How to stop bottle feeding baby
Stopping the Bottle (for Parents)
Reviewed by: Madhu Desiraju, MD
Primary Care Pediatrics at Nemours Children's Health
en español Dejar el biberón
Many toddlers become attached to their bottles. Besides providing nourishment, bottles also mean comfort and security.
It's important for parents to start weaning babies from bottles around the end of the first year and start getting them comfortable drinking from cups. The longer parents wait to start the transition, the more attached kids become to their bottles and the harder it can be to break the bottle habit. Longer bottle use may lead to cavities or cause a child to drink more milk than they need.
Switching from bottle to cup can be challenging, but these tips can make the change easier for parents and kids.
How Should I Start the Switch?
Most doctors recommend introducing a cup around the time a baby is 6 months old. In the beginning, much of what you serve in a cup will end up on the floor or on your baby. But by 12 months of age, most babies have the coordination and hand skills needed to hold a cup and drink from it.
Age 1 is also when doctors recommend switching from formula to cow's milk. It can be a natural change to offer milk in a cup rather than a bottle.
If you're still breastfeeding, you can continue feeding your baby breast milk, but you may want to offer it in a cup.
Tips to Try
Instead of cutting out bottles all at once, try dropping them from the feeding schedule over time.
For example, if your baby usually drinks 3 bottles each day, begin by stopping the morning bottle. Instead of giving a bottle right away, bring your baby to the table and after the feeding has started, offer milk from a cup. You might encourage your baby by saying something like "You're getting so big now and can use a cup like mommy."
As you try to stop the morning bottle, keep offering the afternoon and evening bottles for about a week. That way, if your child asks for the bottle you can say that one is coming later.
The next week, stop another bottle feeding and provide milk in a cup instead. Try to do this when your baby is sitting at the table in a high chair.
Generally, the last bottle to stop should be the nighttime bottle. That bottle tends to be a part of the bedtime routine and is the one that most provides comfort to babies. Instead of the bottle, try offering a cup of milk with your child's dinner and continue with the rest of your nighttime tasks, like a bath, bedtime story, or teeth brushing.
Other tips to keep in mind:
- Spill-proof cups that have spouts designed just for babies ("sippy cups") can help ease the move from the bottle. Dentists recommend sippy cups with a hard spout or a straw, rather than ones with soft spouts.
- When your child does use the cup, offer plenty of praise. If grandma is around, for example, you might say, "See, Emma is such a big girl she drinks milk in a cup!"
- If you keep getting asked for a bottle, find out what your child really needs or wants and offer that instead.
 If your baby is thirsty or hungry, provide nourishment in a cup or on a plate. If it's comfort, offer hugs, and if your little one is bored, sit down and play!
If your baby is thirsty or hungry, provide nourishment in a cup or on a plate. If it's comfort, offer hugs, and if your little one is bored, sit down and play! - As you wean your baby from the bottle, try mixing the milk in the bottle with water. For the first few days, fill half of it with water and half of it with milk. Then slowly add more water until the entire bottle is water. By that time, it's likely that your child will lose interest and be asking for the yummy milk that comes in a cup!
- Get rid of the bottles or put them out of sight.
If you have problems or concerns about stopping the bottle, talk with your child's doctor.
Reviewed by: Madhu Desiraju, MD
Date reviewed: June 2022
How to Transition Your Baby from a Bottle to a Cup
Written by Barbara Brody
Whether you breastfeed, bottle feed, or do a combo of the two, at some point you'll wonder: Is it time to move on to a cup?
If you just breastfeed, the easiest switch is to skip bottles entirely and go straight to cups around the 1-year mark, or whenever you decide to stop nursing. If your child happily sucks on bottles, their first birthday might still be a good choice. That's because you're already changing from formula to cow's milk around that time.
If your child happily sucks on bottles, their first birthday might still be a good choice. That's because you're already changing from formula to cow's milk around that time.
Missed that window? Waiting until your baby is a little older? No worries, but don’t wait too long. The American Academy of Pediatrics suggests saying bye-bye to the bottle before your baby is 18 months old. "I'd say definitely before age 2, but the sooner the better," says Keith T. Ayoob, EdD. He’s an associate clinical professor of pediatrics at Albert Einstein College of Medicine in Bronx, N.Y.
As a registered dietitian who works with kids, Ayoob snatches the bottle from kids as old as 5 -- and he says it isn't pretty. "You have to know your child, but in general, the longer you wait the harder it is."
Why the Bottle Needs to Go
A bottle gives food and comfort to many children, so letting your little one use it for as long as they like might seem harmless enough. But there are several reasons why it's smart to switch to cups:
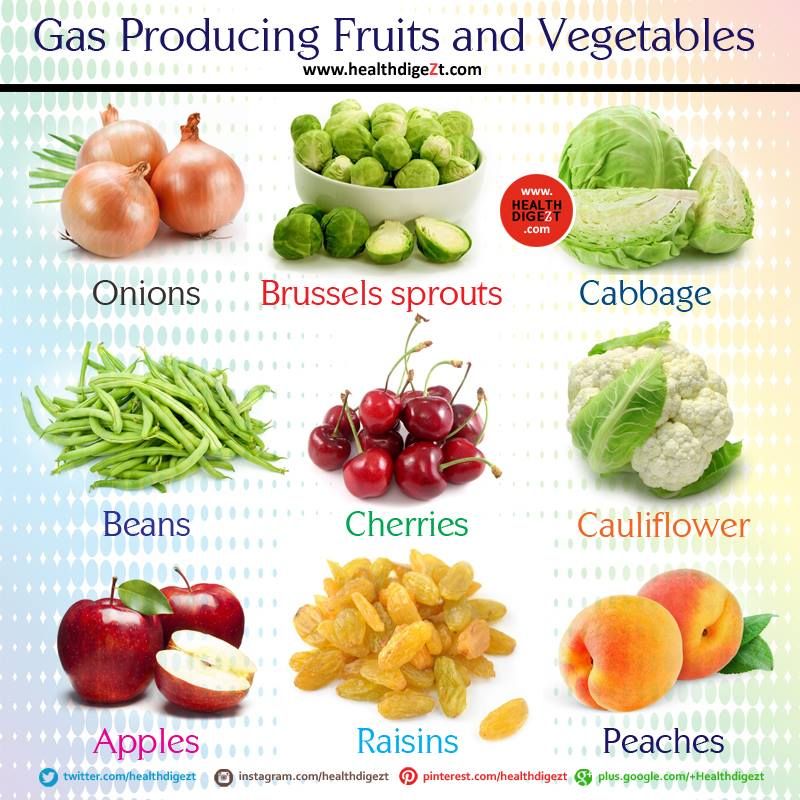
Bottles boost tooth decay.![]() Milk has lactose, a type of sugar. And if you're giving your child juice in a bottle (though you shouldn't), that's even worse. "The acid in juice is a nightmare for teeth," Ayoob says.
Milk has lactose, a type of sugar. And if you're giving your child juice in a bottle (though you shouldn't), that's even worse. "The acid in juice is a nightmare for teeth," Ayoob says.
Milk should remain an important part of your child's diet, and juice is OK now and then. Sucked from a bottle though, the sugar and acid will stay longer on their teeth, which could lead to cavities. Letting a baby go to sleep with a bottle is especially bad, because your body makes less saliva (which helps to wash away food particles) while you're asleep.
Prolonged use of a bottle is linked to obesity. Research shows that kids who are still using a bottle at age 2 are more likely to be obese by the time they're almost 6. Ayoob says some kids walk around with a bottle in their mouths all the time, even though they’re eating plenty of solid food. This can result in too many calories.
He says that being too attached to the bottle could have the opposite effect, too: With some picky eaters, the bottle becomes the “go-to meal," and a child may not be eating enough of his breakfast, lunch, or dinner.
Bottles could mess with her smile. Constant sucking can change the position of her adult teeth down the line. It can affect the development of her facial muscles and palate (roof of her mouth), says Peter Richel, MD. He's the chief of pediatrics at Northern Westchester Hospital in Mount Kisco, N.Y. This can easily lead to an overbite that might later need to be corrected with orthodontia such as braces.
Drinking while laying down increases the chance of ear infections. If your little one loves to curl up with a bottle, watch out.
"Some of the milk kind of gurgles up in the back of the throat, and it just sort of sits there while bacteria grows," Ayoob says. "Bacteria can crawl right up the Eustachian tube [in the throat] and into the ear."
Giving the Bottle the Boot
Your child should know how to drink out of a cup before you take away the bottle. Many pediatricians tell parents to introduce sippy cups around 6 to 9 months. That's when kids commonly start drinking water and other liquids besides formula and breast milk.
If, from a young age, you start giving some milk (not just water) in sippy or regular cups, then things will be easier when you're ready to get rid of the bottle for good, Richel says.
Once you decide to ditch bottles, there are two main ways to go about it: Go cold turkey, or slowly wean her off. Whichever way you choose, experts agree that sticking to it is key. "Cold turkey is the quickest but most difficult for parents, because they feel they are being cruel," Richel says.
Just don't expect either way to be easy. Even if you opt to wean slowly, "there will be some pushback," Ayoob says. "If you're trying to do it without any resistance whatsoever, you're in the wrong business."
Cold turkey: One day, you simply make all the bottles disappear. If your child is old enough to understand, it might help to include them in the process. For example, you can warn them that today is the last day for bottles, and that starting tomorrow, they are going to drink only from "big boy" cups.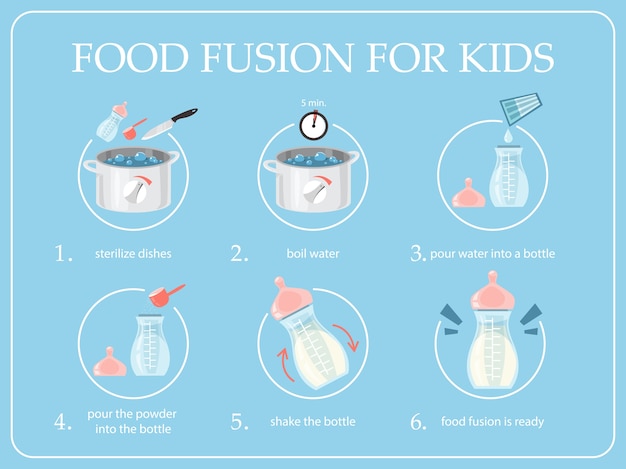
Weaning: The idea is to slowly swap out bottles in favor of cups. For example, you might fill in a cup for the bottle at just one feeding a day, then add a second cup the following week.
No matter how slow (or fast) you want to go, Ayoob says you should take away the mid-day bottles first, then the morning one. Get your child used to eating something solid first thing in the morning, he says, before you remove the morning bottle.
Most experts (and parents!) agree that taking away the nighttime bottle is the toughest final step. "Denying your baby a bottle, especially that last one before bed, can be incredibly challenging for moms and dads,” says Rallie McAllister, MD, MPH, coauthor of The Mommy MD Guide to the Toddler Years. “It makes it far more difficult to get babies to sleep, and when babies don’t sleep, neither do their parents."
To make things easier, she says to have a bedtime ritual in place. This keeps you from solely relying on the bottle to ease your child into sleep. "A nice warm bath, rocking while reading a story, and snuggling with a lovey can be great sources of comfort, security, and relaxation before bedtime, even when the bedtime bottle is no longer a part of the routine," she says.
"A nice warm bath, rocking while reading a story, and snuggling with a lovey can be great sources of comfort, security, and relaxation before bedtime, even when the bedtime bottle is no longer a part of the routine," she says.
Common Concerns
Nervous about stopping the bottle? We asked the experts to offer some extra help and support.
You're thinking: "She hates sippy cups."
The fix: To protect her teeth, try a cup that doesn't have a solid spout. It's too similar to a nipple, says Ayoob, who says a straw is a better choice. But in the end, "the best sippy cup is the one your child will drink from happily and consistently," McAllister says. "Buy a few different types and experiment. When you find one your child likes, buy a few!"
You can also have your child use regular, non-sippy cups. Still, it might take some time for her to learn to use it by herself. Give her something thick -- like vanilla yogurt or some puréed fruit that's been thinned with a little water -- to cut back on spills, Ayoob says.
You're thinking: "She'll drink water or juice from a sippy cup -- just not milk."
The fix: "Some children love the bottle so very much that they will be stubborn to take milk from anything else, but this is a temporary hunger strike!" Richel says.
Not willing to wait it out? Take the nipple off the bottle and offer it with a straw instead. Or start putting water in bottles and milk in cups and give your child a choice. "Tell her, 'Milk comes in a cup now. Water comes in a bottle. Which one do you want?'" Ayoob says. You can also try to make milk in a cup more tempting by flavoring it with puréed strawberries or other fruit. "A strawberry 'milkshake' might tempt her to drink from a cup," McAllister says.
You're thinking: "If she refuses the cup, she won't get enough calcium."
The fix: Don't worry about them not getting enough calcium, even if they refuse milk from a cup for several weeks. Just be sure to feed them other sources, such as cheese and yogurt. Broccoli, soy milk, and calcium-fortified orange juice are good picks, too.
Broccoli, soy milk, and calcium-fortified orange juice are good picks, too.
You're thinking: "He's going to throw a tantrum."
The fix: Let them. Throwing a fit is hardly out of character for a toddler, and they'll get over it. "If the parent is willing to put up with a meltdown for a day or two, it will go away," Ayoob says. "Remember, if he can drink from a cup, you're not denying him liquid."
You're thinking: "She'll never fall asleep."
The fix: Many children are used to having a bottle to settle down, but that will change. "Infants and toddlers can learn to self-soothe without the sucking that they have been accustomed to from pacifiers or bottles," Richel says. "It simply takes a bit of time. But it will happen."
Baby won't take a bottle | Philips Avent
search support iconSearch Keywords
Home ›› What to do when your baby refuses a bottle
↑ top
any problems. If your breastfed baby refuses a bottle, don't worry. This is a common occurrence in many babies who are used to breastfeeding. Obviously, this can create certain difficulties for moms, especially if you need to return to work in the near future. nine0003
If your breastfed baby refuses a bottle, don't worry. This is a common occurrence in many babies who are used to breastfeeding. Obviously, this can create certain difficulties for moms, especially if you need to return to work in the near future. nine0003
3 Philips Avent products to help you bottle feed:
So why is your baby refusing to bottle and crying? There are many ways to quickly and easily teach a breastfed baby to a bottle. Here are important tips on what to do when your baby refuses a bottle.
Is the baby refusing the bottle? Take a step back
If your baby cries while bottle feeding, the first thing to do is to start over and rethink your feeding approach and technique. Try the following steps when bottle feeding your baby: [1]
- Lift and tilt your baby's head forward. Before inserting the pacifier into the baby's mouth, make sure that the baby's head is raised and tilted over his body to avoid choking: so that the baby does not choke and have the opportunity to burp during bottle feeding.
- Insert the pacifier. Bring the pacifier to the baby's lips and gently guide it into the baby's mouth. In no case do not try to press the nipple on the baby's lips and try to push it into his mouth. After touching the pacifier to the baby's lips, wait for the baby to open his mouth and take the pacifier. nine0036
- Hold the bottle at an angle. Tilt the bottle at an angle so that the nipple is only half full. So the child can eat at his own pace.
- Let the baby burp during and after feeding. It can be useful for a child to burp not only after feeding, but also approximately in the middle of the process. This will help reduce gas or tummy discomfort that your baby may experience from swallowing too much air.
- Stop in time, do not overfeed the baby. If the baby begins to turn his head away from the bottle or closes his mouth, then he is full and you need to stop feeding.
- Perhaps the flow of milk from the nipple to the baby is weak or, on the contrary, too fast, so he is naughty and refuses the bottle.
 Try changing the nipple to a nipple with a different flow.
Try changing the nipple to a nipple with a different flow.
Other tips if your baby refuses the bottle
If you've followed the steps above and your baby still refuses the bottle, don't worry. There are other ways to help bottle feed your baby. Here are some simple tricks you can add to your bottle feeding process. nine0029 [2]
1. Remind your child about mom.
Sometimes a child can be fed by someone other than his mother - dad, grandmother or, for example, a nanny. If your baby fusses while bottle feeding, try wrapping the bottle in something that smells like mommy, like a piece of clothing or some fabric. This will make it easier to feed the baby when the mother is not around.
2. Try to maintain skin contact while bottle feeding. nine0006
Some babies need contact with their mother, so try bottle feeding while leaning against you. However, some babies are better at bottle feeding when they are in the exact opposite position than when they are breastfed. For example, there is a position with bent legs. Lay the child on your bent knees, facing you, pointing the child's legs towards your stomach. During feeding, the baby will be able to look at you and contact you in this way. If your baby refuses a bottle, experiment to see which works best. nine0003
For example, there is a position with bent legs. Lay the child on your bent knees, facing you, pointing the child's legs towards your stomach. During feeding, the baby will be able to look at you and contact you in this way. If your baby refuses a bottle, experiment to see which works best. nine0003
3. Move while feeding.
Sometimes all it takes to get your baby to take the bottle is a little wiggle or walk. The next time your baby starts crying while bottle feeding, try moving around a little rhythmically to calm him down.
4. Try changing the milk temperature.
If the baby still does not want to take the bottle, check if the milk in the bottle is too hot or too cold. Before feeding, put some warm breast milk on the inside of your wrist to check the temperature. Milk should be warm, but if it seemed hot to you, just place the bottle for a short while under a stream of cold water. nine0003
Choosing the right bottle for your baby If you plan to combine bottle feeding with breastfeeding, it is advisable to choose bottles with a nipple that will have a wide base as the bottle will grip closer to the breast.
 Also pay attention to the fact that the nipple is firm and flexible, the child must make an effort to drink from the bottle, as well as from the breast. Give preference to nipples with an anti-colic valve that vents air out of the bottle. nine0003
Also pay attention to the fact that the nipple is firm and flexible, the child must make an effort to drink from the bottle, as well as from the breast. Give preference to nipples with an anti-colic valve that vents air out of the bottle. nine0003 Natural bottle allows you to combine breast and bottle feeding. 83.3% of babies switch from a Natural bottle to breastfeeding and back.*
If you choose a bottle for artificial feeding, traditional bottles are fine, but it is desirable that the nipple is made of a hypoallergenic material, such as silicone, has an anti-colic valve and did not stick together when bottle fed. In case your baby spit up often, then use special bottles with anti-colic and anti-reflux valve, which reduces the risk of spitting up and colic.
Bottle with unique AirFree valve reduces the risk of colic, gas and spitting up. With this bottle, you can feed your baby in an upright or semi-upright position to reduce spitting up. Due to the fact that the nipple is filled with milk and not air during feeding, the baby does not swallow air, which means that feeding will be more comfortable.
Both bottles are indispensable if you want to breastfeed, bottle feed or just bottle feed your baby. nine0003
“My baby refuses to breastfeed but bottle feeds – help!”
Sometimes a baby gets used to bottle feeding and refuses to breastfeed. Therefore, it is important to use bottles that are suitable for combining breastfeeding with bottle feeding. If, nevertheless, you are faced with the fact that the child refuses to take the breast, try using silicone nipple covers to make the transition from the bottle to the breast and back more imperceptible. nine0013
Remember that if you want to combine breastfeeding and bottle feeding, it is worth waiting at least a month before offering a bottle, so that you are lactating and have time to get used to each other and develop a breastfeeding regimen.
Breastfeed and bottle feed your baby with pleasure
Remember that it takes a while for your baby to get used to bottle feeding. This is completely normal. If you have to go to work, be sure to set aside enough time to bottle train your baby beforehand. nine0013
This is completely normal. If you have to go to work, be sure to set aside enough time to bottle train your baby beforehand. nine0013
Remember that every child is different, so what works for one may not work for another. With a little time and patience, you will find out what works best for your baby when he refuses a bottle.
You will identify your child's unique needs. However, if your baby still refuses the bottle after all the steps above, check with your pediatrician.
Articles and tips from Philips Avent
References:
*O.L. Lukoyanova, T.E. Borovik, I.A. Belyaeva, G.V. Yatsyk; NTsZD RAMS; 1st Moscow State Medical University THEM. Sechenova, "The use of modern technological methods to maintain successful breastfeeding", RF, 10/02/2012 3 llli.org - The Baby Who Doesn't Nurse
llli.org - Introducing a Bottle to a Breastfed Baby
Baby+ app
Download the app and track your child's development and growth with trackers and save those special moments forever.
Download app:
You are leaving the Philips Healthcare (“Philips”) official website. Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain. nine0003
I understand
You are about to visit a Philips global content page
Continue
You are about to visit the Philips USA website.
I understand
Stopping breastfeeding | Stopping breastfeeding
When is it time to stop breastfeeding and what is the best way to do it? Read our article for useful practical tips on weaning.
Share this information nine0003
How long should breastfeeding continue? Three months? Six? Year? Or maybe a few years?
The World Health Organization (WHO) and other authorities recommend that infants be exclusively breastfed for the first six months and then continue to be breastfed along with other foods (complementary foods) for at least two years. 1
1
The fact is that breast milk is not just food. It is a natural sedative if the child is anxious or tired. In addition, milk contains immune-boosting components, the amount of which increases dramatically when the baby gets sick. nine0029 2
According to anthropologists, the natural age of a person to stop breastfeeding is even more than two years. Given factors such as tooth development, body weight, comparison with other primates, and historical evidence, some scientists believe that breastfeeding may last up to two to four years. A number of researchers even believe that our ancestors breastfed children up to six or seven years of age. 3
Today, more than 60% of mothers in developed countries start giving their babies formula or complementary foods before six months, 4 although not recommended by WHO.
When is it time to stop breastfeeding?
Weaning means that you gradually stop breastfeeding your baby. Ideally, the first step in this process is the gradual introduction of complementary foods, starting at about six months of age. In this case, breastfeeding continues. The weaning process continues until the mother's milk has been completely replaced by other foods and drinks. nine0003
Ideally, the first step in this process is the gradual introduction of complementary foods, starting at about six months of age. In this case, breastfeeding continues. The weaning process continues until the mother's milk has been completely replaced by other foods and drinks. nine0003
“After six months, the baby needs higher doses of certain nutrients, such as iron, zinc, vitamins B and D, that he cannot get from breast milk or from his own reserves,” says Sarah Beeson, health visitor from Great Britain.
“But solid food should at first only supplement the main diet with breast milk and gradually replace it. Mother's milk remains the main source of nutrition for the baby for many months to come.” nine0003
On average, a seven-month-old baby gets 93% of its calories from breast milk. And even between the 11th and 16th months, milk provides him with about half of the daily calorie intake. 5
“Sometimes moms think that breastmilk is not so important once the baby has started solid foods, but in reality, no matter how many months old the baby is, there is nothing better for him than your milk,” continues Sarah.
In fact, the process of finishing breastfeeding can take as long as mother and baby want. “When to stop breastfeeding is up to you,” says Sarah. The only thing that matters is what you think is right for you and your child.” nine0003
How to wean
Whenever you decide to start weaning your baby, it is best to do it gradually. An abrupt cessation of breastfeeding can lead to lactostasis, blockage of the milk ducts and mastitis, and in a child such a sudden change can adversely affect the state of the digestive and immune systems. In addition, it will be difficult for both of you psychologically.
When should I stop breastfeeding?
Sometimes mothers mistakenly believe that it is time to stop breastfeeding, when in fact there is no reason to. If you're returning to work, breastfeeding can be a great way to stay close to your baby during this difficult time for both of you. You can express milk at work, and morning and evening feeding sessions will give you the opportunity to spend time alone with your baby. If you need to leave without your baby, you can also express milk and bring or send it home. nine0003
If you get sick, this is not always a reason to stop breastfeeding. Read our advice in the article on breastfeeding when sick and consult with your healthcare professional.
Weaning up to six months
If you can't continue breastfeeding until six months and want to try weaning your baby, start by replacing one feeding a day with a bottle of formula.
“It's best to start with midday feedings. Babies are very alert and able to smell breast milk nearby, so ask your partner or relative to give your baby a bottle when you're in the other room,” Sarah advises. nine0003
“Be hygienic when preparing meals. Be prepared for the fact that the baby will take fewer servings of expressed milk per day than if he was fed directly from the breast. Don't make him eat more milk than he wants."
You will probably feel that your breasts are fuller and more tender. This is due to the fact that your body is rebuilding to produce less milk. If this creates discomfort, try expressing some milk—just enough to relieve the discomfort without stimulating extra production. nine0003
When your body adjusts to the new volume - usually after a few days - replace with formula for one more meal a day. Continue this until you have changed all feedings and your baby is completely weaned.
“I had complications after my first birth, as a result I lost a lot of weight very quickly, and besides, I developed mastitis. Lactation was very weak, and at three months I was forced to stop breastfeeding,” recalls Jennifer, a mother of two from the UK, “I gradually replaced one feeding, so physically it was easy, but mentally it was hard for me.” nine0003
If you want to maintain closeness with your baby and all the health benefits of breastfeeding, but still need to cut down on breastfeeding, try partial weaning, replacing only a few feeds a day with formula.
Weaning after six months
Once your baby starts eating solid foods (about six months old), you will notice that breastfeeding naturally occurs less and less. For a year, it can be reduced to just a couple of times a day, and feedings will be replaced by full meals and healthy snacks. nine0003
Anyway, if you intend to continue to reduce breastfeeding, do it gradually, replacing one feeding at a time. Use formula milk if your baby is under 12 months old. With cow's milk, you should wait at least up to a year.
“When I decided to wean my son, I breastfed him three times a day and gave him other foods three times plus light snacks. Gradually, I replaced all breastfeedings with formula. By 11 months, we only had one nighttime breastfeed left,” says Ruth, a UK mom. nine0003
There are various ways to distract a child from changes in his diet. Some mothers suggest that instead of breastfeeding something to drink and eat together to maintain a sense of closeness. You can also change your daily routine, play your favorite game, or replace feeding with caresses - from you or from your partner. Some children take longer to get used to the new food, but in the end everything falls into place. If you are having difficulty weaning, ask your healthcare provider for advice. nine0003
You can also change your daily routine, play your favorite game, or replace feeding with caresses - from you or from your partner. Some children take longer to get used to the new food, but in the end everything falls into place. If you are having difficulty weaning, ask your healthcare provider for advice. nine0003
Ending breastfeeding naturally
Ending breastfeeding can be guided by the baby's wishes. This is called baby-initiated weaning, or the natural termination of breastfeeding. Such a process is likely to be long and gradual. Month after month, feeding sessions will become shorter and less frequent, until one day the child completely loses interest in the breast.
“My daughter stopped breastfeeding on her own when she was four years old,” says Sarah, a mother from the UK. And once, when we were on vacation, she seemed to just forget about her breasts. Now, six months later, she sometimes still asks for breasts, but she already knows that there is no milk there. nine0003
nine0003
You will have a huge amount of time for the body to adapt, so there should be no discomfort or swelling of the breast. However, you may find it difficult emotionally, so spend more time petting and bonding with your baby.
“Child-initiated termination of breastfeeding was right for me because I never gave my son formula or a bottle. I didn’t want to abruptly stop feeding and refuse him,” recalls Kelly, a mother from the UK, “He himself lost interest in breasts at the age of two and a half years. For us, it was the best scenario, although emotionally it was not very easy for me.” nine0003
What if you need to stop breastfeeding quickly?
It is best not to stop breastfeeding abruptly, but sometimes it is necessary for medical reasons or because you cannot be near your baby.
If you have been breastfeeding your baby up to this point, you will most likely have to express your milk to avoid breast swelling. Some mothers prefer to use a breast pump for this, others find it easier to express milk manually. You only need to pump a little, just to eliminate the discomfort, otherwise your body will take it as a signal to produce more milk. nine0003
You only need to pump a little, just to eliminate the discomfort, otherwise your body will take it as a signal to produce more milk. nine0003
At first, the breasts may swell and become tender, but this will pass. Breast milk contains a so-called feedback lactation inhibitor. When breastfeeding is stopped, this inhibitor tells your body to slow down milk production, but it can take days or even weeks for your breasts to rebuild.
Certain medications can relieve pain and should be discussed with your doctor. Always follow your pharmacist's instructions or directions, and consult your healthcare professional before taking any medication. nine0003
“I had to abruptly stop breastfeeding when my daughter was eight months old because she had to take strong painkillers,” says Peggy, a mother from Switzerland. “It was very difficult because the baby was constantly looking for a breast and crying. I held her tightly to me as I gave her a bottle. This calmed her, and after a month everything was all right.
Can I continue breastfeeding if I want to get pregnant again?
Breastfeeding is a natural contraceptive. However, this method is not the most reliable, especially after six months or if you are not exclusively breastfeeding. This means that you can get pregnant even while you are breastfeeding. nine0003
Pregnant and breastfeeding mothers sometimes receive conflicting advice about whether to stop breastfeeding. Consistent feeding of two children of different ages is of course possible, and with the advent of the second baby, your body will produce the kind of milk that both of them need.
It is not uncommon for an older child to refuse to breastfeed or skip feedings if the mother is pregnant. This may be due to changes in milk composition that occur during pregnancy. Milk can change the taste and become less sweet. nine0029 6 If your baby is under one year of age when he starts to stop breastfeeding, make sure he continues to gain weight.
Talk to your doctor if you want to continue breastfeeding during pregnancy, but have had a preterm birth or miscarriage, or have any bleeding in the past.
If you need medical help to conceive, certain drugs and procedures may not be suitable while you are breastfeeding. Discuss all possible options before deciding to stop breastfeeding. nine0003
And finally...
Whenever you decide to end breastfeeding, and whatever method you choose to do so, be kind to yourself and your baby. This is a huge change for both of you physically, hormonally, and emotionally, so proceed thoughtfully and carefully.
“Although my body responded normally to stopping breastfeeding, it was psychologically difficult for me. The thing that united us for so long is over, - Jane, a mother of two children from the USA, shares her impressions, - I worked long hours, five days a week, and breastfeeding made me feel that I occupy a special place in the lives of children. But when it stopped, we soon found other ways to be together.” nine0003
Literature
1 World Health Organization. [Internet] Health Topics: Breastfeeding: 2018 [Accessed: 02/08/2018]. Available from : http://www.who.int/topics/breastfeeding/en - World Health Organization. "Health Issues: Breastfeeding" [Internet]. Geneva, Switzerland: WHO; 2018 [Visit 02/08/2018]. Article linked: http://www.who.int/topics/breastfeeding/e
Available from : http://www.who.int/topics/breastfeeding/en - World Health Organization. "Health Issues: Breastfeeding" [Internet]. Geneva, Switzerland: WHO; 2018 [Visit 02/08/2018]. Article linked: http://www.who.int/topics/breastfeeding/e
2 Hassiotou et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin Transl Immunology. 2013;2(4): e 3. - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
3 Dettwyler KA. When to wean: biological versus cultural perspectives.Clin Obstet Gynecol . 2004; 47(3)712-723. - Dettwiler KA, "Time to wean: weaning from a biological and cultural point of view". Klin Obstet Ginekol (Clinical obstetrics and gynecology). 2004; 47(3):712-723.
2004; 47(3):712-723.
4 Victora CG Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. nine0305 2016;387(10017):475-490. - Victor S.J. et al., "Breastfeeding in the 21st century: epidemiology, mechanisms and long-term effects". Lancet 2016;387(10017):475-490.
5 Dewey KG et al. Breast milk volume and composition during late lactation (7-20 months). J Pediatr Gastroenterol Nutr . 1984;3(5):713-720. — Dewey C.G. et al., "Amount and composition of breast milk in late lactation (7-20 months)". nine0305 F Pediatrician Gastroenterol Nutr. 1984;3(5):713-720.
6 Prosser CG et al. Mammary gland function during gradual weaning and early gestation in women. Aust J Exp Biol Med 1984;62( Pt 2):215-228.