumption can interfere with the milk ejection reflex (letdown) while maternal alcohol levels are high. Over time, excessive alcohol consumption could lead to shortened breastfeeding duration due to decreased milk production. Excessive alcohol consumption while breastfeeding could also affect the infant’s sleep patterns and early development.
Alcohol and Caregivers
Caring for an infant while intoxicated is not safe. Drinking alcohol could impair a caregiver’s judgement and his or her ability to safely care for an infant. If a caregiver drinks excessively, he or she should arrange for a sober adult to care for the infant during this time.
Drinking alcohol could impair a caregiver’s judgement and his or her ability to safely care for an infant. If a caregiver drinks excessively, he or she should arrange for a sober adult to care for the infant during this time.
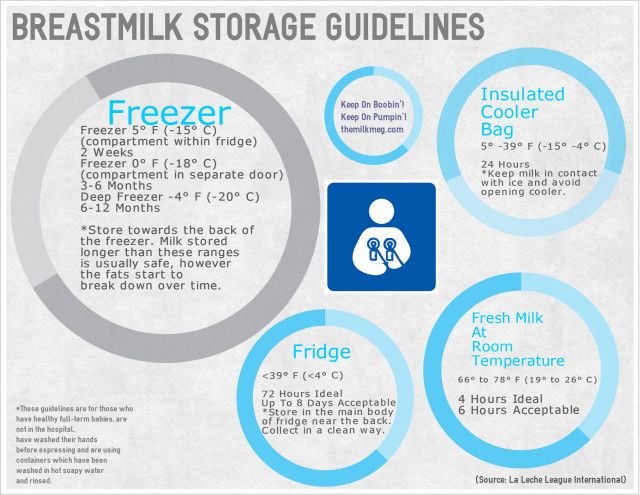
Can expressing/pumping breast milk after consuming alcohol reduce the alcohol in the mother’s milk?
No. The alcohol level in breast milk is essentially the same as the alcohol level in a mother’s bloodstream. Expressing or pumping milk after drinking alcohol, and then discarding it (“pumping and dumping”), does NOT reduce the amount of alcohol present in the mother’s milk more quickly. As the mother’s alcohol blood level falls over time, the level of alcohol in her breast milk will also decrease. A mother may choose to express or pump milk after consuming alcohol to ease her physical discomfort or adhere to her milk expression schedule. If a mother decides to express or pump milk within two hours (per drink) of consuming alcohol, the mother may choose to discard the expressed milk. If a mother has consumed more than a moderate amount of alcohol, she may choose to wait 2 hours (per drink) to breastfeed her child, or feed her infant with milk that had been previously expressed when she had not been drinking, to reduce her infant’s exposure to alcohol. Breast milk continues to contain alcohol as long as alcohol is still in the mother’s bloodstream.
If a mother has consumed more than a moderate amount of alcohol, she may choose to wait 2 hours (per drink) to breastfeed her child, or feed her infant with milk that had been previously expressed when she had not been drinking, to reduce her infant’s exposure to alcohol. Breast milk continues to contain alcohol as long as alcohol is still in the mother’s bloodstream.
Alcohol and breastfeeding: What are the risks?
The harmful effects of alcohol use during pregnancy are well-established.1 We know much less, however, about the consequences of alcohol intake in breastfeeding women and their infants. In the clinic when we review a patient’s medical history, we regularly query women about their use of tobacco, alcohol, and other substances, and we advise women regarding the deleterious effects of these substances when taken during pregnancy.
There seems, however, to be considerable variation in what is recommended for breastfeeding women. With regard to the consumption of alcohol by breastfeeding women, some health care providers urge abstinence, while others state that alcohol consumption by breastfeeding women carries little risk. 2
2
In a recent review, Haastrup and colleagues reported that the prevalence of alcohol consumption in breastfeeding women is high, ranging from
36% to 83% in developed countries.3 Epidemiological studies have shown that while breastfeeding women were less likely to report binge drinking, patterns of drinking at 1 and 3 months after giving birth did not differ significantly between women who chose to breastfeed and women who never breastfed.4
Although information regarding the effects of alcohol consumption on breastfeeding women and their infants is limited, it is essential that women receive accurate information regarding the potential risks of exposure to alcohol transferred to the infant as a result of breastfeeding.
PK and metabolism of alcohol in mother and infant
Alcohol consumed by a mother passes freely into her breast milk; alcohol levels in breast milk are similar to those measured in maternal blood and peak 30 to 60 minutes after an alcoholic beverage is consumed. 3 The amount of alcohol taken in by a nursing infant through breast milk is estimated to be 5% to 6% of the weight-adjusted maternal dose.3
3 The amount of alcohol taken in by a nursing infant through breast milk is estimated to be 5% to 6% of the weight-adjusted maternal dose.3
Alcohol can typically be detected in breast milk for about 2 to 3 hours after a single drink is consumed. However, it must be noted that the length of time alcohol can be detected in breast milk increases according to the amount of alcohol a mother consumes. Alcohol from 1 drink can be detected in breast milk for about 2 to 3 hours but the time period extends to about 4 to 5 hours if a mother consumes 2 drinks and to about 6 to 8 hours if she consumes 3 drinks, and so forth. Other factors influencing the amount of alcohol in breast milk include how fast it is consumed, whether it is consumed with food, the mother’s body weight, and individual variations in alcohol absorption and metabolism.3,5
Blood alcohol levels in a nursing infant depend on the amount of alcohol in breast milk, but also on the infant’s capacity to metabolize alcohol. In a newborn, alcohol is metabolized at 25% to 50% of the rate observed in adults.3,6
In a newborn, alcohol is metabolized at 25% to 50% of the rate observed in adults.3,6
Alcohol and milk production
Breastfeeding women are sometimes told they should drink alcohol to boost breast milk production and that the nutrients contained in dark stout beers, like Guinness, help to nourish the baby. In the early 1900s, beer companies marketed low-alcohol beers or “tonics” specifically for nursing women as a means of increasing their strength and enhancing breast milk production.7,8
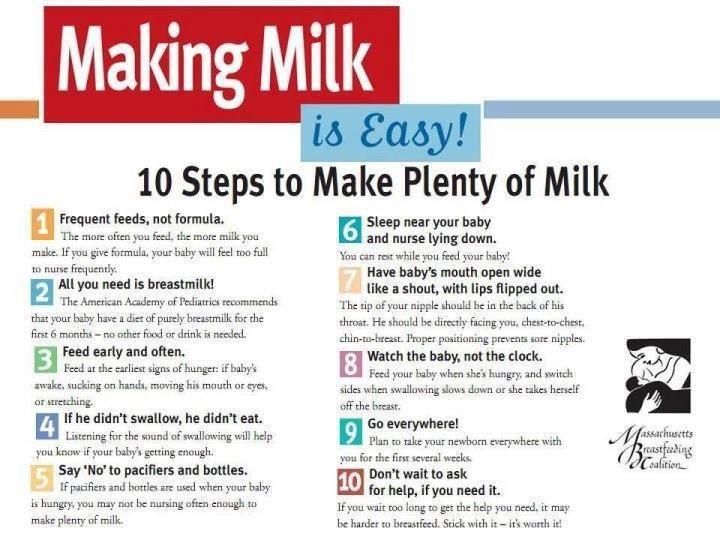
Like many old wives’ tales, there is a grain of truth to these recommendations. The barley used to make beer contains a polysaccharide that increases prolactin production, which in turn stimulates breast milk production.7 However, alcohol on its own actually decreases milk production.
Alcohol also is a potent inhibitor of oxytocin. Because of this effect, it was used clinically in the 1970s to stop contractions and prevent preterm birth. In a nursing mother, however, release of oxytocin associated with ingestion of alcohol stimulates milk ejection, which may also decrease the amount of milk available to the nursing infant.9 The higher the alcohol intake, the greater the effect; however, one study noted that drinking as little as 0.3 g of alcohol per kg (which is less than the amount considered acceptable by the American Academy of Pediatrics) reduced milk production by about 10%.10
In a nursing mother, however, release of oxytocin associated with ingestion of alcohol stimulates milk ejection, which may also decrease the amount of milk available to the nursing infant.9 The higher the alcohol intake, the greater the effect; however, one study noted that drinking as little as 0.3 g of alcohol per kg (which is less than the amount considered acceptable by the American Academy of Pediatrics) reduced milk production by about 10%.10
Short-term effects of alcohol on a nursing infant
Studies have shown that infants breastfed by women who had consumed alcohol prior to nursing consumed approximately 20% less milk in the first 4 hours after maternal alcohol consumption than women who did not drink.7 However, a subsequent study reported that, if mothers did not consume any more alcohol, babies breastfed more frequently and consumed larger amounts of milk in the 8 to 12 hours after maternal alcohol consumption. 11
11
Although some have speculated that this reduction in infant milk consumption may be caused by changes in the taste of the milk, it is probably more related to decreased supply. In fact, Mennella observed that infants actually consumed larger amounts of alcohol-enriched milk than plain breast milk, when provided to them in a bottle.12
Changes in infants’ sleep patterns have also been observed.7,13,14 While 2 studies reported that the total amount of sleep was unchanged after consuming alcohol-containing milk, these studies noted that the sleep was more fragmented.7,13 In contrast, another study demonstrated that total duration of sleep decreased on average by about 25% after infants consumed alcohol-containing milk.14
Long-term effects of alcohol on a nursing infant
Possible long-term effects on infants of alcohol delivered in mother’s milk are less studied, with only a handful of the studies looking at neurodevelopmental outcomes in exposed infants. However, this may be a particularly difficult area of research. Not only must we consider the direct effects related to alcohol exposure via breast milk, it is possible that alcohol consumed by the mother may have an effect on a developing child by altering the mother’s behavior or her capacity to parent.
However, this may be a particularly difficult area of research. Not only must we consider the direct effects related to alcohol exposure via breast milk, it is possible that alcohol consumed by the mother may have an effect on a developing child by altering the mother’s behavior or her capacity to parent.
In a study of 400 infants, Little and colleagues investigated infant development at age 1 year in relation to maternal use of alcohol while breastfeeding.15 Cognitive development, as measured using the Bayley Mental Development Index (MDI), was not affected by maternal use of alcohol. However, indices of motor development, as measured using the Psychomotor Development Index (PDI), were significantly lower in infants exposed regularly to alcohol in breast milk (even after controlling for prenatal alcohol exposure). The researchers observed an inverse dose-response relationship between the frequency of maternal alcohol consumption and scores on the PDI. Infants of breastfeeding mothers who had 1 or more drinks daily had a mean PDI score of 98, compared to a mean score of 103 in infants exposed to less alcohol in breast milk (95% confidence interval of the mean difference, 1.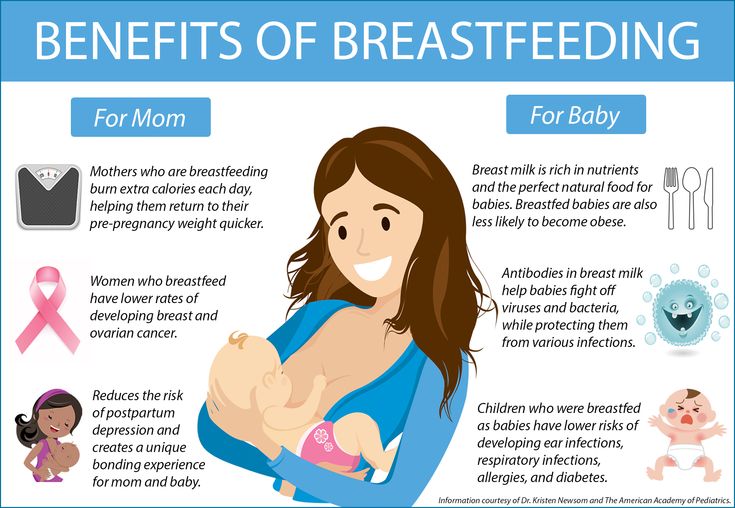 2 to 9.8). This association persisted after controlling for more than 100 potential confounding variables, including smoking and use of other drugs. In addition, the effect was more pronounced when mothers who supplemented breastfeeding with formula were excluded from the analysis.
2 to 9.8). This association persisted after controlling for more than 100 potential confounding variables, including smoking and use of other drugs. In addition, the effect was more pronounced when mothers who supplemented breastfeeding with formula were excluded from the analysis.
However, in a similar study from the same group, there was no association between scores on the Griffiths Developmental Scales and alcohol exposure in a group of 18-month-old children.16 The researchers note that, while the Bayley and Griffith Scales are comparable in terms of their ability to detect neurodevelopmental deficits, these tests, when used in infants and toddlers, are limited in their ability to detect small effects. They suggest that studies of older children may be of greater utility in assessing the effects of drinking while nursing.
More recently, data were analyzed from Growing Up in Australia: The Longitudinal Study of Australian Children, which included 5107 Australian infants and their caregivers recruited in 2004. 17 Information on breastfeeding, alcohol use, and other demographic variables were collected at baseline, and the children were assessed every 2 years. Heavier maternal alcohol consumption at the initial assessment was associated with dose-dependent reductions in abstract reasoning at ages 6 to 7 years in children who had been breastfed. This association was not observed in infants who had never breastfed, suggesting that exposure to alcohol via breastmilk, rather than psychosocial or environmental factors associated with that exposure, was responsible for the reductions in cognitive functioning observed in breastfed infants. This finding was independent of prenatal alcohol use, sex of child, maternal age, income, birth weight, and breastfeeding duration. Smoking while breastfeeding did not impact any of the outcomes studied.
17 Information on breastfeeding, alcohol use, and other demographic variables were collected at baseline, and the children were assessed every 2 years. Heavier maternal alcohol consumption at the initial assessment was associated with dose-dependent reductions in abstract reasoning at ages 6 to 7 years in children who had been breastfed. This association was not observed in infants who had never breastfed, suggesting that exposure to alcohol via breastmilk, rather than psychosocial or environmental factors associated with that exposure, was responsible for the reductions in cognitive functioning observed in breastfed infants. This finding was independent of prenatal alcohol use, sex of child, maternal age, income, birth weight, and breastfeeding duration. Smoking while breastfeeding did not impact any of the outcomes studied.
Clinical implications
While these studies raise concerns about the impact of alcohol on a nursing infant, there are many different patterns of alcohol consumption, and it would be erroneous to assume that having an occasional drink carries the same risk as chronic, heavy drinking or binge drinking. Our understanding of the impact of alcohol consumption is made even more complicated by the fact that there are genetic, psychosocial, cultural, and economic factors that go along with and influence alcohol consumption; these factors may also significantly impact children’s outcomes.
Our understanding of the impact of alcohol consumption is made even more complicated by the fact that there are genetic, psychosocial, cultural, and economic factors that go along with and influence alcohol consumption; these factors may also significantly impact children’s outcomes.
All pregnant and postpartum women should be queried regarding their past and present use of alcohol. National surveys indicate that about 1 in 2 women aged 18 to 44 drink alcohol, and 18% of women who drink alcohol in this age group binge drink. While many women with alcohol use disorders are able to abstain from drinking during pregnancy, relapse rates are high after delivery.18 In addressing maternal use of alcohol, screening for problematic patterns of use and offering treatment when appropriate may help to reduce behaviors that put an infant at risk.
Proximate to delivery, all women should be provided information regarding use of alcohol while breastfeeding. Although the information is incomplete, our current data indicate that maternal alcohol consumption may affect milk production and infant sleep patterns. In addition, the most current studies indicate that alcohol passed through breast milk may have adverse neurodevelopmental effects.
In addition, the most current studies indicate that alcohol passed through breast milk may have adverse neurodevelopmental effects.
Guidelines regarding use of alcohol are varied. According to the most recent recommendations on breastfeeding from the AAP,2 “ingestion of alcoholic beverages should be minimized and limited to an occasional intake but no more than 0.5 g alcohol per kg body weight, which for a 60 kg mother is approximately 2 oz liquor, 8 oz wine, or 2 beers.” Furthermore, they recommend that mothers avoid nursing their infants for 2 hours after their last drink to allow for the alcohol to be cleared from the breast milk.
The Motherisk program in Toronto, Canada, has issued more conservative recommendations,18 stating, “At this time, there are no known benefits of exposing nursing infants to alcohol. Although occasional drinking while nursing has not been associated with overt harm to infants, the possibility of adverse effects has not been ruled out.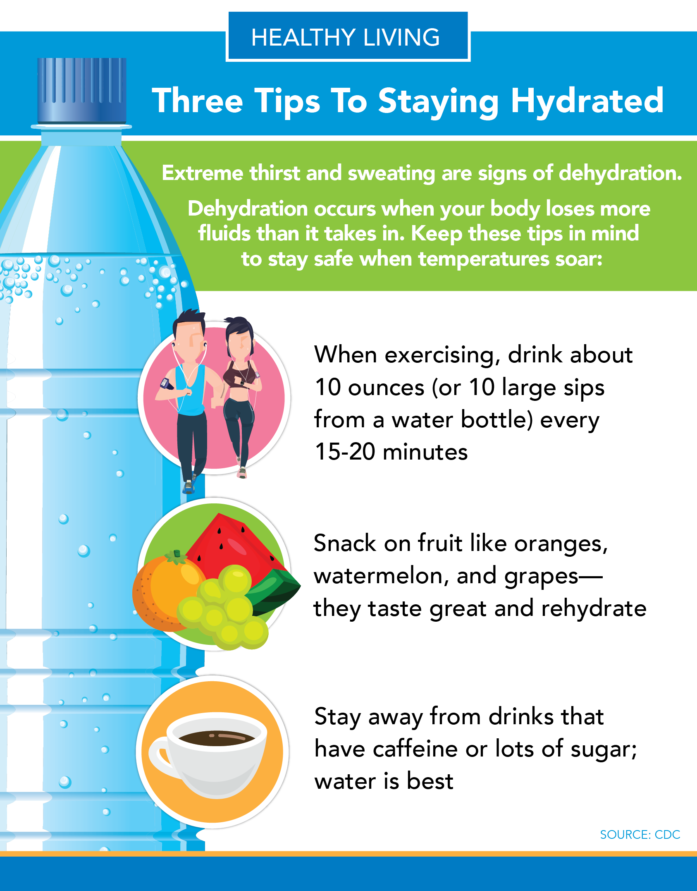 Occasional drinking, however, does not warrant discontinuing breastfeeding, as the benefits of breastfeeding are extensive and well recognized. Until a safe level of alcohol in breast milk is established, no alcohol in breast milk is safest for nursing babies. It is, therefore, prudent for mothers to delay breastfeeding their babies until alcohol is completely cleared from their breast milk.”
Occasional drinking, however, does not warrant discontinuing breastfeeding, as the benefits of breastfeeding are extensive and well recognized. Until a safe level of alcohol in breast milk is established, no alcohol in breast milk is safest for nursing babies. It is, therefore, prudent for mothers to delay breastfeeding their babies until alcohol is completely cleared from their breast milk.”
To minimize exposure, Motherisk has developed a nomogram that can be used to help mothers who choose to drink alcohol while breastfeeding estimate how long it takes to clear alcohol from breast milk, taking into consideration body weight and number of drinks (Table 1).
Information about the long-term effects of exposure to alcohol during breastfeeding remains lacking. Therefore, to minimize the risk of adverse events in nursing children, it is best to counsel mothers on adhering to recommendations from healthcare authorities on alcohol intake in breastfeeding women
Disclosures:
The author reports no potential conflicts of interest with regard to this article.
References:
- Georgieff MK, Tran PV, Carlson ES. Atypical fetal development: Fetal alcohol syndrome, nutritional deprivation, teratogens, and risk for neurodevelopmental disorders and psychopathology. Dev Psychopathol. 2018;30(3):1063-1086.
- Breastfeeding SO. Breastfeeding and the use of human milk. Pediatrics. 2012;129(3):e827-e841.
- Haastrup MB, Pottegård A, Damkier P. Alcohol and breastfeeding. Basic Clin Pharmacol Toxicol. 2014;114(2):168-173.
- Little RE, Lambert MD, Worthington-Roberts B. Drinking and smoking at 3 months postpartum by lactation history. Paediatr Perinat Epidemiol. 1990;4(3):290-302.
- Koren G. Drinking alcohol while breastfeeding. Will it harm my baby? Can Fam Physician Med Fam Can. 2002;48:39-41.
- Pikkarainen PH, Räihä NC. Development of alcohol dehydrogenase activity in the human liver. Pediatr Res. 1967;1(3):165-168.
- Mennella JA, Beauchamp GK. Beer, breast feeding, and folklore.
 Dev Psychobiol. 1993;26(8):459-466.
Dev Psychobiol. 1993;26(8):459-466.
- Bryce E. Should breast-feeding women really drink Guinness? LiveScience. https://www.livescience.com/63122-breastfeeding-moms-guinness-beer.html. Accessed September 8, 2018.
- Mennella JA, Pepino MY, Teff KL. Acute alcohol consumption disrupts the hormonal milieu of lactating women. J Clin Endocrinol Metab. 2005;90(4):1979-1985.
- Mennella JA. Short-term effects of maternal alcohol consumption on lactational performance. Alcohol Clin Exp Res. 1998;22(7):1389-1392.
- Mennella JA. Regulation of milk intake after exposure to alcohol in mothers’ milk. Alcohol Clin Exp Res. 2001;25(4):590-593.
- Mennella JA. Infants’ suckling responses to the flavor of alcohol in mothers’ milk. Alcohol Clin Exp Res. 1997;21(4):581-585.
- Mennella JA, Garcia-Gomez PL. Sleep disturbances after acute exposure to alcohol in mothers’ milk. Alcohol Fayettev N. 2001;25(3):153-158.
- Mennella JA, Gerrish CJ.
 Effects of exposure to alcohol in mother’s milk on infant sleep. Pediatrics. 1998;101(5):E2.
Effects of exposure to alcohol in mother’s milk on infant sleep. Pediatrics. 1998;101(5):E2.
- Little RE, Anderson KW, Ervin CH, Worthington-Roberts B, Clarren SK. Maternal alcohol use during breast-feeding and infant mental and motor development at one year. N Engl J Med. 1989;321(7):425-430.
- Little RE, Northstone K, Golding J, ALSPAC Study Team. Alcohol, breastfeeding, and development at 18 months. Pediatrics. 2002;109(5):E72-72.
- Gibson L, Porter M. Drinking or smoking while breastfeeding and later cognition in children. Pediatrics. 2018;142(2).
- Forray A, Merry B, Lin H, Ruger JP, Yonkers KA. Perinatal substance use: a prospective evaluation of abstinence and relapse. Drug Alcohol Depend. 2015;150:147-155.
Feeding when sick | Medela
If you or your baby are unwell, you may wonder if it is safe to breastfeed. The great news is that breastfeeding when you're sick is most often good for both of you. Read more about this in our article.
Read more about this in our article.
Share this information
Did you know that a breastfed baby is usually much less prone to illness? Although it is impossible to avoid them completely, the protective properties of breast milk help babies get sick less often 1 and recover faster than formula-fed babies.
Breast milk contains antibacterial and antiviral agents. 2 The longer you breastfeed your baby, the lower the risk of colds and flu, ear and respiratory infections, nausea and diarrhea. 1 Scientists are already exploring the use of breast milk to treat everything from conjunctivitis to cancer. 3.4
Should a sick baby be breastfed? nine0021
Yes. Breastfeeding promotes recovery and also helps to calm the baby. Breast milk contains antibodies, white blood cells, stem cells, and protective enzymes that help fight infections and help your baby recover faster. 1,5,6 In addition, the composition of breast milk (the balance of vitamins and nutrients) is constantly adjusted to the baby's body to help him recover as soon as possible. Thus, you will spend less time on sick leave and visit the doctor less often. nine0009 7
1,5,6 In addition, the composition of breast milk (the balance of vitamins and nutrients) is constantly adjusted to the baby's body to help him recover as soon as possible. Thus, you will spend less time on sick leave and visit the doctor less often. nine0009 7
“Breastfeeding gives the baby everything she needs when she is sick. This is his medicine, food, drink and comfort. For a baby, this is the best thing in the world,” says Sarah Beeson, a health visitor from the UK.
Surprisingly, when a child becomes ill, the composition of breast milk changes. When you come into contact with pathogens of bacterial and viral infections, your body begins to produce antibodies to fight them, which are then passed through milk to your baby. nine0009 8 When your baby is sick, your milk also spikes in immune-boosting cells (white blood cells). 5
In addition, breast milk is very easy to digest, making it ideal for babies with indigestion.
“At 12 months my daughter contracted norovirus and could only breastfeed,” recalls Maya, a mother of two in Spain. produce more milk. It was amazing. After 48 hours, I was able to meet the daily requirement for milk. It saved my baby from a drip." nine0003
It should be taken into account that sometimes during an illness it is necessary to change the habitual breastfeeding regimen. For example, with a cold, a baby may want to eat more often, but little by little, both to calm down and because of nasal congestion, which makes it difficult to apply to the chest for a long time. If your baby has a stuffy nose, an upright breastfeeding position may be more comfortable, so don't be afraid to try different breastfeeding positions.
What should I do if my baby is seriously unwell and cannot breastfeed? nine0021
Occasionally, if a child feels unwell, they may not have an appetite or the strength to feed. If your baby is not eating well, seek advice from your healthcare provider, nurse practitioner, or lactation consultant to help prevent dehydration.
You may be asked to express milk to feed your baby with a bottle, a Soft Cup*, or other suitable method that requires minimal effort from the baby. Pumping on a regular breastfeeding schedule will also help keep your milk supply stable. nine0003
You can express milk with one of our convenient breast pumps, such as the modern electronic Swing Flex** or the Harmony** manual breast pump. Rest assured, freshly expressed breast milk is just as good as breast milk, so your baby will get all the protection and support it needs.
If you have concerns about your baby's health or how much milk they are drinking, see your doctor as soon as possible.
Can I continue to breastfeed if I become ill myself? nine0021
You may not want to do this if you feel unwell, but in most cases it is best to continue breastfeeding. If you have a cold, runny nose, diarrhoea, vomiting, or mastitis, continue breastfeeding as normal with your doctor's approval. The baby is unlikely to become infected through breast milk. What's more, the antibodies in your milk will help reduce your baby's risk of contracting the same 13 virus.
What's more, the antibodies in your milk will help reduce your baby's risk of contracting the same 13 virus.
“Breastfeeding when sick is not only safe most of the time, but also beneficial. Your baby is the least at risk of catching your upset stomach or cold, as he is already in close contact with you and receives a daily dose of protective antibodies from milk, ”says Sarah Beeson. nine0003
If there is a risk of contracting a viral infection by airborne droplets, it is advisable to temporarily switch to expressing breast milk and bottle feeding.
In order not to lose the amount of milk produced when the body is still weakened by the disease, it is best to use the Swing Maxi Flex ** double breast pump, which helps to stimulate lactation, increase the amount of milk (by 18% on average) and increase its fat content (+1% ) 14 .
However, breastfeeding and pumping when sick can be very tiring. You need to take care of yourself so that you can take care of the baby. Try to drink more fluids, eat when you can, and get plenty of rest. Crawl under the covers for a few days and ask family or friends to help care for your baby if possible, so you can put all your energy into recovery. nine0003
Try to drink more fluids, eat when you can, and get plenty of rest. Crawl under the covers for a few days and ask family or friends to help care for your baby if possible, so you can put all your energy into recovery. nine0003
“Don't worry about your milk supply, it will last. Most importantly, do not stop breastfeeding abruptly so that mastitis does not develop, ”adds Sarah.
Proper hygiene is very important to reduce the risk of spreading the disease. Wash your hands with soap and water before and after breastfeeding and pumping, preparing and eating food, using the toilet and changing diapers. Use a tissue when coughing and sneezing, or cover your mouth with the crook of your elbow (not your palm) if you don't have a tissue handy. Be sure to wash or sanitize your hands after coughing, sneezing, and blowing your nose. nine0003
Can I take medication while breastfeeding?
In agreement with the attending physician and compliance with the dosage, certain medications are allowed. 9.10
9.10
.
“When talking to a doctor or pharmacist for any reason, always state that you are breastfeeding,” she continues. nine0003
What about long-term treatment?
If you are on long-term treatment for diabetes, asthma, depression, or other chronic conditions, the benefits of breastfeeding may outweigh the risks. “Breastfeeding is often possible for almost any disease, with the exception of some very rare conditions,” Sarah says, “you will be very familiar with the drugs you are taking, and during pregnancy you can discuss them with your doctor or other specialist. There is guidance on the safe use of various medicines that all healthcare professionals use.” In any case, you should consult with your doctor. nine0003
“I was on high doses of epilepsy medication, but I was still able to breastfeed,” recalls Nicola, a mother from the UK. “I saw a neurologist to ensure my son was safe and to minimize the risk of a seizure. Seizures can happen due to lack of sleep, and I fed day and night, but I took good care of myself, and my husband supported me. It was a positive experience."
It was a positive experience."
What if I have to go to the hospital?
If you need to be hospitalized or urgently hospitalized, there are different ways to continue feeding your baby healthy breast milk so that you can return to normal breastfeeding after you are discharged. nine0003
“Express and freeze breast milk so that the caregiver can feed the baby. Practice at home ahead of time and be sure to let your doctors know that you are a breastfeeding mother, both before entering the hospital and while in it, ”recommends Sarah.
“If the baby is very small, you may be allowed to take him with you. Find out if the hospital has a supervising doctor or lactation consultant to contact. This specialist will support you, especially if you are in a general ward. If hospitalization is urgent, warn the doctors that you have a baby so that they take this into account. nine0003
Surgery under local or general anesthesia does not necessarily mean that breastfeeding will have to be stopped, or milk will need to be pumped and discarded.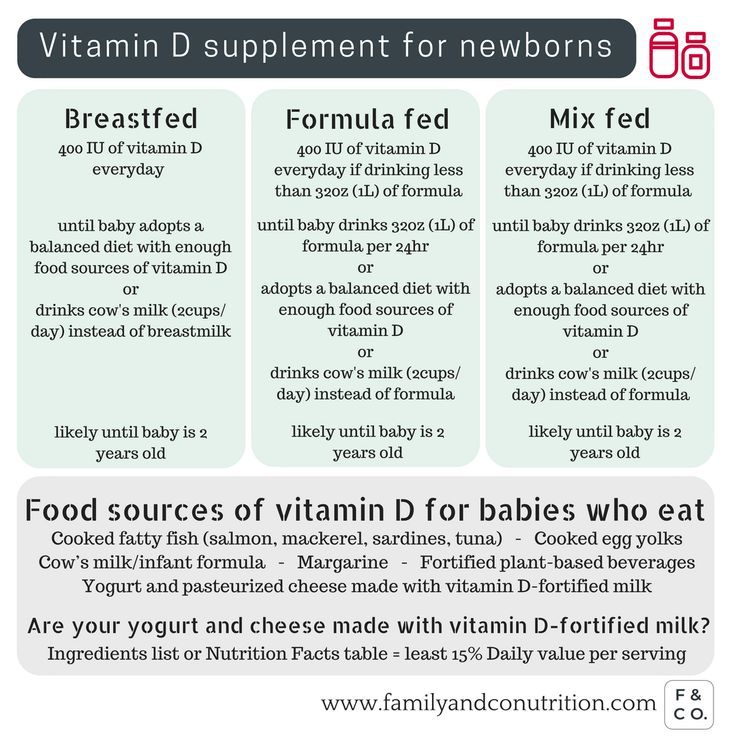 By the time you recover from surgery and can hold your baby, the amount of anesthetic in your breast milk will be minimal, so breastfeeding will be safe in most cases. 10 However, it is always best to consult your doctor or attending physician beforehand. nine0003
By the time you recover from surgery and can hold your baby, the amount of anesthetic in your breast milk will be minimal, so breastfeeding will be safe in most cases. 10 However, it is always best to consult your doctor or attending physician beforehand. nine0003
To ensure that the situation of treatment or departure does not affect the baby's diet, it is advisable to create a breast milk bank. This should be done daily by expressing one extra serving and freezing it in the handy, durable Medela Breast Milk Storage Bags. Even stored for several months and then thawed, your carefully prepared milk will still be incomparably healthier than formula.
For hygienic and easy pumping, use a breast pump with 2-Phase Expression technology for a fast, full flow of milk. For example, the ultra-comfortable Swing Flex** breastpump that adapts to the shape of your breasts and allows you to pump milk in a comfortable position, even lying back on the pillows 15 .
Don't forget to sterilize your breast pump with the Quick Clean microwave bags. Medela milk storage bags do not need to be handled as they are aseptically packaged and ready to use immediately.
Are there times when breastfeeding is not allowed?
In some cases, for the safety of the baby, breastfeeding should be stopped for a while, and instead, milk should be expressed and discarded to maintain milk production until the end of treatment. This includes radiotherapy and chemotherapy for cancer, herpes sores on the chest, and infections such as tuberculosis, measles, or blood poisoning that can be transmitted through breast milk. nine0009 11.12 Consult with a qualified professional about your condition to decide whether breastfeeding can continue in such cases.
For quality lactation support during this period, you can use the dual electronic breast pump with innovative Flex technology or rent a Symphony Clinical Breast Pump** if possible. A list of cities where you can rent a breast pump can be found on the "Rent a Medela Clinical Breast Pump" page. nine0003
nine0003
Literature
1 Victora CG et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet . 2016;387(10017):475-490. - Victor S.J. et al., "Breastfeeding in the 21st century: epidemiology, mechanisms and long-term effects". Lancet 2016;387(10017):475-490.
2 Lönnerdal B. Bioactive proteins in breast milk. J Pediatric Child Health. nine0120 2013;49 Suppl 1:1-7. - Lönnerdahl B., "Biologically active proteins of breast milk". F Pediatrician Child Health. 2013;49 Suppl 1:1-7.
3 Australian Breastfeeding Association [Internet]. Topical treatment with breastmilk: randomized trials. [ cited 2018 Apr 4]. Available from https://www.breastfeeding.asn.au - Australian Breastfeeding Association [Internet].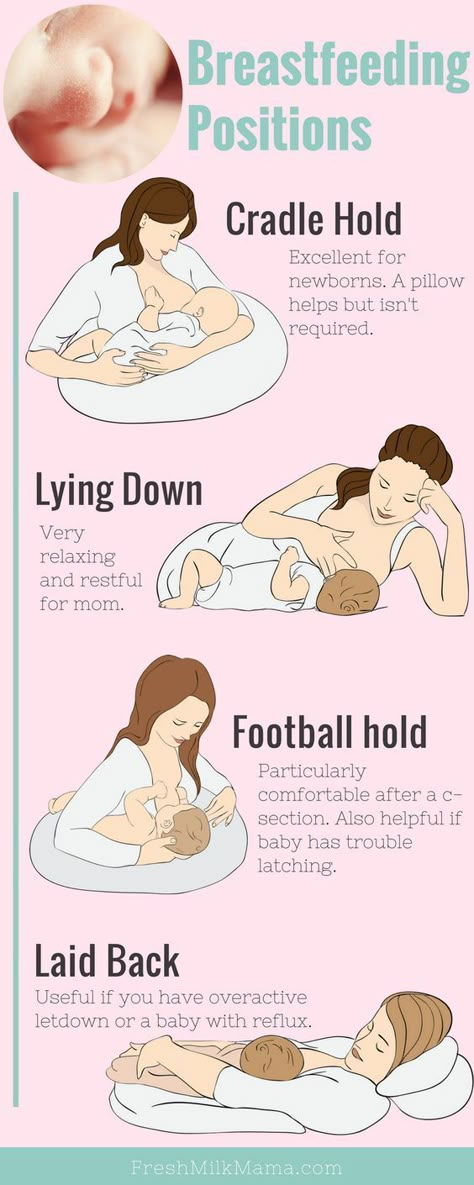 "Topical treatment with breast milk: a randomized trial". [cited 4 April 2018] See article at https://www.breastfeeding.asn.au
"Topical treatment with breast milk: a randomized trial". [cited 4 April 2018] See article at https://www.breastfeeding.asn.au
4 Ho JCS et al. HAMLET–A protein-lipid complex with broad tumoricidal activity. Biochem Biophys Res Commun. 2017;482(3):454-458. - Ho J.S.S. et al., "HAMLET - a protein-lipid complex with extensive antitumor activity". Biochem Biophys Res Comm. 2017;482(3):454-458. nine0120
5 Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin Transl Immunology . 2013;2(4): e 3. - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
6 Hassiotou F, Hartmann PE. At the dawn of a new discovery: the potential of breast milk stem cells . Adv Nutr . 2014;5(6):770-778. - Hassiot F, Hartmann PI, "On the threshold of a new discovery: the potential of breast milk stem cells." Adv. 2014;5(6):770-778.
Adv Nutr . 2014;5(6):770-778. - Hassiot F, Hartmann PI, "On the threshold of a new discovery: the potential of breast milk stem cells." Adv. 2014;5(6):770-778.
7 Ladomenou F et al. Protective effect of exclusive breastfeeding against infections during infancy: a prospective study. Arch Dis Child . 2010;95(12):1004-1008. - Ladomenu, F. et al., "The effect of exclusive breastfeeding on infection protection in infancy: a prospective study." Arch Dis Child. 2010;95(12):1004-1008.
8 Hanson LA. Breastfeeding provides passive and likely long-lasting active immunity. Ann Allergy Asthma Immunol . 1998;81(6):523-533. — Hanson, L.A., "Breastfeeding provides passive and likely long-term active protection against disease." Ann Allergy Asthma Immunol. 1998;81(6):523-533.
1998;81(6):523-533.
9 Hale TW, Rowe HE. Medications and Mothers' Milk 2017. 17th ed. New York, USA: Springer Publishing Company; 2017. 1095 p . — Hale T.W., Rowe H.I., Medications and Breast Milk 2017. 17th edition. New York, USA: Publishing House Springer Publishing Company ; 2017. p. 1095.
10 Reece-Stremtan S et al. ABM Clinical Protocol# 15: Analgesia and anesthesia for the breastfeeding mother, Revised 2017. Breastfeed Med . 2017;12(9):500-506. - Rees-Stromtan S. et al., AVM Clinical Protocol #15: Analgesia and Anesthesia for Nursing Mothers, 2017 edition. Brestfeed Med (Breastfeeding Medicine). nine0120 2017;12(9):500-506.
11 Lamounier JA et al. Recommendations for breastfeeding during maternal infections. J Pediatr 2004;80(5 Suppl ):181-188. - Lamunier J.A. et al., Guidelines for Breastfeeding during Maternal Infectious Diseases. J Pediatrician (Journal of Pediatrics) (Rio J). 2004;80(5 Suppl):181-188. nine0120
- Lamunier J.A. et al., Guidelines for Breastfeeding during Maternal Infectious Diseases. J Pediatrician (Journal of Pediatrics) (Rio J). 2004;80(5 Suppl):181-188. nine0120
12 Hema M et al., Management of newborn infant born to mother suffering from tuberculosis: Current recommendations & gaps in knowledge. Indian J Med Res . 2014;140(1):32-39. - Hema M. et al., "Working with the Infant Born to a Mother with Tuberculosis: Current Recommendations and Gaps". Indian W Med Res. 2014;140(1):32-39.
13 Lönnerdal B. Nutritional and physiologic significance of human milk proteins. Am JClin Nutr. 2003;77(6):1537S-1543S. Lönnerdahl B., "Biologically active proteins of breast milk". F Pediatrician Child Health. 2013;49 Suppl 1:1-7
14 Prime et al., Simultaneous Breast Expression in Breastfeeding Women Is More Efficacious Than Sequential Breast Expression, Breastfeed Med. Dec 2012; 7(6): 442–447. Prime DK and co-authors. "During the period of breastfeeding, simultaneous pumping of both breasts is more productive than sequential pumping." Brestfeed Med (Breastfeeding Medicine). 2012;7(6):442-447. nine0120
Dec 2012; 7(6): 442–447. Prime DK and co-authors. "During the period of breastfeeding, simultaneous pumping of both breasts is more productive than sequential pumping." Brestfeed Med (Breastfeeding Medicine). 2012;7(6):442-447. nine0120
15 ClinicalTrials.gov [Internet]. Bethesda MD: National Library of Medicine, USA, data on file: NCT03091985. Clinical Research.gov [Internet]. Bethesda MD: National Library of Medicine, USA, data on file: NCT03091985.
Check out the instructions, consult with a specialist
* Ru FSZ 2010/07353 dated 07/19/10
** RU No. FCZ 2010/06525 dated 17/03/2021
9000 9000 9000 9000 9000
000 whether to supplement the baby with breastfeeding and artificial feeding, how much water a child can drink
The birth of a baby always involves a lot of questions from parents. Some of them are, of course, related to proper nutrition. And almost always, the first thing moms ask is whether it is necessary to give water during breastfeeding. Will it harm digestion and stool? And if supplemented, then with what water, how often and from what? Let's take a look at all the nuances in order.
Will it harm digestion and stool? And if supplemented, then with what water, how often and from what? Let's take a look at all the nuances in order.
Contents: Hide
- When a baby needs water
- What are the dangers of early water intake
- General recommendations for supplementation
When a baby needs water
breastfeeding, with normal assimilation of mother's milk and regular weight gain, water is not required. Mother's milk quenches thirst and protects against dehydration. However, there are doctors who express a different opinion from this. So, when should you supplement your newborn? nine0003
• With artificial and mixed feeding. Mixtures, even as close as possible in composition to mother's milk, are absorbed longer, and water helps their absorption. Therefore, the use of water in this case is mandatory.
• When breastfeeding with insufficient lactation. Unfortunately, it happens that the mother's milk is not enough for the baby. If the baby cries often, does not gain weight, supplement the baby with water and immediately contact the pediatrician about mixed feeding or a complete transition to the mixture. nine0003
If the baby cries often, does not gain weight, supplement the baby with water and immediately contact the pediatrician about mixed feeding or a complete transition to the mixture. nine0003
• In hot weather. When it's hot, fluid leaves the body much faster, and feeding a child with milk all the time means forcing him to overeat. Water in this case is your salvation.
• For hiccups. As you know, water helps to cope with hiccups. This is true not only for an adult, but also for a baby.
• For vomiting and diarrhea. They wash fluid out of the child's body, which threatens with dehydration. If you experience these problems, give your baby as much water as possible. nine0003
• To bring down high temperatures. If the baby is sick, his temperature has jumped, then the first advice given by all doctors, without exception, is to drink as much as possible. Milk at a high temperature is contraindicated, only fermented milk products are allowed. Therefore, the best way out for mommy will be to give the child some water.
• When the child is older than two months. If a newborn can only get by with mother's milk, then the baby is a little older - no longer. The body grows, as do its needs. Many pediatricians from 2.5 months already recommend to supplement the baby not only with water, but also with dried fruit compotes. nine0003
IMPORTANT! Irina Vostrikova, a pediatrician at the MEDSI clinic, believes that babies do not need to be supplemented, because breast milk is already 90% water. However, this may be necessary if the mother herself does not drink enough fluids. So, a nursing mother should drink at least 2 liters of ordinary non-carbonated water per day.
In hot weather, the baby can be offered water between feedings in a volume of 10-15 ml: if the baby refuses, then now he does not need additional liquid. The same recommendations are valid for artificial feeding. It is better to give water to the child with a spoon, and not from a bottle. Because when feeding from a bottle, the baby has a "sucking confusion", and he begins to take the breast incorrectly - because of this, the effectiveness of stimulating milk production is reduced, and the nipples are injured. nine0003
nine0003
What are the dangers of early water intake? What problems in a newborn can cause frequent water intake?
• Malnutrition. If you give your baby water shortly before feeding, the liquid will take place in the baby's stomach, and he will eat less milk. As a result, the baby will remain hungry, his body will receive fewer nutrients, and the mother will not empty the mammary glands, which threatens to stagnate milk and reduce lactation. nine0003
• Violation of the intestinal microflora. The use of water leads to the appearance in the body of a newborn of the first bacteria, which are not always beneficial. This is a load on the intestines, the likelihood of developing dysbacteriosis.
• Load on the kidneys. The introduction of water into the diet makes the kidneys work more intensively, and the body of a newborn baby may not be ready for this.
IMPORTANT! Elena Shmakova, consultant on breastfeeding and baby care at the Lada Center, teacher of the WHO/UNICEF course "Breastfeeding Counseling", adds that supplementation poses a risk to breastfeeding itself. The fact is that milk is produced in response to sucking, and its amount directly depends on the frequency of breast stimulation. If you give your baby water to drink, he will suckle less often and less, which means that the stimulation of the mammary glands will decrease. nine0003
The fact is that milk is produced in response to sucking, and its amount directly depends on the frequency of breast stimulation. If you give your baby water to drink, he will suckle less often and less, which means that the stimulation of the mammary glands will decrease. nine0003
She is sure that the baby should be supplemented only when breastfeeding does not help with the dehydration of the baby due to malaise. Dehydration can be detected, for example, when the number of urination is less than 6 per day, while the urine is concentrated, dark, it is less than usual.
Read also: Can children be given mineral water
General recommendations for supplementation
baby. nine0003
• Only purified water should be given. The best option would be to buy bottled water. Today in stores you can find bottles of water intended for children: it has gone through all possible purifications and is devoid of harmful bacteria. It is also possible to use well water at home, which has passed through special children's filters. Avoid using tap water, even filtered.
Avoid using tap water, even filtered.
• Use only boiled water. By doing this, you significantly reduce the risk of crumbs of harmful bacteria entering the body (almost all of them die when boiled). nine0003
• If possible, use silverware. Today, at affordable prices, you can find children's spoons and cups made of silverware. This metal has amazing properties to destroy pathogens. Pour water into a silver cup and let it steep. Alternatively, you can use silver water ionizers. This choice will be more economical
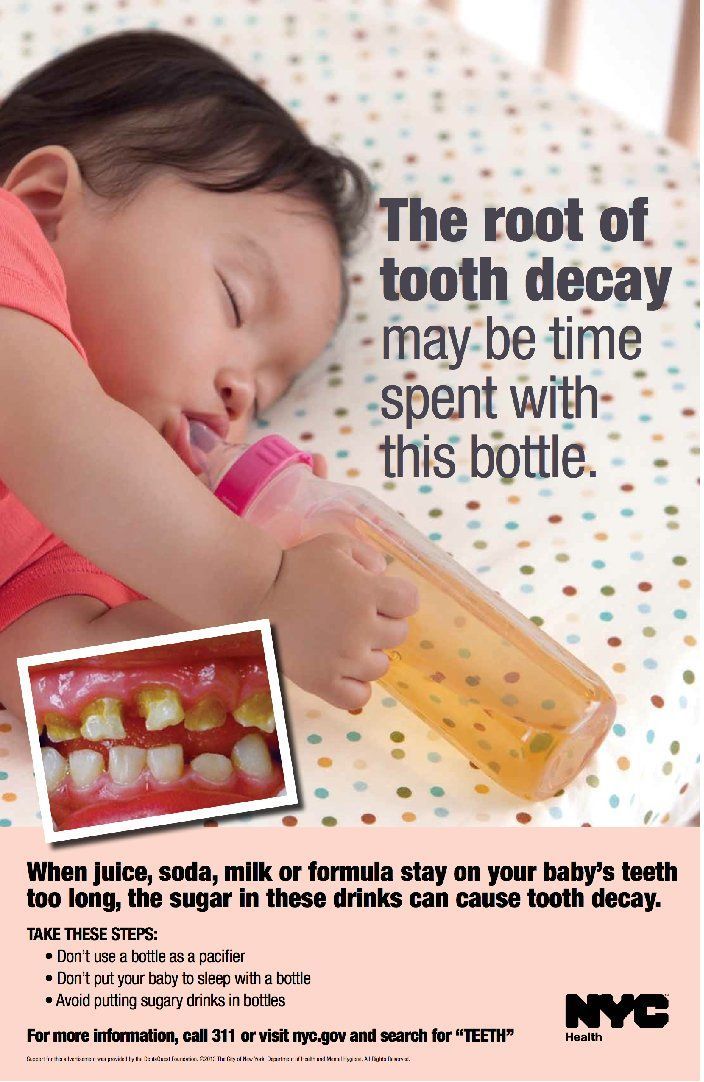
.• If the baby drinks mother's milk, water should be given from a spoon. Drinking from a bottle will be very easy for him, and he may eventually refuse to breastfeed
.• If the baby is healthy and is gaining weight well, then there is no need to insist and forcibly give him some water. So he has enough breast milk.
• Water should be given 10-15 minutes after feeding and between meals. In no case do not let us drink before meals: the crumbs will have a feeling of false satiety.