What to do if baby vomits after feeding
Children and vomiting - Better Health Channel
Summary
Read the full fact sheet- Mild vomiting is normal in most babies and improves over time.
- Most babies need only simple treatment, or none at all.
- Changing feeding and sleeping positions may help.
- Medicine should not be given unless prescribed by your doctor.
- Give a child who is unsettled after vomiting a drink or a little food.
- If your child seems unwell or shows any worrying symptoms, see a doctor.
Vomiting can be part of many illnesses in children and babies. It is not usually a major concern as long as your child seems well in other ways.
Vomiting is common for babies and young children. Vomiting occurs when food is brought back up from the stomach. The amount of vomit can often seem larger than it actually is.
Types of vomiting
There are different types of vomiting, including:
- Possetting – this is when your baby vomits up small amounts after a feed.
- Reflux – this vomiting is common in babies. It is caused when the valve at the top of the stomach accidentally opens. The contents of the stomach come back up the food pipe (oesophagus) slowly. Reflux does not harm babies. They usually grow out of it by the time they are walking.
- Projectile vomiting – this is when your baby brings up the stomach contents in a forceful way. The amount of milk or food can seem large on the floor, but is usually only the amount of the last feed. Babies may projectile vomit occasionally, but if it happens after every feed, see your doctor right away as it may be due to a blockage caused by thickening of the muscle at the outlet of the stomach.
Causes of vomiting
Vomiting is usually caused by:
- minor infections like 'gastro' or the common cold
- gastro-oesophageal reflux
- motion sickness from travelling in a moving vehicle.

Sometimes, vomiting may be part of a more serious illness. Children may vomit if they have an infection, such as a urinary tract infection or meningitis, a bowel obstruction or appendicitis. If vomiting progresses to fever and diarrhoea, it will usually be caused by a virus infection. If this persists for 12 hours or more, dehydration is likely. so see your doctor or local hospital emergency department without delay.
Treatment for vomiting
Most babies and children vomit easily and recover quickly. After vomiting, your child may be hungry and thirsty. Give plenty to drink so your child does not become dehydrated. If your child keeps on vomiting and looks unwell, see your doctor. Do not use medication to try and stop the vomiting.
Reflux vomiting can be prevented or reduced
Different positions for feeding or in bed can help reduce your baby’s chance of vomiting. You can try to:
- Feed your baby in an upright position.
- Prop your baby up after feeds.
- Lay your baby on the left side.
- Avoid bouncing your baby after feeding.
To help with mild reflux, you can thicken your baby’s food with cornflour or infant food thickener. If your child is uncomfortable after vomiting or will not settle, try giving milk or water. This will wash any acid back into the stomach. Some babies get heartburn, which is a burning sensation in the chest. They may be unsettled after feeding or when lying flat. Your doctor can suggest an antacid to relieve heartburn.
When to see your doctor
Take your baby to the doctor if any of these symptoms occur:
- poor weight gain because of the loss of feeds in vomiting
- coughing or choking spells
- blood or yellow-green bile in the vomit
- heartburn
- vomiting increases or becomes forceful after every feed
- your baby seems unwell.
Where to get help
- Your doctor
- NURSE-ON-CALL Tel. 1300 60 60 24 – for expert health information and advice (24 hours, 7 days)
- Your local maternal and child health nurse
- The 24 hour Maternal and Child Health Telephone Service.
 Tel.13 22 29
Tel.13 22 29 - Your local hospital emergency or casualty department
Things to remember
- Mild vomiting is normal in most babies and improves over time.
- Most babies need only simple treatment, or none at all.
- Changing feeding and sleeping positions may help.
- Medicine should not be given unless prescribed by your doctor.
- Give a child who is unsettled after vomiting a drink or a little food.
- If your child seems unwell or shows any worrying symptoms, see a doctor.
This page has been produced in consultation with and approved by:
Vomiting (0-12 Months)
Is this your child's symptom?
- Vomiting (throwing up) stomach contents
- Other names for vomiting are puking, barfing and heaving
Causes of Vomiting
- Viral Gastritis. Stomach infection from a stomach virus is the most common cause. Also called stomach flu. A common cause is the Rotavirus.
 The illness starts with vomiting. Watery loose stools may follow within 12-24 hours.
The illness starts with vomiting. Watery loose stools may follow within 12-24 hours. - Food Allergy. Vomiting can be the only symptom of a food reaction. The vomiting comes on quickly after eating the food. Uncommon in infants, but main foods are eggs and peanut butter.
- Coughing. Hard coughing can also cause your child to throw up. This is more common in children with reflux.
- Serious Causes. Vomiting alone should stop within about 24 hours. If it lasts over 24 hours, you must think about more serious causes. An example is a kidney infection. A serious cause in young babies is pyloric stenosis. See below for more on this.
Pyloric Stenosis (Serious Cause)
- The most common cause of true vomiting in young babies.
- Onset of vomiting is age 2 weeks to 2 months
- Vomiting is forceful. It becomes projectile and shoots out.
- Right after vomiting, the baby is hungry and wants to feed.
 ("hungry vomiter")
("hungry vomiter") - Cause: The pylorus is the channel between the stomach and the gut. In these babies, it becomes narrow and tight.
- Risk: Weight loss or dehydration
- Treatment: Cured by surgery.
Vomiting Scale
- Mild: 1 - 2 times/day
- Moderate: 3 - 7 times/day
- Severe: Vomits everything, nearly everything or 8 or more times/day
- Severity relates even more to how long the vomiting goes on for. At the start of the illness, it's common for a child to vomit everything. This can last for 3 or 4 hours. Children then often become stable and change to mild vomiting.
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much fluid.
- The younger the child, the greater the risk for dehydration.
Dehydration: How to Tell
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much water.

- Vomiting with watery diarrhea is the most common cause of dehydration.
- Dehydration is a reason to see a doctor right away.
- Your child may have dehydration if not drinking much fluid and:
- The urine is dark yellow and has not passed any in over 8 hours.
- Inside of the mouth and tongue are very dry.
- No tears if your child cries.
- Slow blood refill test: Longer than 2 seconds. First, press on the thumbnail and make it pale. Then let go. Count the seconds it takes for the nail to turn pink again. Ask your doctor to teach you how to do this test.
When to Call for Vomiting (0-12 Months)
Call 911 Now
- Can't wake up
- Not moving
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Dehydration suspected. No urine in over 8 hours, dark urine, very dry mouth and no tears.
- Stomach pain when not vomiting. Exception: stomach pain or crying just before vomiting is quite common.

- Age less than 12 weeks old with vomiting 2 or more times. Exception: normal spitting up.
- Vomited 3 or more times and also has diarrhea
- Severe vomiting (vomits everything) more than 8 hours while getting Pedialyte (or breastmilk)
- Head injury within the last 24 hours
- Weak immune system. Examples are sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- Vomiting a prescription medicine
- Fever over 104° F (40° C)
- Fever in baby less than 12 weeks old. Caution: Do NOT give your baby any fever medicine before being seen.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- All other infants (age less than 1 year) with vomiting. See Care Advice while waiting to discuss with doctor.
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.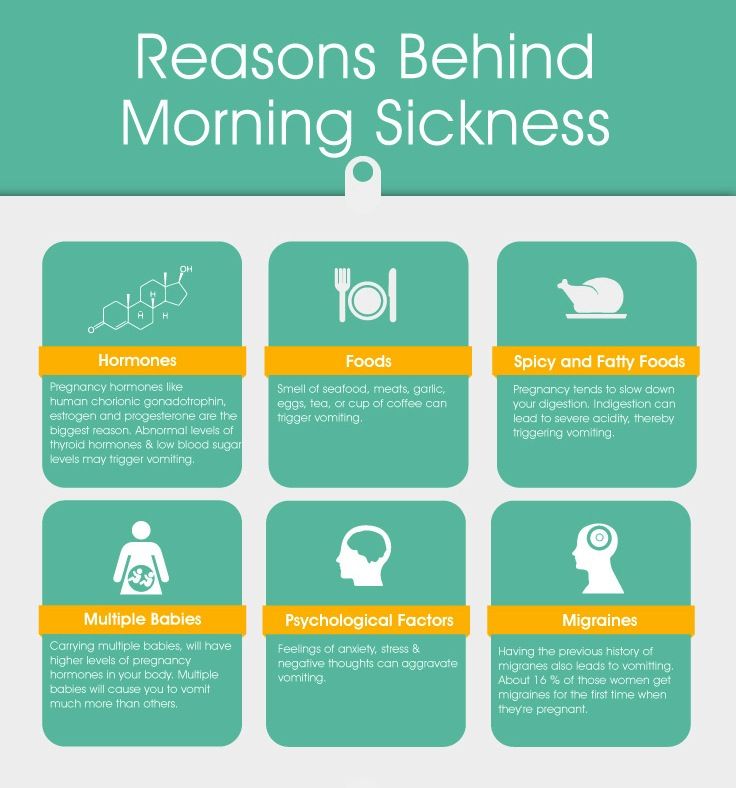
- Bellevue
- Everett
- Federal Way
- Seattle
- Virtual Urgent Care
Care Advice for Vomiting
- What You Should Know About Vomiting:
- Most vomiting is caused by a viral infection of the stomach.
- Vomiting is the body's way of protecting the lower gut.
- The good news is that stomach illnesses last only a short time.

- The main risk of vomiting is dehydration. Dehydration means the body has lost too much fluid.
- Here is some care advice that should help.
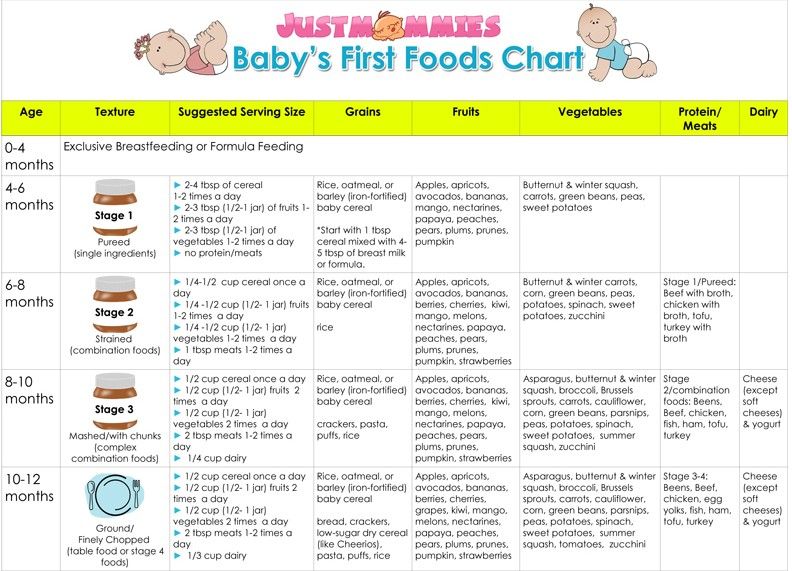
- Formula Fed Babies - May Give Oral Rehydration Solution (ORS) for 8 Hours:
- If vomits once, give half the regular amount of formula every 1 to 2 hours.
- If vomits formula more than once, offer ORS for 8 hours. If you don't have ORS, use formula until you can get some.
- ORS is a special fluid that can help your child stay hydrated. You can use Pedialyte or the store brand of ORS. It can be bought in food stores or drug stores.
- Spoon or syringe feed small amounts. Give 1-2 teaspoons (5-10 mL) every 5 minutes.
- After 4 hours without throwing up, double the amount.
- Return to Formula. After 8 hours without throwing up, go back to regular formula.
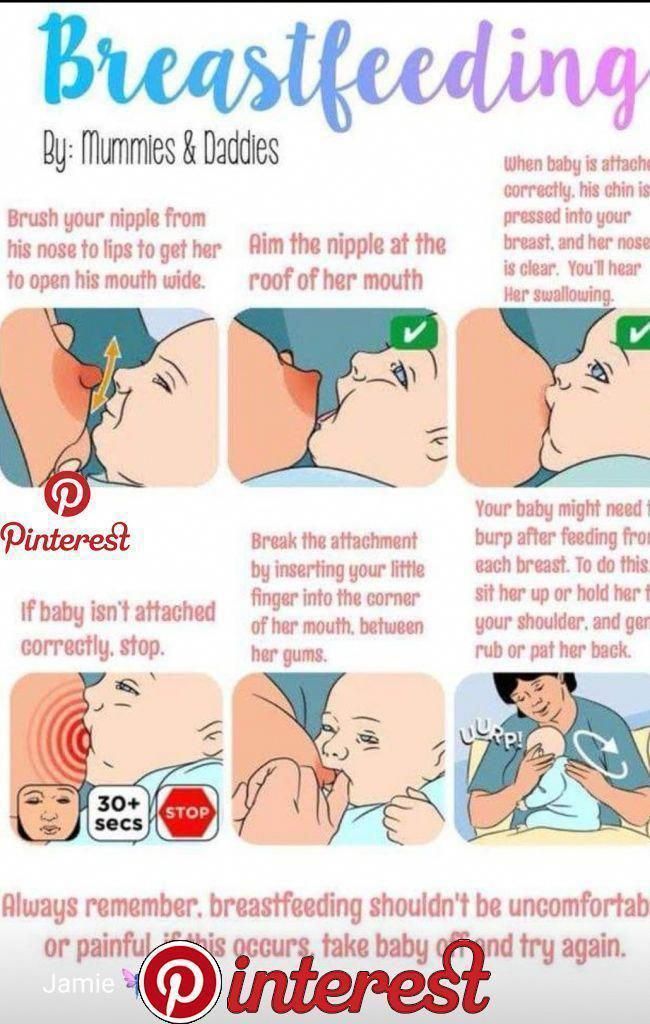
- Breastfed Babies - Reduce the Amount Per Feeding:
- If vomits once, nurse half the regular time every 1 to 2 hours.

- If vomits more than once, nurse for 5 minutes every 30 to 60 minutes. After 4 hours without throwing up, return to regular nursing.
- If continues to vomit, switch to pumped breastmilk. (ORS is rarely needed in breastfed babies. It can be used if vomiting becomes worse).
- Spoon or syringe feed small amounts of pumped milk. Give 1-2 teaspoons (5-10 mL) every 5 minutes.
- After 4 hours without throwing up, return to regular feeding at the breast. Start with small feedings of 5 minutes every 30 minutes. As your baby keeps down the smaller amounts, slowly give more.
- If vomits once, nurse half the regular time every 1 to 2 hours.
- Pumped Breastmilk Bottle-Fed Infants - Reduce the Amount per Feeding:
- If vomits once and bottle-feeding breastmilk, give half the regular amount every 1-2 hours.
- If vomits more than once within last 2 hours, give 1 ounce (30 mL) every 30 to 60 minutes.
- If continues to vomit, give 1-2 teaspoons (5-10 mL) every 5 minutes. Only if not tolerating breastmilk, switch to ORS (e.
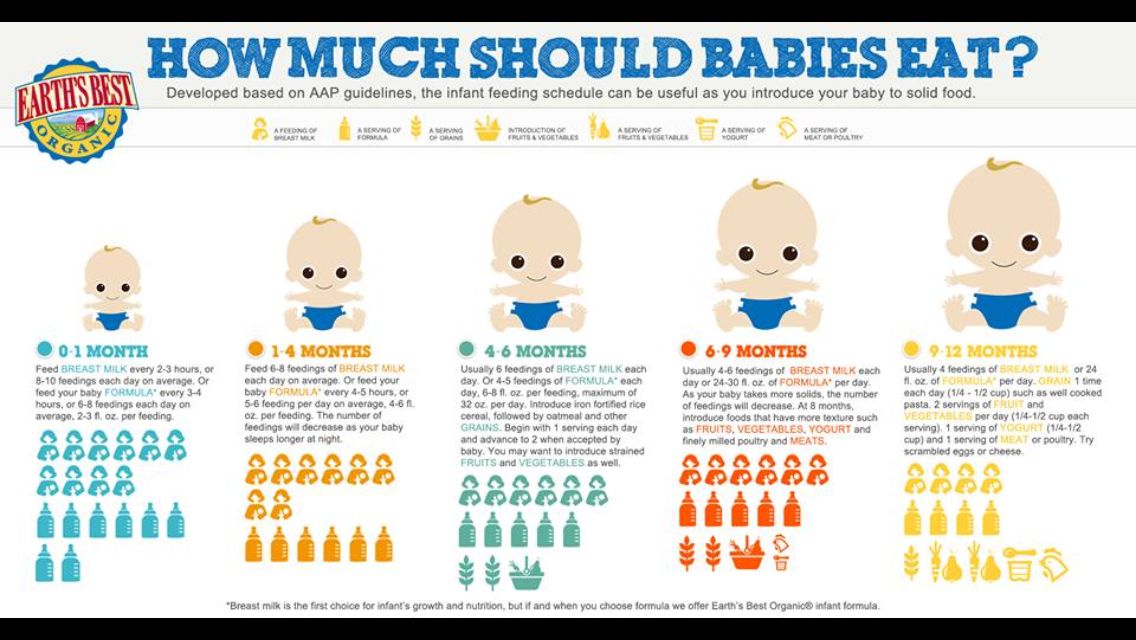 g., Pedialyte) for every 5 minutes for a few hours.
g., Pedialyte) for every 5 minutes for a few hours. - After 4 hours without vomiting, return to regular feedings. Start with 1 ounce (30 mL) every 30 minutes and slowly increase as tolerated.
- Stop All Solid Foods:
- Avoid all solid foods and baby foods in kids who are vomiting.
- After 8 hours without throwing up, gradually add them back.
- If on solid foods, start with starchy foods that are easy to digest. Examples are cereals, crackers and bread.
- Do Not Give Medicines:
- Stop using any drug that is over-the-counter for 8 hours. Reason: Some of these can make vomiting worse.
- Fever. Mild fevers don't need to be treated with any drugs. For higher fevers, you can use an acetaminophen suppository (such as FeverAll). This is a form of the drug you put in the rectum (bottom). Ask a pharmacist for help finding this product. Do not use ibuprofen. It can upset the stomach.

- Call your doctor if: Your child vomits a drug ordered by your doctor.
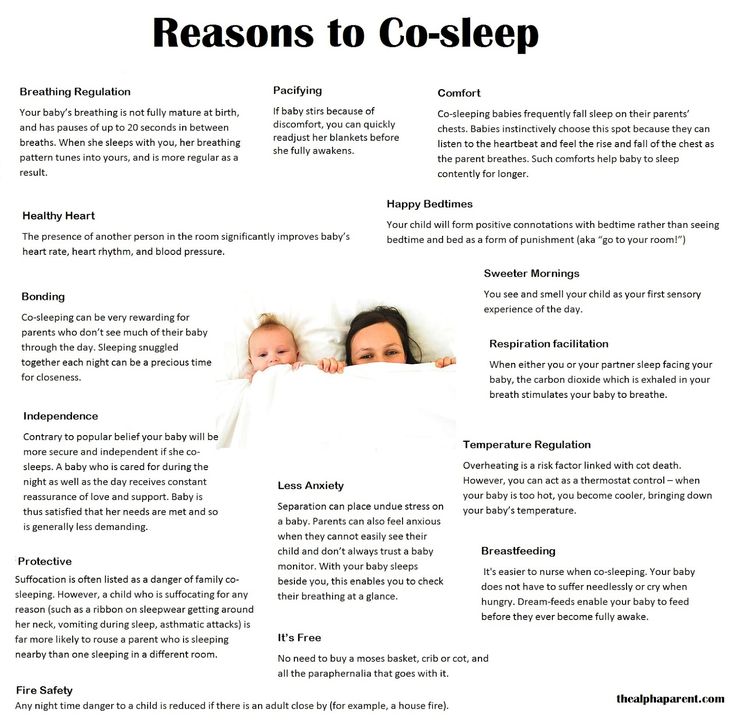
- Try to Sleep:
- Help your child go to sleep for a few hours.
- Reason: Sleep often empties the stomach and removes the need to vomit.
- Your child doesn't have to drink anything if his stomach feels upset and he doesn't have any diarrhea.
- Return to Child Care:
- Your child can return to child care after the vomiting and fever are gone.
- What to Expect:
- For the first 3 or 4 hours, your child may vomit everything. Then the stomach settles down.
- Vomiting from a viral illness often stops in 12 to 24 hours.
- Mild vomiting and nausea may last up to 3 days.
- Call Your Doctor If:
- Vomits clear fluids for more than 8 hours
- Vomiting lasts more than 24 hours
- Blood or bile (green color) in the vomit
- Stomach ache present when not vomiting
- Dehydration suspected (no urine in over 8 hours, dark urine, very dry mouth, and no tears)
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 04/21/2023
Last Revised: 12/30/2022
Copyright 2000-2023 Schmitt Pediatric Guidelines LLC.
Spitting up and vomiting in infants
Spitting up and vomiting in babies is a common reason for visiting a doctor.
Regurgitation and vomiting is a reflex action that occurs when receptors located in various anatomical zones are irritated, incl. in the stomach, esophagus, pharynx, oral cavity. The signal is transmitted to the vomiting center, which is located in the medulla oblongata and a gag reflex occurs.
What is the difference between regurgitation and vomiting?
The difference lies in the volume and kinetics (movement) of the gastric contents expelled to the outside. When regurgitation occurs, leakage occurs without the participation of the diaphragm and abdominal muscles, i. e. passively. There is little content, up to about 10-15 ml. If the child does not swallow it, it quietly expires from the oral cavity. When vomiting, a wave-like bending of the upper half of the body occurs as a result of contraction of the muscles of the diaphragm and the anterior wall of the abdomen, the volume of vomit is greater, and they are erupted with pressure from the oral cavity with an ejection trajectory of up to 50 cm. In children of the first year of life, this is defined by the term "fountain vomiting" .
e. passively. There is little content, up to about 10-15 ml. If the child does not swallow it, it quietly expires from the oral cavity. When vomiting, a wave-like bending of the upper half of the body occurs as a result of contraction of the muscles of the diaphragm and the anterior wall of the abdomen, the volume of vomit is greater, and they are erupted with pressure from the oral cavity with an ejection trajectory of up to 50 cm. In children of the first year of life, this is defined by the term "fountain vomiting" .
Regurgitation is observed only in children of the first year of life and, mainly, up to 6 months. Contribute to this anatomical and physiological features of the esophagus and stomach of the baby. Their esophagus is short and wide, the angle of connection of the esophagus with the stomach is less pronounced, and its obturator function is weak. These regurgitations are physiological. They can be after each feeding, up to 15 ml, do not affect the well-being and weight gain of the baby. They can also be caused by excessive feeding, aerophagia (swallowing air while sucking), straining during intestinal colic. The frequency and volume of such regurgitation decreases with the growth of the child. With the introduction of complementary foods, and this is a thicker food, regurgitation stops or becomes much less frequent.
They can also be caused by excessive feeding, aerophagia (swallowing air while sucking), straining during intestinal colic. The frequency and volume of such regurgitation decreases with the growth of the child. With the introduction of complementary foods, and this is a thicker food, regurgitation stops or becomes much less frequent.
If regurgitation persists in a child older than 1 year, then this is a sign of a pathological process.
Vomiting, unlike regurgitation, is accompanied by vegetative symptoms - increased salivation, pallor of the skin, palpitations. This is due to the fact that next to the vomiting center there are additional centers of autonomic regulation, which are reflexively excited, and active biological substances such as serotonin, dopamine, histamine and others are released into the blood.
Regurgitation and vomiting, from the moment of eating, may occur during feeding, after feeding for the first 20-30 minutes or delayed, sometimes after several hours.
Regurgitation and vomiting that occurs immediately after feeding unchanged breast milk or formula may be due to narrowing of the esophagus. If they persist until the next feeding, and the milk / mixture is curdled, has a sour or musty smell, then this is the result of a long standing food in the stomach. The reason for this may be the low tone of the muscle layer of the stomach and, as a result, its peristalsis or narrowing of the output section due to an anomaly in the development or high tone of the sphincter of the lower stomach. With narrowing of the duodenum, bile is present in the regurgitated masses.
Gastroesophageal reflux is a common cause of regurgitation in infants. It is likely that there is a complex problem here, starting with the immaturity of the gastrointestinal tract and disorders of the central nervous system. Perinatal injuries of the central nervous system accompany every second child. Their manifestations are varied. Regurgitation and vomiting can be facilitated by an increase in intracranial pressure, disorders in the segment of the cervical spine, and so on. Therefore, quite often, when carrying out rehabilitation measures for neurological dysfunctions, a positive effect is manifested in the form of a decrease or cessation of regurgitation. A hernia of the esophageal opening of the diaphragm will also manifest itself in a similar way.
Therefore, quite often, when carrying out rehabilitation measures for neurological dysfunctions, a positive effect is manifested in the form of a decrease or cessation of regurgitation. A hernia of the esophageal opening of the diaphragm will also manifest itself in a similar way.
We should not forget about allergic gastrointestinal reactions in the form of regurgitation and vomiting. The most common cause of this is cow's milk protein. With intolerance to cow's milk protein, inflammation of the mucous membrane of the esophagus, stomach and intestines occurs. And, as a result of this, regurgitation and vomiting, pain and increased gas formation, diarrhea or constipation.
Rare endocrine disorders (adrenogenital syndrome) are manifested by vomiting in children from the first weeks of life. In such cases, vomiting is frequent, there may be an admixture of bile, the child loses weight due to loss of fluid and nutrients, and severe metabolic disorders develop.
Vomiting can also be caused by an intestinal infection.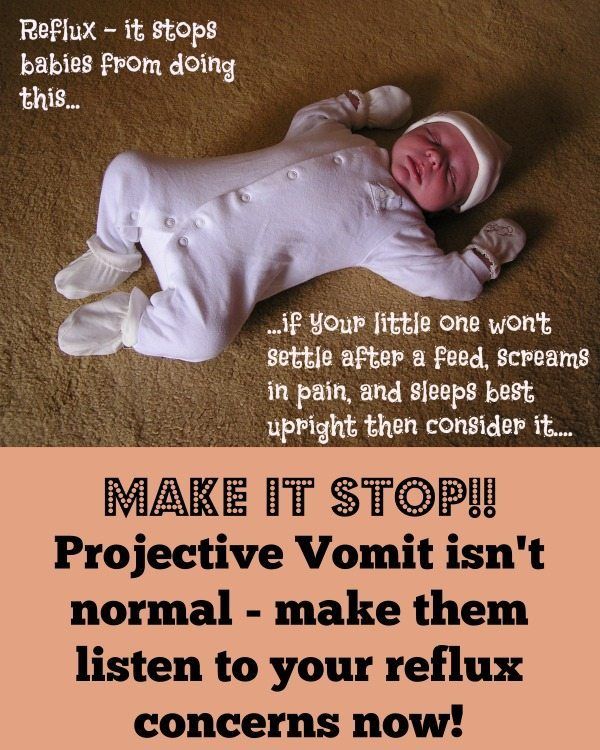 Viral gastroenteritis is now common. It must be remembered that the younger the child, the more severe the disease. Within a few hours, the child's condition can go from satisfactory to extremely serious.
Viral gastroenteritis is now common. It must be remembered that the younger the child, the more severe the disease. Within a few hours, the child's condition can go from satisfactory to extremely serious.
As you can see, the causes of regurgitation and vomiting in children of the first year of life are quite diverse, but most often these are transient conditions that disappear with the growth of the child.
Prevention of regurgitation in children of the first months of life is quite simple. Don't overfeed your baby. If he cries, it does not always mean that he is hungry. Excess feeding leads to increased gas formation and colic, during which the child is worried, straining, thereby increasing the likelihood of spitting up. After feeding, hold the baby more upright so that he can burp the swallowed air. This will take 15-20 minutes. If the child is bottle-fed, do not change his formula milk without the recommendation of a pediatrician.
If the child has frequent regurgitation and vomiting, it is necessary to consult a pediatrician or gastroenterologist to diagnose the cause. To make a diagnosis, it is sometimes enough to carry out simple and affordable diagnostic methods in a polyclinic. These include an ultrasound of the stomach and, if necessary, stool tests. However, the approach in each case is individual. Examination and treatment will be assigned to your baby, depending on the diagnosis. Perhaps it will be preventive measures or a certain milk formula, perhaps drug therapy. Rarely, but it happens that it is necessary to examine the child in a hospital and surgical treatment.
To make a diagnosis, it is sometimes enough to carry out simple and affordable diagnostic methods in a polyclinic. These include an ultrasound of the stomach and, if necessary, stool tests. However, the approach in each case is individual. Examination and treatment will be assigned to your baby, depending on the diagnosis. Perhaps it will be preventive measures or a certain milk formula, perhaps drug therapy. Rarely, but it happens that it is necessary to examine the child in a hospital and surgical treatment.
what to do - useful information for patients, Vitbiomed clinic blog +
Text: Irina Frolova
Vomiting in a child is a serious symptom that should not be ignored. Vomiting may be accompanied by or without additional symptoms, diarrhea, and/or high fever. In this article, we will talk about the possible causes of vomiting without fever and diarrhea and what parents need to do.
Causes of vomiting without fever and diarrhea
Viral gastroenteritis
This disease is also called intestinal or stomach flu. Usually its causative agent is a virus from the group of rotaviruses, less often - norovirus. The disease begins abruptly, with indomitable vomiting, accompanied by rumbling and pain in the abdomen. Diarrhea may also develop after 12 to 24 hours, but this is not necessary. Rotavirus infection often occurs with an increase in temperature to febrile values.
Usually its causative agent is a virus from the group of rotaviruses, less often - norovirus. The disease begins abruptly, with indomitable vomiting, accompanied by rumbling and pain in the abdomen. Diarrhea may also develop after 12 to 24 hours, but this is not necessary. Rotavirus infection often occurs with an increase in temperature to febrile values.
Food allergy
Sometimes the only reaction to a food intolerance is vomiting. In this case, vomiting occurs almost immediately after consumption of the product. The most common food allergies are nuts, fish, seafood, milk, eggs, and soy products.
Gastrointestinal disorders
Non-viral gastritis, pancreatitis, cholecystitis and biliary dyskinesia may cause vomiting. As a rule, in children they are caused by errors in nutrition, but there may be other reasons. To make a diagnosis and prescribe treatment, you need to visit a gastroenterologist.
Taking certain medications
Vomiting can be caused by not following the rules for taking certain medications, such as taking drugs on an empty stomach that irritate the stomach lining.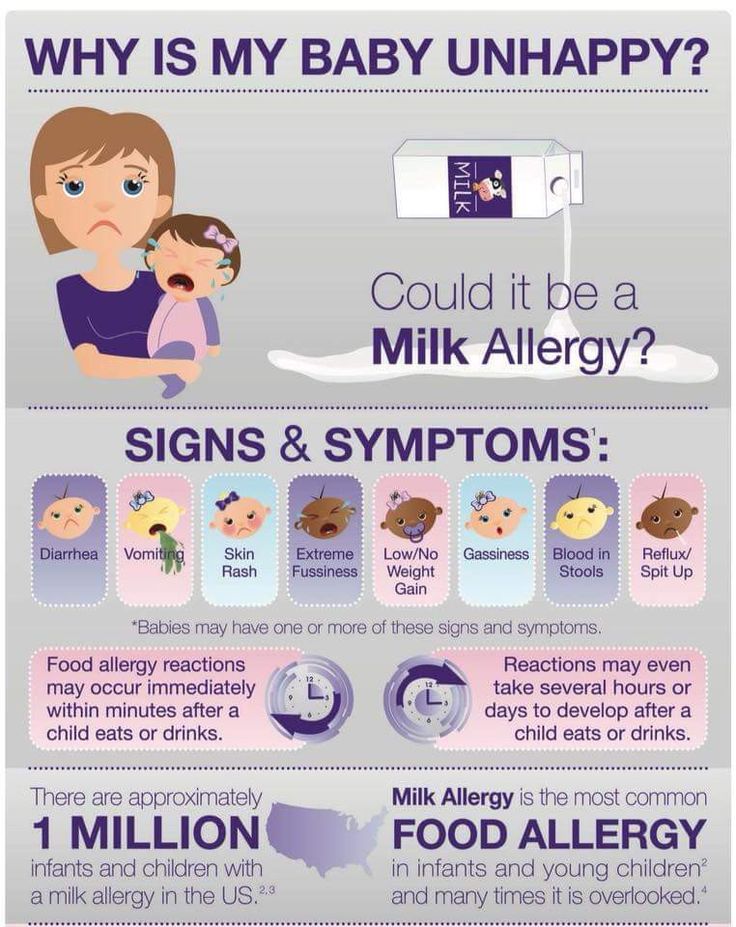 Such drugs, in particular, include paracetamol, ibuprofen, iron preparations, theophylline.
Such drugs, in particular, include paracetamol, ibuprofen, iron preparations, theophylline.
Motion sickness
Motion sickness often causes nausea and vomiting. In this case, the child may experience pain in the abdomen, he may sweat a lot, and then vomiting begins. You can get sick not only on a trip, but even when watching movies shot with camera shake and fast-paced frames.
Cough
A severe cough can sometimes lead to vomiting, especially in children with reflux.
Migraine
About 10% of children suffer from migraine - cases of migraine have been reported in children of two years of age. A migraine attack is often accompanied by vomiting.
Stress
Vomiting can occur during a stressful situation in both children and adults.
Concussion
This is a dangerous condition that occurs after a fall and/or a blow to the head. Vomiting is often its main symptom, but headaches, visual disturbances, speech and gait disturbances may also occur. If you suspect a concussion, you should immediately call a doctor.
If you suspect a concussion, you should immediately call a doctor.
Appendicitis
Usually accompanied by severe abdominal pain and requires an ambulance.
Foreign body in the gastrointestinal tract
Sometimes children swallow various objects - buttons, batteries, and so on. This can lead to serious consequences, including intestinal obstruction, a sign of which is also vomiting.
How to determine the severity of vomiting
- Mild - 1-2 times a day
- Medium - 3-7 times a day
- Severe - more than 8 times a day or after any meal, water
How dangerous vomiting is
It causes dehydration, and the more severe the vomiting, the more severe the dehydration. With severe dehydration, the functions of various body systems are disrupted; in severe cases, death can occur without infusion therapy. Children become dehydrated very quickly, and at the first suspicion of dehydration, it is necessary to call a doctor.
How to tell if you are dehydrated
- The child has dark urine and has not urinated for 8 hours
- Child has dry mouth
- The child cries without tears
If these signs appear, an ambulance should be called. Dehydration is dangerous to the life of a child, especially a younger one.
What to do for parents
As a first aid, help the child to clear the mouth of the remnants of vomit (toddlers clean the mouth of the parents, older children can rinse their mouths themselves), put to bed so that the head is higher than the body, offer water, but do not feed for at least two hours after vomiting.
If vomiting is mild but recurs occasionally, visit a pediatrician and determine the cause. Treatment will depend on the cause.
In case of vomiting that lasts more than a day, you should consult a local pediatrician or call an ambulance.
In case of severe vomiting, if the child cannot be hydrated or if the child's condition worsens, an ambulance should be called.