How to feed baby colostrum
Pumped Colostrum and How to Store It
Now reading: Liquid Gold: Pumped Colostrum and How to Store It
PrevNextThe birth of a baby is an exciting time, but it can also be overwhelming for new mothers. You’re faced with incredible physical and emotional demands, and the new chapter is only beginning. You’re now ready to take your first step along your breastfeeding journey.
It’s common for new mothers to struggle with nursing. In fact, 92% of new mothers struggle with breastfeeding in the first three days post-partum. Breastfeeding isn’t always successful on the first try. Babies often have difficulty latching on, and sometimes a mother’s milk supply isn’t abundant. Luckily, pumping is an effective way to express milk for the baby and helps produce and maintain milk supply for mom.
The earliest supply of milk – colostrum – has some of the most important nutrients mothers can supply their newborns. Colostrum is essential to babies in the first few days after birth. To set yourself up for success, it’s helpful to know what to do with pumped colostrum and how to store it.
Until full milk production begins two to three days after birth, new moms produce small amounts of colostrum. Also called “liquid gold,” this thick, yellowish milk is rich in nutrients and carbohydrates. In addition to providing essential nutrition to the baby, colostrum helps with digestion and bowel movements in newborns. This is important in ridding the baby’s body of toxins that can cause jaundice.
Colostrum is also high in white blood cells and antibodies that develop the baby’s immune system. It builds a protective coating in their digestive system that helps prevent the growth of disease-causing germs. It’s a baby super-food and is an invaluable asset to their health and well-being.
What to Do with Pumped ColostrumA baby only consumes small amounts of colostrum in its first days. Regardless, studies show that expressing these low quantities within the first hour of birth can prevent delays in milk production. If a newborn doesn’t nurse within six hours after birth, it’s a good idea for mom to begin pumping. Make sure your hands are clean and that any collection tools are sterilized for the baby’s safety. Once you’re ready to pump colostrum, you’ll want to follow these next steps.
If a newborn doesn’t nurse within six hours after birth, it’s a good idea for mom to begin pumping. Make sure your hands are clean and that any collection tools are sterilized for the baby’s safety. Once you’re ready to pump colostrum, you’ll want to follow these next steps.
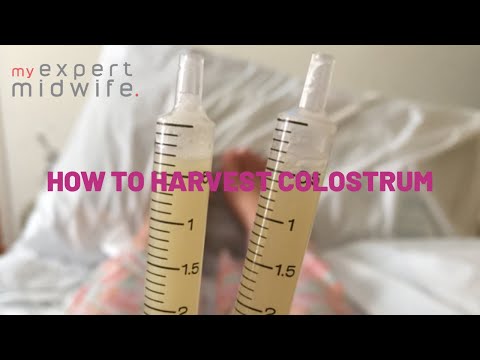
Many new moms prefer to use a syringe or Hegen’s revolutionary press-to-close, twist-to-open airtight storage bottles to collect colostrum. As you pump the breast, you’ll notice beads of liquid forming. Gather this in one of the containers and, once complete, put the syringe in a sealable baggie or close the bottle tightly. Then, write the date on the container so you can keep track of your stored supply.
2. Feed It to Your BabyOnce you’ve collected colostrum, it’s ready for consumption. You can administer it via a syringe or small bottle (remember, quantities will be relatively low). You can also feed drops of it to your baby on a clean finger. Every bit is packed with nutrients to help your baby’s development.
Every bit is packed with nutrients to help your baby’s development.
If your colostrum production is going well and you’re building up a steady supply, you can store it for future use. In fact, some women begin collecting their colostrum before the baby actually arrives. In a typical healthy pregnancy, there’s no need to express colostrum before giving birth. However, in some instances, it’s beneficial to collect colostrum toward the end of the pregnancy. Harvesting colostrum this early may be recommended if:
- You’re having twins – birth weight tends to be low for multiples.
- You have health concerns – gestational diabetes can affect the baby’s glucose levels at birth.
- Your baby has a cleft lip or palate – this can make breastfeeding difficult.
Whatever the case, pumped colostrum can be collected and saved for when the time is right.
4. Bring It to the Hospital
Bring It to the Hospital If you do decide to pump and store your colostrum before giving birth, be sure to include this in your hospital bag list to take along with you when you head to the hospital for delivery. Carry it in an insulated bag with ice packs and ask the nurse to store it in the maternity ward’s refrigerator until you’re ready to use it. This colostrum will be safe for use for up to 48 hours.
4 Tips for Storing ColostrumBreastfeeding mothers can ensure the safety and quality of expressed breast milk by following proper storing techniques. Consider these four tips for storing colostrum safely.
Properly Seal the ContainerTo maintain freshness and quality, be sure your storage container is completely sealed. Never use disposable bags or liners to store pumped colostrum. These aren’t designed to protect against bacteria and germ growth.
Consider Shelf LifeColostrum can be stored at room temperature for up to four hours. It can remain in a refrigerator for up to four days. You can store pumped colostrum in the freezer for up to six months (for best quality) or 12 months, at most. If you’re uncertain about how long your colostrum has been stored, it’s best to dispose of it. Better safe than sorry!
It can remain in a refrigerator for up to four days. You can store pumped colostrum in the freezer for up to six months (for best quality) or 12 months, at most. If you’re uncertain about how long your colostrum has been stored, it’s best to dispose of it. Better safe than sorry!
When storing expressed colostrum in the refrigerator or freezer, set the container at the back of the shelf where temperatures are coolest. Avoid storing it in the door compartment, as opening and closing the fridge will expose stored colostrum to frequent temperature changes that can negatively impact its quality and freshness.
Store It On-the-GoWith careful planning, it’s possible to travel safely with stored colostrum. Pack the container in an insulated bag and surround the colostrum with ice packs. It can remain safe for consumption this way for up to 24 hours. When your journey is over, use it right away or store it in the fridge or freezer.
Additional Colostrum Questions
We've received quite a few questions from moms who have reached out to us.
We will continually add to this post as we receive new questions and want to thank those who have helped to provide us with great questions that will eventually help so many other new moms!
Is Frozen Colostrum good for a sick baby?Yes, frozen colostrum does help a sick baby. Research studies have proven that sick or preterm infants who take colostrum from mothers have “significantly better health outcomes”. Colostrum is made up of immune factors, protein, sugar, and facts. Therefore, every drop counts!
How Long Does Colostrum Last in the Freezer?
Colostrum can last 2 to 6 months with a separate door freezer (5 degrees Fahrenheit or -15 degrees Celsius) with proper storage.
What Should I Do with Frozen Colostrum That's Been Stored For More than 6 Months?
If the colostrum has been stored with a deep chest freezer (-4 Fahrenheit or -20 Celsius) is fine!
How Do I Pump Colostrum After Birth?
Colostrum is thick, sticky, concentrated milk. The best way to collect the colostrum is by hand expressing. Remember the best pump is still the baby. If your baby suckles well, you can just concentrate on latching for the first few days. Unless a baby is separating from his/her mother due to medical reasons, you, as a mother, need to start pumping 8 to 12 times a day.
The best way to collect the colostrum is by hand expressing. Remember the best pump is still the baby. If your baby suckles well, you can just concentrate on latching for the first few days. Unless a baby is separating from his/her mother due to medical reasons, you, as a mother, need to start pumping 8 to 12 times a day.
What is the Best Way to Reheat Colostrum (if any) or Best Methods For Thawing Colostrum For the Baby?
Place the frozen container in the refrigerator the night before you intend to use it. Then warm the milk by placing it in a bowl of warm water or by simply using an electric warmer.
Are There Any Negatives to Giving Colostrum to a Toddler?
Colostrum will not negatively affect toddlers because of the amazing antibodies in the breast milk!
Is Colostrum Considered Better Than Breast Milk?
It is important to note that breast milk changes from colostrum, transitional milk to to mature milk to meet your baby’s nutritional needs at the different stages.
Tips For Hand Expressing Colostrum
Starting by massaging the breast with clean hands to help milk flow. Then by placing your thumb and the rest of your fingers on either side of the areola, about an inch away, gently push your fingers back & towards your chest wall, then compress the milk ducts of the breast, and roll the tissue forward & towards the nipple. Be sure not to squeeze the nipple or slide fingers along your skin.
When is the Best Time to Start Expressing Colostrum?
From 36 weeks of gestational age onwards, mothers are encouraged to harvest colostrum with a proper technique. You can start 2 or 3 times a day and each time for about 3 to 5 minutes, but you'll need to stop if you experience cramps or early contractions to avoid premature delivery.
How Long Do You Produce Colostrum For After Birth?
Colostrum is usually produced for the first few days (usually 3 days ) after the baby’s birth. However, some mothers might not see colostrum until day 5 after giving birth due to various factors.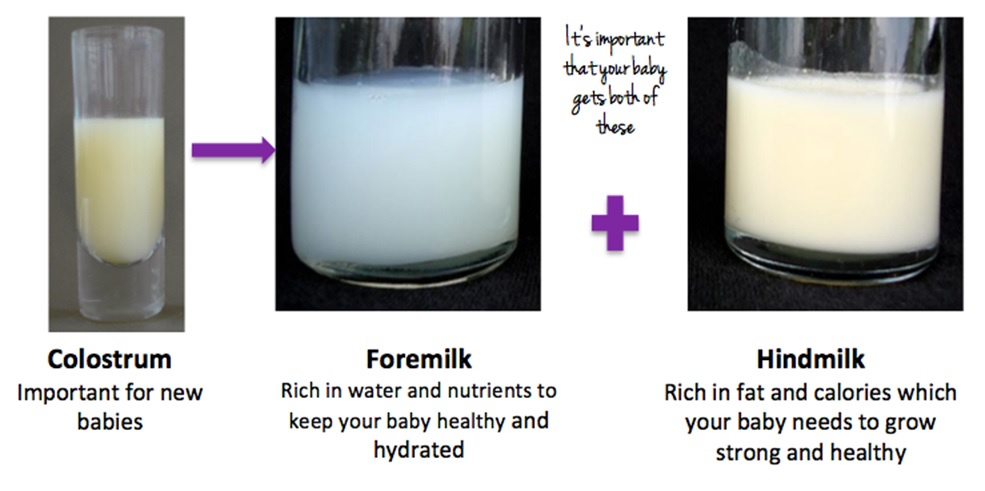
Can you collect some Colostrum and then pump some more later and add to the original bag?
If the colostrum was stored inside the freezer or fridge and you need to add more to it later, you need to ensure the colostrum is the same temperature. We would suggest to first store the second round of colostrum in a different container and keep it inside the fridge for at least 1 hour. This allows the milk to cool to the same temperature as the initial container which makes it safe to combine.
You can also opt to align their temperatures by keeping it out. Please make sure it remains under 77°F (under room temperature). At this temperature, it can last for approximately 4 hours. This allows for ample time to combine the two containers together but do kindly ensure proper hygiene to minimize contamination.
Hegen Helps New Moms Pump and Store Their Colostrum
Today’s women are juggling their passions, careers, and responsibilities with the full-time job of motherhood. While it’s a wonderful adventure, being a mom brings numerous challenges. Breastfeeding shouldn’t be one of them. At Hegen, we want to make breastfeeding easier, rewarding, and empowering. From state-of-the-art breastmilk storage supplies to educational resources, we cover all the bases for you as you transition to your new role.
While it’s a wonderful adventure, being a mom brings numerous challenges. Breastfeeding shouldn’t be one of them. At Hegen, we want to make breastfeeding easier, rewarding, and empowering. From state-of-the-art breastmilk storage supplies to educational resources, we cover all the bases for you as you transition to your new role.
You are free to browse our storage containers as well as our 2 oz bottles (which double as colostrum collectors) which can help you on your breastfeeding journey!
Breastfeeding: the first few days
In the first few days, you and your baby will be getting to know each other. It may take time for both of you to get the hang of breastfeeding.
This happens faster for some women than others. But nearly all women produce enough milk for their baby.
Preparing to breastfeed before the birth
It's good to find out as much as you can about breastfeeding before you have your baby. It may help you feel more confident when you start breastfeeding your baby.
It may help you feel more confident when you start breastfeeding your baby.
Antenatal classes usually cover the most important aspects of breastfeeding, such as positioning and attachment, expressing, and how to tackle common breastfeeding problems.
Find antenatal classes near you.
You can find out about breastfeeding from your midwife, family and friends, and useful helplines and websites.
Find breastfeeding help and support.
There are lots of groups and drop-ins, some specially designed for pregnant women who want to know more about breastfeeding. You can find out more by asking your midwife, health visitor, local peer supporter or GP. Or visit your local Children's Centre.
Find a Sure Start Children's Centre on GOV.UK.
Skin-to-skin contact
Having skin-to-skin contact with your baby straight after giving birth will help to keep them warm and calm and steady their breathing.
Skin-to-skin means holding your baby naked or dressed only in a nappy against your skin, usually under your top or under a blanket.
Skin-to-skin time can be a bonding experience for you and your baby. It's also a great time to have your first breastfeed. If you need any help, your midwife will support you with positioning and attachment.
Skin-to-skin contact is good at any time. It will help to comfort you and your baby over the first few days and weeks as you get to know each other. It also helps your baby attach to your breast using their natural crawling and latching-on reflexes.
You'll still be able to bond with and breastfeed your baby if skin-to-skin contact is delayed for some reason, for example if your baby needs to spend some time in special care.
If necessary, your midwife will show you how to express your breast milk until your baby is ready to breastfeed. They can also help you have skin-to-skin contact with your baby as soon as it's possible.
They can also help you have skin-to-skin contact with your baby as soon as it's possible.
Skin-to-skin after a caesarean
If your baby is delivered by caesarean, you should still be able to have skin-to-skin contact with your baby straight after delivery.
Colostrum: your first milk
The fluid your breasts produce in the first few days after birth is called colostrum. It's thick and usually a golden yellow colour. It's a very concentrated food, so your baby will only need a small amount, about a teaspoonful, at each feed.
Your baby may want to feed quite often, perhaps every hour to begin with. They'll begin to have fewer, but longer feeds once your breasts start to produce more "mature" milk after a few days.
The more you breastfeed, the more your baby's sucking will stimulate your supply and the more milk you'll make.
Your let-down reflex
Your baby's sucking causes muscles in your breasts to squeeze milk towards your nipples. This is called the let-down reflex.
Some women get a tingling feeling, which can be quite strong. Others feel nothing at all.
You'll see your baby respond when your milk lets down. Their quick sucks will change to deep rhythmic swallows as the milk begins to flow. Babies often pause after the initial quick sucks while they wait for more milk to be delivered.
Occasionally this let-down reflex can be so strong that your baby coughs and splutters. Your midwife, health visitor or breastfeeding supporter can help with this.
If your baby seems to be falling asleep before the deep swallowing stage of feeds, they may not be properly attached to the breast. Ask your midwife, health visitor or breastfeeding supporter to check your baby's positioning and attachment.
Sometimes you'll notice your milk letting down in response to your baby crying or when you have a warm bath or shower. This is normal.
How often should I feed my baby?
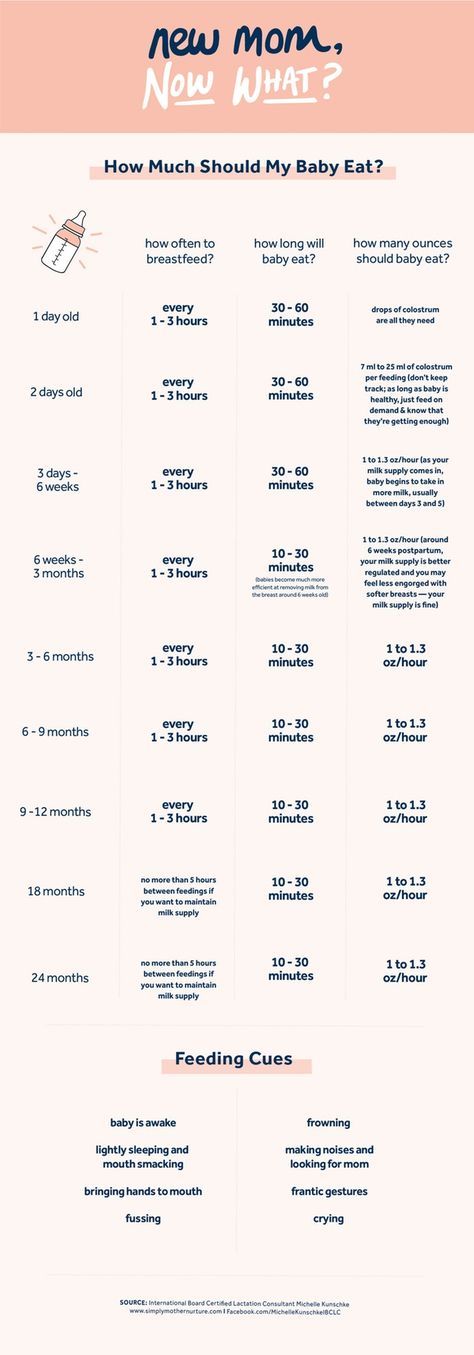
In the first week, your baby may want to feed very often. It could be every hour in the first few days.
Feed your baby as often as they want and for as long as they want. They'll begin to have fewer, but longer feeds after a few days.
As a very rough guide, your baby should feed at least 8 to 12 times, or more, every 24 hours during the first few weeks.
It's fine to feed your baby whenever they are hungry, when your breasts feel full or if you just want to have a cuddle.
It's not possible to overfeed a breastfed baby.
When your baby is hungry they may:
- get restless
- suck their fist or fingers
- make murmuring sounds
- turn their head and open their mouth (rooting)
It's best to try and feed your baby during these early feeding cues as a crying baby is difficult to feed.
Building up your milk supply
Around 2 to 4 days after birth you may notice that your breasts become fuller. This is often referred to as your milk "coming in".
Your milk will vary according to your baby's needs. Each time your baby feeds, your body knows to make more milk for the next feed. The amount of milk you make will increase or decrease depending on how often your baby feeds.
Feed your baby as often as they want and for as long as they want. This is called responsive feeding. In other words, responding to your baby's needs. It's also known as on-demand or baby-led feeding.
In the beginning, it can feel like you're doing nothing but feeding. But gradually you and your baby will get into a pattern and the amount of milk you produce will settle down.
It's important to breastfeed at night because this is when you produce more hormones (prolactin) to build up your milk supply.
In the early weeks, before you and your baby have become comfortable with breastfeeding, "topping up" with formula milk or giving your baby a dummy can lower your milk supply.
Speak to a midwife or health visitor if you are worried about breastfeeding or you think your baby is not getting enough milk.
They might suggest giving your baby some expressed breast milk along with breastfeeding.
Find out more about how to tell if your baby is getting enough breast milk.
Dealing with leaking breasts
Sometimes, breast milk may leak unexpectedly from your nipples.
Wearing breast pads will stop your clothes becoming wet with breast milk. Remember to change them frequently to prevent an infection.
Expressing some milk may also help. Only express enough to feel comfortable as you do not want to overstimulate your supply.
Find out about expressing and storing breast milk.
If your baby has not fed recently, you could offer them a feed as breastfeeding is also about you being comfortable.
Help and support for breastfeeding
- Find out more about positioning and attachment, including how to get comfortable and make sure your baby is properly attached.
- If you are having difficulties with breastfeeding, take a look at common breastfeeding problems.
- Ask a midwife or health visitor for help. They can also tell you about other breastfeeding support available near you.
- Search online for breastfeeding support in your area.
- Call the National Breastfeeding Helpline on 0300 100 0212 (9.30am to 9.30pm daily).
Get Better Health: Start for Life pregnancy and baby emails
Sign up for Start for Life emails for expert advice, videos and tips on pregnancy, birth and beyond.
The first hour of life: breastfeeding a newborn
The first day of life largely determines how successful breastfeeding of a newborn will be.
This page explains the important tasks of initiating and establishing lactation in the first 24 hours.
Share this information
Early Attachment
The first "magic" hour you will have with your baby will be different from anything you've experienced before.
At this time you will have a unique opportunity to start breastfeeding. If a baby latch on in the first 60 minutes of life, it will set off a chain reaction in your body and you will be able to feed and protect your newborn baby.
In many ways, the mechanisms of breast milk formation are determined by hormones, however, in the first hours after childbirth, for the development of lactation, you will need an active stimulator - your baby, who will grasp and suckle rhythmically at the breast. This will “turn on” her cells to start producing milk.
This will “turn on” her cells to start producing milk.
In addition to its role as a lactation activator, early lactation immediately after birth also helps to calm the baby and give him psychological support. Being at the mother's breast, feeling the familiar beating of her heart, the mother's smell and warmth, the baby feels protected, loved and confident in a new unusual environment.
Even if your birth does not go according to plan and you need an emergency caesarean section or other unforeseen interventions, try to put the baby to the breast as early as possible, as this will have a beneficial effect on the establishment of lactation and, in general, on the well-being of you and the baby.
More about the first "magic" hour is described in this chapter: "Birth and the first hours of life."
But that's not all. Immediately after receiving the first drops of colostrum, the baby's body becomes stronger and more adapted to the environment.
Colostrum starts the work of the gastrointestinal tract, pancreas and liver.
Among other things, this means the timely removal of excess bilirubin - which means that the sooner the first application is made and the more colostrum the baby receives on the first day, the less risk he has of developing the so-called "newborn jaundice".
Colostrum also plays a protective role in resistance to various diseases, because the baby's immune system is immature at birth.
For example, immunoglobulin A protects the baby's mucous membranes from bacteria, viruses and parasites.
Alpha-lactalbumin supports the bifidoflora in the baby's intestines, and also forms bioactive lipids that contribute to the destruction of cancer and other foreign cells.
Linoleic and alpha-linoleic acids form the brain and neuroretina of the eye.
All these and many other substances are not artificially reproducible.
It is known that getting even a few drops on the oral mucosa of a premature baby helps to increase the body's defenses and prevent many complications in care.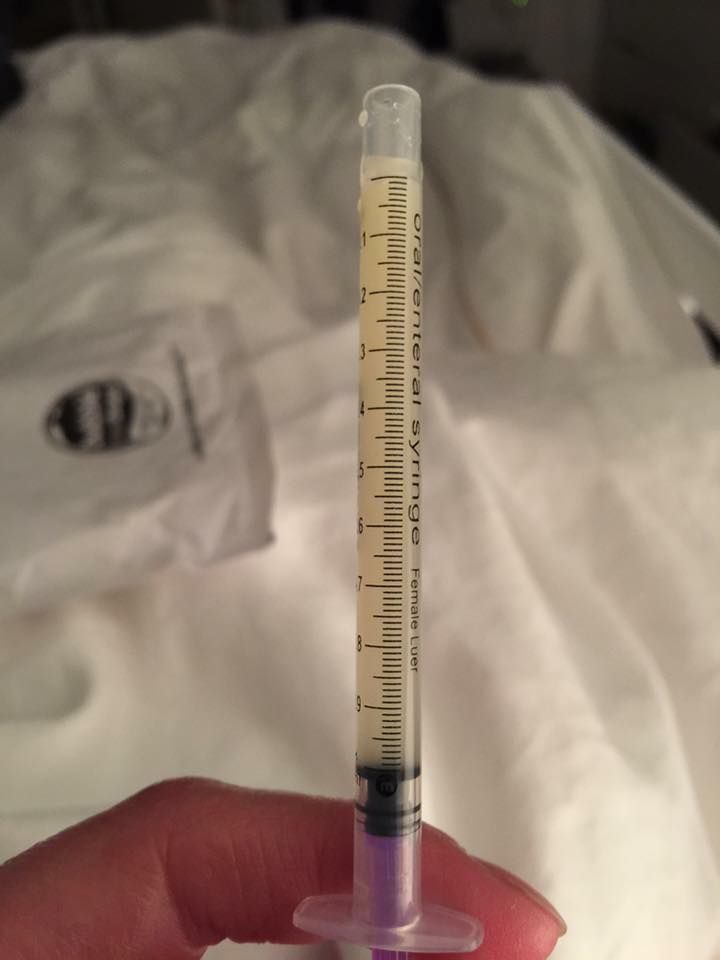
Early receipt of colostrum, among other things, contributes to the timely and soft removal of meconium - the original dark-colored stool.
Feeding on Demand
WHO and UNICEF recommend that breastfeeding is best done "on demand" - that is, every time the baby begins to show signs of anxiety and search for the mother's breast.
This approach, unlike feeding according to the regimen, allows the mother and baby to feel more comfortable, relaxed, to receive all the benefits of breast milk in the amount that the child individually requires.
In the first 24 hours, there may be up to 20 or more such requests. It is believed that the number of feedings that is necessary in the first day of a baby's life should be at least 8.
Frequent feedings are also necessary because very little colostrum is produced at this stage. But the baby's stomach is still so small that this small volume is just what you need. On the first day of life, the baby's stomach can hold only 6 ml of food!
So frequent feeding from birth is a sure way to give your baby the best protection that colostrum provides.
Feeding on demand in the first 24 hours of life and beyond is the right and most harmonious start to breastfeeding imaginable.
Frequent breastfeeding also helps to initiate lactation and prepare the breasts for transitional and then mature milk. Then the volume of breast milk will always meet the growing needs of the baby, he will begin to gain weight well, and you, most likely, will not have a reason to worry about a lack of milk in the future.
There are times when feeding on demand is not possible - for example, the baby is in the intensive care unit or, for one reason or another, is not able to suckle.
Then it is necessary to take measures for the timely development of lactation and providing the child with precious breast milk, organizing pumping with a breast pump. The best way to do this is to use the dedicated INITIATE program on the Symphony* Clinical Breast Pump. In this case, pumping is carried out as often as you would put a baby on - every 2 to 2. 5 hours at least.
5 hours at least.
Correct breastfeeding
One of the first and most important skills that mother and baby must master is the correct breastfeeding.
Incorrect latch is one of the most common causes of sore and subsequently cracked nipples.
One or two sessions of feeding with an incorrect latch can be enough to form painful cracks that cause great concern to the mother and are the "entrance gate" for breast infection.
Not only that, improper latch-on leads to the fact that the baby is simply not able to get enough milk from the breast, he is malnourished, and weak stimulation does not allow lactation to develop as actively as it should.
Cracks, pain, restlessness and malnutrition of the child, sluggish development of lactation, which soon leads to a lack of milk - these are the negative consequences of improper latch that should be tried to prevent.
Therefore, it is very important from the very first day to pay special attention to the correct latch of the baby, and this is another of the main tasks of the first 24 hours of a child's life.
A nurse practitioner, a midwife at the maternity hospital or a lactation consultant can help check if the baby is latching correctly and advise on how to correct the situation if necessary.
Often just stretching the nipples before feeding with a breast pump or Nipple Shaper Pads** can help, as an unshaped, flat or even inverted nipple makes latch on difficult.
For particularly difficult cases, Contact** silicone breast pads are available to help your baby ease in and out of the breast.
Sometimes a lingual frenulum is the cause of a poor grip - then it is important to identify the problem as soon as possible and resolve it quickly. After a small and almost bloodless operation to cut the frenulum, the baby can be immediately applied to the chest.
Also often the problem of grip is explained by the lack of habit, uncomfortable position - all this is quite easily corrected, postures and positions can be mastered under the guidance of experienced mentors, but it is necessary to correct mistakes as soon as possible, in the first 24 hours.
So, here are three important conditions for the key 24 hours after childbirth:
- early attachment;
- feeding on demand;
- correct chest grip.
They help start breastfeeding successfully and harmoniously, ensure the favorable development and protection of the baby's body, and start lactation in a timely manner.
If something went wrong, the main thing is not to despair and not give up. Medela comes to the rescue in every situation with modern and fast solutions.
Literature
Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia. 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
Klaus M. Mother and infant: early emotional ties. Pediatrics. 1998;102( Supplement E 1):1244-1246. — Klaus M., "Mother and Child: The First Emotional Ties". Pediatrix (Pediatrics). 1998; 102 (Appendix E1).
Pediatrics. 1998;102( Supplement E 1):1244-1246. — Klaus M., "Mother and Child: The First Emotional Ties". Pediatrix (Pediatrics). 1998; 102 (Appendix E1).
Sobhy SI, Mohame NA. The effect of early initiation of breast feeding on the amount of vaginal blood loss during the fourth stage of labor. J Egypt Public Health Assoc . 2004;79(1-2):1-2.- Sobhi SI, Moham NA, "Early initiation of breastfeeding and its effect on vaginal bleeding in the fourth stage of labour." G Egypt Public Health Assoc. 2004;79(1-2):1-2. Kim S , et al . Oxytocin and postpartum depression: Delivering on what's known and what's not. brain Res . 2014;1580:219-232. — Kim S. et al., "Oxytocin and postpartum depression: what we know and what we don't know.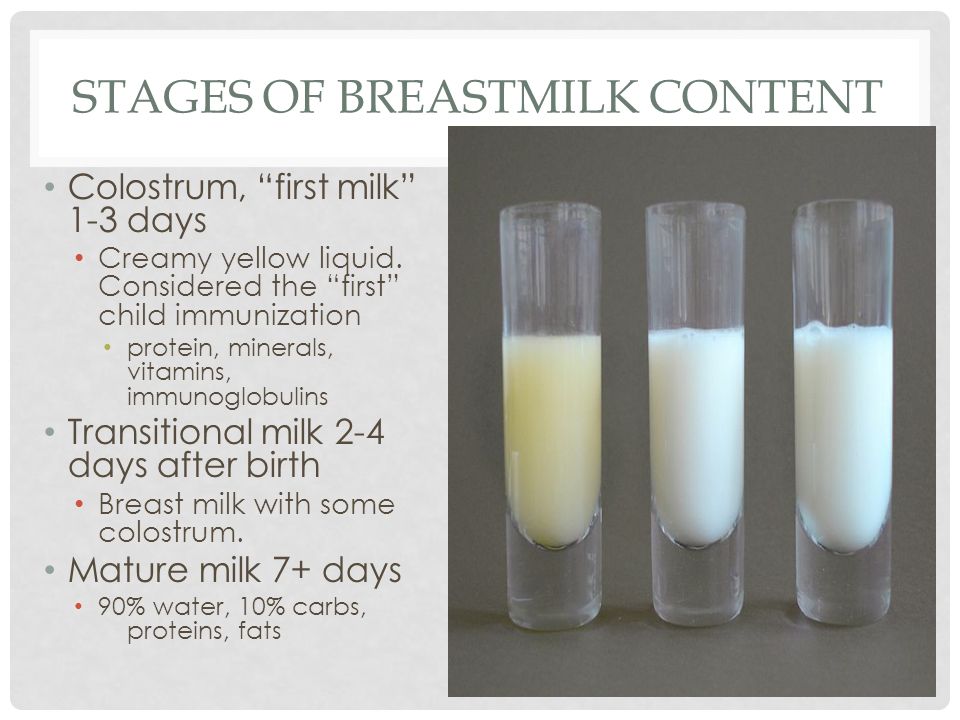 " Brain Res. 2014;1580:219-232.
" Brain Res. 2014;1580:219-232.
Read instructions before use. Consult a specialist about possible contraindications.
* RC No. FZ 2010/06525 dated 01/13/20
** RC No. FZZ 2010/07352 dated 07/19/2010
Breastfeeding a newborn | What to expect in the first week
The first week of a baby's life is a wonderful but hectic time, especially if you haven't breastfed before. Our breastfeeding tips will help you settle in as quickly as possible
Share this information
The first time after childbirth, mothers are often confused. The body is still recovering, and you are already starting to get to know your newborn baby. The emotional state during this period can be unstable, especially between the second and fifth day, when many women have milk 1 and at the same time postpartum depression begins 2 . In addition, people around often expect (and demand) that a woman come to her senses as soon as possible and become a “super mom”.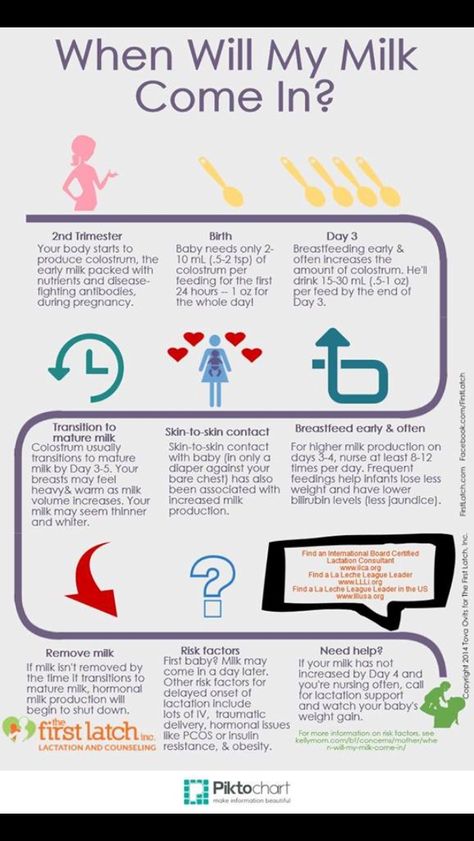 But the best thing to do this first week is just to be with your baby and get breastfeeding going.
But the best thing to do this first week is just to be with your baby and get breastfeeding going.
When should I start breastfeeding my newborn?
Try to breastfeed your baby within the first hour after birth. When the baby latch onto the breast and begins sucking rhythmically, it stimulates the mammary gland cells and starts milk production. 1 It is not for nothing that this time is called the “magic hour”!
“Ideally, the baby should be placed on the mother's stomach immediately after birth so that it can immediately attach to the breast. He won't necessarily eat, but he should be able to,” explains Cathy Garbin, an internationally recognized expert on breastfeeding.
“Hold your baby and let him find the breast on his own and put the nipple in his mouth. This is called the breast-seeking reflex. On the Internet you can watch videos that show what this process looks like. If the baby does not latch onto the nipple on its own, the midwife will help to properly attach it to the breast. But for starters, it’s good to give the baby the opportunity to do it on their own. In this case, the optimal position for the mother is reclining. ”
But for starters, it’s good to give the baby the opportunity to do it on their own. In this case, the optimal position for the mother is reclining. ”
Don't spend that special first hour of your baby's life weighing and swaddling—or at least wait until he's suckling for the first time. Enjoy hugs and close skin-to-skin contact. This promotes the production of oxytocin, the hormone of love, in you and your baby, and oxytocin plays a key role in the supply of the first breast milk - colostrum. 3
“As soon as the obstetricians were convinced that our son was healthy, the three of us — me, my husband and our baby — were left to give us the opportunity to get to know each other. It was a very special hour - an hour of awkwardness, turbulent emotions and bliss. During this time, I breastfed my son twice, ”recalls Ellie, a mother of two from the UK.
Did you know that breastfeeding helps to recover after childbirth? This is because oxytocin stimulates uterine contractions. In the first hours after childbirth, this contributes to the natural release of the placenta and reduces blood loss. 4
In the first hours after childbirth, this contributes to the natural release of the placenta and reduces blood loss. 4
What if the birth didn't go according to plan?
If you had a cesarean section or other complications during childbirth,
You can still establish skin-to-skin contact with your baby and breastfeed him in the first hours after birth.
“If you can't hold your baby, have your partner do it for you and make skin-to-skin contact with the baby. This will give the baby a sense of security, care and warmth so that he can hold on until you recover, ”Katie advises.
If the baby is unable to breastfeed, it is advisable to start expressing milk as early as possible and do so as often as possible until the baby is able to feed on its own. “While breastfeeding in the first hours after birth lays an excellent foundation for the future, it is not so important,” Cathy reassures. “It is much more important to start lactation so that in the future, if necessary, you can start breastfeeding. ”
”
To start milk production, you can express milk manually or use a breast pump that can be given to you at the hospital. 5 And with expressed precious colostrum, it will be possible to feed the child. This is especially important if the baby was born premature or weak, since breast milk is extremely healthy.
If a baby was born prematurely or has a medical condition and cannot be breastfed immediately, this is no reason not to continue breastfeeding. “I have worked with many new mothers who were unable to breastfeed their baby for the first six weeks due to preterm labor or other reasons. Nevertheless, all of them later successfully switched to breastfeeding,” says Kathy.
Does the baby latch on correctly?
Correct breastfeeding is a prerequisite for successful breastfeeding 6 , as it determines how effectively the baby will suckle milk, and therefore grow and develop. Latching on the breast incorrectly can cause sore or damaged nipples, so don't hesitate to ask your doctor to check that your baby is properly attached to the breast, even if you are told that everything is fine and you do not see obvious problems - especially while you are in the hospital.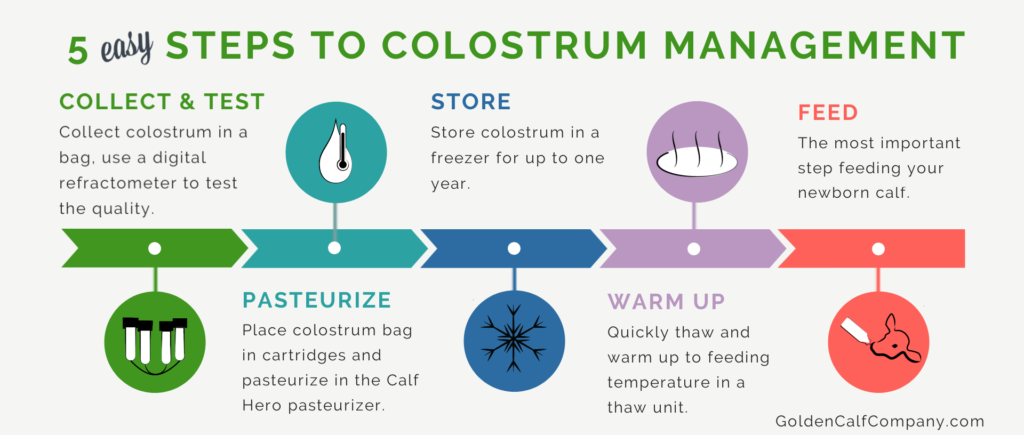
“While I was in the hospital, I called the doctor at every feed and asked me to check if I was breastfeeding correctly,” says Emma, mother of two from Australia. - There were several cases when it seemed to me that everything seemed to be right, but it was painful to feed, and the doctor helped me take the baby off the breast and attach it correctly. By the time I was discharged, I had already learned to do it confidently.”
When applying to the breast, point the nipple towards the palate. This will allow the baby to take the nipple and part of the areola under it into their mouth. It will be easier for him to suck if he has both the nipple and part of the areola around in his mouth. 6
“When a baby latch on properly, it doesn't cause discomfort and it causes a pulling sensation, not pain,” Cathy explains. - The baby's mouth is wide open, the lower lip may be slightly turned outward, and the upper one lies comfortably on the chest. The body language of the child indicates that he is comfortable.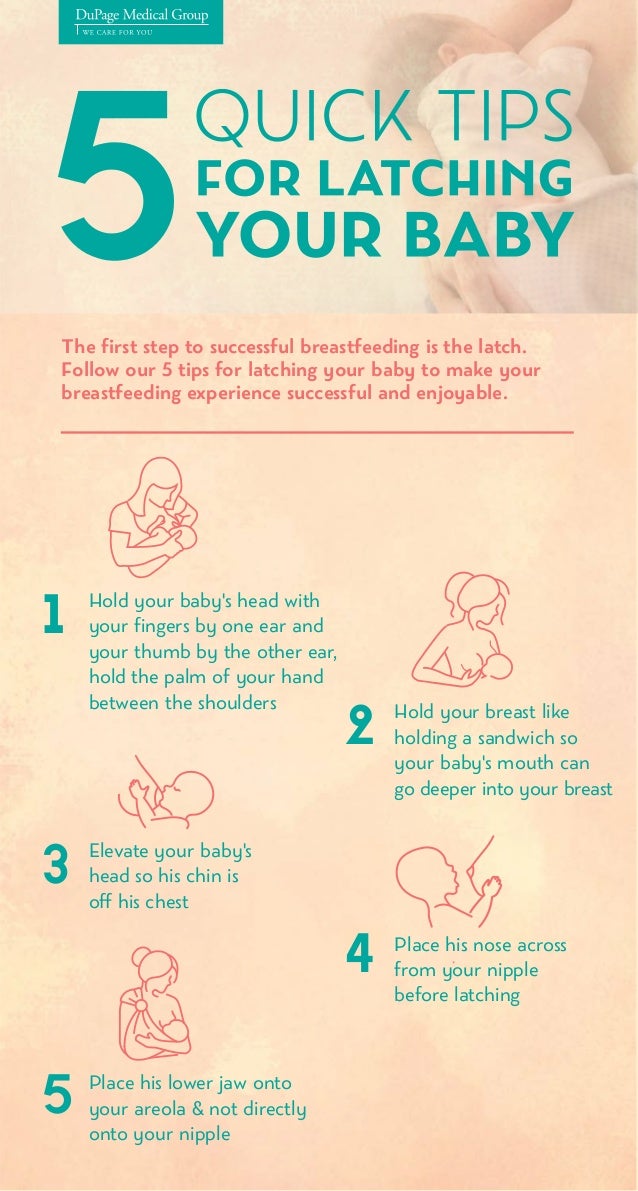 There isn't much milk at this early stage, so you probably won't notice your baby swallowing, but he will suckle a lot and nurse frequently."
There isn't much milk at this early stage, so you probably won't notice your baby swallowing, but he will suckle a lot and nurse frequently."
How often should a newborn be fed?
The frequency and duration of breastfeeding in the first week can vary greatly. “The first 24 hours of life are completely different for different children. Someone sleeps a lot (after all, childbirth is tiring!), And someone often eats, says Katie. - Such a variety greatly confuses young mothers. Everyone gives different advice, so it's important to remember that every mother and child is different."
“Colostrum is thicker than mature breast milk and is produced in smaller amounts, but has many benefits. When the baby eats colostrum, he learns to suck, swallow and breathe until milk begins to flow in more volume, ”explains Cathy.
Milk usually arrives on the second or fourth day after delivery. Until this time, the baby is applied to the breast 8-12 times a day (and sometimes more often!), including at night. 7 Feeding may last 10-15 minutes at this stage, or 45 minutes or even an hour, as the baby is just beginning to develop the muscles and coordination needed to suckle effectively.
7 Feeding may last 10-15 minutes at this stage, or 45 minutes or even an hour, as the baby is just beginning to develop the muscles and coordination needed to suckle effectively.
“At first, the intensity of feeding is very high, often higher than many people realize, and this is shocking to most new mothers,” says Cathy. - Sometimes mom has no time to go to the toilet, take a shower and have a snack. It usually comes as a surprise."
Camille, a mother from Australia, experienced this. “The first week, Frankie ate every two hours, day and night, and each time it took half an hour to an hour to feed,” she recalls. “My husband and I were completely exhausted!”
Should I feed my newborn on a schedule?
The good news is that frequent feeding promotes lactation and stimulates milk production. 7 The more your baby eats, the more milk you will have. Therefore, forget about feeding your newborn on a schedule - this way he will have less chance of feeding. Try to feed your baby when he signals that he is hungry 8 :
Try to feed your baby when he signals that he is hungry 8 :
- toss and turn in his sleep;
- opens eyes;
- turns his head if he feels a touch on his cheek;
- sticks out tongue;
- groans;
- licks lips;
- sucks fingers;
- is naughty;
- whimpers;
- is crying.
Crying is the last sign of hunger, so when in doubt, just offer your baby the breast. If he bursts into tears, it will be more difficult to feed him, especially at first, when both of you are just learning how to do it. As your baby grows, he will likely eat less frequently and take less time to feed, so breastfeeding will seem more predictable.
Does breastfeeding hurt?
You may have heard that breastfeeding is not painful at all, but in fact, in the first days, many new mothers experience discomfort. And this is not at all surprising, given that the nipples are not used to such frequent and strong sucking.
“Breastfeeding can be uncomfortable for the first couple of days – your body and your baby are just getting used to it. If a baby eats for too long and does not latch well, the sensations are almost the same as from unworn new shoes, Cathy compares. Just as tight shoes can rub your feet, improper suckling can damage your nipples. Prevention is always better than cure, so if the pain persists after a few days of feeding, contact a lactation consultant or healthcare professional.”
Maria, a mother from Canada, agrees: “Although my son seemed to latch onto the breast well, he damaged his nipples while feeding, and I was in pain. As it turned out, the reason was a shortened frenulum of the tongue. The breastfeeding specialists at our city clinic have been of great help in diagnosis and treatment.”
In addition, you may experience period cramps during the first few days after breastfeeding, especially if this is not your first baby. This is the so-called postpartum pain.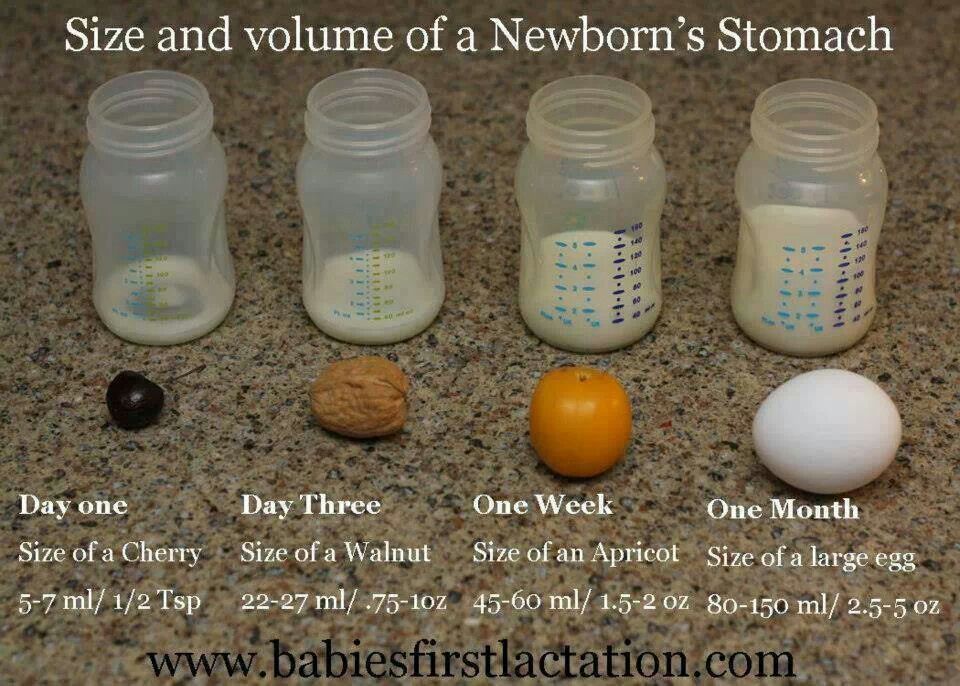 The fact is that oxytocin, which is released during breastfeeding, contributes to further contraction of the uterus to restore its normal size. 4
The fact is that oxytocin, which is released during breastfeeding, contributes to further contraction of the uterus to restore its normal size. 4
When milk arrives, the breasts usually become fuller, firmer and larger than before delivery. In some women, the breasts swell, harden and become very sensitive - swelling of the mammary glands occurs. 10 Frequent breastfeeding relieves these symptoms. For more breast care tips, read our article What is Breast Swelling?
How often does the newborn urinate and defecate?
What goes into the body must go back out. Colostrum
has a laxative effect, helping to eliminate meconium - the original feces. It looks a little scary - black and sticky, like tar. 11 But don't worry, it won't always be like this. Breastfed babies usually have a slightly sweet smell of stool.
How many times a day you will need to change diapers and how the contents should look like, see below.
Day one
- Frequency: once or more.
- Colour: greenish black.
- Texture: sticky like tar.
Second day
- Frequency: twice or more.
- Colour: dark greenish brown.
- Texture: less sticky.
Day three
- Frequency: twice or more.
- Colour: greenish brown to brownish yellow.
- Texture: non-sticky.
Fourth day and then the entire first month
- Frequency: twice or more.
- Color: yellow (feces should turn yellow no later than by the end of the fourth day).
- Texture: grainy (like mustard with grains interspersed). Leaky and watery.
The baby's urine should be light yellow. On average, babies urinate once a day for the first two days. Starting around the third day, the number of wet diapers increases to three, and from the fifth day onwards, diapers have to be changed five times a day or more often. In addition, during the first few days, the weight of wet diapers increases.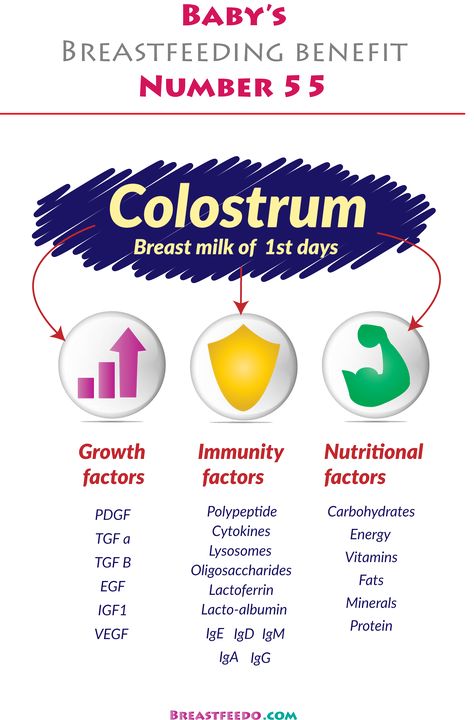 11
11
Is the baby getting enough breast milk?
Since very little milk is produced at first,
you may feel that this is not enough for your baby. But if you feed your baby on demand, you will produce exactly as much milk as he needs. If you want to keep the process under control, be guided by the frequency of diaper changes above. If your baby soils less diapers, check with your doctor.
“For the first three or four weeks, most babies just eat and sleep. If the child is worried and constantly asks for a breast, you should consult with your doctor, ”Katie recommends.
Sometimes the baby may vomit after feeding. If the vomit is the color of milk, this is not a cause for concern. But if there are orange, red, green, brown or black blotches in it, or the child vomits with a "fountain", consult a doctor. You should also consult a doctor if the baby has a high temperature, the fontanel (soft spot on the head) has sunk, blood is found in the stool, and also if the weight recorded at birth has not recovered within two weeks.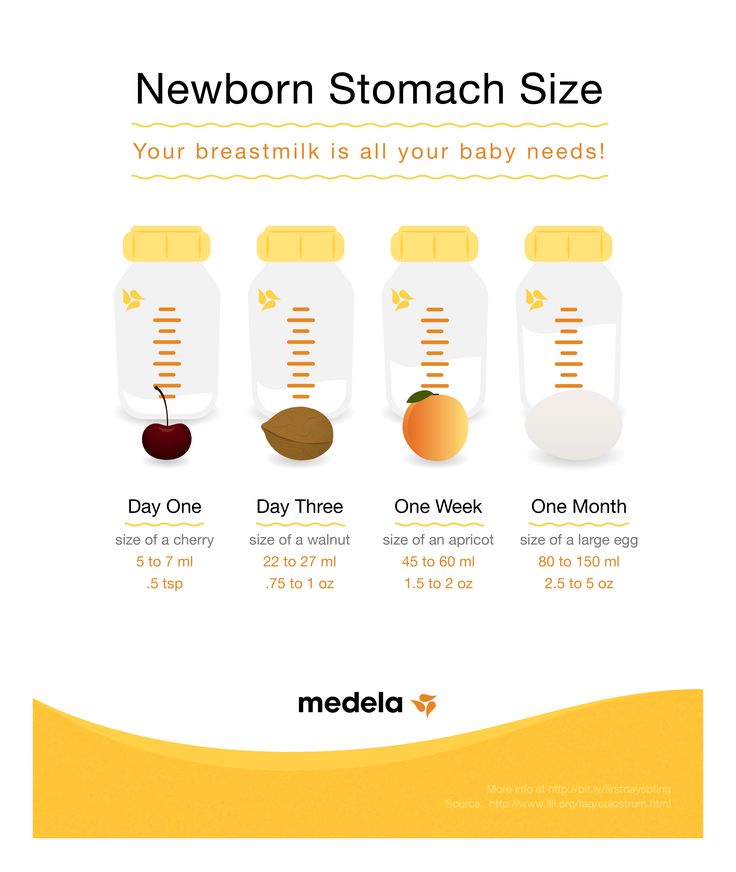 11
11
But if there are no frightening symptoms and the baby is growing at a normal pace, then he has enough milk. Soon you will both get used to breastfeeding and establish a more stable routine.
For the next step in breastfeeding, see Breastfeeding the First Month: What to Expect.
Literature
1 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J9 Gland Biol Neoplasia . 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
2 Shashi R et al. Postpartum psychiatric disorders: Early diagnosis and management. Indian J Psychiatry . 2015; 57( Suppl 2): S 216– S 221.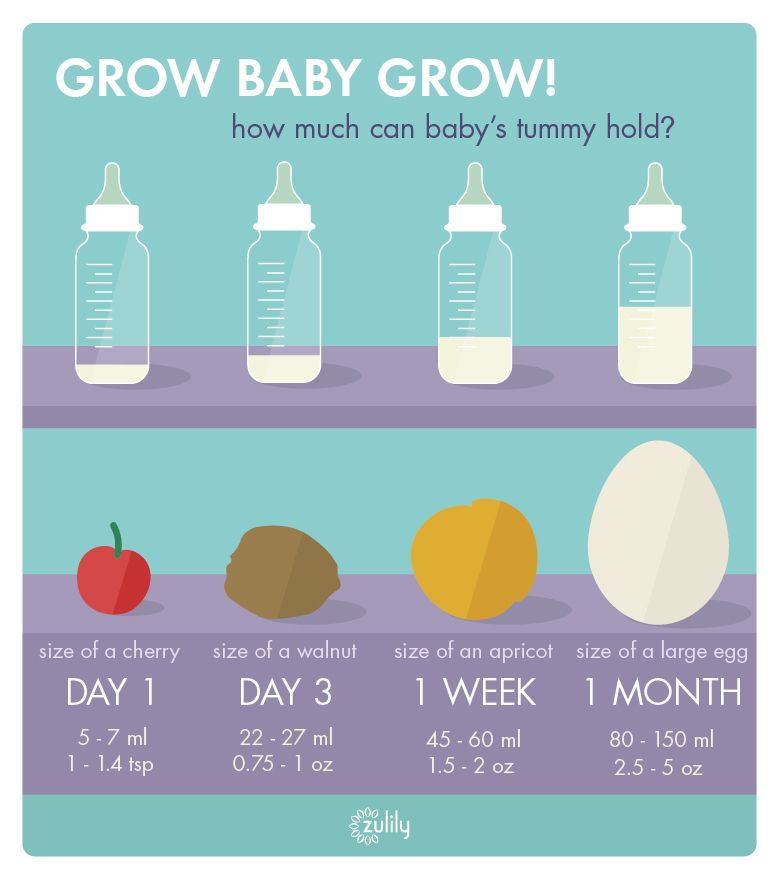 - Shashi R. et al., Postnatal mental disorders: early diagnosis and treatment. Indian J Saikiatri. 2015; 57(App 2):S216-S221.
- Shashi R. et al., Postnatal mental disorders: early diagnosis and treatment. Indian J Saikiatri. 2015; 57(App 2):S216-S221.
3 Moberg KU, Prime DK. Oxytocin effects in mothers and infants during breastfeeding. Infant . 2013;9(6):201-206. - Moberg K, Prime DK, "The effects of oxytocin on mother and child during breastfeeding." Infant. 2013;9(6):201-206.
4 Sobhy SI, Mohame NA. The effect of early initiation of breast feeding on the amount of vaginal blood loss during the fourth stage of labor. J Egypt Public Health Assoc . 2004;79(1-2):1-12. - Sobhi SI, Moham NA, "Early initiation of breastfeeding and its effect on vaginal bleeding in the fourth stage of labor." G Egypt Public Health Assoc. 2004;79(1-2):1-2.
5 Meier PP et al. Which breast pump for which mother: an evidence-based approach to individualizing breast pump technology. J Perinatol . 2016;36(7):493. - Meyer P.P. et al., Breastpump Selection: A Scientific Approach to Customizing Pumping Technology. J Perinatol (Journal of Perinatology). 2016;36(7):493-499.
J Perinatol . 2016;36(7):493. - Meyer P.P. et al., Breastpump Selection: A Scientific Approach to Customizing Pumping Technology. J Perinatol (Journal of Perinatology). 2016;36(7):493-499.
6 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women s Health . 2007;52(6):638-642. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
7 Kent JC et al. Principles for maintaining or increasing breast milk production. J Obstet , Gynecol , & Neonatal Nurs . 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
8 Australian Breastfeeding Association [ Internet ]. Feeding cues ; 2017 Sep [ cited 2018 Feb ]. - Australian Breastfeeding Association [Internet], Feed Ready Signals; September 2017 [cited February 2018]
9 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe Frauenheilkd . 2013;73(12):1202-1208. - Jacobs, A. et al., Guidelines S -3 for the management of inflammatory breast disease during breastfeeding. Geburtskhilfe und Frauenheilkünde. 2013;73(12):1202-1208.
10 Lawrence RA, Lawrence RM. Breastfeeding: A guide for the medical profession.