Pumping how much to feed baby
Feeding expressed milk | introducing bottle
When can you start feeding your baby expressed breast milk? What’s the best way to do it? And should you be concerned about ‘nipple confusion’? We answer your questions about expressed milk feeding
Share this content
When should I start giving my baby expressed milk?
If your baby is healthy and breastfeeding is going well, there’s no need to rush into giving her expressed milk. For the first four weeks, you’re working together to initiate and build your breast milk supply while she learns to breastfeed efficiently. While there is limited data,1 it is thought that unnecessarily introducing bottles during this crucial first month could interfere with these processes.
But if your newborn struggles to latch or suck for any reason, then start expressing milk as soon as possible after the birth. Read our articles on overcoming problems in the first week and feeding breast milk to your premature baby or infant with special needs for more advice, as well as getting support from your healthcare professionals.
How can I feed expressed milk to my baby?
There is a range of expertly designed feeding solutions that can help you give expressed milk to your baby, depending on your and her needs.
For example, Medela’s innovative Calma teat will only allow milk to flow when babies create a vacuum by sucking. This means they can feed from a bottle using the same technique, tongue motion and jaw movement they would at the breast.2,3 Developed with breastfeeding experts from the University of Western Australia, Calma allows your baby to suck, swallow, pause and breathe just as she does when breastfeeding.4 By maintaining babies’ natural sucking behaviour, Calma is designed to make it easy to switch from breast to bottle-feeding and back again.
Medela also makes conventional bottle teats in two flow versions. And all our teats can be attached directly to the bottles you express milk into, minimising the risk of spillages.
If your newborn needs expressed milk, but you don’t want to offer her a bottle until she’s become used to breastfeeding, you could use a baby cup designed for short-term feeding. This allows your baby to sip or lap your expressed milk – be careful to avoid spills! It’s advisable to have a healthcare professional on hand the first time you use the baby cup, to make sure you’re both getting the hang of it.
This allows your baby to sip or lap your expressed milk – be careful to avoid spills! It’s advisable to have a healthcare professional on hand the first time you use the baby cup, to make sure you’re both getting the hang of it.
For babies who need expressed milk supplements in addition to regular breastfeeding, a supplemental nursing system (SNS) can be helpful. This has a thin, flexible feeding tube that can be fixed alongside your nipple to give your baby expressed milk while you’re breastfeeding her. This allows your baby to stay at your breast longer, which further stimulates your breasts to help maintain your milk supply, and also helps improve her breastfeeding skills. It can be useful for mums with low milk supply or with adopted or surrogate babies.
If your baby can’t create the suction needed to breastfeed – perhaps because of a disability, congenital condition or weakness – you could try a feeder designed for babies with special needs. These allow infants who can’t suck to feed using gentle compression instead.
What’s the best way to introduce a bottle?
If breastfeeding is going well and you’ve decided it’s the right time to give your baby a bottle of expressed milk, follow these tips:
Take your time
Don’t wait until your big night out or first day back at work to introduce your baby to the bottle. Start trying with a small amount of expressed milk, in a relaxed and unhurried way, a couple of weeks beforehand. Gradually build up to giving a full feed of expressed breast milk from a bottle.
Pick your moment
Ideally your breastfed baby should be alert, but not too hungry, the first time she has a bottle of expressed milk, so that she is as relaxed as possible.
Delegate feeding duties
Your baby may be confused or frustrated when you offer a bottle, as she’s used to your breast. It might be easier if someone else gives the first bottle, and you stay out of the room so your baby can’t see or smell you.
Not too hot, not too cold
Your baby may be more likely to take the expressed milk if it’s around body temperature, 37 °C (98.6 °F).
Dip and sip
Try dipping the bottle teat into some expressed milk before offering it, so it tastes and smells of your breast milk. Then gently stimulate your baby’s top lip with the teat to encourage her to open her mouth.
Positioning for bottle-feeding
Feed your baby on demand and cuddle her in a semi-upright position. Never bottle-feed her while she’s lying flat or prop her up with the bottle, in case of choking. Go at her pace, with as many pauses as she needs – you can even try switching sides during the feed.
Be patient
Don’t worry if she doesn’t take to the bottle straight away – it may take several tries. If she pushes the bottle away or becomes upset, comfort her and wait a few minutes before trying again. If she still won’t drink from the bottle, wait a few more minutes and then breastfeed her as normal.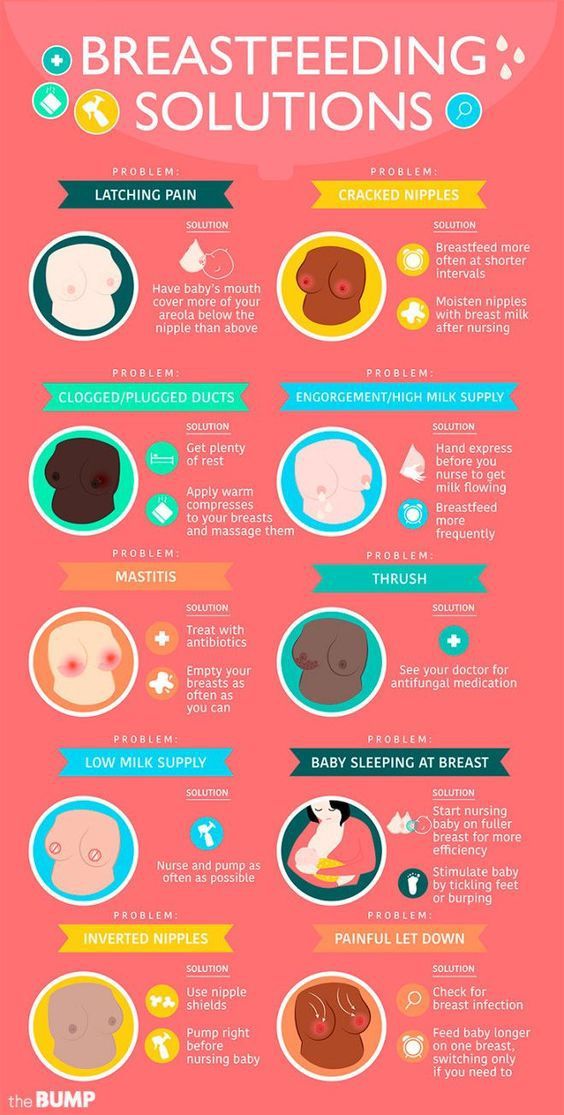 Try again with the bottle at a different time of day.
Try again with the bottle at a different time of day.
How much expressed milk should I give my baby?
Every baby is different. Research shows that in babies aged one to six months, one baby may take as little as 50 ml during a feed while another may take as much as 230 ml. Start by preparing a bottle with around 60 ml, and see if your baby needs more or less. You'll soon learn how much she typically takes – but don’t ever pressure her to finish the bottle.
How can I ensure bottle-feeding is safe for my baby?
Always clean and sanitise your breast pump set and bottles according to the instructions, and wash your hands before pumping, handling milk or feeding your baby. Follow our guidelines for storing and thawing your expressed milk safely.
If warming your breast milk, place the milk bottle or bag into a bowl of warm water or a warmer, or run it under a warm tap (max 37 °C or 98.6 °F). Never warm breast milk in the microwave or on the stove top.
Will my baby cope with switching from breast to bottle?
Mums sometimes worry that if they introduce a bottle too soon, their baby will get accustomed to the artificial teat and struggle to return to breastfeeding. Others are concerned about the opposite problem – if they don’t get their baby used to a bottle early she may never accept one later. Both of these problems are commonly referred to as ‘nipple confusion’.
Others are concerned about the opposite problem – if they don’t get their baby used to a bottle early she may never accept one later. Both of these problems are commonly referred to as ‘nipple confusion’.
Experts disagree on whether nipple confusion is really an issue.1 Certainly sucking from a conventional bottle teat that doesn’t require a vacuum to be created is less effort for a baby than sucking from mum’s nipple, as the milk flows more freely and gravity lends a hand. And some babies do seem to have a preference for breast or bottle, and never take to the other. But many babies switch happily between the two.
If you’re still struggling to feed your baby expressed breast milk, speak to a lactation consultant or breastfeeding specialist.
References
1 Zimmerman E, Thompson K. Clarifying nipple confusion. J Perinatol. 2015;35(11):895-899.
2 Geddes DT et al. Tongue movement and intra-oral vacuum of term infants during breastfeeding and feeding from an experimental teat that released milk under vacuum only. Early Hum Dev. 2012;88(6):443-449.
Early Hum Dev. 2012;88(6):443-449.
3 Segami Y et al. Perioral movements and sucking pattern during bottle feeding with a novel, experimental teat are similar to breastfeeding. J Perinatol. 2013;33(4):319-323.
4 Sakalidis VS et al. Oxygen saturation and suck-swallow-breathe coordination of term infants during breastfeeding and feeding from a teat releasing milk only with vacuum. Int J Pediatr. 2012;2012:130769.
How much expressed milk will my baby need? • KellyMom.com
By Kelly Bonyata, BS, IBCLC
- How much milk do babies need?
- What if baby is eating solid foods?
- Is baby drinking too much or too little expressed milk?
- Other ways of estimating milk intake
- References
Image credit: Jerry Bunkers on flickr
How much milk do babies need?
Many mothers wonder how much expressed breastmilk they need to have available if they are away from baby.
Now infants can get
all their vitamin D
from their mothers’ milk;
no drops needed with
our sponsor's
TheraNatal Lactation Complete
by THERALOGIX. Use PRC code “KELLY” for a special discount!
Use PRC code “KELLY” for a special discount!
In exclusively breastfed babies, milk intake increases quickly during the first few weeks of life, then stays about the same between one and six months (though it likely increases short term during growth spurts). Current breastfeeding research does not indicate that breastmilk intake changes with baby’s age or weight between one and six months. After six months, breastmilk intake will continue at this same level until — sometime after six months, depending in baby’s intake from other foods — baby’s milk intake begins to decrease gradually (see below).
The research tells us that exclusively breastfed babies take in an average of 25 oz (750 mL) per day between the ages of 1 month and 6 months. Different babies take in different amounts of milk; a typical range of milk intakes is 19-30 oz per day (570-900 mL per day).
We can use this information to estimate the average amount of milk baby will need at a feeding:
- Estimate the number of times that baby nurses per day (24 hours).

- Then divide 25 oz by the number of nursings.
- This gives you a “ballpark” figure for the amount of expressed milk your exclusively breastfed baby will need at one feeding.
Example: If baby usually nurses around 8 times per day, you can guess that baby might need around 3 ounces per feeding when mom is away. (25/8=3.1).
What if baby is eating solid foods?
Sometime between six months and a year (as solids are introduced and slowly increased) baby’s milk intake may begin to decrease, but breastmilk should provide the majority of baby’s nutrition through the first year. Because of the great variability in the amount of solids that babies take during the second six months, the amount of milk will vary, too. One study found average breastmilk intake to be 30 oz per day (875 ml/day; 93% of total intake) at 7 months and 19 oz (550 ml/day; 50% of total energy intake) at 11-16 months.
Several studies have measured breastmilk intake for babies between 12 and 24 months and found typical amounts to be 14-19 oz per day (400-550 mL per day). Studies looking at breastmilk intake between 24 and 36 months have found typical amounts to be 10-12 oz per day (300-360 mL per day).
Studies looking at breastmilk intake between 24 and 36 months have found typical amounts to be 10-12 oz per day (300-360 mL per day).
Is baby drinking too much or too little expressed milk?
Keep in mind that the amount of milk that baby takes at a particular feeding will vary, just as the amount of food and drink that an adult takes throughout the day will vary. Baby will probably not drink the same amount of milk at each feeding. Watch baby’s cues instead of simply encouraging baby to finish the bottle.
If your baby is taking substantially more than the average amounts, consider the possibility that baby is being given too much milk while you are away. Things that can contribute to overfeeding include:
- Fast flow bottles. Always use the lowest flow bottle nipple that baby will tolerate. Even with a slower flowing nipple, it is important to pace the bottle feed to allow baby to better control his intake.
- Using bottle feeding as the primary way to comfort baby.
 Some well-meaning caregivers feed baby the bottle every time he makes a sound. Use the calculator above to estimate the amount of milk that baby needs, and start with that amount. If baby still seems to be hungry, have your caregiver first check to see whether baby will settle with walking, rocking, holding, etc. before offering another ounce or two.
Some well-meaning caregivers feed baby the bottle every time he makes a sound. Use the calculator above to estimate the amount of milk that baby needs, and start with that amount. If baby still seems to be hungry, have your caregiver first check to see whether baby will settle with walking, rocking, holding, etc. before offering another ounce or two. - Baby’s need to suck. Babies have a very strong need to suck, and the need may be greater while mom is away (sucking is comforting to baby). A baby can control the flow of milk at the breast and will get minimal milk when he mainly needs to suck. When drinking from a bottle, baby gets a larger constant flow of milk as long as he is sucking. If baby is taking large amounts of expressed milk while you are away, you might consider encouraging baby to suck fingers or thumb, or consider using a pacifier for the times when mom is not available, to give baby something besides the bottle to satisfy his sucking needs.
- If, after trying these suggestions, you’re still having a hard time pumping enough milk, see I’m not pumping enough milk.
 What can I do?
What can I do?
If baby is taking significantly less expressed milk than the average, it could be that baby is reverse-cycling, where baby takes just enough milk to “take the edge off” his hunger, then waits for mom to return to get the bulk of his calories. Baby will typically nurse more often and/or longer than usual once mom returns. Some mothers encourage reverse cycling so they won’t need to pump as much milk. Reverse cycling is common for breastfed babies, especially those just starting out with the bottle.
If your baby is reverse cycling, here are a few tips:
- Be patient. Try not to stress about it. Consider it a compliment – baby prefers you!
- Use small amounts of expressed milk per bottle so there is less waste.
- If you’re worrying that baby can’t go that long without more milk, keep in mind that some babies sleep through the night for 8 hours or so without mom needing to worry that baby is not eating during that time period.
 Keep an eye on wet diapers and weight gain to assure yourself that baby is getting enough milk.
Keep an eye on wet diapers and weight gain to assure yourself that baby is getting enough milk. - Ensure that baby has ample chance to nurse when you’re together.
Other ways of estimating milk intake
There are various ways of estimating the amount of milk intake related to the weight of the baby and the age of the baby, based upon formula intake – research has shown that after the early weeks these methods overestimate the amount of milk that baby actually needs. These are the estimates that we used for breastfed babies for years, with the caveat that most breastfed babies don’t take as much expressed milk as estimated by these methods. Current research tells us that breastmilk intake is quite constant after the first month and does not appreciably increase with age or weight, so the current findings are validating what moms and lactation counselors have observed all along.
More:
- Breast Versus Bottle: How much milk should baby take? By Nancy Mohrbacher, IBCLC, FILCA
- Supplementation Guidelines from LowMilkSupply.
 org
org
References
Onyango, Adelheid W., Receveur, Olivier and Esrey, Steven A. The contribution of breast milk to toddler diets in western Kenya. Bull World Health Organ, 2002, vol.80 no.4. ISSN 0042-9686.
Salazar G, Vio F, Garcia C, Aguirre E, Coward WA. Energy requirements in Chilean infants. Arch Dis Child Fetal Neonatal Ed. 2000 Sep;83(2):F120-3.
Kent JC, Mitoulas L, Cox DB, Owens RA, Hartmann PE. Breast volume and milk production during extended lactation in women. Exp Physiol. 1999 Mar;84(2):435-47.
Persson V, Greiner T, Islam S, and Gebre-Medhin M. The Helen Keller international food-frequency method underestimates vitamin A intake where sustained breastfeeding is common. Food and Nutrition Bulletin, vol.19 no.4. Tokyo, Japan: United Nations University Press, 1998.
Cox DB, Owens RA, Hartmann PE. Blood and milk prolactin and the rate of milk synthesis in women. Exp Physiol. 1996 Nov;81(6):1007-20.
Dewey KG, Heinig MJ, Nommsen LA, Lonnerdal B. Maternal versus infant factors related to breast milk intake and residual milk volume: the DARLING study. Pediatrics. 1991 Jun;87(6):829-37.
Maternal versus infant factors related to breast milk intake and residual milk volume: the DARLING study. Pediatrics. 1991 Jun;87(6):829-37.
Neville MC, et al. Studies in human lactation: milk volumes in lactating women during the onset of lactation and full lactation. Am J Clin Nutr. 1988 Dec;48(6):1375-86.
Dewey KG, Finley DA, Lonnerdal B. Breast milk volume and composition during late lactation (7-20 months). J Pediatr Gastroenterol Nutr. 1984 Nov;3(5):713-20.
Butte NF, Garza C, Smith EO, Nichols BL. Human milk intake and growth in exclusively breast-fed infants. J Pediatr. 1984 Feb;104(2):187-95.
Dewey KG, Lonnerdal B. Milk and nutrient intake of breast-fed infants from 1 to 6 months: relation to growth and fatness. J Pediatr Gastroenterol Nutr. 1983;2(3):497-506.
Brown K, Black R, Robertson A, Akhtar N, Ahmed G, Becker S. Clinical and field studies of human lactation: methodological considerations. Am J Clin Nutr 1982;35:745-56.
Jelliffe D, Jelliffe E. The volume and composition of human milk in poorly nourished communities: a review. Am J Clin Nutr 1978;31:492-515.
The volume and composition of human milk in poorly nourished communities: a review. Am J Clin Nutr 1978;31:492-515.
| Summary of Research Data | ||||
| Baby’s Age | Average Milk Intake per 24 hours | Reference | ||
| g | ml | oz | ||
| 5 days | 498 +/- 129 g | 483 ml | 16 oz | Neville 1988 |
| 1 mo | 728 g | 706 ml | 24 oz | Salazar 2000 |
| 1 mo | — | 673 ml | 23 oz | Dewey 1983 |
| 1 mo | 708 +/- 54.7 g | 687 ml | 23 oz | Cox 1996 |
| 1-6 mo | 453.6+/-201 g per breast | 440 ml x2 = 880 ml | 30 oz | Kent 1999 |
| 3 mo | 818 g | 793 ml | 27 oz | Dewey 1991 |
| 3-5 mo | 753 +/- 89 g | 730 ml | 25 oz | Neville 1988 |
| 6 mo | — | 896 ml | 30 oz | Dewey 1983 |
| 6 mo | 742 +/- 79. 4 g 4 g | 720 ml | 24 oz | Cox 1996 |
| 7 mo | — | 875 ml (93% of total energy intake) | 30 oz | Dewey 1984 |
| 11-16 mo | — | 550 ml (50% of total energy intake) | 19 oz | Dewey 1984 |
| 11-16 mo | 502 +/- 34 g | 487 ml (32% of total energy intake) | 16.5 oz | Onyango 2002 |
| 12-17 mo | 563 g | 546 ml | 18 oz | Brown 1982 |
| 12-23 mo | 548 g | 532 ml | 18 oz | Persson 1998 |
| 15 mo | 208.0+/-56.7 g per breast | 202 ml x2 = 404 ml | 14 oz | Kent 1999 |
| 18-23 mo | 501 g | 486 ml | 16 oz | Brown 1982 |
| >24 mo | 368 g | 357 ml | 12 oz | Brown 1982 |
| 24-36 mo | 312 g | 303 ml | 10 oz | Persson 1998 |
Specific Gravity of Mature Human Milk = 1. 031, so Density of Mature Human Milk ~ 1.031 g/ml;1 oz = 29.6 ml;Numbers in gray were derived using the above conversion factors. 031, so Density of Mature Human Milk ~ 1.031 g/ml;1 oz = 29.6 ml;Numbers in gray were derived using the above conversion factors. | ||||
Expressing, storing and thawing breast milk
Unlike breastfeeding, which is a natural process, pumping works a little differently. That is why efforts should be made to keep the milk flowing during pumping. Here are some ways that can make pumping easier:
- Calm and pleasant environment
- Optimistic attitude
- Self-confidence and support of others
- Confidence in an emotional connection with the infant
- Having the baby present during pumping (if this is not possible, sometimes looking at his picture or smelling his clothes is enough)
- Soothing warm drink (not coffee)
- Hot shower or hot compresses before pumping
- Gently massage the nipples
- Gently stroke the areola and nipples with the fingertips
- Gently massage with clenched fists over the breast towards the nipple
- Massage the back between the shoulder blades along the spine with circular movements of the thumbs for several minutes
How to express milk?
First of all, wash your hands with soap and water. It is not necessary to wash the nipple specifically.
It is not necessary to wash the nipple specifically.
Principle of pumping:
In the first 3 days after birth, pump 5 minutes on each side, 3 times on each breast. From the fourth day (when milk already appears), you should express until the milk stops flowing and then switch to the second breast. A double-ended pump can express for at least 10 minutes. It should be pumped 8 times a day: once before bedtime, once after sleep and 6 more times during the day. There should be no more than 6 hours between evening and morning pumping, otherwise it may make pumping difficult.
You can massage your nipples with breast milk after every pumping.
If the mother is interested in breastfeeding in the future, this method is very important especially in the first weeks after childbirth, as it stimulates the production of milk in an amount sufficient for the child.
For your information: pumping is a temporary option. Once your baby is able to latch on (each baby has a different developmental rhythm), you can gradually transition to breastfeeding
- In the skin-to-skin position, you can let it slide a little lower towards the chest to get used to the position, sniff and lick the nipple name.
- It is advisable to give the baby fresh milk
- If you bring fresh milk in the morning or in the evening, they will prefer to use it first, and only then the frozen leftovers
- At a certain stage, the infant will begin to receive a breast milk supplement - HMF (Human Milk Fortifier), a fortifying supplement containing protein, calcium and phosphorus, which are not supplied to premature babies in sufficient quantities

Rules of behavior in the pumping room
- Wash hands before using the pumping device
- Only breastfeeding mothers are allowed to enter the pumping room, fathers are not allowed to enter so as not to cause discomfort to other women
- You can’t eat in the pumping room, you can and should drink
- Cleanliness and order should be observed
- After pumping, disassemble the bottles into parts and wash them in a specially designed machine
Storage of mother’s milk
Mother’s milk is stored in plastic sealed container, which can be obtained from a nurse. The label on the container will include your name, the date and time you pumped, and a sticker with your baby's details.
The label on the container will include your name, the date and time you pumped, and a sticker with your baby's details.
For premature babies and newborns, store milk in the refrigerator compartment for up to 24 hours, in the freezer for up to 4 months.
At home, you can store your expressed milk in the refrigerator for up to 4 days and in the freezer (not in the door) for up to 4 months.
In a cold place, breast milk separates into a more watery and fatty layer, you can shake it a little before drinking.
Again, freshly expressed milk is most preferred by the infant. If you are going to bring expressed milk from home, you must arrive at the office before 9in the morning so that fresh milk can be used on the same day, since the daily portions are prepared only in the morning.
Milk should be brought fresh or frozen in a container with ice.
Thawing breast milk
- Thawing breast milk is done at room temperature
- Thawed milk can be stored in the refrigerator for up to 24 hours
- Do not refreeze thawed milk
- Fresh milk is always preferred, but when the baby first starts eating it will be before total frozen colostrum used, in date and hour order (within the first 4 days of pumping).
- Heating breast milk after being in the refrigerator will only be heated in a special device by the ward nurse. Parents are not allowed to touch it. Heating milk in a microwave oven is not recommended, as the radiation destroys some of the ingredients.
Article "Pumping - when and how?"
There are times in the life of mother and baby when breastfeeding is either impossible or difficult for some reason. For example, a child has to be left without a mother for several hours - which means that a supply of milk is needed for him. Or in the case when the baby sucks badly at the breast, but eats well from the bottle, and pumping is the only way to feed him.
This can happen if the baby is born prematurely, and the very process of sucking the mother's breast turns out to be hard physical work for him - such an infant can also be offered expressed milk.
The same applies to the situation when the baby is ill and feeling unwell prevents him from fully sucking, as he is too weak to make the efforts necessary to "extract" breast milk. In this case, it should be expressed for 2 reasons: firstly, to provide the child with complete and optimal nutrition for him, and secondly, to maintain lactation.
In this case, it should be expressed for 2 reasons: firstly, to provide the child with complete and optimal nutrition for him, and secondly, to maintain lactation.
Situations are different, so it is important to understand why pumping is necessary, how to do it correctly and what are the conditions for storing breast milk.
When and why to express?
Pumping is the process by which a nursing mother manually or with the help of a breast pump extracts milk from her breast.
This is not a mandatory procedure for everyone, and it does not need to be carried out after each feeding, since the milk in the female breast is formed exactly as much as is needed to saturate the baby at a certain age. Those. how much milk the baby ate in one feeding - so much will appear in the breast by the next.
But if, after applying, you also express the rest of the milk, then by the upcoming feeding it will be produced more than the child can eat - and this often leads to stagnation of milk (lactostasis).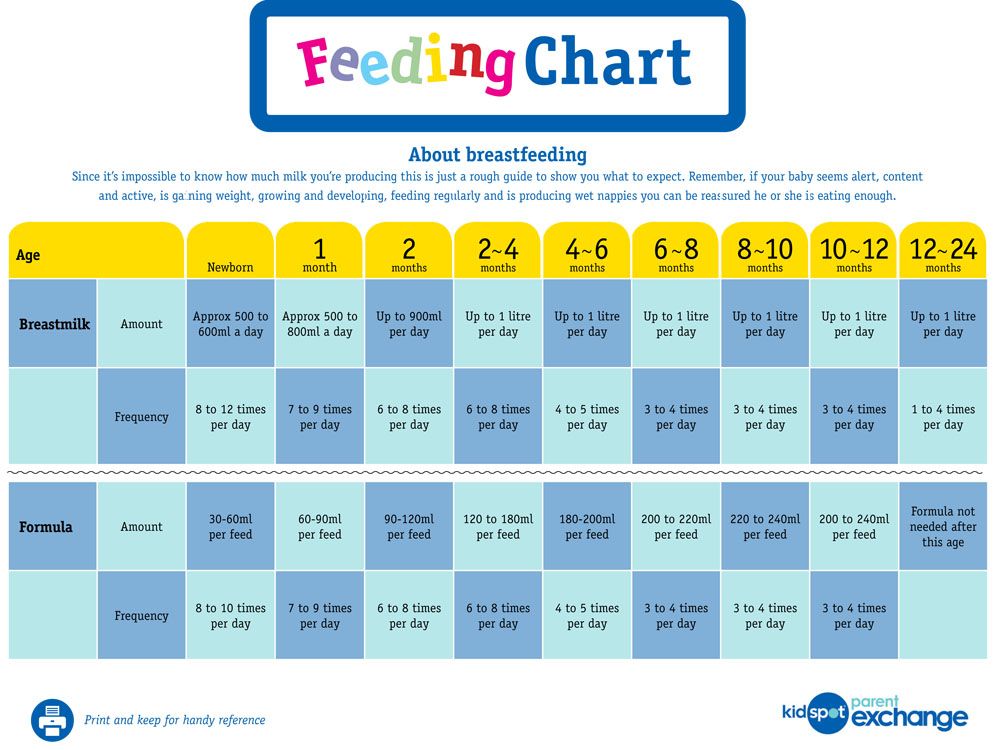
Milk should be expressed when:
-
Having to bottle feed or supplement a baby for one reason or another. If at the same time the pediatrician did not forbid the baby to eat breast milk, then the mother needs to feed the baby expressed.
-
The baby is left without a mother for a long time. There are times when a woman needs to go away, and she cannot take the child with her. In this case, you can leave a supply of milk for several hours, after decanting it.
-
Mom is sick. It happens that during lactation a woman becomes seriously ill and is forced to take medications that penetrate into breast milk, which is strictly forbidden to give to a child. Medicines contained in milk, once in the child's body, can have an adverse effect on it. To prevent this from happening, the pediatrician will help you choose the milk formula that you need to feed the baby during the mother’s illness. Pumping in such a situation will help a woman maintain lactation until recovery.
-
Mom goes to work. A mother's return to work before the end of lactation can put her before a choice: transfer the baby to formula milk or feed it with expressed milk. Recently, more and more parents are choosing the latter option, since breast milk is much healthier than artificial nutrition.
-
Injured nipples. With improper care and attachment of the child to the breast, cracks may appear on the nipples. Feeding in this condition of the nipples becomes very painful for the mother, and then the baby should be briefly transferred to expressed milk from a bottle. This is useful because the nipples are less likely to get irritated when they are expressed than when they are sucked by an infant. In a few days, the nipples will heal, and it will be possible to resume feeding the crumbs directly from the breast.
-
There is a risk of lactostasis. A child, especially in the first days after birth, is not always able to suck out all the milk.
 To avoid lactostasis, mom needs to express excess milk. If this is not done in a timely manner, stagnation of milk can lead to inflammation of the mammary gland - mastitis. However, you must follow all the rules of pumping and do not resort to it after each feeding: this will only increase the flow of milk.
To avoid lactostasis, mom needs to express excess milk. If this is not done in a timely manner, stagnation of milk can lead to inflammation of the mammary gland - mastitis. However, you must follow all the rules of pumping and do not resort to it after each feeding: this will only increase the flow of milk. -
Not enough milk is produced. Pumping will help normalize lactation, as it leads to an increase in the production of milk in the breast, which can be useful during a lactation crisis.
5 pumping inhibitions
In order not to harm herself and not leave the baby without breast milk, the mother must know and be sure to follow the basic rules of pumping:
-
Do not express more than 3 times a day if pumping is combined with breastfeeding because this will lead to excess milk production. If the mother is sick and the baby is not applied to the breast, it is necessary to express with a frequency approximately equal to the number of feedings (on average, once every 3 hours - 8 times a day).

-
Do not express immediately after feeding, as this may lead to hyperlactation, ie. increased milk production.
-
Do not express "to the last drop". The main indicator by the end of pumping should be a feeling of relief in the chest. The female body regards the emptying of the breast without a trace as an increased need for milk by the child - and begins to produce more milk, which the baby cannot eat, therefore, there will be a threat of milk stagnation.
-
Do not express during the night, as this may also lead to the formation of excess milk. The main hormone responsible for milk production - prolactin - has a daily rhythm of formation, most of all it is produced at night, in response to the baby sucking or pumping.
-
Do not express on the first day after the arrival of milk. Usually, when lactation begins, more milk is produced than the newborn needs, and it is necessary to get rid of its excess. Therefore, just at the time of the arrival of milk, you can not express everything without a trace.
 If the breast is very dense, then it is recommended to express only a small amount of milk so that it becomes softer and the baby can fully capture and eat it.
If the breast is very dense, then it is recommended to express only a small amount of milk so that it becomes softer and the baby can fully capture and eat it.
Substances that signal that milk is being produced in excess appear in the filled breast after about 1 day. If you express all the milk accumulated in the chest earlier than in a day, then it will be produced in the same amount.
Hand Expression Technique
There are two ways to express - manually and with a breast pump. Usually, each mother chooses the most convenient option for her. It is better to do it manually at home, when a woman has enough time, since the whole process will take some time. Breast pumps will help a working mother, which greatly facilitate the pumping process.
Rules for hand pumping
It is best to express milk 10-15 minutes after the end of feeding the baby. Wash your hands thoroughly beforehand. If you use any breast cream, wipe the skin and nipples with a cotton swab or pad soaked in breast milk. Prepare a wide-mouth milk container by first washing it under running water and then sterilizing it (by boiling, in a steam sterilizer or in a dishwasher).
Prepare a wide-mouth milk container by first washing it under running water and then sterilizing it (by boiling, in a steam sterilizer or in a dishwasher).
Sit comfortably, keeping your back straight, because pumping can take some time, and an uncomfortable position can cause back pain.
Gently grasp the chest: the little finger is under the chest at the ribs, the remaining fingers are positioned so as to support the chest from below. The thumb lies on top, about 3-4 cm from the nipple. In this case, the thumb and forefinger are located opposite each other, forming the letter "C".
Use your thumb and forefinger to gently press down on your chest and hold this position for a few seconds. In no case do not bring your fingers together, they should remain in the same position, the letter "C".
Repeat pressing, moving the palm in a circle - this way you will use all the ducts of the mammary gland.
Be patient, milk may not come out immediately, but only after a while. If you are pumping for the first time, check with your doctor or lactation consultant beforehand to show you how to proceed.
If you are pumping for the first time, check with your doctor or lactation consultant beforehand to show you how to proceed.
Manual pumping errors
Do not squeeze the nipple: this way you will only hurt yourself and injure the breast, and you will not express milk fully.
Do not press the palm too tightly against the skin, moving the hand across the chest so that there is no irritation and microtrauma.
Do not give up at the first unsuccessful attempts, be patient.
Breast pumps
Breast pumps make pumping much easier, as they are designed to fit all the anatomical features of the female breast.
Which one to choose? Breast pumps are divided into mechanical and electrical. In the first case, the pumping process is carried out manually: by squeezing the “pear”, the woman starts the suction mechanism. Electric models are good because they work independently: from the mains or from batteries (batteries, accumulators) and do not require additional effort on the part of the woman.
Mom usually chooses a breast pump model according to her taste and financial capabilities. It should be borne in mind that devices powered by batteries lose power faster than devices powered by the mains.
Many women are confused by the fact that electric breast pumps are loud enough. To date, there are a large number of silent devices, which is recommended to pay attention to when buying. The most effective are electric breast pumps that express both breasts at the same time and have the option of adjusting the thrust force and suction speed.
When choosing a breast pump, pay attention to the presence of the “boil and sterilize” marking. There must be the possibility of such heat treatment of parts of the apparatus. If the model cannot be boiled and sterilized, it is better to refuse to purchase it and look for another one.
Rules for expressing with a breast pump
Before pumping for the first time, carefully read the instructions for the device. Check that it is properly assembled.
Check that it is properly assembled.
Sterilize the funnel and sump (boil or use a sterilizer).
Position the funnel so that the nipple is in the center of the funnel.
The draw should be the lowest, especially at first, until the breast is accustomed to expressing with a breast pump. Each breast must be pumped until a feeling of relief, add 2 minutes to this time. On average, the process will take about 15 minutes.
Pumping, like manual pumping, should be carried out some time after feeding.
Basic mistakes when expressing with a breast pump
Incorrect position of the funnel of the breast pump can cause pain to the woman. Remember: the nipple should be located strictly in the center of the funnel of the device.
Very long pumping. Do not exceed the time required to collect milk, this can lead to hyperlactation (production of excess milk).
Very strong traction. If your breast pump has a selectable thrust function, you should use the smallest one so as not to hurt your breasts.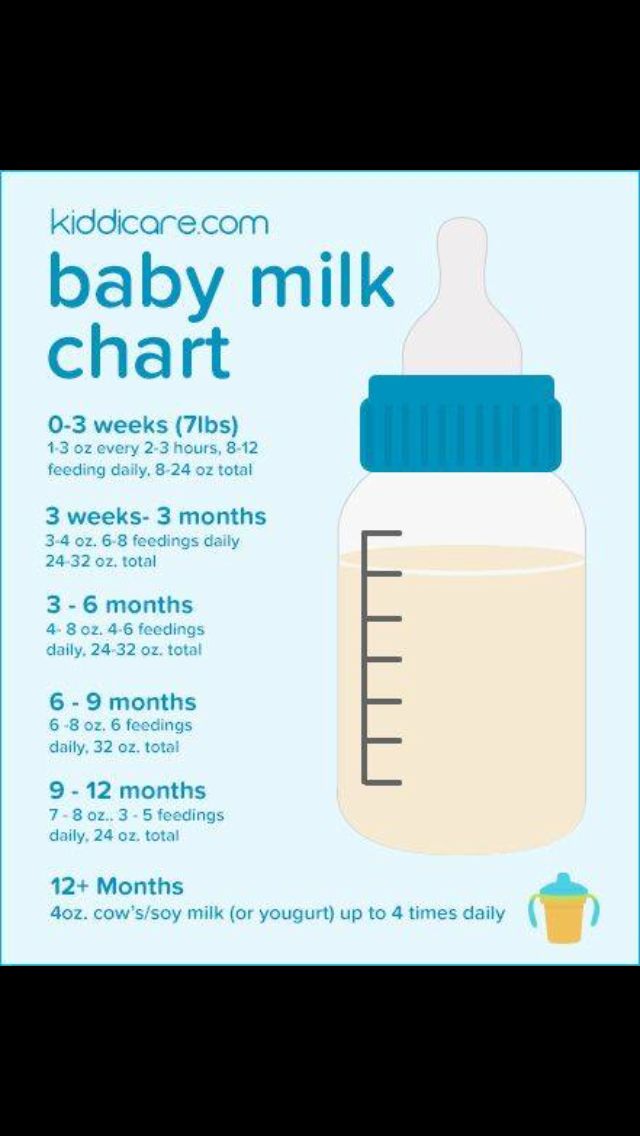
Care of the breast pump. A breast pump, like any machine, needs proper care. It must not be clogged so as not to contaminate the milk.
Each model has a care instruction, which you should definitely read before using the device.
When washing, always disassemble the pump completely, removing even the smallest parts. This will prevent stagnation of milk residues in them.
Before each use, sterilize all parts of the machine that come into contact with milk. This can be done with a sterilizer.
Milk defrosting
Never thaw or heat breast milk in a microwave oven. When heated in the microwave, the milk warms up unevenly, while feeding the baby can burn. Also, due to the rapid heating of frozen milk when using a microwave, most of the useful properties of this invaluable product are lost.
To defrost breast milk, place it on the refrigerator shelf, and when it becomes liquid, heat it up. To do this, lower the milk bottle into hot water or put it under hot water.