When to bottle feed breastfed baby
Introducing a Bottle to a Breastfed Baby
The information in this post is also contained in our Working & Breastfeeding.
Here is one approach to beginning pumping and introducing bottles that has worked well for many mothers as they prepared to return to work:
- Once breastfeeding is well established – usually after about four weeks – begin pumping after one feeding a day where your breasts still feel a little full. Remember you are pumping “leftovers” and should only expect a small amount.
- Freeze that first pumping immediately. You can add other pumpings to it after they have been cooled in the freezer.
- Your pediatrician may have given you a total number of ounces your baby may feed in a day or a range from the smallest probable amount to the largest, based on your baby’s weight.
- If dealing with a total volume over a 24-hour period, divide that by the typical number of times your baby feeds for a target volume for the first bottle.
- If dealing with a range, store volumes of the lower amount.
- Store some extra small volumes in case baby is hungrier than expected.
- When you have enough stored to equal the expected volume and a bit more, you can begin to plan a time to introduce a bottle.
- EXAMPLE for offering the first bottle:
- Your pediatrician suggests that your baby probably takes about 24 ounces a day.
- You know that he feeds between eight and 12 times a day.
- That means he could take anywhere from 2 to 3 ounces.
- You pump until you have a 2-ounce bottle and then have several 1/2 ounce bottles to equal at least three ounces or more saved.
- Choose a day that your primary support person will be available and a feeding time where baby tends to be more pleasant and patient for his feeding.
- Baby may accept a bottle more easily from someone other than you. He knows milk comes from you and may not understand why he’s not going there instead of to this foreign object.

- Thaw out the 2-ounce bottle in the refrigerator overnight.
- When baby begins to stir, place the bottle from the refrigerator in a bowl of warm water (bath temperature) or a bottle warmer while the person offering the bottle goes to get baby from his bed, changed and ready for the feeding.
- Often it helps to run the bottle nipple under warm water, if it was also in the refrigerator, to make it more acceptable to the baby.
- Baby should be held in an upright, almost sitting, position that is similar to the position usually used by the support person.
- The warmed bottle should be held at an angle tilted just enough to fill the nipple to allow baby to keep control of when and how fast the milk comes.
- Tickle the baby’s mouth to encourage an open mouth then bring baby up onto the bottle nipple, aiming the nipple toward the palate.
- Some have found that it can help to have an article of clothing you have worn, like a nightgown or t-shirt, to place on their arm, shoulder, or chest where the baby can smell your scent.

- It is usually best if you are close but not present in the room during this first “experiment” with bottle feeding. Your baby is very wise and will wait for you to come feed her if she knows you are nearby.
- If dealing with a total volume over a 24-hour period, divide that by the typical number of times your baby feeds for a target volume for the first bottle.
Once the feeding is completed, you will pump to create a bottle equal to what the baby consumed. Remember that the baby is always better than a pump! If you do not pump as much as the baby took, it is more likely a pump issue than an issue of not enough milk. Just pump after another breastfeeding and add that amount to what you pumped to get the amount baby took.
You will continue this pattern until you have enough milk stored in your freezer to get you through a normal work day plus a few extra for any hectic day at work where you may not have been able to pump as often. Plan to fully breastfeed for all feedings when not separated from your baby.
Working and Breastfeeding
Feeding Breastmilk From a Bottle
Pumping
Cleaning and Sanitizing Pumping Accessories
Hand Expressing
Published August 2018.
Eight Tips for How to Introduce Bottle-Feeding
As a nurse in the Institute for Maternal-Fetal Health at Children’s Hospital Los Angeles, I meet many moms who are intimidated when it comes to knowing when and how to introduce bottle-feeding to their babies. It can be especially intimidating because of the many myths associated with starting bottle-feeding. My experience helping moms on this issue is what inspired this post and I hope to help ease the anxiety for those who wonder when and how to introduce bottle-feeding.
There are no mandatory rules about when to add a bottle to a baby’s feeding routine, but here are some expert tips that may make the process easier. (Tweet this)
1. Add a bottle after a healthy milk volume is established from your breast. If you are exclusively breastfeeding and want to keep it that way, then only introduce a bottle after you have established a healthy milk volume and breastfeeding routine.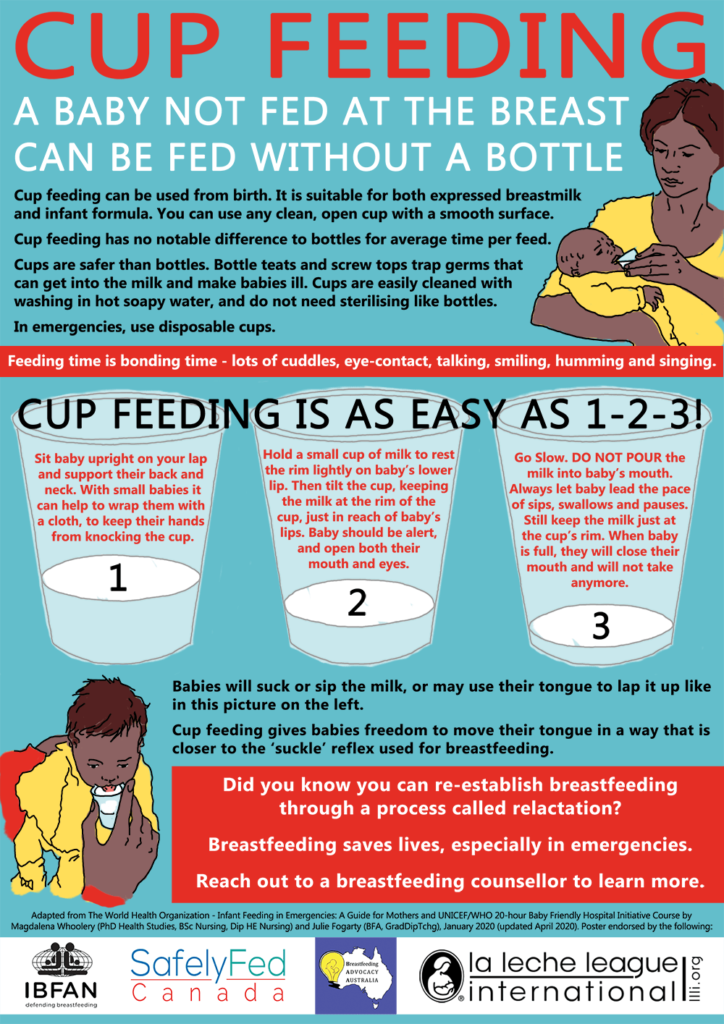 This can take up to four weeks after birth.
This can take up to four weeks after birth.
2. Continue breastfeeding or pumping to maintain milk volume. When your baby is feeding from the bottle, make it a priority to pump (and breastfeed when your baby is not using the bottle). Decreasing the amount of times milk is expressed from your breast can lead to a decrease in the volume produced.
3. Nipple confusion versus nipple preference. Many people believe that babies don’t want to be breastfed after bottle feeding or don’t want to bottle-feed after exclusively breastfeeding because of nipple confusion. This is not true. Babies do not get confused about the different feeding methods. But they do get accustomed to the breast or bottle and establish a nipple preference, which only means that they prefer one method over the other!
4. Use a bottle nipple that is wide-based, which is similar in size and shape to your nipple. I recommend wide-based nipples. Purchase a bottle with a nipple that is more similar to the human breast. These nipples are usually wide-based with shorter nipple heights. The nipple requires that the baby take a larger amount of the nipple into its mouth, similar to breastfeeding.
Purchase a bottle with a nipple that is more similar to the human breast. These nipples are usually wide-based with shorter nipple heights. The nipple requires that the baby take a larger amount of the nipple into its mouth, similar to breastfeeding.
5. Purchase one nipple and bottle style at a time. Some babies are very picky when it comes to bottles, especially if they have been exclusively breastfeed. It is a good idea to buy one set of a certain bottle and nipple style at a time to make sure your baby can feed well before buying a larger supply. Sometimes babies will try out multiple bottles and nipples before they decide on a favorite.
6. Use a slow-flow feeding style. A slow-flow feeding style with a bottle closely resembles that of breastfeeding. Babies that breastfed are used to working for their food and it comes out at a slower rate. Whereas, bottle-feeding is easy and takes little effort. The rate is much quicker and babies can get used to this fast rate, making breastfeeding more frustrating when returning from bottle-feeding.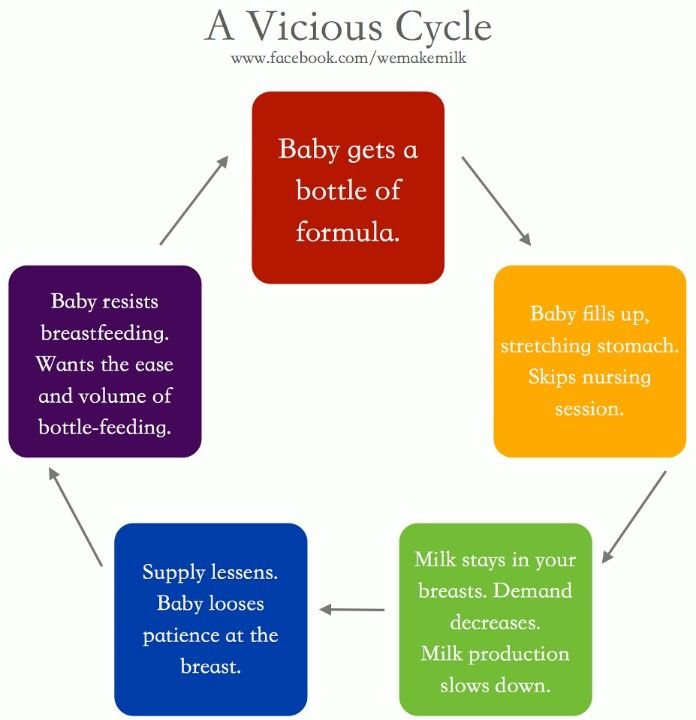 If you are using a regular nipple allow the baby to take five to ten sucks and remove the bottle. Allow your baby to swallow and breathe. Then reinsert the bottle and start again. This process should encourage your baby to slow down their feeding. The feeding should take roughly 15 minutes, similar to that of a breastfeeding session.
If you are using a regular nipple allow the baby to take five to ten sucks and remove the bottle. Allow your baby to swallow and breathe. Then reinsert the bottle and start again. This process should encourage your baby to slow down their feeding. The feeding should take roughly 15 minutes, similar to that of a breastfeeding session.
7. It takes time. Many exclusively breastfed babies do not accept a bottle right away, so it may take a couple of attempts before your baby gets the hang of it. Be patient and continue to offer the bottle to your baby.
8. Introduce bottle-feeding two to four weeks before going back to work. By doing this, you can establish a pumping routine, allow your baby time to adjust to the bottle and give you a chance to see that your baby is able to feed from the bottle effectively. The above tips will help you a lot when you begin your journey of bottle-feeding your baby. Most of the time a baby will accept a bottle very well, but there are a few that can really make the transition frustrating.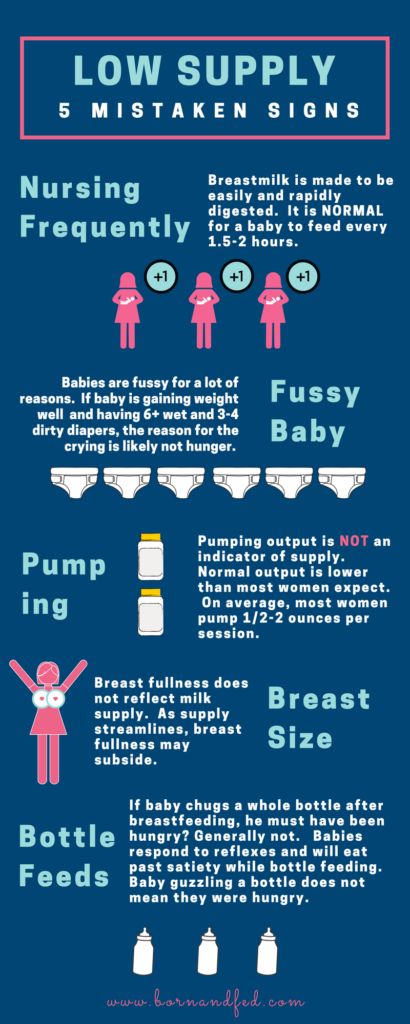 If you are having a difficult time introducing bottles or your baby does not seem to be feeding as well with a bottle, please enlist the help of a breastfeeding expert.
If you are having a difficult time introducing bottles or your baby does not seem to be feeding as well with a bottle, please enlist the help of a breastfeeding expert.
Thank you for taking the time to read my post, I hope you found this information helpful. If you want advice on a specific topics please feel free to write a comment and I can address your needs in future posts.
Feeding with expressed milk | breastfeeding
When can I start breastfeeding my baby with expressed breast milk? How to do it right? Is it worth worrying that the child will confuse the pacifier with the breast? In this article we will answer your questions.
Share this information
When can I start breastfeeding my baby?
If your baby is healthy and breastfeeding well, there is no need to give him expressed milk. For the first four weeks, you work together to start and increase milk production, and your baby also learns to suckle properly at the breast.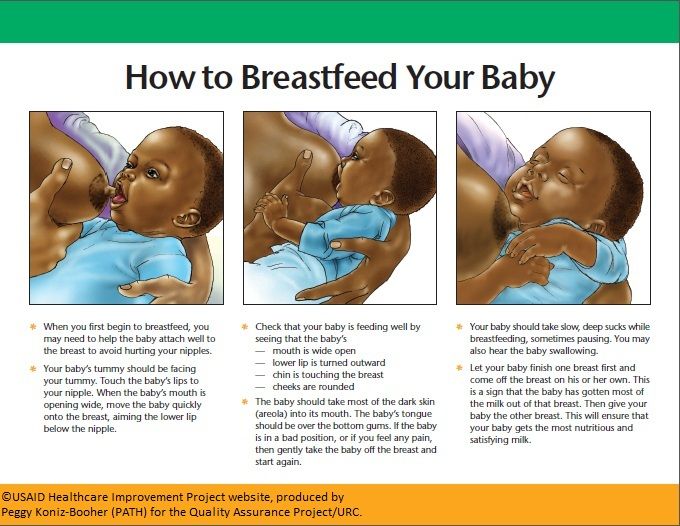 There is not enough scientific data on this yet, 1 but there is an opinion that bottle feeding in the first month may adversely affect the process of establishing breastfeeding.
There is not enough scientific data on this yet, 1 but there is an opinion that bottle feeding in the first month may adversely affect the process of establishing breastfeeding.
However, if the newborn is unable to latch on or suckle for some reason, start expressing milk as soon as possible after delivery. Read more about this in our articles on coping with problems in the first week, breastfeeding premature babies and babies with special needs, and seeking help from your healthcare provider.
How can I feed my baby with expressed breast milk?
There are many expert feeding solutions that allow you to give your baby expressed milk in a variety of ways, depending on your and your baby's needs.
For example, the innovative Calma smart pacifier only lets milk through when the baby creates a vacuum by suckling. This means that when feeding from a bottle, he will make the same movements with his tongue and jaws as when sucking at the breast. 2. 3 Calma was developed with the help of breastfeeding experts from the University of Western Australia. When using this pacifier, the baby can suck, swallow, pause and breathe in the same way as when breastfeeding. 4 Preserving natural sucking habits allows baby to transition easily from breast to bottle and back.
3 Calma was developed with the help of breastfeeding experts from the University of Western Australia. When using this pacifier, the baby can suck, swallow, pause and breathe in the same way as when breastfeeding. 4 Preserving natural sucking habits allows baby to transition easily from breast to bottle and back.
In addition, Medela also offers regular bottle teats* in two versions that produce milk at different rates. All Medela* nipples can be placed directly on bottles used for expressing milk, minimizing the risk of spillage.
If you need to feed your baby with expressed milk, but you do not want to bottle feed him until he is learning to breastfeed, you can use a sippy cup* for temporary feeding. The baby will be able to drink milk from such a mug, but you should be careful not to spill the milk. For the first time, it is advisable to feed the child from a drinking cup under the supervision of the attending physician in order to learn how to do it correctly.
If your baby needs to be supplemented with expressed milk in addition to regular breastfeeding, the Supplementary Feeding System (SNS)* can be used. It is equipped with a thin, flexible capillary that can be clipped close to the nipple to give your baby expressed milk while breastfeeding. Thanks to this, the baby suckles the breast for longer, thereby developing sucking skills and stimulating the production of milk from the mother. This can be helpful when there is a shortage of breast milk, as well as when feeding adopted or surrogate children.
If the baby is unable to breastfeed because he is too weak or has a congenital disease, you can use the Special Needs Cup*, which releases milk with gentle pressure, making it suitable for feeding these babies.
How to teach a child to bottle feed?
If breastfeeding is going well and you decide to start bottle feeding your baby with expressed breast milk, follow these guidelines.
Start early and take your time
Don't wait until the first day of work or the first time you leave the house to start bottle feeding your baby. Start accustoming your baby to small portions of expressed milk a couple of weeks before the desired date, calmly and without haste. Gradually build up to one full serving of pumped milk from a bottle.
Start accustoming your baby to small portions of expressed milk a couple of weeks before the desired date, calmly and without haste. Gradually build up to one full serving of pumped milk from a bottle.
Choose a time
Ideally, at the first bottle feeding, the baby should be hungry, but not too hungry - in this state, he is as relaxed as possible.
Let others feed
Your baby is used to feeding from your breast, so when you offer him a bottle it can be confusing. The process can go faster if the first time the baby is bottle-fed by someone else while you are not in the room, so that your sight and smell do not embarrass the baby.
Maintain optimal temperature
Your baby will be more willing to eat expressed milk if the temperature is around 37°C, close to body temperature.
Dip the nipple in milk
Try dipping the nipple in expressed milk before offering it to your baby. This way it will taste and smell like your breast milk. Lightly touch the baby's upper lip with the nipple to open the mouth.
This way it will taste and smell like your breast milk. Lightly touch the baby's upper lip with the nipple to open the mouth.
Choose the right position for bottle feeding
Feed your baby on demand and keep him reclining during feeding. Never bottle feed your baby when he is lying or sitting, otherwise he may choke. Listen to the wishes of the child - take as many pauses as he needs. You can even try to shift it from one hand to another during feeding.
Be patient
Don't worry if your baby doesn't take the bottle right away - it may take several tries. If he pushes the bottle away or starts crying, calm him down, wait a few minutes and try again. If he still doesn't want to bottle feed, wait a few more minutes and breastfeed him as usual. Repeat the bottle experiment at a different time of day.
How much pumped milk should I give my baby?
All children are different. Research shows that between the ages of one and six months, a baby can consume between 50 and 230 ml of milk per feeding. To start, prepare about 60 ml and observe how much your baby needs - more or less. You will soon realize how much milk he usually eats. Just never force him to finish the cooked portion.
To start, prepare about 60 ml and observe how much your baby needs - more or less. You will soon realize how much milk he usually eats. Just never force him to finish the cooked portion.
How can I keep my baby safe when bottle feeding?
Always clean and sterilize your pump and bottles according to the manufacturer's instructions. Wash your hands before expressing, pouring milk, and feeding your baby. Follow our instructions for safely storing and thawing your expressed milk.
If breastmilk needs to be warmed, place the bottle or bag in a bowl of warm water or a heater or under running water at a maximum of 37°C. Never heat breast milk in the microwave or on the stove.
Will the baby be able to transition from breast to bottle?
Some mothers worry that if they start bottle feeding too early, the baby will get used to the artificial nipple and not want to breastfeed. Others, on the contrary, are worried that if the child is not immediately accustomed to the bottle, then he will no longer eat from it. In general, in these cases, they say that the child confuses the nipple with the breast.
In general, in these cases, they say that the child confuses the nipple with the breast.
Experts disagree on whether such confusion is a problem. 1 Without a doubt, it is easier for a baby to suckle milk from a regular bottle with a nipple, which does not require a vacuum, than from the breast, since the milk flows faster, also under the influence of gravity. And some babies really have clear preferences: only the breast or only the nipple. However, many babies are comfortable suckling both the breast and the pacifier.
If you are unable to feed your baby with expressed breast milk, seek help from a lactation consultant or specialist.
Literature
1 Zimmerman E, Thompson K. Clarifying nipple confusion. J. Perinatol. 2015;35(11):895-899. - Zimmerman I., Thompson K., "On the issue of breastfeeding." Zh Perinatol (Journal of Perinatology). 2015;35(11):895-899.
2 Geddes DT et al. Tongue movement and intra-oral vacuum of term infants during breastfeeding and feeding from an experimental teat that released milk under vacuum only. Early Hum Dev . 2012;88(6):443-449. - Geddes D.T. et al., "Language Movements and Oral Vacuum Generation in Term Infants During Breastfeeding and Feeding from an Experimental Vacuum-Delivery Teat". Airlie Hume Dev. 2012;88(6):443-449.
Early Hum Dev . 2012;88(6):443-449. - Geddes D.T. et al., "Language Movements and Oral Vacuum Generation in Term Infants During Breastfeeding and Feeding from an Experimental Vacuum-Delivery Teat". Airlie Hume Dev. 2012;88(6):443-449.
3 Segami Y et al. Perioral movements and sucking pattern during bottle feeding with a novel, experimental teat are similar to breastfeeding. J. Perinatol. 2013;33(4):319-323. - Segami I. et al., "Perioral movements and sucking during bottle feeding with a new experimental nipple are very similar to sucking from the breast." Zh Perinatol (Journal of Perinatology). 2013;33(4):319-323.
4 Sakalidis VS et al. Oxygen saturation and suck-swallow-breathe coordination of term infants during breastfeeding and feeding from a teat releasing milk only with vacuum. Int J Pediatr. 2012;2012:130769. - Sakalidis V. S. et al., "Oxygenation and Coordination of Sucking, Swallowing, and Breathing in the Term Infant During Breastfeeding and Feeding from a Purely Vacuum Teat". Int J Pediatrician 2012;2012:130769.
S. et al., "Oxygenation and Coordination of Sucking, Swallowing, and Breathing in the Term Infant During Breastfeeding and Feeding from a Purely Vacuum Teat". Int J Pediatrician 2012;2012:130769.
Read instructions before use. Consult a specialist about possible contraindications.
* RC № ФСЗ 2010/07353 of 07/19/2010
Storage, freezing and thawing of breast milk
Expressed breast milk is the best food for your baby when you are not around. How to store and use breast milk correctly?
Share this information
If you go to work, go to the gym or simply ask your partner to feed your baby and you want to get some sleep yourself, you can express breast milk so that the baby can eat even when you are not around. Most of the beneficial properties are retained in expressed breast milk, so if you are forced to skip breastfeeding, it will be a better replacement than any formula. But an important guarantee of the safety of expressed milk for your baby is hygiene. Read the article to learn how to properly store breast milk.
But an important guarantee of the safety of expressed milk for your baby is hygiene. Read the article to learn how to properly store breast milk.
What is the best way to store breast milk?
Any type of breast milk is better for the baby than formula. But freshly expressed breast milk is better than chilled, and chilled breast milk is better than frozen. The fact is that freshly expressed milk fights bacteria better, it contains more antioxidants, vitamins and fats than chilled or frozen milk 4 .
How long expressed breast milk lasts
Once your breast milk is properly collected in a clean container, you can store it at room temperature, in the refrigerator or in the freezer, depending on how soon you plan to use it. Follow the guidelines below:
Recommendations for storing expressed breast milk (for feeding healthy term babies) 2, 3
| Storage location | Room temperature | Refrigerator | Freezer | Pre-frozen |
| Safe shelf life | Up to four hours Up to six hours for milk expressed under extra clean conditions* | Up to three days Up to five days for milk expressed under extra clean conditions* | Up to six months Up to nine months for milk expressed under extra clean conditions* | Up to two hours at room temperature Up to 24 hours refrigerated Do not freeze again! |
* "Very clean environment" refers to strict adherence to the instructions in the article on cleaning and sterilizing the Medela 9 breast pump0104 . These instructions for storing and thawing breast milk are guidelines only. For more information, contact a lactation consultant or healthcare professional.
These instructions for storing and thawing breast milk are guidelines only. For more information, contact a lactation consultant or healthcare professional.
If the baby is in the neonatal intensive care unit (NIU) or intensive care unit, stricter cleaning and storage guidelines may apply in accordance with the hospital's internal policies.
Before placing expressed milk in the refrigerator or freezer, be sure to mark the bottles or bags with the amount of milk and the date of expression. This will make it easier to manage your pumped milk supply.
Recommendations for feeding expressed breast milk
During storage, breast milk usually separates into layers and the fats (cream) it contains rise to the top. Shake the bottle lightly to mix the layers before giving it to your baby. Strong mixing and shaking can destroy some of the nutritional and protective components of breast milk 5 .
When a baby is fed expressed breast milk from a cup or bottle, bacteria from the mouth naturally enters the milk. Therefore, it is best to throw out all the unfinished milk one to two hours after the first feeding. In order to waste as little expressed milk as possible, it is best to store it in small portions and use just enough for one feeding 2 .
Therefore, it is best to throw out all the unfinished milk one to two hours after the first feeding. In order to waste as little expressed milk as possible, it is best to store it in small portions and use just enough for one feeding 2 .
How to Store Breast Milk in the Refrigerator
2, 3Follow the guidelines below to safely store expressed milk in the refrigerator.
- Refrigerate breast milk as soon as possible after pumping.
- Store milk in clean BPA-free breast milk bottles or breast milk storage bags. Its long-term effects on the human body are not well understood and manufacturers are now moving away from the use of this chemical in plastic containers and covers.
- After pre-cooling, a small amount of expressed milk can be added to the milk container stored in the refrigerator. Do not add warm breast milk to already chilled milk.
- Store breast milk in the coldest part of the refrigerator, on the back of the shelf above the vegetable drawer.
 Do not store milk in the refrigerator door where the temperature is not as constant.
Do not store milk in the refrigerator door where the temperature is not as constant.
How to store breast milk in the freezer
2, 3The following are guidelines for the safe freezing of breast milk.
- Freeze breast milk as soon as possible after pumping.
- After pre-cooling, expressed milk can be added to the already frozen milk container. Do not add warm breast milk to already frozen milk.
- To simplify defrosting and reduce waste, store milk in small portions (less than 60 ml). Once thawed, portions can be mixed.
- Make sure the breast milk container is suitable for freezing: some containers (eg glass bottles) may burst at low temperatures. Medela Breast Milk Storage Bags are ideal for storing frozen breast milk: they are ready to use, cold-resistant and easy to label.
- Do not fill bottles or bags more than 3/4 full as milk expands when frozen.
- Store frozen breast milk in the back of the freezer where the temperature is constant.
 Do not place it against the walls of freezers with automatic defrosting.
Do not place it against the walls of freezers with automatic defrosting.
Feeding frozen breast milk
2, 3Follow these guidelines when thawing breast milk to keep it safe for your baby.
- Breast milk can be thawed in the refrigerator, usually takes about 12 hours. You can place the bottle or bag of frozen milk under running warm water (max. 37 °C). Do not thaw breast milk at room temperature.
- Fully thawed breast milk can be stored for up to two hours at room temperature and up to 24 hours in the refrigerator.
- Do not thaw or reheat frozen breast milk in a microwave oven or in boiling water. This can negatively affect the nutritional and protective properties of breast milk, and due to uneven heating, the baby can burn.
- If, after defrosting, you left breast milk at room temperature, but did not feed it to the baby within two hours, the milk must be discarded.
- Do not refreeze breast milk.
How to warm up expressed breast milk
2, 3 Healthy full-term babies can be given breast milk at room temperature or heated to body temperature. Some children care about the temperature of the milk, while others drink milk at any temperature.
Some children care about the temperature of the milk, while others drink milk at any temperature.
- To warm breast milk, place the bottle or bag in a cup, mug or bowl of warm water for a few minutes until the milk is at body temperature (37°C). You can use a bottle warmer. Do not heat milk above 40°C or microwave it to avoid overheating.
- Slightly shake the milk in the bottle or bag to mix the separated fat (see above). Do not stir or shake the milk too hard.
Why does milk smell strange after storage?
Chilled or thawed breast milk may smell different from fresh
. This is due to the action of lipase, an enzyme that breaks down fats into fatty acids, preventing the growth of dangerous bacteria.
Some mothers report that their milk smells rancid or soapy after storage. But if you followed all the recommendations for safe storage given in this article, such milk is absolutely safe 2 .
Storing breastmilk on the road
If you need to transport your breastmilk from work to home or nursery, use the cool bag with ice packs 2 . For more information on pumping and storing breastmilk on the go, see the article on pumping on the go.
For more information on pumping and storing breastmilk on the go, see the article on pumping on the go.
Literature
1 US Food & Drug Administration. Using a breast pump. [Internet]. Silver Spring, MD, USA: US Department of Health and Human Services; 2018 [updated 2018 Feb 04; cited 2018 Apr 12] Available from: www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/HomeHealthandConsumer/ConsumerProducts/BreastPumps/ucm061944.htm. "Instructions for using the breast pump". [Internet] Silver Spring, Maryland, USA: Department of Health and Human Services; 2018 [updated February 4, 2018; cited April 12, 2018] Article referenced: www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/HomeHealthandConsumer/ConsumerProducts/BreastPumps/ucm061944.htm
3 Eglash,A., Simon,L., & The Academy of Breastfeeding Medicine. ABM clinical protocol #8: human milk storage information for home use for full-term infants, revised 2017. Breastfeed Med 12, (2017). - Eglash A, Simon L and Academy of Breastfeeding Medicine, AVM Clinical Protocol #8: Home Storage of Milk for Term Infants 2017 Revision. Brestfeed Med (Breastfeeding Medicine) 12 (2917).
Breastfeed Med 12, (2017). - Eglash A, Simon L and Academy of Breastfeeding Medicine, AVM Clinical Protocol #8: Home Storage of Milk for Term Infants 2017 Revision. Brestfeed Med (Breastfeeding Medicine) 12 (2917).
4 Human Milk Banking Association of North America. 2011 Best practice for expressing, storing and handling human milk in hospitals, homes, and child care settings. (HMBANA, Fort Worth, 2011).- North American Breast Milk Banks Association. Fort Worth: SABGM; 2011.
5 García-Lara NR et al. Effect of freezing time on macronutrients and energy content of breastmilk. Breastfeeding Medicine. 2012;7(4):295-301. - Garcia-Lara N.R. et al., "Effect of Freezing Duration on Macronutrients and Energy in Breast Milk". Brestfeeding Honey (Breastfeeding Medicine) . 2012;7(4):295-301.
6 Office on Women’s Health.