Reflux baby feeding position
How to Feed a Baby With Reflux – bökee
We know spit up down the front of your shirt isn’t your best look, but for many new moms, it’s a rite of passage. You finally just go with it because changing would mean even more laundry added to the ever-growing pile of burp cloths. But the truth is that changing the way you feed your baby can actually reduce or eliminate their uncomfortable reflux that’s causing all that spit-up.
Even though young babies’ immature digestive systems make them prime candidates for reflux, there are several feeding strategies we suggest to improve it. Not only does reflux cause spit-up, but it can also cause your baby a lot of discomfort, and we know more than anything you want your baby to feel good.
You’ll first want to identify if your baby is experiencing reflux and what might be causing it. Then we’ll give you our top tips to get your baby’s tummy back on track (and your shirts back to pristine condition.)
What is acid reflux in babies?When a baby drinks breast milk or formula, it has a tendency to back up from her stomach. This is referred to as reflux, or gastroesophageal reflux (GER). Reflux is most common during the newborn stage (0-4 months) and improves as time goes on.
According to the Mayo Clinic, this is because an infant’s ring of muscle between the esophagus and the stomach is not fully mature, allowing the contents of the stomach to flow backward.
So how do you know if your baby has reflux?
How to Identify Acid Reflux or GER in Your BabyMild reflux in young babies is common. According to Medline Plus, “About half of all babies spit up many times a day in the first 3 months of their lives.”
And even more will spit up about once or twice per day. In other words, it’s generally not a condition to be concerned about (and it’s temporary.)
Usually most parents just take the spitting up in stride if their baby seems comfortable and happy. In these cases, it’s mostly a nuisance to you while they could care less!
But there are also babies who may experience gas along with their reflux making them pretty uncomfortable or they might have what is called “silent reflux.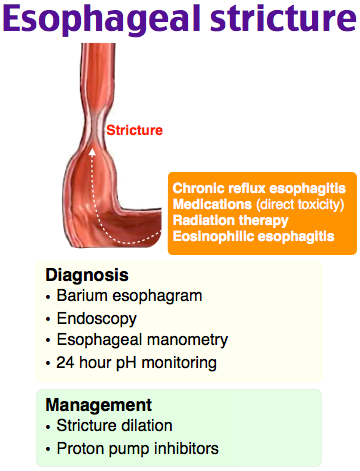 ”
”
Whereas a baby who spits up will usually feel instantly better, a baby experiencing silent reflux will likely be in pain. This is because the acid will come up the throat, but then they swallow it back down.
If you have a baby showing the following symptoms, they’re likely suffering from one of the types of reflux:
- Frequent spit-ups
- Arching body during or after feeding
- Crying when laid on their back
- Inconsolable crying after feeding (but could also be hours later)
- Pulling legs up
- Trouble sleeping
If your baby is under 4 months and growing well, you don’t need to be concerned about your baby’s reflux. But even though you don’t need to be “concerned,” it's still stressful when you feel like your baby isn't feeling their best but you can't help them.
Identifying your baby’s symptoms as reflux is the first step to fixing it. Knowing what causes it helps, too. That's when you’ll be able to utilize our tips to help your baby feel their best (while keeping the spit up to a minimum. )
)
The cause of reflux in a young baby is pretty straightforward. It’s really not about anything you’re doing wrong, instead, you just have a tiny little human on your hands whose digestive system is still maturing.
Other than that, the fact that babies lie on their backs so often and are on a completely liquid diet make them susceptible to reflux symptoms. Premature babies, especially, have a hard time.
This all sounds pretty standard, right? And the fact that your baby is on a 100% liquid diet is out of your control. Luckily, there are some easy strategies that you can start implementing today that will improve your baby’s reflux or even eliminate it altogether.
Feeding a Baby with Reflux: Top TipsWe at bökee are all parents. Though we can’t say necessarily that we’ve experienced it all, we’ve certainly experienced a lot raising babies. What we do know is that no two are alike and what works perfectly for your first baby will surely be the one thing that doesn’t work with the next.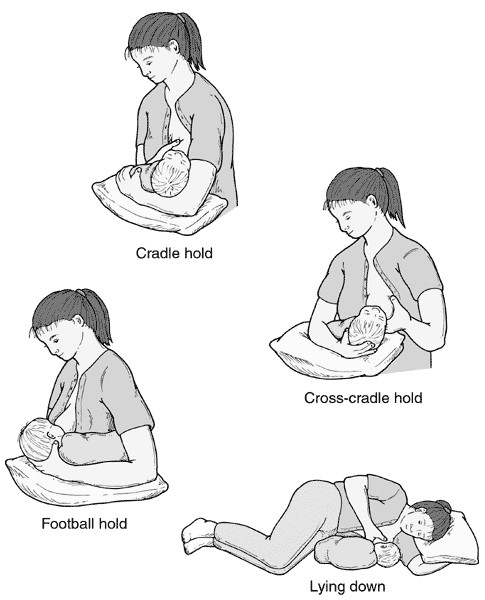 With that said, we suggest giving these different strategies a shot in order to help your baby through their reflux.
With that said, we suggest giving these different strategies a shot in order to help your baby through their reflux.
1.) Try Paced Bottle Feeding
If you bottle feed, implementing paced bottle feeding is a good place to start.
In a nutshell, paced bottle feeding utilizes the following:
- A slow-flow nipple
- An upright feeding position
- Only 20-30 seconds of continuous feeding and then pull the bottle back to give your baby a break
With paced bottle feeding, you slow down a bottle-feed in order to better mimic typical breastfeeding patterns. “Paced feeding reduces the risk of overfeeding that may result in discomfort to the baby,” writes the Minnesota Department of Health.
In our article, “How Paced Bottle Feeding Will Benefit Your Baby,” we discuss this feeding strategy further and give you the steps on how to put it into practice.
2.) Feed in Smaller Quantities, but More FrequentlyJust as paced bottle feeding reduces the likelihood that your baby will overeat and get reflux, feeding your baby in smaller quantities but more often can have the same effect.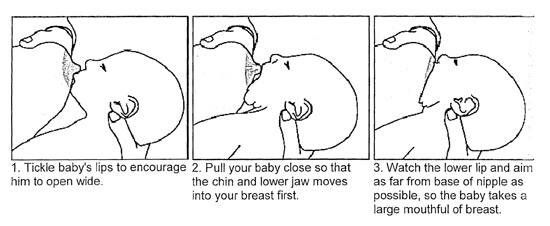
When babies take in a large meal at one time, it can be difficult to digest all at once. It also makes it more likely that some will come right back up through your baby’s immature ring muscle between the esophagus and stomach.
With this strategy, your baby will still drink the same amount of breast milk or formula in a 24-hour period, but could be given in 10 feeds instead of 7 (as an example.)
3.) Keep Baby in an Upright Position During Feeding and AfterBabies sleep a lot and that means a lot of laying down. But reducing this amount of time is one of the easiest ways to prevent reflux symptoms.
We recommend the following:
- Keep baby upright during feeds
- Hold your baby upright for the 20 - 30 minutes following a feed
- Wear your baby in a baby carrier so you can get a break while being able to keep your baby upright more often
With this said, we want to caution you against usually sleep positioners.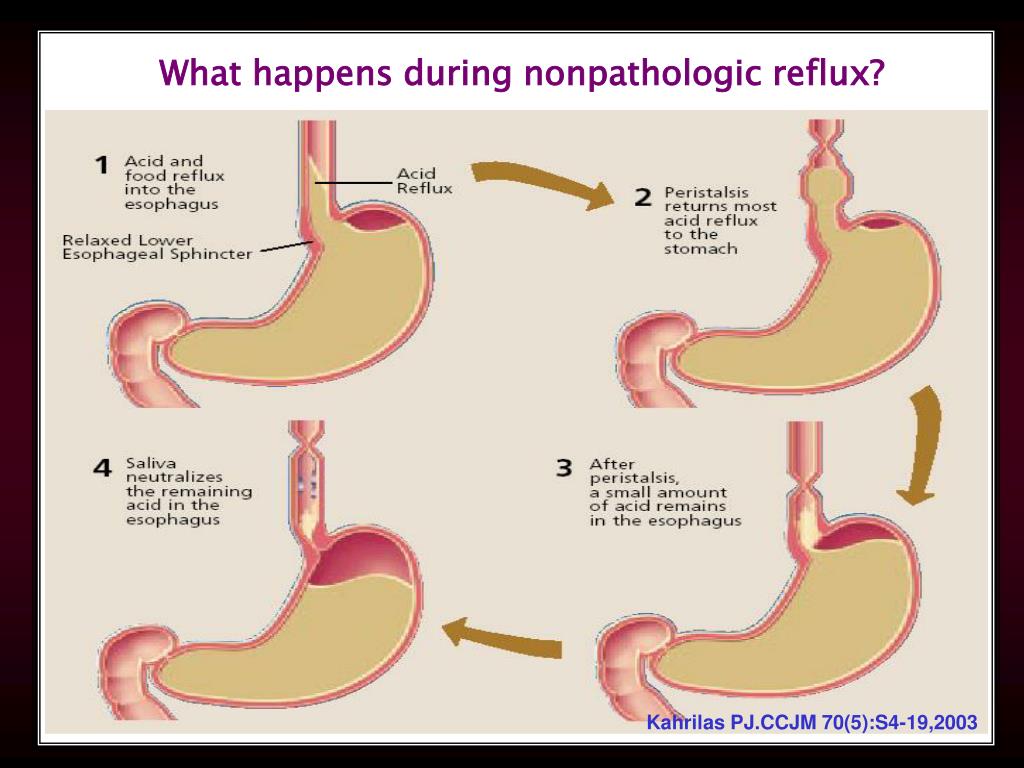 You may be tempted to try these due to their promises of reducing a baby’s reflux, but the AAP advises against their use due to SIDS concerns. Even babies with reflux should be placed on their back on a flat mattress to sleep.
You may be tempted to try these due to their promises of reducing a baby’s reflux, but the AAP advises against their use due to SIDS concerns. Even babies with reflux should be placed on their back on a flat mattress to sleep.
This works great with a paced bottle feeding approach. Every 20-30 seconds try burping your baby. At a minimum, you should burp your baby after every 1-2 ounces of milk ingested.
The best way to burp a baby experiencing reflux is by holding them with their tummy side against your chest and burping them over your shoulder.
This will allow for removal of trapped gas and acid from your baby’s system before giving them further milk to drink. They may still have “wet burps” but that's a whole lot better than a full-blown spit-up at the end of a feed!
The tips we just covered are the easiest to implement right away. And for many babies, it will be all you need to do! If your baby is still spitting up or is experiencing irritability related to gas or silent reflux, we recommend trying these last two suggestions:
5. ) Consider “Drops” Prior to or After Feeding
) Consider “Drops” Prior to or After FeedingGripe Water is a natural remedy that helps to relieve reflux and other infant stomach aches. The herbs can help ease digestion. Utilizing these drops in combination with the above recommendations will likely work for many babies.
If you think your baby’s discomfort is related to gas, Mylicon is an over-the-counter remedy that many parents swear by. It’s common for babies to have both reflux and gas, so it’s worth a shot if what you’ve done hasn’t shown a lot of improvement.
We love using these two options with the bökee. Because a baby experiencing silent reflux or gas is often crying and inconsolable, this leaves you having to open these bottles one-handed while you carry your baby in the other. The last thing you want to do is put your baby down in these moments. The bökee may have originally been designed for easier bottle prep, but it works great to stabilize medicine bottles to get the tops off so you can get the medicine to your baby more quickly.
Though it can be annoying to have to go out and buy a brand new set of bottles, getting the right bottle can often be the solution you’re looking for to eliminate your baby’s reflux. You'll want to look for bottles with a type of vent system that eliminates air bubbles in your baby's breast milk or formula.
You can find some great anti-reflux bottle options here.
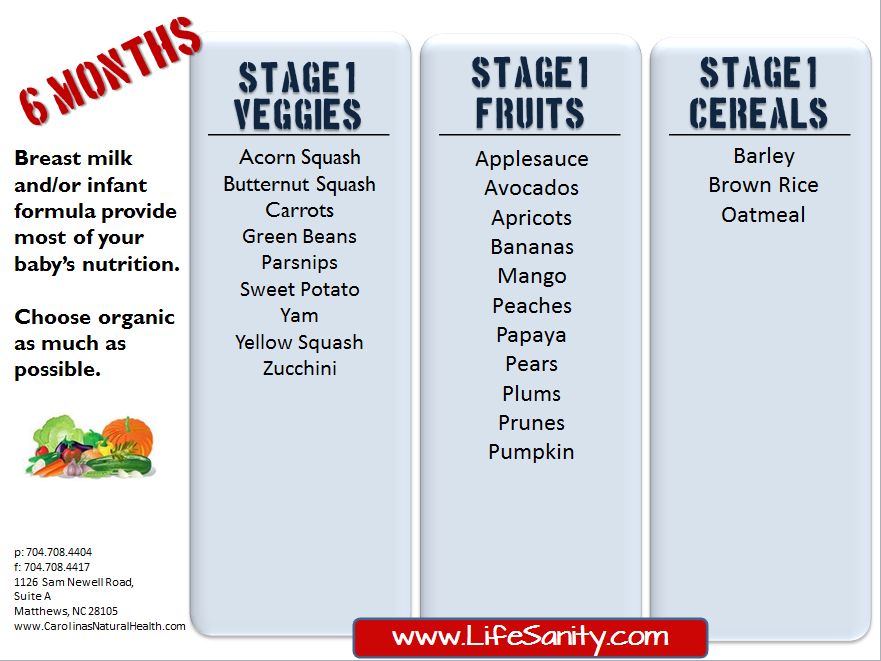
You may also see recommendations to use a special formula designed for reflux relief or to put rice cereal in your baby’s bottle to thicken your baby’s milk (making it more difficult for them to bring it back up). But these two options should be done at the direction of your doctor. So, how do you know when it’s time to contact your pediatrician?
When to Consult a Doctor for Your Baby’s RefluxThough mild cases of reflux can usually be improved by using the above strategies, some babies may need further intervention if those don’t help.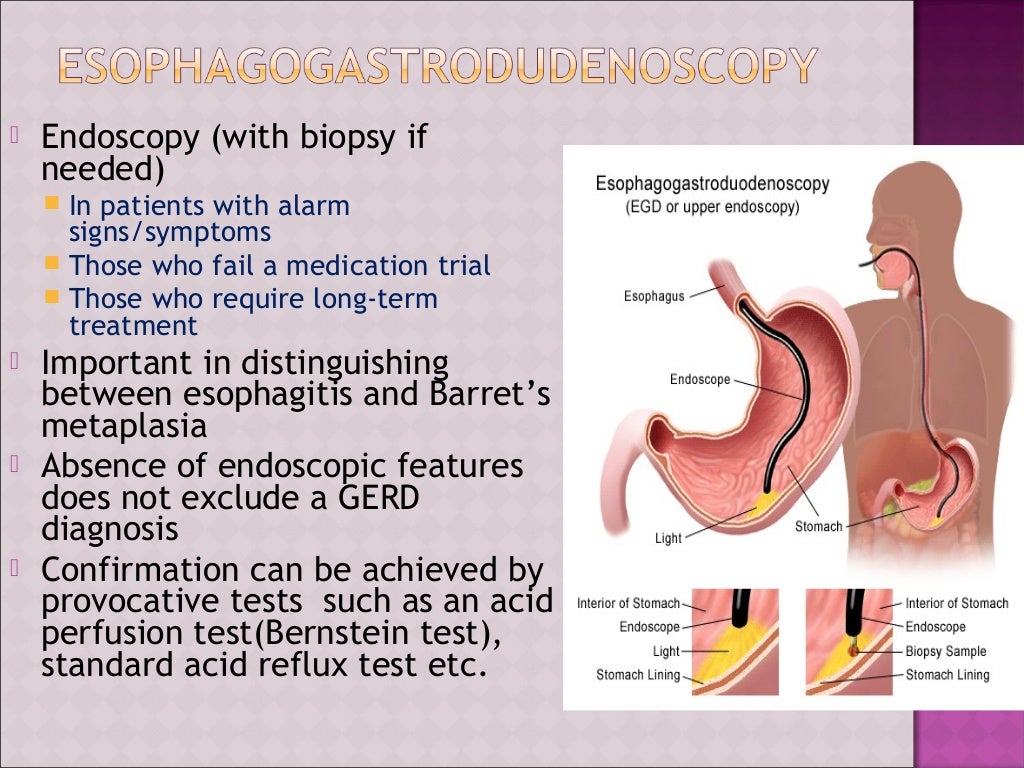
Babies who experience further distress may be experiencing a more severe form of reflux called GERD. Consulting a doctor at this time is necessary.
This may be noted by the following symptoms:
- Large volumes of spit-up
- Vomiting
- Difficulty eating
- low/no weight gain
If you notice any of these in your baby, getting direction from your doctor is imperative.
Final Word on Feeding a Baby With RefluxLuckily for most families, dealing with reflux and spit-up is a challenge that’s easy enough to work through. Taking the time to implement a few of the simple strategies above will help you avoid the milk stain while keeping a smile on your sweet baby’s face.
Best Breastfeeding Positions For Reflux, According To Experts
Breastfeeding
miniseries/E+/Getty Images
Gravity is your friend here.
by Cat Bowen
My son had the devil’s throat as a baby — also known as acid reflux. His was so bad that it would make him look like he was gasping for air. Doctors were confounded with its severity, especially because he was exclusively breastfed. For months we struggled, and it wasn’t until I learned how he needed to be held while he was breastfeeding, and after, that he started to improve. Certain breastfeeding positions for babies with reflux can make all the difference in their comfort.
But the thing about breastfeeding positions — especially breastfeeding positions for babies with reflux — is that they matter almost as much for the mom as they do the baby. If you can’t sustain that hold, you’re not going to do it. Many of these breastfeeding reflux positions are greatly eased with the help of a solid breastfeeding pillow. I know that they might seem like a frivolous purchase when you’re registering for your shower or strolling the beautiful lands of Target, but they’re a total lifesaver.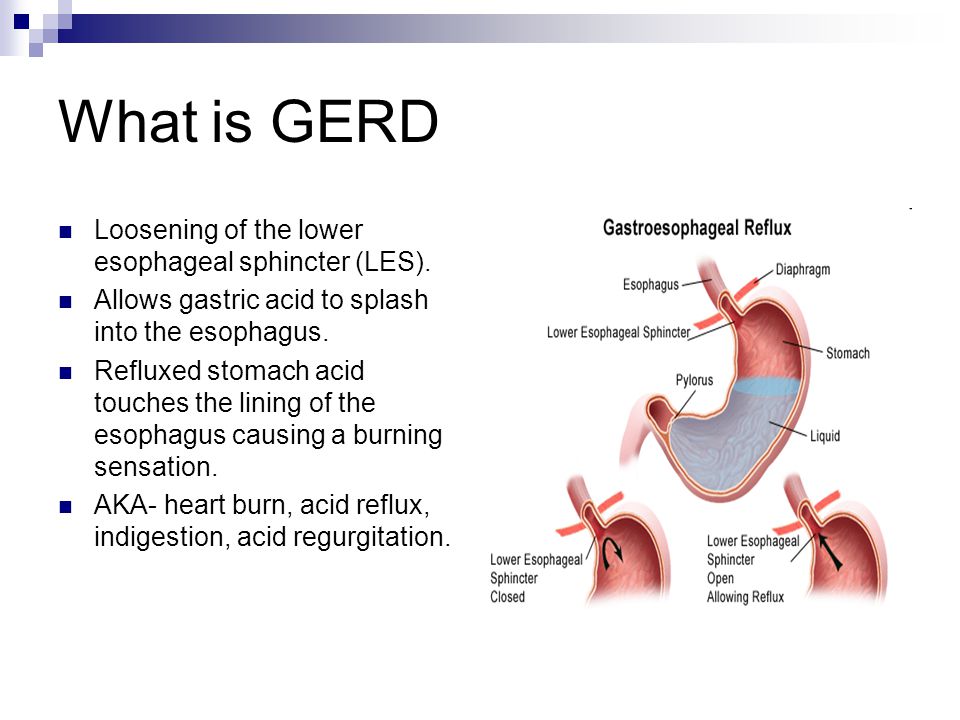
Thankfully, once you get comfortable, these breastfeeding positions for babies with reflux can really help you when you feel like you’re at your end, and trust me, I know what that’s like. Lactation consultants and feeding therapists have devised myriad solutions for these problems, and they’re more than willing to share. However, it’s important to get your baby seen by a pediatrician to determine if it is, in fact, reflux that is causing their discomfort and agitation before you do anything else.
1
Keep Your Baby’s Head Higher Than Their Belly
Oscar Wong/Moment/Getty ImagesJocelyn Bermudez, international board-certified lactation consultant (IBCLC) and host of the breastfeeding podcast The Snarky Boob Queens, tells Romper, “When a baby is struggling with reflux, we recommend positions where the baby's head is higher than their belly.” This might be with an upright or “koala” hold, where the mother essentially holds the baby in a vertical position in relation to their nipple.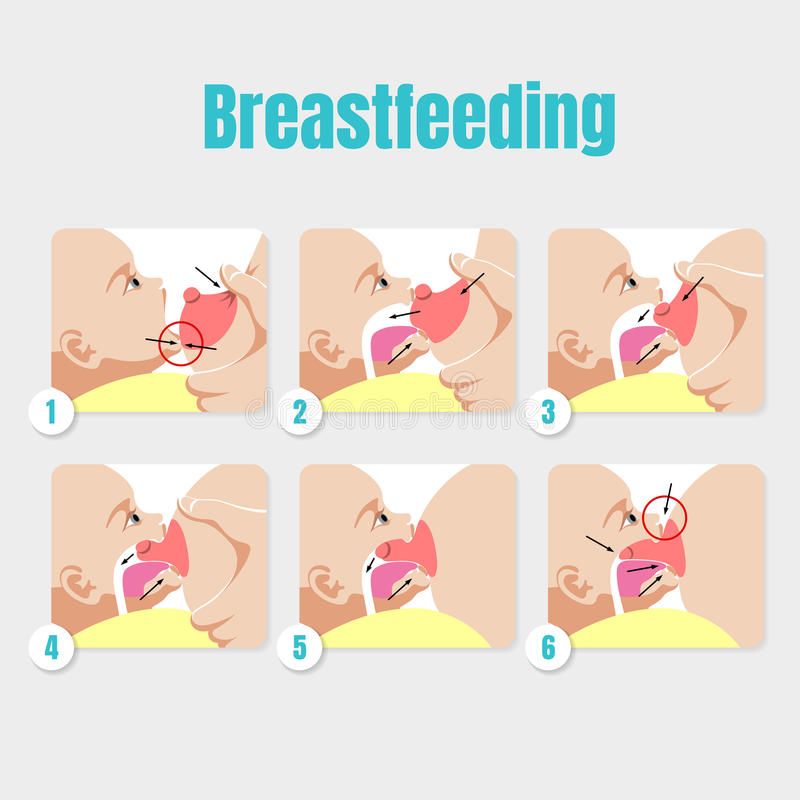 (Baby wrap-style carriers can be a godsend for this.)
(Baby wrap-style carriers can be a godsend for this.)
“The goal is to work with gravity to help aid in digestion,” she says. “Additionally, mothers should keep the baby upright after feedings, and burp when switching sides and at the end of the feeding.”
2
Position Your Baby Upright After Feeding, Too
Christine Miroddi, a feeding therapist and certified lactation supporter, cautions that parents should have their child evaluated before beginning therapeutic treatments. She notes that what you think may be reflux may actually be something else. But, if it is reflux, she echoes Bermudez’s recommendations. “There are several positions that allow the mom to hold baby upright,” Miroddi says, and you should try one of those.
But she also says, “A lot of remediation is also what happens after breastfeeding. That is just as important, if not more so.” These may take the form of burping, moving your baby, and baby positioning after feeding, according to the Seattle Children’s Hospital.
3
Football Hold
Andrea Tran, RN and IBCLC, tells Romper, “The football hold with baby in a sitting position is one of the best positions for reflux. This keeps the baby in a position where gravity helps keep the milk in the stomach.” This is where you hold the baby like you would a football, to the side, with their bottoms lower than their heads, with the assist of a pillow.
“Another good position is the straddle position for the same reason,” Tran says. The straddle position is similar to the koala, with a bit more assistance for the baby’s head.
Keeping baby’s head above their little body seems to be the universally accepted way of keeping reflux at bay, and that makes sense. Think of when you’ve had reflux (hello, third trimester!) — lying flat on your back after eating was torture, right? When you were slightly elevated, or sitting up, things were a lot more comfortable. The trick to feeding your baby with reflux is similar. Keep them upright, keep them burped, and hold them in that position for as long as necessary.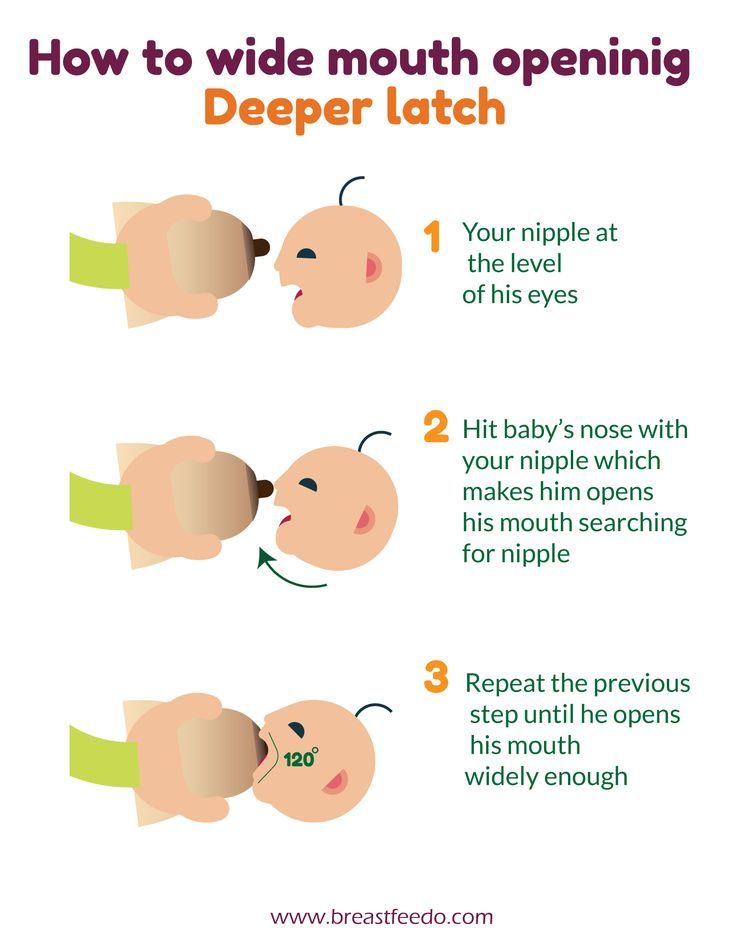 And as ever, talk to your provider about your child’s discomfort.
And as ever, talk to your provider about your child’s discomfort.
Experts:
Jocelyn Bermudez, IBCLC, host of The Snarky Boob Queens
Christine Miroddi MA CCC-SLP, CLSE, TSSLD
Andrea Tran, RN, IBCLC
Infant Reflux: Symptoms and Treatment
Search Support IconSearch Keywords
Home ›› What is Reflux in Infants?
Home ›› What is reflux in babies?
↑ Top
Signs and what to do
Post-feed regurgitation is a common occurrence in the first few months of life. This is usually harmless and completely normal, but parents should read about gastroesophageal reflux (GER) and laryngopharyngeal reflux (LPR) in infants and how long it lasts to give them peace of mind.
We look at signs of reflux in babies, symptoms of different types of reflux, and how to help a child with signs of reflux. If you require further information, always contact your healthcare provider.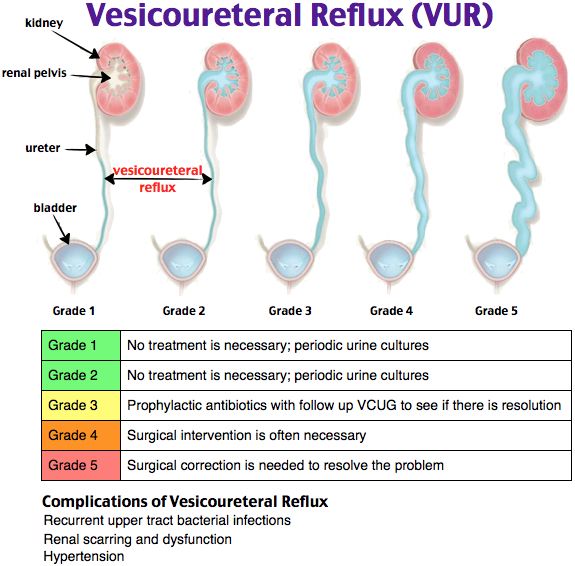
What is reflux in babies?
So we know reflux is common, but what causes reflux in babies? Because young children have not yet fully developed the lower esophageal sphincter (LES), that is, the muscle at the bottom of the esophagus that opens and closes to let food into the stomach and keep it there, food can easily pass back up the esophagus.
Acid reflux, also known as gastroesophageal reflux (GER), is a normal reflux that occurs in babies. This type of reflux is considered normal and occurs in 40-65% of babies.
How do I know if my child has acid (gastroesophageal) reflux?
If a baby is spitting up milk after a feed, it is most likely acid reflux. As babies get older, GER usually goes away on its own without any intervention. If a baby has complications beyond just spitting up a small amount of milk (such as feeding difficulties and discomfort), they may have gastroesophageal reflux disease (GERD).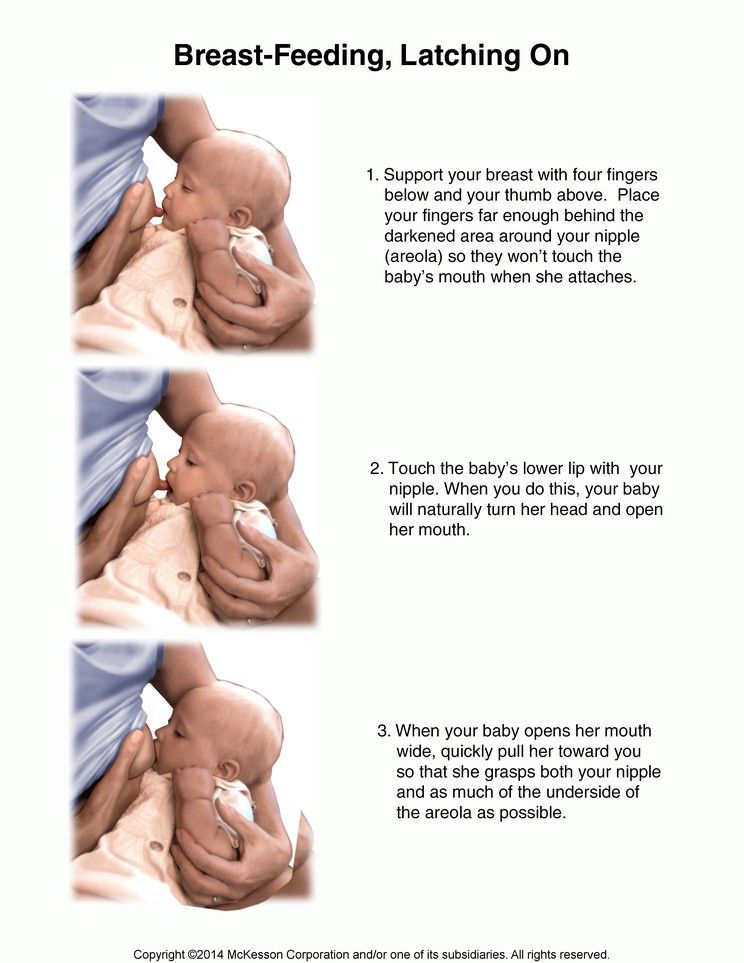
Symptoms of GERD include:
- baby arching during or after feeding;
- crying more than three hours a day for no apparent reason;
- cough;
- gag reflex or difficulty swallowing;
- irritability, restlessness after eating;
- eating little or not eating;
- poor weight gain or loss;
- difficult breathing;
- severe or frequent vomiting.
GERD usually occurs when LES muscles are not toned in time, causing stomach contents to back up into the esophagus.
How do I know if my child has Laryngopharyngeal Reflux?
Another type of reflux, laryngopharyngeal reflux (LPR), also called silent reflux, is when the contents of the baby's stomach leak back into the larynx, the back of the nasopharynx. This type of reflux does not always cause external symptoms, which is why it is called "silent". Babies can have GERD and silent reflux at the same time, but their symptoms are somewhat different.
The following are some of the symptoms of laryngopharyngeal reflux:
- breathing problems;
- gag reflex;
- chronic cough;
- swallowing problems;
- hoarseness;
- regurgitation;
- poor weight gain or weight loss.
We have looked at the signs of reflux in infants, now we will move on to the treatment and duration of silent reflux in children, as well as the treatment of GERD.
How to deal with laryngopharyngeal reflux in babies while breastfeeding?
Breastfeeding mothers may need to review their diet if their babies show signs of reflux. The American Academy of Pediatrics (AAP) recommends breastfeeding mothers cut eggs and milk from their diet for two to four weeks to see if their baby's reflux symptoms improve or disappear. It may be worth eliminating acidic foods from your diet.
In most cases, GER and laryngopharyngeal reflux go away on their own.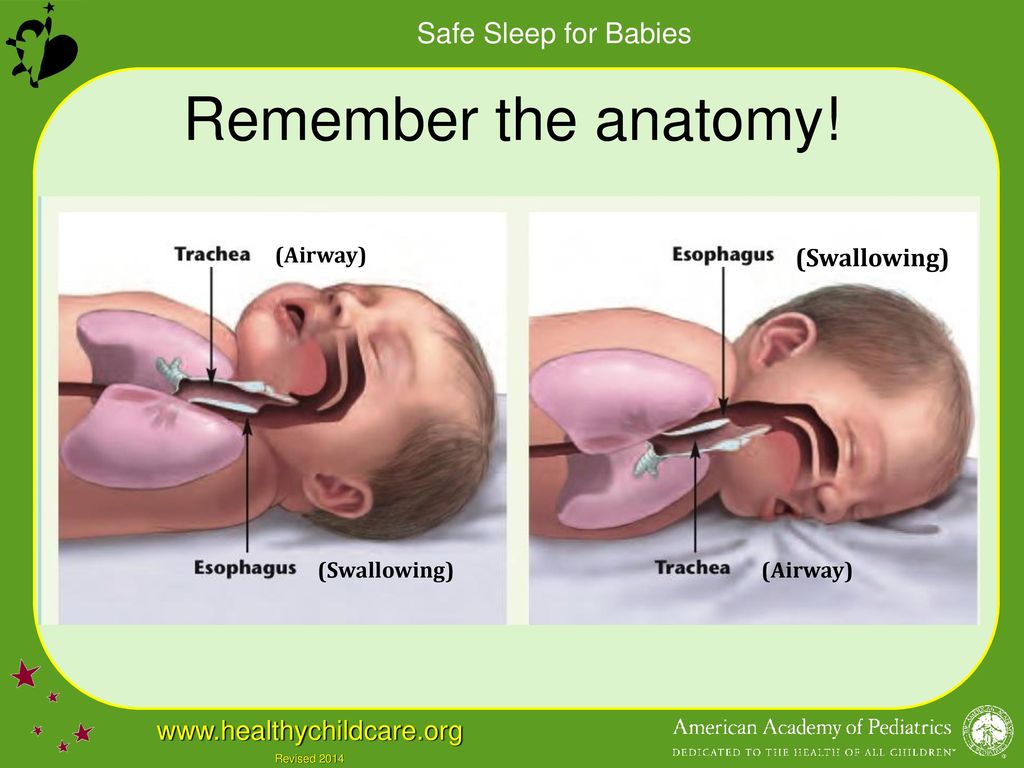 Typically, children outgrow reflux in the first year of life. If a child has persistent symptoms of laryngopharyngeal reflux, parents should consult a doctor. If your baby has severe vomiting, blood in the stool, or any of the symptoms of GERD listed above, parents should contact their pediatrician as soon as possible.
Typically, children outgrow reflux in the first year of life. If a child has persistent symptoms of laryngopharyngeal reflux, parents should consult a doctor. If your baby has severe vomiting, blood in the stool, or any of the symptoms of GERD listed above, parents should contact their pediatrician as soon as possible.
How can I help my child with reflux or GERD?
Reflux symptoms in babies usually go away on their own, but the following tips can help relieve symptoms:
- Thicken food with rice or a special milk thickener.
- Hold the bottle at an angle that fills the nipple completely with milk to reduce the amount of air your baby swallows. This can help prevent colic, gas, and reflux.
- Try the AirFree anti-colic bottle, designed to reduce air swallowing during feeding.
4. Let the baby burp during and after feeding. If the baby is bottle fed, parents can let him burp after every 30-60 ml. If the mother is breastfeeding, she may let the baby burp when changing breasts.
5. Hold baby upright after feeding. As a rule, in order for the milk to remain in the stomach, after feeding the baby, it is necessary to hold it in an upright position for 10-15 minutes. But, if the child has reflux, parents should keep him upright a little longer.
These tips may help relieve symptoms, but they do not replace a doctor's advice.
Parents should not change their infant formula formula without first talking to their healthcare provider.
Don't panic! Reflux is very common in babies during the first three months of life, and most babies outgrow it without any consequences. Although GERD is a slightly more serious condition, there are many treatments, ways to manage it, and help newborns. Feel free to contact your doctor with any questions or concerns you may have.
4 Seattle Children’s Hospital
5 The National Institute of Diabetes and Digestive and Kidney Diseases - Treatment for GER & GERD in Infants
Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain.
Philips makes no warranties regarding any third party websites or the information they contain.
I understand
You are about to visit a Philips global content page
Continue
You are about to visit the Philips USA website.
I understand
Different breastfeeding positions
Try different breastfeeding positions to find the one that works best for you and your baby. You can see the options in our selection of photos
Share this information
There is no right or wrong way to hold your baby while
feeding, and mom and baby are sure to find their favorite position.
It is important that both you and your baby feel comfortable. 1.2 It's good to learn a few different breastfeeding positions and techniques because life's circumstances often require us to be flexible, especially as your baby gets older and you start to leave the house more often.
Whatever position you choose to breastfeed your baby, remember a few simple rules.
- Prepare everything you need before feeding, including drinks, food, mobile phone, TV remote control, book or magazine. And do not forget to go to the toilet - the feeding process can take a long time!
- Make sure your baby is comfortable. Whichever position you choose, it's important to keep your baby strong, level, and provide good support for their head, neck, and spine.
- You should also be comfortable. Don't stress. If necessary, use pillows of different sizes or rolls of towels to support your back or arms.
- Make sure your baby is latching on correctly. Proper grip is the key to comfort when breastfeeding.
- If your baby does not latch on well or you experience pain while feeding, contact a lactation consultant for help. The specialist will also be able to show you how to hold your baby more comfortably.
1. Relaxed feeding or reclining position
Relaxed feeding position, also known as biological feeding, 1 is often the first position for most mothers. If, immediately after birth, the baby is placed on the mother’s chest or stomach, normally, he instinctively reaches for the breast and tries to grab the nipple. This phenomenon is known as the breast seeking reflex. Skin-to-skin contact stimulates the infant's feeding instinct, and gravity helps him to latch onto the breast and maintain balance.
If, immediately after birth, the baby is placed on the mother’s chest or stomach, normally, he instinctively reaches for the breast and tries to grab the nipple. This phenomenon is known as the breast seeking reflex. Skin-to-skin contact stimulates the infant's feeding instinct, and gravity helps him to latch onto the breast and maintain balance.
But it's not just newborns that can be fed in the reclining position - this position is great for babies of all ages. It can be especially helpful if your baby does not latch well in other positions or does not like to be touched during feeding, and also if you have too much milk flow or too large breasts. Isabelle, a mother from the UK, shares her experience: “I had large breasts, and the baby was born small - 2.7 kg, so it was not easy to find a comfortable position at first. After a few weeks, it became clear that there was no “correct” posture for me. As a result, I most often fed lying down, putting the baby on my chest. ”
It is more convenient to feed not lying flat on your back, but half-sitting, leaning on pillows. So you will have a back support and you will be able to watch the baby during feeding.
So you will have a back support and you will be able to watch the baby during feeding.
2. Cradle position
This is the classic
pose that comes to mind when breastfeeding a baby. Mom sits
straight, and the baby lies on her side on her arm, pressing her stomach against her stomach. 3 Although this is a very popular position, it is not always easy to master with newborns because it gives the baby less support. Try putting a pillow under your back, and put a special breastfeeding pillow on your knees and lean on it with your hands. So you can more reliably support the child, without overstraining your back and shoulders. Just make sure that the baby does not lie too high on the pillow for feeding. The breast should remain at a natural level so that the baby can grab it without effort, otherwise sore nipples cannot be avoided.
“I breastfed in the cradle position because it suited me perfectly! It was comfortable and I loved just sitting and looking at my little one,” recalls Rachel, a mother of two from Italy.
3. Cross Cradle
This breastfeeding position looks almost exactly like the cradle, but the baby is on the other arm. 3 This gives baby support around the neck and shoulders so he can tilt his head to latch on. This position is great for breastfeeding newborns and small babies, as well as for babies who do not latch well. Since the baby lies completely on the other hand, it becomes easier to control his position and you can adjust the chest with your free hand.
Julie, a UK mother of two, finds this position very practical: “I usually breastfeed my youngest in the cross cradle position. So I have a free second hand, and I can take care of an older baby at the same time. ”
Do not hold the baby's head at first, otherwise you may inadvertently press his chin against his chest. Because of this, the child will not be able to take the breast deeply, because the nipple will rest against the base of the tongue, and not against the palate, which will lead to inflammation of the nipples. As the child grows, this position becomes more comfortable, and he can rest his head on your palm (as shown in the photo above).
As the child grows, this position becomes more comfortable, and he can rest his head on your palm (as shown in the photo above).
4. Underarm breastfeeding
In this position, also known as the "ball grip", the mother sits with the baby lying along her arm at the side, legs towards the back of the chair (or any other seat). 3 This is another comfortable position for newborn breastfeeding, in which you can give your baby good support, have full control of his position and have a good view of his face. And the baby feels safe in close contact with the mother's body. This position is especially good for those who have had a caesarean section or a premature birth, as well as mothers of twins and women with large breasts.
“When I breastfed my first daughter, I had very large K-sized breasts—twice the size of her head,” recalls Amy, an Australian mother of two. - I put rolls of towels under each breast, because they were very heavy, and fed my daughter in a pose from under the arm, but only sitting straighter so as not to crush her.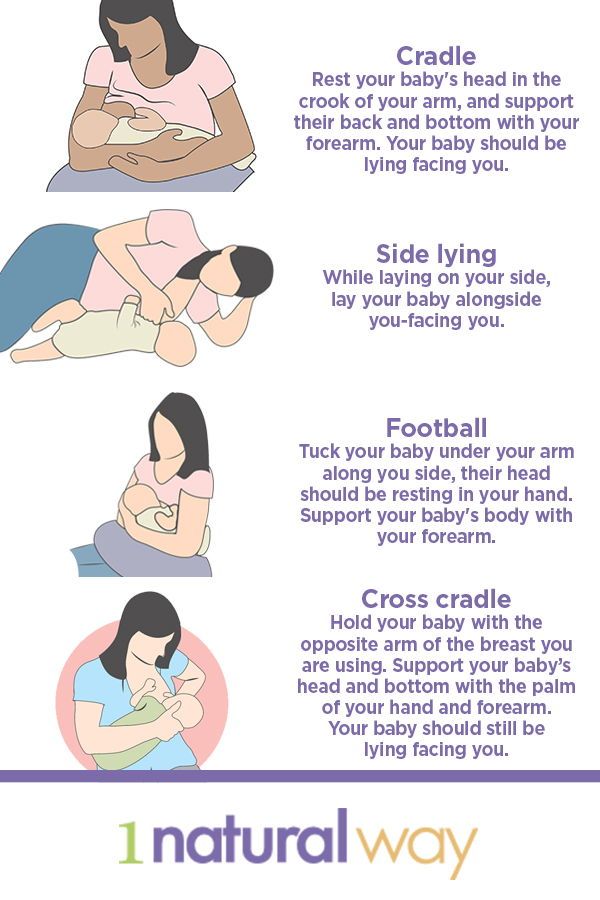 This position was also convenient because I had a caesarean section and could not put the baby on my stomach.”
This position was also convenient because I had a caesarean section and could not put the baby on my stomach.”
5. Side-lying position
The side-lying position is ideal for relaxed
feeding at night in bed or on the couch. If you had a
caesarean section or ruptures during childbirth, this position may be more comfortable than sitting down. 3 In this position, mother and baby lie side by side, tummy to tummy.
“It was difficult for me to sit during endless night feedings, firstly because of the caesarean section, and secondly because of lack of sleep,” recalls Francesca, a mother from the UK. “And then I discovered that you can feed your baby lying on your side and rest at the same time.”
“Because of the short tongue frenulum, Maisie could only properly latch on to her breasts while lying on her side. The lactation consultant showed me how it's done. In this position, the flow of milk was optimal for my daughter, and it was easier for her to keep the nipple in her mouth.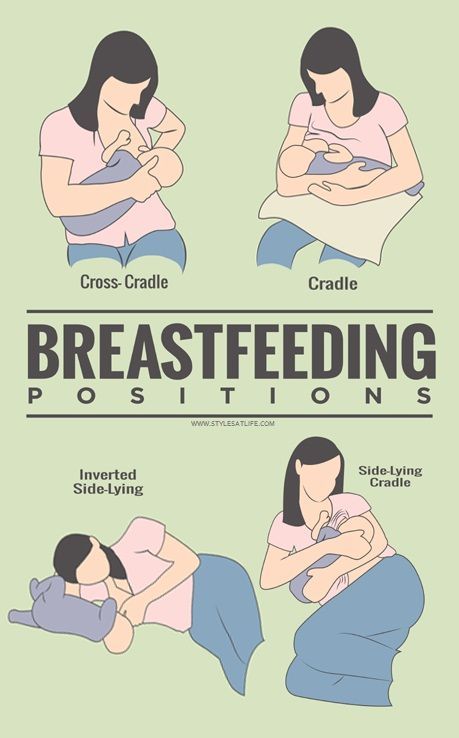 As she got older, she became much better at grabbing her breasts in normal positions,” says Sarah, mother of two from Australia.
As she got older, she became much better at grabbing her breasts in normal positions,” says Sarah, mother of two from Australia.
6. Relaxed breastfeeding after caesarean section
If you can't find a comfortable position for breastfeeding after caesarean section, 3 try to hold the baby on the shoulder while reclining — this does not put pressure on the postoperative suture and allows you to breastfeed the baby comfortably. You can also try side feeding.
7. Upright breastfeeding or “koala pose”
When breastfeeding in an upright position or “koala pose”, the baby sits with a straight back and head up on the mother's hip. 4 This position can be tried even with a newborn if it is well supported, but it is especially convenient for feeding a grown child who can already sit up by himself. The upright sitting position, or “koala pose,” is great for toddlers who suffer from reflux or ear infections and feel better sitting. In addition, this pose may be suitable for children with a shortened frenulum of the tongue or reduced muscle tone.
“When my daughter got a little older, I would often feed her in an upright position, which was more comfortable for both of us, and I could still hold her close,” recalls Peggy, a mother from Switzerland. “Besides, it was possible to discreetly breastfeed her in public places.”
8. Overhanging position
In this position, the baby lies on his back, and the mother bends over him
on all fours so that the nipple falls directly into his mouth. 4 Some mothers have said that this breastfeeding position is good to use from time to time for mastitis, when touching the breasts is especially unpleasant. Some say that this breastfeeding position helps with blockage of the milk ducts, although there is no scientific evidence for this yet. You can also feed in the “overhanging” position while sitting, kneeling over the baby on a bed or sofa, as well as reclining on your stomach with support on your elbows. Pillows of various sizes that you can lean on will help you avoid back and shoulder strain.
“I have breastfed several times in the 'overhang' position for clogged milk ducts when no other means of dissolving the blockage worked. And this pose seems to have helped. I think it's because of gravity, and also because the breasts were at a completely different angle than with normal feeding, and my daughter sucked her differently, ”says Ellie, a mother of two from the UK.
Feeding in the "overhanging" position is unlikely to be practiced regularly, but in some cases this position may be useful.
“I used to breastfeed in the overhang position when my baby was having trouble latch-on,” says Lorna, mother of two in the UK. - This, of course, is not the most convenient way, but then I was ready for anything, if only he could capture the chest. We succeeded and have been breastfeeding for eight months now!”
9. Feeding a baby in a sling or “on the fly”
Breastfeeding in a sling takes some practice, but it can be used to go out of the house, look after older children or even do a little household chores.
The sling is also useful if the baby does not like to lie down or is often attached to the breast. Lindsey, a mother of two in the US, notes: “I used the carrier frequently for both of my children. When we were out, I tied the sarong around my neck and covered the carrier with it. Under such a cape, the baby can eat as much as he wants until he falls asleep.
This breastfeeding position is best when the baby is already good at breastfeeding and can hold his head up by himself. Any slings are suitable for breastfeeding, including elastic and rings, as well as carrying bags. Whatever option you choose, the main thing is that you can always see the face of the child, and his chin does not rest against his chest.
10. Double hand-held breastfeeding
Double hand-held breastfeeding (or “double-ball grab”) is great for moms of twins—you can breastfeed both at the same time and still have relatively free hands. 4 When feeding in this position, it is advisable to use a special pillow for breastfeeding twins, especially at first.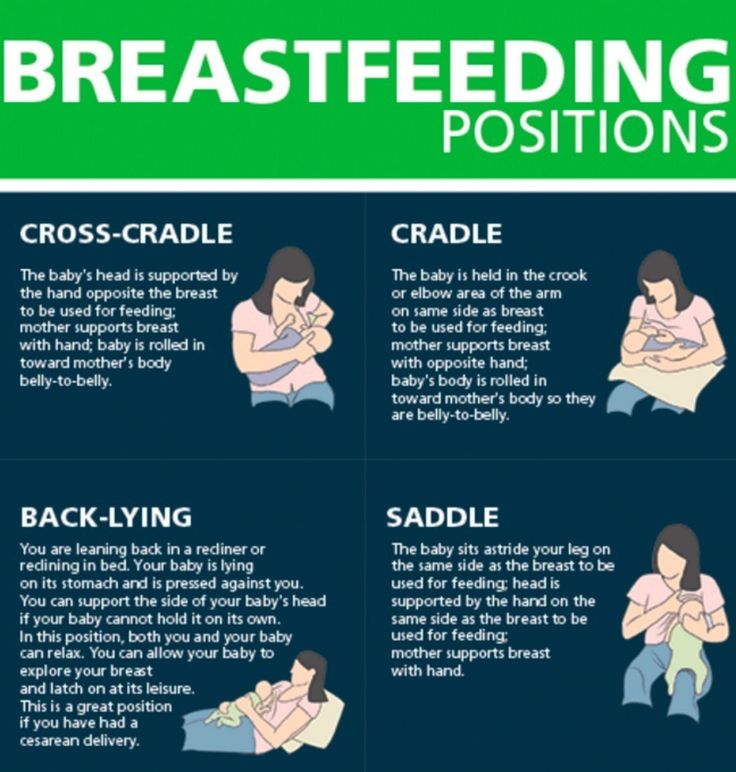 It will provide extra support and help keep both babies in the correct position, as well as reduce the burden on the abdomen if you had a caesarean section. In addition, the hands are freer, and if necessary, you can deal with one child without interfering with the second.
It will provide extra support and help keep both babies in the correct position, as well as reduce the burden on the abdomen if you had a caesarean section. In addition, the hands are freer, and if necessary, you can deal with one child without interfering with the second.
“My twins were born very tiny and had to be fed every two hours at any time of the day or night. Very soon it became clear: if I want to do anything besides feeding, I need to feed them both at the same time, - says Emma, mother of two children from the UK. “I breastfed them two by hand using a breastfeeding pillow.”
Other good positions for breastfeeding twins are two criss-cross cradles, one baby in the cradle and the other close at hand, reclining feeding, or sitting upright (one baby on one side, the other on the other).
11. Breastfeeding in the “arm-supported” or “dancer's-hand” position
muscle tone (which is typical for premature babies, children suffering from various diseases or Down syndrome), try supporting his head and your chest at the same time. 4 Grab your chest with your palm underneath so that your thumb is on one side and all the other fingers are on the other. Move your hand slightly forward so that your thumb and forefinger form a "U" just in front of your chest. With the other three fingers, continue to support the chest. With your thumb and forefinger, hold the baby's head while feeding so that his chin rests on the part of the palm between them, your thumb gently holds the baby on one cheek, and your index finger on the other. So the baby gets excellent support, and you can control his position and see if he is holding his breast.
4 Grab your chest with your palm underneath so that your thumb is on one side and all the other fingers are on the other. Move your hand slightly forward so that your thumb and forefinger form a "U" just in front of your chest. With the other three fingers, continue to support the chest. With your thumb and forefinger, hold the baby's head while feeding so that his chin rests on the part of the palm between them, your thumb gently holds the baby on one cheek, and your index finger on the other. So the baby gets excellent support, and you can control his position and see if he is holding his breast.
Literature
1 Colson SD et al. Optimal positions for the release of primitive neonatal reflexes stimulating breastfeeding. Early Hum Dev . 2008;84(7):441-449. - Colson S.D. et al., "Optimal Positions for Provoking Primitive Innate Reflexes to Induce Breastfeeding." Early Hume Dev. 2008;84(7):441-449.
2 UNICEF UK BFHI [ Internet ].