Premature babies and breast feeding
Breastfeeding Premature Babies - La Leche League International
Teresa Pitman
Originally published Sept 2015, updated June 2016 and republished with the express permission of the author.
Breastfeeding premature babies: how it promotes better health, but rarely happens. What helps mothers who want to breastfeed a premature baby?
About ten years ago, I was writing an article for a magazine about breastfeeding a premature baby. I contacted the pediatrician who was overseeing the Neonatal Intensive Care Unit at a large regional hospital, where most of the premature babies in my area would be looked after. My own grandson had been transported there when he was born eight weeks early and he had been exclusively breastfed.
However, when I talked to the pediatrician, he saw little point in my writing the article. Breastfeeding a premature baby? In his experience, that hardly ever happened. He felt that so few premature babies were breastfed that it wasn’t worth talking about.
It’s true that, compared to full-term babies, the number of premature babies who are breastfed continues to be low, especially in babies who are born earlier than 32 weeks. In the Loire Infant Follow-Up Team (LIFT) study of 1733 babies in 2008, only 16% were breastfeeding at time of discharge from hospital.
Hospital policy on breastfeeding premature babiesIt’s also true that some hospitals and physicians do not promote breastfeeding for premature babies, since these infants tend to gain weight more quickly with formula.
When my grandson was born, one of the first things the nurse said to my daughter-in-law was that she should know that breastfeeding isn’t always the best thing for a premature baby.
That nurse’s comment is not supported by research.
A 2012 study (1), which combined data from the LIFT study and an earlier study, following 2163 babies (the EPIPAGE study) described what the authors call “the breastfeeding paradox.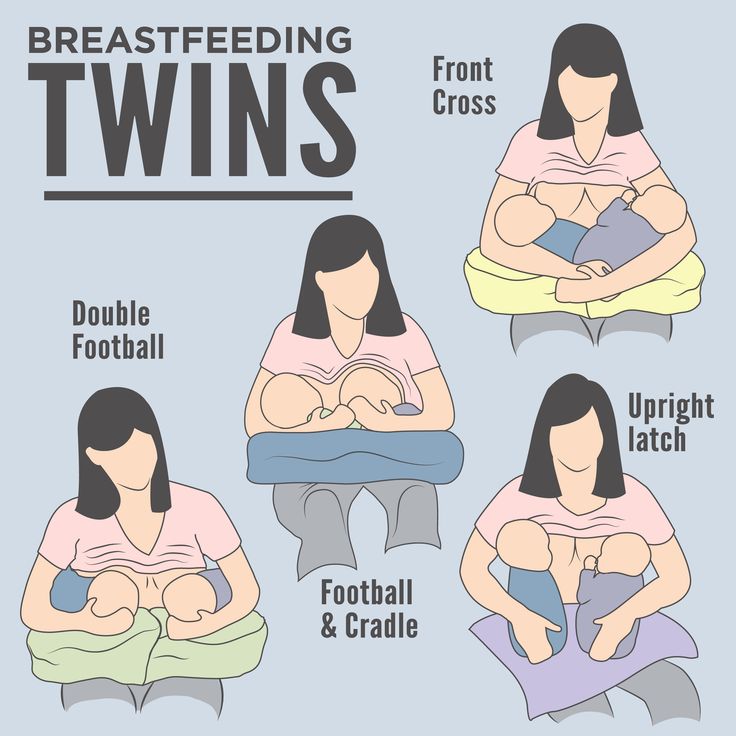 ”
”
Their analysis showed that the breastfed babies did indeed tend to gain weight more slowly than the formula-fed babies, even though fortifiers were added to the mother’s milk. However, when the baby’s neurodevelopmental status was assessed at two years of age and at five years of age, those who were breastfed had significantly higher scores than those who were not. Even the babies who received human milk only during the time they were in hospital showed higher scores than those who had only formula in hospital. Babies who were breastfed for longer than two months (corrected age) had the best scores of all.
Better physical healthBreastfeeding can be life-saving for many of these tiny babies.
Human milk is protective against necrotizing enterocolitis (NEC), a serious condition in which the baby’s intestines are damaged by infection. It occurs in about 10% of premature babies and there is a high mortality rate. Some have recommended probiotics as an alternate way to prevent NEC, but a 2015 study (2) found that the probiotics only reduced the rate of NEC in breastfed infants, not in those fed formula, who of course already had a higher incidence of NEC than the babies who were getting human milk.
Some have recommended probiotics as an alternate way to prevent NEC, but a 2015 study (2) found that the probiotics only reduced the rate of NEC in breastfed infants, not in those fed formula, who of course already had a higher incidence of NEC than the babies who were getting human milk.
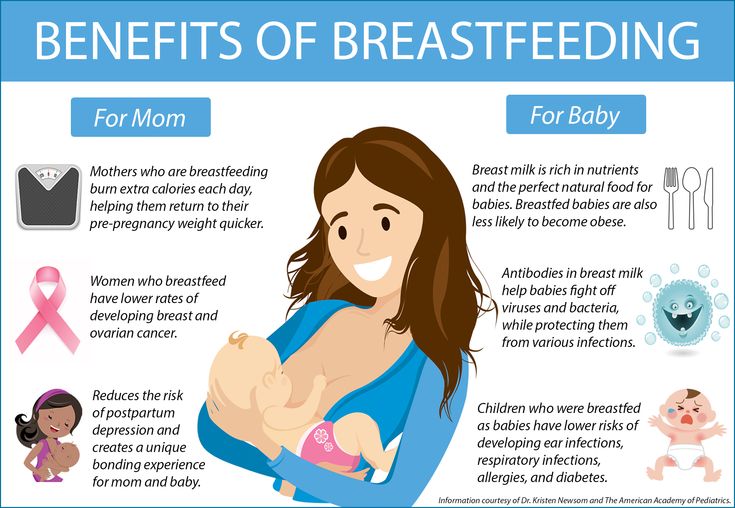
Breastfeeding promotes better physical health later in life, especially for babies born early.
Research suggests that premature infants are at higher risk of cardiovascular problems later in life. A 2001 study (3) followed up nearly 1,000 children born prematurely in the United Kingdom who had been randomized to receive either formula or banked breast milk. As teenagers, those who had been given formula had significantly higher blood pressure than those who had been given breast milk. Those who had the highest proportions of human milk had the lowest blood pressures. This is important because high blood pressure is known to be a risk factor for cardiovascular problems such as heart attacks.
Some health care providers have been concerned that fragile premature infants might be infected by bacteria in breast milk or by contact with the breastfeeding mother. However, a 2011 study (4) examined such concerns and determined that there was no correlation between finding bacteria in breast milk and the baby developing an infection. There was also no relationship between skin-to-skin contact with the baby and infection rates. They strongly advised against culturing the mother’s milk for bacteria before feeding, describing this as not a useful practice.
With all this supportive research, why do breastfeeding rates remain so low for premature babies?
Partly to blame are hospital routines that often make it difficult for mothers to establish milk production and get the baby latching well. It is often common practice to schedule feedings and some require babies to be drinking from a bottle before the baby is “allowed” to start breastfeeding.
This is also a difficult time emotionally for the parents. Many parents find it hard to believe their baby will survive. It’s hard to focus on building up a good milk supply when you are not sure your baby will ever be big enough to drink it.
Supporting breastfeeding is often not a priority for members of hospital staff who are focused on other aspects of caring for babies who may have significant medical problems and needs.
I recall with my grandson that sometimes staff would be impatient while he was breastfeeding (and he was not a fast eater) because he was scheduled for some test or treatment. On one occasion, before he was able to feed at the breast, a nurse appeared with a bottle of formula for the baby, ignoring the container of pumped milk that Esmaralda had worked so hard to get. When we stopped her, she shrugged and said, “Oh, I forgot you were giving him breast milk.”
Kangaroo careWhile quite a few NICUs have recognized the impressive amount of research and adopted “kangaroo care”—having mother or father skin-to-skin with the baby—they don’t always adopt the “kangaroo mother care” approach put forward by Dr. Nils Bergman. Often “kangaroo care” just means parent and baby get an hour or so in skin-to-skin contact each day. But in Bergman’s version—the version that is the foundation of the research demonstrating how this helps babies grow and develop—breastfeeding is part of it. In his version, the baby spends most of the time (not just an hour a day) in skin-to-skin contact and has free access to the breast.
Nils Bergman. Often “kangaroo care” just means parent and baby get an hour or so in skin-to-skin contact each day. But in Bergman’s version—the version that is the foundation of the research demonstrating how this helps babies grow and develop—breastfeeding is part of it. In his version, the baby spends most of the time (not just an hour a day) in skin-to-skin contact and has free access to the breast.
Kangaroo mother care originated in developing countries where incubators and other technology were in short supply. But as research showed how helpful it was to the wellbeing of the premature baby, more and more hospitals in developed countries also began using it. Here’s how Bergman suggests getting started:
“Immediately after birth, the low birth weight baby should be dried, placed on mother’s abdomen or chest, and covered with a cloth or blanket, just as described for a full term baby. Routine midwifery care and medical assessment should be completed speedily, with the newborn remaining on mother. Observations and monitoring will determine what medical support should be provided, and how this should be done.
Observations and monitoring will determine what medical support should be provided, and how this should be done.
This may in our current contexts require that the baby be separated, which must be accepted. A very premature infant may be too physically immature to exhibit the self-attachment behaviors of the full term baby, but the opportunity for early skin-to-skin contact is important nevertheless.
A premature baby will need help to breastfeed. Colostrum should be expressed and given by spoon or cup, or by gavage (tube) if necessary. For premature newborns, mothers should recline at an angle of 30 degrees, and should avoid moving about too much. This helps the baby’s breathing and sense of balance. Newborns should be stimulated as little as possible in this period.
After the first hour
Many premature babies will be stable in skin-to-skin contact after 90 minutes, often to the surprise of health professionals. Decisions need to be made about feeding and fluids and continued care. Oxygen by mask or by CPAP [or continuous positive airway pressure] can easily be arranged while in skin-to-skin contact, drips and feeding tubes can be secured sideways.
Decisions need to be made about feeding and fluids and continued care. Oxygen by mask or by CPAP [or continuous positive airway pressure] can easily be arranged while in skin-to-skin contact, drips and feeding tubes can be secured sideways.
If the baby is stable and the mother well, the carrier can be used. A premature baby should not be fed on demand, it needs to be fed far more frequently, every hour or two, day and night. This means loosening the wrapper regularly, so that mother can express breast milk. This is good for the baby and mother, though baby must never get cold.”
For more information about this approach to caring for a premature baby and some of the research supporting it, see kangaroomothercare.com.
And see our post on kangeroo care and skin-to-skin contact.
- Know the facts about why breastfeeding is so important for your baby.
- Seek out support. La Leche League Leaders can be a great resource for breastfeeding help and may be able to put you in touch with other mothers who have been through the experience of mothering a premie.
 When Sebastian was born, a mother from my LLL group dropped by the hospital to leave food and drinks for Esmaralda. She knew from her own experience as the mother of a baby born at 30 weeks how important it was to stay well fed and hydrated. You’ll also need practical help when you take your baby home as caring for him will mean extra work. Find local LLL support here.
When Sebastian was born, a mother from my LLL group dropped by the hospital to leave food and drinks for Esmaralda. She knew from her own experience as the mother of a baby born at 30 weeks how important it was to stay well fed and hydrated. You’ll also need practical help when you take your baby home as caring for him will mean extra work. Find local LLL support here. - Find out what arrangements are possible for staying near your baby. In some hospitals, you may be able to stay 24/7 in a room attached to the premature nursery; in others there may be no options other than to come in during the day and go home at night. It never hurts to ask: one mother I know was given a bed in an on-call room to sleep so she could be present for her baby’s night feedings.
- Maximize skin-to-skin time and do kangaroo care if at all possible. Just having your baby skin-to-skin will increase your milk production.
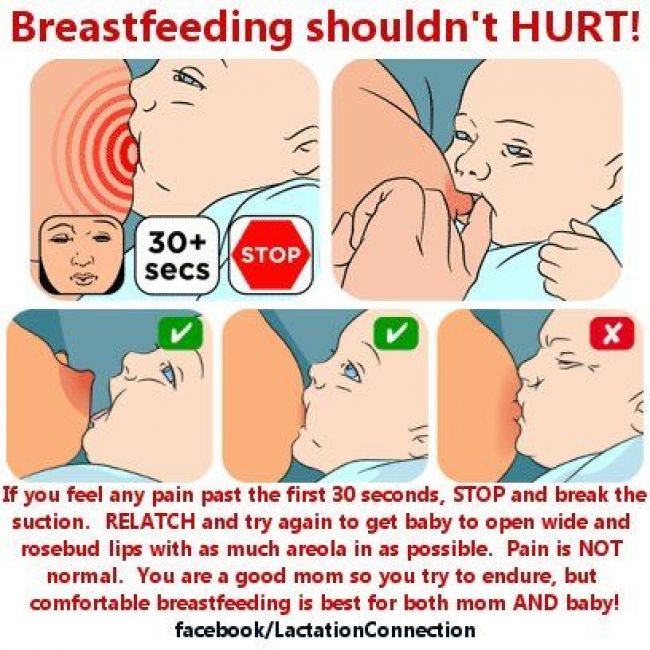
- Remove milk from the breast frequently, day and night. Short, frequent feedings are more helpful in establishing milk production than longer, widely spaced feedings.
 Hand expression may be most effective at first; a breast pump may be helpful later. (Hand expressing after you pump can increase milk removal and therefore milk production.) Of course, as soon as the baby is able to breastfeed, that becomes another way to remove milk. You may find that you are producing more milk than your baby needs at first. That’s okay, he’ll catch up!
Hand expression may be most effective at first; a breast pump may be helpful later. (Hand expressing after you pump can increase milk removal and therefore milk production.) Of course, as soon as the baby is able to breastfeed, that becomes another way to remove milk. You may find that you are producing more milk than your baby needs at first. That’s okay, he’ll catch up! - Avoid bottles if possible. Sometimes hospital policies require that babies have bottles prior to breastfeeding, and fighting the policy may be more stress than parents can deal with. Working with a La Leche League Leader or lactation consultant can help you get your baby breastfeeding effectively even if bottles have been given.
- Watch your baby for signs of readiness to breastfeed. Your baby may have become used to the nursery routines, but as he gets stronger you’ll want to respond to his hunger cues.
Every baby is an individual, and premature babies will have different challenges than those who are full term.
The first key to success is continuing to remove milk so that you have a generous supply ready when your baby develops the strength and skills he needs to feed at your breast. The second is having good, patient helpers who can help you and your baby figure out an approach to breastfeeding that will work in your situation.
Today, my eight-week-early grandson is thirteen years old. He’s a healthy, very active boy who loves to camp and do anything outdoors, and whose current career ambition is to be a history professor. He breastfed for about three-and-a-half years and that gave him a solid foundation despite his surprise arrival two months before we expected to meet him.
References- Roze, J-C., Darmaun, D. et al. The apparent breastfeeding paradox in very preterm infants: relationship between breastfeeding, early weight gain and neurodevelopment based on results from two cohorts, EPIPAGE and LIFT. BMJ Open 2012;2:e000834, doi: 10.
 1136/bmjopen-2012-000834.
1136/bmjopen-2012-000834. - Repa, A., Thanhaeuser, M. et al. Probiotics prevent NEC in VLBW infants fed breastmilk but not formula. Pediatr Res 2015 Feb;77(2): 381-8.
- Singhal, A., Cole T.J. et al. Early nutrition in preterm infants and later blood pressure: two cohorts after randomised trials. Lancet 2001 Feb 10;357 (9254): 413-9.
- Schanler, R.J., Fraley, J.K., et al, Breastmilk cultures and infection in extremely premature infants. J Perinatol 2011 May;31(5):335-8.
Premies: Breastfeeding
Premies: Kangaroo Care and Skin-to-Skin Contact
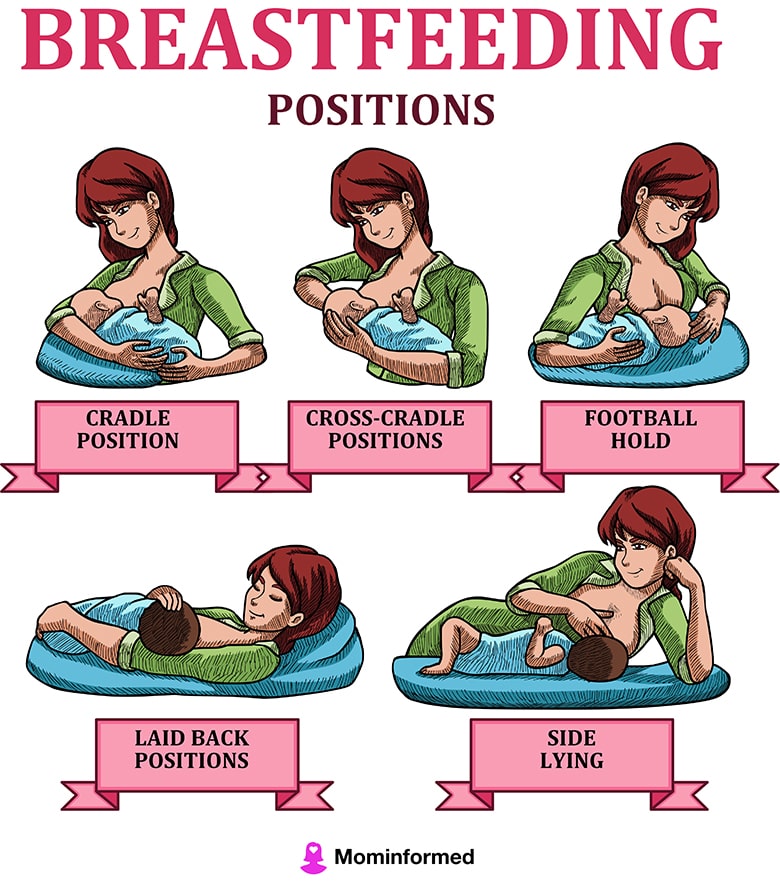
Premies: Positioning
Premies: Pumping
Jill Bergman, Skin-to-Skin Contact
LLLGB Twins
Baley, J. MD, Committee on Fetus and Newborn, AAP, Skin-to-skin care for term and preterm infants in the neonatal ICU Pediatr, 2015: 136(3): 596-599.
Gibbs, D., Boshoff, K. & Stanley, M. (2015). Becoming the parent of a preterm infant: A meta-ethnographic synthesis. British Journal of occupational therapy, doi: 10.1177/0308022615586799.
(2015). Becoming the parent of a preterm infant: A meta-ethnographic synthesis. British Journal of occupational therapy, doi: 10.1177/0308022615586799.
Lewandowski, Adam. Lamata, P et al. Breast milk consumption in preterm neonates and cardiac shape in adulthood Pediatrics June 2016.
Mohrbacher, N. Breastfeeding Answers Made Simple “Breastfeeding The Preterm Baby: When to Start Breastfeeding.” Hale Publishing 2010; 339–340.
Palmer, L. F. Fortify Milk for Premature Infants? Baby Poop, Sunny Lane Press, 2015.
Teresa Pitman has been a La Leche League Leader for 40 years. She is one of the co-authors of the LLLI books The Womanly Art of Breastfeeding and Sweet Sleep and is the author of 16 other books with a 17th book coming out in January 2019 (on starting solids!). She is the mother of four grown children and the grandmother of ten.
Breastfeeding your premature baby - NHS
Your breast milk is important to your baby at any age.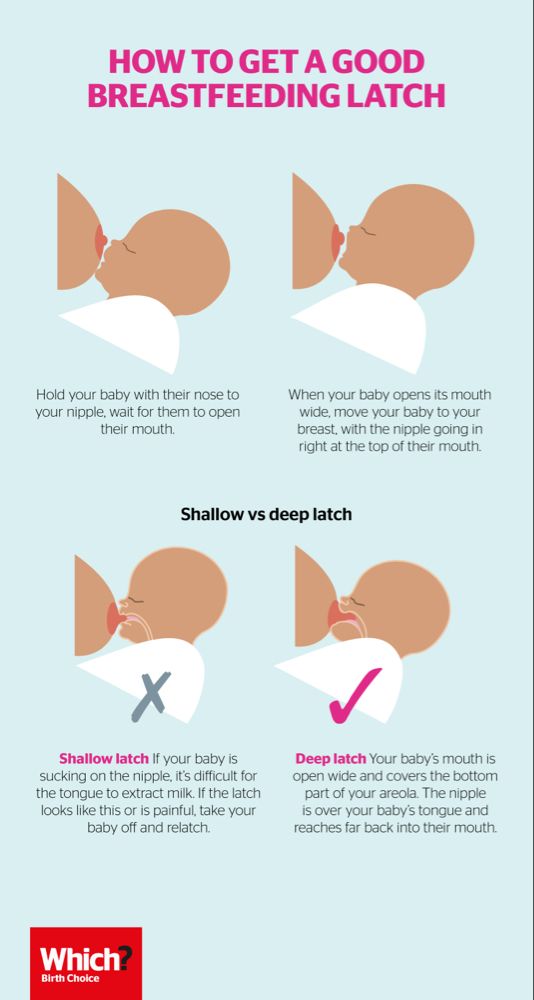 Giving your premature baby your breast milk benefits their health as well as yours.
Giving your premature baby your breast milk benefits their health as well as yours.
Breast milk:
- helps protect your baby from infections, particularly of their gut – premature babies are more likely to get infections
- contains hormones, nutrients and growth factors that help your baby to grow and develop
- is easier for your baby to digest than formula milk, because it's human milk specially designed by your body for your baby
See other benefits of breastfeeding.
If your baby is very small or sick, they may not be able to breastfeed from your breast at first. But you can start regularly collecting your breast milk (called expressing) as soon as possible after your baby is born.
This will help get your milk supply going and the milk you express can be frozen so you can give it to your baby later. Then you can start breastfeeding from the breast once you and your baby are ready.
Then you can start breastfeeding from the breast once you and your baby are ready.
Even if you were not planning to breastfeed, you could express your breast milk for a while to help boost your baby's immune system in the early weeks after birth.
Spending lots of time close together with your baby can help boost your breast milk supply and establish breastfeeding.
Skin-to-skin contact with your premature baby
If your baby is well enough, you'll usually be encouraged to spend time holding them against your skin as soon as possible. This is sometimes called kangaroo care.
Your baby will usually be dressed just in a nappy, hat and socks and then placed inside your top, under a blanket, or in a soft sling so they can be held securely against your skin. If it's cold outside, you can also put them in a sleeveless vest with an open neck.
This skin-to-skin contact helps you feel close to your baby. Your partner can enjoy this kind of contact as well.
For your premature baby, skin-to-skin contact:
- reduces stress and pain
- promotes healthy weight gain
- helps to establish breastfeeding
- helps them sleep better
- helps to regulate and support their heart rate and breathing
For mums, skin-to-skin contact:
- helps reduce your chance of developing postnatal depression
- increases your confidence as a new parent
- can help make breastfeeding easier and increase the amount of milk you make
For dads and partners, holding your baby skin to skin:
- helps you bond with your baby – babies can hear both parents' voices in the womb and will be calmed by the sound of your voice as well as their mum's
- helps you feel more confident as a parent
Expressing milk if your baby is premature
It's recommended you express often, ideally at least 8 times a day to begin with – including at least once at night – to keep your milk supply up.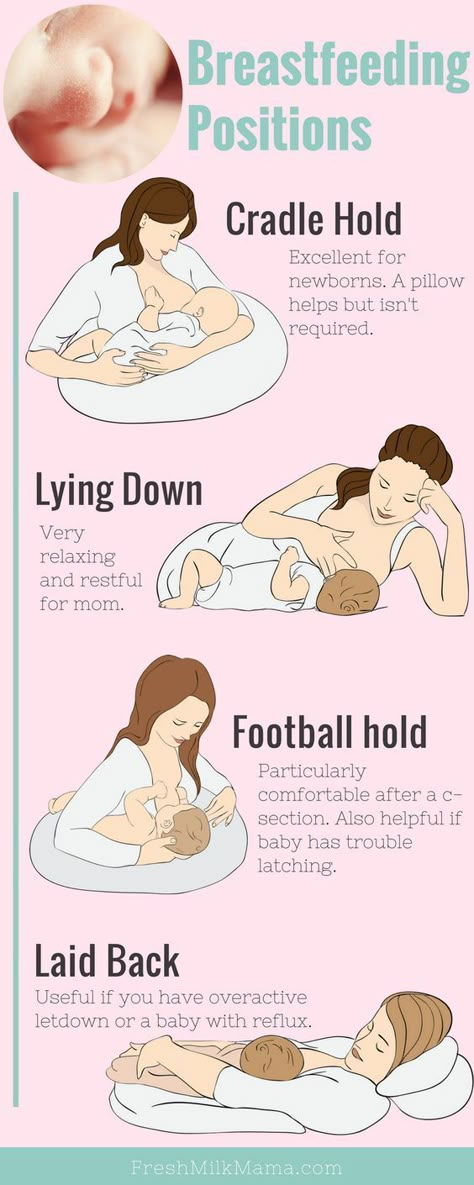
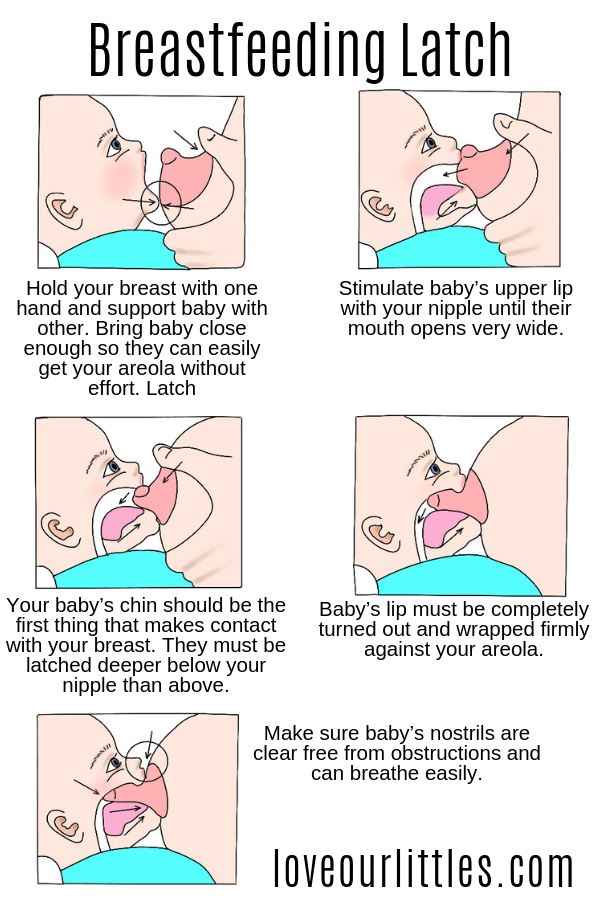
In the early days, it's often easier to express your milk by hand. Your midwife or a breastfeeding supporter can show you how.
You'll probably only express a few drops to begin with but, if you hand express often, this will increase. Even if you are only expressing a small amount it will still help your baby.
In the early days you can collect your breast milk in a small, sterile cup and store it in a syringe.
Once you are producing more milk, you could try using a breast pump. If your baby is in a neonatal unit, the hospital will usually be able to lend you an electric breast pump for expressing your milk. If they cannot lend you one, you can hire one.
Read more about breastfeeding help and support to find out about hiring a pump, or phone the National Breastfeeding Helpline on 0300 100 0212.
The staff, your midwife or a breastfeeding supporter can give you advice about how to increase your milk supply. They can also show you how to encourage your milk to flow and how to use a breast pump.
They can also show you how to encourage your milk to flow and how to use a breast pump.
Always ask for help early if you have any worries or questions.
Tube feeding your baby
Babies do not normally learn to co-ordinate the sucking, swallowing and breathing needed for feeding until about 34 to 36 weeks of pregnancy.
If your baby is born before this time, they may need to have breast milk through a feeding tube to begin with. This goes through their nose or mouth into their stomach. The staff in the neonatal unit can show you how to feed your baby this way.
Babies who are very premature or sick may need to be fed through an intravenous (IV) line to begin with. A fluid containing nutrients is fed straight into your baby's vein.
The Bliss website has more information and advice about tube feeding
Using donor breast milk
Some hospitals can provide donated breast milk for your baby to have until your own supply is established.
See the United Kingdom Association for Milk Banking (UKAMB) website for more information about donor breast milk
If donor breast milk is not available, your baby can have formula milk until you're producing enough breast milk.
It's recommended you do not buy donor milk over the internet. This is because the source cannot be confirmed and you cannot be sure whether the donor or the milk has been screened for infections.
Moving on to breastfeeding your premature baby
While holding your baby, you may notice them try to move towards your breast. Gradually, as they develop and get stronger, they will be able to breastfeed directly.
The first time you try it, the hospital staff may ask you to express first, then put your baby to your breast. This is so your baby is not overwhelmed when your milk lets down.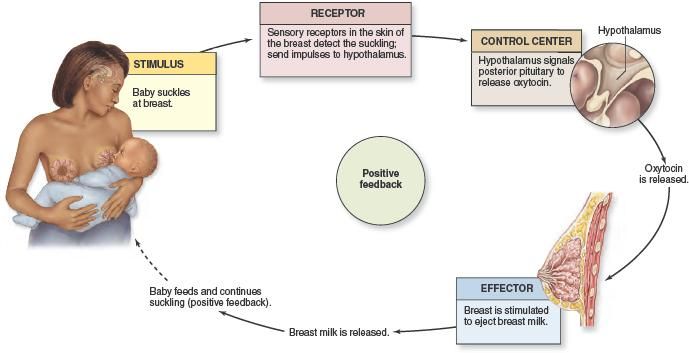
At first, your baby may only lick the breast, then next time take a few sucks until they gradually become happy and confident feeders.
You can combine tube feeding with breastfeeding until your baby is getting everything they need from the breast only.
Using a lactation aid (supplementer)
You could also consider using a lactation aid. This is a way of supplementing your baby's breastfeeds with either expressed breast milk or formula.
A tiny tube is taped next to your nipple so your baby can get milk through the tube as well as from your breast while attached to your breast. This helps to support your baby as they get used to attaching to the breast.
Got a breastfeeding question?
Sign into Facebook, or use an Amazon Alexa or Google Home and use the Start4Life Breastfeeding Friend chatbot for fast, friendly, trusted NHS advice anytime, day or night.
Feeding premature babies | Breastfeeding premature babies
Premature babies have a special need for breast milk, but it can be difficult to breastfeed them directly. Our expert advice will help you provide your premature baby with healthy breast milk.
Share this information
Professor Katsumi Mizuno, Department of Pediatrics, Showa University Koto Toyosu Hospital:
Katsumi is a Certified Breastfeeding Consultant, Professor of Pediatrics at Showa Medical University, and one of Japan's leading pediatric neonatologists. His research focuses on neonatal suckling skills, breast milk banking, and the use of breast milk for feeding premature babies in neonatal intensive care units.
Babies born before the 37th week of pregnancy are considered premature. 1 The causes of preterm birth are not always obvious, but certain factors increase the likelihood of such an event. These include: twin or multiple pregnancy, certain diseases of the mother or fetus, as well as a history of premature birth. nine0003
nine0003
Because premature babies spend less time in the womb, they are not mature enough and may be more susceptible to infection and disease. They often require hospitalization in the neonatal intensive care unit.
Why is breast milk so important for premature babies?
Breast milk is essential for optimal growth and development of term babies, but it is even more important for premature babies.
During pregnancy, the fetus receives important substances from the mother through the placenta, such as DHA (a fatty acid essential for brain and eye development) and immunoglobulin G (an antibody). nine0012 2.3 A premature infant did not receive all of these substances. However, the milk produced by a premature mother contains more fat and secretory immunoglobulin than mothers of full-term babies. 4
In addition, premature babies have an underdeveloped gastrointestinal tract, which can make digestion and absorption of nutrients difficult, so they need food that their sensitive stomach and intestines can easily digest. Breast milk contains enzymes that make it easier for the baby to digest, 5 as well as epidermal growth factor, which accelerates the development of the gastrointestinal tract 6 . Premature infants who are predominantly breastfed have much lower intestinal permeability than formula-fed infants, meaning fewer potentially harmful particles from the stomach and intestines enter their bloodstream. 7
Breast milk contains enzymes that make it easier for the baby to digest, 5 as well as epidermal growth factor, which accelerates the development of the gastrointestinal tract 6 . Premature infants who are predominantly breastfed have much lower intestinal permeability than formula-fed infants, meaning fewer potentially harmful particles from the stomach and intestines enter their bloodstream. 7
Breast milk is so important for premature babies that if the baby's mother does not produce enough breast milk at first for any reason, it is recommended that the deficiency be replenished with donor milk rather than formula. nine0003
Does breast milk improve the condition of premature babies?
Breast milk contains protective substances that can prevent serious diseases that preterm infants are susceptible to, 8 such as severe infections, 9 retinopathy of prematurity (which can cause vision loss) 10 and bronchopulmonary dysplasia (chronic lung disease). 11
11
The more milk your baby gets, the lower the risk of developing diseases. nine0012 12 Every additional 10 ml of milk per kilogram of body weight per day reduces the risk of sepsis by 19%. 9 The risk of developing necrotizing enterocolitis (a potentially fatal bowel disease) in premature infants who are breastfed is ten times lower than those who are formula fed. 13 That's why every drop counts!
Most importantly, premature infants who are breastfed are typically discharged an average of two weeks earlier than formula-fed infants. nine0012 14 They also have a 6% lower risk of readmission in the first year of life. 15
Breast milk has been proven to have a beneficial effect on mental and physical development in the long term. Studies show that low-birth-weight babies who are breastfed in the neonatal intensive care unit have an average IQ of up to five points higher than those who are not breastfed. 15 In addition, their cardiovascular system works better during their lifetime. nine0012 17
15 In addition, their cardiovascular system works better during their lifetime. nine0012 17
Will milk be produced if the baby is born prematurely?
Yes, the mother's body is ready to produce milk by the middle of pregnancy. After the baby is born and the placenta is born, the level of progesterone, the pregnancy hormone, drops, and the production of colostrum, the first milk, starts in the breast. This usually happens after the newborn is put to the breast and begins to suckle rhythmically, but if the baby was born prematurely, he most likely will not be able to latch on at first. nine0003
To replicate the sensations that trigger milk production, you can manually stimulate the breasts and nipples, or use a breast pump to express nutrient-rich colostrum for your baby. 18 Read below for more information on what to do if your premature baby is not yet able to breastfeed.
Breast milk usually comes in two to four days after birth, but if it was premature, the milk supply may be delayed. However, a recent study shows that moms who started pumping within one hour of giving birth had milk coming in as expected. nine0012 19 This is why it is important to start expressing breast milk as early as possible.
However, a recent study shows that moms who started pumping within one hour of giving birth had milk coming in as expected. nine0012 19 This is why it is important to start expressing breast milk as early as possible.
How to prepare if the baby is expected prematurely?
Visit the neonatal intensive care unit to see how it works and how premature babies are cared for. In addition, it will be useful to learn how breast milk is produced and secreted and why it is not only a healthy food, but also an important medicine for premature babies. Read more about this in our free e-book Surprising Breast Milk Facts .
What if a premature baby cannot breastfeed?
Many babies born before 34 weeks have difficulty coordinating sucking, swallowing and breathing. Until the baby masters these skills, nurses will feed him through a tube that is inserted into the nose or mouth and provides food directly into the stomach. In this way, the baby can be fed continuously until he is ready to breastfeed.
If your baby is too weak to latch on and suckle milk, you can use a breast pump* available at the hospital or maternity hospital to “do the job for the baby”. Breast stimulation with research-based technology, 20 mimics the rhythm of the baby's suckling, plays an important role in starting and maintaining milk production in the first hours after birth 21 .
Milk should be expressed at the same frequency as term infants are usually fed every two to three hours, i.e. 8 to 12 times a day.
You can try putting a small amount of expressed breast milk into the baby's mouth with a syringe, or putting milk-soaked cotton swabs in the baby's mouth. 22 This is how your baby learns the taste of your milk, which will facilitate the transition to breastfeeding in the future. In addition, the protective substances that make up breast milk will help strengthen the local immunity of the baby's oral cavity. You can be involved in the care of your premature baby in a variety of ways - check with your healthcare provider for details.
Very low birth weight babies - less than 1.5 kg - usually need extra protein, calcium and phosphorus, so they are given fortified breast milk. In some countries, such additives are made on human milk, and, for example, in Japan, on cow's milk. nine0003
Recommendations for pumping milk
If the baby will be in the neonatal intensive care unit for a long time, neonatologists recommend using a double breast pump for pumping. I always recommend Medela Symphony*. Double pumping not only speeds up the process, but also produces an average of 18% more milk than pumping from each breast in turn. 23
In addition, I advise you to create the most comfortable conditions for pumping. It is generally agreed that it is best to express milk during or after prolonged skin-to-skin contact with the baby (more on this "kangaroo method" below). Another good option is to sit next to the crib and watch your baby while he pumps. Oxytocin (the hormone that stimulates milk flow) is released when you look at your baby, touch him, smell him and think about him, 24 Therefore, comfortable and calm conditions must be created for this in the neonatal intensive care unit.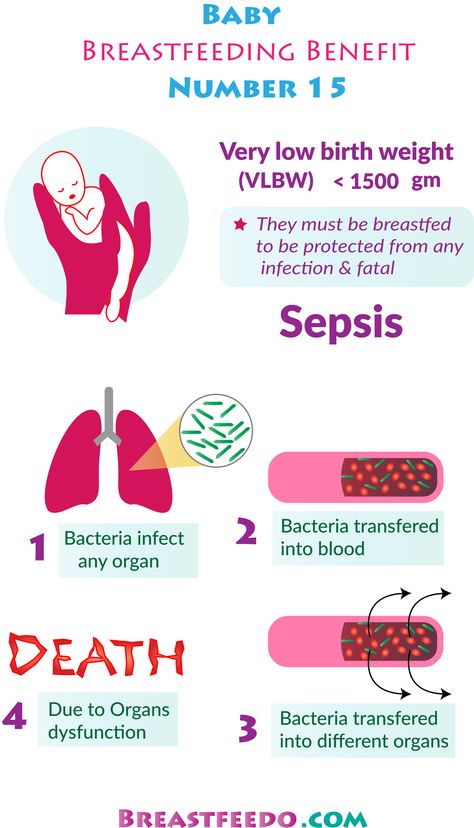
What is kangaroo care for premature babies?
The so-called kangaroo method involves prolonged skin-to-skin contact between parents and infant. This is extremely beneficial for you and your baby, as well as for milk production. Skin-to-skin contact normalizes the baby's breathing and heartbeat, keeps him warm and allows him to be as close to the parent as possible. Kangaroo care is believed to have a beneficial effect on the health of premature babies, 25 and it helps mothers express more milk 26 and breastfeed longer. 27 Skin-to-skin contact 30-60 minutes before feeding gives baby time to wake up and be hungry so he can eat without being forced.
What if the neonatal intensive care unit offers formula feeding?
Feel free to state that you want to breastfeed your baby instead of formula. If you don't have enough breast milk to feed your baby, ask the ward for help to increase your milk supply. nine0003
It is natural for mothers whose babies are in the neonatal intensive care unit to experience anxiety and stress. Sometimes these experiences interfere with milk production, so it's important to ask for any help you may need. Remember that you have the right to seek support. Your healthcare provider may be able to recommend a suitable lactation specialist, such as a lactation consultant, for you.
Sometimes these experiences interfere with milk production, so it's important to ask for any help you may need. Remember that you have the right to seek support. Your healthcare provider may be able to recommend a suitable lactation specialist, such as a lactation consultant, for you.
How to switch from pumping to breastfeeding? nine0018
At whatever gestational age a baby is born, if the baby is stable enough for skin-to-skin contact, it can seek the breast for sedative suckling. This is the perfect way for your baby to learn sucking skills before they learn to coordinate sucking, swallowing and breathing.
Babies love the smell of breastmilk, so you can put some milk on the nipple before putting your baby to the breast to make him want to suckle. He might even be able to suck some milk. Don't worry if your baby seems to suck very little - he learns every time. He can start with one or two sips and gradually move on to full breastfeeding. Until then, the baby can be fed through a tube, pressed to the breast, so that the taste of milk and touching the breast is associated with a feeling of satiety. nine0003
nine0003
You can put your baby to the breast for sedative suckling as soon as you are ready for kangaroo care, unless your baby is suffering from bradycardia (slow heartbeat) or low oxygen levels in the blood. You can switch to breastfeeding as soon as the baby is ready for it. Gradually, he will gain enough strength to suckle longer and suck out more milk.
Literature
1 World Health Organization. Geneva, Switzerland; 2018. Media Centre: Preterm birth fact sheet; November 2017 [03/26/2018]. Available from : http://www.who.int/mediacentre/factsheets/fs363/en/ - World Health Organization. Geneva, Switzerland; 2018. "Media Center: Prematurity Fact Sheet"; November 2017 [3/26/2018]. Article at: http://www.who.int/mediacentre/factsheets/fs363/en/
2 Duttaroy AK. Transport of fatty acids across the human placenta: a review. nine0085 Prog Lipid Res .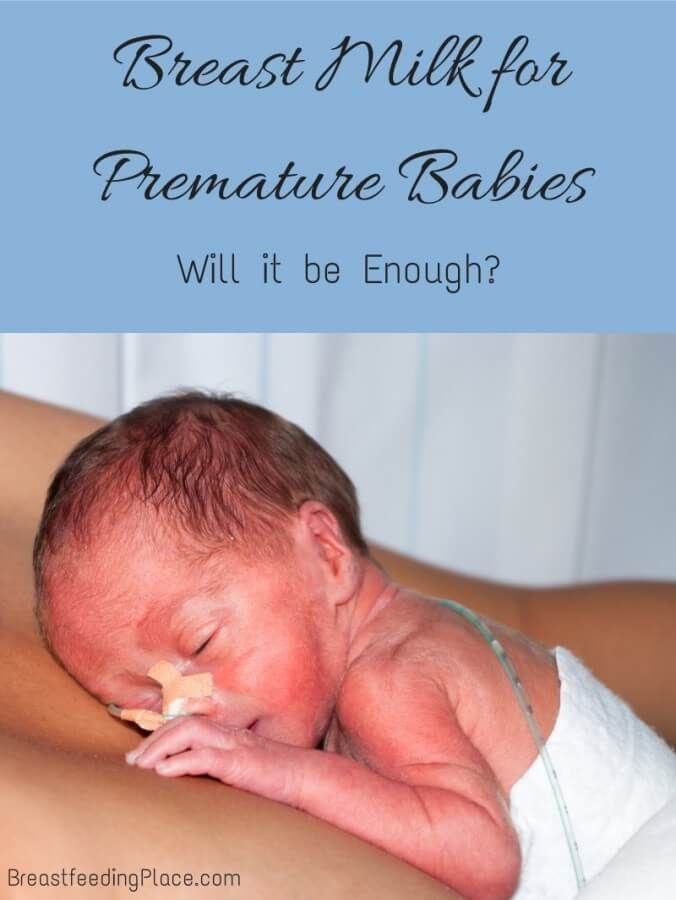 2009;48(1):52-61. - Duttaroy A.K., "Transfer of fatty acids across the human placenta: a review". Prog Lipid Res. 2009;48(1):52-61.
2009;48(1):52-61. - Duttaroy A.K., "Transfer of fatty acids across the human placenta: a review". Prog Lipid Res. 2009;48(1):52-61.
3 Palmeira P et al. IgG placental transfer in healthy and pathological pregnancies. Clin Dev Immunol. 2012;2012: 985646. - Palmeira P. et al., Placental transfer of immunoglobulin G through the placenta with healthy and pathological pregnancy. " Klin Virgo Immunol. 2012: 985646.
4 Underwood Ma. Human Milk Formature North Am . 2013;60(1):189-207. - Underwood, M.A., "Breast milk for the premature baby." 1):189-207.
5 Pamblanco M et al. Bile salt - stimulated lipase activity in human colostrum from mothers of infants of different gestational age and birthweight.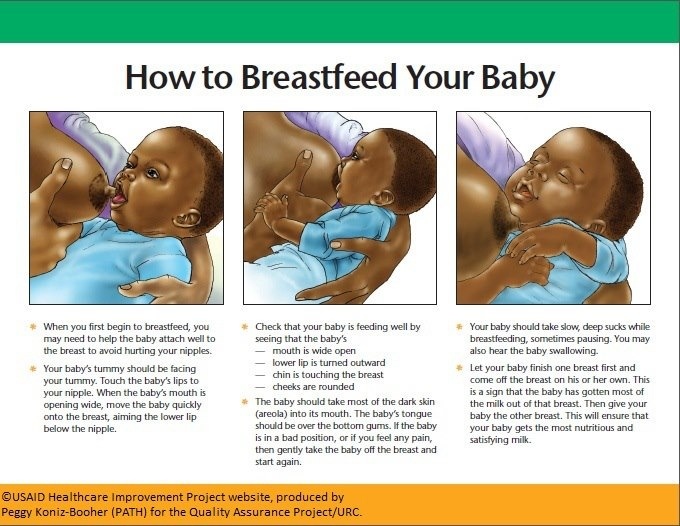 Acta Paediatr. 1987;76(2):328-331. - Pamblanco M. et al., "Bile salt-activated lipase and its activity in colostrum of mothers of infants of various gestational ages and birth weights." Akta Pediatr. 1987;76(2):328-331.
Acta Paediatr. 1987;76(2):328-331. - Pamblanco M. et al., "Bile salt-activated lipase and its activity in colostrum of mothers of infants of various gestational ages and birth weights." Akta Pediatr. 1987;76(2):328-331.
6 Dvorak B. Milk epidermal growth factor and gut protection. J Pediatr. 2010;156(2): S 31-35. - Dvorak B., "Epidermal growth factor in milk and gut protection". F Pediatrician (Journal of Pediatrics). 2010;156(2):S31-35.
7 Taylor SN et al. Intestinal permeability in preterm infants by feeding type: mother's milk versus formula. Breastfeed Med . 2009;4(1):11-15.- Theilon S.N. et al., "Intestinal permeability in preterm infants and its association with type of feeding: breast milk or formula." Brestfeed Med (Breastfeeding Medicine). 2009;4(1):11-15.
8 Newburg DS. Innate immunity and human milk. J Nutr . 2005;135(5):1308-1312. — Newburgh, D.S., "Natural Immunity and Breast Milk." F Int. 2005;135(5):1308-1312. nine0085
Innate immunity and human milk. J Nutr . 2005;135(5):1308-1312. — Newburgh, D.S., "Natural Immunity and Breast Milk." F Int. 2005;135(5):1308-1312. nine0085
9 Patel AL et al. Impact of early human milk on sepsis and health-care costs in very low birth weight infants. J Perinatol . 2013;33(7):514-519.- Patel A.L. et al., "Impact of early breast milk on sepsis and health care costs in extremely low birth weight infants". Zh Perinatol (Journal of Perinatology). 2013;33(7):514-519.
10 Zhou J et al . Human milk feeding as a protective factor for retinopathy of prematurity: a meta-analysis. Pediatrics. 2015;136(6): e 1576-1586. - Zhou Q. et al., "Breastfeeding as a protective factor against retinopathy of prematurity: a meta-analysis. " Pediatrix (Pediatrics). 2015;136(6):e1576-1586.
" Pediatrix (Pediatrics). 2015;136(6):e1576-1586.
11 Patel AL et al. Influence of own mother's milk on bronchopulmonary dysplasia and costs. Arch DIS Child Neonat ED . 2017;102(3): F 256- F 261. - Patel A.L. et al., "Effect of breast milk on bronchopulmonary dysplasia and health care costs." Arch Dis Child Fetal Neonate Ed. 2017;102(3): F 256- F 261. 12 MEIER PP ET AL AL AL AL . Improving the use of human milk during and after the NICU stay. Clin Perinatol. 2010;37(1):217-245. - Meyer P.P. et al., "Optimizing the use of breast milk during and after a stay in the neonatal intensive care unit." nine0085 Perinatol wedge. 13 Lucas A, Cole TJ. Breast milk and neonatal necrotising enterocolitis. Lancet. 1990;336(8730-8731):1519-1523. — Lucas A, Cole TJ, "Breast milk and neonatal necrotizing enterocolitis." Lancet 1990;336(8730-8731):1519-1523. 14 Schanler RJ et al. Randomized trial of donor human milk versus preterm formula as substitutes for mothers' own milk in the feeding of extremely premature infants. nine0085 Pediatrics. 2005;116(2):400-406. - Chanler R.J. et al., "Randomized Trial of Donor Human Milk Versus Prematurity Formula as a Breast Milk Substitute in Severely Preterm Infants". Pediatrix (Pediatrics). 2005;116(2):400-406. 15 Vohr BR et al. Beneficial effects of breast milk in the neonatal intensive care unit on the developmental outcome of extremely low birth weight infants at 18 months of age. nine0085 Pediatrics. 16 Victora CG et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. nine0085 2016;387(10017):475-490. - Victor S.J. et al., "Breastfeeding in the 21st century: epidemiology, mechanisms and long-term effects". Lancet (Lancet). 2016;387(10017):475-490. 17 Lewandowski AJ et al. Breast milk consumption in preterm neonates and cardiac shape in adulthood. Pediatrics. 2016;138(1): pii : e 20160050. - Lewandowski, A.J. et al., "Breastfeeding in preterm infants and cardiovascular health in adulthood." nine0085 Pediatrix (Pediatrics). 2016;138(1):pii:e20160050. 18 Meier PP et al. Which breast pump for which mother: an evidence-based approach to individualizing breast pump technology. J. Perinatol. 2016;36(7):493-499. - Meyer P.P. et al., Breastpump Selection: A Scientific Approach to Customizing Pumping Technology. J Perinatol (Journal of Perinatology). 2016;36(7):493-499. 19 Parker LA et al. Effect of early breast milk expression on milk volume and timing of lactogenesis stage II among mothers of very low birth weight infants: a pilot study. J Perinatol. 2012;32(3):205-209. - Parker L.A. et al., "Effect of early pumping on milk supply and timing of the second stage of lactogenesis in mothers of extremely low birth weight infants: a pilot study." J Perinatol (Journal of Perinatology). 2012;32(3):205-209. 20 Meier PP et al. Breast pump suction patterns that mimic the human infant during breastfeeding: greater milk output in less time spent pumping for breast pump-dependent mothers with premature infants. 21 Parker LA et al. Association of timing of initiation of breastmilk expression on milk volume and timing of lactogenesis stage II among mothers of very low-birth-weight infants. Breastfeed Med . 2015;10(2):84-91. - Parker L.A. et al., "Effect of early pumping on milk supply and timing of the second stage of lactogenesis in mothers of extremely low birth weight infants: a pilot study." nine0085 Brestfeed Med (Breastfeeding Medicine). 2015;10(2):84-91. 22 Lee J et al. Oropharyngeal colostrum administration in extremely premature infants: an RCT. Pediatrics. 2015;135(2): e 357-366. 23 Prime PK et al. Simultaneous breast expression in breastfeeding women is more efficacious than sequential breast expression. Breastfeed Med 2012; 7(6):442–447. - Prime D.K. and co-authors. "During the period of breastfeeding, simultaneous pumping of both breasts is more productive than sequential pumping." Brestfeed Med (Breastfeeding Medicine). 2012;7(6):442-447. 24 Uvn ä s Moberg K Oxytocin effects in mothers and infants during breastfeeding. Infant 2013; 9(6):201–206. - Uvenas-Moberg K, Prime DK, "Oxytocin effects on mother and child during breastfeeding". Infant. 2013;9(6):201-206. 25 Boundy EO et al. nine0085 Kangaroo mother care and neonatal outcomes: a meta-analysis. Pediatrics. 2015;137(1): e 20152238. - Boundi I.O. and co-authors, "The Kangaroo Method and Its Impact on Newborns: A Meta-Analysis". Pediatrix (Pediatrics). 2015;137(1): e20152238. 26 Acuña-Muga J et al. Volume of milk obtained in relation to location and circumstances of expression in mothers of very low birth weight infants. nine0085 J Hum Lact . 2014;30(1):41-46 - Akunya-Muga, J. et al., "The amount of milk expressed by location and circumstances of pumping in mothers of extremely low birth weight infants." F Hum Lakt. 2014;30(1):41-46 27 Nyqvist KH et al. Towards universal kangaroo mother care: recommendations and report from the first European conference and seventh international workshop on kangaroo mother care. 28 American Academy of Pediatrics - Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics . 2012;129(3): e 827-841.- American Academy of Pediatrics - Section "Breastfeeding", "Breastfeeding and the use of breast milk". Pediatrix (Pediatrics). 2012;129(3): e 827-841. *RU No. ФСЗ 2010/06525 dated 03/17/2021 Successful nursing of premature newborns, in addition to therapeutic measures, largely depends on the creation of optimal external conditions and adequate nutrition. Proper and nutritious nutrition in the early stages of life affects the overall development of the child, and also contributes in direct proportion to the reduction of the development of chronic diseases in adulthood (such as diabetes and arterial hypertension). nine0003 The purpose of enteral nutrition is to provide the body with the nutrients it needs to grow and develop. Providing a premature newborn with an optimal amount of nutrients is quite difficult, given the morphofunctional immaturity of the digestive system and the lability of metabolic processes. The relatively high need of premature infants for nutrients is in conflict with the limited ability to assimilate them. Feeding methods for premature babies are determined by the severity of their condition and depend on the body weight and gestational age of the baby at birth. Successful feeding of a newborn is possible when sucking, swallowing and breathing become well coordinated. The swallowing reflex is well developed already by 28-30 weeks of gestational age, but it is very quickly depleted. Fully matures by 34 weeks of gestation. When does sucking and swallowing coordinate? Already at 28 weeks of gestational age, all the components of sucking and swallowing take place, but the child is not yet able to coordinate them. Partially, this occurs by 32-34 weeks of gestation. Coordination of sucking and swallowing fully matures around 36-38 weeks of gestational age. From 37 to 38 weeks of gestational age, newborns are able to coordinate sucking, swallowing, and breathing without difficulty. nine0003 When feeding premature babies, you should pay attention to four points: when, with what, in what volume, by what method to feed. The first feeding should be started as soon as it becomes clinically possible. Earlier introduction of breast milk helps to reduce the frequency of infections, maturation of the gastrointestinal tract, immune functions, and improved calcium metabolism. Newborns weighing more than 2000 g and gestational age more than 33 weeks, who do not have other diseases, can be attached to the mother's breast as early as the first day of life. In this case, you should carefully monitor the appearance of signs of fatigue (cyanosis of the nasolabial triangle, shortness of breath, etc.). Their appearance is an indication for the transition to feeding expressed breast milk from a bottle. Efforts should be aimed at preserving breast milk as much as possible, taking into account the special biological value of mother's native milk for an immature child and the important role of mother-child contact during feeding. For premature babies, free feeding is unacceptable due to their inability to regulate the amount of sucked milk and the high incidence of perinatal pathology. Babies born before 33 weeks' gestation are usually tube-fed to avoid the risk of aspiration resulting from a lack of coordination between sucking and swallowing. With a non-severe condition of the child and a body weight approaching 2000 g, a trial feeding from a bottle can be carried out, with unsatisfactory sucking activity, tube feeding is prescribed in full or in part. In order to maintain and maintain lactation in the mother, regular expression of breast milk is necessary. nine0003 Enteral feeding of very preterm infants (weighing less than 1500 g and less than 30 weeks' gestation) is carried out through a tube. The caloric method is used to calculate the required amount of feeding for premature babies. The calorie content of the diet of a prematurely born child increases gradually and daily. Caution and Graduality Feeding Guidelines for Premature Babies Less Than 33 Weeks Gestational Age Less Than 2000g For a premature baby, the best bioavailability is the milk of a woman who has given birth prematurely, then formulas for premature babies, and then the milk of a woman who has given birth at term. Women's milk after preterm birth has a special composition, it contains more protein, less lactose with the same total level of carbohydrates. In addition, it has a higher content of a number of protective factors, in particular lysozyme and secretory IgA. Despite the special composition, the milk of women who gave birth prematurely can satisfy the nutritional needs of only premature babies with a relatively large body weight - more than 1800-2000 g. Premature babies with a lower body weight are deficient in a number of nutrients. For them, breast milk must be further enriched with protein, calcium, phosphorus, iron, and vitamins. This can be achieved by replacing part of the required amount of breast milk with a specialized formula for premature babies or by adding breast milk enhancers. When enrichers (enhancers) are used, the main advantages of breastfeeding are preserved and at the same time the high nutritional requirements of the premature baby are ensured. With artificial feeding, specialized mixtures intended for feeding premature babies should be used. (Clinical perinatology). 2010;37(1):217-245.
(Clinical perinatology). 2010;37(1):217-245.  2006;118(1): e 115-123. - Thief B.R. et al., Developmental Beneficial Effects of Breast Milk in the Intensive Care Unit on Extremely Low Birth Weight Infants by 18 Months of Age. Pediatrix (Pediatrics). 2006;118(1):e115-123.
2006;118(1): e 115-123. - Thief B.R. et al., Developmental Beneficial Effects of Breast Milk in the Intensive Care Unit on Extremely Low Birth Weight Infants by 18 Months of Age. Pediatrix (Pediatrics). 2006;118(1):e115-123. 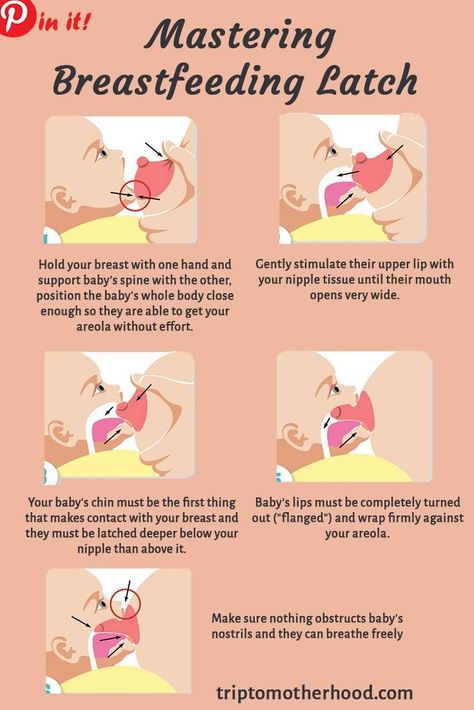
 J Perinatol. 2012;32(2):103-110. - Meyer P.P. et al., "Pumping patterns that mimic breastfeeding behavior: more milk and less time for constantly pumping mothers of preterm infants." nine0085 J Perinatol (Journal of Perinatology). 2012;32(2):103-110.
J Perinatol. 2012;32(2):103-110. - Meyer P.P. et al., "Pumping patterns that mimic breastfeeding behavior: more milk and less time for constantly pumping mothers of preterm infants." nine0085 J Perinatol (Journal of Perinatology). 2012;32(2):103-110.  - Lee J. et al., "Oropharyngeal colostrum ingestion in very preterm infants: a randomized controlled clinical trial." Pediatrix (Pediatrics). 2015;135(2):e357-366. nine0085
- Lee J. et al., "Oropharyngeal colostrum ingestion in very preterm infants: a randomized controlled clinical trial." Pediatrix (Pediatrics). 2015;135(2):e357-366. nine0085 
 nine0085 Acta Paediatr . 2010;99(6):820-826.- Nukvist K.H. et al., "On the Universality of the Kangaroo Method: Recommendations and Report from the First European Conference and the Seventh International Kangaroo Method Workshop". Akta Pediatr. 2010;99(6):820-826.
nine0085 Acta Paediatr . 2010;99(6):820-826.- Nukvist K.H. et al., "On the Universality of the Kangaroo Method: Recommendations and Report from the First European Conference and the Seventh International Kangaroo Method Workshop". Akta Pediatr. 2010;99(6):820-826. Read instructions before use. Consult a specialist about possible contraindications.
Features of feeding premature babies
 According to modern theory of nutrition programming the quantity and quality of nutrients supplied during the prenatal period and the first months of a child's life determines the nature of metabolism and, as a result, affects a person's health throughout later life.
According to modern theory of nutrition programming the quantity and quality of nutrients supplied during the prenatal period and the first months of a child's life determines the nature of metabolism and, as a result, affects a person's health throughout later life. 
 nine0003
nine0003