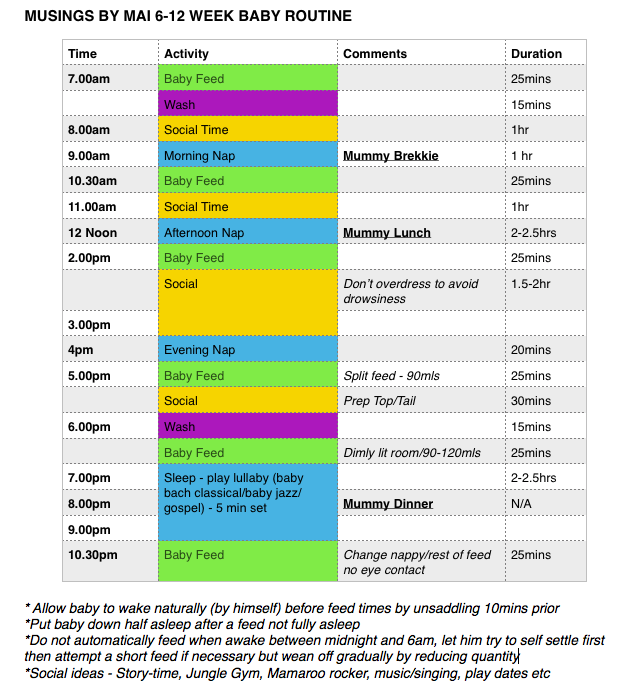
How to pace feed a breastfed baby
Paced Bottle-Feeding: How to Mimic Breast-Feeding
Breast-feeding offers a host of benefits for your baby, but it’s not without its challenges.
Namely, if you are on a feeding schedule with your baby, it’s likely at some point in time that you may need to utilize bottle-feedings to allow yourself to return to work or simply be less of a slave to your breast-feeding schedule.
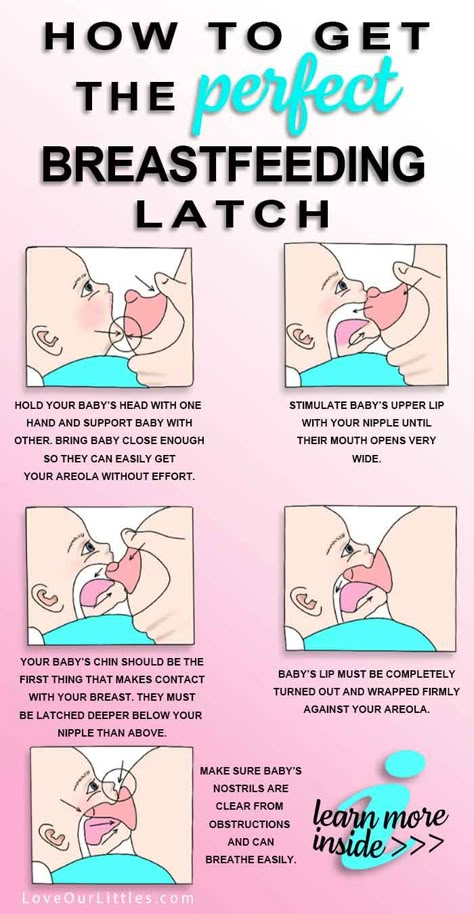
The challenge with bottle-feedings is the risk for “nipple confusion.” While modern science has made bottles as close to the real thing as possible, there’s still little substitute for the breast. Bottle-feedings are traditionally easier for the baby and can sometimes affect a baby’s latching ability — one of the most important aspects of breast-feeding.
One approach to reducing the risk for nipple confusion is to use a paced bottle-feeding approach. Through paced bottle-feeding, you may be able to closely mimic nursing.
Traditional bottle-feeding involves giving babies bottles and allowing them to drink them at a steady rate.
While this accomplishes the task of feeding, a baby often receives the milk at a faster rate than when breast-feeding. This can affect a baby’s ability to return to the breast and also cause a baby to take in too much milk too quickly if you notice that your baby seems to suck without pausing using a traditional bottle-feeding method.
Paced bottle-feeding aims to slow feedings to closely mimic breast-feeding. Using techniques like keeping the bottle’s nipple half full and allowing the baby to pull the bottle’s nipple in, paced feeding can seem more like breast-feeding.
To pace feed, you will need a milk source, like formula or pumped milk. You will also need a bottle and a nipple for the bottle. Many nipple options are available on the market.
Share on Pinterest
However, for paced feedings, a wide-based, slow-flow nipple is recommended. This option can feel more like a mother’s nipple to a baby. If your baby has trouble accepting this nipple option, you may need to try a different option.
To pace feed your baby, place your baby in an upright position with plenty of head and neck support. Gently touch the bottle’s nipple to your baby’s mouth, much as you would during a breast-feeding session.
When your baby opens their mouth, gently advance the bottle’s nipple. If needed, you can stroke the baby’s cheek to encourage them to open the mouth. The ideal position will be where the nipple is at the top of the tongue, which helps to minimize air intake.
Hold the bottle parallel to the ground, and allow your baby to take in between five and 10 sucks of the bottle. The parallel position will allow for better flow control. Slightly pull the bottle backward to where the nipple is still touching the lower lip.
Allow your baby to pull the nipple back in, much like they would during a feeding. Another option is to reduce the bottle’s tilt to slow the flow until your baby starts sucking harder.
Remember to burp your baby frequently during the feeding. You can also switch the sides that your baby is held on, which can more closely mimic breast-feeding.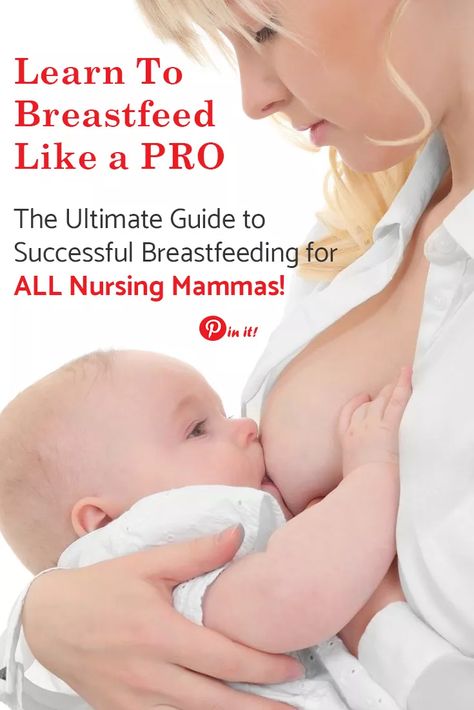
Paced feedings require closely watching your baby and the feeding cues that can indicate when more or less milk is needed, and when your baby is finished.
During breast-feeding, a baby is better able to control how much is eaten and the rate.
Bottle-feedings can make this process different, so it’s important to look for signs that your baby is taking in milk at too fast a rate. These include:
- body that appears to stiffen
- grimacing during feeding
- choking, gagging, or labored breathing while drinking
- lips that appear to turn blue
- milk that overflows from the mouth
- nasal flaring
- opening eyes widely
If you observe these signs, discontinue the feeding. If you resume the feeding, slow the height at which you hold the bottle.
Remember that you don’t have to finish a bottle with every feeding. Just as your baby may fall off the breast, the baby may not want to drink all of the milk available in the bottle.
Like breast-feeding, paced feeding is a baby-controlled method for feeding your little one.
By mimicking the pattern and flow of breast-feeding, a baby is more likely to be able to switch between breast and bottle, if desired. By watching your baby’s cues, paced feedings can seem more natural to a baby.
How to Do It and Why You'd Want To
Paced bottle feeding is a method of feeding your baby that mimics breastfeeding. Find out why it’s so beneficial to feed baby this way, plus get step-by-step guidance.
If you’re planning to go back to work after baby, you’ve probably started pumping, storing milk, and have chosen a good bottle for breastfed babies. Now, you need to know how to properly feed baby with a bottle. Paced bottle feeding is the answer.
Paced bottle feeding can help reduce some of the drawbacks of bottle feeding and keep baby and mama happy and healthy.
What is paced bottle feeding?
Paced bottle feeding is a method of feeding your baby that mimics breastfeeding. As the name suggests, it involves pacing your feedings to allow baby to be in “control” of, process, and recognize his own “satiety,” or feeling of fullness. Baby is going to eat more slowly and work harder to get the milk (like he would with breast-feeding) as opposed to typical bottle feeding.
As the name suggests, it involves pacing your feedings to allow baby to be in “control” of, process, and recognize his own “satiety,” or feeling of fullness. Baby is going to eat more slowly and work harder to get the milk (like he would with breast-feeding) as opposed to typical bottle feeding.
Video of paced bottle feeding
The best way to really “describe” paced bottle feeding is to show you how it’s done…
In this video by Emerald Doulas you’ll notice that the:
- Baby is sitting more upright
- Caregiver tickles baby’s lips with bottle
- Nipple is then put into baby’s mouth
- The bottle is held horizontally, which slows the flow significantly
- After 20–30 seconds of feeding, the bottle is tipped downward or removed from baby’s mouth to stop the flow of milk (creating a similar pattern as in breastfeeding)
Get free updates on baby’s first year! – Free Updates on First Year [In-article]
Sign me up!
How to bottle feed the breast-fed baby: Paced bottle feeding
These tips are designed to replicate breast-feeding for breast-fed babies while mom’s away, but they can absolutely be helpful for formula-fed babies too!
When should baby be fed?
Whenever baby is hungry. A schedule can be helpful as a loose guideline (for example, feeding baby every 2–3 hours), but look for feeding cues first and foremost instead of going by the clock.
A schedule can be helpful as a loose guideline (for example, feeding baby every 2–3 hours), but look for feeding cues first and foremost instead of going by the clock.
Some signs baby is hungry include:
- Smaking lips
- Sucking fists
- Rooting (baby turning with mouth wide open toward any object that touches her cheek)
- Acting fussy or restless
Baby position
Hold baby in an upright position, as opposed to laying down. This helps baby to control the flow of milk better. He doesn’t have to be at an uncomfortable 90-degree angle, but only slightly reclined so that the bottle isn’t pouring down into baby’s mouth.
Offer the bottle horizontally
Lay the bottle nipple across baby’s lips (nipple pointed up) when baby starts rooting and opening his mouth. Let baby draw the nipple into his mouth and close his lips on the base of the nipple. Baby essentially is going to “latch” on the bottle nipple like he would a breast.
Once he’s latched on, keep the bottle horizontal. This allows baby to control the flow of milk better. This also helps the bottle to last the entire length of a normal feeding, usually 10–20 minutes, rather than baby gulping a bottle down in 5 minutes.
Baby learns to recognize when he’s full because he is not filling his belly before the signals of satiety can reach his brain.
You may also consider not allowing the milk to reach the nipple of the bottle for a few minutes while baby sucks. This mimics the letdown of breast-feeding and can help reduce the chances of nipple preference.
One caveat would be if you have a really fast letdown. If your baby only nurses for 5 minutes per feeding, holding bottle at a horizontal angle is not quite as important. And frankly, paced bottle feeding probably won’t be a necessity for you since your baby is already used to a fast flow.
Pausing
Babies at the breast will pause and take breaks often throughout a feeding. Baby’s caregiver should encourage pausing while bottle-feeding as well. If baby gets tense or starts gulping, lean him forward to allow the milk to flow away from the nipple to give him a break. If he pauses on his own, great!
Baby’s caregiver should encourage pausing while bottle-feeding as well. If baby gets tense or starts gulping, lean him forward to allow the milk to flow away from the nipple to give him a break. If he pauses on his own, great!
Switch sides
Just as mom does while breast-feeding, move baby from one side to the other halfway through the feeding. This helps baby avoid a side preference, and allows for new views and eye contact, which is excellent for his development.
Ending the feeding
One big drawback of bottle feeding is the risk of over-feeding. Look for cues that baby may be getting full, such as:
- Slower sucking
- Eyes wandering
- Falling asleep
- Hands are open and relaxed
When you think baby’s getting close to being full, remove the nipple from his mouth by gently twisting. Offer it again, and if he accepts, give him about 10 sucks, and repeat until he refuses. This will help teach him the feelings of satiety and reduce the chance of over-feeding.
Likewise, don’t coerce baby into drinking the last few drops of milk in the bottle. If he falls asleep, he is finished (an exception being newborns who may need to be awakened in the first few days to feed).
Benefits of paced bottle feeding
Breast-feeding is the biological design, so it makes sense that we would want to recreate this dynamic as best we can when bottle feeding. Paced bottle feeding has many benefits, which will help your child both in the short and long-term.
Baby avoids being under- or over-fed
If the caregiver is in charge of when and how much baby eats, baby is not likely to get the correct amount of milk. Paced bottle feeding helps baby be in charge, just like when he’s at the breast.
Less stressful for baby
Babies can become very stressed when laid on their backs to eat from a bottle. When baby swallows milk from a bottle, the negative pressure forces more milk out of the bottle. Baby has to keep gulping to avoid choking.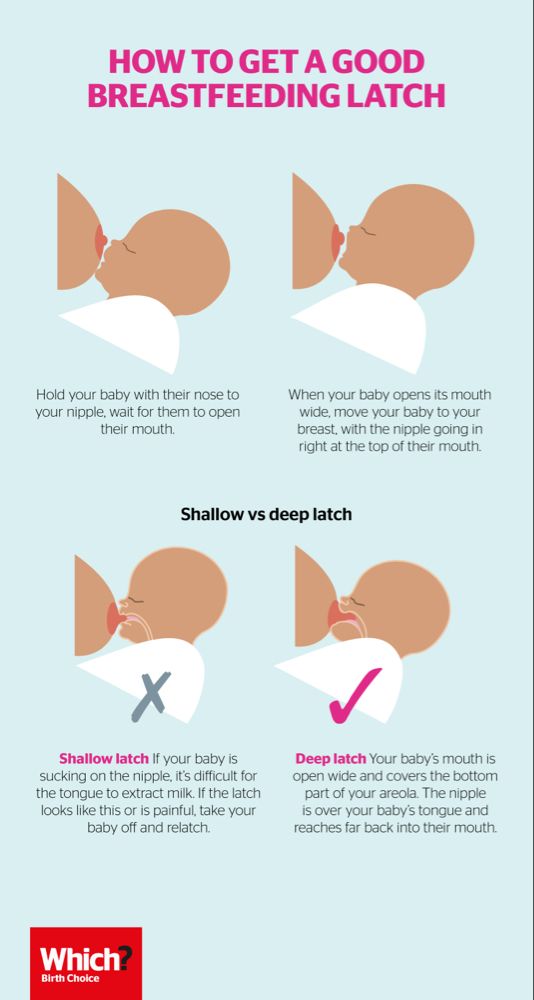 Paced feeding gives baby the time and space to eat at his or her own pace.
Paced feeding gives baby the time and space to eat at his or her own pace.
Avoid colic
Proper feeding techniques and a good bottle can minimize colic-like symptoms. When milk pours into baby’s mouth, as happens with conventional bottle feeding, baby gulps to keep up, ingesting air in the process, which can cause gas.
Easier pumping for mom
If baby is being over-fed, mom needs to continually pump extra milk to replace the milk that’s being fed. Sometimes this leads to mama believing she has low milk supply. When baby is in charge, it’s much more likely that the amount mom pumps is exactly what baby needs. (Need more pumping tips? Check out this post!)
Supports breast-feeding relationship
Using a feeding technique that resembles breast-feeding is a great way to support the breast-feeding relationship and avoid a bottle preference. We are learning that babies don’t struggle as much with “nipple confusion” as with “flow preference.” If you are consistently giving a breast-fed baby fast-flowing bottles, they will probably prefer that easier, faster milk versus the breast.
May improve health later in life
One reason that breast-feeding is so great is that it allows baby to eat at his own pace, allowing him to learn his body’s cues for satiety. Studies have found that bottle feeding plays a large part in teaching overeating. Therefore, paced bottle feeding may contribute to healthier eating habits in the future.
Which is the best bottle to use?
Some lactation consultants like a narrower nipple found in traditional bottles versus the more breast-like nipples on some bottles. They prefer this style because baby can “latch” deeply on the narrower nipple, like with a breast. Other lactation consultants say it isn’t the bottle that matters as much as the pace of milk flow.
I like the breast-shaped nippled bottles because they are almost always a slow-flow bottle and the baby has to work for the milk, regardless of how you hold it (horizontal or vertical). Here’s our post on the best bottles for breastfed babies.
Will paced bottle feeding make my baby gassy?
When I first saw demos of this feeding method, I instantly thought of baby getting gassier. However, many lactation consultants say that air isn’t what causes gas. It’s more due to baby’s immature nervous and digestive systems.
If you notice an increase in gas, switch to a breast-shaped nipple bottle, which is slow flow. Also, try holding the bottle more horizontally so that less air interferes with the feeding.
Final word on paced bottle feeding
Whether you’re going back to work full-time, part-time, are exclusively pumping, or feed formula, paced bottle feeding can be a great way to support yourself, and especially, your baby.
How about you?
Have you tried paced feeding? How has it helped your baby?
References
- https://www.llli.org/docs/0000000000000001WAB/WAB_Tear_sheet_Toolkit/22_bfabreastfedbaby.pdf
- https://www.emeralddoulas.com/
Various breastfeeding positions
Try different breastfeeding positions to find the one that works best for you and your baby. You can see the options in our selection of photos
You can see the options in our selection of photos
Share this information
There is no right or wrong way to hold the baby while
feeding, and mom and baby are sure to find their favorite position.
It is important that both you and your child feel comfortable. nine0011 1.2 It's good to learn a few different breastfeeding positions and techniques because life's circumstances often require us to be flexible, especially as your baby gets older and you start to leave the house more often.
Whatever position you choose to breastfeed your baby, remember a few simple rules.
- Prepare everything you need before feeding, including drinks, food, mobile phone, TV remote control, book or magazine. And do not forget to go to the toilet - the feeding process can take a long time! nine0018
- Make sure your baby is comfortable. Whichever position you choose, it's important to keep your baby firm, level, and provide good support for their head, neck, and spine.

- You should also be comfortable. Don't stress. If necessary, use pillows of different sizes or rolls of towels to support your back or arms.
- Make sure your baby is latching on correctly. Proper grip is the key to comfort when breastfeeding. nine0018
- If your baby does not latch on well or you experience pain while feeding, contact a lactation consultant for help. The specialist will also be able to show you how to hold your baby more comfortably.
1. Relaxed feeding or reclining position
The relaxed feeding position, also known as biological feeding, 1 is often the first position for most mothers. If, immediately after birth, the baby is placed on the mother’s chest or stomach, normally, he instinctively reaches for the breast and tries to grab the nipple. This phenomenon is known as the breast seeking reflex. Skin-to-skin contact stimulates the infant's feeding instinct, and gravity helps him to latch onto the breast and maintain balance. nine0003
nine0003
But not only newborns can be fed in the reclining position - this position is great for babies of any age. It can be especially useful if the baby does not latch well in other positions or does not like touching the head during feeding, and also if you have too much milk flow or too large breasts. Isabelle, a mother from the UK, shares her experience: “I had large breasts, and the baby was born small - 2.7 kg, so it was not easy to find a comfortable position at first. After a few weeks, it became clear that there was no “correct” posture for me. As a result, I most often fed lying down, putting the baby on my chest. ” nine0003
It is more convenient to feed not lying flat on your back, but half-sitting, leaning on pillows. So you will have a back support and you will be able to watch the baby during feeding.
2. Cradle position
This is the classic
first thought of breastfeeding. Mom sits straight
, and the baby lies on her side on her arm, pressing his stomach against her stomach. 3 Although this is a very popular position, it is not always easy to master with newborns because it gives the baby less support. Try putting a pillow under your back, and put a special breastfeeding pillow on your knees and lean on it with your hands. So you can more reliably support the child, without overstraining your back and shoulders. Just make sure that the baby does not lie too high on the pillow for feeding. The breast should remain at a natural level so that the baby can grab it without effort, otherwise sore nipples cannot be avoided. nine0003
3 Although this is a very popular position, it is not always easy to master with newborns because it gives the baby less support. Try putting a pillow under your back, and put a special breastfeeding pillow on your knees and lean on it with your hands. So you can more reliably support the child, without overstraining your back and shoulders. Just make sure that the baby does not lie too high on the pillow for feeding. The breast should remain at a natural level so that the baby can grab it without effort, otherwise sore nipples cannot be avoided. nine0003
“I breastfed in the cradle position because it suited me perfectly! It was comfortable and I loved just sitting and looking at my little one,” recalls Rachel, a mother of two from Italy.
3. Cross Cradle
This breastfeeding position looks almost the same as Cradle, but the baby is on the other arm. 3 This gives your baby support around the neck and shoulders so he can tilt his head to latch on.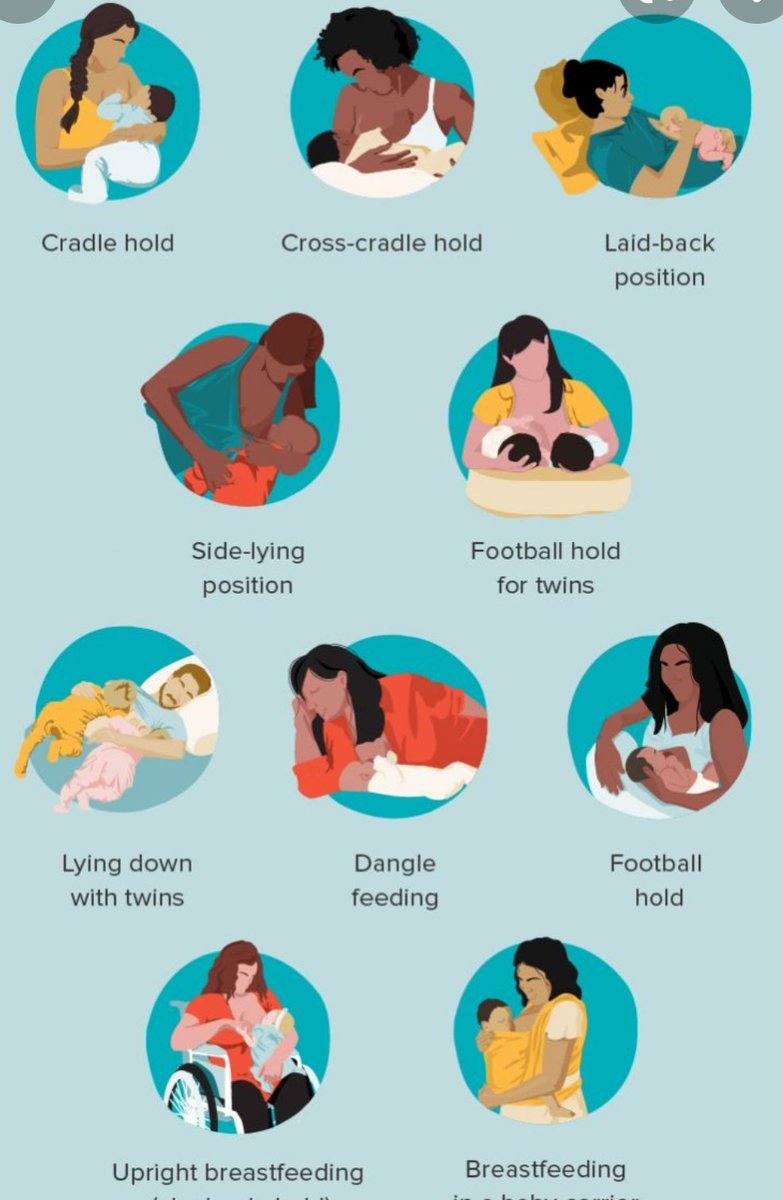 This position is great for breastfeeding newborns and small babies, as well as for babies who do not latch well. Since the baby lies completely on the other hand, it becomes easier to control his position and you can adjust the chest with your free hand. nine0003
This position is great for breastfeeding newborns and small babies, as well as for babies who do not latch well. Since the baby lies completely on the other hand, it becomes easier to control his position and you can adjust the chest with your free hand. nine0003
Julie, a mother of two from the UK, finds this position very practical: “I usually feed my youngest in the cross cradle position. So I have a free second hand, and I can take care of an older baby at the same time. ”
Do not hold the baby's head at first, otherwise you may inadvertently press his chin against his chest. Because of this, the child will not be able to take the breast deeply, because the nipple will rest against the base of the tongue, and not against the palate, which will lead to inflammation of the nipples. As the child grows, this position becomes more comfortable, and he can rest his head on your palm (as shown in the photo above). nine0003
4. Underarm breastfeeding
In this position, also known as the “ball grip”, the mother sits with the baby lying along her arm at the side, legs towards the back of the chair (or any other seat). 3 Another comfortable position for newborn breastfeeding, you can give your baby good support, full control of his position and a good view of his face. And the baby feels safe in close contact with the mother's body. This position is especially good for those who have had a caesarean section or a premature birth, as well as mothers of twins and women with large breasts. nine0003
3 Another comfortable position for newborn breastfeeding, you can give your baby good support, full control of his position and a good view of his face. And the baby feels safe in close contact with the mother's body. This position is especially good for those who have had a caesarean section or a premature birth, as well as mothers of twins and women with large breasts. nine0003
“When I breastfed my first daughter, I had very large K-sized breasts—twice the size of her head,” recalls Amy, an Australian mother of two. - I put rolls of towels under each breast, because they were very heavy, and fed my daughter in a pose from under the arm, but only sitting straighter so as not to crush her. This position was also convenient because I had a caesarean section and could not put the baby on my stomach.”
5. Side-lying position
The side-lying position is ideal for a relaxed
nighttime feeding in bed or on the couch. If you had a
caesarean section or ruptures during childbirth, this position may be more comfortable than sitting down. 3 In this position, mother and baby lie side by side, tummy to tummy.
3 In this position, mother and baby lie side by side, tummy to tummy.
“It was difficult for me to sit during endless night feedings, firstly because of the caesarean section, and secondly because of lack of sleep,” recalls Francesca, a mother from the UK. “And then I discovered that you can feed your baby lying on your side and rest at the same time.” nine0003
“Because of the short tongue frenulum, Maisie could only properly latch on to her breasts while lying on her side. The lactation consultant showed me how it's done. In this position, the flow of milk was optimal for my daughter, and it was easier for her to keep the nipple in her mouth. As she got older, she became much better at grabbing her breasts in normal positions,” says Sarah, mother of two from Australia.
6. Relaxed breastfeeding after caesarean section
If you can't find a comfortable position for breastfeeding after caesarean section, 3 try holding the baby on your shoulder in a reclining position – this does not stress the postoperative suture and allows you to breastfeed your baby comfortably. You can also try side feeding.
You can also try side feeding.
7. Sitting upright breastfeeding or “koala pose”
When breastfeeding in an upright position or “koala pose”, the baby sits with a straight back and a raised head on the mother's hip. 4 This position can be tried even with a newborn if it is well supported, but it is especially convenient for feeding a grown child who can already sit up by himself. The upright sitting position, or “koala pose,” is great for toddlers who suffer from reflux or ear infections and feel better sitting. In addition, this pose may be suitable for children with a shortened frenulum of the tongue or reduced muscle tone. nine0003
“When my daughter got a little older, I would often feed her in an upright position, which was more comfortable for both of us, and I could still hold her close,” recalls Peggy, a mother from Switzerland. “Besides, it was possible to discreetly breastfeed her in public places.”
8. Overhanging position
In this position, the baby lies on his back, and the mother bends over him
on all fours so that the nipple falls directly into his mouth. 4 Some moms say this breastfeeding position is good to use occasionally for mastitis, when touching the breasts is especially unpleasant. Some say that this breastfeeding position helps with blockage of the milk ducts, although there is no scientific evidence for this yet. You can also feed in the “overhanging” position while sitting, kneeling over the baby on a bed or sofa, as well as reclining on your stomach with support on your elbows. Pillows of various sizes that you can lean on will help you avoid back and shoulder strain. nine0003
4 Some moms say this breastfeeding position is good to use occasionally for mastitis, when touching the breasts is especially unpleasant. Some say that this breastfeeding position helps with blockage of the milk ducts, although there is no scientific evidence for this yet. You can also feed in the “overhanging” position while sitting, kneeling over the baby on a bed or sofa, as well as reclining on your stomach with support on your elbows. Pillows of various sizes that you can lean on will help you avoid back and shoulder strain. nine0003
“I have breastfed several times in the overhang position for clogged milk ducts when no other means of resolving the clogs worked. And this pose seems to have helped. I think it’s because of gravity, and also because the breasts were at a completely different angle than with normal feeding, and my daughter sucked her differently, ”says Ellie, a mother of two from the UK.
Feeding in the "overhanging" position is unlikely to be practiced regularly, but in some cases this position may be useful. nine0003
nine0003
“I used to breastfeed in the overhang position when my baby was having trouble latch-on,” says Lorna, mother of two in the UK. - This, of course, is not the most convenient way, but then I was ready for anything, if only he could capture the chest. We succeeded and have been breastfeeding for eight months now!”
9. Breastfeeding in a sling or in a sling
Breastfeeding in a sling takes some practice, but it can be used to go out, look after older children, or even do a little household chores. nine0003
The sling is also useful if the baby does not like to lie down or is often attached to the breast. Lindsey, a mother of two in the US, notes: “I used the carrier frequently for both of my children. When we were out, I tied the sarong around my neck and covered the carrier with it. Under such a cape, the baby can eat as much as he wants until he falls asleep.
This breastfeeding position is best when the baby is already good at breastfeeding and can hold his head up by himself. Any slings are suitable for breastfeeding, including elastic and rings, as well as carrying bags. Whatever option you choose, the main thing is that you can always see the face of the child, and his chin does not rest against his chest. nine0003
Any slings are suitable for breastfeeding, including elastic and rings, as well as carrying bags. Whatever option you choose, the main thing is that you can always see the face of the child, and his chin does not rest against his chest. nine0003
10. Double hand-held breastfeeding
Double hand-held breastfeeding (or “double-ball grab”) is great for mothers of twins—you can breastfeed both at the same time and keep your arms relatively free. 4 When feeding in this position, it is advisable to use a special pillow for breastfeeding twins, especially at first. It will provide extra support and help keep both babies in the correct position, as well as reduce the burden on the abdomen if you had a caesarean section. In addition, the hands are freer, and if necessary, you can deal with one child without interfering with the second. nine0003
“My twins were born very tiny and had to be fed every two hours at any time of the day or night. Very soon it became clear: if I want to do anything besides feeding, I need to feed them both at the same time, - says Emma, mother of two children from the UK.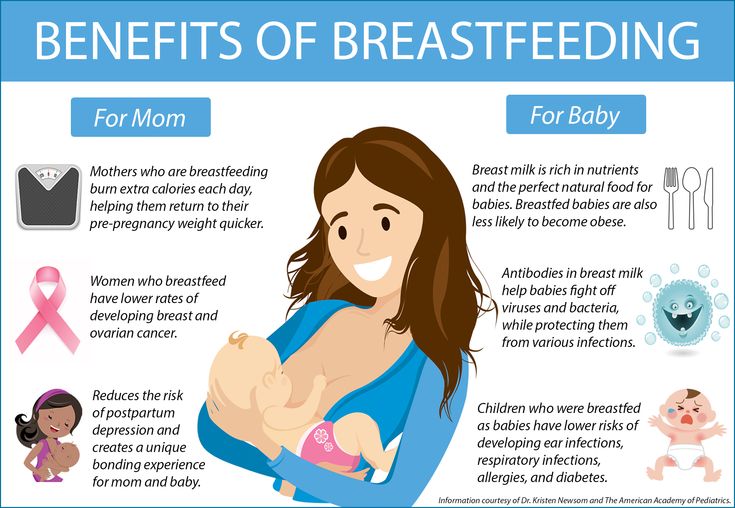 “I breastfed them two by hand using a breastfeeding pillow.”
“I breastfed them two by hand using a breastfeeding pillow.”
Other good positions for breastfeeding twins are two criss-cross cradles, one baby in the cradle and the other close at hand, reclining feeding, or sitting upright (one baby on one side, the other on the other). nine0003
11. Breastfeeding in the "hand-supported" or "dancer's hand" position
muscle tone (which is typical for premature babies, children suffering from various diseases or Down syndrome), try supporting his head and your chest at the same time. 4 Grasp your chest with your palm underneath so that your thumb is on one side and all the others are on the other. Move your hand slightly forward so that your thumb and forefinger form a "U" just in front of your chest. With the other three fingers, continue to support the chest. With your thumb and forefinger, hold the baby's head while feeding so that his chin rests on the part of the palm between them, your thumb gently holds the baby on one cheek, and your index finger on the other.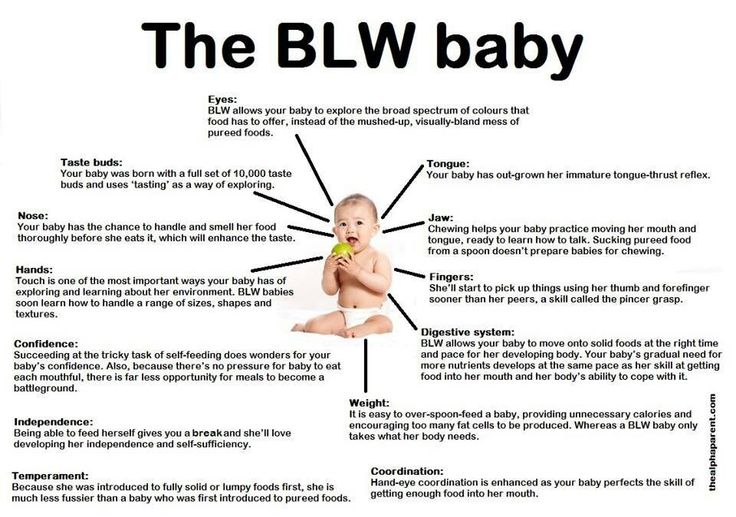 So the baby gets excellent support, and you can control his position and see if he is holding his breast. nine0003
So the baby gets excellent support, and you can control his position and see if he is holding his breast. nine0003
Literature
1 Colson SD et al. Optimal positions for the release of primitive neonatal reflexes stimulating breastfeeding. Early Hum Dev . 2008;84(7):441-449. - Colson S.D. et al., "Optimal Positions for Provoking Primitive Innate Reflexes to Induce Breastfeeding." Early Hume Dev. 2008;84(7):441-449.
2 UNICEF UK BFHI [ Internet ]. Off to the best start ; 2015 [ cited 2018 Feb ]. - UNICEF UK, Baby-Friendly Hospital Initiative, Start the Best You Can [Internet]. 2015 [cited February 2018].
3 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women's Health. nine0133 2007;52(6):638-642. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
J Midwifery & Women's Health. nine0133 2007;52(6):638-642. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
4 Wambach K, Riordan J, editors. Breastfeeding and human lactation. Jones & Bartlett Learning ; 2014. 966 p . - Wambach K., Riordan J., "Breastfeeding and female lactation". Burlington, MA: Publishing House Jones & Bartlett Learning ; 2014. Pp. 966.
Breastfeeding with pierced, flat or inverted nipples
The shape and size of nipples can vary greatly from woman to woman. Our practical tips will help you make breastfeeding easier, no matter what your nipples are.
Share this information
Most women's nipples protrude, enlarge and swell when touched, but some have flat or even inward nipples. In addition, some women pierce one or both nipples. Usually flat, inverted or pierced nipples do not cause problems when breastfeeding, but in some cases additional help may be needed.
In addition, some women pierce one or both nipples. Usually flat, inverted or pierced nipples do not cause problems when breastfeeding, but in some cases additional help may be needed.
“Don't panic if you have flat or inverted nipples. As a rule, this does not interfere with breastfeeding in any way,” says Shawnad Hilton, a lactation consultant, health visitor and newborn care specialist who has worked with Medela in the UK for more than a decade. “Remember that your baby takes into his mouth not only the nipple, but also part of the breast.” nine0003
However, in the early days, when the baby's mouth is still very small and suckling skills have not developed, inverted or flat nipples can make feeding difficult, especially if the baby is unwell or born prematurely.
“Flat or inverted nipples may not reach the baby's palate and therefore not trigger the sucking reflex,” Schoned explains. “That is, the baby may have trouble grasping and holding the breast in the mouth, and the baby will not get enough milk. ” nine0003
” nine0003
How to tell if you have flat or inverted nipples
Flat nipples 1 do not protrude much from the areola (the darker
area surrounding the nipple) even when stimulated.
Inverted nipples seem to be recessed in the center. They may look like this all the time or only if they are stimulated. Sometimes inverted nipples are on the same level with the areola, and sometimes even sink deep into the breast tissue.
This feature may occur on one or both nipples. It is estimated that approximately 10% of nulliparous women have at least one retracted nipple. nine0011 2 If you're not sure what type of nipples you have, try a simple pinch test: Gently squeeze your breast with your thumb and forefinger on both sides of the areola. The nipple should come forward. If your nipple hides inside, creating a depression, then it is retracted.
Preparing inverted and flat nipples during pregnancy
You may have noticed that during pregnancy your breasts have changed and your nipples have become more protruding. If this does not happen and you are concerned that the shape of your nipples will make breastfeeding difficult, try using nipple formers* in consultation with your doctor. These are soft and flexible silicone discs that are discreetly placed in the bra and gently squeeze the nipples, helping to pull them out. nine0003
If this does not happen and you are concerned that the shape of your nipples will make breastfeeding difficult, try using nipple formers* in consultation with your doctor. These are soft and flexible silicone discs that are discreetly placed in the bra and gently squeeze the nipples, helping to pull them out. nine0003
“In a normal pregnancy, nipple formers can be worn from 32 weeks,” advises Schoned. - Start wearing them for an hour a day, gradually increasing the time to eight hours. If you have an incompetent (weakened) cervix or are at risk of preterm labor, check with your healthcare provider about when you can start using shapers, as nipple stimulation can trigger contractions.”
“Nipple formers can be worn after childbirth,” adds Schoned. “Try to put them in a bra 30 to 60 minutes before feeding.” nine0003
“I have inverted nipples, and after two or three weeks of constantly trying to latch on, I almost switched to formula,” recalls Nina, a mother from Germany. “I turned to La Leche Liga for help, and one nice woman came to me and supported me to continue to feed. She suggested trying nipple shapers and they really helped me. Somehow my baby began to understand what to do! Breastfeeding went well and I nursed him until he was 21 months old.” nine0003
She suggested trying nipple shapers and they really helped me. Somehow my baby began to understand what to do! Breastfeeding went well and I nursed him until he was 21 months old.” nine0003
How to help your baby latch on to flat or inverted nipples
If your baby enjoys sucking on your thumb but isn't as interested in your breasts, chances are your nipple isn't reaching the palate. The baby may become nervous, push off the breast and cry or even fall asleep on your chest. If this happens, ask a lactation consultant or healthcare professional to check the grip.
There are several tricks you can use before every feed to make your nipples more comfortable to latch on to. Schoned recommends the following:
- twist the nipple between thumb and forefinger so that it protrudes better;
- Place fingers in a "V" or "C" shape and squeeze the breast just behind the areola to push out the nipple;
- apply a cold compress or ice cube to the nipple to push it forward;
- Express milk manually or with a breast pump for a couple of minutes before feeding so that the nipple comes out more.
“I had a flat nipple, but I only found out when I noticed that Austin had trouble suckling on that side,” says Jennifer, mother of two in the UK. “From an anatomical point of view, there is nothing abnormal in this, it’s just that my nipple does not protrude so much, and this requires some skill when feeding. Before giving this breast, I always pinched and squeezed the nipple a little and tried to put it into the baby's mouth. It was a little difficult at first, but over time I learned.” nine0003
Using nursing pads
If none of the above work and your baby still has difficulty latch-on, your lactation consultant or healthcare professional may recommend that you breastfeed with a nursing pad*. They are thin and flexible nipple-shaped silicone funnels with holes at the tip through which milk will flow.
It is easier for the baby to put the feeding pad in his mouth, as it is larger and more rigid. In addition, such an overlay will reach him to the sky, causing a sucking reflex. Do not use nursing pads for a long time. If you experience pain or other problems, contact your lactation consultant or healthcare professional to check that your baby is latching on properly with a breastfeeding pad. You will also need to monitor your baby's weight gain to ensure that milk production is meeting his needs. nine0011 3
Do not use nursing pads for a long time. If you experience pain or other problems, contact your lactation consultant or healthcare professional to check that your baby is latching on properly with a breastfeeding pad. You will also need to monitor your baby's weight gain to ensure that milk production is meeting his needs. nine0011 3
Over time, as your baby learns to suckle properly and your nipples get used to breastfeeding, you will be able to breastfeed without breast pads.
“My nipples are rather flat. The doctor advised me nursing pads, and I was successfully able to feed my two babies,” says Ann-Sophie, mother of two from Sweden. “My secret is to make them adhere better to the skin, I lightly wet the edges before use.”
Breastfeeding with pierced nipples
Many women with pierced nipples find it does not affect their ability to breastfeed. However, jewelry must be removed before feeding, as the child may choke on them or injure their tongue, gums or palate.
“I had a nipple piercing, but I got it off a year later when I got pregnant because my breasts were very sensitive,” says Kelly, mother of three from the UK. “I breastfed my daughter exclusively, and then her two younger brothers, and never had any problems. And the pierced nipple was my favorite!” nine0003
Some women report that milk can leak from piercings, while others believe that piercing scars reduce milk production 4 - but this has not been well researched.
“You can't predict how a piercing will affect breastfeeding until milk production starts,” Schoned explains. - If you are concerned, talk to a lactation consultant or healthcare professional. And remember that one breast may be enough for babies to get the nutrition they need if there are problems with the second. ” nine0003
What to do if you can't breastfeed with flat or inverted nipples
If you've tried all the options and still can't breastfeed, you still shouldn't deprive your baby of breastmilk.
“Mom and baby's health is the most important thing,” says Schoned. “Maybe you should switch to full pumping and feed your baby only expressed milk. You can also try the supplementary feeding system** where the baby continues to feed at the breast while receiving additional expressed milk through a tube. That is, the baby will still suck on the breast and stimulate the production of milk, which, in turn, will help you pump even more. nine0003
“I have inverted nipples. After the disastrous experience of breastfeeding my first son with my second, I decided to get my way after all,” says Babettli, mother-of-two from Italy. - On the advice of experts, I tried nipple formers and nursing pads, but everything was unsuccessful. In the end, pumping with the Medela Symphony*** Double Electronic Clinical Breast Pump proved to be the best solution for us. I fed exclusively on expressed milk for up to four months.” nine0003
Care for different types of nipples
Flat or inverted nipples may require extra care as the baby may squeeze them harder and they may become inflamed at first. Tips on how to care for sore nipples can be found in Nursing Nipple Care.
Tips on how to care for sore nipples can be found in Nursing Nipple Care.
If your nipples become inverted after a feed, any moisture can lead to inflammation and increase the risk of infections, including thrush. Blot your nipples dry after each feed before they have time to hide inside. nine0003
With swelling of the mammary glands, when even protruding nipples can become flat, flat or inverted nipples can be difficult. Read the helpful tips in the article on breast swelling.
The good news is that continuous breastfeeding or pumping can change the shape of your nipples and breastfeeding will become easier over time. With the arrival of the next child, you may not have to face this problem at all, as happened with Leanne, a mother of two from the UK. nine0003
“The second feeding was like a fairy tale,” she says. “After almost four months of pumping for my first son, my flat nipples were so extended that with my second son I no longer had to use breast pads - he was able to suck directly from the breast. The youngest is now nine months old and I still breastfeed him.”
The youngest is now nine months old and I still breastfeed him.”
Literature
1 Pluchinotta AM. The Outpatient Breast Clinic. Springer International Publishing ; 2015. - Pluchinotta A.M., "Treatment of breast diseases on an outpatient basis". Springer International Publishing. 2015.
2 Alexander JM, Campbell MJ. Prevalence of inverted and non-protractile nipples in antenatal women who intend to breast-feed. The Breast . 1997;6(2):72-78. — Alexander JM, Campbell MJ, "Prevalence of inverted and intractable nipples in pregnant women who intend to breastfeed." nine0133 Ze Brest (Chest). 1997;6(2):72-78.
3 McKechnie AC, Eglash A. Nipple shields: a review of the literature.Breastfeeding Medicine. 2010;5(6):309-314. — McKechnie A.S., Eglash A., "Nipple Covers: A Review of the Literature". Brestfeeding Medicine (Breastfeeding Medicine).