Nhs baby feeding guidelines
Bottle feeding advice - NHS
If you're planning to bottle feed with expressed breast milk or infant formula, these tips will help you feed your baby and keep them safe and healthy.
If you decide to use infant formula, first infant formula (first milk) should always be the first formula you give your baby. You can use it throughout the first year.
Buying bottle feeding equipment
You'll need several bottles, teats and a bottle brush, as well as sterilising equipment, such as a cold-water steriliser, microwave or steam steriliser.
There's no evidence that 1 type of teat or bottle is better than any other. Simple bottles that are easy to wash and sterilise are probably best.
Making up bottles for your baby
Make sure you sterilise bottles and teats until your baby is at least 12 months old. Wash your hands thoroughly before handling sterilised bottle and teats.
If you're using infant formula, follow the instructions on the packaging carefully when you make up the feed.
See how to make up baby formula.
How to bottle feed your baby
Bottle feeding is a chance to feel close to your baby and get to know and bond with them. Babies will feel more secure if most feeds are given by you, your partner or their main caregiver.
Make sure you're sitting comfortably with your baby close to you. Enjoy holding your baby, look into their eyes and talk to them as you feed them.
Hold your baby in a semi-upright position for bottle feeds. Support their head so they can breathe and swallow comfortably.
Brush the teat against your baby's lips and when they open their mouth wide let them draw in the teat.
Always give your baby plenty of time to feed.
Do not leave your baby alone
Never leave your baby alone to feed with a propped-up bottle as they may choke on the milk.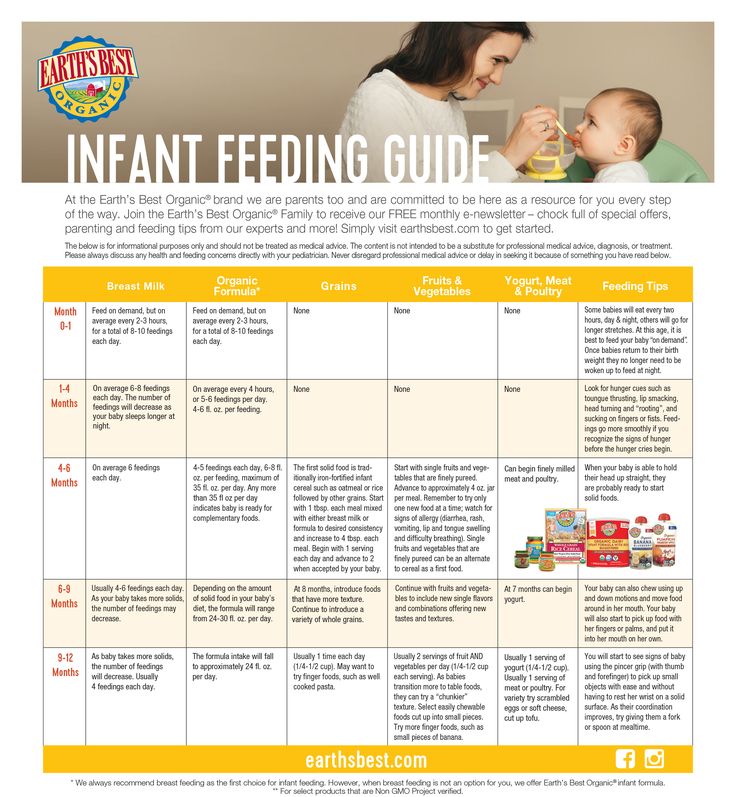
Keep the bottle horizontal
Gently place the teat into the baby’s mouth. Keep the bottle in a horizontal position (just slightly tipped). This will allow the milk to flow steadily and help prevent your baby from taking in air.
If the teat goes flat while you're feeding, pull gently on the corner of your baby's mouth to release the suction.
If the teat gets blocked, replace it with another sterile teat.
Be guided by your baby
All babies are different. Your baby will know how much milk they need. Some want to feed more often than others. Just follow your baby's lead.
Feed your baby when they seem hungry and do not worry if they do not finish the bottle.
Winding your baby
Your baby may take short breaks during a feed and may sometimes need to burp.
When your baby has had enough milk, hold them upright and gently rub or pat their back to bring up any wind.
Throw away unused milk
Throw away any unused formula or breast milk after you've finished bottle feeding your baby.
Only make up the feed when needed – one feed at a time.
Help with bottle feeding
Talk to your midwife, health visitor or other mothers who have bottle fed if you need help and support.
You'll find the phone number for your health visitor in your baby's personal health record (red book).
Your questions about bottle feeding
Why if my baby does not settle after feeds?
If your baby swallows air while bottle feeding, they may feel uncomfortable and cry.
After a feed, hold your baby upright against your shoulder or propped forward on your lap. Gently rub their back so any trapped air can find its way out.
Your baby may sometimes only burp up a small amount of air.
Why is my baby sometimes sick after feeds?
It's normal for babies to bring up a little milk during or just after a feed. This is called possetting, regurgitation or reflux.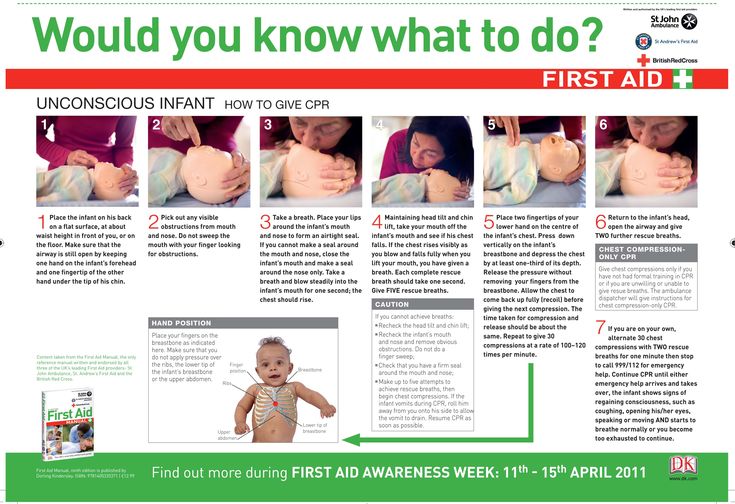
Keep a muslin square handy just in case.
Check that the hole in your baby's teat is not too big. Drinking milk too quickly can make your baby sick.
Do not force them to take more milk than they want during a feed. This may be distressing for your baby and can lead to overfeeding.
Sitting your baby upright on your lap after a feed may help.
If it happens a lot, or your baby is violently sick, seems to be in pain or you're worried for any other reason, talk to your health visitor or GP.
Can formula make my baby constipated?
When using formula, always use the amount of powder recommended on the packaging.
Do not add extra formula powder. Using too much can make your baby constipated and may cause dehydration.
If your baby is under 8 weeks old and has not done a poo for 2 to 3 days, talk to your midwife, health visitor or GP, particularly if your baby is gaining weight slowly.
Your baby should be gaining weight and have plenty of wet and dirty nappies.
Infant formula and allergies
If you think your baby might be allergic to or intolerant of formula, talk to your GP. If necessary, they can prescribe a special formula feed.
Some formula is labelled as hypoallergenic, but this is not suitable for babies with a diagnosed cows' milk allergy.
Soya formula should only be given to babies under medical supervision.
Always talk to your GP before using hypoallergenic or soya-based formula.
Read more about cows' milk allergy and lactose intolerance.
Get Start4Life pregnancy and baby emails
For information and advice you can trust, sign up for weekly Start4Life pregnancy and baby emails.
The Start4Life website also has more information and advice about expressing and bottle feeding
Your baby's first solid foods
When to start introducing solid foods
Introducing your baby to solid foods, sometimes called complementary feeding or weaning, should start when your baby is around 6 months old.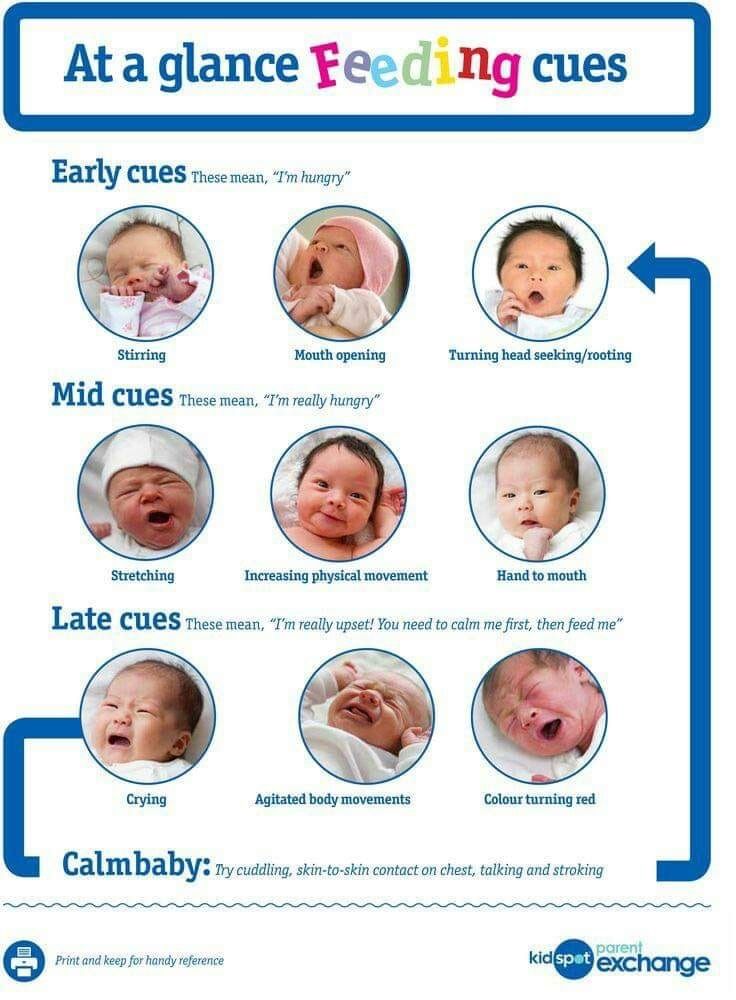
At the beginning, how much your baby eats is less important than getting them used to the idea of eating.
They'll still be getting most of their energy and nutrients from breast milk or first infant formula.
Giving your baby a variety of foods, alongside breast or formula milk, from around 6 months of age will help set your child up for a lifetime of healthier eating.
Gradually, you'll be able to increase the amount and variety of food your baby eats until they can eat the same foods as the rest of the family, in smaller portions.
If your baby was born prematurely, ask your health visitor or GP for advice on when to start introducing solid foods.
Why wait until around 6 months to introduce solids?
It’s a good idea to wait until around 6 months before introducing solid foods because:
- breast milk or first infant formula provide the energy and nutrients your baby needs until they're around 6 months old (with the exception of vitamin D in some cases)
- if you're breastfeeding, feeding only breast milk up to around 6 months of age will help protect your baby against illness and infections
- waiting until around 6 months gives your baby time to develop so they can cope fully with solid foods – this includes solid foods made into purées, cereals and baby rice added to milk
- your baby will be more able to feed themselves
- your baby will be better at moving food around their mouth, chewing and swallowing it – this may mean they'll be able to progress to a range of tastes and textures (such as mashed, lumpy and finger foods) more quickly, and may not need smooth, blended foods at all
Signs your baby is ready for solid foods
There are 3 clear signs which, when they appear together from around 6 months of age, show your baby is ready for their first solid foods alongside breast milk or first infant formula.
They'll be able to:
- stay in a sitting position and hold their head steady
- co-ordinate their eyes, hands and mouth so they can look at the food, pick it up and put it in their mouth by themselves
- swallow food (rather than spit it back out)
The following behaviours can be mistaken by parents as signs that their baby is ready for solid foods:
- chewing their fists
- waking up in the night (more than usual)
- wanting extra milk feeds
These are all normal behaviours for babies and not necessarily a sign that they're hungry or ready to start solid food.
Starting solid foods will not make your baby any more likely to sleep through the night. Sometimes a little extra milk will help until they're ready for solid foods.
Get tips to help your baby sleep well
How to start solid foods
In the beginning your baby will only need a small amount of food before their usual milk feed.
Do not worry about how much they eat. The most important thing is getting them used to new tastes and textures, and learning how to move solid foods around their mouths and how to swallow them.
They'll still be getting most of their energy and nutrients from breast milk or infant formula.
There are some foods to avoid giving to your baby. For example, do not add sugar or salt (including stock cubes and gravy) to your baby's food or cooking water.
Babies should not eat salty foods as it's not good for their kidneys, and sugar can cause tooth decay.
Tips to get your baby off to a good start with solid foods:
- Eating is a whole new skill.
 Some babies learn to accept new foods and textures more quickly than others. Keep trying, and give your baby lots of encouragement and praise.
Some babies learn to accept new foods and textures more quickly than others. Keep trying, and give your baby lots of encouragement and praise. - Allow plenty of time, especially at first.
- Go at your baby's pace and let them show you when they're hungry or full. Stop when your baby shows signs that they've had enough. This could be firmly closing their mouth or turning their head away. If you're using a spoon, wait for your baby to open their mouth before you offer the food. Do not force your baby to eat. Wait until the next time if they're not interested this time.
- Be patient and keep offering a variety of foods, even the ones they do not seem to like. It may take 10 tries or more for your baby to get used to new foods, flavours and textures. There will be days when they eat more, some when they eat less, and then days when they reject everything. Do not worry, this is perfectly normal.
- Let your baby enjoy touching and holding the food.
 Allow them to feed themselves, using their fingers, as soon as they show an interest. If you're using a spoon, your baby may like to hold it or another spoon to try feeding themselves.
Allow them to feed themselves, using their fingers, as soon as they show an interest. If you're using a spoon, your baby may like to hold it or another spoon to try feeding themselves. - Keep distractions to a minimum during mealtimes and avoid sitting your baby in front of the television, phone or tablet.
- Show them how you eat. Babies copy their parents and other children. Sit down together for family mealtimes as much as possible.
Texture progression
Once you've started introducing solid foods from around 6 months of age, try to move your baby on from puréed or blended foods to mashed, lumpy or finger foods as soon as they can manage them.
This helps them learn how to chew, move solid food around their mouth and swallow.
Some babies like to start with mashed, lumpy or finger foods.
Other babies need a little longer to get used to new textures, so may prefer smooth or blended foods on a spoon at first.
Just keep offering them lumpy textures and they'll eventually get used to it.
Safety and hygiene
When introducing your baby to solid foods, it's important to take extra care to not put them at risk.
Key food safety and hygiene advice:
- always wash your hands before preparing food and keep surfaces clean
- cool hot food and test it before giving it to your baby
- wash and peel fruit and raw vegetables
- avoid hard foods like whole nuts, or raw carrot or apple
- remove hard pips and stones from fruits, and bones from meat or fish
- cut small, round foods, like grapes and cherry tomatoes, into small pieces
- eggs produced under the British Lion Code of Practice (stamped with the red lion) are considered very low risk for salmonella and safe for babies to eat partially cooked
Always stay with your baby when they're eating in case they start to choke.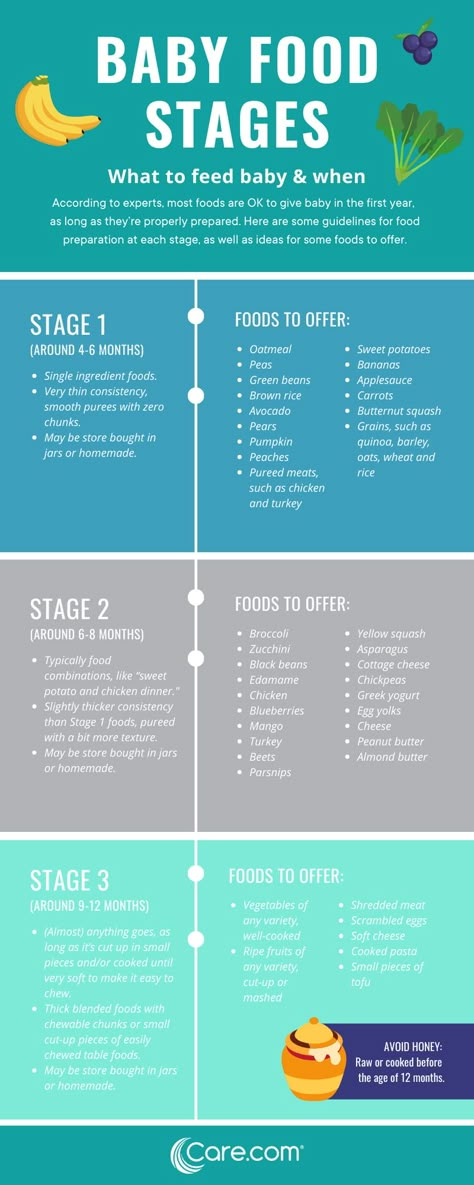
Choking is different from gagging. Your baby may gag when you introduce solid foods.
This is because they're learning how to deal with solid foods and regulate the amount of food they can manage to chew and swallow at one time.
If your baby is gagging:
- their eyes may water
- they might push their tongue forward (or out of their mouth)
- they might retch to bring the food forward in their mouth or vomit
Equipment checklist
- High chair. Your baby needs to be sitting safely in an upright position (so they can swallow properly). Always use a securely fitted safety harness in a high chair. Never leave babies unattended on raised surfaces.
- Plastic or pelican bibs. It's going to be messy at first!
- Soft weaning spoons are gentler on your baby's gums.

- Small plastic bowl. You may find it useful to get a special weaning bowl with a suction base to keep the bowl in place.
- First cup. Introduce a cup from around 6 months and offer sips of water with meals. Using an open cup or a free-flow cup without a valve will help your baby learn to sip and is better for their teeth.
- A messy mat or newspaper sheets under the high chair to catch most of the mess.
- Plastic containers and ice cube trays can be helpful for batch cooking and freezing small portions.
Find out more:
- tips to help your baby enjoy new foods
- children's food: safety and hygiene
- foods to avoid giving babies and young children
- how to stop a child from choking
- baby and toddler safety
Feeding your baby: from 0 to 6 months
Breast milk is the best food your baby can have during their first 6 months of life.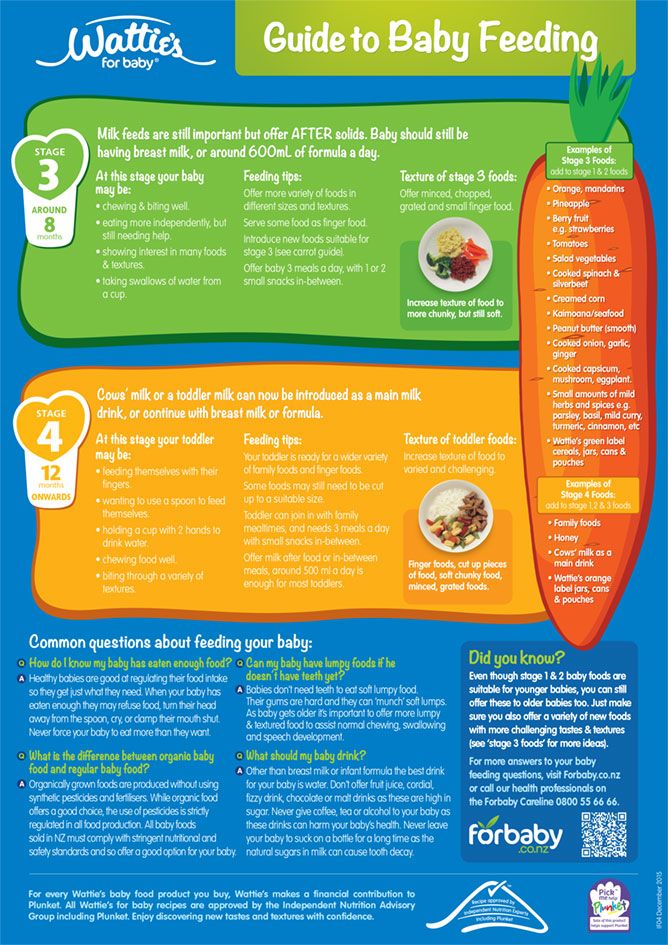
It's free, always available and at the perfect temperature, and is tailor-made for your baby.
First infant formula is the only suitable alternative if you do not breastfeed or choose to supplement breast milk.
Other milks or milk substitutes, including cows' milk, should not be introduced as a main drink until 12 months of age.
"Follow-on" formula is not suitable for babies under 6 months, and you do not need to introduce it after 6 months.
Babies do not need baby rice to help them move to solid foods or sleep better.
When using a bottle, do not put anything (such as sugar or cereals) in it other than breast milk or infant formula.
Vitamins for babies
It's recommended that breastfed babies are given a daily supplement containing 8.5 to 10 micrograms (µg) of vitamin D from birth, whether or not you're taking a supplement containing vitamin D yourself.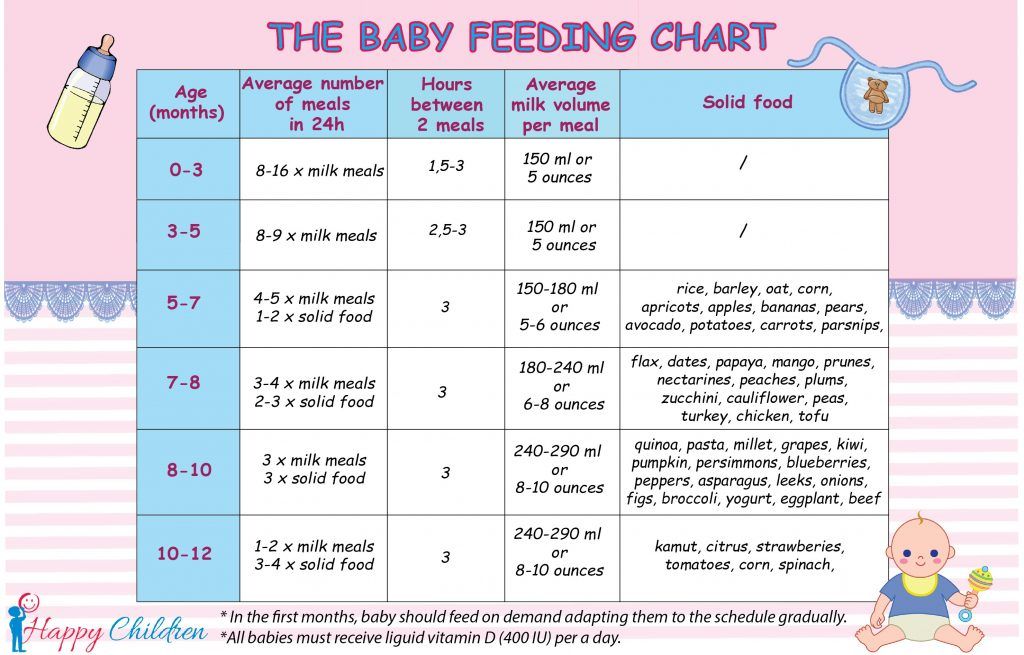
Babies having 500mls (about a pint) or more of formula a day should not be given vitamin supplements.
This is because formula is fortified with vitamin D and other nutrients.
All children aged 6 months to 5 years should be given vitamin supplements containing vitamins A, C and D every day.
Find out more:
- benefits of breastfeeding
- how to make up baby formula
- vitamins for children
Feeding your baby: from around 6 months
When they first start having solid foods, babies do not need 3 meals a day. Babies have tiny tummies, so start by offering them small amounts of food (just a few pieces, or teaspoons of food).
Pick a time that suits you both, when you do not feel rushed and your baby is not too tired.
Start offering them food before their usual milk feed as they might not be interested if they're full, but do not wait until your baby is too hungry.
Allow plenty of time and let your baby go at their own pace.
Keep offering different foods, even foods your baby has already rejected.
It can take 10 tries or more before your baby will accept a new food or texture, particularly as they get older.
Your baby will still be getting most of their energy and nutrients from breast milk or first infant formula.
Breast milk or infant formula should be their main drink during the first year. Do not give them whole cows' (or goats' or sheep's) milk as a drink until they're 1 year old.
You can continue breastfeeding for as long as you both want.
Introduce a cup from around 6 months and offer sips of water with meals.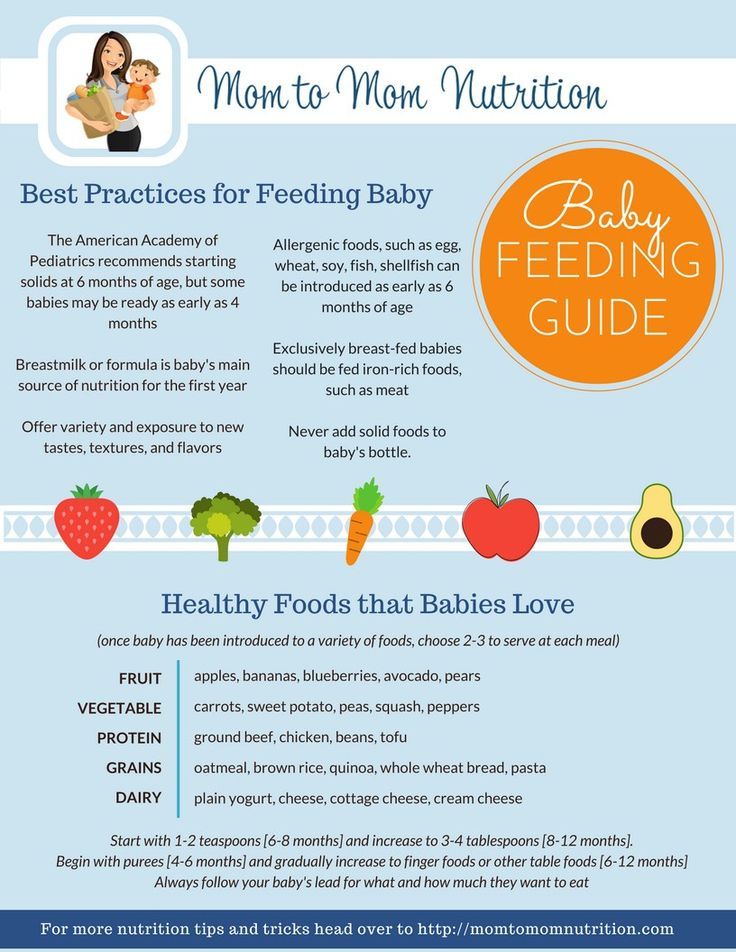 Using an open cup or a free-flow cup without a valve will help your baby learn to sip and is better for their teeth.
Using an open cup or a free-flow cup without a valve will help your baby learn to sip and is better for their teeth.
First foods
You might want to start with single vegetables and fruits.
Try mashed or soft cooked sticks of parsnip, broccoli, potato, yam, sweet potato, carrot, apple or pear.
Include vegetables that are not sweet, such as broccoli, cauliflower and spinach.
This will help your baby get used to a range of flavours (rather than just the sweeter ones, like carrots and sweet potato) and might help prevent them being fussy eaters as they grow up.
Make sure any cooked food has cooled right down before offering it to your baby.
Foods containing allergens (such as peanuts, hens' eggs, gluten and fish) can be introduced from around 6 months of age, 1 at a time and in small amounts so you can spot any reaction.
Cows' milk can be used in cooking or mixed with food from around 6 months of age, but should not be given as a drink until your baby is 1 year old.
Full-fat dairy products, such as pasteurised cheese and plain yoghurt or fromage frais, can be given from around 6 months of age. Choose products with no added sugar.
Remember, babies do not need salt or sugar added to their food (or cooking water).
Finger foods
As soon as your baby starts solid foods, encourage them to be involved in mealtimes and have fun touching, holding and exploring food.
Let them feed themselves with their fingers when they want to. This helps develop fine motor skills and hand-eye co-ordination.
Your baby can show you how much they want to eat, and it gets them familiar with different types and textures of food.
Offering your baby finger foods at each meal is a good way to help them learn to self-feed.
Finger food is food that's cut up into pieces big enough for your baby to hold in their fist with a bit sticking out.
Pieces about the size of your own finger work well.
Start off with finger foods that break up easily in their mouth and are long enough for them to grip.
Avoid hard food, such as whole nuts or raw carrots and apples, to reduce the risk of choking.
Examples of finger foods include:
- soft cooked vegetables, such as carrot, broccoli, cauliflower, parsnip, butternut squash
- fruit (soft, or cooked without adding sugar), such as apple, pear, peach, melon, banana
- grabbable bits of avocado
- cooked starchy foods, such as potato, sweet potato, cassava, pasta, noodles, chapatti, rice
- pulses, such as beans and lentils
- fish without bones
- hardboiled eggs
- meat without bones, such as chicken and lamb
- sticks of pasteurised full-fat hard cheese (choose lower salt options)
Baby-led weaning
Baby-led weaning means giving your baby only finger foods and letting them feed themselves from the start instead of feeding them puréed or mashed food on a spoon.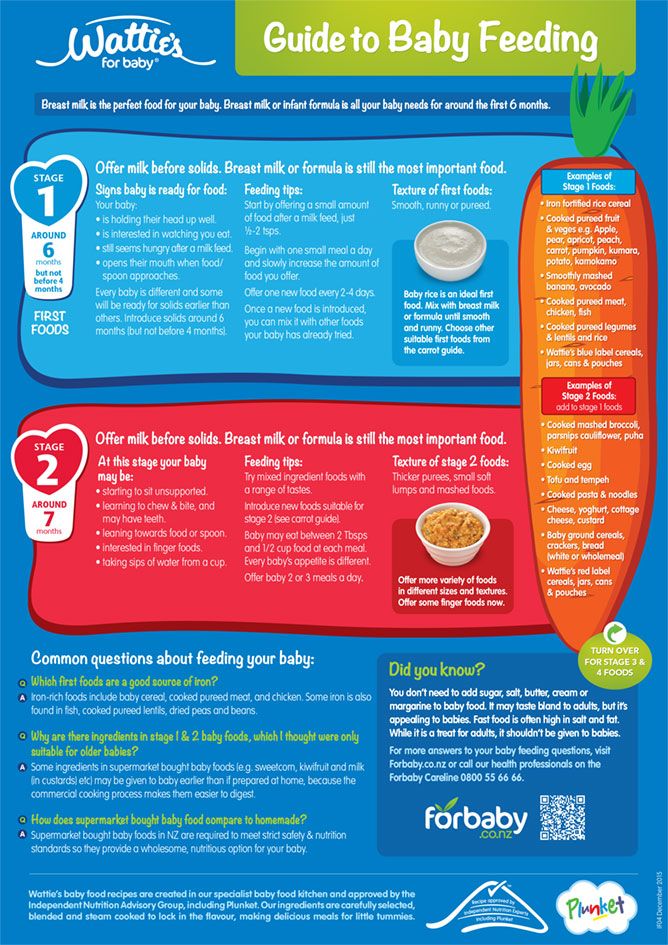
Some parents prefer baby-led weaning to spoon feeding, while others do a combination of both.
There's no right or wrong way. The most important thing is that your baby eats a wide variety of food and gets all the nutrients they need.
There's no more risk of choking when a baby feeds themselves than when they're fed with a spoon.
Find out more:
- help your baby enjoy new foods
- drinks and cups for babies and young children
- food allergies in babies and young children
- foods to avoid giving babies and young children
Feeding your baby: from 7 to 9 months
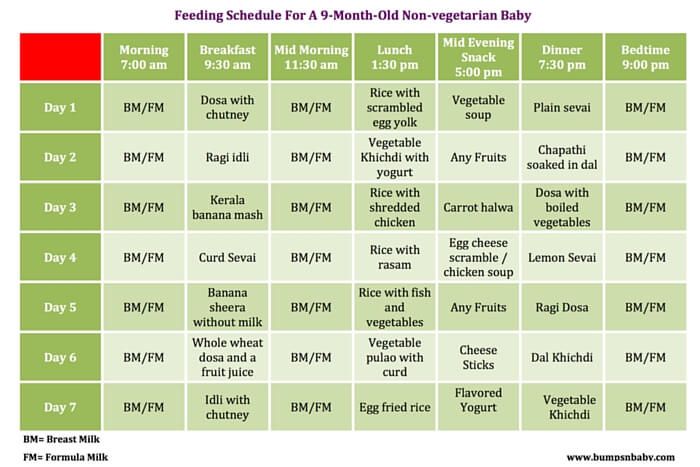
From about 7 months, your baby will gradually move towards eating 3 meals a day (breakfast, lunch and tea), in addition to their usual milk feeds, which may be around 4 a day (for example, on waking, after lunch, after tea and before bed).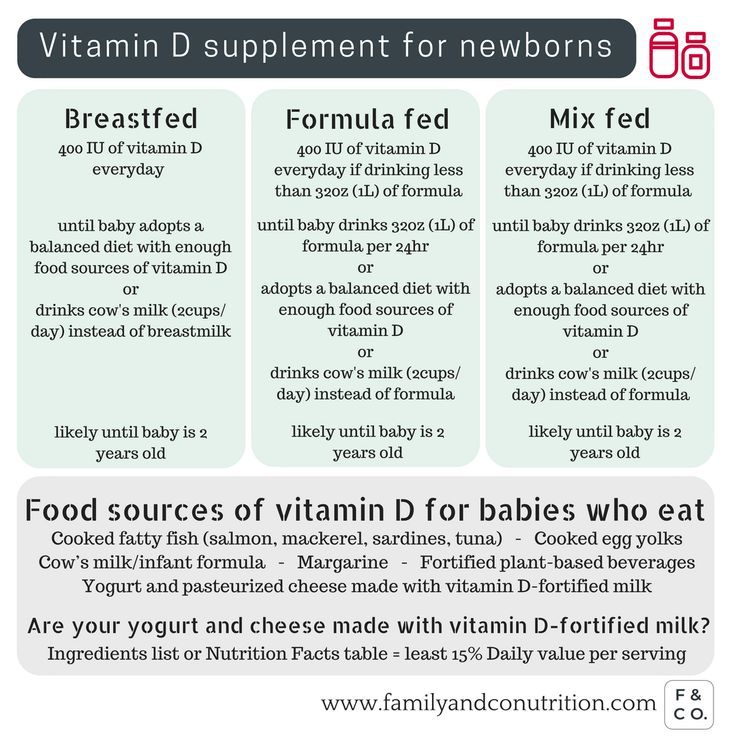
As your baby eats more solid foods, they may want less milk at each feed or even drop a milk feed altogether.
If you're breastfeeding, your baby will adapt their feeds according to how much food they're having.
As a guide, formula-fed babies may need around 600ml of milk a day.
Gradually increase the amount and variety of food your baby is offered to ensure they get the energy and nutrients they need.
Try to include food that contains iron, such as meat, fish, fortified breakfast cereals, dark green vegetables, beans and lentils, at each meal.
Your baby's diet should consist of a variety of the following:
- fruit and vegetables, including ones with bitter flavours, such as broccoli, cauliflower, spinach and cabbage
- potatoes, bread, rice, pasta and other starchy foods
- beans, pulses, fish, eggs, meat and other non-dairy sources of protein
- pasteurised full-fat dairy products, such as plain yoghurt and cheese (choose lower salt options)
As your baby becomes a more confident eater, remember to offer them more mashed, lumpy and finger foods.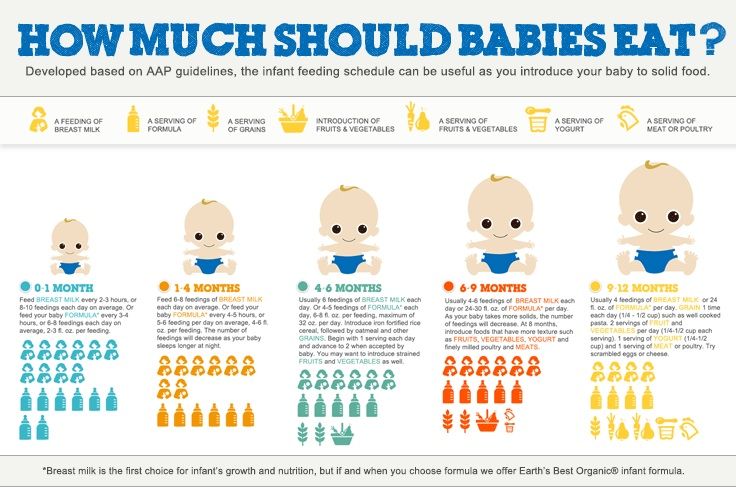
Providing finger foods as part of each meal helps encourage infants to feed themselves, develop hand and eye co-ordination, and learn to bite off, chew and swallow pieces of soft food.
Remember, babies do not need salt or sugar added to their food (or cooking water).
Feeding your baby: from 10 to 12 months
From about 10 months, your baby should now be having 3 meals a day (breakfast, lunch and tea), in addition to their usual milk feeds.
Around this age, your baby may have about 3 milk feeds a day (for instance, after breakfast, after lunch and before bed).
Breastfed babies will adapt their milk consumption as their food intake changes.
As a guide, babies fed infant formula will drink about 400ml daily.
Remember that formula-fed babies should take a vitamin D supplement if they're having less than 500ml of formula a day.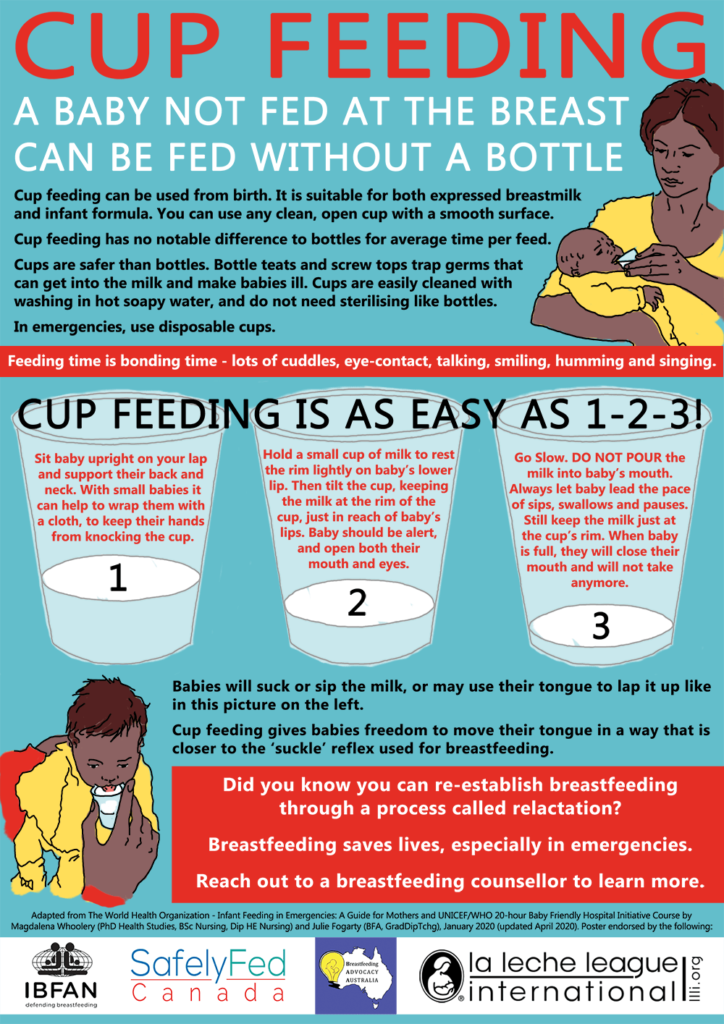
All breastfed babies should take a vitamin D supplement.
By now, your baby should be enjoying a wide range of tastes and textures.
They should be able to manage a wider range of finger foods, and be able to pick up small pieces of food and move them to their mouth. They'll use a cup with more confidence.
Lunches and teas can include a main course, and a fruit or unsweetened dairy-based dessert, to move eating patterns closer to those of children over 1 year.
As your baby grows, eating together as a family encourages them to develop good eating habits.
Remember, babies do not need salt or sugar added to their food (or cooking water).
Feeding your baby: from 12 months
From 12 months, your child will be eating 3 meals a day containing a variety of different foods, including:
- a minimum of 4 servings a day of starchy food, such as potatoes, bread and rice
- a minimum of 4 servings a day of fruit and vegetables
- a minimum of 350ml milk or 2 servings of dairy products (or alternatives)
- a minimum of 1 serving a day of protein from animal sources (meat, fish and eggs) or 2 from vegetable sources (dhal, beans, chickpeas and lentils)
Your child may also need 2 healthy snacks in between meals.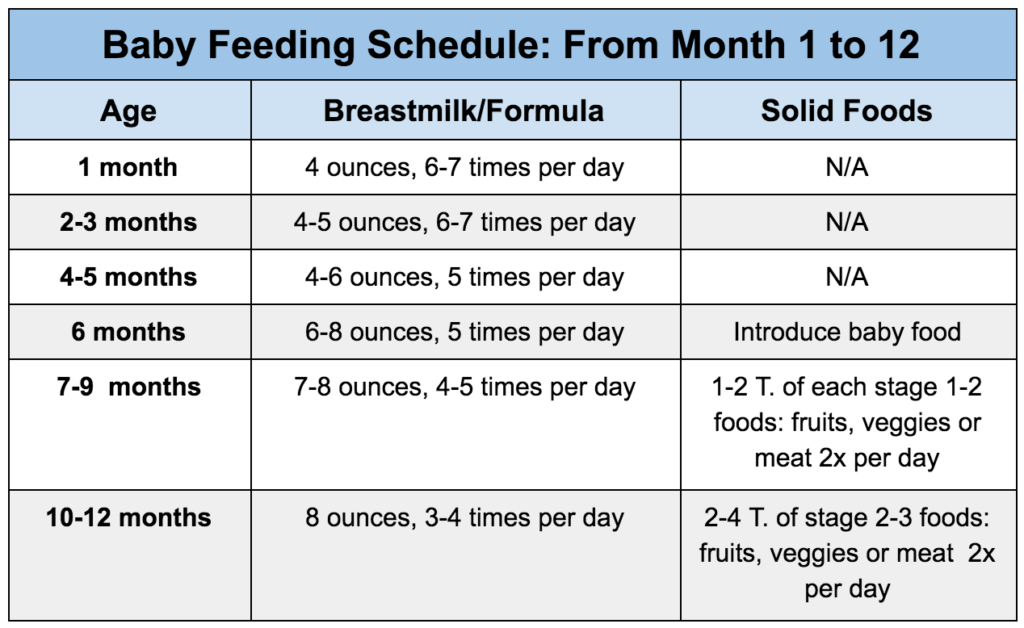
Go for things like:
- fresh fruits, such as apple, banana or small pieces of soft, ripe, peeled pear or peach
- cooked or raw vegetable, such as broccoli florets, carrot sticks or cucumber sticks
- pasteurised plain full-fat yoghurt
- sticks of cheese (choose a lower salt option)
- toast, pitta or chapatti fingers
- unsalted and unsweetened rice or corn cakes
The World Health Organization recommends that all babies are breastfed for up to 2 years or longer.
You can keep breastfeeding for as long as it suits you both, but your child will need less breast milk to make room for more foods.
Once your child is 12 months old, infant formula is not needed and toddler milks, growing-up milks and goodnight milks are also unnecessary.
Your baby can now drink whole cows' milk. Choose full-fat dairy products, as children under 2 years old need the vitamins and extra energy found in them.
From 2 years old, if they're a good eater and growing well, they can have semi-skimmed milk.
From 5 years old, 1% fat and skimmed milk is OK.
You can give your child unsweetened calcium-fortified milk alternatives, such as soya, oat or almond drinks, from the age of 1 as part of a healthy, balanced diet.
Children under 5 years old should not be given rice drinks because of the levels of arsenic in these products.
Find out more:
- what to feed young children
- foods to avoid giving babies and young children
- drinks and cups for babies and young children
- vitamins for children
Get Start4Life pregnancy and baby emails
For information and advice you can trust, sign up for weekly Start4Life pregnancy and baby emails.
What to eat while breastfeeding | Breastfeeding Diet
You know that breast milk is the best food for your baby. What about your own nutrition while breastfeeding? We asked the nutritionist a few questions about the nutrition of a nursing mother.
Share this information
Priya Tew, UK-based registered dietitian :
Priya is a nutritionist, M.D., multi-award winning member of the British Dietetic Association and the Health Professions Council. She has three children, and she breastfed each of them for up to 18 months. nine0003
During breastfeeding, there is no need to follow a special diet, the main thing is that your diet is balanced. It should include plenty of fruits and vegetables, whole grains such as oats, brown rice, various cereals, and breads labeled "whole grain", "wholemeal" or "wholemeal". These foods, along with potatoes, pasta, and couscous, are high in starch, an important source of energy.
In addition, you need lean proteins found in chicken, eggs, legumes, lentils, fish, and lean beef, as well as healthy fats found in olive oil, nuts, seeds, avocados, and fatty fish such as salmon and mackerel. Oily fish is very good for your health and development of your baby, but you should not eat more than two servings per week (about 140 g), as it may contain harmful impurities. nine0014 1
Should I take vitamins while breastfeeding?
The most important is vitamin D. It is essential for healthy bones, you and your baby. We get most of this vitamin from the sun. If you live in a region with insufficient solar activity, especially in winter, your body may lack it. In this case, the doctor may advise taking vitamin D supplements. 2
You also need to get enough calcium, as it is excreted from the body during breastfeeding. nine0014 3 Try to eat four servings of foods rich in this mineral a day. These can be dairy products such as milk, yogurt, and cheese, or non-dairy products such as nuts, tofu, sesame seeds, and leafy vegetables. One serving may consist of, for example, half a cup of green vegetables or a small piece of cheese (50 g).
One serving may consist of, for example, half a cup of green vegetables or a small piece of cheese (50 g).
What foods should I avoid while breastfeeding?
The good news is that you can eat almost anything while breastfeeding. Only the consumption of oily fish should be limited. In small quantities, even caffeine is acceptable - more on this below. nine0003
If you are not allergic to peanuts, there is no reason to deny yourself products that contain peanuts. Recent studies show that if you eat peanuts while breastfeeding and gradually introduce them into your baby's diet during the first year, your baby will be less likely to become allergic to them in the future. 4
Are extra calories needed while breastfeeding?
Breastfeeding mothers need about 500 more calories a day. nine0014 5 But every mother is unique and your energy needs will change throughout your breastfeeding period. The number of calories you need depends on your baby's age, appetite, height, and weight, as well as your body mass index (BMI), your activity, and factors such as whether you are exclusively breastfeeding or not, and whether you are breastfeeding twins or multiple babies.
Can I go on a diet while breastfeeding?
Trying to lose weight while breastfeeding is not a good idea because you need to get enough nutrients for you and your baby. The fat accumulated during pregnancy is used to produce milk, so breastfeeding in itself will help you shed those extra pounds. nine0003
If your weight changes by more than 1 kg per week, check if you are eating a healthy and balanced diet and adjust if necessary. You can also ask your doctor for advice.
How can I find time to prepare healthy meals?
Having devoted yourself to feeding a child, you can forget about your own nutrition. However, it is important to ensure that your diet does not consist only of sweets and cookies. Of course, sweet snacks are easy and quick, but they do not bring any benefit to your body. nine0003
Opt for quick yet nutritious meals like scrambled eggs with spinach or fried chicken with brown rice. Oatmeal is great for breakfast, as it provides a slow release of energy from grains and soluble dietary fiber, which is what you need to restore strength in the morning after a night of breastfeeding.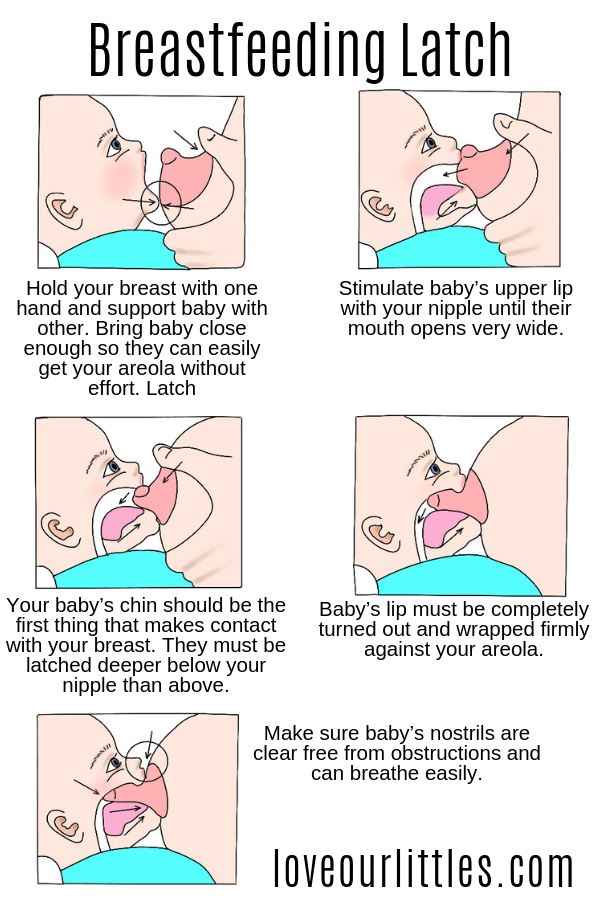
Store pre-cut fruits and vegetables in the refrigerator for light snacks, or carry unsalted nuts in your bag. It's much easier than peeling tangerines with one hand while holding a baby with the other. nine0003
Should I drink more water while breastfeeding?
Breastfeeding can make you thirsty, so it's important to drink enough water. A person needs six to eight glasses of fluid a day, and even more if breastfeeding. 6 Make it a habit to drink a glass of water, milk or fruit juice without sugar every time you feed your baby.
I love coffee. Do I need to quit caffeine?
Coffee, like everything you eat or drink, passes into your breast milk, so it is advisable to limit your intake while breastfeeding. Legal coffee limits vary by country, but the average recommendation is not to exceed 200-300 mg of caffeine per day (300 mg is equivalent to two cups of filtered coffee or four cups of tea). Talk to your doctor about the acceptable amount of coffee consumption for you. Also, don't forget that caffeine is found in cola and energy drinks, and a small bar of dark chocolate can contain up to 50 mg. nine0014 7
Also, don't forget that caffeine is found in cola and energy drinks, and a small bar of dark chocolate can contain up to 50 mg. nine0014 7
If I eat a varied diet, will my baby be less picky?
Breast milk has the flavor of everything you eat. 8 Therefore, if you eat a variety of foods during breastfeeding, giving your baby different tastes to try, he may like them in the future.
If you like spicy and spicy foods, there is no reason to refuse them while breastfeeding. When my first child was born, I ate a lot of spicy food. When my daughter was two years old, we went to Sri Lanka, coincidence or not, but she ate absolutely everything. nine0003
Can something in my diet not be suitable for a child?
At an early age, babies often suffer from colic or are picky eaters, so mothers naturally wonder if their diet is causing this. Most likely no. Studies show that the proportion of children who are allergic to any component of breast milk is only slightly more than 1%.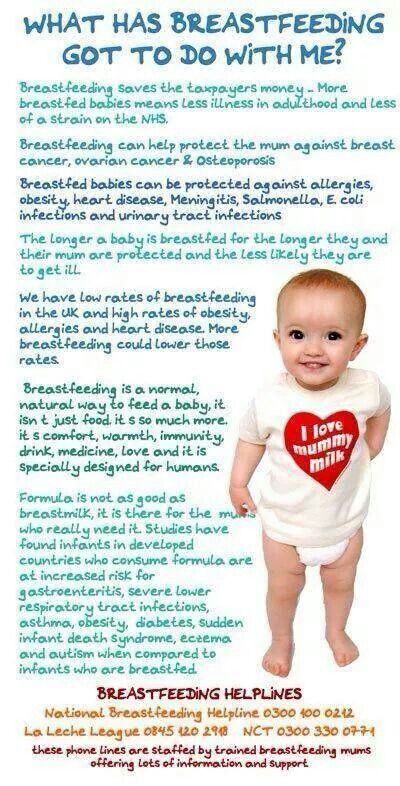 9 Cow's milk, eggs, corn, and soy proteins in moms' diets are much more likely to cause allergic reactions than spicy foods, hot sauces, or cruciferous vegetables, which moms usually worry about. nine0003
9 Cow's milk, eggs, corn, and soy proteins in moms' diets are much more likely to cause allergic reactions than spicy foods, hot sauces, or cruciferous vegetables, which moms usually worry about. nine0003
If your baby is allergic to substances in your milk, it can cause profuse vomiting, rash, bloody stools, or prolonged constipation. If your baby has an intolerance to any food, you will notice symptoms such as moodiness and crying after feeding, burping, diarrhea, or the baby will press his knees to his chest. Contact your doctor if something is bothering you. He may suggest eliminating certain foods for a couple of weeks, and then see if the child's behavior changes after eating them again. nine0003
You can also keep a food diary: write down everything you eat and drink, as well as your child's symptoms, and you may notice some patterns. However, before cutting out any foods, such as dairy, always check with your doctor, as it's important to know that you're getting the nutrients you need from other sources. Depending on where you live, you will be referred to a nutritionist or other specialist.
Depending on where you live, you will be referred to a nutritionist or other specialist.
Does a vegetarian diet affect breast milk? nine0018
If you are getting enough calories and all the nutrients your body needs (carbohydrates, proteins, fats, vitamins and minerals), then you have nothing to worry about. A vegetarian or vegan diet requires plenty of vitamin B12, vitamin D, calcium, and omega-3 fatty acids while breastfeeding, so opt for foods and supplements that provide you with these essential nutrients.
If you are on a vegetarian, vegan, macrobiotic, or other special diet, you may need additional medical advice to make sure you are getting all the nutrients your baby needs. nine0003
Literature
1 National Health Service (NHS) [Internet]. Burnley, UK: Department of Health; 2018. Should pregnant and breastfeeding women avoid some types of fish?; 2015 Jul 06 [cited 2018 Apr 12]; Available from: https://www.nhs.uk/chq/Pages/should-pregnant-and-breastfeeding-women-avoid-some-types-of-fish.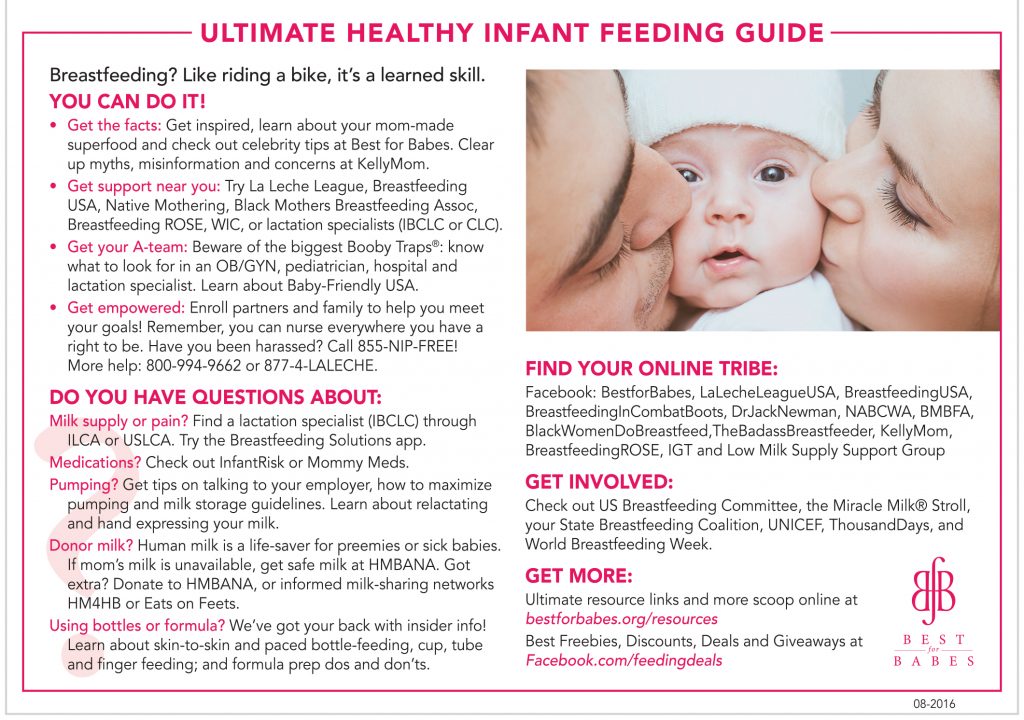 aspx - National Health Service (NHS) [Internet]. Burnley, UK: Department of Health; 2018. "Should a pregnant and lactating woman refrain from eating certain types of fish?"; July 6, 2015 [cited April 12, 2018]; See article on site https://www.nhs.uk/chq/Pages/should-pregnant-and-breastfeeding-women-avoid-some-types-of-fish.aspx
aspx - National Health Service (NHS) [Internet]. Burnley, UK: Department of Health; 2018. "Should a pregnant and lactating woman refrain from eating certain types of fish?"; July 6, 2015 [cited April 12, 2018]; See article on site https://www.nhs.uk/chq/Pages/should-pregnant-and-breastfeeding-women-avoid-some-types-of-fish.aspx
2 Oberhelman SS et al. Maternal vitamin D supplementation to improve the vitamin D status of breast-fed infants: a randomized controlled trial. Mayo Clin Proc. 2013;88(12):1378–1387. - Oberhelman S.S. et al., Introduction of Vitamin D to the Diet of Nursing Mothers to Increase Vitamin D in children: a randomized controlled trial. Mayo Klin Prok. 2013;88(12):1378–1387. : effects on the mother and the fetus. Am J Obstet Gynecol. 2006;194(4):937-945. - Thomas M., Weisman S. M., "Calcium supplementation during pregnancy and lactation: effects on the mother and on the fetus". Am J Obstet Ginekol (American Journal of Obstetrics and Gynecology). 2006;194(4):937-945.
Am J Obstet Ginekol (American Journal of Obstetrics and Gynecology). 2006;194(4):937-945.
4 Pitt et al Reduced risk of peanut sensitization following exposure through breast-feeding and early peanut introduction. J Allergy Clinic Immunol. 2018;141(2):620-625. e 1 - Pitt et al., "Reducing the Risk of Peanut Allergy by Introducing Peanuts into the Breastfeeding Mother's Diet and as a Baby's First Food." nine0095 G Allergy Clean Immunol. 2018;141(2):620-625.e1
5 Dewey KG. Energy and protein requirements during lactation. Annu Rev Nutr. 1997 Jul;17(1):19-36. - Dewey K. J., "Energy and Protein Requirements During Lactation". Anna Rev Nutr . 1997 Jul;17(1):19-36.
6 Food Standards Agency (FSA) [Internet]. London, UK: Crown copyright 2002.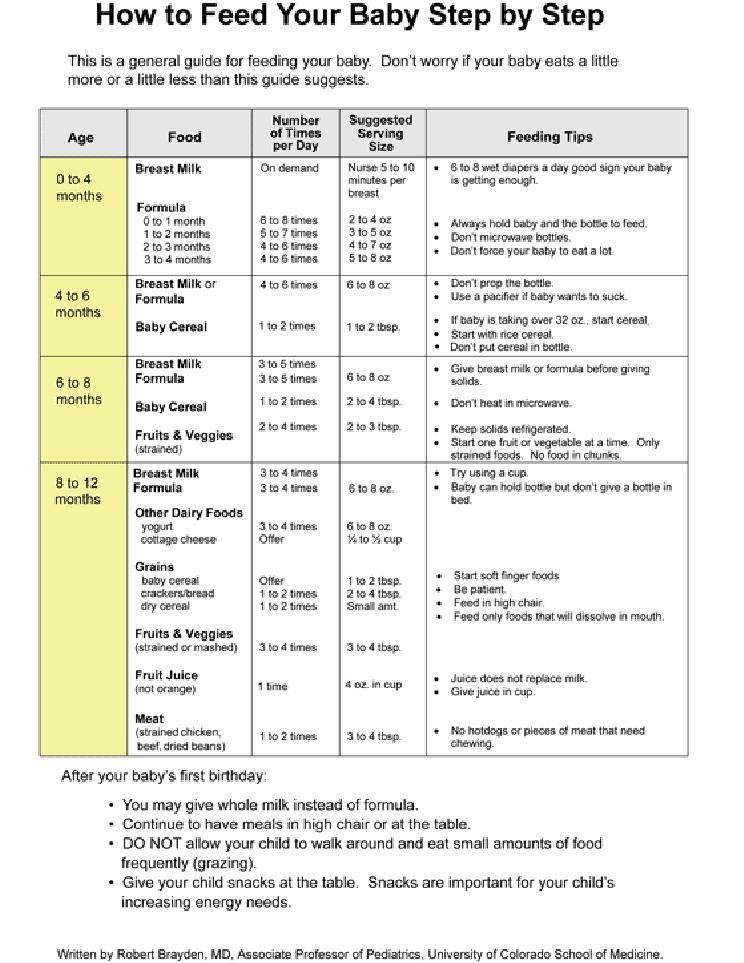 Eating for breastfeeding; [cited 2018 Apr 13]; Available from: https://www.food.gov.uk - Food Standards Agency (FSA) [Internet]. London, UK: State Copyright 2002. "Eat to feed" [cited April 13, 2018]. See article on https://www.food.gov.uk
Eating for breastfeeding; [cited 2018 Apr 13]; Available from: https://www.food.gov.uk - Food Standards Agency (FSA) [Internet]. London, UK: State Copyright 2002. "Eat to feed" [cited April 13, 2018]. See article on https://www.food.gov.uk
7 National Health Service (NHS) [Internet]. Burnley, UK: Department of Health; 2018. Breastfeeding and diet; 2016 Jan 29 [cited 2018 Apr 12]; Available from: https://www.nhs.uk/conditions/pregnancy-and-baby/breastfeeding-diet - National Health Service (NHS) [Internet]. nine0095 Burnley, UK: Department of Health 2018. Breastfeeding and Diet; 29 January 2016 [cited 12 April 2018] See article at https://www.nhs.uk/conditions/pregnancy -and-baby/breastfeeding-diet
8 Mennella JA et al. A. et al., Prenatal and postnatal recognition of odors in children. Pediatrix (Pediatrics). 2001;107(6):e88.
9 Academy of Breastfeeding Medicine. ABM clinical protocol# 24: allergic proctocolitis in the exclusively breastfed infant.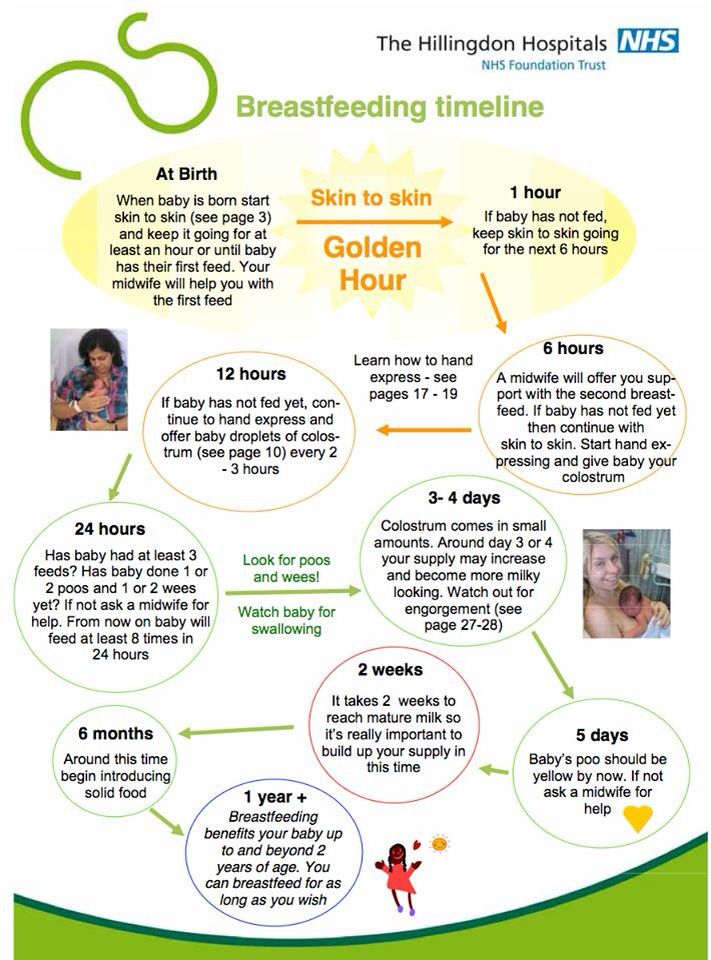 Breastfeed Med . 2011;6(6). - Academy of Breastfeeding Medicine. "AVM Clinical Protocol #24: Allergic Proctocolitis in an Exclusively Breastfed Child". Brestfeed Med (Breastfeeding Medicine). 2011;6(6). nine0095
Breastfeed Med . 2011;6(6). - Academy of Breastfeeding Medicine. "AVM Clinical Protocol #24: Allergic Proctocolitis in an Exclusively Breastfed Child". Brestfeed Med (Breastfeeding Medicine). 2011;6(6). nine0095
Feeding for cow's milk protein allergy
- Nestlé Health Science
- health care
- Feeding with CMPA
Feeding and treatment of CMPA
The appearance of allergy symptoms in an infant always causes fear in parents. The first step is to consult a doctor who will conduct an examination, make the correct diagnosis and prescribe competent treatment. With the right approach, most symptoms will disappear within 2-4 weeks. nine0003
Important! Do not experiment with a diet that excludes cow's milk protein without the advice and direction of a doctor.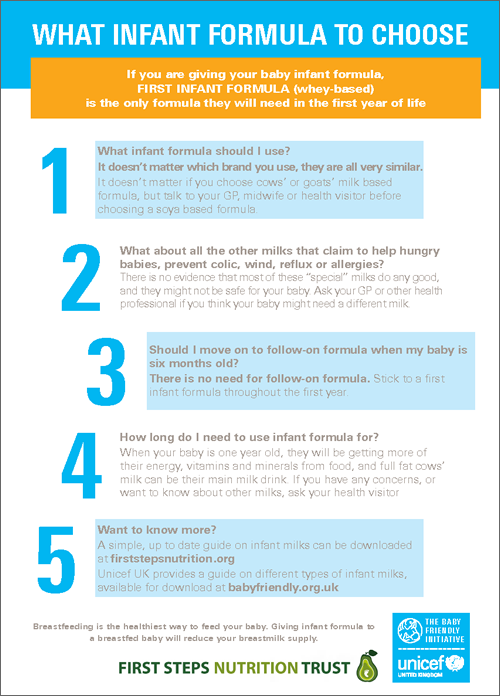
Breastfeeding is the best nutritional option for you and your baby. Even if your baby has been diagnosed with CMPA, breastfeeding should continue. Based on the severity of the symptoms and the presence of other types of food allergies in the child, the doctor will help determine the most appropriate diet for your child to quickly resolve the symptoms of the allergy. nine0003
Continue breastfeeding
A diagnosis of CMPA should not affect breastfeeding. Breastfeeding is the best nutritional option for your baby. Breast milk contains all the nutrients your baby especially needs during the first 6 months and continues to be beneficial for a long time to come. In addition to nutritional properties, breast milk contains antibodies, leukocytes and immune complexes, which together form the baby's immunity. In rare cases where the baby's immune system reacts to cow's milk proteins in breast milk, your doctor may recommend that you start a diet eliminating cow's milk proteins entirely (remember that a dairy-free diet may not be sufficient, as all traces of cow's milk must be eliminated) . nine0003
nine0003
Early start: The sooner you start breastfeeding, the better. According to doctors, starting breastfeeding within 1 hour of birth ensures that your baby receives first milk (colostrum) and the protective factors it contains as soon as possible.
Emotional Benefit: Breastfeeding is an important factor in establishing and maintaining a strong emotional bond with your baby.
Long-term health benefits: Breastfeeding will also help develop your baby's immune system and thus protect your baby's health in the long term.
Protection for you and your baby: Studies have shown that breastfeeding reduces the risk of further infections in children, digestive diseases, diabetes, obesity and even leukemia. Breastfeeding is also good for you! Mothers who breastfeed have a reduced risk of developing diabetes, as well as breast and ovarian cancer. nine0003
Importance and benefits of breastfeeding
The sooner the better
- Breastfeeding during the first hour of birth ensures that the baby receives its first milk called colostrum
- Exclusive breastfeeding recommended for first 6 months
Protective role for you and your child
- Breast milk is rich in protective factors that promote healthy growth and development in babies and reduce the risk of developing diseases later on.
- Mothers who breastfeed have a lower risk of developing diabetes and developing breast and ovarian cancer
Emotional Benefits
- You and your child develop and maintain a strong emotional bond. nine0225
What type of food is best for my child?
The only way to eliminate symptoms is to eliminate cow's milk proteins from the child's diet.
Important! Do not experiment with a diet that excludes cow's milk protein without the advice and direction of a doctor.
If breastfeeding is not possible or supplemented with infant formula, your doctor will help you select an appropriate infant formula that does not contain cow's milk proteins. These infant formulas are formulated with children in mind and contain all the necessary nutrients to support growth and development. nine0003
These specialized infant formulas can be based on:
- cow's milk processed in a certain way so that the proteins are no longer recognized by the baby's immune system and therefore do not cause an allergic reaction
- amino acids
The table below describes the differences between the two types of infant formula.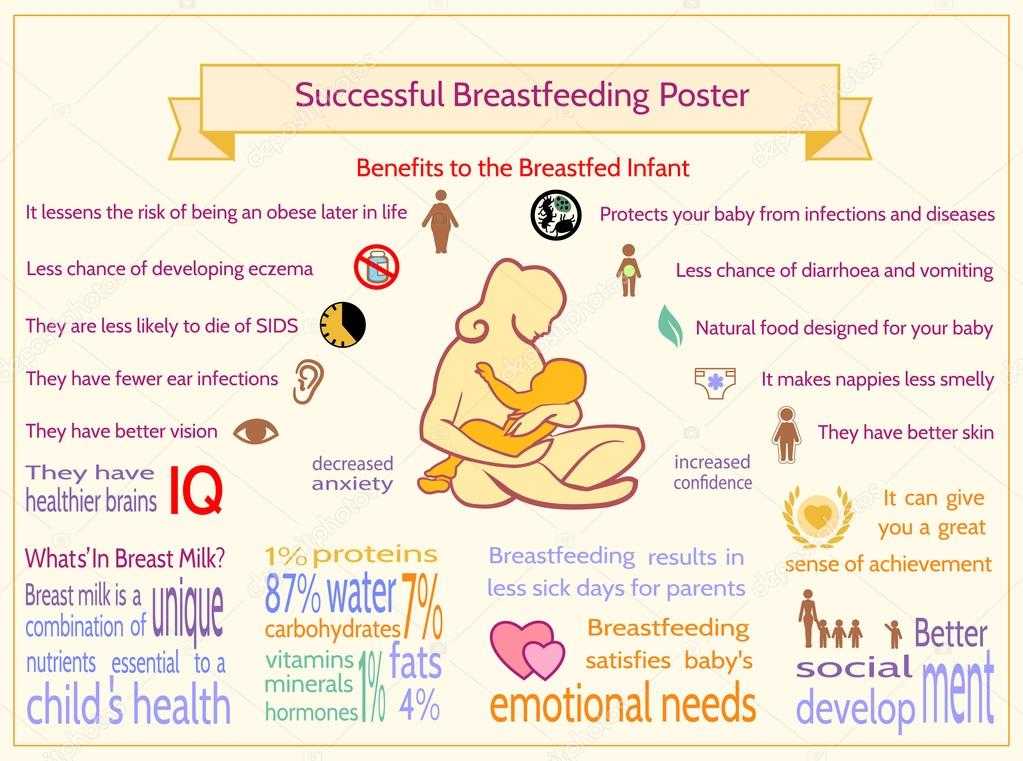
| SOGSB | COA | |
| What is it? | WGHB stands for "Whey Protein Hydrolysate Blend". The proteins in cow's milk that cause allergic reactions in a baby are severely broken down (hydrolyzed). | COA stands for "amino acid blend". This mixture does not contain any cow's milk proteins. |
| What does it consist of? | Cow's milk proteins have been broken down into smaller particles, which means they can no longer be recognized by the baby's immune system. Mixtures contain the macro- and micronutrients necessary for the child. nine0317 | For severe allergies, an amino acid mixture is used. This mixture does not contain any cow's milk proteins. The mixture is also enriched with all the necessary elements to support healthy growth and development. |
When and how to introduce complementary foods
At 6 months of age, breastfeeding (or special infant formula) is no longer sufficient to fully support a child's growth and development, and additional foods must be introduced into the diet. But throughout this time, breastfeeding (or special infant formula) is still the main source of nutrition for the baby. nine0003
But throughout this time, breastfeeding (or special infant formula) is still the main source of nutrition for the baby. nine0003
It is important to introduce complementary foods on time. The reflex responsible for moving solid foods in the mouth and swallowing them usually develops between 4 and 7 months of age. If you start solid foods too early, the baby will not be ready for it. Similarly, if you start too late, your child may not get all the nutritional support he or she needs, which increases the child's risk of developing essential vitamin and mineral deficiencies and stunting. Along with the nutritional benefits, introducing complementary foods will also provide sensory stimulation and improve your baby's motor skills. nine0003
IMPORTANT NOTE: : It is possible to continue breastfeeding if the infant is allergic to cow's milk protein. To do this, the mother needs a special diet with the exclusion of all sources of cow's milk protein. Only if these measures do not bring the desired effect, the doctor recommends the use of a special therapeutic mixture intended for children from 0 to 1 year old.