Non dairy baby food
Meal Plans & Recipe Ideas for Your Dairy-Free Baby or Tot
Some babies and toddlers are not able to tolerate dairy, whether from a lactose intolerance or a cow’s milk protein allergy.1 Knowing what foods and beverages to feed your little one while avoiding dairy can help make sure they are getting the nutrients needed for growth and development.
When do babies need to avoid dairy?Breastfed Baby
If your breastfed baby has been diagnosed with a cow’s milk protein allergy or lactose intolerance, you can likely continue to breastfeed as long as you eliminate sources of dairy from your own diet.2,3 Continue to work with your or your child’s health care provider as you eliminate sources of dairy.
Be sure to always read all foods labels to see if there are any dairy ingredients in the product you purchase.
Read more:
Meal Plan & Tips to Eat Dairy Free while Breastfeeding
Is Your Baby Reacting to Something in your Milk?
Formula Fed Baby
If your formula fed baby has been diagnosed with a cow’s milk protein allergy or sensitivity to lactose, you will likely need to choose either a low lactose or lactose-free formula, or a formula that does not contain intact cow’s milk protein.4
Always speak with your child’s health care provider before switching formulas.
Read more:
Does Your Baby Need a Sensitive Formula?
Does my Baby Need a Hypoallergenic Formula?
Once your baby begins to eat solids, look at labels carefully to avoid dairy ingredients. Read on for information, tips, and meal ideas.
For more information on lactose intolerance versus a cow’s milk protein allergy, check out this article:
Does my Baby or Toddler have a Milk Allergy or a Lactose Intolerance?
Making sure your child gets the right nutrition while eliminating dairyDairy foods provide several important nutrients, including protein, calcium, and vitamin D (which is often fortified, or added to, dairy products). 5 When eliminating dairy, it is necessary to incorporate other food sources (in the texture your baby is ready for) that are rich in these particular nutrients.6
5 When eliminating dairy, it is necessary to incorporate other food sources (in the texture your baby is ready for) that are rich in these particular nutrients.6
Food sources of calcium: Fortified plant-based milk alternatives, fortified orange juice, canned sardines and salmon with bones, fortified dairy alternatives such as a non-dairy yogurt, tofu, soybeans, spinach, kale.8
Read more: Why Does Calcium Matter for Babies, Tots, and Mama
Food sources of vitamin D: Salmon, fortified plant-based milk alternatives, fortified cereals, eggs, canned light tuna, portabella mushrooms, and sunlight.9
Read more: Why Does Vitamin D Matter for Babies, Tots, and Mama
Food sources of protein: Fish, poultry, meat, beans, legumes, peas, nuts, seeds, tofu, eggs, whole grains.
Read more: Protein: Getting Enough and the Best Sources
Offer a wide variety of dairy-free foods to your childIt’s important to know that there are plenty of other foods that do not contain dairy. Offer these foods often as long as your child is not allergic to them. All whole fruits, vegetables, whole grains, legumes, beans, nuts, seeds, poultry, fish, and eggs are dairy free. Be sure to feed your child a wide variety of these foods to help meet their nutrient needs.
Offer these foods often as long as your child is not allergic to them. All whole fruits, vegetables, whole grains, legumes, beans, nuts, seeds, poultry, fish, and eggs are dairy free. Be sure to feed your child a wide variety of these foods to help meet their nutrient needs.
Non-dairy alternatives can be used for a child with a lactose intolerance or allergy, such as plant-based milk alternatives and plant-based yogurt alternatives. But it’s important to note that not all of these products have the same nutrients as their dairy equivalent.1
If you do choose a plant-based milk alternative, such as almondmilk or oatmilk, be sure the product is fortified with calcium and vitamin D.
Note that plant-based yogurt alternatives often have more added sugar and less protein than regular yogurt. Read nutrition fact labels and ingredient lists to ensure you’re providing your little one with foods that best meet their nutritional needs.
*While a plant-based milk alternative can be used in small amounts in baked or cooked foods, or plant-based yogurt alternative can be provided as a snack or part of a meal, babies under the age of 12 months should not be given cow’s milk nor a plant-based milk alternative to drink by the cup-full.11
These drinks do not contain all the nutrition your baby needs, and adding them in by the cup may take up valuable space in your baby’s tummy – edging out more nutritious foods, formula, and/or breastmilk.
Read more: What Type of Milk Should My Toddler Drink?
Reach out to your child’s healthcare providerIf you suspect that your child has lactose intolerance or a cow’s milk protein allergy, call their healthcare provider immediately for further support.
Wondering what might be the best choice for your baby or tot? Reach out to our team of registered dietitians and lactation consultants for free! They’re here to help on our free to live chat from Monday – Friday 8am - 6pm (EST).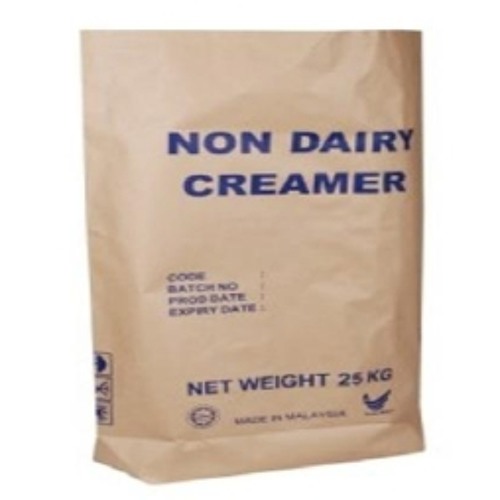 Chat Now!
Chat Now!
Pro Tip:
Some babies and toddlers will react to dairy ingredients that are “hidden” and not so obvious.10
Hidden dairy may be found in foods like breads, cereals, crackers, pancakes, waffles, soups, sauces, toppings, dressings, and deli meats. It’s important to read labels and avoid any foods that list “contains milk or milk ingredient.”10
The below meal plan, snack, and recipe ideas will help you choose the right foods for your baby when progressing from mostly single purees to more advanced textures and finger foods, while also excluding dairy.
Be sure to check all labels for both obvious and hidden sources of dairy.
Breakfast
Option 1: Scrambled eggs, clementine
Option 2: Dairy free yogurt such as soy, coconut, or almond, with sliced berries
Option 3: Strawberry Quinoa Cereal for Baby
Option 4: Whole grain French toast fingers with nut butter* and 100% fruit spread
Option 5: Banana pancakes (combine 1 ripe banana, 1 egg and 2 tbsp.
 whole wheat flour. Cook 3 minutes on each side over medium heat)
whole wheat flour. Cook 3 minutes on each side over medium heat)
Lunch
Option 1: Whole grain tortilla strips with mashed avocado dip
Option 2: Tuna sandwich cut into quarters, side of sliced peaches
Option 3: Chickpeas with soft cooked carrots
Option 4: Cubed and roasted butternut squash, with turkey slivers
Option 5: Mini Sweet Potato Chicken Meatballs with Cauliflower Rice and Steamed Broccoli
Dinner
Option 1: Black beans with soft cooked peppers
Option 2: Whole grain pasta with ground turkey, marinara, and roasted veggies
Option 3: Baked fish fingers with cubed and roasted sweet potato
Option 4: Mild Curry Chicken & Veggies with Brown Rice
Option 5: Lean hamburger cut into pieces with baked zucchini fries
Snacks:
Option 1: Soft cooked veggies with hummus
Option 2: Warm Peach Chunks with Nutmeg
Option 3: Hard-boiled egg, diced
Option 4: Fruited dairy free yogurt such as coconut, soy, or almond
Option 5: Applesauce mixed with small amount of nut* or seed butter
*Speak with your baby’s pediatrician before introducing allergenic foods
Let's Chat!We know parenting often means sleepless nights, stressful days, and countless questions and confusion, and we want to support you in your feeding journey and beyond.
Our Happy Baby Experts are a team of lactation consultants and registered dietitians certified in infant and maternal nutrition – and they’re all moms, too, which means they’ve been there and seen that. They’re here to help on our free, live chat platform Monday - Friday 8am - 6pm (Et).Chat Now!
Read more about the experts that help write our content!
For more on this topic, check out the following articles:Does my Child Have a Food Allergy or a Food Intolerance?
Guidance When Raising a Child with Food Allergies
Introducing Major Food Allergens to your Infant
Our meal plans offer recipe and meal suggestions for your child. They are not designed to replace your doctor’s recommendations, nor do they take into account special nutritional needs, including allergies and intolerances, other than lactose intolerance and a cow’s milk protein allergy. The meal plans suggest serving sizes that may or may not be appropriate for your child. Please consult your doctor to determine what is best for your child.
Please consult your doctor to determine what is best for your child.
Sources
Your guide to dairy free baby food for cow's milk protein allergy
It is estimated that 1 in 14 children under the age of three will have some sort of food allergy, with the most common allergies to milk, eggs, peanuts, tree nuts, soya, fish and wheat.
Did you know that around 2% of babies have an allergy to milk or Cow’s Milk Protein Allergy (CMPA)?[1]
It’s the most common nutritional issue that babies have and it’s on the rise. Research hasn’t yet found a reason why, but as a paediatric dietitian, I am coming across more and more babies and children with CMPA.
If you would like a PDF version of this blog delivered directly to your inbox, pop your details below.
What is CMPA?Cow’s milk naturally contains a variety of nutrients, including protein. The proteins found in cow’s milk are called casein and whey. When some babies consume cow’s milk, their bodies react to these proteins and trigger an immune response releasing antibodies.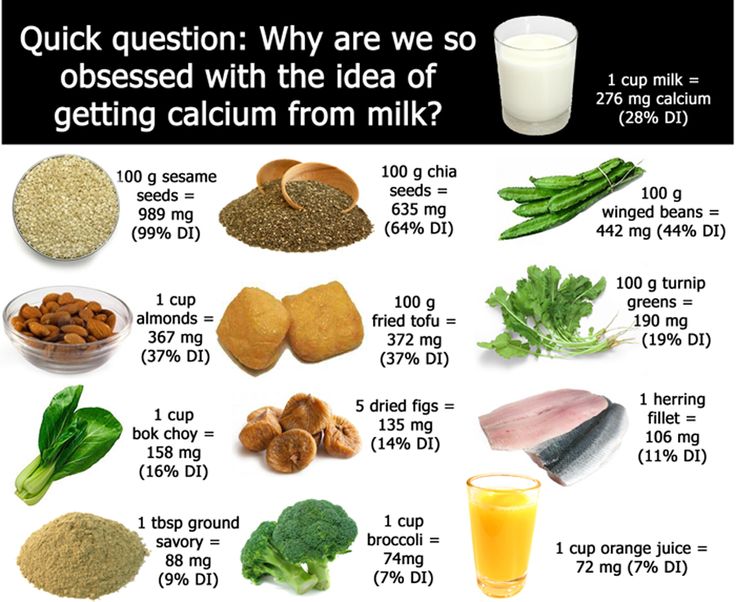 These allergic reactions can happen immediately after eating any cows milk products – called an IgE mediated response, or can be delayed – called a non-IgE mediated response.
These allergic reactions can happen immediately after eating any cows milk products – called an IgE mediated response, or can be delayed – called a non-IgE mediated response.
Whatever type of milk allergy your baby has it is very important that they follow a completely dairy free diet. This doesn’t just mean avoiding cows milk but any foods that contain any cows milk products, such as butter, yoghurt, cheese, custard and ice-cream.
What about goats milk?As the proteins in cow’s milk are quite similar to the proteins of other mammalian milks, your child will also need to avoid milk from other animals too like goat’s milk, sheep milk and buffalo milk, which includes cheeses made from these milks.
What about traces of milk in manufactured foods?Milk or milk products are often used as an ingredient in lots of processed foods, like bread or flavourings, so it’s really important to check all food labels on any food products. By law, if food contains any products in any form, they have to declare it prominently on the label. For example, many manufacturers display allergens in bold so it is easy to spot.
By law, if food contains any products in any form, they have to declare it prominently on the label. For example, many manufacturers display allergens in bold so it is easy to spot.
Until your dietitian tells you otherwise, you should avoid all traces of milk in foods including where the label says ‘may contain’ or ‘traces of milk’.
What are the symptoms of CMPA?Symptoms of an allergic reaction can be immediate (IgE) or delayed (non-IgE). The difference between an IgE and non-IgE reaction is the way that the reaction takes place using different parts of the immune system. Immediate means that they come on typically within 30 minutes after eating a food containing the allergen but they can take up to 2 hours. Delayed symptoms can take anywhere from two hours to several days later to show! Symptoms can include (but not limited to):
-
Eczema
-
Red skin
-
Hives
-
Swelling of the lips, tongue, mouth or body
-
Difficulty breathing
-
An itchy, runny nose
-
Tummy troubles such as vomiting, constipation or diarrhoea
-
Reflux
-
Tummy pain
-
Poor growth
-
Asthma
-
Anaphylaxis (in extreme cases)
If your baby shows any of the symptoms of CMPA, it is really important that they are seen by a healthcare professional such as your GP as soon as possible. If it’s an IgE reaction you will be referred to a paediatrician in your local hospital to confirm the diagnosis.
If it’s an IgE reaction you will be referred to a paediatrician in your local hospital to confirm the diagnosis.
IgE allergies are diagnosed in a hospital under the guidance of a Paediatrician. Your child may have skin prick tests where a small amount of the suspected allergen food is put on your baby’s skin. The surface of the skin is then scratched and the size of the ‘wheel’ it creates is measured.
They are notoriously inaccurate in babies under 1 where skin is sensitive and false positives are common.
Alternatively, a blood sample can be taken and sent off for further analysis, the results take several days to come back.
A very detailed allergen focussed history will be taken from you so it’s good to have a food diary and symptom record if possible. It is this coupled with the tests that will confirm the diagnosis.
Delayed onset reactionsIf it’s a non-IgE reaction your GP will take an allergen focussed history and may suggest an ‘exclusion diet and challenge. ’ Essentially this is a 2-4 week trial of a milk free diet to see if this improves their symptoms.
’ Essentially this is a 2-4 week trial of a milk free diet to see if this improves their symptoms.
If you are breastfeeding and you think that your little one is reacting to cow’s milk through your breastmilk, this will involve you avoiding dairy foods in your diet. If your baby is weaning, they will need to avoid cow’s milk too.
Your GP should organise a referral to a Registered Dietitian too as the diagnosis is only confirmed when your baby is ‘challenged’ i.e. when the food is reintroduced producing a return of their symptoms.
This can be carried out at home for most non-IgE babies, and best practice is to do this alongside a Registered Dietitian. You should be aware that access to an NHS dietitian can be scarce in some areas and an appointment may not be offered in time.
If this is the case, you are welcome to book an appointment with one of my fully qualified paediatric dietitians on the team. The link to book is here.
I’ve seen other tests I can buy online. Are these any good?
Are these any good? There are lots of alternative tests marketed to diagnose allergies such as IgG, vega testing, iridology, hair analysis, kinesiology or cytotoxic testing. These are widely available online and the costs can vary.
However, none have scientific evidence for their use and can’t diagnose an allergy or intolerance.
The only evidence based methods of diagnoses are the ones outlined above and all others should be avoided.
My baby reacted to milk challenges – what happens next?Once the diagnosis is confirmed, you will be advised to continue following the dairy free diet. You must be immediately referred to a Registered Dietitian with paediatric expertise if you haven’t already because by cutting out milk you are cutting out a key food group from your growing baby which if not appropriately replaced can result in poor growth and development and nutritional deficiencies, leading to health problems. It is essential that those missing nutrients are replaced with other foods in your little one’s diet.
You might have heard people use the phrase ‘cow’s milk protein intolerance’, however, this doesn’t actually exist. It’s a term that healthcare professionals have previously used to describe delayed onset or non-IgE milk allergy, but it sometimes is still used today.
What about lactose intolerance, is that different?This is not an allergy to dairy foods and is a separate condition. Lactose is the sugar that is found naturally in milk. Children with lactose intolerance have trouble breaking down the lactose in foods because they are missing the ‘lactase’ enzyme.
Often this is temporary following a nasty tummy bug, as the ‘lactase’ has been washed away. In rare cases, it is a genetic disorder where lactase isn’t produced by the body in sufficient amounts.
Lactose doesn’t cause an allergic reaction and there is no need for your baby to follow a dairy free diet. You can buy lactose free baby milk as well as lactose free versions of milk and yoghurt. Cheese is naturally low in lactose so it’s fine to have. Alternatively, you can add a couple of drops of the ‘lactase’ enzyme to normal milk.
Cheese is naturally low in lactose so it’s fine to have. Alternatively, you can add a couple of drops of the ‘lactase’ enzyme to normal milk.
Again, if you think your baby has lactose intolerance, it is really important to go see your healthcare professional for further advice.
I suspect my baby has CMPA, can I try a milk free weaning diet without seeing my GP?If you suspect that your baby/child has CMPA, you have to be very careful as by cutting out milk, your baby is at risk of being deficient in lots of nutrients, which will affect their growth and development. Below is a list of just some of the key nutrients a dairy free diet is at risk of being deficient in:
Milk and dairy foods are one of the five main food groups and contribute to a significant amount of your baby’s nutrition.
If your baby is breastfed, they will receive small amounts of dairy protein through breast milk and if formula fed, all of their nutrition comes from dairy as the majority of infant formula are derived from animal milks.
Once weaning starts, the amount of milk (and the nutrition coming from milk) gradually decreases as food intake goes up. However, milk and dairy foods still play a significant role in nourishing your little one right through their childhood.
Always seek the advice of a healthcare professional before you try a diet that avoids a whole food group as babies can become deficient in nutrients quite quickly which can impact on their future health and development.
Here is a quick list of foods a CMPA baby can have to replace some of those key nutrients:
Foods containing calcium:-
Fish with soft edible bones e.g. tinned sardines, tinned salmon and anchovies – it’s the bones that contain calcium so blend / mash them up well rather than picking them out
-
Oranges
-
Dried apricots, currants and figs
-
Nut butters such as peanut butter and almond butter
-
Tofu that has been set with calcium sulphate
-
Tahini and hummus
-
Fortified non-dairy breakfast cereals such as Ready-Brek
-
Fortified bread such as Kingsmill Vitamin Boost or Warburtons Milk Roll
-
Soya milks and yoghurts that have calcium added
-
Green veg such as kale and broccoli – however, it’s not so well absorbed by the body
-
Meat – particularly red meat such as beef or lamb for its iron content
-
Poultry – the darker meat is more nutritious
-
Fish
-
Eggs
-
Lentils
-
Beans and other pulses
-
Tofu and soya (if tolerated)
-
Nut butters
People often think that egg is a dairy food and therefore has to be avoided if your baby has CMPA. The good news is that unless your baby has a specific egg allergy, egg does not contain the same proteins as milk so your CMPA baby can enjoy eggs as part of their diet which, incidentally are an excellent source of nutrition.
The good news is that unless your baby has a specific egg allergy, egg does not contain the same proteins as milk so your CMPA baby can enjoy eggs as part of their diet which, incidentally are an excellent source of nutrition.
Seeing a Registered Dietitian is crucial because dietitians are the only nutrition professionals regulated by law that can advise you on how to manage a free-from diet without risks to your baby’s health.
Unfortunately, NHS dietitians are scarce in some areas and so it’s important to make arrangements to attend either a group or one-to-one appointment when it’s offered.
If you feel the waiting list is too long, you can also self-refer to a Registered Dietitian in private practice – look for one who is experienced in paediatrics and allergies.
What will the dietitian do?If you are breastfeeding, the dietitian will advise on the dietary changes you’ll need to make to your own diet. You don’t need to stop breastfeeding. As well as excluding dairy foods you will need to add in other foods in order to ensure your milk supply and milk quality isn’t affected. The dietitian will also be considering how your diet needs to look so that your own health is optimised.
You don’t need to stop breastfeeding. As well as excluding dairy foods you will need to add in other foods in order to ensure your milk supply and milk quality isn’t affected. The dietitian will also be considering how your diet needs to look so that your own health is optimised.
If you are formula feeding, the dietitian will assess your baby’s diet, growth, and allergy symptoms and advise the GP on which of the prescription dairy free formula would be best for your baby. There are currently 13 variants, all with their own unique formulation.
Your dietitian will decide on the most appropriate one for your baby’s unique needs.
I’m breastfeeding and my baby has CMPA – Do I need to cut milk out of my diet too?The short answer is maybe…We aren’t sure why, but CMPA is rare in breastfed babies by comparison to those on formula. One of the potential explanations is the immune benefits that breast milk contains, as well as the ‘microbiome’ or healthy gut bacteria that breastfed babies have [2].
It is important to note here that whilst CMPA is more commonly seen in formula fed babies, it can still occur in breastfed babies. Cow’s milk passes through breast milk at 100,000 times lower than that which is in cow’s milk.
What this means is that the amount of cow’s milk that gets to the baby through their mother’s milk is a lot lower than if they were to directly consume cows milk. Therefore most allergic babies are able to tolerate their mother’s milk. It also means that the vast majority of mums don’t need to follow a milk-free diet either.
However, if your baby is one of the rare ones who does react to your breastmilk, then you can try a milk free diet for a period of time (usually around 2-6 weeks) to see if the symptoms improve.
It’s essential to see a dietitian, as it is important the quality of mum’s diet doesn’t suffer, particularly their calcium intake, and also to ensure that the quality of the breast milk isn’t impacted.
It’s crucial that breastfeeding mums meet their daily calcium and vitamin D requirements. Did you know that as a breastfeeding mum, your calcium requirements increase from 700mg/day to 1250 mg/day whilst you are nursing?
Did you know that as a breastfeeding mum, your calcium requirements increase from 700mg/day to 1250 mg/day whilst you are nursing?
You will need approximately a litre of calcium enriched plant-based milk each day as well as a 10mcg vitamin D supplement just to meet your requirements.
If you don’t get enough calcium and vitamin D, it’s likely your own bone health will suffer as your baby will take the calcium and vitamin D they need from your stores instead.
If after a milk free diet your baby’s symptoms don’t improve, then your dietitian will be able to advise on what you need to do next.
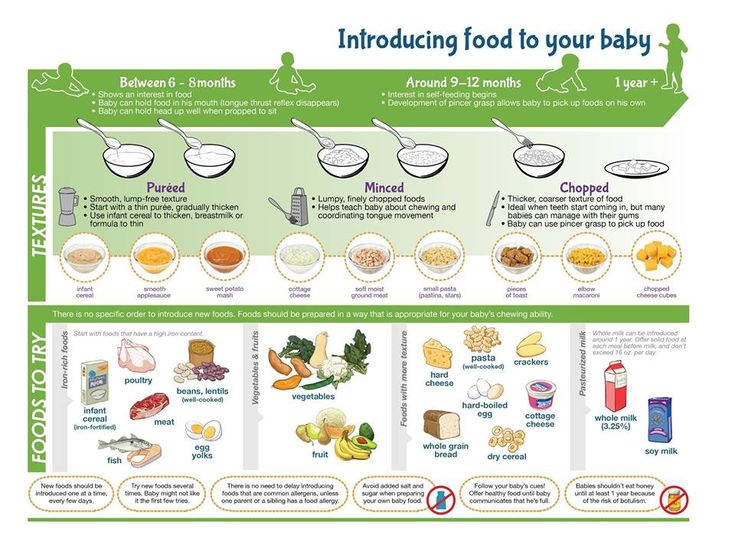
Weaning on a Dairy Free DietStage 1 (around 6 months)
Research has shown that at the start of weaning it is best to start with single vegetables then fruits but progressing on to iron rich foods quite quickly. You can read more about this in my blog called ‘Why Food Before One is Just for Fun is Not True’. You don’t need to do anything differently at the start of weaning if your baby has CMPA as fruits, vegetables and all my suggested iron rich foods are dairy free.
If you need to thin down purees that are too thick, you can use expressed breast milk or some of the prescribed formula you have been given. If your dietitian has advised that your baby can have soya, you could use a little calcium and iodine fortified soya milk providing they are over 6 months old. Soya isn’t suitable for babies under 6 months.
Stage 2 onwards (7 months +)As weaning progresses and your baby is taking 3 meals a day, you will start to try and balance their meals by including protein foods such as eggs, meat, fish, beans and pulses and starchy carbohydrate foods alongside their fruits and vegetables.
However, you will need to ensure that your baby avoids all forms of milk, butter, cheese and yoghurt, and any foods that contain milk by checking all food labels to ensure foods do not contain milk.
Cross contamination can be a real problem when eating outside the home or at nursery. For example, when foods containing milk have been prepared in the same area, the milk proteins can occasionally contaminate dairy free foods and cause an allergic reaction if eaten. Do let restaurants know before you order and have a good long chat with your childcare provider before they start nursery.
Do let restaurants know before you order and have a good long chat with your childcare provider before they start nursery.
As weaning progresses and your baby starts to drop milk feeds, you need to be in close contact with your dietitian as most babies who follow a dairy-free diet need to take more breastmilk or formula than non-allergic babies in order to meet their nutritional requirements.
The dietitian will also advise on how best to balance your infant’s diet depending on what known allergies they have and also whether they require any supplements.
The limiting nutrients protein, fat, energy, calcium, iodine, vitamin A and certain B vitamins will be considered alongside your typical routine and family meals to help you plan a way of eating that meets your baby’s nutritional needs. The nutrients that your baby receives in the first two years of life affects their growth and development including their brain development and intellect [3].
When your baby has a food allergy, they are more likely to have another. This also includes little ones with severe eczema requiring regular steroid cream [4].
The advice is to introduce the other allergenic foods, one at a time between 4 months and 12 months of age. Delaying introduction of these foods beyond 12 months can actually make the likelihood of having an allergy greater [5].
It is advisable to start with egg and then peanut, after that the other allergens detailed on the list below can be offered. If you would like to know exactly how to introduce all of the allergens you can find out how in my mini online course ‘Introducing Allergens’.
Egg
Choose British red lion stamped eggs and offer both the white and the yolk together. Something like mashed or scrambled egg works well for spoon feeding or omelette strips as a finger food.
Peanuts
You mustn’t give your baby whole nuts due to the risk of choking, and peanut butter on a spoon can also pose the same risk. Puffed peanut snacks, peanut powder mixed into food or a small amount of smooth peanut butter warmed and thinned down with some of your baby’s usual milk or hot water are better options. You can add this thinned peanut butter to pureed fruits or vegetables.
Puffed peanut snacks, peanut powder mixed into food or a small amount of smooth peanut butter warmed and thinned down with some of your baby’s usual milk or hot water are better options. You can add this thinned peanut butter to pureed fruits or vegetables.
If your baby tolerates these foods without a reaction, continue offering them regularly as part of their normal diet. This repeated exposure has a protective effect.
Other allergenic foods
You can then start to offer the other common allergenic foods alongside other tolerated foods. Just offer one at a time (no more frequently than one new food per day) and just ¼ to ½ teaspoons worth, so that if your baby does react you know which one was the culprit.
-
Tree-nuts – almond, cashew, walnuts, brazil nuts, pecans, hazelnuts etc prepared in the same way as peanuts above.
-
Wheat – breakfast cereals, pasta, bread, couscous, breadsticks
-
Sesame – such as houmous which contains tahini (sesame paste)
-
Fish & seafood – cod, haddock, salmon, trout, tuna, prawns, crab, mussels
Again, if your baby tolerates them continue offering them regularly as part of their normal diet to capitalise on the protective effect of repeated exposure.
There are other foods that can cause allergic reactions when eaten, the Food Standards Agency (FSA) recognises 14 common allergens, which by Law must be declared prominently when they are an ingredient in any food.
It is possible that anyone can develop an allergy to anything, so it is very important to be aware of the symptoms of an allergic reaction.
If you are concerned that a certain food is causing a reaction to your baby, stop offering that food and seek medical advice from a health professional.
For more information on the 14 allergens please visit the FSA website.
The Food Standards Agency’s 14 allergensWhilst the list below is not exhaustive of all allergens (it is possible for anyone to be allergic to anything), this is the list of the 14 most common allergenic foods, that must be legally declared when they are used as an ingredient in food in the UK:
-
Celery
-
Cereals containing gluten – the protein found in wheat
-
Crustaceans – a type of seafood like prawns, crab and lobster
-
Eggs
-
Fish
-
Lupin – a flower that’s found in flour
-
Milk
-
Molluscs – shelled foods like mussels, whelks, snails
-
Mustard
-
Tree nuts
-
Peanuts
-
Sesame seeds
-
Soya
-
Sulphur dioxide – used as a preservative in dried fruits and some sausages
If your baby has IgE or immediate onset CMPA, there is no need to be concerned about them being allergic to soya.
There is a link however between non-IgE or delayed onset CMPA where up to 50% of babies/children may also show a similar allergic reaction to the proteins found in soya [6]. The current advice would be to try introducing a small amount of soya once weaning is well established and use a stepwise soya ladder to increase quantities. Your dietitian will go through what this looks like with you.
I heard that soya was bad for babies and they should avoid it, is this true?It is recommended that babies under 6 months don’t have soya infant formula but this has nothing to do with allergies. Soya also contains phyto-oestrogens which are similar to female hormones. An old study in male marmoset monkeys found changes in male monkeys fertility when they were fed soya [7].
As a precaution, the NHS advises that babies should not have soya infant formula under 6 months of age but this can be given after 6 months when weaning has started and milk is no longer the sole source of nutrition.
After reading this you might be worried that there’s not much left that your little one CAN eat. It can be so easy to focus on all of the foods that your little one needs to avoid that you forget about all of the wonderful foods that they can enjoy!
There are lots of foods that are naturally free from dairy. Fruits and vegetables, meats, fish and seafood, eggs, nuts and seeds, grains such as rice and couscous. The list really is endless. If you’re struggling to think of the foods that your little one can eat, have a chat with your dietitian who will be able to give you some more ideas.
How do I know if my baby has outgrown her milk allergy?If your baby has been symptom-free for 6 months and is older than 9 months of age they can undergo a stepwise challenge to see if they are still allergic. The Milk Ladder is a step by step approach that is carried out under the supervision of a dietitian if your baby has non-IgE delayed onset type of allergy.
For those who have an IgE or immediate onset milk allergy, the milk ladder is carried out in hospital under close medical supervision.
What is the milk ladder?The milk ladder is a six-step approach to re-introducing milk, initially in a baked form alongside other proteins as this is less allergenic and moving stepwise in increasing amounts, other proteins and less baking time as it progresses.
There are specific recipes to accompany the first 3 steps on the milk ladder and it’s important not to alter these recipes which have been created in a specific way to measure tolerance.
If your child doesn’t tolerate a certain step, they remain on the step before and include these foods in their diet until a date is arranged to try again.
Dairy free baby food recipes for weaning:Here are my top 10 dairy free baby food recipes for each stage of weaning:
Stage 1-
Carrot puree
-
Broccoli Puree
-
Trio of Root Veg
-
Courgette and pea mash
-
Apple and Beetroot puree
-
Carrot and spinach puree
-
Parsnip and Pear puree
-
Cauliflower, apple and sweet potato
-
Avocado smash with banana
-
Apple and apricot pudding
-
2 ingredient pancakes
-
Omelette fingers
-
Veggie Curry
-
Pork and paprika
-
Omega-3 rich quinoa balls
-
Pizza and Pasta sauce
-
Fish risotto with peas
-
Pork Casserole
-
Fruity chicken
-
Bolognese
My Baby’s First Birthday Cake recipe
-
Blueberry porridge
-
Moroccan Lamb with couscous
-
Jacket Potato with Bean Chilli
-
Chicken meatballs
-
Beef curry
-
Home made fish fingers
-
Lentil Dhal
-
Chicken coconut curry
-
Dairy free mini lasagnes
-
Baby’s 1st Birthday Cake (made with dairy free milk)
For younger babies there are 13 different variants and the one your baby needs will be determined by the dietitian, Essentially there are two main differences:
Extensively Hydrolysed FormulaThese are processed so that the protein within the cow’s milk is broken down into smaller parts so that they become hypoallergenic and are able to pass by the immune system without causing symptoms.
Examples include Althera, Nutramigen LGG 1&2, Pregestamil Lipil, Aptamil Pepti 1&2, Aptamil Pepti Junior, Infantrini Peptisorb and Simlac Alimentum.
Amino Acid FormulaThese are only prescribed in the most severe cases of food allergy. The proteins are completely broken down to amino acids and so are unrecognisable to your baby’s immune system.
Examples include Alfamino, PurAmino, Neocate LCP and Neocate Syneo.
Both extensively hydrolysed formula and amino acid formula will taste and smell differently to standard baby formula. For young babies, such as under 4 months, they tend to just get used to this and accept it. However, older babies who are used to the taste and smell of standard formula, are likely to struggle to accept the new formula.
Your dietitian can work with you to make this transition easier and increase the chances of your baby accepting the new milk.
If your baby is over 6 months of ageA soya based infant formula may be a suitable alternative to standard formula assuming your baby can tolerate soya.
It’s important not to give soya formula to babies under 6 months as the levels of oestrogens are too high for developing babies. You should also be aware that soya infant formula contains a type of sugar which isn’t good for your baby’s teeth.
How long should my baby stay on their special formula?In order to ensure your baby is getting all the nutrition they need, it is likely they will likely stay on their infant formula until around 2 years of age which is the current World Health Organisation Guideline, however if they eat a balanced and varied diet and are not fussy, your dietitian may suggest certain plant-based milk alternatives. It is important to follow their advice as not all plant milks are nutritionally equal.
If this is the case it’s likely that additional calcium and vitamin D in the form of a supplement will be needed.
Could I not just give my CMPA plant milk to drink instead of formula?There are lots of plant-based milks available on the market such as almond milk, oat milk, hemp milk and pea milk. Whilst these do not contain any milk, they are a poor source of nutrition for your baby as they do not contain the right balance of nutrients, particularly calories, fat and protein as well as lots of other nutrients.
Whilst these do not contain any milk, they are a poor source of nutrition for your baby as they do not contain the right balance of nutrients, particularly calories, fat and protein as well as lots of other nutrients.
Calcium and iodine fortified unsweetened soya milk can be used in cooking, but should not replace breastmilk or formula or be given as a drink until at least 2 years of age. Your dietitian will advise if the other plant-based milks can be used in cooking with your individual baby.
Again, it’s not a one size fits all approach as the context of the rest of their diet has to be considered.
Rice milk is not suitable for children under 5 due to the naturally occurring high levels of inorganic arsenic.
How long does CMPA last?Research shows that most babies with CMPA will have outgrown their allergy by the age of three. However, it can last throughout childhood and even into adulthood in some rare cases.
It is possible to desensitise the body to milk using the milk ladder described above, so including milk containing foods at the level your baby reached on the milk ladder as part of their normal diet is important.
As eliminating milk from the diet is associated with nutritional risks, challenging your little one at regular intervals in encouraged.
Can probiotics help my baby with a milk allergy?Probiotics may help a baby with the symptoms of a cow’s milk protein allergy however the evidence that we have isn’t good enough to make this recommendation. We are still waiting on more research to see if these could help[8].
How do I access a dietitian?Your health visitor or GP can refer you to an NHS dietitian or you can find a private practice one here. Make sure your dietitian is a paediatric dietitian with experience in food allergies in order to support you fully.
How can I find out more about CMPA?There is information available on CMPA on the Allergy UK website
Are there any alerts I should sign up to?I would recommend signing up to the Food Standards Agency (FSA) allergy food alerts. You can receive email/text reminders whenever there is a food safety recall due to an allergen not being present on a food label and therefore a risk to anyone with a food allergy.
You can receive email/text reminders whenever there is a food safety recall due to an allergen not being present on a food label and therefore a risk to anyone with a food allergy.
You can follow me on Instagram and Facebook for daily tips and advice or you can join my Happy Healthy Weaning course where I will guide you every step of the way along your baby’s weaning journey.
Sarah Almond Bushell MPhil, BSc (Hons) RD MBDA – Registered Dietitian & Children’s Nutritionist
0003Fat 3g
Fiber -
Energy {{foodstuff.foodstuff.energy}} kcal{{foodstuff.foodstuff.energy}} kJ
= {{ unitConvert(foodstuff.foodstuff.energy,0.239) | number : 0}} kcal= {{ unitConvert(foodstuff.foodstuff.energy,4.184) | number : 0}} kJ
Protein {{foodstuff.foodstuff.protein}} g-
Carbohydrate {{foodstuff.foodstuff.carbohydrate}} g-
Fat {{foodstuff. foodstuff.fat}} g-
foodstuff.fat}} g-
Fiber {{foodstuff.foodstuff.fiber}} g-
Energy 95 kcal
Proteins 2 g
Carbohydrates 14 g
Fat 3 g
Fibers -
Food values
| Belts | 2 g 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 | 14 g | |||||
| sugar | 0 g | ||||||
| fat |
| Name | Energy (kcal) | ||
|---|---|---|---|
| Zucchini stew with vegetables | Sprat in Tom Cubley Sauce | 130 | add_circle Contribute |
{{feedback. text}}
text}}
See all reviews
| ).join(' ')}}products in our database
{{(userCount | number : 0).split(',').join(' ')}}
registered in Calorie Table
Baby food: ✔Gerber ✔Nutrition ✔Baby ✔Nestle
It's amazing, but baby food is a little over 150 years old. No, before that, of course, children were also fed, but not in the same way as today. Modern mothers, if necessary, can replace breast milk with a similar analogue in composition and safely diversify the children's menu. We are talking about mixtures and complementary foods from jars and bags, which, with their appearance, changed the centuries-old diet. And before that, they didn’t feed babies with anything!
In ancient Greece, as a first food, children were given liquid barley stew, to which they added bull's blood in Sparta so that the boys would grow up to be real warriors.
Mammal
I would not want to make it an absolute custom to feed children food so that they do not scream for nothing, but there is something in it. At least the mouth is busy for a while. Well, if mother's milk. But not everyone was lucky. So the she-wolf raised Romulus and Remus, according to this myth. And the ancient Greek gods, starting with the main one, Zeus, grew up on the milk of goats, although they also claimed the breasts of mother goddesses.
At least the mouth is busy for a while. Well, if mother's milk. But not everyone was lucky. So the she-wolf raised Romulus and Remus, according to this myth. And the ancient Greek gods, starting with the main one, Zeus, grew up on the milk of goats, although they also claimed the breasts of mother goddesses.
In the Middle Ages, baby bottles were made of leather and wood. At the beginning of the 19th century, they began to produce porcelain teats with leather or suede teats.
In different countries at different times, milk from almost all animals capable of producing it was used, that is, for the benefit of baby food. The babies left without mother's milk were fed by goats and cows, sheep and camels, llamas and donkeys.
Not documented, but the story that one of the children of Charles Darwin was fed donkey milk is still not forgotten. Apparently, the English naturalist made a natural selection - he chose a donkey as a wet nurse, believing that her milk is closest in composition to human milk.
Drink, children
AG Venetsianov "A nurse with a child" • source: wikimedia.org / СС BYChildren were deprived of their mother's milk not always by nature. Sometimes women themselves refused to feed their offspring. The poor were hindered by work, the rich by whims. In the Middle Ages, it was believed that breastfeeding distracted the mother from the birth of other children, and in modern times - from secular life. A woman of a noble family had to give birth to as many children as possible, and any other woman could feed them. This approach led to the fact that in Europe and Russia, wealthy mothers gave newborns to nurses. In France, this tradition was most common. In the second half of the 18th century, the first agencies for hiring wet nurses appeared in Paris.
Paris, 1845. The authorities united four such agencies into a municipal nursing office, which defended their rights and guaranteed their wages. The bureau survived the French Revolution and closed in 1876. But then dry milk formula was already invented and distributed throughout Europe.
But then dry milk formula was already invented and distributed throughout Europe.
Milk replacement
Henri Nestlé , founder of Nestlé • source: wikimedia.org / CC BYThe loss of a stable income for breadwinners is due to science. Since the beginning of the 19th century, European scientists have been trying to invent a scientifically based alternative to mother's milk. And the necessary conditions for this gradually developed: they learned how to preserve and disinfect products, and in 1855 the Englishman Grimweid invented powdered milk. But, if not for Henri Nestle, all these discoveries might have existed on their own.
Henri Nestle's Milk Flour
source: blick.ch / SS BY
The problem of baby food affected Nestle after the birth of his first child, who was not suitable for mother's milk, and progressive at that time parents did not want to feed cows. A certified pharmacist and pharmacy owner in a Swiss town in 1867 made a mixture of powdered cow's milk, wheat flour and sugar, which he called "Henri Nestlé Milk Flour". Diluted with water, it became the world's first artificial baby food.
Diluted with water, it became the world's first artificial baby food.
Post passed
The duration of breastfeeding in pre-revolutionary Russia was established by the church and amounted to three strictest fasts (only Great and Assumption were taken into account ). These terms were not strictly related to age and depended on the time of birth. If a child was born during Great Lent, they were fed from Dormition to Dormition; if after the Dormition Fast (the Great was considered the first, the Dormition Fast was the second, the Great again was the third), then they were fed until almost two years old and were weaned only before the Dormition Fast.
Mixture and only
Martinus van der Hagen ,founder of Nutricia • source: wikimedia.org / СС BY
well-fed. The last option is a consequence of a considerable amount of sugar in the first mixtures. This was taken into account by the Dutchman Martinus van der Hagen, who in 1896 invented his own method of drying milk in a bakery.
His milk formula contained significantly less flour and sugar than that of its main competitor, and therefore received the approval of the then doctors and, largely thanks to them, became popular. Thus began the history of Nutricia. In the US, they also appreciated the charm of a new way to feed hungry children. The production of baby food was put on stream by Clapp's Baby Food and Beech-Nut.
source: artinvestment.ru / CC BY
Russia was still a few decades before the opening of its own production of baby dry mixes "Malyutka", on which a good part of Soviet toddlers will then grow. And exactly one hundred years before that, in 1872, “milk flour” began to be sold in St. Petersburg, and then throughout the country, the agent of the Nestlé company, Alexander Wenzel. The merchant advertised a new product in the newspapers of that time: a girl, satisfied with life and the taste of milk flour, joyfully licks her finger next to a source of full pleasure - a can of mixture at a price of 1 ruble 10 kopecks. But not everyone was appreciated and not immediately. And even more so where the press was not able to read.
But not everyone was appreciated and not immediately. And even more so where the press was not able to read.
The old fashioned way
The final weaning from breast milk in pre-revolutionary Russia took place in the period from one to two or three years and was expressed in the change of the nickname "sidun" to "hodun". Often it happened "for berries", that is, in the summer months, when berries and fruits ripened, which were given to children "to calm down" - as a consolation.
The farther from the capitals, the less was not only dry mixes, but also knowledge about them. Children continued to be fed by other women for money or thanks, they were given diluted animal milk and they began to supplement them very early. Usually liquid boiled porridges. In Europe - oatmeal, in Asia - rice, in Russia - semolina and semolina. In pre-revolutionary Russia, in addition to cereals, a child already six months old usually knew the taste of potatoes, onions, cucumbers, including pickles.
Some Soviet pediatricians, and after them mothers and grandmothers of that time, believed that it would be good for children to taste salty after sweet milk. So often two-three-month-old babies were given to suck on a chicken bone, a crust of black bread, pickles or lard.
It was considered normal to feed him cabbage soup and sauerkraut. Even earlier, they gave "zhevka" - a cloth with wrapped chewed bread, sometimes soaked in sweetened water, kvass or home brew. However, this idea - to occupy a child's mouth with a rag with dubious contents from the point of view of hygiene and pediatrics - was adopted from Europe. It’s just that in our country she stayed longer than in her “homeland”.
And so, when the rag was already taken out of the mouth, but they had not yet been invited to the common table, and the children continued to be indignant, they had to somehow get out. More precisely, twist gauze with chopped vegetables and fruits so that they give all their juices for the benefit of children's health. By the way, they just started to take care of him. Enlightened minds have finally traced the connection between what children eat and how long they live without suffering from disease.
By the way, they just started to take care of him. Enlightened minds have finally traced the connection between what children eat and how long they live without suffering from disease.
Until the beginning of the 20th century in Russia, a horn hollowed out of a cow's horn was used as a pacifier. The contents were knocked out of it and a groove was made at the end for pulling on the "tit" - the nipple of the cow's udder, which was soaked in milk, vegetable oil, sugar and honey water.
And from a can is simpler
source: wipo.int / SS BYBy that time (1870), Henri Nestlé had released a novelty - condensed milk. It was invented back in 1856 by American Gail Borden, but it was Henri Nestle and his company who made condensed milk a popular children's treat. True, the doctors were unhappy: few followed the recommendation to dilute condensed milk with water in a ratio of 1 to 10 and only then give it to children.
Condensed milk was eaten with spoons, sometimes with jars. And this, of course, led to rapid weight gain. Doctors insisted: it is better to feed children with vegetables and fruits. But twisting the gauze is already pretty tired. And then there were jars.
And this, of course, led to rapid weight gain. Doctors insisted: it is better to feed children with vegetables and fruits. But twisting the gauze is already pretty tired. And then there were jars.
Daniel Frank GerberNot only in the dark times of the Middle Ages, but also in the century before last, children and their nutrition were not particularly awe-inspiring. We already heard something about hygiene and even visited doctors, but, of course, there was no special children's menu. On the contrary, children in even the poorest families of the 19th century were fed what was worse.
founder of the Gerber Company
source: wikimedia.org / СС BY
Michigan manufacturer Daniel Gerber established the first large-scale production of canned food for children. It was again a matter of personal interest—the need for special nutrition for Sally's daughter. Gerber's wife learned how to make vegetable, fruit and meat puree for a sick child, and then convinced her husband to start mass production.
In 1928, Gerber Foods' baby food went on sale. It is still there.
Dairy kitchens and non-dairy rivers
Children in our country also wanted to eat. Especially those who lacked scarce imported food. In the 1920s, dairy kitchens appeared, where milk mixtures, fermented milk products, cottage cheese were made from fresh products, and juices and mashed potatoes were made from fruits and vegetables.
In the 1950s, mass production of baby food began in the Soviet Union: canned juices and purees, powdered milk mixtures, cereals and kissels. Since then, for several decades, dairy kitchens did not prepare food, but simply gave out jars and bags.
In the 1950s, complementary foods were started as early as 2-4 months, and if the child is bottle-fed, then even earlier. And this is not only a Soviet trend.
In the first edition of the well-known book by the American doctor Spock on the upbringing of children (1946), there is this passage:
“Many doctors now recommend giving meat from 2-6 months.
Meat for a small child is either turned in a meat grinder several times, or rubbed through a sieve, or rubbed on a grater. Therefore, it is easy for a child to eat it, even while he has no teeth.”
Toddlers of the 1970s owe a lot, if not to everything, to these dairy kitchens, dry mixes "Malyutka", and also to the canned food of the Odessa Cannery and the Moscow Poultry Plant. It was fashionable to eat from jars, boxes and tubes, because the main characters of that time, the astronauts, ate like that.
The glass feeding bottle was patented in 1841 by Charles Windshiel of Massachusetts.
Approximate scheme of "Soviet-style" complementary foods according to the recommendations of the Ministry of Health 1976 years
- 1 month - fruit juices
- 1.5 months - applesauce (grated apple)
- 3.5 months - cottage cheese (dairy)
- 4 months - egg yolk
- 4.

.