Reflux baby night feeding
GERD in Infants: Tips for Better Sleeping
Spitting up, or reflux, is very common in younger infants and can result from:
- overfeeding
- weak abdominal muscles
- an immature or weak lower esophageal sphincter
- a slow digestive system
In some rare cases, reflux in older infants is due to food allergies. In older children, it can also be a result of lactose intolerance. This is when the body is unable to process lactose, a sugar found in milk.
In people with acid reflux, acid from the stomach comes up into the esophagus. Reflux is common in infants and doesn’t usually cause symptoms other than spitting up.
Most babies grow out of it by the time they’re 12 months old and don’t require treatment other than simple home remedies.
Babies who have more severe symptoms may receive a diagnosis of gastroesophageal reflux disease (GERD). These symptoms may include:
- irritability
- poor weight gain
- vomiting consistently
Babies with these symptoms may need to take medication or even have surgery.
GERD can be painful for babies, causing irritability and discomfort. This can make it difficult for them to fall or stay asleep. If you’re having trouble getting your infant with GERD to sleep, here are some suggestions that may help.
Because acid reflux occurs after meals, don’t put your infant to bed immediately after a feeding.
Instead, burp them and wait 30 minutes before lying your baby down for a nap or for the evening. This will help make sure their body digested the meal.
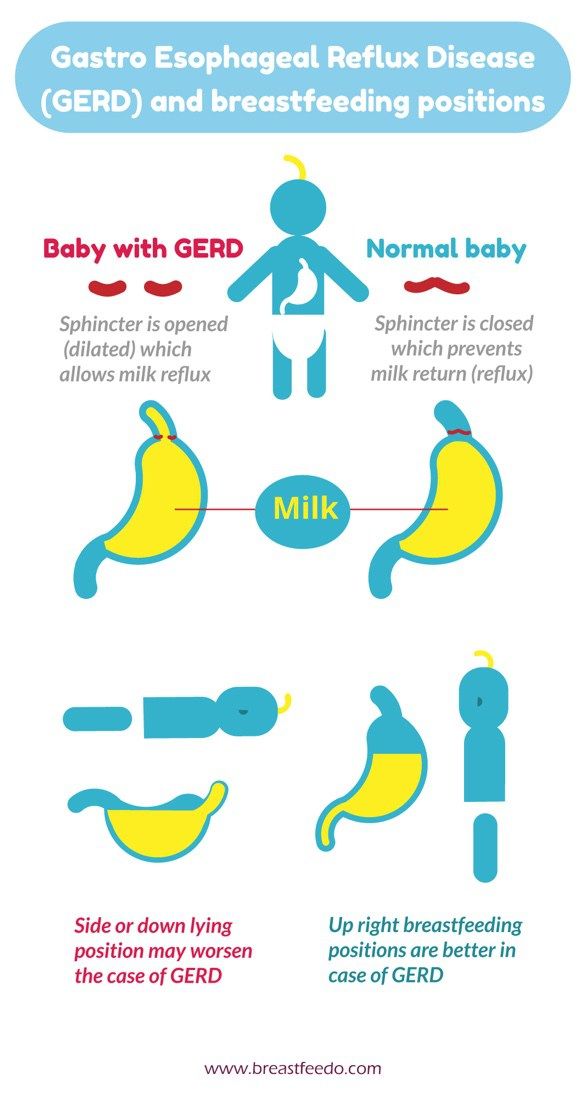
Similar to acid reflux in adults, acid reflux in infants can be made worse by their position, especially after eating.
Because very young infants can’t sit up by themselves, make sure your baby remains upright for 30 minutes after eating. This will help aid digestion before your child sleeps.
Many parents may have received the advice that raising the head of your baby’s crib can help relieve acid reflux symptoms.
However, the American Academy of Pediatrics (AAP) says that the practice has not been found to be effective, and it actually increases the likelihood that your child could shift into an unsafe position while sleeping.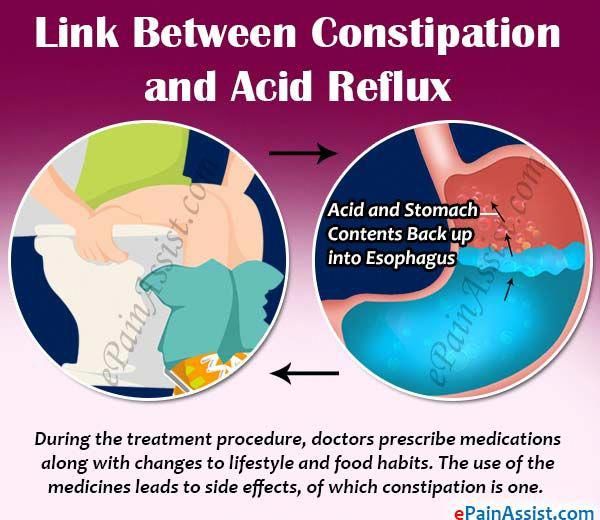
The AAP calls for infants to always sleep on their backs on a flat, firm surface. Only a fitted sheet should be used.
Blankets, pillows, and other soft objects like toys should be kept away from the area where your child sleeps. This reduces the risk of sudden infant death syndrome (SIDS).
The group also recommends sleeping in the same room as your child for the first 6 to 12 months after birth. However, your baby should sleep on a separate surface placed near but not on your bed. This can help prevent suffocation and strangulation.
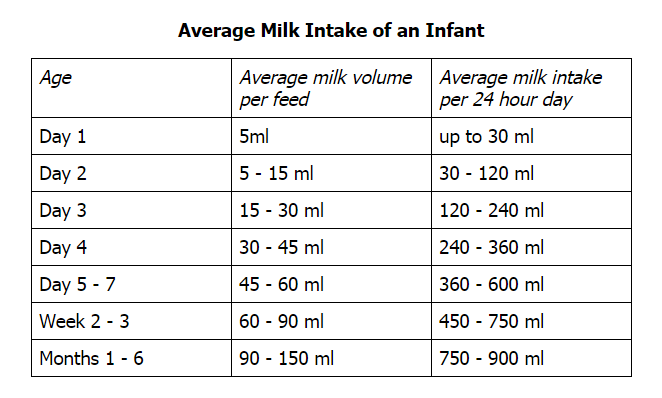
Sometimes acid reflux causes babies to throw up everything they’ve eaten. A baby who hasn’t had enough to eat will likely have trouble getting to sleep.
Talk with your child’s pediatrician if you think acid reflux is causing your baby to have difficulty sleeping. They can help you find a solution.
Your infant may need medication, a change in formula, or — in rare cases — surgery. Your pediatrician can also recommend ways to help your baby sleep.
If your baby has GERD and is taking medication, make sure you give them the medication exactly as prescribed by a pediatrician. Be aware of any side effects and when to call your doctor in an emergency.
Sleep is important, both for infants and for their parents and caregivers. Make sure to establish a consistent bedtime routine, then follow it nightly.
Rocking your infant in an upright position until they’re drowsy and almost asleep can help soothe them and may lessen symptoms of GERD or acid reflux.
Getting a baby to sleep can be tricky for anyone, but acid reflux may add yet another challenge. Talk with your child’s pediatrician about how acid reflux may be affecting your baby’s sleep and how you can help them sleep better.
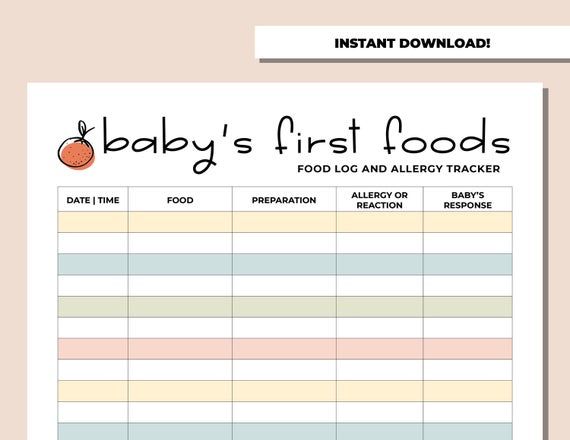
The doctor can suggest tips and tricks that will help your baby feel more comfortable. You should also take notes on any triggers you see affecting your baby’s condition and speak with your child’s pediatrician about them.
Reflux & Baby Sleep | Taking Cara Babies
When parents are trying to help their baby sleep, reflux can be a topic of concern.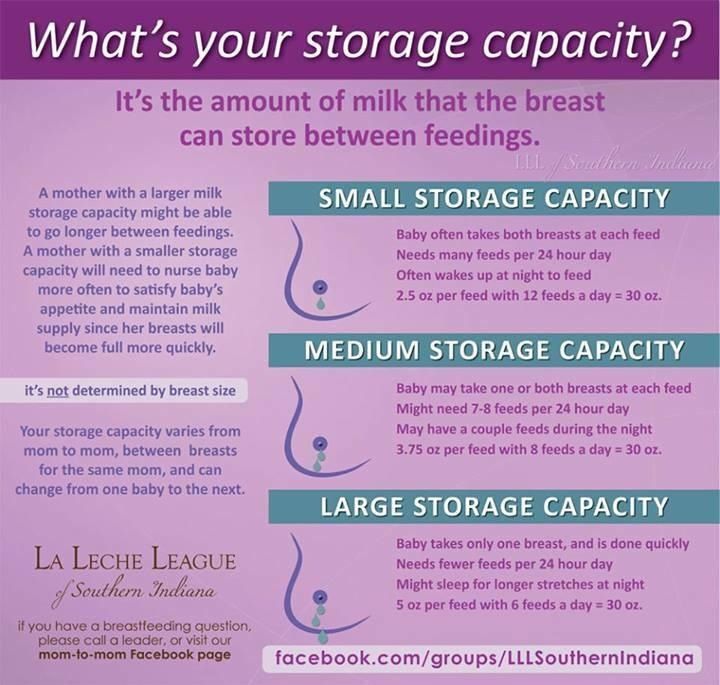
Why? Because when parents see their babies struggle with sleep, they often wonder if a physical issue like reflux could be causing rough nights.
Even though I have twenty years of experience as a nurse, please know that this blog in no way represents medical advice. My goal is to give you a brief understanding of reflux and some practical tips related to baby sleep because we do get so many questions regarding reflux. Please talk with your doctor about this and all medical concerns.
What is reflux?#
In short, reflux means that the stomach contents are being pushed into the esophagus. For most babies, this is not associated with pain; for some, there is pain involved.
If you’re concerned about how often or how much “spit-up” or refluxed milk you’re seeing, make sure to check out this video.
Here’s a bit deeper explanation:#
Our stomachs are full of the food we eat and digestive acids. A little muscle at the top of the stomach holds everything in place. However, if that muscle is weak or not working properly, the contents from the stomach are pushed up into the esophagus. For most babies, there is no reason for concern. These babies are sometimes referred to as “Happy Spitters.”
However, if that muscle is weak or not working properly, the contents from the stomach are pushed up into the esophagus. For most babies, there is no reason for concern. These babies are sometimes referred to as “Happy Spitters.”
However, for some babies the acid from the stomach can cause pain in the esophagus. These babies need to be seen by a doctor for the appropriate diagnosis and support.
Some things you might see if your baby is suffering from painful reflux:#
spitting up and vomiting associated with pain
difficulty being soothed/constant crying
becoming fussy following feedings
arching away from the nipple during feedings
frequent coughing or congestion in the absence of illness
wheezing or trouble breathing
irritability during feedings
refusal to eat
poor weight gain
difficult and disrupted sleep
I took my baby to see our doctor about reflux.
 Why does it feel like she isn’t concerned?#
Why does it feel like she isn’t concerned?#It’s estimated that over half of all babies spit up and show signs of reflux.
Remember, some reflux-type symptoms can be normal. Reflux is caused by an immature muscle that holds contents in the stomach. All babies are born with this immature muscle. Eventually, that muscle will get stronger and will only open when a baby swallows. It will remain tightly closed at other times, keeping everything in the stomach where it belongs.
In my opinion, many doctors see parents as overly eager for a reflux diagnosis, treatment, and medication if a baby is a bit cranky, spits up at all, or struggles with sleep in the slightest.
Not all babies who show reflux symptoms need treatment. However, if you feel like you see pain and your concerns are not being heard, please consider a second opinion; reach out to another doctor or a pediatric gastroenterologist to explore your concerns further.
When do doctors get concerned?#
Doctors get concerned when babies begin to suffer with severe pain, have trouble gaining weight, show blood in their stool, refuse to eat, or begin to experience respiratory issues. It’s so important for everyone to work together (parents and physicians) to determine if reflux pain is truly impacting the baby.
It’s so important for everyone to work together (parents and physicians) to determine if reflux pain is truly impacting the baby.
If your doctor determines that your baby is suffering from reflux pain (referred to as GERD), you may hear some of the recommendations below.
What are ways to help and why?#
1) Feed baby in an upright position. Keep the baby’s head higher than the stomach.
Why? Gravity can assist milk down the esophagus.
2) Hold baby upright for 20-30 minutes after each feeding.
Why? Gravity can help keep milk down in the stomach until it begins to digest.
3) Talk to your doctor about a good probiotic. (Example: Gerber Soothe).
Why? The study, published in JAMA Pediatrics, found that administering five drops of the probiotic lactobacillus reuteri results in much shorter crying episodes, less spitting up, and less constipation.
4) Burp after every 2-3 ounces or when you switch breasts.
Why? Burping decreases the chance for an air bubble to cause spitting up.
5) Offer a pacifier.
Why? Sucking can ease the pain by increasing saliva and downward contractions of the esophagus.
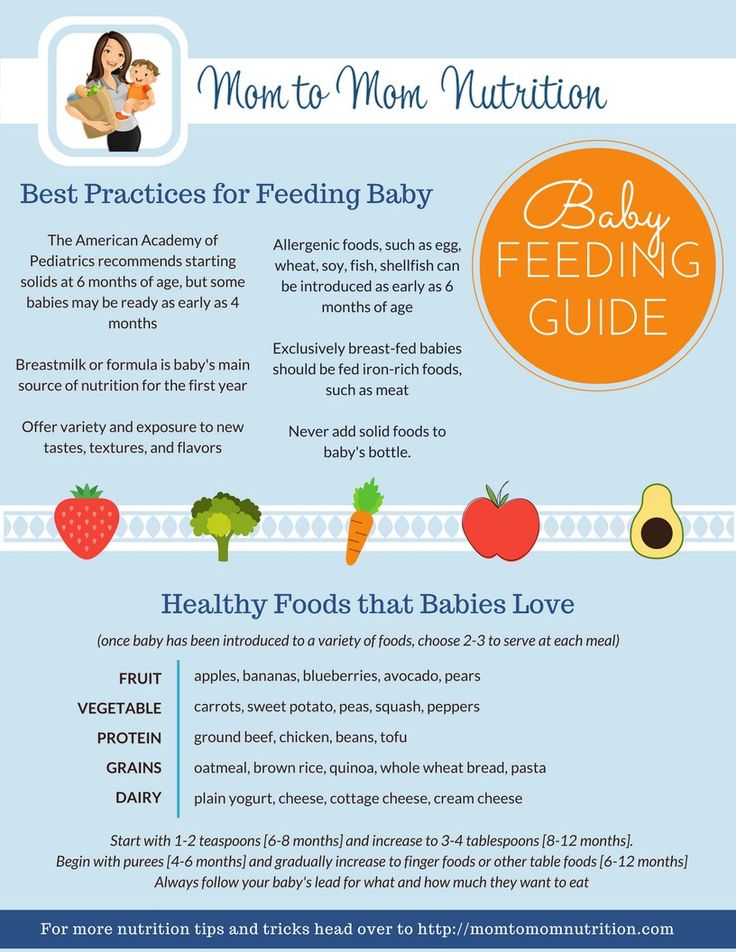
Should I start an elimination diet if nursing or change baby’s formula?#
This can help, but please discuss any dietary changes for you or your baby with your doctor/pediatrician first.
Cow’s milk can increase painful reflux symptoms for many babies dealing with GERD. (Check labels for casein, the milk protein.) Soy can also be a huge culprit. Again, each baby can have unique sensitivities, so please work closely with your doctor before making any big dietary changes.
What about medication?#
Not all babies with reflux need medication, but some may. If your baby does need treatment, you will need to work closely with your pediatrician/pediatric GI specialist to find the correct medication and dosage for your baby. If you are not seeing improvement, please keep in constant communication with the doctor. Finding the correct medication and dosage for your baby may take time.
If you are not seeing improvement, please keep in constant communication with the doctor. Finding the correct medication and dosage for your baby may take time.
Remember: As your baby grows, the dosage may need to be adjusted.
Should my baby sleep with his head elevated?#
Although many parents truly believe that elevating the head of the crib or using a Rock N Play helps with reflux, the American Academy of Pediatrics does not recommend it. In this article, the AAP reports that “elevating the head of the infant’s crib is not effective in reducing reflux. It may result in the infant sliding to the foot of the crib into a position that may compromise respiration and therefore is not recommended.”
If you are currently using a Rock 'n Play (which was recalled in April of 2019), I have tips to help you wean out.
Should my baby sleep on his back? What if he spits up? Won’t he choke?#
All babies should sleep on their back even babies with reflux.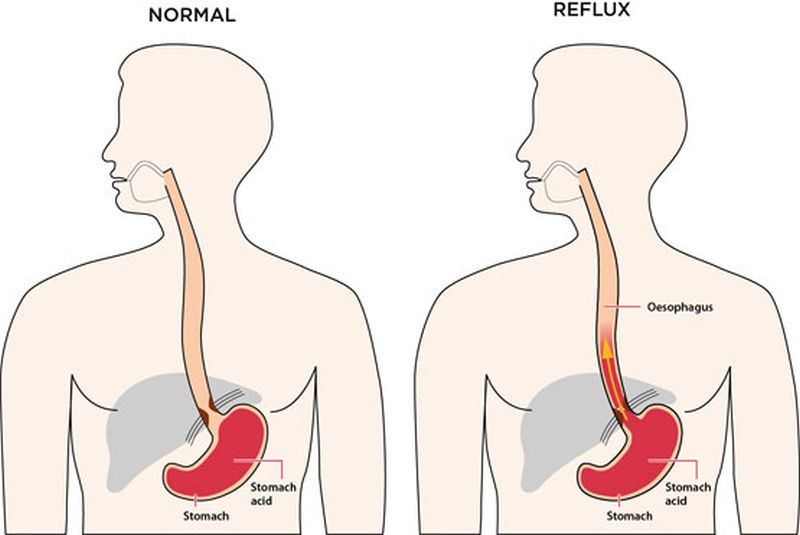 * This position does NOT increase the risk of choking. It is, indeed, safe.
* This position does NOT increase the risk of choking. It is, indeed, safe.
The AAP says this: “Sleep position does not increase the risk of choking and aspiration in infants, even those with gastroesophageal reflux, because infants have airway anatomy and mechanisms that protect against aspiration.”
This video will help you understand why it IS safe for a baby (even one with reflux) to sleep on his or her back:
Photo by the National Institute of Child Health and Human Development
Notice that if the baby spits up while on her back, it drains into the esophagus which goes to the stomach instead of the lungs. As the picture demonstrates, the safer position is for a baby to lay on his back while sleeping- even with reflux.
*Once a baby can independently roll from back to belly, they have the muscle strength and neck control to lift their head and safely sleep on their tummy. (Be sure arms are out of the swaddle. )
)
When I hold my baby upright after feedings, he falls asleep. How can he learn to fall asleep independently?#
We know that a baby falling asleep independently is so helpful in learning to sleep through the night.
Here are some tips to keep a baby awake while being held upright after daytime feedings:
Turn your baby away from you and walk around the house, look in the mirror, or show him toys.
Babywear with baby in an upright position (turned outward when age appropriate).
Use an exersaucer or baby jumper (when age appropriate).
Prop your baby up on your legs with your knees elevated and talk to her.
At bedtime, offer a feeding before bath time. Many bathtubs naturally hold baby in an upright position, so it serves as a great activity to break up feeding and sleep while still maintaining the position necessary to decrease reflux concerns.
For night feedings, your little one will, most likely, fall asleep while being held upright. This is okay and to be expected.
This is okay and to be expected.
*Please Note: Certain positions, such as in a swing or car seat, can cause pressure on the stomach and make reflux symptoms worse. Try to avoid car seats and swings for 20-30 minutes after a feeding.
Will your sleep classes and resources work for a baby with reflux?#
The Taking Cara Babies newborn class (for babies birth - 12 weeks) can help a baby with reflux. Even though this class can NOT take away the pain of reflux, it can hand parents tools to make progress on sleep skills and differentiate between overtiredness and true discomfort.
The newborn class may not turn a reflux baby into a perfect little sleeper, but it can still give parents the ability to read sleepy cues, soothe their fussy little one, and begin to lay a healthy sleep foundation.
For those facing the Four Month Sleep Regression, our e-book Navigating Months 3 + 4 can guide parents through this tricky developmental stage; however, babies in pain will continue to struggle with sleep.
For those who struggle to fall asleep independently, wake multiple times a night, eat often throughout the night, or suffer from inadequate naps, Taking Cara Babies has an online class for babies 5–24 months called The ABC’s of Sleep.This 14-night program has a 98% success rate in helping babies achieve 10-12 hours of consolidated night sleep AFTER reflux pain is well controlled. (Please note, the 2% that do not see success typically have some sort of medical concern including, but not limited to, untreated, painful reflux.) It is very important to treat the pain of reflux and ensure adequate caloric intake before beginning any sleep training program.
A Final Thought About Reflux:#
Having a baby with reflux is challenging. As parents, we do whatever it takes to make our babies comfortable, and we SHOULD. Sometimes this leaves us with sleep associations and habits that are hard to break. If you are in this boat, please know you haven’t done anything “wrong. ” You are comforting your baby and meeting his/her physical needs. This is exactly the RIGHT thing to do. Here’s what we know: when babies are in pain, sleep is so difficult.
” You are comforting your baby and meeting his/her physical needs. This is exactly the RIGHT thing to do. Here’s what we know: when babies are in pain, sleep is so difficult.
Please understand, once the pain is treated, Taking Cara Babies is here to help you conquer your rough nights and naps. Until then, work closely with your doctor and remember...you can do this, Mama.
GASTROESOPHAGEAL REFLUX: FROM NORM TO PATHOLOGY
If your child often suffers from acute respiratory diseases, it may be time for you, do not be surprised, to contact a gastroenterologist. Today we will talk about gastroesophageal reflux (GER) with Ph.D., head of the pediatric department of the Consultative and Diagnostic Center of the Children's Hospital No. G.N. Speransky Elena Vladislavovna Vigurzhinskaya, who will tell you why it is impossible to give yogurt to a child at night, which children with GERD also need the treatment of a neurologist.
Gastroesophageal reflux, or GER, is the backflow of contents from the stomach into the esophagus. Curious fact: Symptoms of reflux in children under 7 years of age are associated with structural features of the upper gastrointestinal tract and the immaturity of the sphincter apparatus of the digestive system. Please note: Reflux in children under one year old is a regurgitation syndrome. Spitting up to a tablespoon after each feeding is a variant of the norm. If the baby spits up in a larger volume, sometimes not immediately after feeding, and at the same time begins to gain weight poorly, then in this case a correction is already required - there are therapeutic, anti-reflux mixtures for this (if the child is artificially fed). Important: During the first months of a breastfed child's life, the mother must follow a strict hypoallergenic diet with a restriction of dairy, sweet foods and foods that increase gas formation: legumes, yeast bread, pastry, grapes, mushrooms, etc. With increased gas formation, reflux in babies it intensifies and frequent regurgitation occurs.
Curious fact: Symptoms of reflux in children under 7 years of age are associated with structural features of the upper gastrointestinal tract and the immaturity of the sphincter apparatus of the digestive system. Please note: Reflux in children under one year old is a regurgitation syndrome. Spitting up to a tablespoon after each feeding is a variant of the norm. If the baby spits up in a larger volume, sometimes not immediately after feeding, and at the same time begins to gain weight poorly, then in this case a correction is already required - there are therapeutic, anti-reflux mixtures for this (if the child is artificially fed). Important: During the first months of a breastfed child's life, the mother must follow a strict hypoallergenic diet with a restriction of dairy, sweet foods and foods that increase gas formation: legumes, yeast bread, pastry, grapes, mushrooms, etc. With increased gas formation, reflux in babies it intensifies and frequent regurgitation occurs.
- In some children, over time, reflux becomes pathological and triggers a cascade of many other problems, including the child suffering from frequent, viral infections, ENT diseases - explains Elena Vladislavovna Vigurzhinskaya . - This happens because when gastric contents (gastric secretion or food bolus) are thrown into the esophagus and, possibly, into the oropharynx, the pH changes, the flora of the oral cavity is disturbed and local immunity decreases, and the child falls into the so-called group "often ill children". In older children, GER clinically manifests itself in the form of heartburn, belching (air and food) Parents may also experience bad breath
Important: Plaque on the teeth, geographical tongue, bad breath, frequent ENT pathologies, croup and obstructive bronchitis are a serious reason to seek advice from a gastroenterologist!
Interesting fact: In impulsive and emotional children, GER may be more pronounced. In this case, the child will fall into the hands of not only a gastroenterologist, but also a neurologist.
Factors contributing to the development of GER : anatomical features of the structure of the upper gastrointestinal tract in young children, morpho-functional immaturity of the sphincter apparatus, hereditary predisposition, stressful situations, great physical and psychological stress, violation of the daily routine, malnutrition.
– If you undergo treatment, adjust your diet and adjust your daily routine, then you can get rid of GER, says the head of the pediatric department. - Do not give your child sour foods at night. Previously, kefir was advised to children at bedtime, but this dairy product acidifies the stomach and acts aggressively. With reflux, we do not recommend acidic foods (and especially before bedtime) - yogurt, kefir, as well as juices, sour berries and fruits. You can drink fermented baked milk or eat neutral yogurt in the afternoon. But in general, I recommend limiting acidic foods, including dairy products.
How is GER diagnosed? The specialist decides on an individual basis which test to order.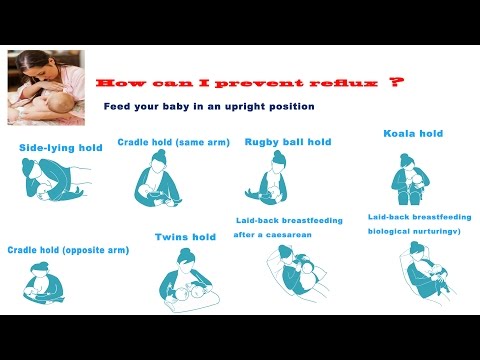 First of all, taking an anamnesis: the doctor asks the parents about the child's complaints. Then, an ultrasound examination of the abdominal cavity is prescribed (strictly on an empty stomach, do not brush your teeth) with a water-siphon test. Fibrogastroduodenoscopy and a chest x-ray with barium may be prescribed.
First of all, taking an anamnesis: the doctor asks the parents about the child's complaints. Then, an ultrasound examination of the abdominal cavity is prescribed (strictly on an empty stomach, do not brush your teeth) with a water-siphon test. Fibrogastroduodenoscopy and a chest x-ray with barium may be prescribed.
Treatment of GER: Gastroenterologists prescribe prokinetics, antacids, proton pump inhibitors (drugs that reduce the production of hydrochloric acid by stomach cells)
. Important: Gastroesophageal reflux can be a symptom of Helicobacter pylori infection. Therefore, first of all, it is necessary to identify and remove the bacterium. Another possible cause of reflux is a gastrointestinal form of food allergy. Keeping a food diary will help parents understand what kind of “inedible” product the child’s stomach is trying to get rid of.
What happens if GER is not treated? It is possible to develop a chronic condition that can lead to inflammation, erosions and even ulcers in the esophagus, the replacement of normal cells in the esophagus by pathological ones.
- I repeat that a diet and a healthy daily routine must be maintained for life, - says the gastroenterologist. - The child needs fractional nutrition. You can not overeat, eat dry food, drink food best with water, weak tea, compote (pear, apple). It is also not recommended to go to bed on a full stomach. Chocolate and buns, alas, are banned.
Lifestyle advice for gastroesophageal reflux
September 6, 2021
Repina Nadezhda Arkadievna
Gastroenterology
Have you been diagnosed with GERD (gastroesophageal reflux)?
Gastroesophageal reflux is manifested by a number of unpleasant symptoms that significantly reduce the quality of life. Heartburn, burning and pain behind the sternum, difficulty in swallowing food... However, timely diagnosis, treatment and lifestyle changes can neutralize these manifestations.
So, here are some recommendations for lifestyle modification in gastroesophageal reflux:
- It is recommended to sleep on a bed with a raised head end of 10-15 cm, which is achieved with supports or the use of a "wedge" pillow (only if reflux symptoms occur at night).
- Gradual moderate decrease in excess body weight. It has been proven that excess weight contributes to an increase in intra-abdominal pressure and the reflux of gastric contents into the esophagus (reflux).
- Avoid overeating. It is recommended to observe three to four meals a day (breakfast, lunch and dinner +/- 1 snack during the day) with small portions.
- You should not snack at night looking. The last meal should be no later than 2 hours before bedtime.
- Foods consumed must be neither too hot nor too cold. To determine the temperature of drinks, use the “bowl” rule: if you can hold the cup by the walls, and not by the handle, when drinking, then everything is fine - the temperature of the drink is not high.
- Do not wear corsets, bandages or tight belts that increase intra-abdominal pressure.
- After eating, avoid work that requires a long stay in a bent position (“gardener” position), lifting weights of more than 8-10 kg on both hands, as well as physical exercises associated with overstrain of the abdominal muscles.
- It is recommended to refuse to take a horizontal position within 1-1.5 hours after eating.
- Stop smoking and drinking alcohol. Smoking and alcoholic beverages relax the smooth muscles of the esophagus, increase the time the acid is exposed to the esophageal mucosa, and decrease the pressure of the lower esophageal sphincter (the valve between the esophagus and stomach).
Dietary advice for gastroesophageal reflux
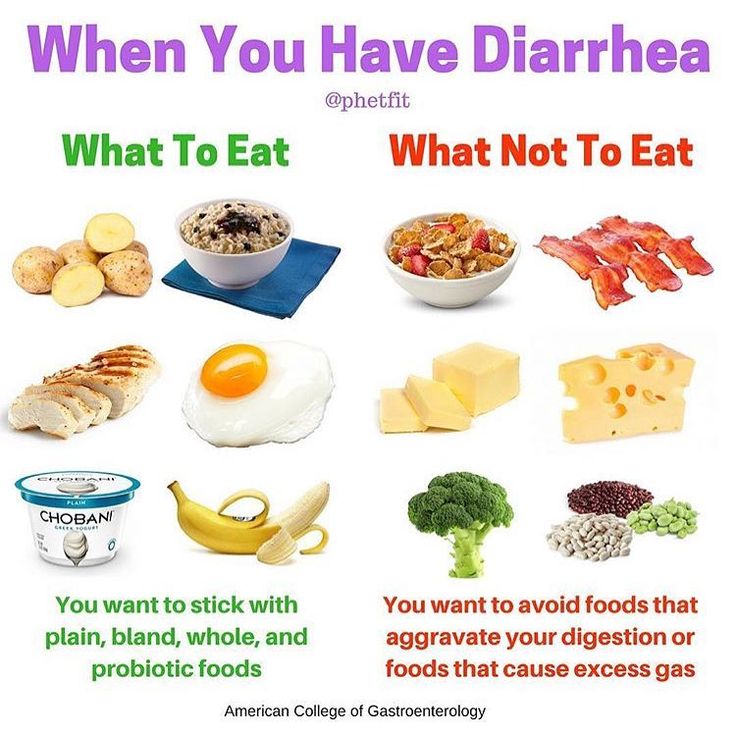
Certain types of foods can exacerbate the symptoms of gastroesophageal reflux. To identify foods that aggravate symptoms (heartburn, belching), it is you who need to keep a food diary.
Most common triggers to avoid:
- Coffee and other caffeinated drinks (black tea, hot chocolate) - help to relax the lower esophageal sphincter.
- Citrus fruits (oranges, limes, lemons, grapefruits, tangerines, pomelo), as well as juices from them - contain a large amount of acids.

- Tomatoes and tomato-containing sauces, dishes (eg lecho) have a high level of acidity.
- Carbonated drinks (cola, kvass, lemonade, energy drinks, carbonated mineral water, etc.) create increased pressure in the stomach cavity, due to which reflux symptoms increase.
- Chocolate, due to the content of a caffeine-like substance - methylxanthine, helps to relax the lower esophageal sphincter.
- Peppermint, onion and garlic help relax the lower esophageal sphincter.
- When chewing gum, a large amount of air is swallowed, and the presence of sweeteners in its composition provokes belching and bloating.
- Slowdown of evacuation from the stomach is provoked by an abundance of fatty foods, which include 20% cream, butter, margarine, cakes with cream filling, fatty fish - herring, mackerel, trout; fatty meat: pork, beef
- Spicy (mustard, pickles, pickles, vinegar) and fried foods have a direct damaging effect on the mucosa of the esophagus.

Follow these rules and the unpleasant manifestations of the disease will recede. And if the correction of lifestyle and nutrition does not bring relief, this is a reason to turn to a gastroenterologist.
The leaflet was prepared by gastroenterologist Repina Nadezhda Arkadyevna.
This website uses cookies in order to proper provision of services, as well as to collect statistics and commercial purposes. Additional information in our Privacy Policy.
Good
ATTENTION!
You have confirmed the reception. We are waiting for you at the clinic.
This technique requires preparation.
Familiarize
Close
You have accepted. We are waiting for you at the clinic.
Good
ATTENTION!
Documents are automatically processed on the owner of this account.