When to start solid food for premature babies
Introducing solid foods to preterm infants in developed countries
. 2012;60 Suppl 2:31-8.
doi: 10.1159/000335336. Epub 2012 Apr 30.
D J Palmer 1 , M Makrides
Affiliations
Affiliation
- 1 School of Paediatrics and Child Health, University of Western Australia, Perth, WA, Australia. [email protected]
- PMID: 22555187
- DOI: 10.1159/000335336
Free article
D J Palmer et al. Ann Nutr Metab. 2012.
Free article
. 2012;60 Suppl 2:31-8.
doi: 10.1159/000335336. Epub 2012 Apr 30.
Authors
D J Palmer 1 , M Makrides
Affiliation
- 1 School of Paediatrics and Child Health, University of Western Australia, Perth, WA, Australia. [email protected]
- PMID: 22555187
- DOI: 10.1159/000335336
Abstract
The addition of solid foods to an infant's diet is required to provide adequate nutrition, as eventually an infant will be unable to consume a sufficient volume of breast milk to meet their nutritional needs. The timing of this important dietary change for infants born preterm (<37 weeks of gestation) should take into consideration their delayed early gross motor developmental progress, increased nutritional requirements, organ immaturity, increased gut permeability and increased risk of hospitalization from infections. Good head control is important for safe eating of solid foods: this developmental milestone may be delayed in preterm infants up to 3 months of corrected age. One randomized controlled trial has demonstrated improved nutritional intakes with the introduction of nutrient-dense solid foods from 13 weeks of uncorrected age, resulting in improved nutritional iron status and greater rate of growth during infancy. There is neither current evidence for an increased infection rate with an early introduction of solid foods in developed countries, nor is there evidence that in preterm infants maturation of renal function is reduced. However, one observational study has determined that preterm infants who had 4 or more solid foods introduced prior to 17 weeks of corrected age, or who had any solid foods introduced prior to 10 weeks of corrected age, had an increased risk of eczema development.
The timing of this important dietary change for infants born preterm (<37 weeks of gestation) should take into consideration their delayed early gross motor developmental progress, increased nutritional requirements, organ immaturity, increased gut permeability and increased risk of hospitalization from infections. Good head control is important for safe eating of solid foods: this developmental milestone may be delayed in preterm infants up to 3 months of corrected age. One randomized controlled trial has demonstrated improved nutritional intakes with the introduction of nutrient-dense solid foods from 13 weeks of uncorrected age, resulting in improved nutritional iron status and greater rate of growth during infancy. There is neither current evidence for an increased infection rate with an early introduction of solid foods in developed countries, nor is there evidence that in preterm infants maturation of renal function is reduced. However, one observational study has determined that preterm infants who had 4 or more solid foods introduced prior to 17 weeks of corrected age, or who had any solid foods introduced prior to 10 weeks of corrected age, had an increased risk of eczema development.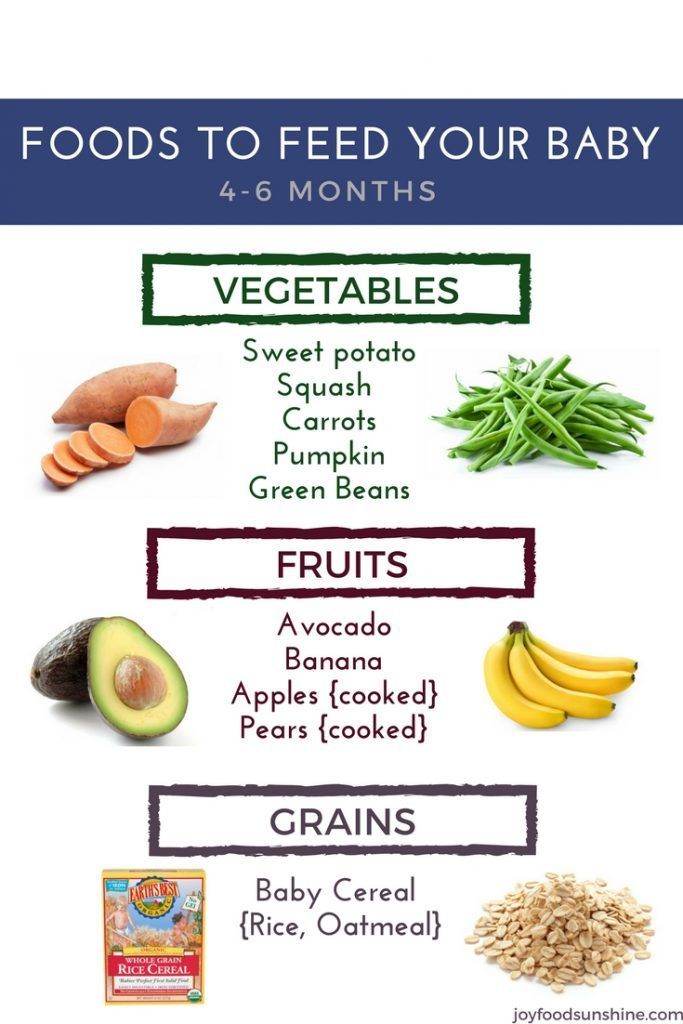 A compromise is needed to balance the nutritional benefits of commencing solid foods from 13 weeks of uncorrected age with the risks of increased eczema development, along with ensuring developmental readiness. Based on the current evidence, 3 months (13 weeks) of corrected age seems to be an appropriate age to commence nutrient-dense solid foods for most preterm infants. Further research, with an emphasis on immediate as well as longer-term consequences, would be valuable to provide more specific evidence-based guidelines regarding the introduction of solid food for preterm infants.
A compromise is needed to balance the nutritional benefits of commencing solid foods from 13 weeks of uncorrected age with the risks of increased eczema development, along with ensuring developmental readiness. Based on the current evidence, 3 months (13 weeks) of corrected age seems to be an appropriate age to commence nutrient-dense solid foods for most preterm infants. Further research, with an emphasis on immediate as well as longer-term consequences, would be valuable to provide more specific evidence-based guidelines regarding the introduction of solid food for preterm infants.
Copyright © 2012 S. Karger AG, Basel.
Similar articles
-
Nutritional needs of the micropreterm infant.
Tudehope D, Fewtrell M, Kashyap S, Udaeta E. Tudehope D, et al. J Pediatr. 2013 Mar;162(3 Suppl):S72-80. doi: 10.1016/j.jpeds.2012.11.056. J Pediatr.
 2013. PMID: 23445852
2013. PMID: 23445852 -
Infant feeding practices.
Marlin DW, Picciano MF, Livant EC. Marlin DW, et al. J Am Diet Assoc. 1980 Dec;77(6):668-76. J Am Diet Assoc. 1980. PMID: 7440862
-
Nutrient needs and feeding of premature infants. Nutrition Committee, Canadian Paediatric Society.
[No authors listed] [No authors listed] CMAJ. 1995 Jun 1;152(11):1765-85. CMAJ. 1995. PMID: 7773894 Free PMC article.
-
Weaning and complementary feeding in preterm infants: management, timing and health outcome.
Barachetti R, Villa E, Barbarini M. Barachetti R, et al. Pediatr Med Chir. 2017 Dec 22;39(4):181.
 doi: 10.4081/pmc.2017.181. Pediatr Med Chir. 2017. PMID: 29502384 Review.
doi: 10.4081/pmc.2017.181. Pediatr Med Chir. 2017. PMID: 29502384 Review. -
Postdischarge nutrition of preterm infants: more questions than answers.
Cooke RJ. Cooke RJ. Nestle Nutr Workshop Ser Pediatr Program. 2007;59:213-24; discussion 224-8. doi: 10.1159/000098538. Nestle Nutr Workshop Ser Pediatr Program. 2007. PMID: 17245102 Review.
See all similar articles
Cited by
-
Complementary feeding in preterm infants: a position paper by Italian neonatal, paediatric and paediatric gastroenterology joint societies.
Baldassarre ME, Panza R, Cresi F, Salvatori G, Corvaglia L, Aceti A, Giannì ML, Liotto N, Ilardi L, Laforgia N, Maggio L, Lionetti P, Agostoni C, Orfeo L, Di Mauro A, Staiano A, Mosca F; Italian Society of Paediatrics (SIP), Italian Society of Neonatology (SIN) and Italian Society of Paediatric Gastroenterology, Hepatology and Nutrition (SIGENP).
 Baldassarre ME, et al. Ital J Pediatr. 2022 Aug 5;48(1):143. doi: 10.1186/s13052-022-01275-w. Ital J Pediatr. 2022. PMID: 35932061 Free PMC article. Review.
Baldassarre ME, et al. Ital J Pediatr. 2022 Aug 5;48(1):143. doi: 10.1186/s13052-022-01275-w. Ital J Pediatr. 2022. PMID: 35932061 Free PMC article. Review. -
Complementary Feeding: Recommendations for the Introduction of Allergenic Foods and Gluten in the Preterm Infant.
Chiale F, Maggiora E, Aceti A, Liotto N, Coscia A, Peila C, Baldassarre ME, Bertino E, Cresi F. Chiale F, et al. Nutrients. 2021 Jul 20;13(7):2477. doi: 10.3390/nu13072477. Nutrients. 2021. PMID: 34371985 Free PMC article.
-
Longitudinal Study Depicting Differences in Complementary Feeding and Anthropometric Parameters in Late Preterm Infants up to 2 Years of Age.
Gómez-Martín M, Herrero-Morín D, Solís G, Suarez M, Fernández N, Arboleya S, Gueimonde M, González S.
 Gómez-Martín M, et al. Nutrients. 2021 Mar 18;13(3):982. doi: 10.3390/nu13030982. Nutrients. 2021. PMID: 33803743 Free PMC article.
Gómez-Martín M, et al. Nutrients. 2021 Mar 18;13(3):982. doi: 10.3390/nu13030982. Nutrients. 2021. PMID: 33803743 Free PMC article. -
Introduction and feeding practices of solid food in preterm infants born in Salzburg!
Hofstätter E, Köttstorfer V, Stroicz P, Schütz S, Auer-Hackenberg L, Brandner J, Wald M. Hofstätter E, et al. BMC Pediatr. 2021 Jan 27;21(1):56. doi: 10.1186/s12887-021-02505-6. BMC Pediatr. 2021. PMID: 33499832 Free PMC article.
-
Complementary Feeding in the Preterm Infants: Summary of Available Macronutrient Intakes and Requirements.
Salvatori G, Martini L, The Study Group On Neonatal Nutrition And Gastroenterology-Italian Society Of Neonatology OBO. Salvatori G, et al. Nutrients.
 2020 Nov 30;12(12):3696. doi: 10.3390/nu12123696. Nutrients. 2020. PMID: 33266017 Free PMC article.
2020 Nov 30;12(12):3696. doi: 10.3390/nu12123696. Nutrients. 2020. PMID: 33266017 Free PMC article.
See all "Cited by" articles
MeSH terms
Substances
Readiness for Babies to Start Solid Food
Not sure how you want to start solids? See our page on methods of starting solids.
Is baby ready to start solids?
Most healthy, full-term, typically developing babies are ready to start eating solid food around 6 months old. Before you dive in, however, make sure your baby has reached these critical developmental milestones:
- Sitting: Baby is able to sit with minimal support
- Head Control: Baby is able to hold head upright and steady while seated for duration of meal (about 15 minutes)
- Reach & Grab: Baby is able to pick up objects while seated and easily bring them to the mouth
- Interest: Baby intently watches you eat, mouths for food, or leans forward for it
 Another week of floor time and she may be ready.
Another week of floor time and she may be ready. Babies who are showing all of the above developmental milestones have the foundational skills needed to safely explore solid foods. While some pediatricians still advise starting babies on rice cereal and purées around 4 months old, this is outdated advice: as of 2021, the American Academy of Pediatrics, U.S. National Institutes for Health, and World Health Organization all recommend waiting until your baby is around 6 months old and showing signs of readiness to introduce solids. Further, studies have shown that starting solids before 4 months of age can be associated with unhealthy weight gain, both in infancy and early childhood.1
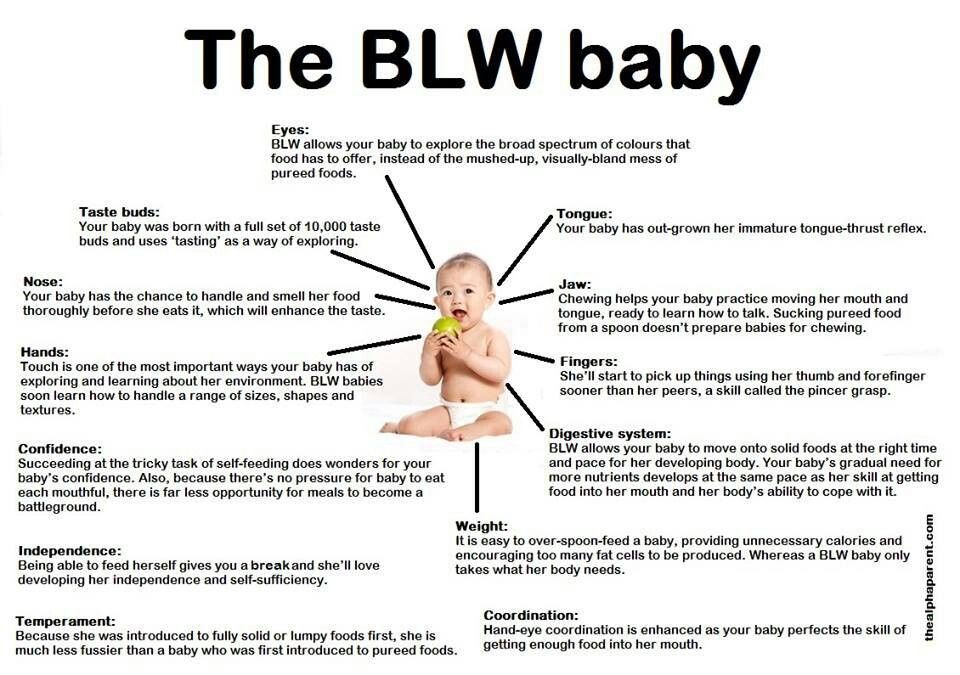
You may have heard that one of the signs of readiness for solid food is the disappearance of the tongue thrust. This claim, however, is not supported by research and it is our strong professional opinion that you need not wait for the thrust to disappear and that the thrust can actually be helpful when starting solids. Read more.
Read more.
Ready for solids? Let’s get started! See our guides and videos on starting solids and preventing picky eating.
What if my baby is 6 months old but cannot sit independently?
In general, we align with AAP and WHO recommendations to start solids. Baby should be able to sit with minimal support before starting solids, including purées, which are essential for safe chewing and swallowing, and the baby’s ability to self-feed by reaching with the arms to bring food to the mouth. Baby should maintain their head and neck upright without slouching in any direction when seated in a high chair. Head and neck stability are crucial; if the baby needs support holding the head upright, consider waiting to start solids and focus on developmental play, including tummy time and side-lying. Some babies are not ready to eat until 6.5-7 months old.
How to get started on solid food
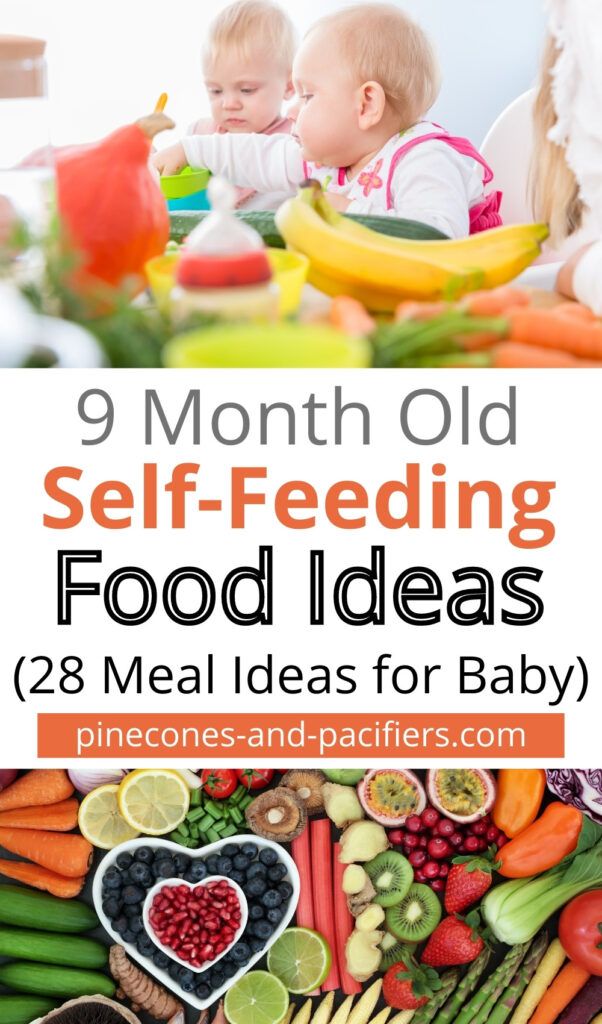
If your baby is showing all of the above signs of readiness, hooray! A food adventure awaits! There is no perfect way to introduce solid food to your baby for the very first time, but there are three general approaches to feeding: baby-led weaning (finger food first), spoon-feeding, and combo feeding (a mix of spoon-feeding and self-feeding). Regardless of the approach you take, solid food should complement—not replace breast/human milk or formula until your baby is at least one year old.
Regardless of the approach you take, solid food should complement—not replace breast/human milk or formula until your baby is at least one year old.
To learn more about each of these feeding approaches, hop over to our section on methods and feel free to improvise. Food is cultural and every family is different.
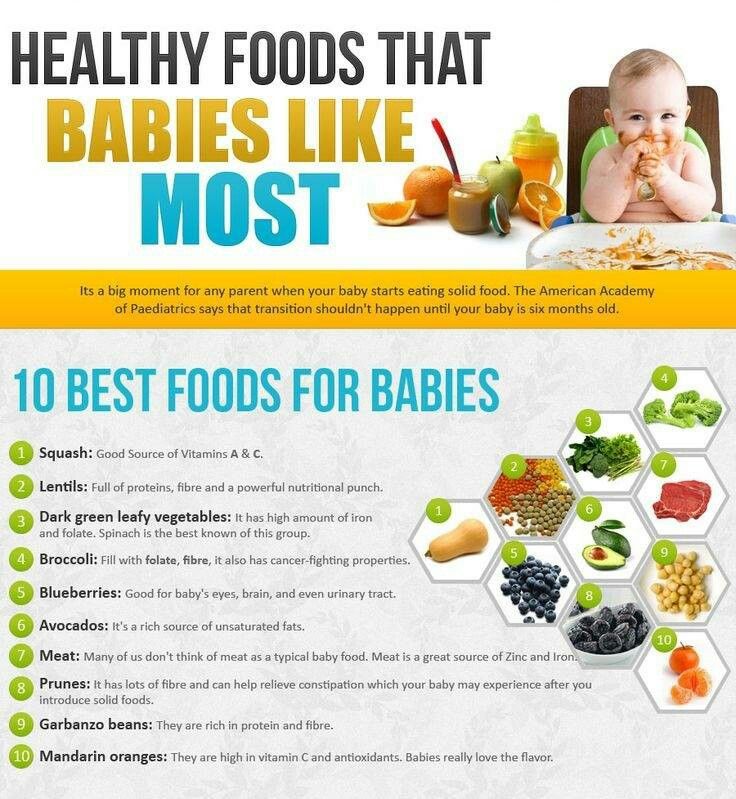
What are the best first foods for babies?
Contrary to popular belief, babies do not need to start solids with bland rice cereal and watery purées. In fact, most commercial baby food contains ingredients like rice, carrots, and sweet potatoes that are naturally high in toxic metals (arsenic, cadmium, lead, and mercury) and are not the best choices for developing brains and bodies.2
Oatmeal as an alternative to rice cerealIn terms of the best first foods, there are many nutritious options, but what is “best” for your baby will be different than what is best for another’s. Nutritionally, the best first foods for babies are those high in iron, protein, calcium, vitamins A, C, D and zinc, with iron being one of the most critical of these nutrients.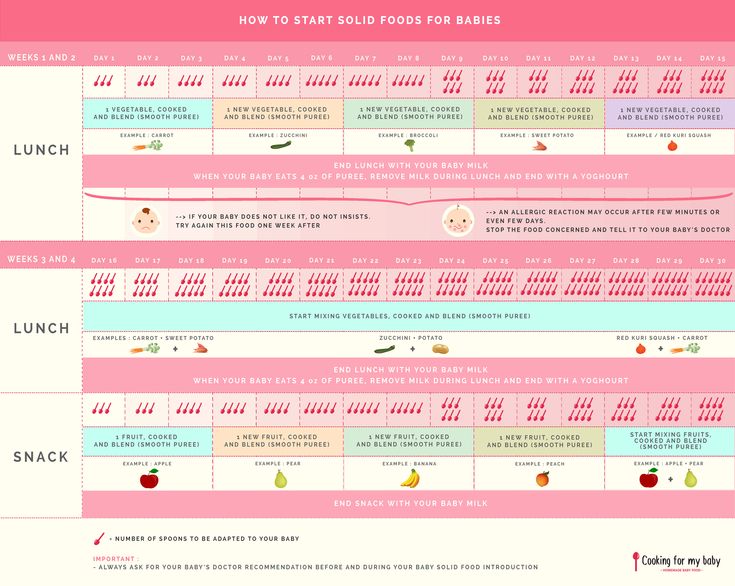 3 For our favorite first foods for babies, check out our guides, or browse our free First Foods® database.
3 For our favorite first foods for babies, check out our guides, or browse our free First Foods® database.
In addition to nutrients, consider which foods you and your family love when choosing your baby’s first foods. Because there are significant benefits to parent modeling, or eating the same foods at the same time as your baby4, first foods are best served as part of a family meal from the start, where you can model for your baby both the enjoyment and skills involved in eating.
Studies have shown that babies who are repeatedly exposed to a variety of foods in their first year of solids are more likely to accept new foods later on5 and that babies who are mostly fed a diet of bland, textureless foods are more likely to prefer these kinds of foods later in life.6
In terms of equipment, there are two categories of things you’ll want to have on hand before starting solids: items that help you create a safe eating environment and items that minimize the mess.
To prevent picky eating and to ensure you are offering the nutrients your baby needs, focus on serving a wide variety of iron-rich food, including beans, lentils, red meat, organs (such as liver), poultry, nuts, peas, and low-mercury fish, such as salmon and sardines.
When should I start solids with a premature baby?There is a lack of research on optimal timing for introduction of solids to preterm infants. For healthy preterm babies, our experts recommend beginning to look for signs of readiness (above) around six months chronological age, assuming that most (not necessarily all) preemies are ready sometime between 6 months chronological and 6 months adjusted (or corrected) age. There is some research to suggest that solids should not be introduced prior to 3 months adjusted or corrected age, even if baby is at 6+ months chronological age.7
For babies born prior to 32 weeks or babies with other co-occurring or underlying medical conditions or developmental differences, we’d recommend you consult with your medical and therapy teams to better assess when your baby is ready and if they would benefit from additional support or modifications.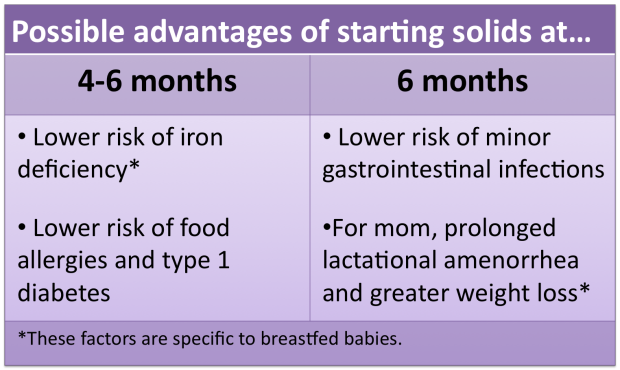 In general, signs of readiness are more important than age, but for some babies, due to more significant developmental delays or medical needs, adaptations may be necessary to ensure that they are given opportunities to explore foods in a safe manner during the second six months of adjusted (or corrected) age.
In general, signs of readiness are more important than age, but for some babies, due to more significant developmental delays or medical needs, adaptations may be necessary to ensure that they are given opportunities to explore foods in a safe manner during the second six months of adjusted (or corrected) age.
Just like for full term babies, consumption should not be the focus when starting solids. Starting solids is a time for learning brand new skills and motor patterns, so prioritize skill building, not how many bites are taken or how much gets swallowed at the table. Premature babies may have increased nutritional needs compared to full term babies, but those needs should be met primarily by breast (human) milk or formula, not solids, from 6-12 months old. Aim to offer your baby just one solid food meal opportunity per day the first 1-2 months of starting solids, increasing to 2 times per day after that, then moving towards 3 times per day close to 12 months adjusted or corrected age.
While there is no perfect food to start with for premature babies, aim to introduce a wide variety of nutrient dense solids over those first several months of starting solids. This way, any amount that is swallowed has a big impact. Use our first food database to filter by 5-star foods, to find the most nutrient dense options that suit your family and culture, and serve these. Keep in mind that premature babies may have developmental delays, medical issues (such as respiratory concerns, cardiac anomalies, or gastrointestinal differences), or sensory processing differences, which can all impact the speed of learning new skills and may put a premature baby at increased risk for choking compared with full term peers. Due to this, we advise you to default to the safest food preparations possible when starting solids, go slow, and use extra caution when advancing to finger foods.
When should I wean a premature baby?While you may have heard that toddlers can technically be weaned fully off the bottle and off breast/chest feeding by around 12 months old, many full term, typically developing babies are not quite ready for this until closer to 15-18 months old. We would expect many premature babies to need additional time beyond this before being ready to wean fully off breast (human) milk or formula, likely not until closer to 18-24 months old. This additional time assures that they have strong chewing skills and can eat a wide variety of solid foods efficiently. Weaning however is a very personal decision and should be done when it feels right for your baby and you.
We would expect many premature babies to need additional time beyond this before being ready to wean fully off breast (human) milk or formula, likely not until closer to 18-24 months old. This additional time assures that they have strong chewing skills and can eat a wide variety of solid foods efficiently. Weaning however is a very personal decision and should be done when it feels right for your baby and you.
Most premature babies are able to catch up to peers with regards to development by around 2 years old adjusted or corrected age, when the American Academy of Pediatrics recommends no longer correcting for prematurity. We would expect most premature babies to catch up with their feeding and oral motor skills by that time as well. If they have not, or as soon as you realize that they will likely not be able to catch up by 24 months, speak with your child’s doctor about a referral to a feeding specialist (an occupational therapist or speech and language pathologist who specializes in pediatric feeding).
Is sitting with support bad for babies?
Placing babies in sitting “containers” like a bumbo seat, swing, bouncer, or stander for extended periods of time can be detrimental to a baby’s development. The less time babies spend in unrestricted floor time, the less they practice moving and learning to get in and out of positions on their own. Containers/sitting devices that place the hips in what’s called posterior pelvic tilt—think of sitting with your knees higher than your hips and your butt tucked (like a bumbo seat) may cause issues with the musculoskeletal development of the spine. From a research standpoint, there is data to support that babies spending more time on the floor is conducive to the faster acquisition of motor skills. But the rest is more assumed/ correlated not proved causative.
Using supported sitting during short periods of play to facilitate baby’s use of their extensor muscles and core stabilizers is a widely accepted therapeutic practice, for children with and without developmental delay. There is no research to support the idea that short periods of play in sitting on the floor with a caregiver assisting is in anyway detrimental to motor or musculoskeletal development, and on the contrary, can help develop the muscles of the back and spine as baby learns to shift weight and correct for loss of balance.
There is no research to support the idea that short periods of play in sitting on the floor with a caregiver assisting is in anyway detrimental to motor or musculoskeletal development, and on the contrary, can help develop the muscles of the back and spine as baby learns to shift weight and correct for loss of balance.
What you’ll need to get started
In addition to a proper high chair, there are a few things you’ll need before you start your baby on solid food. But of equal importance to the equipment, is your own mental readiness. Make sure to create a safe eating environment. Familiarize yourself with the methods of introducing solids. And lastly, manage your expectations: learning to eat is a process and it will take your baby some time to get the hang of it.
Safety Equipment:
- High chair: Upright seat, adjustable footplate, and removable tray so baby can eat at the table with you. Learn more about what to look for in a high chair (or how to modify one you already have) in our Ultimate Guide to High Chairs for Babies.

- Open Cup: Age-appropriate, small open cup that won’t break or shatter.
- Plates & Bowls: Dinnerware that won’t shatter or hurt someone when it flies across the room. Those that suction to the table and have a rim work best for self-feeding.
Minimizing the Mess:
- Splat Mats: 2-3 waterproof mats for underneath and around the high chair.
- Bibs & Smocks: Bib with a catch basin and 3-4 smocks (can be worn beneath the bib)
- Washcloths: Lots of them!
Note: This page has been created with typically developing infants and children in mind. The information here is generalized for a broad audience and is for informational purposes only. Your child is an individual and may have needs or considerations beyond generally accepted practices. If your child has underlying medical or developmental differences, including but not limited to prematurity, developmental delay, hypotonia, airway differences, chromosomal abnormalities, craniofacial anomalies, gastrointestinal differences, cardiopulmonary disease, or neurological differences, we strongly recommend and encourage you to discuss your child’s feeding plan and when and how to start solids and finger food with the child’s doctor, health care provider or therapy team.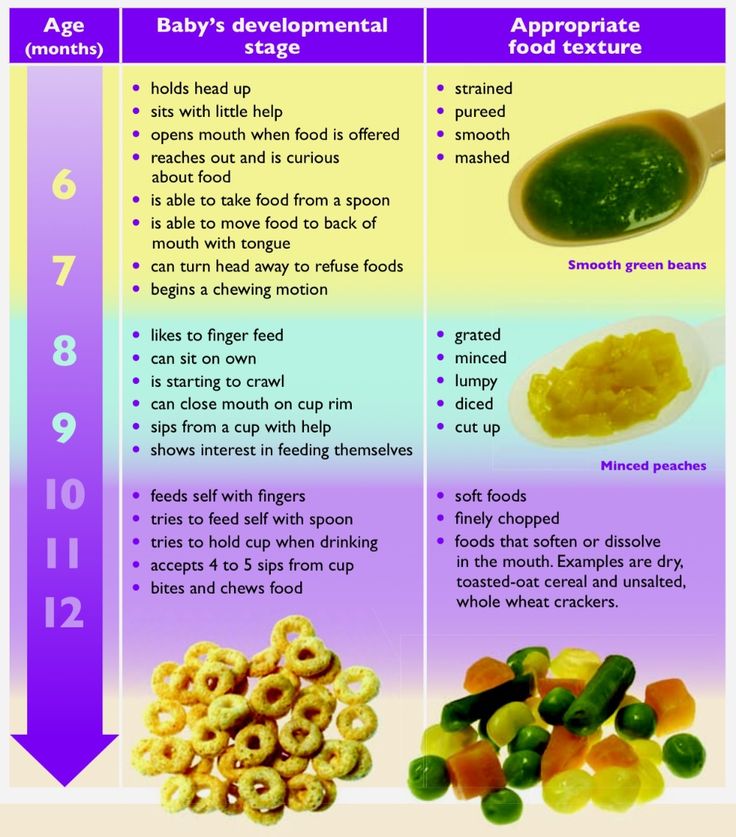 Close consultation with a feeding and swallowing specialist can provide safe guidance for the child’s feeding journey. Always seek the advice of your doctor, health care provider or therapy team with any questions you may have regarding your child’s development and capacity for starting solid foods.
Close consultation with a feeding and swallowing specialist can provide safe guidance for the child’s feeding journey. Always seek the advice of your doctor, health care provider or therapy team with any questions you may have regarding your child’s development and capacity for starting solid foods.
- Pediatrics, Official Journal of the American Academy of Pediatrics. Timing of Solid Food Introduction and Risk of Obesity in Preschool-Aged Children. Susanna Y. Huh, Sheryl L. Rifas-Shiman, Elsie M. Taveras, Emily Oken and Matthew W. Gillman Pediatrics. March 2011, 127 (3) e544-e551.
- Healthy Babies, Bright Futures, Lowering the Levels: A Healthy Baby Food Initiative 2019.
- NCBI, Infant and Young Child Feeding, 2009.
- Wardle J., Cooke L. Genetic and environmental determinants of children’s food preferences. Brithish Journal of Nutrition. 2008; 99(1): S15-S21. doi: 10.1017/S000711450889246X
- Bouhlal S., Issanchou S., Chabanet C., Nicklaus S. ‘Just a pinch of salt’.
 An experimental comparison of the effect of repeated exposure and flavor-flavor learning with salt or spice on vegetable acceptance in toddlers. Appetite. 2014;83:209–217. doi: 10.1016/j.appet.2014.07.032.
An experimental comparison of the effect of repeated exposure and flavor-flavor learning with salt or spice on vegetable acceptance in toddlers. Appetite. 2014;83:209–217. doi: 10.1016/j.appet.2014.07.032. - Bently, Amy. Inventing Baby Food. p 159. (2014).
- Cleary, J., Dalton, S., Harman, A., & Wright, I. (2020). Current practice in the introduction of solid foods for preterm infants. Public Health Nutrition, 23(1), 94-101. doi:10.1017/S1368980019002337
PECULIARITIES OF ARTIFICIAL FEEDING OF PREMATURE CHILDREN OF THE FIRST YEAR OF LIFE
Every year more and more children are born who need medical nutrition from the first year of life. The reasons are well known: ecology, stress and infections. The latest technology in the manufacture of baby products allows you to cope with the most difficult situations .
Significant advances in the care of premature babies over the past decades are largely due to improved approaches to feeding them.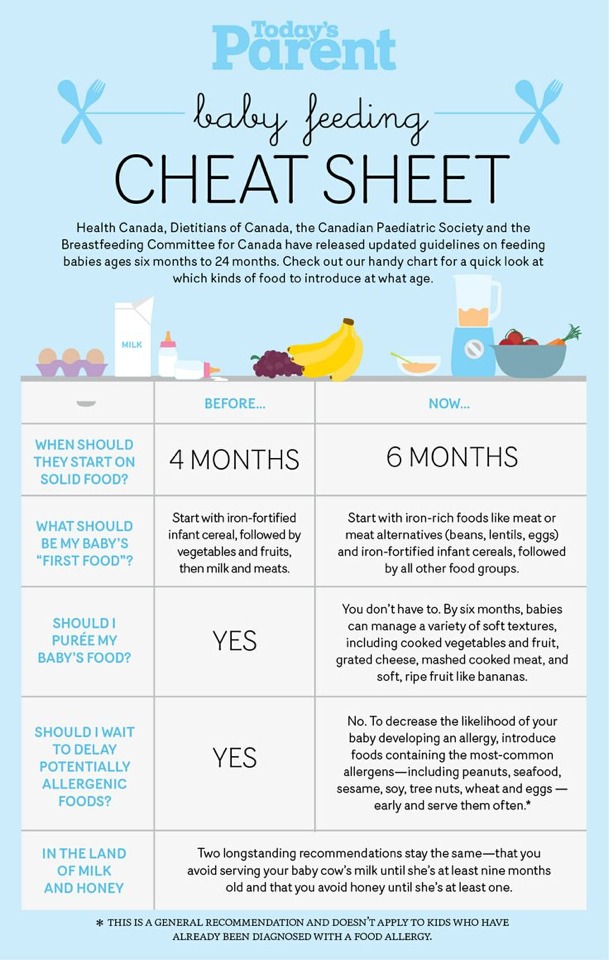 Prematurely born children are characterized by faster growth rates compared to full-term ones and therefore need a more intensive intake of energy and plastic material with food. At the same time, the functional ability of the digestive system to absorb nutrients is relatively limited, which requires special care when prescribing nutrition.
Prematurely born children are characterized by faster growth rates compared to full-term ones and therefore need a more intensive intake of energy and plastic material with food. At the same time, the functional ability of the digestive system to absorb nutrients is relatively limited, which requires special care when prescribing nutrition.
A balanced diet for premature babies requires that the chemical composition of the food is in accordance with the physiological capabilities of their digestive system. Mother's milk meets these requirements more than all other foodstuffs. Thus, for a premature baby, breastfeeding is the best way to feed.
However, unfortunately, in some cases, breastfeeding a premature baby is impossible: most mothers have hypogalactia or agalactia after premature birth, and newborns may have intolerance to breast milk proteins. The situation is aggravated by the fact that children have a reduced or absent sucking reflex due to deep prematurity, which further contributes to the extinction of lactation.
Thus, the indication for artificial feeding of premature babies is the complete absence of mother's milk and its intolerance. In this regard, there is a need to use specialized mixtures for feeding premature babies. Their development takes into account the special needs of such infants for energy and nutrients and, of course, takes into account the insufficient maturity of the digestive system, which is a limiting factor in the absorption of a number of essential nutrients (lactose, fats, fat-soluble vitamins, etc.). The composition of these mixtures is modeled in such a way as to best meet the needs of the body of a prematurely born child. At present, a number of specialized mixtures have been developed in Russia and abroad, in which the composition of breast milk of women after premature birth is taken as a standard.
These products differ in composition from standard milk formulas. In the nutrition of children born prematurely, only specialized mixtures intended for feeding premature babies (in particular, preNAN, Nestle) should be used. These products differ in composition from standard milk formulas: they contain more protein, a prerequisite is the predominance of whey proteins over caseins, the energy value of these products is slightly higher (75-80 kcal / 100 ml). Most preterm infant foods contain medium chain triglycerides in the fat portion. The carbohydrate component, in addition to lactose, is represented by maltodextrin. The content of vitamins and minerals is increased. The mixture of preNAN contains long-chain polyunsaturated fatty acids that contribute to the maturation of the nervous system and the organ of vision.
These products differ in composition from standard milk formulas: they contain more protein, a prerequisite is the predominance of whey proteins over caseins, the energy value of these products is slightly higher (75-80 kcal / 100 ml). Most preterm infant foods contain medium chain triglycerides in the fat portion. The carbohydrate component, in addition to lactose, is represented by maltodextrin. The content of vitamins and minerals is increased. The mixture of preNAN contains long-chain polyunsaturated fatty acids that contribute to the maturation of the nervous system and the organ of vision.
An essential component of these mixtures is the amino acid taurine, which plays an important role in the development of nervous tissue and the brain. The protein content in products for premature babies is higher than in analogues for full-term babies: protein is used to build tissues and cells, and a premature baby must gain weight more actively than usual. In the preNAN formula, the only one of all specialized mixtures for premature babies, the protein is even more prepared for absorption, because it is partially hydrolyzed (has smaller parts).
Soy formula should not be used in premature infants as it is difficult to digest.
TRANSFER TO ARTIFICIAL FEEDING
A specialized product should be introduced into the child's diet, taking into account individual intolerance, gradually over 5-7 days. Artificial feeding with such a mixture should be continued until the child reaches a weight of 2500-3000 g. The abolition of specialized products for premature babies and the transfer to standard mixtures is carried out gradually, with a sufficient weight gain serving as the main guideline. In the future, if necessary (a small increase in body weight), these mixtures can remain in the diet of a premature baby for several months in a small amount (1-2 feedings or can be used to breed cereals).
If necessary (profound prematurity combined with insufficient weight gain), these mixtures can be used in limited volume in combination with mixtures for term infants for several months (up to 9 months of age).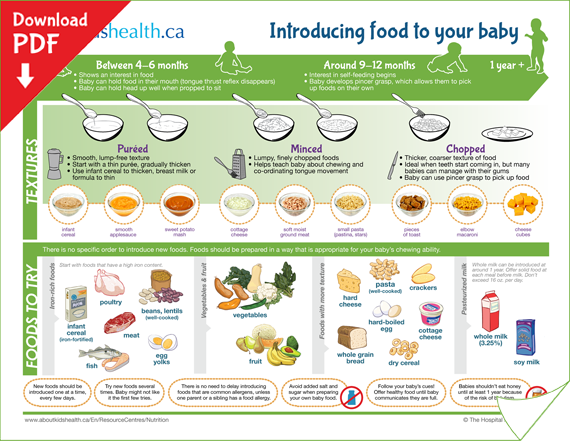 Long-term use of specialized milk formulas in a small amount (1/3-1/4 of the daily volume) makes it possible to better provide very premature babies with nutrients and increase their growth rate.
Long-term use of specialized milk formulas in a small amount (1/3-1/4 of the daily volume) makes it possible to better provide very premature babies with nutrients and increase their growth rate.
FEEDING FOR PREMATURE CHILDREN
Complementary foods for premature babies are introduced from 4-4.5 months. Since low-weight children who received massive therapy in the neonatal period, including antibacterial, are characterized by various disorders of the motility of the gastrointestinal tract, the sequence of introducing products in them has its own characteristics.
The expansion of the diet begins with the introduction of fruit puree, vegetable puree or porridge. Preference should be given to industrial products for baby food. In this case, environmentally friendly raw materials are used in their preparation, they have an appropriate degree of grinding, a guaranteed composition, and are enriched with vitamins and minerals. The introduction of complementary foods begins with monocomponent products (mashed potatoes of the Gerber trademark).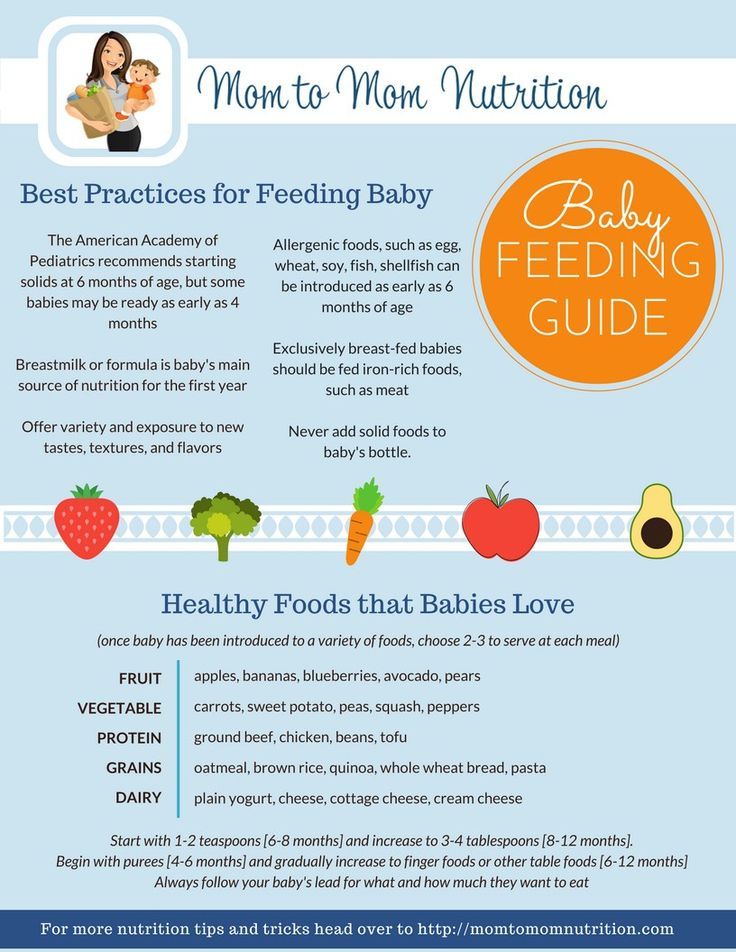 Porridges can be prescribed earlier than vegetable or fruit puree (especially if the child has malnutrition or iron deficiency anemia), but not earlier than 4 months of age. Gluten-free (buckwheat, rice) and dairy-free cereals are introduced first. They are bred with those milk mixtures that the child is currently receiving. Porridge should not contain any additives (fruit, sugar, etc.).
Porridges can be prescribed earlier than vegetable or fruit puree (especially if the child has malnutrition or iron deficiency anemia), but not earlier than 4 months of age. Gluten-free (buckwheat, rice) and dairy-free cereals are introduced first. They are bred with those milk mixtures that the child is currently receiving. Porridge should not contain any additives (fruit, sugar, etc.).
With the development of iron deficiency anemia, meat can be introduced from 5-5.5 months, given the good absorption of iron from it. Cottage cheese for premature babies is prescribed after 6 months, since the protein deficiency in the first half of the year is replenished through the partial use of high-protein mixtures intended for feeding premature babies. It is advisable to introduce juices later after 5-6 months, since if given early, they can contribute to the development of regurgitation, intestinal colic, diarrhea, and allergic reactions.
The proposed complementary feeding schemes are optimal for premature babies, and their implementation helps to prevent the development of malnutrition and health status of children.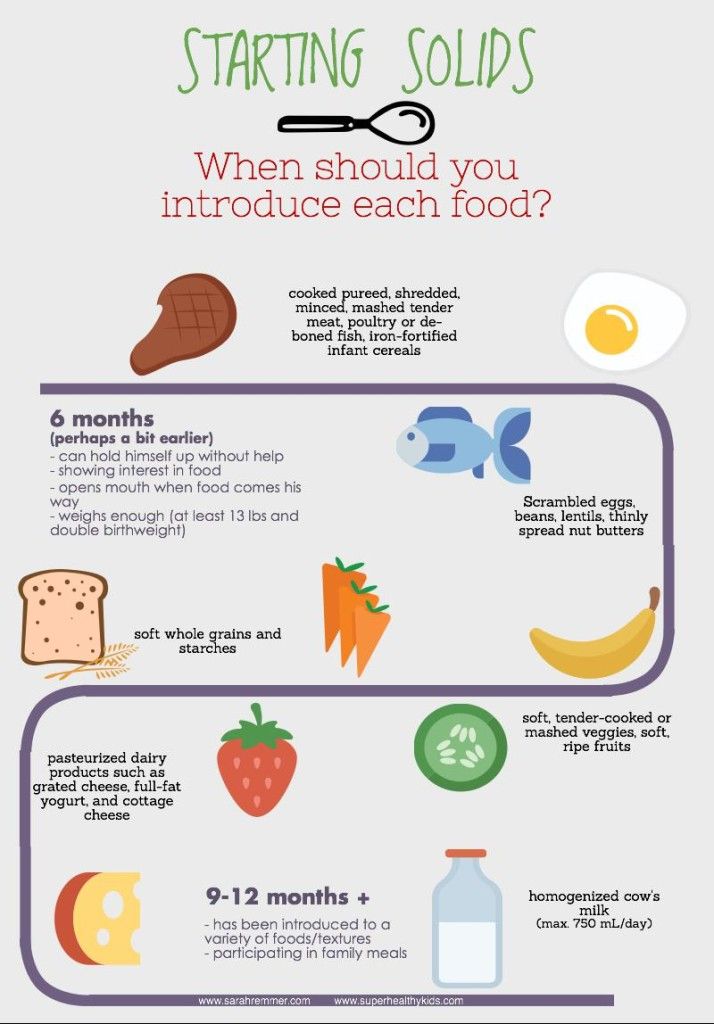
Thus, the rational feeding of premature babies should be organized taking into account their anatomical and physiological characteristics, the characteristics of their metabolism, using modern technologies. Providing a premature baby with adequate nutrition is of great importance, as it is a factor that determines not only the state of health and development of the child in the neonatal period, but also its subsequent development and learning abilities.
Budanova M.V., Ph.D. N.N. Burdenko
Complementary foods for premature babies | How to introduce complementary foods correctly
When a baby is born prematurely, many developmental milestones do not occur as usual. This directly applies to nutrition.
Saturday, March 21st, 2020
- Seal
- Share
How do you know when it's time for your baby to try new foods? And how to properly feed premature babies?
Complementary foods are what to start when breast milk is no longer enough to fully meet the nutritional needs of the baby. From now on, there is a need for other food.
From now on, there is a need for other food.
The early introduction of properly selected products helps to improve the health and physical development of the baby, strengthen the immune system, and improve the nutrition system. But if the baby is premature, what rules and features of the transition from breastfeeding to food should be followed?
See also: Nutrition for premature babies develop faster. Meanwhile, treatment and the difficulties that arose after childbirth significantly reduce the ability to absorb products. In this regard, the choice of the period when to introduce complementary foods to a premature baby depends on the physical condition of the baby and the speed of its development.
There are generally accepted guidelines for the introduction of complementary foods from the United Nations Children's Fund UNICEF and the World Health Organization. They advise that when breastfeeding, the first complementary foods should be introduced from 6 months, and with artificial or mixed - from 5 months.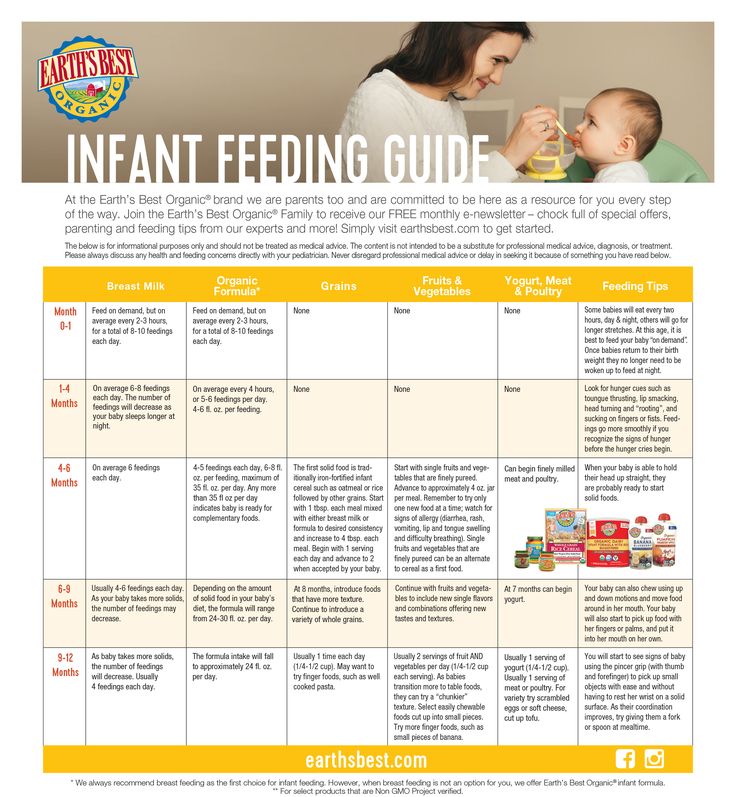 For premature babies, the moment of introduction of complementary foods can be calculated by adding to the generally accepted age the time that the baby was supposed to spend in the womb. For example, if a child was born two months prematurely, then it is advisable to start introducing complementary foods from 8 months.
For premature babies, the moment of introduction of complementary foods can be calculated by adding to the generally accepted age the time that the baby was supposed to spend in the womb. For example, if a child was born two months prematurely, then it is advisable to start introducing complementary foods from 8 months.
Intense juicy pear flavor, natural flavor, no sugar or starch - this is Gerber® Williams Pears one-component puree.
BUY
It is important to be aware that if complementary foods are introduced at the wrong time, this can adversely affect the child's health. A very early introduction to food can lead to problems with the still unprepared enzyme system of the stomach due to excess load. Moreover, scientists have concluded that the early introduction of complementary foods can cause growth retardation, the development of food allergies, as well as an increased risk of developing otitis media and pneumonia.
Also, the consequences of early introduction of complementary foods can affect the mother's lactation. As the intervals between breastfeeds increase, the stimulation of the breast decreases and the supply of milk becomes smaller.
As the intervals between breastfeeds increase, the stimulation of the breast decreases and the supply of milk becomes smaller.
But delaying the introduction of complementary foods too long is also not recommended: soon breastfeeding will not be enough to cope with the baby's nutritional needs. Lack of nutrients can adversely affect the development of the child and cause various diseases.
Signs that preterm babies are ready for complementary foods
When should you consider starting complementary foods for a premature baby? Here are some tips:
- Your baby should weigh 2.5 times its birth weight
- Tongue pushing reflex not as strong as before
- Child can sit confidently without additional assistance
- Longer intervals between breastfeeds
- Baby puts everything in his mouth that gets in his way
- Baby's first teeth erupt
Curiosity about the food that everyone at the table eats and trying to taste it is an important sign to start feeding premature babies
See also:
Where to start?
When you decide it's time to introduce complementary foods, your first step is to see your doctor.
In no case should the start of complementary feeding of premature babies coincide with preventive vaccinations!
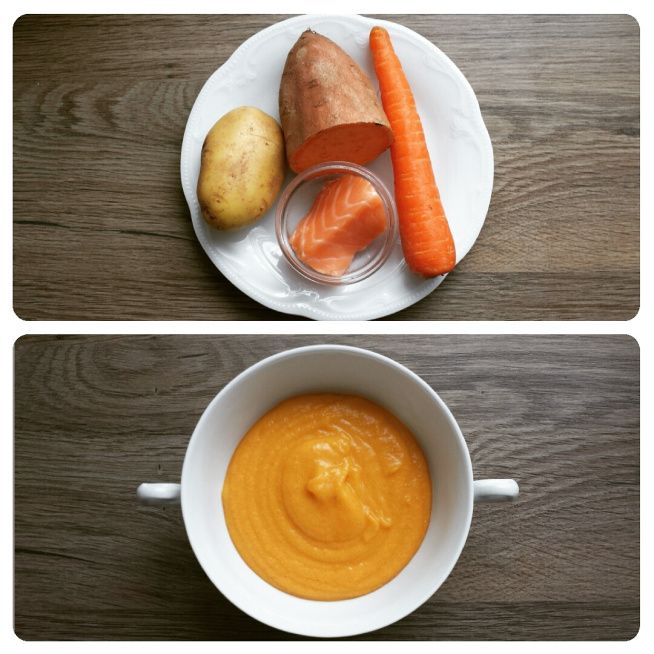
When you are convinced that the child is absolutely ready for complementary foods according to all criteria, it is recommended to start acquaintance with cereals rich in iron, which is so necessary for premature babies. After that, you can add vegetable purees to the diet. You need to start with small portions. Even if the baby liked the new food, there is no need to rush into it. Increase the amount of food gradually. If we talk about fruits, it is also desirable to add them to the menu over time, since they are an important source of vitamins. It is recommended to start each type of complementary food in the morning so that you can follow the possible reaction of the child to a new product.
The main thing is to watch the baby and how he reacts to changes in nutrition. It is also advisable to consult your doctor from time to time on this issue.