Over feeding bottle baby
How To Tell If You're Overfeeding Baby
We spend so much time fussing over whether baby is getting enough formula or breast milk—and for new parents it can be hard to tell what’s actually enough. Many parents may try to coax baby to finish their bottle or worry that baby isn’t eating enough, when really, baby has just had their fill. So can that well-intentioned fussing possibly lead to overfeeding baby?
Keep in mind that signs of a healthy baby may differ across cultures. “Different cultures have different feelings about how much a baby should eat, how often they should eat and what they should look like,” says Alanna Levine, MD, a pediatrician at Orangetown Pediatric Associates in Orangeburg, New York. Some parents consider a roly-poly baby a sign of a job well done, while other parents see a round baby and visualize an obese teen.
While cultural perceptions of a healthy baby may vary, when it comes to feeding, there are few things to keep in mind. Read on to learn how overfeeding baby can happen, signs to look for and what to do going forward.
In this article:
Can you overfeed a baby?
What leads to overfeeding?
Signs of overfeeding baby
How to avoid overfeeding baby
Can You Overfeed a Baby?
You can probably breathe a sigh of relief: Overfeeding baby is almost impossible, and most of the anxiety over babies’ food intake and appearance is pointless. “If baby is gaining weight and growing and your pediatrician isn’t concerned, you don’t need to worry,” Levine says. Different babies grow at different rates and eat different amounts at different times.
Babies come with an incredibly sophisticated self-regulation system: When they’re hungry, they eat, and when they’re full, they stop. (Sadly, we’ve lost this mechanism by the time we become parents.) So when babies turn away from the bottle or breast and refuse to even consider another nip, they’re telling you they’re full. When baby keeps coming back for more, that’s a sign they’re truly hungry (even if they just finished a full six ounces!).
Overfeeding breastfed babies vs. formula-fed babies
Pediatricians Dina DiMaggio, MD, and Anthony F. Porto, MD, MPH, authors of The Pediatrician’s Guide to Feeding Babies and Toddlers, echo the importance of listening to your child’s cue, regardless of whether they’re breastfed or formula-fed. “We are often asked, ‘how come my child didn’t finish their bottle of formula?’ but are rarely asked that when children are breastfed.” (Probably because it’s a lot easier to see—and worry about—how much milk went into a bottle.)
On average, a full-term newborn drinks 2 ounces of formula per bottle every three to four hours, or breastfeeds on demand (about eight to 12 times a day), according to DiMaggio and Porto. At one month old, baby will likely drink 3 to 4 ounces of formula per bottle every three to four hours, while a breastfeeding baby may feed approximately seven or eight times a day. This pattern of baby drinking more ounces of formula or breastfeeding fewer times a day lasts until they are eight to 12 months old, at which point baby may drink seven to eight ounces of formula per bottle or breastfeed three to four times a day.
While these figures will vary with each child, it’s important to remember it’s perfectly normal for baby not to finish their bottle, as long as they’re hydrated and eating enough throughout the day. “Infants have a better understanding of when they’re full and, unlike most adults, don’t just eat whatever serving size is put in front of them,” DiMaggio and Porto say.
What Leads to Overfeeding?
Overfeeding baby is very rare, but it can happen. It’s more common in bottle-fed babies, simply because it’s easier for parents to see how much food their child is consuming. It also takes less effort to drink from a bottle, so babies (who love to suck) may inadvertently get too much milk while feeding.
If you’re concerned about possibly overfeeding baby, talk to your pediatrician. The doctor will look at baby’s length, weight and development, but as long as baby is thriving, they’re probably eating just fine.
Signs of Overfeeding Baby
The good news is, since you’ll likely be visiting a pediatrician often in first few months, you can track baby’s weight gain and feeding patterns. But don’t rely on weight as an indicator of whether you’re overfeeding baby. Instead, spitting up could be a sign you’ve pushed baby to take in extra food—for example, if baby spits up after draining a bottle you kept offering after they turned away. But more often than not, spitting up is a typical infant reaction or reflux.
But don’t rely on weight as an indicator of whether you’re overfeeding baby. Instead, spitting up could be a sign you’ve pushed baby to take in extra food—for example, if baby spits up after draining a bottle you kept offering after they turned away. But more often than not, spitting up is a typical infant reaction or reflux.
If you’re worried baby is eating too much for their age or has symptoms of vomiting, your pediatrician might recommend limiting how many ounces baby is drinking or how many times they feed, DiMaggio and Porto say. In most cases, however, as long as baby is healthy and doing well, feeding changes aren’t necessary.
How to Avoid Overfeeding Baby
If you learn you’ve been overfeeding baby, make a point of respecting your child’s feeding cues going forward. “If baby turns away before the bottle is finished or before your usual nursing time is up, accept the fact that they may not be hungry now,” Levine says. Don’t focus on the numbers: It doesn’t matter how many ounces baby finishes at each feeding.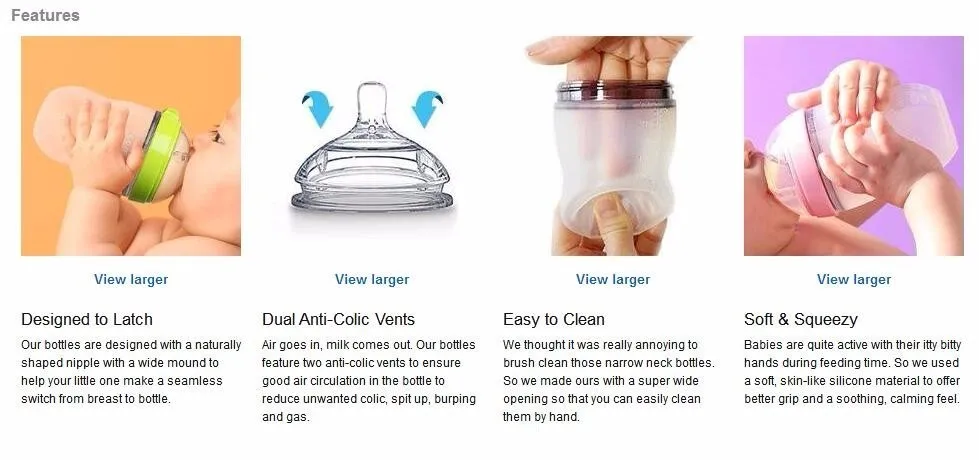 What matters is that baby is healthy and happy overall.
What matters is that baby is healthy and happy overall.
Updated February 2020
Expert bios:
Alanna Levine, MD, is a pediatrician at Orangetown Pediatric Associates in Orangeburg, New York, and works on staff at Englewood Hospital and Medical Center in New Jersey. In addition, she serves as a spokesperson for the American Academy of Pediatrics.
Dina DiMaggio, MD, and Anthony F. Porto, MD, MPH, are co-authors of The Pediatrician’s Guide to Feeding Babies and Toddlers: Practical Answers to Your Questions on Nutrition, Starting Solids, Allergies, Picky Eating and More, as well as spokespeople for the American Academy of Pediatrics. DiMaggio is a clinical assistant professor in the department of pediatrics at NYU Langone in New York City, and Porto is a pediatric gastroenterologist at Yale New Haven Health and medical director of the Yale Pediatric Celiac Program in New Haven, Connecticut.
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances. Plus, more from The Bump:
Your Ultimate Guide to How to Bottle-Feed a Baby
Breastfeeding 101: How to Breastfeed Baby
What You Need to Know About Baby Growth Spurts
Is My Baby Overfeeding? – Baby Care Advice
Infant overfeeding is a common problem, particularly for newborn bottle-fed babies. It’s a problem that is frequently overlooked because of the flawed assumption that only fat babies are overfed babies and because of false claims that it’s not possible to overfeed a baby. As a result, gastro-intestinal symptoms linked to overfeeding can be mistakenly attributed to conditions such as colic, reflux, or milk allergy or intolerance.
Overfeeding, also called over-nutrition, refers to a baby receiving more food than his stomach can hold and/or more nutrients than his intestinal tract is able to digest.
A baby could receive excess nutrients from large volume feeds or an accumulative effect of small volume feeds. Overfeeding can occur if baby receives regular strength infant formula or breast milk, or high-energy feeds.
A baby might overfeed due to circumstances that affect his ability to self-regulate his milk intake (decide for himself how much to eat). Or, he could be overfed as a result of being pressured to consume more milk than he needs.
Which babies are at risk of overfeeding?Newborn babies (birth to 3 months of age) are vulnerable to overfeeding due to developmental limitations that affect their ability to control their milk intake.
Bottle-fed babies are at increased risk of overfeeding because it’s harder for a baby to control the flow of milk and easier to pressure a baby to feed from a bottle compared to breastfeeding.
Overfeeding typically occurs due to a combination of the following reasons:
- Mistaking baby's hunger cues
Hunger is one of the first things blamed when a baby cries, has broken sleep, and when he indicates he wants to suck. A newborn baby crying or wanting to suck does not provided proof of hunger. Babies cry for many reasons, most of which have nothing to do with hunger. Babies are in an oral stage of development and gain comfort from sucking. Most babies enjoy sucking when they’re hungry, tired, bored, uncomfortable, upset, and for pleasure.
If a baby’s behavioral cues are misread, it means he’s going to be offered feeds at times when he’s not hungry.
- Active sucking reflex
Babies under the age of 3 months have an active sucking reflex. The sucking reflex is triggered by pressure on baby’s tongue and roof of his mouth by the nipple of a feeding bottle, his mother’s nipple, a pacifier, his fist or fingers, or a parent’s finger. A reflex is an automatic, involuntary action. When a baby’s sucking reflex is triggered he will suck because it is an involuntary reaction.
A reflex is an automatic, involuntary action. When a baby’s sucking reflex is triggered he will suck because it is an involuntary reaction.
An active sucking reflex means a newborn has limited ability to control the flow of milk from a bottle or stop when he has had enough. He may appear to hungrily guzzle down the milk, but will do so regardless of whether he’s hungry or not.
- Baby feeds too quickly
It takes time for our brain to register the sensation of satisfaction that occurs after eating a meal in both adults and babies. The faster a newborn feeds the greater the risk he may overfeed.
The nipple speed (determined by the size of the hole) and baby’s sucking ability influence how quickly milk flows from through the nipple. Babies vary considerably in their strength and sucking ability. Just because a nipple is designed for babies of a specific age group doesn’t guarantee that it’s a suitable speed for an individual baby. (See How long should a bottle-feed take.)
(See How long should a bottle-feed take.)
- Overlooking or ignoring satiety cues
Satiety means a baby’s hunger is satisfied. When a baby has had enough to eat he will stop sucking. If he’s over the age of 3 months, he might also push the nipple out with his tongue, clamp his lips together, turn his head away, arch back or push the bottle away.
A caregiver might overlook or ignore baby’s cues of satiety in an attempt to encourage him to drink a pre-determined volume of milk. It’s not difficult to make a baby eat more than he wants while his sucking reflex is active.
- Overestimation of baby's milk requirements
Calculations used by health professionals to estimate babies’ milk needs are based on averages. Such figures do not take into account the many reasons why an individual baby might require less milk than average. (See How much milk does baby need for reasons).
Overestimation of a baby’s milk requirements will not cause overfeeding unless the parent tries to make baby drink the overestimated amount, which is a natural response when a parent has been led to believe their baby needs that amount. Parents are often told or may get the impression that the estimated amount is a ‘should have’ or ‘must have’ target. As a result many parents overlook or ignore their baby’s satiety cues and try to make their baby consume the recommended amount.
Parents of preterm babies are often taught to believe they must control how much their baby eats. Something they may have needed to do when their baby was very young and weak, but not forever. They need to allow baby to decide how much his body needs by the time he is 8 weeks adjusted age or younger. They're not the only parents who believe they need to make sure their bottle-fed baby eats ‘enough’ (usually an amount decided by others and not baby). This is a flawed belief when you consider that breastfed babies don’t need others to decide how much they 'should' or 'must' eat.
- Babies that drink high-energy milk
High-energy milk means it contains more calories in less volume compared to normal strength infant formula or breast milk, which provides 20 kCal per ounce. Nutrients and calories might be increased as a result of adding extra scoops of formula, a milk fortifier, oils, carbohydrates, rice cereal or oatmeal. Or it could be a commercially produced high-energy formula, which range from 22 to 30 kCal per ounce.
Providing high-energy feeds makes it easier for weak or sick babies to get the calories they need with less effort. However, high-energy feeds also make it easier for a healthy newborn to overfeed or be overfed.
- Parent’s opinion of a ‘healthy’ baby
Many parents and cultures consider chubbiness in infancy to be a sign of good health. A parent might try to pressure their baby to drink more than he’s willing to drink in order to ‘fatten him up’, or make him grow faster or bigger. Small babies and lean babies are at greater risk of being pressured to eat compared to others. However, chubby, overweight babies are at increased risk of having their milk needs overestimated using standard calculations that estimate milk requirements based solely on age and weight.
Small babies and lean babies are at greater risk of being pressured to eat compared to others. However, chubby, overweight babies are at increased risk of having their milk needs overestimated using standard calculations that estimate milk requirements based solely on age and weight.
- Babies that have broken sleep
Feeding and sleeping are closely linked. A baby’s sleeping pattern will influence his feeding pattern. Short naps usually mean short intervals between feeds.
Broken sleep means baby wakes before his sleep needs are met. If he wakes too soon, it won’t be long before he becomes irritable due to tiredness. Baby's tired cues, which involve fussing, crying and desire to suck, are commonly mistaken as hunger.
A major reason for babies to experience broken sleep is because they often learn to rely on negative sleep associations as a way to fall asleep. Because parents in general are unaware of the effects of sleep associations on their baby’s ability to sleep, some assume baby is waking because of hunger. And as a result, they overlook or ignore their baby's satiety cues while trying to make him drink larger volumes. Others add cereal to their baby’s milk mistakenly believing more nutrients will make him sleep longer.
And as a result, they overlook or ignore their baby's satiety cues while trying to make him drink larger volumes. Others add cereal to their baby’s milk mistakenly believing more nutrients will make him sleep longer.
- Feeding-sleep association
If a baby regularly falls asleep while feeding, feeding can become a sleep association. When a baby has learned to rely on feeding as a way to fall asleep he will appear hungry whenever he’s tired and ready to sleep. He may also want to feed as a way to return to sleep if his sleep is broken.
A feeding-sleep association makes it difficult for a parent to tell the difference between baby’s hunger and tiredness cues.
How a baby's body responds to overfeedingWhile the nutrients consumed as a result of overfeeding exceed the amount a baby needs for normal growth this won’t automatically cause large weight gains.
Our bodies have thousands of homeostatic mechanisms that automatically act to maintain an internal state of balance or harmony. These compensate or minimize the effects of overfeeding in multiple ways. Two examples include:
These compensate or minimize the effects of overfeeding in multiple ways. Two examples include:
- When baby drinks too much
A baby’s stomach will expand as he eats and contract as food slowly empties into his intestinal tract. However, there are limits on how far it can stretch. If stretch receptors in the lining of baby’s stomach stretch beyond a normal range, he will regurgitate (reflux) his stomach contents - ranging from small spit ups to large projectile vomits - during or shortly after the feed has ended
If an overfed baby regurgitates large amounts of milk he may be spared from the effects of over-nutrition. If not, excess nutrients will pass into this intestinal tract where other homeostatic mechanisms take action.
- When over-nutrition occurs
A baby’s immature digestive system has a limited ability to produce digestive enzymes within a specific time period. A healthy baby can digest enough nutrients for healthy growth but his intestinal tract might not be able to digest an excess of nutrients.![]() If nutrients are not digested (broken down by digestive enzymes) they cannot be absorbed into his blood stream, and therefore the energy (calories) from undigested nutrients is not stored as body fat. Instead undigested nutrients pass through his intestinal tract and are pooped out.
If nutrients are not digested (broken down by digestive enzymes) they cannot be absorbed into his blood stream, and therefore the energy (calories) from undigested nutrients is not stored as body fat. Instead undigested nutrients pass through his intestinal tract and are pooped out.
In the case of overfeeding, you might observe your baby display the following signs and symptoms:
Gastric symptoms- milk regurgitation due to hyper-extension of baby’s stomach;
- belching due to swallowing large amounts of air while speed-feeding.
- frequent sloppy, foul smelling bowel motions if baby is formula-fed, or watery, explosive bowel motions if baby receives breast milk;
- extreme flatulence;
- intestinal spasms or cramps (baby often fusses, cries or grunts while bearing down like he's trying to poop).
These intestinal symptoms occur as a result of fermentation of undigested lactose in baby’s large intestine. (See Lactose overload for more).
(See Lactose overload for more).
- irritability;
- sleep disturbance.
When a baby’s stomach is stretched beyond a normal range and/or when his intestinal tract is churning in an attempt to deal with an excess consumption of nutrients, is it any wonder that he would be irritable and have trouble sleeping.
These signs and symptoms primarily relate to baby’s homeostatic mechanisms doing exactly what they’re designed to do – correct the imbalance between what baby needs and what he receives. While the actions of homeostatic mechanisms can cause a baby varying degrees of physical discomfort, they protect him from greater harm that would occur from an excessive accumulation of body fat.
Baby's growthA baby’s current weight or weekly weight gain is not a good indicator of overfeeding. An overfed baby could be underweight, overweight or within a normal weight range.
Homeostatic mechanisms explain why an overfed baby doesn’t necessarily gain large amounts of weight.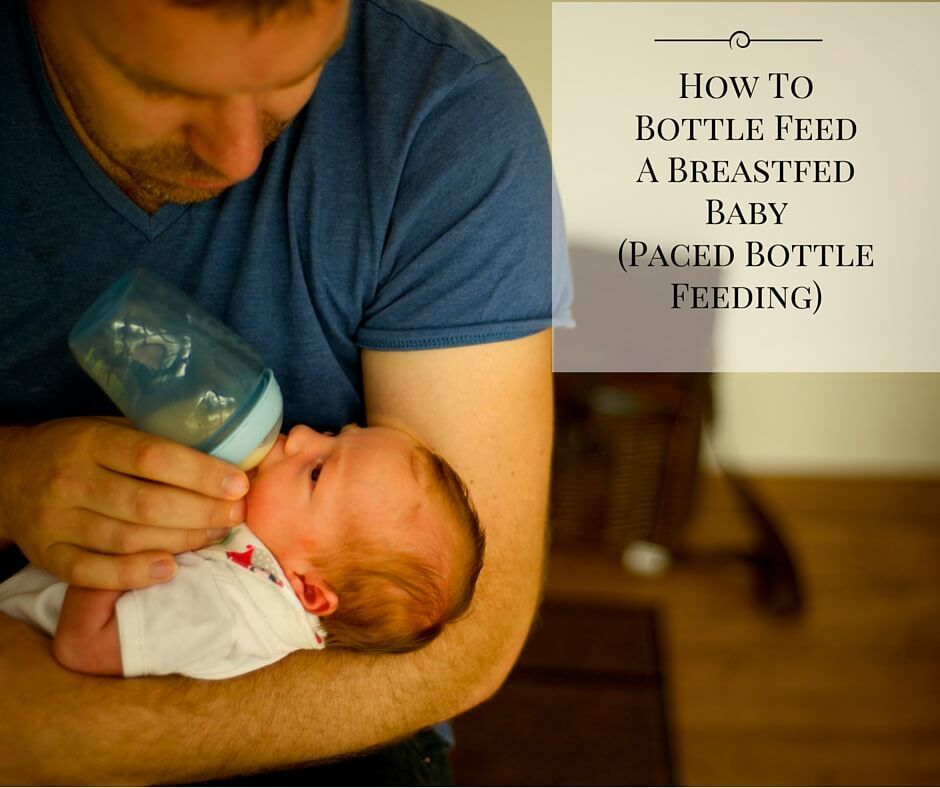 A baby could overfeed and his weight gains consistently remain within a normal range.
A baby could overfeed and his weight gains consistently remain within a normal range.
Some babies are naturally inclined to accumulate body fat more readily than others. Others may gain large amounts of weight because their homeostatic mechanisms are unnaturally prevented from working by certain medications and dietary changes (explained below). As a result some overfed babies lay down large stores of body fat which cause them to become overweight or obese. However, an overweight or obese baby is not necessarily overfeeding or overfed at the present time. He might have gained large stores of fat in the womb or as a result of previous overfeeding. So it can’t be assumed a baby is currently overfed simply because he’s overweight.
An overfed baby could display slow or poor growth as a result of extreme milk regurgitation or vomiting. When an overfed baby throws up, the amount won’t necessarily be limited to the excess. Once reflux or vomiting mechanisms are triggered, he could all but empty his stomach. In some cases where babies overfeed, less is more. Less milk -> less vomiting -> better growth.
In some cases where babies overfeed, less is more. Less milk -> less vomiting -> better growth.
A baby could overfeed and yet gain less than expected weight in the case of catch-down growth – a normal variation of growth that is often mistaken as poor growth.
How to prevent overfeeding your babyThe goal is to support your baby to self-regulate his milk intake. You can achieve this in the following ways:
- Check that your expectations of your baby’s milk requirements are realistic. See How much milk does a baby needs.
- Check that your baby is not feeding too quickly. See How long should a bottle-feed take. If necessary slow down feeds by switching to a slower nipple.
- Follow a semi-demand feeding pattern to minimize the risk of misinterpreting his hunger cues. (See feeding patterns for bottle-fed babies.)
- Learn to recognize your baby’s cues that indicate he has had enough. Don’t try to make him drink more than he’s willing to drink.
 Never pressure your baby to feed.
Never pressure your baby to feed. - Check that your baby is getting enough sleep. See How much sleep do babies need? If he’s not getting close to average sleep for age, then find out if this could be due to a sleep association. See my book ‘Your Sleepless Baby’ for strategies on how to promote healthy sleep habits.
- Discourage a feeding-sleep association by preventing your baby from falling asleep while feeding.
- Satisfy your baby’s desire to suck using means other than feeding. Offer him a pacifier or your finger for him to suck on. If he’s hungry, he will let you know. He won’t be content to suck on a pacifier or your finger.
- Don't assume he's hungry every time he fusses, cries or wants to suck. If its too early for a feed try other soothing methods first, but feed if they aren't working.
Don’t restrict your baby’s milk intake. Dietary restriction is a band-aid solution because it doesn’t address the underlying reasons for overfeeding to occur. It’s not your role to decide how much your baby should drink. That’s his job. Your job as your baby’s caregiver is to remove any barriers (such as those described in 'Why babies overfeed' section) which might cause him to overfeed.
It’s not your role to decide how much your baby should drink. That’s his job. Your job as your baby’s caregiver is to remove any barriers (such as those described in 'Why babies overfeed' section) which might cause him to overfeed.
Gastro-intestinal symptoms associated with overfeeding are often misdiagnosed as colic, reflux, milk protein allergy or intolerance, lactose intolerance or gastroparesis (delayed gastric emptying).
Reasons for misdiagnosis include:
- The possibility of overfeeding is not considered unless baby is overweight or gaining excessive amounts of weight. Even then, overfeeding can be overlooked as a cause of a baby’s gastro-intestinal symptoms.
- Parents are not asked about their baby’s milk intake, feeding and sleeping patterns, or their infant feeding and settling practices. So the common reasons for overfeeding described under 'Why babies overfeed' are not assessed and therefore not addressed.
- Medical doctors are not trained to advise parents on behavioral strategies to prevent overfeeding. They're trained to diagnose medical conditions based on symptoms; so that’s what they do.
In the absence of knowledge regarding behavioral causes for healthy babies to display gastro-intestinal symptoms (described in this article) assumptions are made and misdiagnoses occur. As a result, parents don’t receive effective advice on how to adjust their infant feeding practices to prevent overfeeding; instead baby receives medical treatment.
Medical treatmentsMedical treatments do not cure conditions such as colic, reflux, milk allergy or intolerance, or gastroparesis (or problems such as overfeeding). The purpose of treatment is to relieve the symptoms associated with these conditions, i.e. reduce milk regurgitation; neutralize acid reflux; minimize intestinal gas; relieve discomfort due to intestinal spasms, normalize bowel motions and alleviate discomfort assumed to occur as a result of these conditions.
Colic is often, but not always, the first problem blamed for an overfed baby’s distress and intestinal symptoms.
Medications to treat colic:-
- Colic remedies containing symethicone can help a baby burp up swallowed air that occurs while feeding, but has no effect on other symptoms associated with overfeeding. Other over-the-counter colic mixtures have minimal or no effect on overfeeding symptoms.
- Antispasmodic medications such as dicyclomine and hyscyamine can relieve intestinal spasms associated with over-nutrition.
- Antihistamines like diphenhydramine have a mildly sedative effect that may reduce baby’s irritability.
Antispasmodics or antihistamines require a doctor’s prescription because they can have serious side effects. (See Colic medications for more.)
DIAGNOSIS 2: RefluxAn overfed baby might be diagnosed with reflux (gastro-esophageal reflux disease or GERD) if he regurgitates milk or ‘silent reflux’ if he doesn’t. Either way it’s assumed his distress is due to burning effects of regurgitated acidic stomach contents.
Either way it’s assumed his distress is due to burning effects of regurgitated acidic stomach contents.
Medications to treat acid reflux:-
- Acid suppressing medications such as ranitidine, omeprazole or lansoprazole, might have a small effect on symptoms associated with overfeeding. Because lack of stomach acid hinders the breakdown of proteins in the stomach, these meds can slow down gastric emptying time (the time it takes for milk to empty from the stomach). This means nutrients empties into the intestinal tract slowly and as a result may reduce intestinal symptoms associated with over-nutrition. (More time enables more nutrients to be digested.) (See Antacid medications for more.)
If medications make no noticeable difference to baby’s symptoms, milk allergy or intolerance might be the next diagnosis he receives.
Dietary change to treat milk protein allergy or intolerance:-
- Lactose-fee formulas, which includes cows’ milk based formula with lactose removed, soy infant formulas and hypoallergenic formulas, can relieve intestinal symptoms because an absence of lactose eliminates the possibility of lactose overload symptoms occurring in baby’s large intestine.

- Lactose-reduced formulas, for example anti-colic and AR formulas, can reduce intestinal symptoms by reducing lactose overload symptoms.
- Food thickeners added to a baby’s milk or already in AR formulas can reduce milk regurgitation. Because they slow down gastric emptying time and intestinal motility (the speed which food and waste travels through the intestinal tract) they can reduce intestinal symptoms linked to over-nutrition.
- High-energy feeds can reduce milk regurgitation but may increase intestinal symptoms due to over-nutrition.
- Maternal dietary restrictions. Breastfeeding mothers may be advised to eliminate dairy and other specific foods from their diet. This will have no effect on the symptoms caused by overfeeding.
If acid suppressing medications and dietary changes fail to make a difference, baby might then be diagnosed with gastroparesis.
Medications to treat gastroparesis:-
- Prokinetics medications, such as domperidone and erythromycin (which is also an antibiotic), speed up gastric and intestinal motility. In the case of overfeeding, these can reduce milk regurgitation but may increase intestinal symptoms.
Medications and dietary change have varying effects on gastro-intestinal symptoms that occur in response to overfeeding and over-nutrition. Some have no effect. Others reduce some symptoms but increase others. The reason these treatments reduce or increase gastro-intestinal symptoms is because they hinder or enhance the actions of a baby’s homeostatic mechanisms.
Even when medications appear to help, symptoms will return once the effect wears off. While a baby receives medications he’s exposed to the potential of unwanted side effects directly linked to the medications or indirectly linked as a result of inhibiting or enhancing the actions of his homeostatic mechanisms. (See Colic medications and Antacid medications for more.)
(See Colic medications and Antacid medications for more.)
None of these treatments address the underlying cause of symptoms. Failure to address the cause can result in multiple diagnoses, multiple medications and dietary changes.
Fix the problem and not the symptoms! Prevention of overfeeding trumps medical treatments that mask the symptoms.
Written by Rowena Bennett
© Copyright www.babycareadvice.com 2020. All rights reserved. Permission from author must be obtained to reproduce all or any part of this article.
Baby won't take a bottle | Philips Avent
search support iconSearch Keywords
Home ›› What to do when your baby refuses a bottle
↑ top
any problems. If your breastfed baby refuses a bottle, don't worry. This is a common occurrence in many babies who are used to breastfeeding. Obviously, this can create certain difficulties for moms, especially if you need to return to work in the near future.
3 Philips Avent products to help you bottle feed:
So why is your baby refusing to bottle and crying? There are many ways to quickly and easily teach a breastfed baby to a bottle. Here are important tips on what to do when your baby refuses a bottle.
Is the baby refusing the bottle? Take a step back
If your baby cries while bottle feeding, the first thing to do is to start over and rethink your feeding approach and technique. Try the following steps when bottle feeding your baby: [1]
- Lift and tilt your baby's head forward. Before inserting the pacifier into the baby's mouth, make sure that the baby's head is raised and tilted over his body to avoid choking: so that the baby does not choke and have the opportunity to burp during bottle feeding.
- Insert the pacifier. Bring the pacifier to the baby's lips and gently guide it into the baby's mouth. In no case do not try to press the nipple on the baby's lips and try to push it into his mouth.
 After touching the pacifier to the baby's lips, wait for the baby to open his mouth and take the pacifier.
After touching the pacifier to the baby's lips, wait for the baby to open his mouth and take the pacifier. - Hold the bottle at an angle. Tilt the bottle at an angle so that the nipple is only half full. So the child can eat at his own pace.
- Let the baby burp during and after feeding. It can be useful for a child to burp not only after feeding, but also approximately in the middle of the process. This will help reduce gas or tummy discomfort that your baby may experience from swallowing too much air.
- Stop in time, do not overfeed the baby. If the baby begins to turn his head away from the bottle or closes his mouth, then he is full and you need to stop feeding.
- Perhaps the flow of milk from the nipple to the baby is weak or, on the contrary, too fast, so he is naughty and refuses the bottle. Try changing the nipple to a nipple with a different flow.
Other tips if your baby refuses the bottle
If you've followed the steps above and your baby still refuses the bottle, don't worry. There are other ways to help bottle feed your baby. Here are some simple tricks you can add to your bottle feeding process. [2]
There are other ways to help bottle feed your baby. Here are some simple tricks you can add to your bottle feeding process. [2]
1. Remind your child about mom.
Sometimes a child can be fed by someone other than his mother - dad, grandmother or, for example, a nanny. If your baby fusses while bottle feeding, try wrapping the bottle in something that smells like mommy, like a piece of clothing or some fabric. This will make it easier to feed the baby when the mother is not around.
2. Try to maintain skin contact while bottle feeding.
Some babies need contact with their mother, so try bottle feeding while leaning against you. However, some babies are better at bottle feeding when they are in the exact opposite position than when they are breastfed. For example, there is a position with bent legs. Lay the child on your bent knees, facing you, pointing the child's legs towards your stomach. During feeding, the baby will be able to look at you and contact you in this way. If your baby refuses a bottle, experiment to see which works best.
During feeding, the baby will be able to look at you and contact you in this way. If your baby refuses a bottle, experiment to see which works best.
3. Move while feeding.
Sometimes all it takes to get your baby to take the bottle is a little wiggle or walk. The next time your baby starts crying while bottle feeding, try moving around a little rhythmically to calm him down.
4. Try changing the milk temperature.
If the baby still does not want to take the bottle, check if the milk in the bottle is too hot or too cold. Before feeding, put some warm breast milk on the inside of your wrist to check the temperature. Milk should be warm, but if it seemed hot to you, just place the bottle for a short while under a stream of cold water.
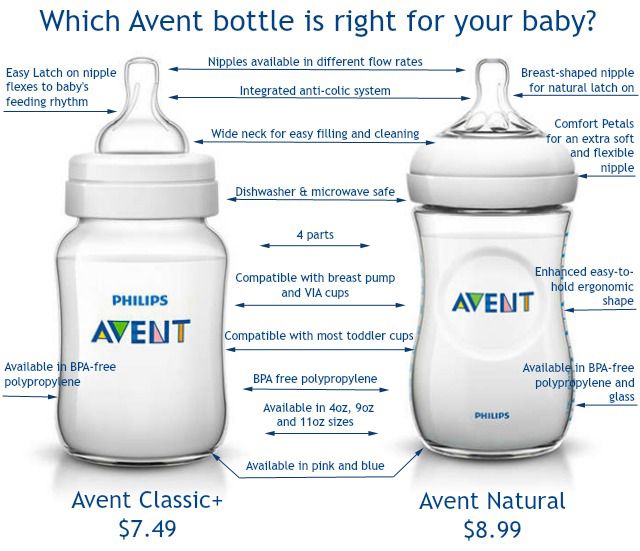
Choosing the right bottle for your baby If you plan to combine bottle feeding with breastfeeding, it is advisable to choose bottles with a nipple that will have a wide base as the bottle will grip closer to the breast.
 Also pay attention to the fact that the nipple is firm and flexible, the child must make an effort to drink from the bottle, as well as from the breast. Give preference to nipples with an anti-colic valve that vents air out of the bottle.
Also pay attention to the fact that the nipple is firm and flexible, the child must make an effort to drink from the bottle, as well as from the breast. Give preference to nipples with an anti-colic valve that vents air out of the bottle. Natural bottle allows you to combine breast and bottle feeding. 83.3% of babies switch from a Natural bottle to breastfeeding and back.*
If you choose a bottle for artificial feeding, traditional bottles are fine, but it is desirable that the nipple is made of a hypoallergenic material, such as silicone, has an anti-colic valve and did not stick together when bottle fed. In case your baby spit up often, then use special bottles with anti-colic and anti-reflux valve, which reduces the risk of spitting up and colic.
Bottle with unique AirFree valve reduces the risk of colic, gas and spitting up. With this bottle, you can feed your baby in an upright or semi-upright position to reduce spitting up. Due to the fact that the nipple is filled with milk and not air during feeding, the baby does not swallow air, which means that feeding will be more comfortable.
Both bottles are indispensable if you want to breastfeed, bottle feed or just bottle feed your baby.
“My baby refuses to breastfeed but bottle feeds – help!”
Sometimes a baby gets used to bottle feeding and refuses to breastfeed. Therefore, it is important to use bottles that are suitable for combining breastfeeding with bottle feeding. If, nevertheless, you are faced with the fact that the child refuses to take the breast, try using silicone nipple covers to make the transition from the bottle to the breast and back more imperceptible.
Remember that if you want to combine breastfeeding and bottle feeding, it is worth waiting at least a month before offering a bottle, so that you are lactating and have time to get used to each other and develop a breastfeeding regimen.
Breastfeed and bottle feed your baby with pleasure
Remember that it takes a while for your baby to get used to bottle feeding. This is completely normal. If you have to go to work, be sure to set aside enough time to bottle train your baby beforehand.
This is completely normal. If you have to go to work, be sure to set aside enough time to bottle train your baby beforehand.
Remember that every child is different, so what works for one may not work for another. With a little time and patience, you will find out what works best for your baby when he refuses a bottle.
You will identify your child's unique needs. However, if your baby still refuses the bottle after all the steps above, check with your pediatrician.
Articles and tips from Philips Avent
References:
*O.L. Lukoyanova, T.E. Borovik, I.A. Belyaeva, G.V. Yatsyk; NTsZD RAMS; 1st Moscow State Medical University THEM. Sechenova, "The use of modern technological methods to maintain successful breastfeeding", RF, 10/02/2012 3 llli.org - The Baby Who Doesn't Nurse
llli.org - Introducing a Bottle to a Breastfed Baby
Baby+ app
Download the app and track your child's development and growth with trackers and save those special moments forever.
Download app:
You are leaving the Philips Healthcare (“Philips”) official website. Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain.
I understand
You are about to visit a Philips global content page
Continue
You are about to visit the Philips USA website.
I understand
How to bottle feed properly
Feeding your baby is not only important for healthy growth and development, but also a way to establish close emotional contact with the baby and build trusting and loving relationships. The transition from breastfeeding to bottle feeding should be carried out after the mother and the child are fully prepared for this. We are talking about both the moral aspect, and about choosing the right bottle and getting adults the necessary skills so that eating brings only positive emotions and benefits to the baby. In this article, we will talk more about how to properly bottle feed your baby and where to start.
In this article, we will talk more about how to properly bottle feed your baby and where to start.
How to prepare your baby for bottle feeding
If this way of eating is a completely new experience for the baby, or if parents decide to bottle feed their baby from a very young age, then slow flow teats should be preferred. So you protect the child from the possibility of choking while eating. Over time, you can gradually switch to bottles with nipples, which would provide faster and more intense feeding.
Feeding bottle selection and daily care
All baby accessories should be kept clean and sterilized regularly and thoroughly.
There are several ways to sterilize dishes:
- select the appropriate mode when using the dishwasher;
- or place the bottle and teat in a vessel of boiling water for 5 minutes.
Before using this method of cleaning the bottle, make sure that the material it is made of can be exposed to high temperatures. Since some types of plastic contain various chemicals in their composition, after sterilization they can become dangerous for their little user. For this reason, experts recommend choosing glass bottles.
Since some types of plastic contain various chemicals in their composition, after sterilization they can become dangerous for their little user. For this reason, experts recommend choosing glass bottles.
The need for thorough cleansing of everything that the baby will touch is caused by the fact that in the first months of life, the child's immune system is just beginning to strengthen. Before sterilizing the teat, it can be cleaned with dishwashing detergent. There are special products for washing children's dishes, without a strong odor and with a safe composition.
How to bottle feed your baby
Before starting a meal, mom or dad should wash their hands well with soap and warm running water. Particular attention should be paid to the area between the fingers and under the nails. The hand washing process should take at least 20 seconds. And after carrying out this hygienic procedure, hands should be wiped dry with a paper towel or clean towel.
The next step is to prepare for the meal. If you plan to fill the bottle with formula, then dilute it with water in accordance with the instructions in the instructions. Improper proportions can lead to dehydration or bloating. It should also be remembered that for the preparation of the mixture you need to use only clean drinking water.
If you plan to fill the bottle with formula, then dilute it with water in accordance with the instructions in the instructions. Improper proportions can lead to dehydration or bloating. It should also be remembered that for the preparation of the mixture you need to use only clean drinking water.
Breast milk is the most beneficial for a newborn. Despite this, pediatricians advise breastfeeding babies for as long as possible. Even if the mother is ready to give up breastfeeding, milk can be expressed into a bottle and gradually accustom the baby to the nipple. If, for one reason or another, the mother does not have the opportunity to feed herself, then the only alternative is feeding with a special mixture.
In the first six months after birth, cow's or goat's milk or its substitute in the form of soy milk should not be included in the baby's diet. Valid options for supporting healthy development of a newborn are breast milk or formula milk only.
What temperature should the bottle filler be? Under no circumstances should the bottle be heated on the stove or in the microwave.
 If the temperature of the bottle and its filling exceed 37°C, the baby may be burned. It is recommended to use special bottle warmers. If this is not possible, then use the following method:
If the temperature of the bottle and its filling exceed 37°C, the baby may be burned. It is recommended to use special bottle warmers. If this is not possible, then use the following method: - put a saucepan on the stove with a little water;
- bring the water to a boil, then remove the pan from the heat;
- place a bottle of milk in a vessel and heat it up to 37◦С;
- check the temperature with a pre-cleaned thermometer or a special device for measuring the temperature of foodstuffs.
You can also check the temperature of the bottle ready for use:
- turn the bottle over;
- drip several times into your wrist area.
In this way, you can check not only the temperature of the milk or formula, but also how well the liquid flows out of the bottle. If you have to shake or squeeze the bottle hard to drip, the nipple is blocked and needs to be cleaned out. If, on the contrary, the filler pours out when the bottle is turned over, this means that the nipple is damaged and another nipple should be used to feed the baby, having previously sterilized it.![]()
How to bottle feed your baby lying down
There are several techniques for feeding your baby. However, it is the feeding of the child lying down from the bottle that young parents consider the most comfortable. It is worth noting that eating in this position will only be safe when the baby's head is slightly raised. Otherwise, the child may simply choke. In the prone position, the child should be placed on his arm bent at the elbow. After feeding, you should place the baby in an upright position, taking him in your arms and putting his stomach to your chest.
Make sure that the feeding bottle is closed correctly: the ring at the connection of the nipple to the bottle must not be too tight. Air must enter the bottle, otherwise a vacuum will be created there, which, in turn, will complicate the consumption of food for the child.
How to bottle feed without spitting up
Since the newborn is not able to fully control the process of feeding, along with milk, he can also take in air. This may be the reason that at one meal the child could not master the planned portion. In view of this, it is recommended to take small breaks during feeding.
This may be the reason that at one meal the child could not master the planned portion. In view of this, it is recommended to take small breaks during feeding.
As soon as you notice that the baby has stopped sucking on the pacifier, is tired or thoughtful, pick him up and press his face to you, holding his head and back. To help burp excess air, you can make a light massage between the shoulder blades, pat on the back or pope.
The air will quickly rise up and the baby will burp it without any extra effort. However, you should be prepared for the fact that, along with the air, part of the consumed mixture or milk may also return. Therefore, before taking the baby in your arms, cover yourself with a diaper, because it will be easier to wash it than clothes.
Never leave your baby alone with the bottle or let him fall asleep while using it. After eating, mom or dad must help their child burp. This will help to avoid colic, bloating and other manifestations of stomach discomfort.




/help-my-baby-is-spitting-up-blood-284376_color1-5b76d10746e0fb00259fc43a.png)