Order of baby food introduction
When, What, and How to Introduce Solid Foods | Nutrition
For more information about how to know if your baby is ready to starting eating foods, what first foods to offer, and what to expect, watch these videos from 1,000 Days.
The Dietary Guidelines for Americans and the American Academy of Pediatrics recommend children be introduced to foods other than breast milk or infant formula when they are about 6 months old. Introducing foods before 4 months old is not recommended. Every child is different. How do you know if your child is ready for foods other than breast milk or infant formula? You can look for these signs that your child is developmentally ready.
Your child:
- Sits up alone or with support.
- Is able to control head and neck.
- Opens the mouth when food is offered.
- Swallows food rather than pushes it back out onto the chin.
- Brings objects to the mouth.
- Tries to grasp small objects, such as toys or food.
- Transfers food from the front to the back of the tongue to swallow.
What Foods Should I Introduce to My Child First?
The American Academy of Pediatrics says that for most children, you do not need to give foods in a certain order. Your child can begin eating solid foods at about 6 months old. By the time he or she is 7 or 8 months old, your child can eat a variety of foods from different food groups. These foods include infant cereals, meat or other proteins, fruits, vegetables, grains, yogurts and cheeses, and more.
If your child is eating infant cereals, it is important to offer a variety of fortifiedalert icon infant cereals such as oat, barley, and multi-grain instead of only rice cereal. Only providing infant rice cereal is not recommended by the Food and Drug Administration because there is a risk for children to be exposed to arsenic. Visit the U.S. Food & Drug Administrationexternal icon to learn more.
How Should I Introduce My Child to Foods?
Your child needs certain vitamins and minerals to grow healthy and strong.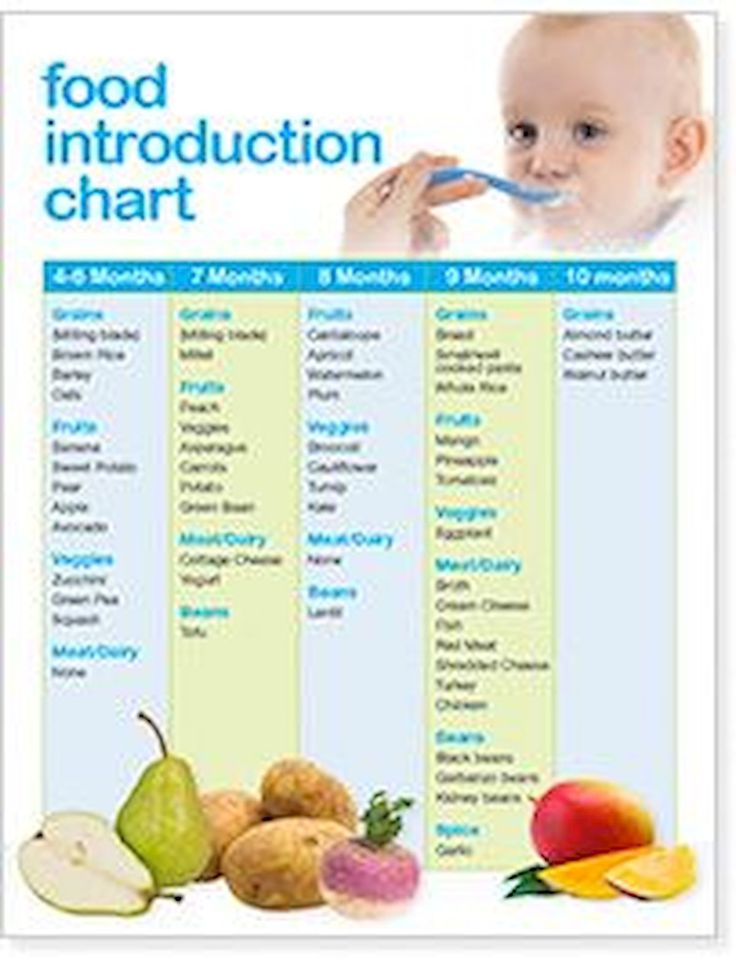
Now that your child is starting to eat food, be sure to choose foods that give your child all the vitamins and minerals they need.
Click here to learn more about some of these vitamins & minerals.
Let your child try one single-ingredient food at a time at first. This helps you see if your child has any problems with that food, such as food allergies. Wait 3 to 5 days between each new food. Before you know it, your child will be on his or her way to eating and enjoying lots of new foods.
Introduce potentially allergenic foods when other foods are introduced.
Potentially allergenic foods include cow’s milk products, eggs, fish, shellfish, tree nuts, peanuts, wheat, soy, and sesame. Drinking cow’s milk or fortified soy beverages is not recommended until your child is older than 12 months, but other cow’s milk products, such as yogurt, can be introduced before 12 months. If your child has severe eczema and/or egg allergy, talk with your child’s doctor or nurse about when and how to safely introduce foods with peanuts.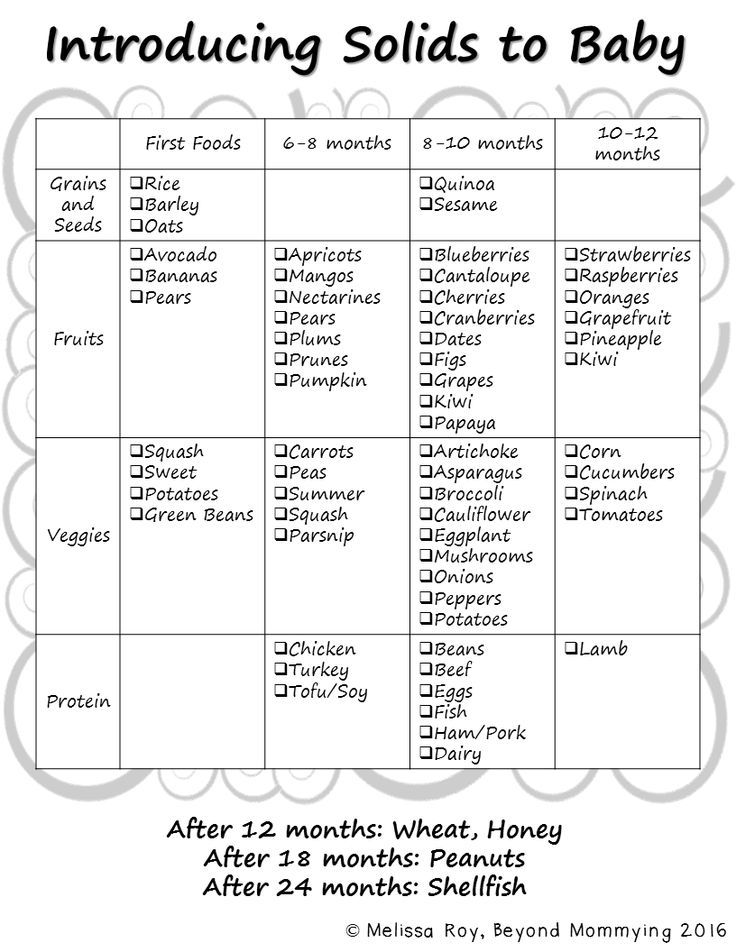
How Should I Prepare Food for My Child to Eat?
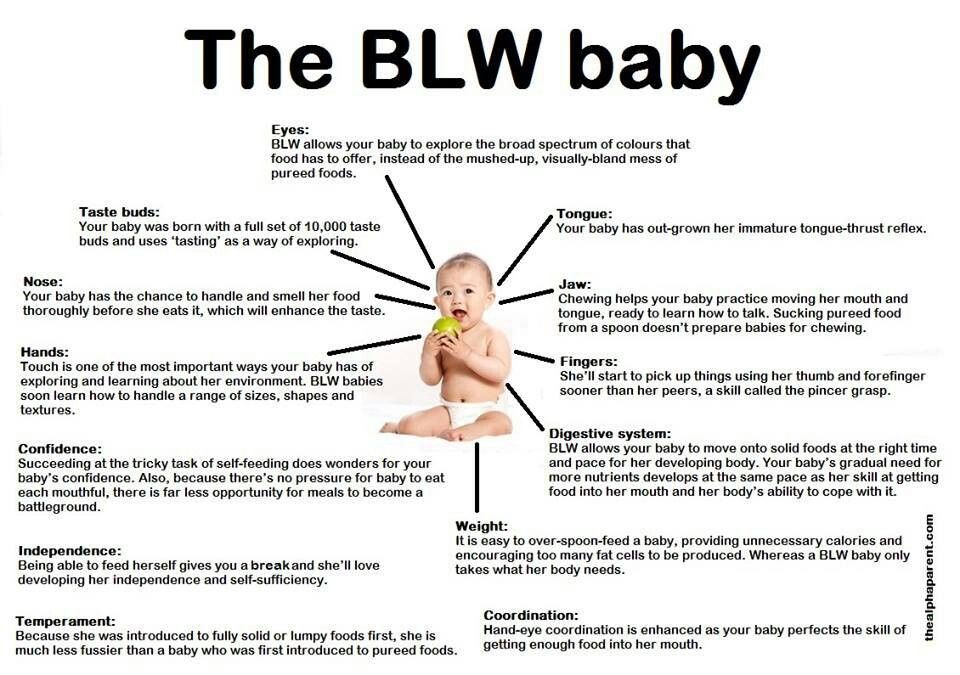
At first, it’s easier for your child to eat foods that are mashed, pureed, or strained and very smooth in texture. It can take time for your child to adjust to new food textures. Your child might cough, gag, or spit up. As your baby’s oral skills develop, thicker and lumpier foods can be introduced.
Some foods are potential choking hazards, so it is important to feed your child foods that are the right texture for his or her development. To help prevent choking, prepare foods that can be easily dissolved with saliva and do not require chewing. Feed small portions and encourage your baby to eat slowly. Always watch your child while he or she is eating.
Here are some tips for preparing foods:
- Mix cereals and mashed cooked grains with breast milk, formula, or water to make it smooth and easy for your baby to swallow.
- Mash or puree vegetables, fruits and other foods until they are smooth.

- Hard fruits and vegetables, like apples and carrots, usually need to be cooked so they can be easily mashed or pureed.
- Cook food until it is soft enough to easily mash with a fork.
- Remove all fat, skin, and bones from poultry, meat, and fish, before cooking.
- Remove seeds and hard pits from fruit, and then cut the fruit into small pieces.
- Cut soft food into small pieces or thin slices.
- Cut cylindrical foods like hot dogs, sausage and string cheese into short thin strips instead of round pieces that could get stuck in the airway.
- Cut small spherical foods like grapes, cherries, berries and tomatoes into small pieces.
- Cook and finely grind or mash whole-grain kernels of wheat, barley, rice, and other grains.
Learn more about potential choking hazards and how to prevent your child from choking.
Top of Page
Helpful Resources | Nutrition | CDC
If you would like more information on topics related to feeding your baby or toddler, here are some resources:
General
CDC’s Infant and Toddler Nutrition microsite syndication
CDC offers a free Web Content Syndication service that gives public health partners the opportunity to syndicate CDC content directly to their sites without having to monitor or copy updates.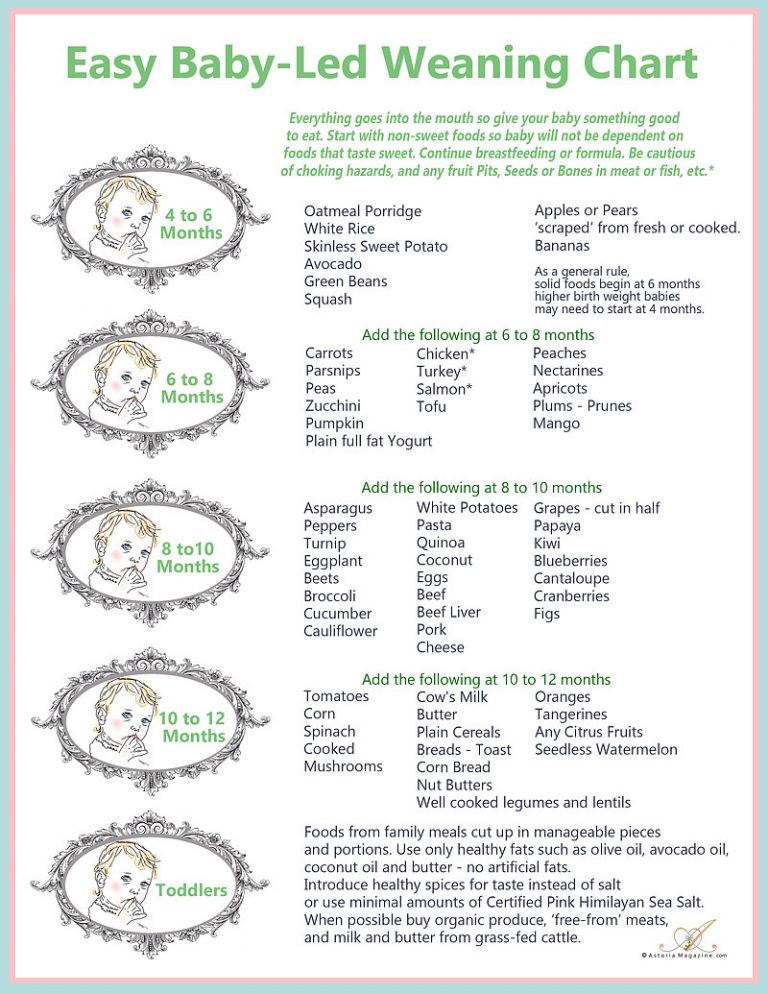 To search the CDC infant and toddler nutrition website available for syndication as well as other resources you can share, visit the CDC Public Health Media Library and browse or search for “infant and toddler nutrition”. Learn more about content syndication and how to add CDC syndicated content on your site.
To search the CDC infant and toddler nutrition website available for syndication as well as other resources you can share, visit the CDC Public Health Media Library and browse or search for “infant and toddler nutrition”. Learn more about content syndication and how to add CDC syndicated content on your site.
CDC’s Child and Teen Resources
This collection of resources provides parents and caregivers, health care providers, and partners with tools and information to help children and teens maintain a healthy weight and prevent obesity.
CDC’s Child Development Positive Parenting Tips (Infants)
This CDC website provides information about infants’ development, as well as tips for positive parenting and promoting the safety and health of infants.
CDC’s Learn the Signs. Act Early.
This website includes tools to track children’s milestones and resources about children’s development.
CDC’s Parent Information
This CDC website provides resources and information on pregnancy, infants and toddlers, children, and teens.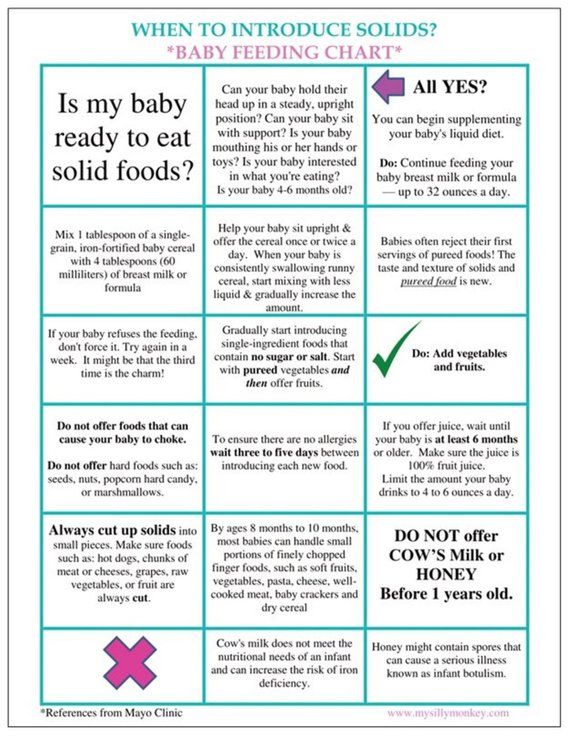 Learn how to handle common parenting challenges through interactive activities, videos, and more. Healthcare professionals and researchers can also find information on children’s health and safety.
Learn how to handle common parenting challenges through interactive activities, videos, and more. Healthcare professionals and researchers can also find information on children’s health and safety.
CDC’s Division of Oral Health
Tooth decay (cavities) is one of the most common chronic diseases of childhood in the United States. Untreated tooth decay can cause pain and infections that may lead to problems with eating, speaking, playing, and learning. CDC’s Division of Oral Health provides information on what parents and caregivers can do to ensure good oral health for your child.
Dietary Guidelines for Americans 2020–2025 pdf icon[PDF-30.6MB]external icon
These guidelines provide science-based advice for Americans on what to eat and drink to promote health, reduce chronic disease, and meet nutrient needs. The 2020–2025 edition provides recommendations for all life stages, including infants and toddlers.
Feeding Guidelines for Infants and Young Toddlers: A Responsive Parenting Approachexternal icon
This report presents recommendations for promoting healthy nutrition and feeding patterns for infants and toddlers from birth to 24 months, with an emphasis on dietary quality, portion sizes, and mealtime environment.
Healthy Childrenexternal icon
This website was developed by the American Academy of Pediatrics for parents. It features thousands of articles in English and Spanish on children’s health and safety, as well as interactive tools.
United States Department of Agriculture Special Supplemental Nutrition Program for Women, Infants, and Children (WIC)external icon
The WIC Program provides support to low-income pregnant, postpartum, and breastfeeding women, babies, and children up to age 5. WIC provides nutritious foods, information on healthy eating, breastfeeding promotion and support, and referrals to health care.
United States Department of Agriculture Supplemental Nutrition Assistance Program (SNAP)external icon
SNAP provides benefits to low-income individuals and families and provides economic benefits to communities.
Feeding and Beverage Recommendationsexternal icon
Healthy Eating Research, a national program of the Robert Wood Johnson Foundation, offers science-based recommendations for parents and caregivers. Tips are available for feeding children from birth through 24 monthsexternal icon and beverages for children from birth through 5 yearsexternal icon. Tips for older children are also available.
Tips are available for feeding children from birth through 24 monthsexternal icon and beverages for children from birth through 5 yearsexternal icon. Tips for older children are also available.
U.S. Food and Drug Administration (FDA) and Environmental Protection Agency’s (EPA) Advice About Eating Fishexternal icon
The U.S. FDA and EPA provide advice regarding eating fish. This advice can help people make informed choices when it comes to the types of fish that are nutritious and safe to eat. It is especially important for those who might become pregnant, who are pregnant, or who are breastfeeding, as well as for parents and caregivers who are feeding children. This advice supports the recommendations of the Dietary Guidelines for Americans.
Top of Page
Breastfeeding
CDC’s Breastfeeding Information
CDC’s Division of Nutrition, Physical Activity, and Obesity (DNPAO) is committed to increasing breastfeeding rates throughout the United States. CDC provides information for public health professionals and others to help support breastfeeding mothers, such as managing breastfeeding during various maternal and infant illnesses and conditions, any precautions for vaccines during breastfeeding, and recommendations for proper storage and handling of expressed human milk.
CDC provides information for public health professionals and others to help support breastfeeding mothers, such as managing breastfeeding during various maternal and infant illnesses and conditions, any precautions for vaccines during breastfeeding, and recommendations for proper storage and handling of expressed human milk.
International Lactation Consultant Association (ILCA)external icon
ILCA is the member association for professionals who care for breastfeeding families. ILCA’s “Find a Lactation Consultant Directory” can help you find a lactation consultant to get the breastfeeding support you need.
United States Lactation Consultant Association (USLCA)external icon
USLCA is a professional association for International Board Certified Lactation Consultants (IBCLCs) and other health care professionals who care for breastfeeding families. USLCA’s “Find an IBCLC” can help you find a lactation consultant to get the breastfeeding support you need.
WIC, the Special Supplemental Nutrition Program for Women, Infants, and Children—Breastfeeding Support external icon
The United States Department of Agriculture Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) Breastfeeding Support website includes resources for expectant and current mothers about breastfeeding, overcoming common challenges, and thriving to make breastfeeding work for their families.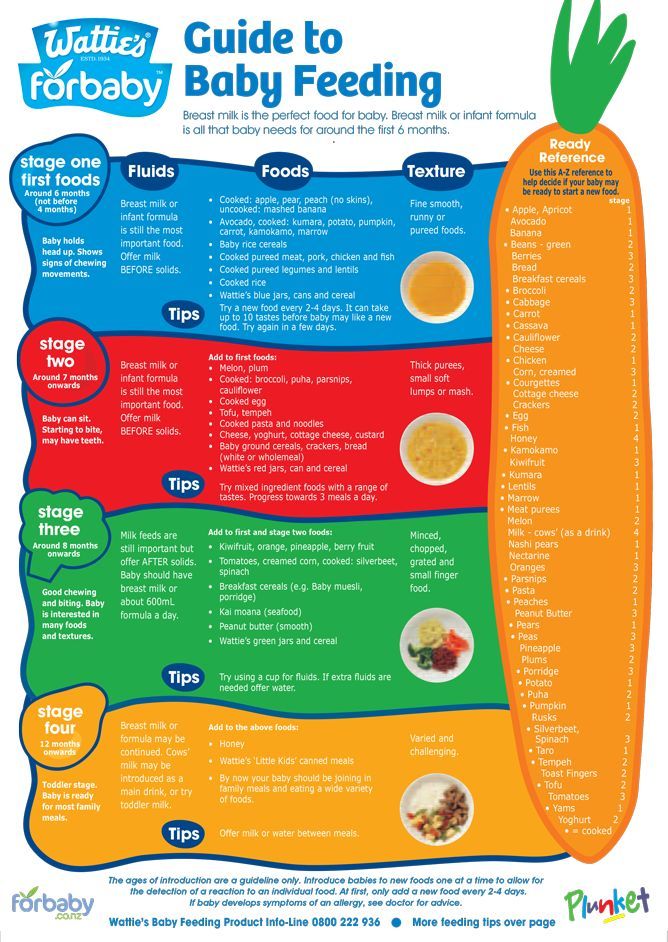
La Leche League USAexternal icon
La Leche League USA helps mothers to breastfeed through mother-to-mother support, encouragement, information, and education and promotes a better understanding of breastfeeding as an important element in the healthy development of the baby and mother.
Office on Women’s Healthexternal icon
The Office on Women’s Health’s vision is for all women and girls to achieve the best possible health outcomes. They provide information on breastfeeding to help women make infant feeding decisions and to guide mothers through the breastfeeding process.
Top of Page
Infant Formula
Questions & Answers for Consumers Concerning Infant Formulaexternal icon
The U.S. Food & Drug Administration regulates infant formula and has a list of questions and answers about infant formula.
Infant Formula Do’s and Don’tsexternal icon
The U.S. Food and Drug Administration provides information on infant formula preparation and storage, as well as other tips on how to keep infant formula safe.
Top of Page
Food Safety
Food Safety Concerns for Children Under Fiveexternal icon
Food safety is particularly important for young children. Foodsafety.gov provides information on safely preparing food for your child.
Top of Page
Meal Time
Fruits & Veggies—Have a Plant Movementexternal icon
A resource designed to help spread the word about the health benefits of adding more fruits and veggies to your diet.
USDA MyPlate Kitchenexternal icon
This online tool features a large collection of recipes and resources to support building healthy and budget-friendly meals. Site features include:
- Extensive search filters on cuisine, cooking equipment, nutrition content, and more.
- Detailed nutrition information.
- Cookbooks to browse and download or build your own.
- Recipe star ratings, review comments, and sharing on social networks.
Video Series on How to Introduce Solid Foods
1,000 Days has developed helpful videos about introducing solid foods to your baby.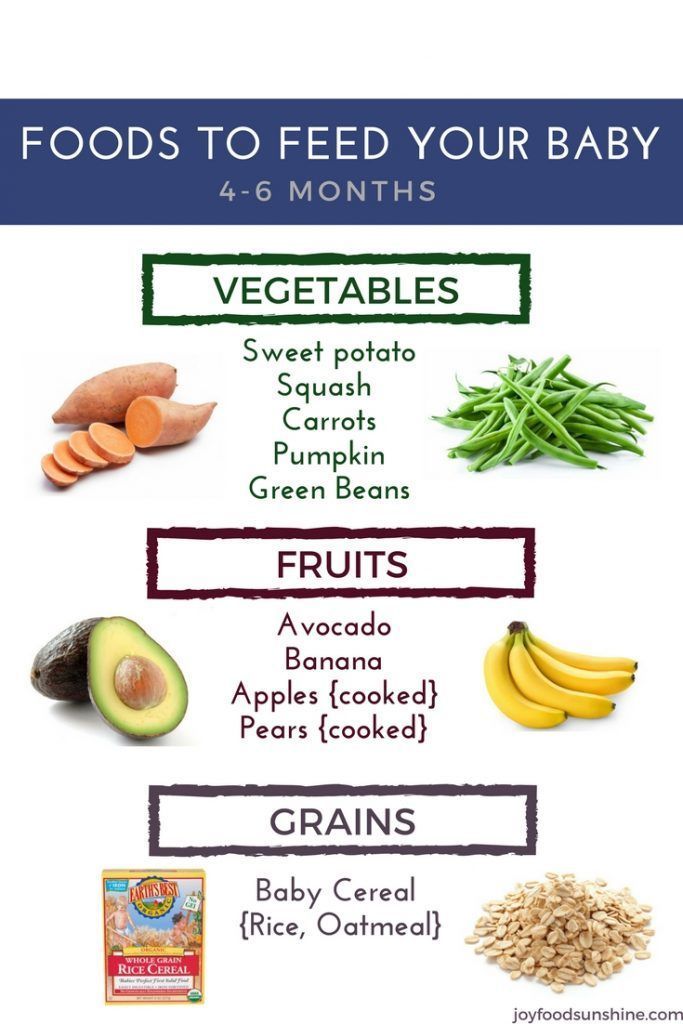 Topics include:
Topics include:
- Is your baby ready to start eating foods?
- What is a good first food for your baby?
- What to expect when introducing first foods
- How much should I feed my baby?
- How to win at mealtimeexternal icon
- What foods should my baby avoid?
- What should your baby eat in the first year?
Top of Page
Vitamins and Minerals
Vitamin and Mineral Fact Sheetsexternal icon
The National Institutes of Health’s Office of Dietary Supplements has fact sheets for consumers and health professionals about vitamins, minerals, and dietary supplements.
Top of Page
WHO recommendations for the introduction of complementary foods
08.08.2019
Readiness of the child to complementary foods According to the WHO recommendation, existing for 2018, it is optimal to introduce complementary foods to an infant at 6-8 months. Until six months, the baby's gastrointestinal tract is still not sufficiently formed, all the necessary enzymes are not produced for the assimilation of food other than mother's milk or formula.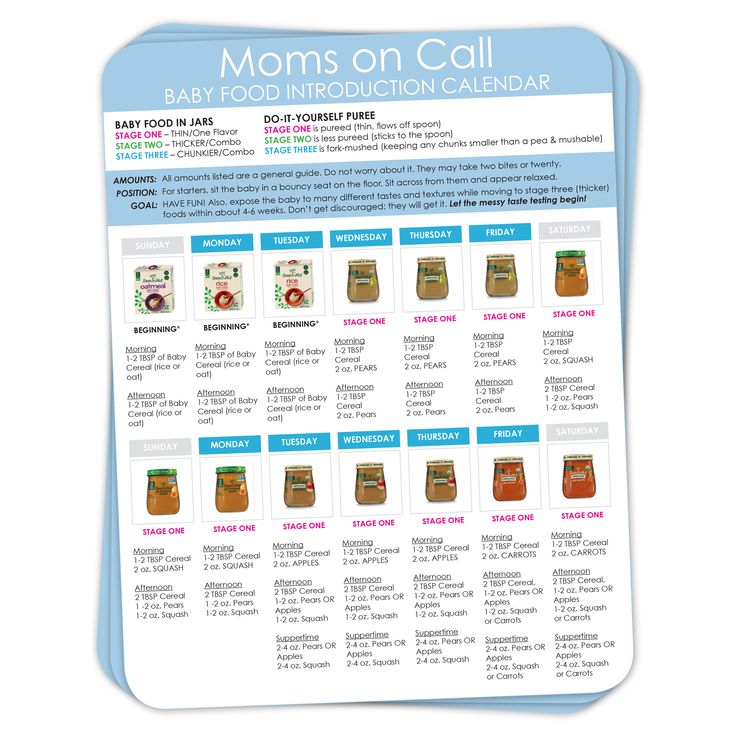 And by 9-10 months, the child can already form stable stereotypes of eating only liquid food, and overcoming them will be painful and difficult for the baby.
And by 9-10 months, the child can already form stable stereotypes of eating only liquid food, and overcoming them will be painful and difficult for the baby.
Thus, WHO defines the following signs of a child's readiness for the introduction of complementary foods: the maturity of the digestive system; extinction of the solid food ejection reflex; the appearance of the first teeth, making it possible to chew; the readiness of the baby to be stable in an upright position; emotional readiness for new tastes and sensations.
Complementary feeding system WHO has developed recommendations for three complementary feeding options: cereals, vegetables, and meat.
Fruit complementary foods are not recommended for cereals and vegetables. This is due to the fact that up to 8-9 months the gastrointestinal tract of the baby is not ready for the absorption of raw fruits and fruit juices. It is vegetables and cereals that will populate the intestines with the necessary bacteria for the absorption of fruits.
Kefir, according to the WHO, is not considered complementary foods because it is not a solid food. The WHO complementary feeding scheme includes kefir only as an additional food from 8 months. The introduction of cow's milk is recommended by WHO only from 12 months.
Any complementary feeding scheme assumes that portions of complementary foods will systematically increase from half a teaspoon to 100-200 g. The first dishes for complementary foods are prepared exclusively with one-component. Each next component is introduced only after complete addiction to the previous one (6-7 days).
Product sequence
The following sequence of introduction of complementary foods is proposed.
- Vegetables at 6 months.
- Porridges on the water (oatmeal, buckwheat, corn) at 6.5 - 7 months.
- Fruit puree, yolk at 8 months.
- Milk porridge at 8-9 months.
- Meat puree at 9 months.

- Meat by-products at 9-10 months.
- Kefir, cottage cheese, yogurt at 9-10 months.
- Fish at 10 months.
- Juice at 10-12 months.
- Berry puree at 12 months.
- Meat broths at 12 months.
The introduction of vegetable oil (olive, sunflower) in puree and porridge is allowed from 6 months: a scheme with 1 drop with a gradual increase to a volume of 1 teaspoon. The introduction of butter begins at 7 months: the scheme is from 1 g to 10 g in porridge.
For formula-fed babies, the first feeding schedule is similar, with a few exceptions. For these babies, it is better to introduce complementary foods from 5 months, because the milk mixture does not give the small body all the “building material”. The introduction of complementary foods differs only in terms: vegetable purees and cereals are introduced a month earlier.
First cereals
If the child's weight is significantly less than normal, WHO recommends starting complementary foods with non-dairy cereals.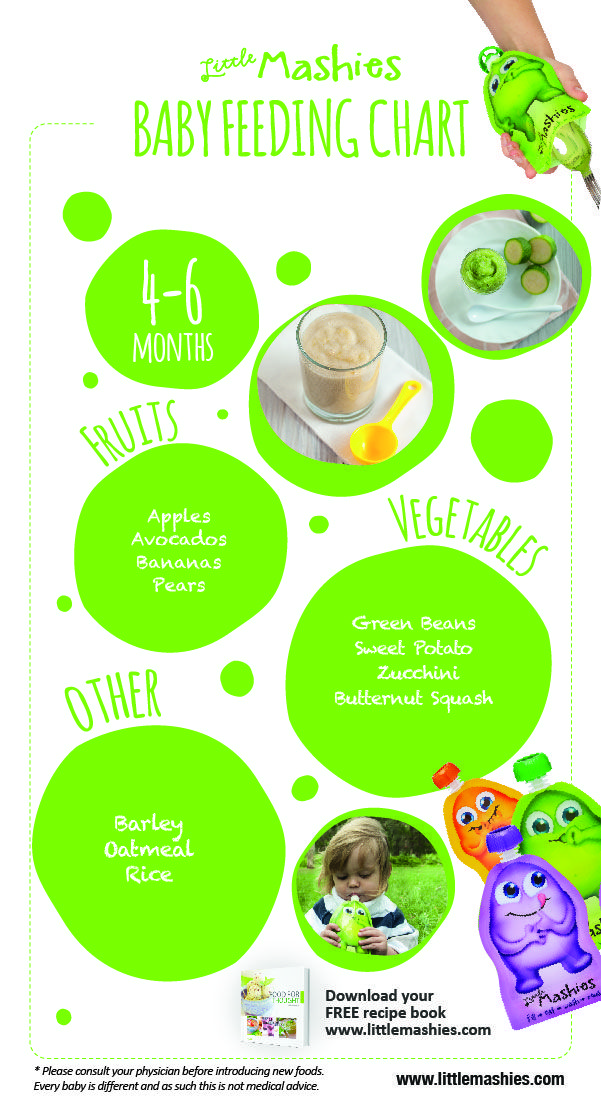 For babies, cereals are prepared only with non-dairy, unsalted, semi-liquid, absolutely homogeneous in consistency. The first cereals are prepared from cereal flour (the sorted and washed cereals are carefully ground and crushed).
For babies, cereals are prepared only with non-dairy, unsalted, semi-liquid, absolutely homogeneous in consistency. The first cereals are prepared from cereal flour (the sorted and washed cereals are carefully ground and crushed).
The following sequence of introduction of cereals is proposed: buckwheat, rice, corn, oatmeal, semolina. It is recommended to cook semolina porridge only once a week, because it contains practically no nutrients, but it is rich in gluten, which can cause problems in the intestines. Proportion for the preparation of the first porridge: 5 g of cereal flour per 100 ml of water. After slightly cooling the finished porridge, chop again. In the finished porridge, you can add 1-2 drops of vegetable oil or a little expressed breast milk.
From 9 months, the baby's nutrition system involves multicomponent cereals, from products already well known to the child. You can already add vegetables and fruits familiar to the baby to cereals. At 9 months, it is allowed to cook barley and millet porridge for babies. And by 10-11 months, cereals on the water will be a great addition to meat and fish meatballs and steam cutlets.
And by 10-11 months, cereals on the water will be a great addition to meat and fish meatballs and steam cutlets.
Vegetable food
The first purees are made from one vegetable.
The sequence of introducing vegetables into complementary foods for babies suggests the following order: zucchini, cauliflower, pumpkin, potatoes, carrots, green peas, beets. These vegetables are introduced within 6-9baby months. After 1 year, you can give your child cucumbers, eggplants, tomatoes, sweet peppers, white cabbage. After preparing the puree, make sure that the mass is completely homogeneous, there are no fibers and small particles, the consistency is semi-liquid. Don't salt. Add 1-2 drops of vegetable oil or expressed milk.
If the child refuses vegetable complementary foods, cancel this product for 1-2 weeks. Try to temporarily replace it with another and return to it after a while.
Meat supplements
From 9 months old, the first meat purees are recommended for babies.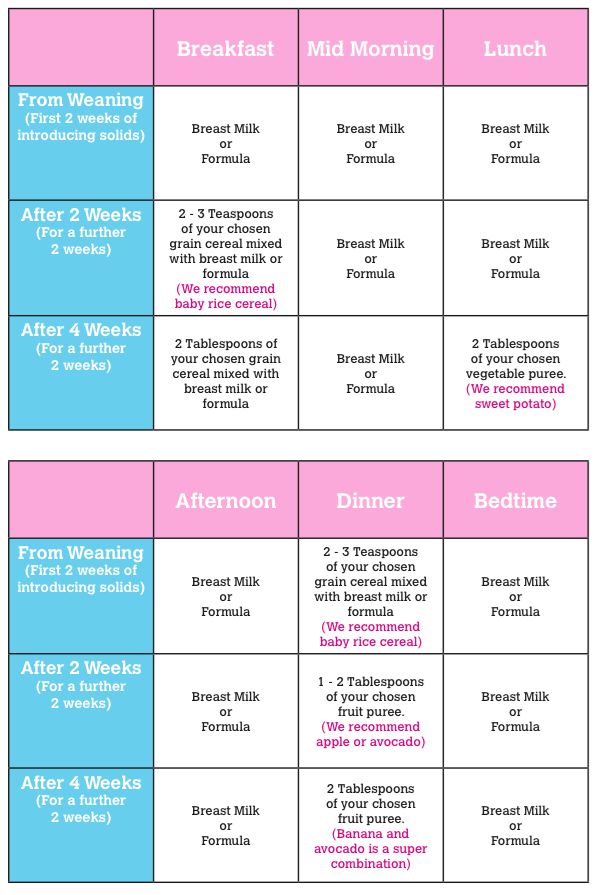 The first courses are recommended to be prepared from lean meats: rabbit; quail; turkey; chicken.
The first courses are recommended to be prepared from lean meats: rabbit; quail; turkey; chicken.
Complementary foods for a 6-month-old baby are recommended to be introduced in the morning. This will allow you to track the child's reaction to an unfamiliar product before a night's sleep: is there a rash, intestinal disorders, anxiety in the baby, profuse regurgitation. It is better to give vegetables or porridge first, and then saturate with breast milk or formula. Gradually, porridge and a vegetable dish will replace one full meal. The dish must be warm and freshly cooked. Gradually, by the age of 1, your baby will develop taste preferences. You will know what dishes he eats with pleasure. In the meantime, try to fully expand the child's diet with products necessary for growth and development.
Be healthy!!!
Union of Pediatricians of Russia
Introduction of complementary foods
How to introduce complementary foods correctly is one of the most pressing issues that concern parents.
In the first months of life, the main food for the baby is breast milk or an adapted milk formula, however, as the child grows and develops, this becomes insufficient and it is necessary to think about the introduction of complementary foods.
Your baby is over 4 months old. He has noticeably grown up, become more active, is interested in objects that fall into his field of vision, carefully examines them and reaches for them. The child's emotional reactions have become much richer: he smiles happily at all people, makes various sounds. Perhaps you notice that the child looks into your plate with interest, closely monitors what and how you eat, does this mean that it is time to introduce complementary foods? And where is the best place to start? Let's figure it out!
When should complementary foods be started?
According to the Program for optimizing the feeding of infants in the first year of life in the Russian Federation (2019), the recommended age for the introduction of complementary foods is in the range from 4 to 6 months.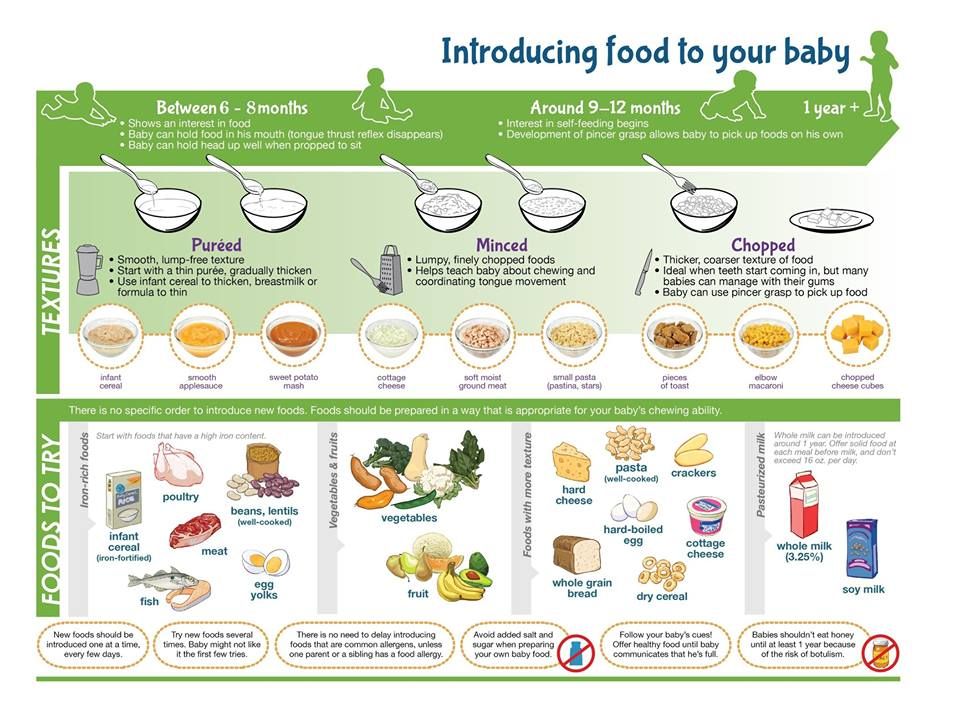
The following points will help determine the readiness of the baby for the introduction of complementary foods:
1. Food interest - you can check its presence as follows: during your meal, give the baby an empty spoon or fork, and if he plays with it, licks it, then there is no food interest yet; but if the child is dissatisfied with the fact that the spoon is empty, food interest has probably appeared. “But how does a child understand that there should be food in a spoon?” Parents often ask. The answer is quite simple: take your baby to the table with you so that he can see how you eat!
2. The child can sit alone or with support. It is unacceptable to feed the child lying down, because he may choke.
3. Extinction of the “pushing out” reflex - when the baby pushes out of the mouth both the offered food and the pacifier, etc.
Why is it not recommended to introduce complementary foods before 4 and after 6 months of life?
Before 4 months of life, the baby is not yet ready to digest food other than breast milk or infant formula.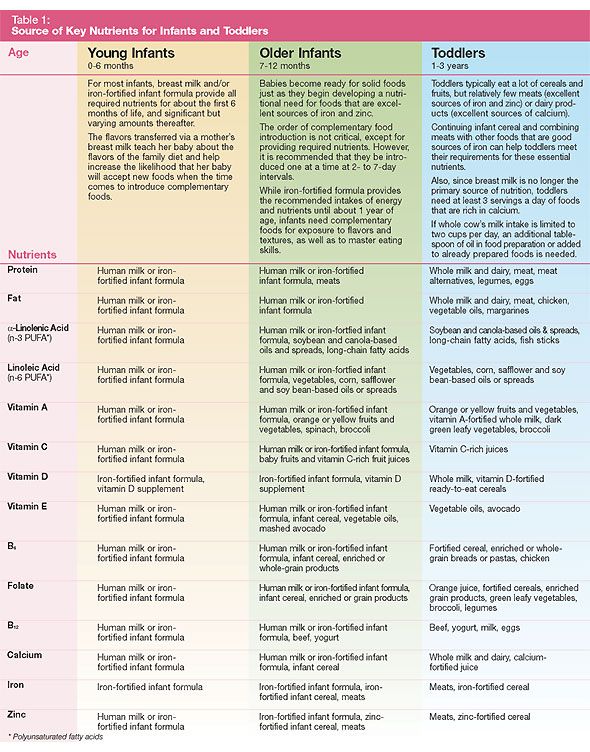 By this age, a number of digestive enzymes mature, a sufficient level of local immunity is formed, which reduces the risk of developing allergic reactions, the child acquires the ability to swallow semi-liquid and thicker food, which is due to the extinction of the “spoon ejection reflex”. The introduction of complementary foods after 6 months can cause a pronounced deficiency of micronutrients (iron, zinc, etc.) and lead to a delay in the formation of chewing skills for thick foods. Too late the introduction of a variety of products increases the risk of allergic reactions. Remember that the timing of the introduction of complementary foods is set individually, taking into account the readiness of the child to accept new foods.
By this age, a number of digestive enzymes mature, a sufficient level of local immunity is formed, which reduces the risk of developing allergic reactions, the child acquires the ability to swallow semi-liquid and thicker food, which is due to the extinction of the “spoon ejection reflex”. The introduction of complementary foods after 6 months can cause a pronounced deficiency of micronutrients (iron, zinc, etc.) and lead to a delay in the formation of chewing skills for thick foods. Too late the introduction of a variety of products increases the risk of allergic reactions. Remember that the timing of the introduction of complementary foods is set individually, taking into account the readiness of the child to accept new foods.
Complementary feeding guidelines:
1. introduce a new product in the first half of the day to track possible reactions to it;
2. cereals, vegetable / fruit / meat purees should be introduced, starting with monocomponent ones, gradually adding other products of this group;
3. start giving a new product with 1/2 teaspoon, gradually increasing the volume to the age norm within a week;
start giving a new product with 1/2 teaspoon, gradually increasing the volume to the age norm within a week;
4. It is not recommended to introduce new products during acute infectious diseases or at some special moments (moving to another apartment, leaving the city, on vacation, illness of parents, etc.).
What is the best way to start complementary foods?
The first complementary food can be anything. Often parents worry that if the child first tries the fruit, then because of its sweet taste, he will refuse other foods. We hasten to reassure you: breast milk is also sweet, so babies may like sweet fruits / berries more, but this does not mean at all that he will refuse vegetables or cereal. Traditionally, they begin to introduce complementary foods in the form of mashed potatoes, but if the child shows interest in “pieces”, then, observing the safety rules, you can give them. Also, along with the introduction of complementary foods, you can offer the child water.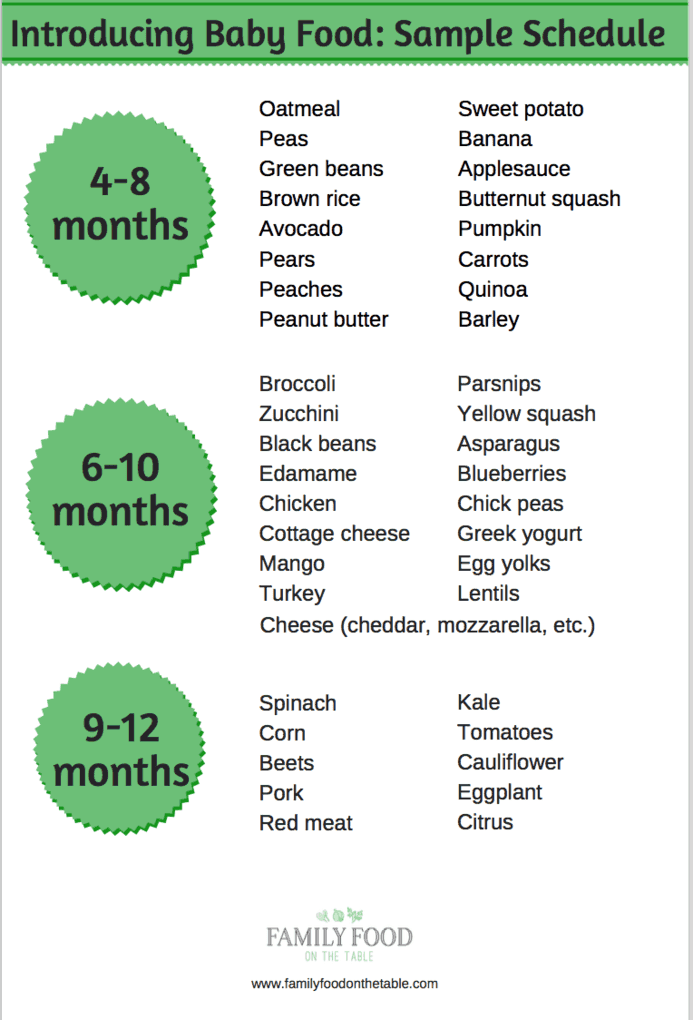
With the start of the introduction of complementary foods, the child is gradually transferred to a 5-time feeding regimen. If the baby shows that he is full and no longer wants to eat (for example, leaning back or turning away from food), then you should not continue to force him to feed, because this can lead to eating disorders in the future. Also, do not force the child to eat as much as possible before bedtime in the hope that he will not wake up for nightly feedings.
Traditionally, in our country, complementary foods begin with vegetables or cereals.
Vegetables: zucchini, broccoli, cauliflower, pumpkin, etc. If the child did not like the dish, for example, broccoli, do not give up on your plan and continue to offer this vegetable in small quantities daily, you can even not once, but 2-3 times, and after a while (7-14 days) the baby will get used to the new taste. This diversifies his diet, will help form the right taste habits in the child.
As for cereals, it is worth starting with dairy-free gluten-free ones - buckwheat, corn, rice.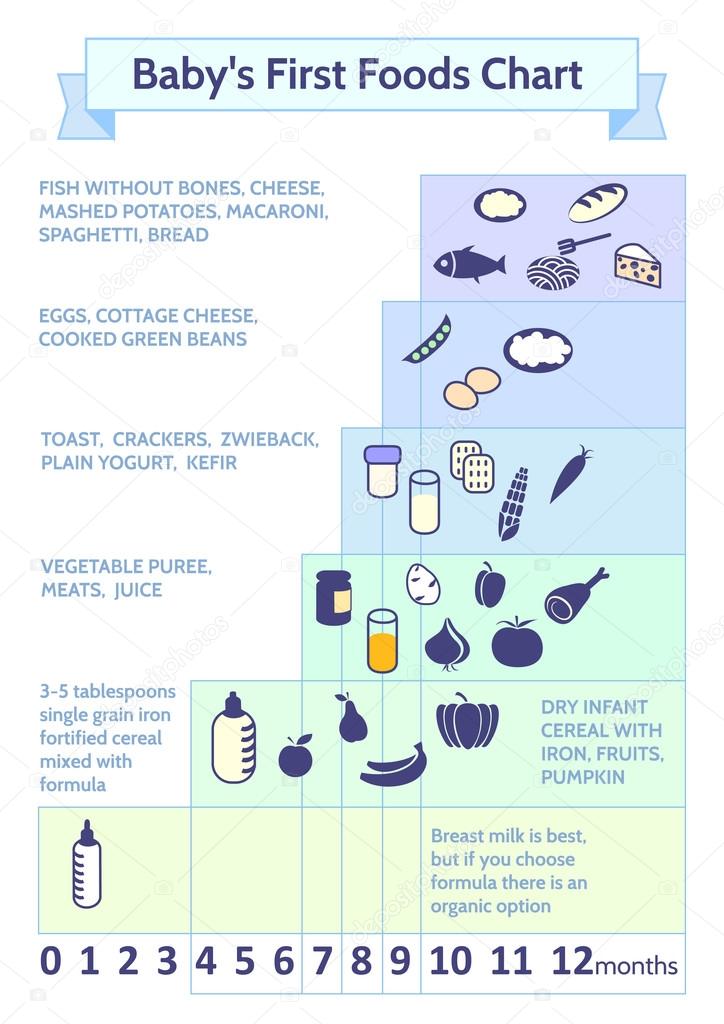 You can use commercial baby food porridge, which is enriched primarily with iron. In addition, such porridge is already ready to eat, you just need to dilute it with water, which will save you a lot of time.
You can use commercial baby food porridge, which is enriched primarily with iron. In addition, such porridge is already ready to eat, you just need to dilute it with water, which will save you a lot of time.
It is also recommended to add oil to food, for example, vegetable puree to vegetable puree, and butter to porridge.
Of meat products, lean meats, such as mashed turkey or rabbit, are most preferred to start complementary foods. Meat puree contains iron, which is easily absorbed, and adding meat to vegetables improves the absorption of this micronutrient from them. Subsequently, the daily use of children's enriched porridge and mashed meat allows you to meet the needs of babies for iron, zinc and other micronutrients.
When introducing fruit purees (apple, pear, peach, prunes, etc.) into your baby's diet, you should pay special attention to the composition of the product - it is important that it does not contain added sugar.
Fish is a source of easily digestible protein and contains a large amount of polyunsaturated fatty acids, including the omega-3 class, as well as vitamins B2, B12, and minerals. Preference should be given to oceanic fish, preferably white (cod, hake, pollock, sea bass, etc.), salmon can be recommended from red, and pike perch from river.
Preference should be given to oceanic fish, preferably white (cod, hake, pollock, sea bass, etc.), salmon can be recommended from red, and pike perch from river.
Fermented milk products are prepared using a special starter culture that breaks down milk protein, so that the baby can get an indispensable set of amino acids in a well-available form. Some foods have added prebiotics, certain vitamins and minerals. Their regular use favorably affects the functioning of the intestines, increases appetite and the absorption of micronutrients.
Recommendations and timing of the introduction of complementary foods for children at risk of developing food allergies and suffering from food allergies are the same as for healthy children. Delayed introduction of highly allergenic foods has previously been recommended to prevent the development of allergic diseases in children at risk. There is now evidence that this practice may lead to an increase rather than a decrease in the incidence of food allergies. The most common highly allergenic foods include cow's milk, chicken eggs, soybeans, wheat, peanuts, tree nuts, shellfish and fish. If a child has a high risk of developing allergies or an existing allergic disease, it is recommended to consult a pediatrician, an allergist-immunologist before introducing highly allergenic products.
The most common highly allergenic foods include cow's milk, chicken eggs, soybeans, wheat, peanuts, tree nuts, shellfish and fish. If a child has a high risk of developing allergies or an existing allergic disease, it is recommended to consult a pediatrician, an allergist-immunologist before introducing highly allergenic products.
By the age of 8 months, when all the main food groups have already been introduced and your baby is improving his skills to eat on his own, special attention should be paid to the diversity of the composition of dishes and the change in food consistency - from puree to finely and coarsely ground. Soft foods cut into small pieces (fruits, vegetables, meat, etc.) are perfect for a little gourmet, which diversifies his diet and will contribute to the formation of chewing skills.
By 9-12 months, most babies have the dexterity to drink from a cup (holding with both hands) and to eat foods prepared for other family members. This behavior needs to be encouraged, but combined with regular feeding to meet energy and nutrient requirements.
It is advisable to use industrial products that are designed specifically for young children after a year.
What should not be given to the baby?
It is not recommended to add salt or sugar to food to enhance the taste.
Drinks that should be avoided include fruit juices, whole cow and goat milk (whole milk is not recommended for children under one year old, and even longer, due to a high risk of developing iron deficiency and increased kidney stress), sweet fruit drinks, compotes and carbonated drinks.
Also, some foods should be excluded from the diet of infants: solid round foods (for example, nuts, grapes, raw carrots, raisins, peas, etc.), due to the fact that the child can choke on them.
It is not recommended to eat products with added sugar, for example, confectionery (marshmallow, marshmallow, marmalade, jam, jam, cookies, waffles, etc.), etc.
You should not give your child the meat of large predatory fish (shark, bigeye tuna, king mackerel, swordfish): these types of fish accumulate more harmful substances than others.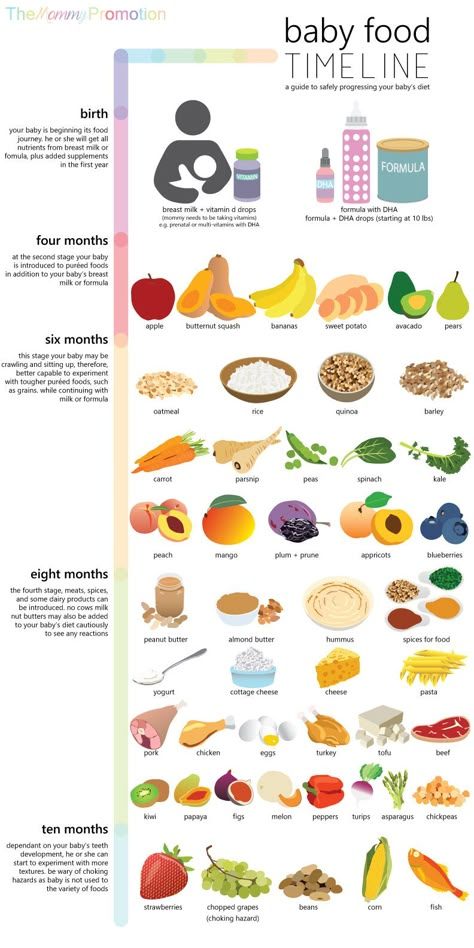
It is forbidden to give honey to children under one year old due to the fact that it may contain spores of Clostridium botulinum bacteria, which in the still immature digestive system of babies are able to multiply, produce toxins directly inside the intestines and, thus, cause infant botulism, which can be fatal. outcome.
Do not give babies raw meat, fish, eggs, caviar, salted fish, soft pickled cheeses because of the risk of intestinal infections.
If you follow all these simple rules, your baby will grow up healthy and happy!
Diets for different ages
References:
1. Methodological recommendations. The program for optimizing the feeding of children in the first year of life in the Russian Federation. [Internet]. - M.: Union of Pediatricians of Russia, 2019. [Methodicheskie rekomendaczii. Programma optimizaczii vskarmlivaniya detej pervogo goda zhizni v Rossijskoj Federaczii. [Internet]. – Moscow: Soyuz pediatrov Rossii, 2019.