How to feed premature babies at home
Feeding your premature baby at home
This content is mainly aimed that the person that will be trying to breastfeed their baby. But there is also information here about alternative methods of feeding, depending on your family’s health and circumstances.
Some people prefer to use the term ‘chest feeding’. If so, don’t be afraid to speak to your healthcare professional about your preferred use of language.
While you're in hospital
If you’re breast or bottle feeding your baby, the healthcare team may ask you to keep a record of how often they feed and for how long. The team at the hospital will help you know when and how often to feed your baby, depending on their individual needs.
If you’re using formula, you may also need to record how much milk your baby has taken at each feed. If they’re taking enough milk, they should be having 6–8 wet nappies a day.
But try to remember that when it comes to dirty nappies, every baby is different. Some will poo several times a day, other will poo less often, and some won’t even poo every day. The medical and nursing teams will help you recognise what is normal for your baby and know when to seek help.
You can read about feeding your premature baby in the hospital.
Can I tube feed my baby at home?
With support from the healthcare team, you may be able to tube feed your baby at home if you would like to and your baby is well enough.
Before you leave the baby unit, the healthcare team will show you how to tube feed your baby and who to contact if you have any problems at home. Once you’re home, the baby unit home team or community nursing team will show you how to help your baby learn to suck. This helps your baby gradually move from tube feeding to breast or bottle feeding.
Don’t worry if you don’t feel ready to look after your tube-fed baby at home. You can carry on caring for your baby in the baby unit until they are fully breast or bottle feeding until you’re ready to go home.
Breastfeeding at home
Giving your baby breast milk will help with their development and reduce their risk of infection. You may choose to breastfeed or give your baby bottles of expressed milk.
You may choose to breastfeed or give your baby bottles of expressed milk.
Premature babies can take a few weeks to learn how to breastfeed. If you have had difficulty breastfeeding, it can feel daunting to feed your baby at home without the support of the healthcare team. But there is still help available.
What is responsive feeding?
Responsive feeding is the idea that feeding isn’t only about nutrition. It’s also about love, comfort and reassurance between baby and mother. This means focusing all your attention on your baby during feeds and responding to their cues.
For example, you may offer your breast to your baby when your baby is hungry, distressed or irritable. Breastfeeding can help settle your baby during or after an immunisation or blood test, if your baby is unwell or to reassure them in an unfamiliar environment.
Some parents who aren’t breastfeeding may worry that they are missing an opportunity to bond with their baby. But you can still develop a loving relationship and strong emotional bond with your baby by formula feeding responsively. It is also a good opportunity for dads and partners to be involved in the feeding process.
It is also a good opportunity for dads and partners to be involved in the feeding process.
The UNICEF UK Baby Friendly Initiative suggests:
- sitting comfortably, holding your baby close and looking into their eyes while feeding
- holding your baby fairly upright, supporting their head
- brushing the teat against your baby’s lips – when they open their mouth wide, allow them to draw in the teat
- pulling gently on the corner of your baby’s mouth to release the teat if it becomes flattened during feeding
- offering your baby short breaks during the feed so they have a chance to burp
- supporting your baby to pace the feed – they can put their tongue over the hole to slow the flow or push the teat out of their mouth when they’ve had enough
- never forcing your baby to feed or take ‘all’ the milk if they don’t want it
- feeding your baby skin to skin – this means having your baby on you, their naked skin next to yours with a blanket over both of you for warmth.
Read more about responsive feeding
How do I know if breastfeeding is going well?
You will know breastfeeding is going well when your baby:
- is generally calm and relaxed during feeds and is content after most feeds
- is feeding for between 5 and 40 minutes at each feed (or a time that is normal for them)
- is not showing any signs of jaundice
- has wet and dirty nappies
- is gaining weight
- is swallowing frequently during the feed.
Remember to wind your baby after every feed.
Contact the community team or your health visitor as soon as possible if you have any questions or worries or if you feel you’re not coping. If you find breastfeeding painful, they can give you advice on how to position your baby so they are latching on correctly. Other possible causes of breast pain include thrush, a blocked milk duct or mastitis.
Thrush
If you still find breastfeeding painful after making sure your baby is latching on properly, your health visitor or GP may check to see if you have thrush. This is a fungal infection that can affect cracked or damaged nipples. Babies can also get thrush in their mouths.
This is a fungal infection that can affect cracked or damaged nipples. Babies can also get thrush in their mouths.
Thrush can cause severe pain in both nipples or breasts after a feed. If you have pain in only 1 breast, thrush is unlikely to be the cause. If your baby has oral thrush, they may:
- have creamy white patches on their lips or inside their mouth
- have nappy rash that doesn’t get better
- be unsettled when they’re feeding.
If you have thrush, your GP will treat you and your baby at the same time with an antifungal treatment. You can still breastfeed while you’re having treatment.
To prevent thrush spreading, it’s important to wash your hands carefully after changing nappies. You should also wash any dummies or toys your baby puts in their mouth.
The NHS website has more information about breastfeeding and thrush.
Blocked milk duct
In the early days, your breasts may get too full of milk, making them feel hard and painful. This is called engorgement. If this continues, it can lead to a blocked milk duct, which can cause a tender lump in your breast and pain while breastfeeding.
This is called engorgement. If this continues, it can lead to a blocked milk duct, which can cause a tender lump in your breast and pain while breastfeeding.
Feeding your baby regularly from the affected breast may help to clear the blockage. A warm shower or flannel may help your milk to flow more easily. You could also try gently massaging the lump towards the nipple during feeds.
Mastitis
If a blocked milk duct doesn’t get better, it can lead to mastitis. Symptoms include flu-like symptoms, such as a high temperature, and painful breasts. If you have these symptoms, it’s important to contact your GP or out-of-hours service as soon as possible.
Your GP may advise you to:
- continue breastfeeding or expressing, massaging the breast to clear any blockage – stopping breastfeeding can make symptoms worse
- take paracetamol or ibuprofen to relieve pain
- drink plenty of fluids.
Contact your GP again if your symptoms don’t get better after a few hours or if you feel worse.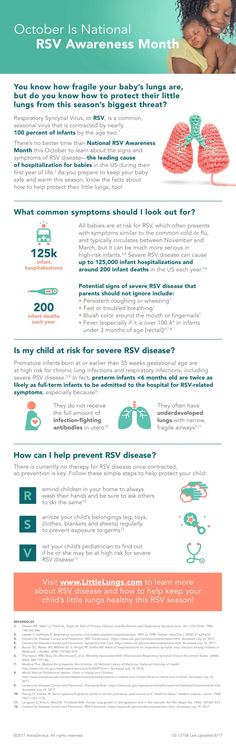 They may give you a type of antibiotic that you can take while breastfeeding.
They may give you a type of antibiotic that you can take while breastfeeding.
The NHS website has more information about mastitis.
Expressing milk at home
You may have expressed milk in hospital if your baby wasn’t able to breastfeed. Now that you’re home you may choose to express milk to store or for someone else to feed to your baby. You can express by hand or you can use an electric or hand pump.
Speak to your health visitor or GP straight away if you’re worried your milk supply is slowing down or stopping.
Tips for Feeding Premature Babies – Children’s Health
Share:
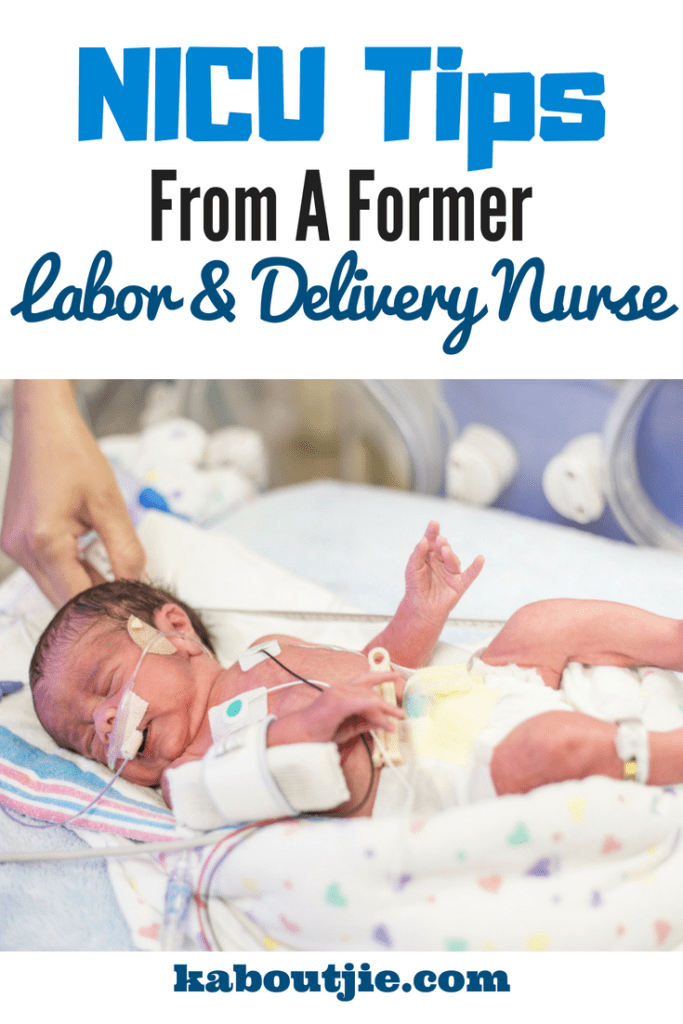
When babies are born prematurely (before 37 weeks of pregnancy), they may have special feeding and nutritional needs. Preemies often need extra support to grow and continue developing, and parents may have questions about breastfeeding, bottles or feeding schedules.
Kikelomo Babata, M.D., a neonatologist at Children's Health℠ and Assistant Professor at UT Southwestern, answers these questions and shares advice for feeding your premature baby.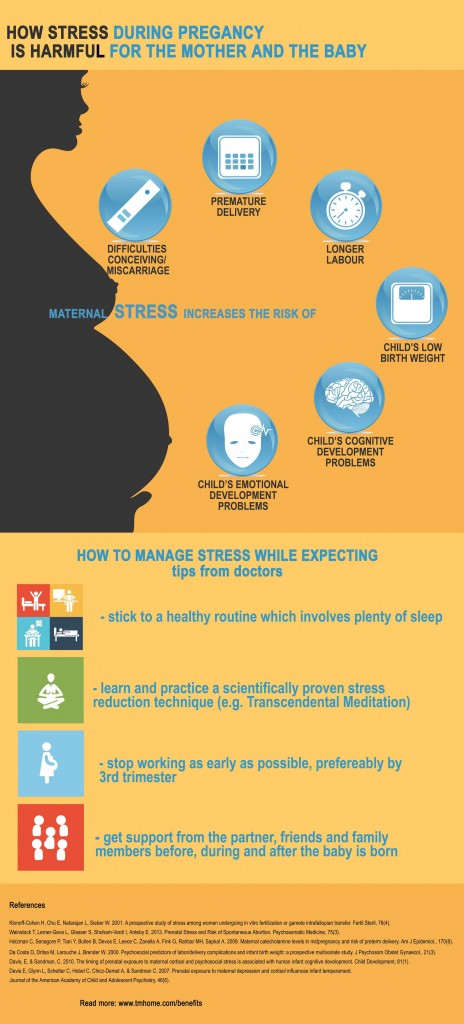
What are common feeding problems in premature infants?
Premature babies may face different feeding problems depending on their age and development. "Post-conceptual age is more important than chronological age for a baby's development," explains Dr. Babata. "A 4-week-old infant born at 32 weeks may not be as developmentally ready to feed as a 2-week-old infant born at 35 weeks. And every baby is different."
Some premature babies have difficulty breastfeeding or bottle-feeding for the first few weeks of their lives. This is because infants, both full-term and premature, continue developing their ability to suck, swallow and breathe after birth. This is a skill they need to feed, so they can coordinate how to suck, swallow then breathe through their nose. Additionally, premature babies may be sleepy and get tired during their feeds.
Premature infants might also have underdeveloped lungs. They might need to be on oxygen, which can make it difficult for them to eat.
Other common feeding problems in premature babies can include:
- Apnea (episodes where they stop breathing)
- Episodes of bradycardia (slow heartbeat that can cause oxygen levels to drop)
- Immature feeding pattern (sucking, swallowing and breathing incorrectly or out of order)
- Oral aversion (not taking a bottle or breast)
- Risk of aspiration (breathing in milk or formula)
If your baby experiences these feeding problems, they may need to be fed through a feeding tube. This tube is placed through the nose and down into the esophagus. If your baby has a feeding tube, they'll stay in the hospital until it is removed.
Once your baby goes home, your pediatrician can offer tips on feeding your baby and the importance of good nutrition. If needed, they can refer you to speech therapist for more support.
Can I breastfeed my premature baby?
Yes, you can breastfeed a premature baby. Your breastfeeding experience may depend on your baby's development and nutritional needs.
Your breastfeeding experience may depend on your baby's development and nutritional needs.
Breastmilk offers many benefits for premature babies, such as:
- Boosting digestion
- Helping baby’s immune system fight infection
- Promoting eye and brain development
- Providing bonding opportunities
"Breastmilk is linked to a lower risk of necrotizing enterocolitis, an illness that can be devastating for preterm infants," says Dr. Babata. Necrotizing enterocolitis is inflammation that can seriously damage or destroy intestinal tissue in babies. It can increase their risk of death or neurodevelopmental problems.
Breastfed infants also have a lower risk of ear infections, respiratory infections like respiratory syncytial virus (RSV) and bronchiolitis, rashes and gastroenteritis. Breastfeeding can have long-lasting benefits as well – lowering your child's risk for chronic illnesses in the future.
Advice for breastfeeding a premature baby
It's important to know that breastfeeding a premature infant might look different than breastfeeding a full-term infant. Breastfeeding may take more coordination for a preemie than bottle feeding, and depending on how premature your baby is, they may have difficulty latching. You may need to use bottles for a few weeks if your baby is having difficulty nursing. You can still choose to pump and provide breastmilk in a bottle. See tips for increasing your milk supply while pumping and how to safely store your breast milk.
Breastfeeding may take more coordination for a preemie than bottle feeding, and depending on how premature your baby is, they may have difficulty latching. You may need to use bottles for a few weeks if your baby is having difficulty nursing. You can still choose to pump and provide breastmilk in a bottle. See tips for increasing your milk supply while pumping and how to safely store your breast milk.
If your premature baby can breastfeed, they still might need bottles of supplemental formula. Often, premature babies cannot exclusively breastfeed because they have higher caloric needs to support growth. Special high-calorie formula or human milk fortifiers can help your child grow while still getting the benefits of breastmilk.
If your premature baby is on a feeding tube, talk to your care team to learn what you can do and whether you should pump your breastmilk.
What type of bottle and formula is best for my premature infant?
Whether you give breastmilk or formula in a bottle, you should use a slow flow bottle nipple designed for premature infants.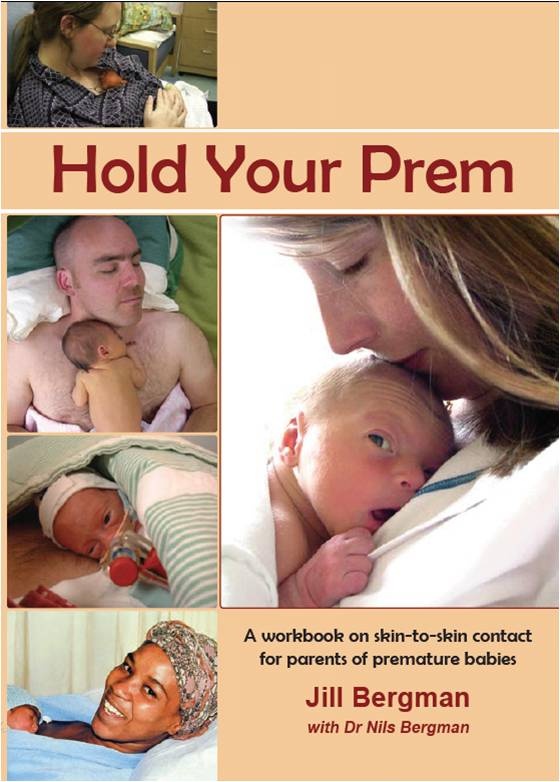 These bottle nipples help prevent your baby from getting more liquid than they can handle at once.
These bottle nipples help prevent your baby from getting more liquid than they can handle at once.
Most premature babies will use a special formula designed for preterm babies. Your pediatrician or neonatologist can recommend the right formula for your baby's needs. Depending on your baby's diet, they can also advise if any other nutritional supplements are needed, such as vitamin D or iron.
How much should I feed my premature baby and how often?
How much your baby needs to eat will change as they grow. Premature babies need 150 to 160 milliliters per kilogram of body weight each day. Your lactation consultant or pediatrician can help you determine how much this is for your baby.
No matter how much they eat per feeding, preemies need to eat at least every 3 to 4 hours.
When can my premature baby eat solids?
A premature baby can start eating solid foods when their adjusted or conceptual age is 4 to 6 months. A conceptual or adjusted age means that instead of counting your baby’s age from their date of birth, it's calculated from their due date. For instance, if your baby is born 10 weeks before their due date, their age at 10 weeks past their due date is 10 weeks (even though they were born 20 weeks ago).
A conceptual or adjusted age means that instead of counting your baby’s age from their date of birth, it's calculated from their due date. For instance, if your baby is born 10 weeks before their due date, their age at 10 weeks past their due date is 10 weeks (even though they were born 20 weeks ago).
Around the adjusted age of 4 to 6 months, premature babies should be able to support their head and have lost their tongue-thrust reflex. This reflex causes them to spit out anything put in their mouth that's not milk or formula. This is a good time to introduce solids.
Taking care of a baby is a challenging job. While these special feeding needs can add extra stress to those early days of your child's life, parents should remember that patience is key.
"Most babies will eventually learn to feed orally," says Dr. Babata. "Just take it one step at a time and be sure to notice and enjoy progress as it occurs."
Learn more
With the only nationally ranked Level IV NICU in North Texas, Children's Health provides expert multidisciplinary care for a wide variety of complex neonatal conditions. Learn more about our top-ranking Neonatology program.
Learn more about our top-ranking Neonatology program.
Children’s Health Family Newsletter
Get health tips and parenting advice from Children’s Health experts sent straight to your inbox twice a month. Sign up now.
Peculiarities of caring for premature babies at home
Each premature baby is purely individual, it differs from a full-term baby not only in appearance, its internal organs and systems are imperfect and not ready for extrauterine life.
The first days of life are of particular importance for premature babies. The first week of life of premature babies is allocated in a special period - the period of adaptation (adaptation) to new environmental conditions. The process of adaptation to extrauterine life in premature babies is longer and more difficult than in full-term babies. In very premature babies, it is 1.5-2 months. nine0004
Today, prematurity is not a critical diagnosis for a baby. Modern equipment and qualified specialists are able to organize an effective process of caring for premature babies in the first days of life.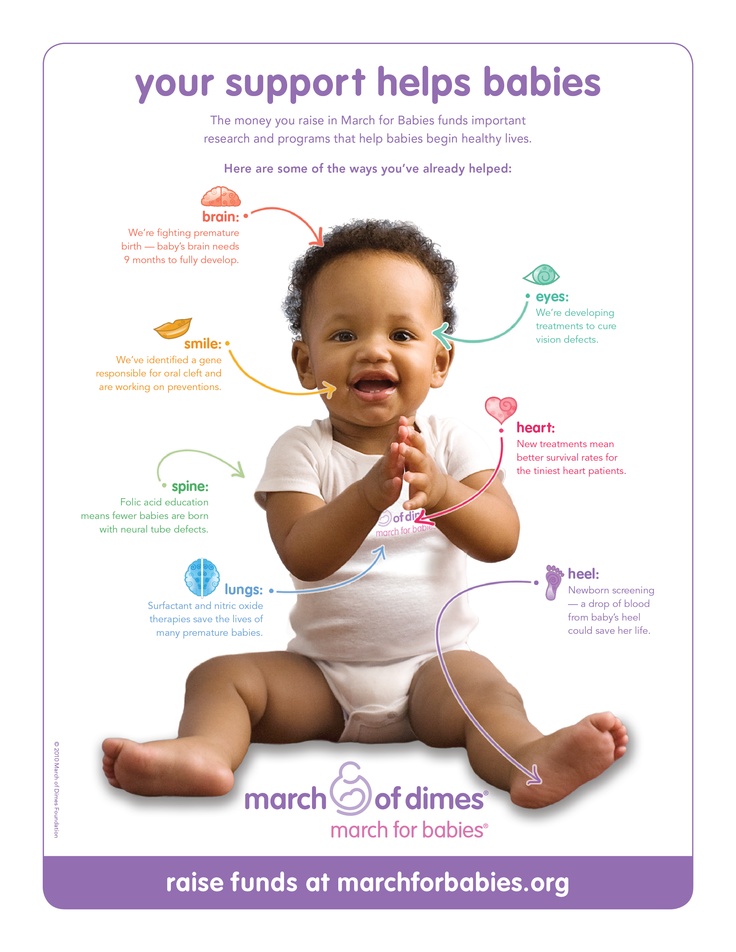 In the future, the care of the child falls entirely on the shoulders of the parents.
In the future, the care of the child falls entirely on the shoulders of the parents.
First of all, this is the creation of a favorable environment for the child, it is also necessary to protect him from external risk factors, such as infection and stress.
The first days after the birth of a premature baby
Pregnancy is almost always a joy. And happy parents begin to calculate the timing of childbirth in order to have time to prepare. But it often happens that the baby, contrary to the expectations of parents and doctors, is born ahead of schedule. Babies born before 37 weeks are called preterm.
As a rule, these children have a body weight and height that is much less than the established standards. The modern equipment available in the arsenal of doctors today, used in the care of premature babies, gives them a better chance of survival. But even 15-20 years ago, such kids had practically no chance. nine0005
The first days are the most critical and decisive. After all, his lungs have not yet fully developed, and it is difficult to breathe on his own. At this time, the child needs specialized care, which should be provided by doctors in the maternity hospital. They put him in a special box - a couvez, where a special microclimate is organized for him.
After all, his lungs have not yet fully developed, and it is difficult to breathe on his own. At this time, the child needs specialized care, which should be provided by doctors in the maternity hospital. They put him in a special box - a couvez, where a special microclimate is organized for him.
The microclimate in the incubator is comparable to the climate in the mother's womb, where the baby has been in the last months. The air mixture supplied there has a high percentage of oxygen content. All organs of the baby are still immature and he needs specialized care of medical personnel and constant monitoring. nine0005
But now the time has come for discharge, after which the child completely passes under the care of the parents. And if there are no particular problems with hospital provision of the necessary conditions, then parents need to be taught the rules for caring for premature babies, because at home it is rather difficult to protect him from various infections.
Features of caring for a premature baby at home
The main problem of is the underweight of the newborn.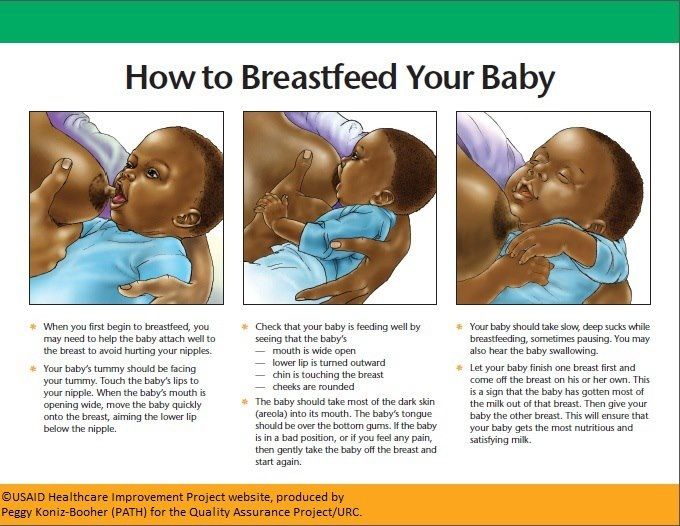 It is in the last weeks of pregnancy that the weight of the child increases and a protective fatty layer is formed, which provides sufficient skin nutrition. In this regard, parents have to pay great attention to the moments of newborn skin care, the fight against diaper rash and irritation. nine0005
It is in the last weeks of pregnancy that the weight of the child increases and a protective fatty layer is formed, which provides sufficient skin nutrition. In this regard, parents have to pay great attention to the moments of newborn skin care, the fight against diaper rash and irritation. nine0005
It is necessary to look through the delicate skin of the child at each swaddle. Careful attention should be paid to the choice of diapers. Preference should be given to soft natural fabrics, as well as carefully choose detergents and powders for washing baby clothes.
It is strictly contraindicated to swaddle the baby in an elastic manner. This will avoid chafing on the skin. But the main reason lies in the fact that the bones of the child and the respiratory organs are still weak, it can simply be difficult for him to breathe, moreover, the blood circulation does not yet function properly. nine0005
The next important point is ensuring optimal and comfortable temperature conditions in the house and in the baby's room in particular. The absence of subcutaneous fat makes the baby vulnerable to the surrounding climate, which makes the risk of infectious diseases many times higher. For this reason, the temperature regime should be monitored with a thermometer. The temperature in the room should be 22-24 o C.
The absence of subcutaneous fat makes the baby vulnerable to the surrounding climate, which makes the risk of infectious diseases many times higher. For this reason, the temperature regime should be monitored with a thermometer. The temperature in the room should be 22-24 o C.
Change your baby's clothes as soon as possible, using warm underwear and diapers. It should also be kept in closed spaces where it is easiest to provide the desired temperature: strollers, cradles. Overheating the baby is also dangerous, for this reason it is important to check the temperature around the baby regularly. nine0005
Feeding
Caring for a premature baby at home has a number of rules during feeding. This applies not only to compliance with the frequency of feeding procedures, but also to the features of the process. First of all, it is important to consider that the process of sucking for a premature baby is a lot of hard work. The lungs are still weak, and the process of sucking milk requires holding the breath. As an alternative to breastfeeding, expressing milk is often recommended. Then feed them to the baby through the nipple. After feeding, immediately put the child in the cradle or crib should not be. The fact is that premature babies spit up more often and more abundantly than healthy children. You should hold the child in your arms in an almost vertical position or laying on your shoulder. nine0005
As an alternative to breastfeeding, expressing milk is often recommended. Then feed them to the baby through the nipple. After feeding, immediately put the child in the cradle or crib should not be. The fact is that premature babies spit up more often and more abundantly than healthy children. You should hold the child in your arms in an almost vertical position or laying on your shoulder. nine0005
Bathing
Bathing procedures should be daily. The water temperature should be 37 degrees, closer to six months, and as the baby gets stronger, you can lower it to 35 degrees in order to harden.
Walks
Walks should be more careful. In summer, they can be started already on the third day after discharge, and in winter - no earlier than 7 or even 10 days later. The duration of the walk is up to 15 minutes. The first exit can be limited to a 5-minute walk, and then gradually increase the time of walking with the baby on the street.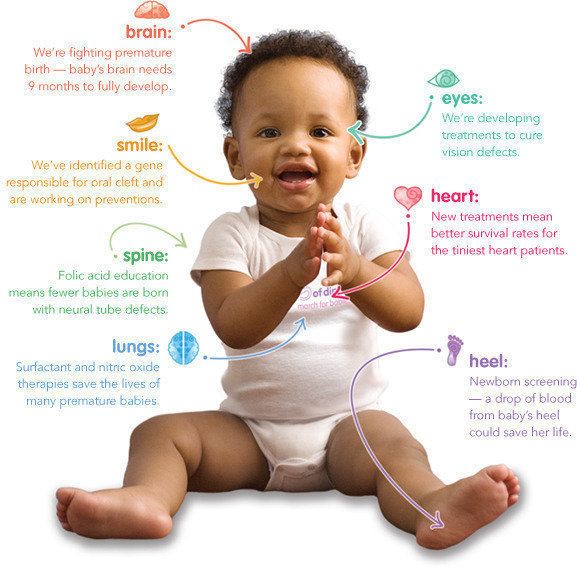 nine0005
nine0005
Anesthesiologist-resuscitator Ivashevich A.S.
Feeding premature babies | Breastfeeding premature babies
Premature babies have a special need for breast milk, but it can be difficult to breastfeed them directly. Our expert advice will help you provide your premature baby with healthy breast milk.
Share this information
nine0016 Professor Katsumi Mizuno, Department of Paediatrics, Showa University Koto Toyosu Hospital:
Katsumi is a Certified Breastfeeding Consultant, Professor of Pediatrics at Showa Medical University, and one of Japan's leading pediatric neonatologists. His research focuses on neonatal suckling skills, breast milk banking, and the use of breast milk for feeding premature babies in neonatal intensive care units.
Babies born before the 37th week of pregnancy are considered premature. nine0044 1 The causes of preterm birth are not always obvious, but certain factors increase the likelihood of such an event. These include: twin or multiple pregnancy, certain diseases of the mother or fetus, as well as a history of premature birth.
These include: twin or multiple pregnancy, certain diseases of the mother or fetus, as well as a history of premature birth.
Because premature babies spend less time in the womb, they are not mature enough and may be more susceptible to infection and disease. They often require hospitalization in the neonatal intensive care unit. nine0005
Why is breast milk important for premature babies?
Breast milk is essential for optimal growth and development of term babies, but it is even more important for premature babies.
During pregnancy, the fetus receives important substances from the mother through the placenta, such as DHA (a fatty acid essential for brain and eye development) and immunoglobulin G (an antibody). 2.3 A premature infant did not receive all of these substances. However, the milk produced by a premature mother contains more fat and secretory immunoglobulin than mothers of full-term babies. nine0044 4
In addition, premature babies have an underdeveloped gastrointestinal tract, which can make digestion and absorption of nutrients difficult, so they need food that their sensitive stomach and intestines can easily digest. Breast milk contains enzymes that facilitate the digestion of the baby, 5 as well as epidermal growth factor, which accelerates the development of the gastrointestinal tract 6 . Premature infants who are predominantly breastfed have much lower intestinal permeability than formula-fed infants, meaning fewer potentially harmful particles from the stomach and intestines enter their bloodstream. nine0044 7
Breast milk contains enzymes that facilitate the digestion of the baby, 5 as well as epidermal growth factor, which accelerates the development of the gastrointestinal tract 6 . Premature infants who are predominantly breastfed have much lower intestinal permeability than formula-fed infants, meaning fewer potentially harmful particles from the stomach and intestines enter their bloodstream. nine0044 7
Breast milk is so important for premature babies that if the baby's mother does not produce enough breast milk at first for any reason, it is recommended to make up for the shortage with donor milk rather than formula.
Does breast milk improve the condition of premature babies?
Breast milk contains protective substances that can prevent serious illnesses that preterm infants are susceptible to, 8 e.g. severe infections, 9 retinopathy of prematurity (which can cause vision loss) 10 and bronchopulmonary dysplasia (chronic lung disease). 11
11
The more milk your baby gets, the lower the risk of developing diseases. 12 Every additional 10 ml of milk per kilogram of body weight per day reduces the risk of developing sepsis by 19%. 9 The risk of developing necrotizing enterocolitis (a potentially fatal bowel disease) in premature infants who are breastfed is ten times lower than those who are formula fed. nine0044 13 That's why every drop counts!
Most importantly, preterm infants who are breastfed are typically discharged an average of two weeks earlier than formula-fed infants. 14 They also have a 6% lower risk of readmission in the first year of life. 15
Breast milk has been proven to have a beneficial effect on mental and physical development in the long term. Studies show that low-birth-weight babies who are breastfed in the neonatal intensive care unit have an average IQ of up to five points higher than those who are not breastfed. nine0044 15 In addition, their cardiovascular system works better during their lifetime. 17
nine0044 15 In addition, their cardiovascular system works better during their lifetime. 17
Will milk be produced if the baby is born prematurely?
Yes, the mother's body is ready to produce milk by the middle of pregnancy. After the baby is born and the placenta is born, the level of progesterone, the pregnancy hormone, drops, and the production of colostrum, the first milk, starts in the breast. This usually happens after the newborn is put to the breast and begins to suckle rhythmically, but if the baby was born prematurely, he most likely will not be able to latch on at first. nine0005
To replicate the sensations that trigger milk production, you can manually stimulate the breasts and nipples, or use a breast pump to express nutrient-rich colostrum for your baby. 18 Read below for more information on what to do if your premature baby is not yet able to breastfeed.
Breast milk usually comes in two to four days after birth, but if it was premature, the milk supply may be delayed. However, a recent study shows that moms who started pumping within one hour of giving birth had milk coming in as expected. nine0044 19 This is why it is important to start expressing breast milk as early as possible.
However, a recent study shows that moms who started pumping within one hour of giving birth had milk coming in as expected. nine0044 19 This is why it is important to start expressing breast milk as early as possible.
How to prepare if the baby is expected prematurely?
Visit the neonatal intensive care unit to see how it works and how premature babies are cared for. In addition, it will be useful to learn how breast milk is produced and secreted and why it is not only a healthy food, but also an important medicine for premature babies. Read more about this in our free e-book Surprising Breast Milk Facts .
What if a premature baby cannot breastfeed?
Many babies born before 34 weeks have difficulty coordinating sucking, swallowing and breathing. Until the baby has mastered these skills, nurses will feed him through a tube that is inserted into the nose or mouth and provides food directly into the stomach. In this way, the baby can be fed continuously until he is ready to breastfeed.
If your baby is too weak to latch on and suckle milk, you can use a breast pump* available at the hospital or maternity hospital to “do the job for the baby”. Breast stimulation with research-based technology, 20 reproduces the rhythm of the suckling of the baby, plays an important role in starting and maintaining milk production in the first hours after birth 21 .
Milk should be expressed at the same frequency as term infants are usually fed every two to three hours, i.e. 8 to 12 times a day.
You can try putting a small amount of expressed breast milk into the baby's mouth with a syringe, or putting milk-soaked cotton swabs in the baby's mouth. 22 This way your baby will recognize the taste of your milk, which will facilitate the transition to breastfeeding in the future. In addition, the protective substances that make up breast milk will help strengthen the local immunity of the baby's oral cavity. There are many ways you can participate in the care of your premature baby - check with your healthcare provider for details.
Very low birth weight babies - less than 1.5 kg - usually need extra protein, calcium and phosphorus, so they are given fortified breast milk. In some countries, such additives are made on human milk, and, for example, in Japan, on cow's milk. nine0005
Recommendations for pumping milk
If the baby will be in the neonatal intensive care unit for a long time, neonatologists recommend using a double breast pump for pumping. I always recommend Medela Symphony*. Double pumping not only speeds up the process, but also produces an average of 18% more milk than pumping from each breast in turn. 23
In addition, I advise you to create the most comfortable conditions for pumping. It is generally agreed that it is best to express milk during or after prolonged skin-to-skin contact with the baby (more on this "kangaroo method" below). Another good option is to sit next to the crib and watch your baby while he pumps. Oxytocin (the hormone that stimulates milk flow) is released when you look at your baby, touch him, smell him and think about him, 24 Therefore, comfortable and calm conditions must be created for this in the neonatal intensive care unit.
What is kangaroo care for premature babies?
The so-called kangaroo method involves prolonged skin-to-skin contact between parents and infant. This is extremely beneficial for you and your baby, as well as for milk production. Skin-to-skin contact normalizes the baby's breathing and heartbeat, keeps him warm and allows him to be as close to the parent as possible. Kangaroo care is believed to have a beneficial effect on the health of premature babies, 25 and it helps mothers to express more milk 26 and breastfeed longer. 27 Skin-to-skin contact 30-60 minutes before feeding gives baby time to wake up and be hungry so he can eat without being forced.
What if the neonatal intensive care unit offers formula feeding?
Feel free to state that you want to breastfeed your baby instead of formula. If you don't have enough breast milk to feed your baby, ask the ward for help to increase your milk supply. nine0005
It is natural for mothers whose babies are in the neonatal intensive care unit to experience anxiety and stress. Sometimes these experiences interfere with milk production, so it's important to ask for any help you may need. Remember that you have the right to seek support. Your healthcare provider may be able to recommend a suitable lactation specialist, such as a lactation consultant, for you.
Sometimes these experiences interfere with milk production, so it's important to ask for any help you may need. Remember that you have the right to seek support. Your healthcare provider may be able to recommend a suitable lactation specialist, such as a lactation consultant, for you.
How to switch from pumping to breastfeeding? nine0089
At whatever stage of pregnancy a baby is born, if the baby is stable enough for skin-to-skin contact, it can seek the breast itself for sedative suckling. This is the perfect way for your baby to learn sucking skills before they learn to coordinate sucking, swallowing and breathing.
Babies love the smell of breast milk, so you can put some milk on the nipple before you put your baby to the breast to make him want to suckle. He might even be able to suck some milk. Don't worry if your baby seems to suck very little - he learns every time. He can start with one or two sips and gradually move on to full breastfeeding. Until then, the baby can be fed through a tube, pressed to the breast, so that the taste of milk and touching the breast is associated with a feeling of satiety. nine0005
nine0005
You can put your baby to the breast for sedative suckling as soon as you are ready for kangaroo care, unless your baby is suffering from bradycardia (slow heartbeat) or low oxygen levels in the blood. You can switch to breastfeeding as soon as the baby is ready for it. Gradually, he will gain enough strength to suckle longer and suck out more milk.
Literature
1 World Health Organization. Geneva, Switzerland; 2018. Media Centre: Preterm birth fact sheet; November 2017 [03/26/2018]. Available from : http://www.who.int/mediacentre/factsheets/fs363/en/ - World Health Organization Geneva, Switzerland; 2018. "Media Center: Prematurity Fact Sheet"; November 2017 [3/26/2018]. Article linked: http://www.who.int/mediacentre/factsheets/fs363/en/
2 Duttaroy AK. Transport of fatty acids across the human placenta: a review. nine0004 Prog Lipid Res . 2009;48(1):52-61. - Duttaroy A.K., "Transfer of fatty acids across the human placenta: a review". Prog Lipid Res. 2009;48(1):52-61.
2009;48(1):52-61. - Duttaroy A.K., "Transfer of fatty acids across the human placenta: a review". Prog Lipid Res. 2009;48(1):52-61.
3 Palmeira P et al. IgG placental transfer in healthy and pathological pregnancies. Clin Dev Immunol. 2012;2012: 985646. - Palmeira P. et al., Placental transfer of immunoglobulin G Through the placenta with healthy and pathological pregnancy. ” Klin Virgo Immunol. 2012: 985646.
4 Underwood Ma. Human Milk for North Am . 2013;60(1):189-207. - Underwood M.A., "Breast milk for the premature baby." 1):189-207.
5 Pamblanco M et al. Bile salt - stimulated lipase activity in human colostrum from mothers of infants of different gestational age and birthweight. Acta Paediatr. 1987;76(2):328-331. - Pamblanco M. et al.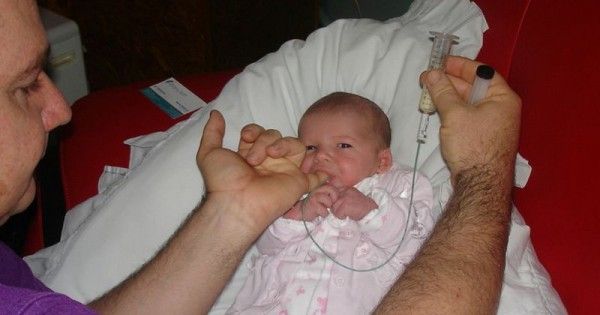 , "Bile salt-activated lipase and its activity in colostrum of mothers of infants of various gestational ages and birth weights." Akta Pediatr. 1987;76(2):328-331.
, "Bile salt-activated lipase and its activity in colostrum of mothers of infants of various gestational ages and birth weights." Akta Pediatr. 1987;76(2):328-331.
6 Dvorak B. Milk epidermal growth factor and gut protection. J Pediatr. 2010;156(2): S 31-35. - Dvorak B., "Epidermal growth factor in milk and gut protection". F Pediatrician (Journal of Pediatrics). 2010;156(2):S31-35.
7 Taylor SN et al. Intestinal permeability in preterm infants by feeding type: mother's milk versus formula. Breastfeed Med . 2009;4(1):11-15.- Theilon S.N. et al., "Intestinal permeability in preterm infants and its association with type of feeding: breast milk or formula." Brestfeed Med (Breastfeeding Medicine). 2009;4(1):11-15.
8 Newburg DS. Innate immunity and human milk. J Nutr .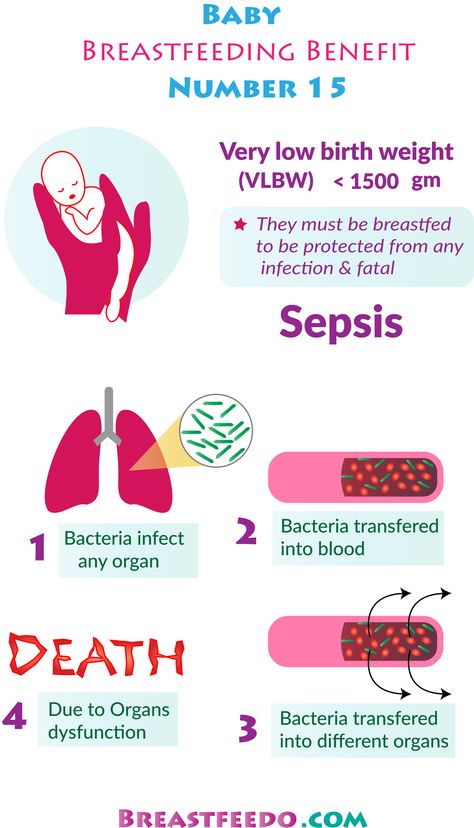 2005;135(5):1308-1312. — Newburgh, D.S., "Natural Immunity and Breast Milk." F Int. 2005;135(5):1308-1312. nine0004
2005;135(5):1308-1312. — Newburgh, D.S., "Natural Immunity and Breast Milk." F Int. 2005;135(5):1308-1312. nine0004
9 Patel AL et al. Impact of early human milk on sepsis and health-care costs in very low birth weight infants. J Perinatol . 2013;33(7):514-519.- Patel A.L. et al., "Impact of early breast milk on sepsis and health care costs in extremely low birth weight infants". Zh Perinatol (Journal of Perinatology). 2013;33(7):514-519.
10 Zhou J et al . Human milk feeding as a protective factor for retinopathy of prematurity: a meta-analysis. Pediatrics. 2015;136(6): e 1576-1586. - Zhou Q. et al., "Breastfeeding as a protective factor against retinopathy of prematurity: a meta-analysis." Pediatrix (Pediatrics). 2015;136(6):e1576-1586.
11 Patel AL et al. Influence of own mother's milk on bronchopulmonary dysplasia and costs. Arch DIS Child Fetal NEONAT ED . 2017;102(3): F 256- F 261. - Patel A.L. et al., "Effect of breast milk on bronchopulmonary dysplasia and health care costs." Arch Dis Child Fetal Neonate Ed. 2017;102(3): F 256- F 261.
12 MEIER PP ET Al . Improving the use of human milk during and after the NICU stay. Clin Perinatol. 2010;37(1):217-245. - Meyer P.P. et al., "Optimizing the use of breast milk during and after a stay in the neonatal intensive care unit." nine0004 Perinatol wedge. (Clinical perinatology). 2010;37(1):217-245.
2010;37(1):217-245.
13 Lucas A, Cole TJ. Breast milk and neonatal necrotizing enterocolitis. Lancet. 1990;336(8730-8731):1519-1523. — Lucas A, Cole TJ, "Breast milk and neonatal necrotizing enterocolitis." Lancet (Lancet). 1990;336(8730-8731):1519-1523.
14 Schanler RJ et al. Randomized trial of donor human milk versus preterm formula as substitutes for mothers' own milk in the feeding of extremely premature infants. nine0004 Pediatrics. 2005;116(2):400-406. - Chanler R.J. et al., "Randomized Trial of Donor Human Milk Versus Prematurity Formula as a Breast Milk Substitute in Severely Preterm Infants". Pediatrix (Pediatrics). 2005;116(2):400-406.
15 Vohr BR et al. Beneficial effects of breast milk in the neonatal intensive care unit on the developmental outcome of extremely low birth weight infants at 18 months of age. nine0004 Pediatrics. 2006;118(1): e 115-123. - Thief B.R. et al., Developmental Beneficial Effects of Breast Milk in the Intensive Care Unit on Extremely Low Birth Weight Infants by 18 Months of Age. Pediatrix (Pediatrics). 2006;118(1):e115-123.
2006;118(1): e 115-123. - Thief B.R. et al., Developmental Beneficial Effects of Breast Milk in the Intensive Care Unit on Extremely Low Birth Weight Infants by 18 Months of Age. Pediatrix (Pediatrics). 2006;118(1):e115-123.
16 Victora CG et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. nine0004 2016;387(10017):475-490. - Victor S.J. et al., "Breastfeeding in the 21st century: epidemiology, mechanisms and long-term effects". Lancet (Lancet). 2016;387(10017):475-490.
17 Lewandowski AJ et al. Breast milk consumption in preterm neonates and cardiac shape in adulthood. Pediatrics. 2016;138(1): pii : e 20160050. - Lewandowski, A.J. et al., "Breastfeeding in preterm infants and cardiovascular health in adulthood." nine0004 Pediatrix (Pediatrics). 2016;138(1):pii:e20160050.
18 Meier PP et al. Which breast pump for which mother: an evidence-based approach to individualizing breast pump technology. J. Perinatol. 2016;36(7):493-499. - Meyer P.P. et al., Breastpump Selection: A Scientific Approach to Customizing Pumping Technology. J Perinatol (Journal of Perinatology). 2016;36(7):493-499.
19 Parker LA et al. Effect of early breast milk expression on milk volume and timing of lactogenesis stage II among mothers of very low birth weight infants: a pilot study. J Perinatol. 2012;32(3):205-209. - Parker L.A. et al., "Effect of early pumping on milk supply and timing of the second stage of lactogenesis in mothers of extremely low birth weight infants: a pilot study." J Perinatol (Journal of Perinatology). 2012;32(3):205-209.
20 Meier PP et al. Breast pump suction patterns that mimic the human infant during breastfeeding: greater milk output in less time spent pumping for breast pump-dependent mothers with premature infants. J Perinatol. 2012;32(2):103-110. - Meyer P.P. et al., "Pumping patterns that mimic breastfeeding behavior: more milk and less time for constantly pumping mothers of preterm infants." nine0004 J Perinatol (Journal of Perinatology). 2012;32(2):103-110.
J Perinatol. 2012;32(2):103-110. - Meyer P.P. et al., "Pumping patterns that mimic breastfeeding behavior: more milk and less time for constantly pumping mothers of preterm infants." nine0004 J Perinatol (Journal of Perinatology). 2012;32(2):103-110.
21 Parker LA et al. Association of timing of initiation of breastmilk expression on milk volume and timing of lactogenesis stage II among mothers of very low-birth-weight infants. Breastfeed Med . 2015;10(2):84-91. - Parker L.A. et al., "Effect of early pumping on milk supply and timing of the second stage of lactogenesis in mothers of extremely low birth weight infants: a pilot study." nine0004 Brestfeed Med (Breastfeeding Medicine). 2015;10(2):84-91.
22 Lee J et al. Oropharyngeal colostrum administration in extremely premature infants: an RCT. Pediatrics. 2015;135(2): e 357-366.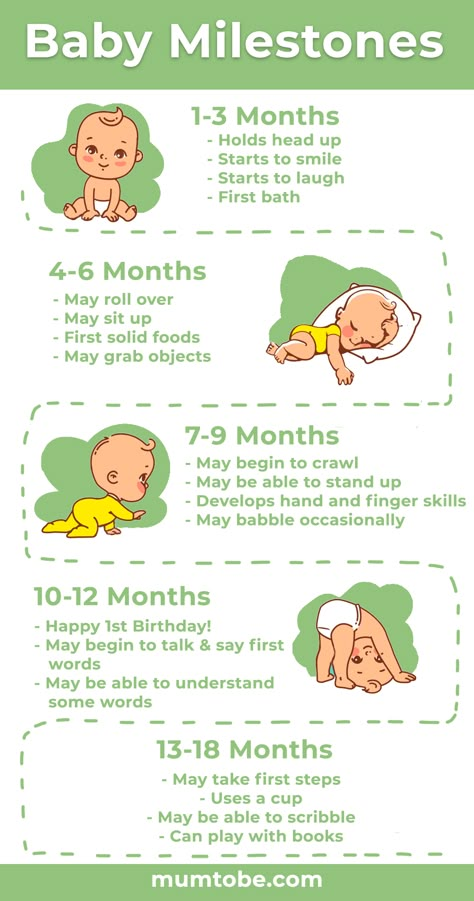 - Lee J. et al., "Oropharyngeal colostrum ingestion in very preterm infants: a randomized controlled clinical trial." Pediatrix (Pediatrics). 2015;135(2):e357-366. nine0004
- Lee J. et al., "Oropharyngeal colostrum ingestion in very preterm infants: a randomized controlled clinical trial." Pediatrix (Pediatrics). 2015;135(2):e357-366. nine0004
23 Prime PK et al. Simultaneous breast expression in breastfeeding women is more efficacious than sequential breast expression. Breastfeed Med 2012; 7(6):442–447. - Prime D.K. and co-authors. "During the period of breastfeeding, simultaneous pumping of both breasts is more productive than sequential pumping." Brestfeed Med (Breastfeeding Medicine). 2012;7(6):442-447.
24 Uvn 9 ä s Moberg K Oxytocin effects in mothers and infants during breastfeeding. Infant 2013; 9(6):201–206. - Uvenas-Moberg K, Prime DK, "Oxytocin effects on mother and child during breastfeeding". Infant. 2013;9(6):201-206.
25 Boundy EO et al. nine0004 Kangaroo mother care and neonatal outcomes: a meta-analysis. Pediatrics. 2015;137(1): e 20152238. - Boundi I.O. and co-authors, "The Kangaroo Method and Its Impact on Newborns: A Meta-Analysis". Pediatrix (Pediatrics). 2015;137(1): e20152238.
26 Acuña-Muga J et al. Volume of milk obtained in relation to location and circumstances of expression in mothers of very low birth weight infants. nine0004 J Hum Lact . 2014;30(1):41-46 - Akunya-Muga, J. et al., "The amount of milk expressed by location and circumstances of pumping in mothers of extremely low birth weight infants." G Hum Lakt. 2014;30(1):41-46
27 Nyqvist KH et al. Towards universal kangaroo mother care: recommendations and report from the first European conference and seventh international workshop on kangaroo mother care.
Learn more