3 week old baby crying after every feed
Baby Cries After Feeding: What Should I Do?
Medically reviewed by Karen Gill, M.D. — By Chaunie Brusie on October 3, 2018
My daughter, the “crier”
My second daughter was what my oldest fondly referred to as a “crier.” Or, in other words, she cried. A lot. The crying with my baby girl seemed to intensify after every single feeding and particularly at night.
It was those hellish hours between darkness and dawn when my husband and I would take turns walking around the house with her in our arms, praying and, mostly in my case, sobbing because we couldn’t console our baby.
I didn’t know it then in my sleep-deprived state, but my daughter’s crying after feedings wasn’t that uncommon. In combination with her frequent spitting up, it was pretty much a classic textbook case of colic.
Colic
Colic, in technical terms, simply means a “crying, fussy baby that doctors can’t figure out.”
OK, so that’s not really the definition, but in essence, that’s what it boils down to. The British Medical Journal (BMJ) lists one criterion for colic: A baby that cries for at least three hours a day, three or more days a week, and is under 3 months old. Check, check, and check.
There isn’t one single known cause of colic. Even the actual clinical incidence of colic, estimated by BMJ to be around 20 percent of all babies, can be tricky.
Acid reflux
One of those causes of crying after feeding and spitting up in babies is actually acid reflux. This condition is known as gastroesophageal reflux disease (GERD) if it also causes significant symptoms such as poor weight gain.
When my “crier” daughter was 5, she frequently complained of her stomach hurting and as a result, had to undergo a series of testing with a gastroenterologist, a doctor that specializes in the GI system.
At our first appointment, the very first question he asked me was if she had colic as a baby and if she spit up a lot, to both of which I practically shouted, “Yes! How did you know?!”
He explained that acid reflux or GERD can manifest as symptoms similar to colic in babies, stomach pain in school-aged children, and later as actual heartburn pain in adolescents.
While many infants spit up, fewer have actual GERD, which can be caused by an underdeveloped flap between the esophagus and stomach or a higher-than-normal production of stomach acid.
In most cases, a diagnosis of infant reflux is simply based on your baby’s symptoms. If your doctor suspects a severe case however, there are several different tests that actually diagnose infant reflux.
Testing can involve taking a biopsy of your baby’s intestine or using a special type of X-ray to visualize any affected areas of obstruction.
Food sensitivities and allergies
Some babies, especially breastfed babies, may be allergic to certain food particles that their mothers are eating.
The Academy of Breastfeeding Medicine notes that the most common offender is cow’s milk protein in the mother’s milk, but even a true allergy is very rare. Only about 0.5 to 1 percent of exclusively breastfed babies are thought to be allergic to cow’s milk protein.
The other most common culprits, according to the ABM, are egg, corn, and soy, in that order.
If your baby is displaying symptoms of extreme irritability after feedings and has other symptoms, such as bloody stools (poop), you should speak with your healthcare provider about getting them tested for allergies.
Aside from a true allergy, there’s also been some evidence that following a low allergen diet while breastfeeding (essentially avoiding those top allergy foods, such as dairy, eggs, and corn) may be beneficial for infants with colic.
Strict elimination diets can have their own risks, so speak with your doctor before significantly changing your diet.
In our situation, I found that dairy, caffeine, and certain seeded fruit exacerbated my daughter’s crying and spitting up. By eliminating those foods and substances from my diet, I was able to help lessen her discomfort.
If you have a baby with colic, you might want to try anything at all to help ease your baby’s crying. If you’re curious to see if your diet has any effect, you can start by logging your food in a food journal and writing down your baby’s reactions after each meal.
Next, you can eliminate one food at a time and see if reducing your intake of certain foods seems to make a difference in your baby’s behavior. If you hit on one you feel helps your baby to cry less, this does not mean they will not be able to eat that food in the future.
Just be sure to keep in mind that a true allergy is rare. Also, be sure to monitor for any additional symptoms, such as blood in your baby’s poop.
Gas
If your baby is crying a lot after every feeding, it may simply be a buildup of air swallowed while eating. It’s thought that bottle-fed babes in particular may be more prone to swallowing a lot of air during a feeding. This can trap gas in their stomachs and be uncomfortable.
In general, breastfed babies swallow less air while eating simply due to the way they eat. But every baby is different and even breastfed babies may need to be burped after a feeding.
Trying keeping your baby upright after a feeding and burping gently from the bottom of their back and up through the shoulders to work the gas bubbles up and out. Also check out this illustrated guide to burping a sleeping baby.
Also check out this illustrated guide to burping a sleeping baby.
Formula
If your baby is formula-fed, swapping out the formula you use may be a simple solution to a crying baby after feedings. Every formula is a little bit different and certain brands make formulas for more sensitive baby tummies.
If you decide to try this, talk to your baby’s pediatrician about whether an elemental formula would be a good choice to try for a week. If you try one different brand and you see no change in your baby’s fussiness, continuing to try different brands is unlikely to help.
Takeaway
Colic, along with a few other common conditions, might be the culprit if you too have a “crier” on your hands.
If your baby doesn’t find relief after dietary changes or additional burping, then make an appointment to see their doctor.
Share on Pinterest
Chaunie Brusie, BSN, is a registered nurse with experience in labor and delivery, critical care, and long-term care nursing. She lives in Michigan with her husband and four young children, and is the author of the book “Tiny Blue Lines.”
She lives in Michigan with her husband and four young children, and is the author of the book “Tiny Blue Lines.”
Last medically reviewed on October 3, 2018
- Parenthood
- Baby
- 06 Months
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- ABM clinical protocol #24: Allergic proctocolitis in the exclusively breastfed infant. (2011). DOI:
10.1089/bfm.2011.9977 - Harrel MC, et al. (2015). Is there a correlation between maternal diet in breastfeeding mothers and infantile colic? DOI:
10.1097/01.EBP.0000541032.94135.ca - Mayo Clinic Staff. (2018). Infant reflux.
mayoclinic.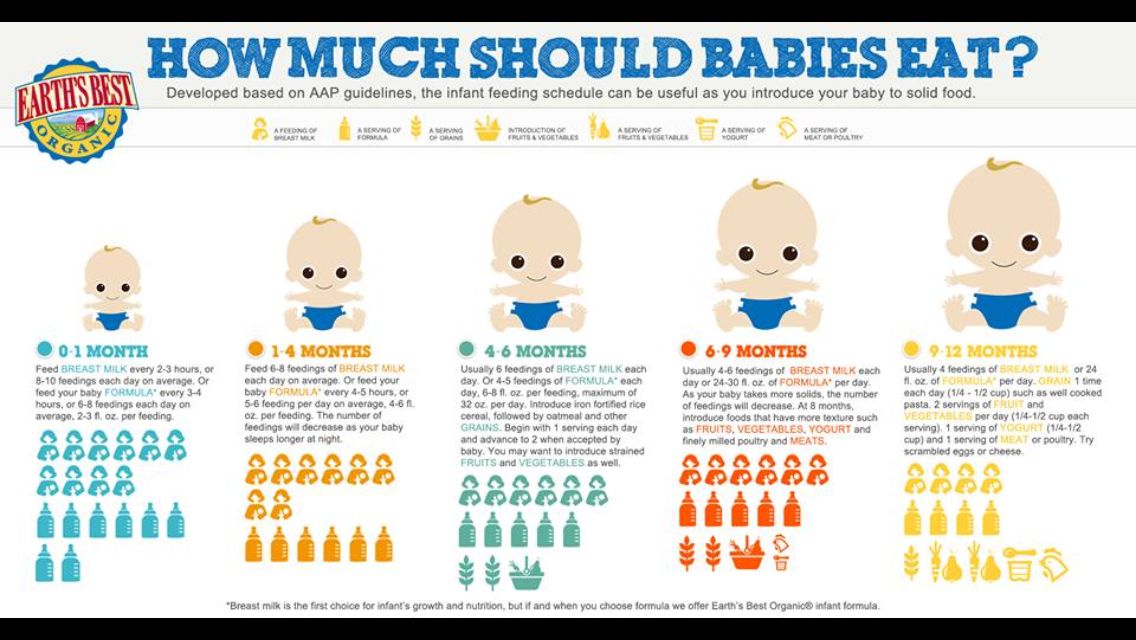 org/diseases-conditions/infant-acid-reflux/diagnosis-treatment/drc-20351412
org/diseases-conditions/infant-acid-reflux/diagnosis-treatment/drc-20351412 - Rosen LD, et al. (2007). Complementary, holistic, and integrative medicine.
pedsinreview.aappublications.org/content/28/10/381 - Saavedra MA, et al. (2003). Infantile colic incidence and associated risk factors: A cohort study. .
ncbi.nlm.nih.gov/pubmed/14502331 - Sung V, et al. (2014). Treating infant colic with the probiotic Lactobacillus reuteri: Double blind, placebo controlled randomised trial. DOI:
10.1136/bmj.g2107 - Symptoms & causes of GER and GERD in infants. (2015).
niddk.nih.gov/health-information/digestive-diseases/acid-reflux-ger-gerd-infants/symptoms-causes
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Oct 3, 2018
Written By
Chaunie Brusie
Edited By
Nizam Khan (TechSpace)
Medically Reviewed By
Karen Richardson Gill, MD
Share this article
Baby Crying After Feeding: What Should You Do?
Did you imagine watching your new bundle of joy gently slip off to sleep in your arms while eating? Is your reality a screaming baby who can’t seem to get comfortable after feedings?
You’re not alone; it happens more frequently than you think. As moms, we’ve dealt with this ourselves. And as medical practitioners, we’ve seen plenty of parents with the same issue.
As moms, we’ve dealt with this ourselves. And as medical practitioners, we’ve seen plenty of parents with the same issue.
There are several reasons your baby might be feeling discomfort after feeding. We’ll look at some of the main causes of why your baby cries after feeding, and we’ll share some proven techniques you can use to make your baby more comfortable and your evenings calmer.
Why Do Babies Cry After Feeding?
If you’re dealing with an inconsolable child after feedings, you may have noticed some of the following symptoms of abdominal discomfort:
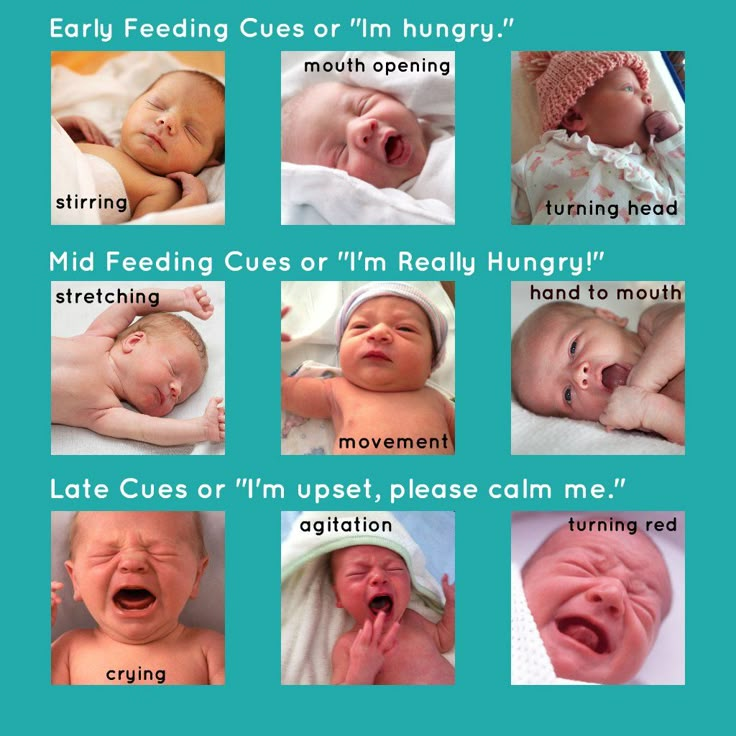
- Crying: Babies seem to experience more discomfort during the evening hours. If you’ve heard the cry before, you know it’s unmistakably a cry of pain. An urgency and intensity suggest it’s more than just complaining.
- Pulling up or extending their legs: Is your baby bringing their knees up to their chest or rigidly extending their legs? They are likely experiencing abdominal pain.
- Distended bellies: Most post-feeding discomfort can be linked to excessive gas in the baby’s system. If it’s trapped in their digestive system, it may lead to a hardened or swollen tummy. Their crying may be exacerbating the discomfort they’re already experiencing.
There are many possible causes of your baby’s discomfort. While this is not an exhaustive list, we’ll talk about some of the main sources of digestive discomfort in young babies.
1. Colic
Perhaps you’ve heard a baby referred to as colicky. Your pediatrician may have even given you the diagnosis. This designation came about after a pediatrician’s study on extremely fussy children and has been around for decades.
Having a colicky baby basically means you have a baby who cries — a lot. You can expect a baby with colic to cry at least three hours a day for at least three days a week (1). Using this definition, nearly a quarter of all infants will experience colic.
The good news is that 50% of babies with colic outgrow the condition by the time they’re three months old. By the time your baby reaches nine months old, there’s a 90% chance they’ll have outgrown the colic.
There’s usually no discernible cause for colic. But it’s clear your baby is uncomfortable. This discomfort is typically linked to the digestive system and follows feedings.
You may need to hold your colicky baby more often and provide lots of comfort. While it can be nerve-wracking and frustrating, having a colicky baby doesn’t mean your baby is unhealthy.
2. Acid Reflux
Also known as gastroesophageal reflux disease (GERD), acid reflux is a common cause of post-feeding discomfort. It can be upsetting to hear your baby is experiencing reflux. But reflux isn’t uncommon; it affects up to 50% of babies during the first few months of life.
If your child is suffering from GERD, there may be additional accompanying symptoms, like difficulty gaining or maintaining weight. Children with GERD frequently spit up and may even experience aggressive vomiting (2).
When your child is experiencing acid reflux, it’s usually because the gastrointestinal system is not working properly. If the difficulty your baby is experiencing is related to an immature digestive system, a child may outgrow GERD. When this happens — as it does for about 95% of children — it usually does so by their first birthday.
There’s also a remote possibility your baby will not outgrow GERD. If this is the case, your doctor can help you create an ongoing treatment plan to support your child’s needs. If you suspect your child has GERD, you should make an appointment with a pediatric gastroenterologist to discuss your concerns.
3.
 Gas
GasAnother common reason babies cry after feeding has to do with gas. Babies’ bodies are still developing their basic skills. A baby who swallows too much air during feedings may not be able to process the extra gas easily.
This leads to pressure and distension and can cause crying and extreme discomfort after meals. It may not be possible to keep your baby from taking in too much air during feedings. However, there are some things you can do to keep air intake to a minimum:
- Frequently burp your baby: Burping can help remove some of the excess air from your baby’s system and leave them feeling more comfortable. To successfully burp your baby, hold them upright, supporting their head well, and pat or rub their back. Some babies seem to burp a lot, while others might have one good burp per feeding.
- Feed in a more upright position: Keep your baby upright for at least 20 to 30 minutes after meals to reduce gas discomfort. If your little one is uncomfortable during sleep, you can also try an inclined mattress, following safe sleep guidelines (3).
- Cycle your baby’s legs: If your baby is visibly uncomfortable, you can lie them on their back and cycle their legs as though they’re riding a bike. This can help push the air through their system and provide them with some relief.
- Try to catch the crying early: It can be tempting to let your baby work through the crying and get to sleep. If it’s likely your child won’t stop, intercept the crying as soon as possible. Crying usually involves gulping air, which will lead to more gas — and more crying.
- Don’t put your baby to sleep directly after a large meal: We all know it’s best for your baby to sleep on their back. But putting a baby down on their back with a full stomach can be a recipe for discomfort. Hold your little one for 20 minutes post-feeding, even if they’re already asleep.
These approaches are great whether you’re nursing or formula feeding. However, there are some specific things you’ll want to look out for, depending on how you feed.
Nursing
- Pay attention to how you eat: What you eat directly impacts your breast milk. Certain foods, including broccoli, beans, and onions, are notoriously difficult for your baby to break down. If you notice gas is especially bad for your baby after you eat a particular type of food, you can limit it in your diet.
- Food sensitivity: Something in your diet may be making your baby fussy. The most common culprits are dairy and caffeine. Usually, there are additional symptoms. Keeping a food journal may help you pinpoint the offending item so you can eliminate it from your diet.
- Nurse your baby in positions that keep their head above their stomach: This will help limit the amount of air intake and encourage digestion.
- Get rid of the excess gas: Plan on burping your baby before switching sides and after feeding.
Bottle Feeding
- Pay attention to the bottle nipple you’re using: If your bottle nipple releases fluid more quickly than your baby can comfortably eat, they will guzzle their meal.
 This leads to an increase in air intake and plenty of gas. Using a slow-flow nipple can help avoid this problem.
This leads to an increase in air intake and plenty of gas. Using a slow-flow nipple can help avoid this problem. - Position your bottle properly: Make sure your bottle is tilted enough to allow the milk to cover the nipple completely. This will help prevent your baby from sucking in the air that’s in the bottle along with their meal.
- Force out the extra air: Expect to burp your baby after every ounce of milk or formula is consumed.
Gas can be highly uncomfortable for your little one. Following these tips will help you mitigate gas and discomfort for your baby.
4. Food Sensitivities
It’s possible that some of your child’s crying after eating is related to an intolerance or allergy.
Everything you consume is passed on to your child in your milk. Some foods — like dairy and eggs — are frequently associated with food sensitivities (4).
If you’re nursing, the best way to determine what’s agitating your child is by charting your food intake. Keep a food journal; you may be surprised at where correlations begin to appear.
Early on, my youngest was inconsolable after the last meal of the day — just when the time came to settle into sleep.
The common link to the discomfort? Spicy food and cheese during my dinner. I cut back on those, and my baby was happier for it.
We were fortunate our baby was only intolerant of these foods and didn’t have a true allergy. Sometimes a young system has difficulty handling certain foods. If your child has a true allergy, you’ll notice more symptoms than abdominal distress.
Be on the lookout for hives, skin rashes, vomiting, diarrhea, difficulty breathing, and any face or tongue swelling (5). If you suspect your child has an allergy, you should consult your pediatrician immediately. And if your little one is struggling with breathing after eating, call 911.
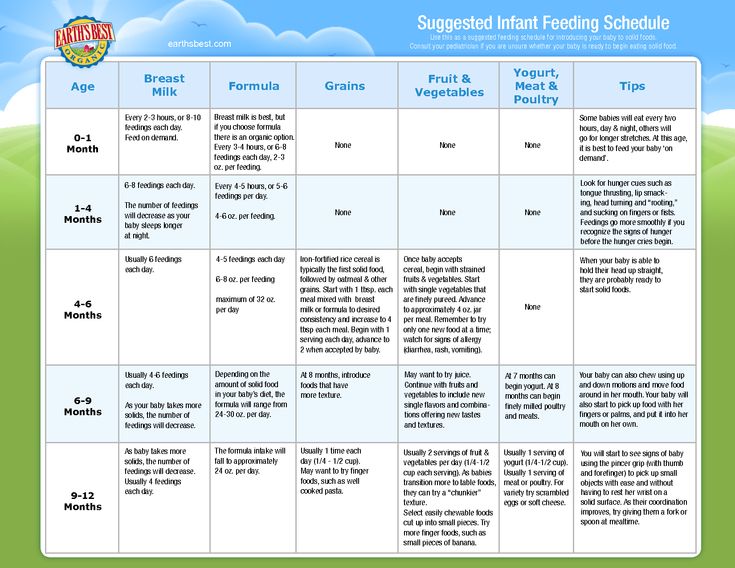
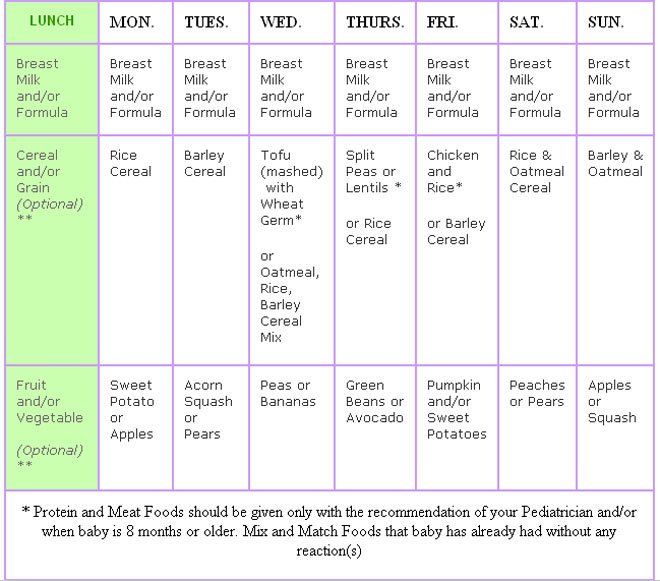
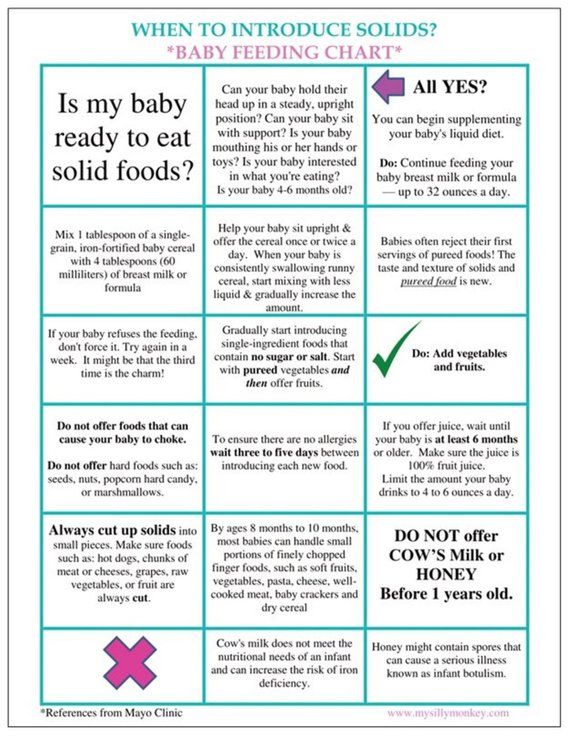
When starting solids, always introduce one new food at a time to your little one to determine what might have caused the response.
Formula feeding your baby? If you notice signs of a food allergy before introducing solid foods, your baby may be allergic to the formula (most commonly the cow’s milk protein). If you think this might be the case, work closely with your pediatrician to determine a suitable alternative formula.
Other Reasons For Crying After Eating
Many causes of post-feeding crying come back to the digestive process. They aren’t the only reasons, though. Some other things may cause your baby to cry.
5. Teething
Most babies will begin teething between 4 and 6 months of age. This doesn’t guarantee the teeth will show up shortly afterward, though. Some babies could go through several months of teething before the teeth break through the gums.
Unfortunately, your child will likely experience inflammation and extreme discomfort in the mouth and gums during this time. This can make even usually benign experiences, like nursing or bottle-feeding, incredibly painful.
If your baby is experiencing teething-related pain, you can help by numbing their gums with cool water before feeding. Just dip your thumb in water and rub directly onto the gums (6). Or let them chew on a washcloth that has been wet and then slightly frozen.
Other pain management approaches can include numbing oral medications and anti-inflammatories (though you’ll want to ask your baby’s doctor before using these). You’ll also want to provide plenty of opportunities for your baby to practice gnawing on things. This can help relieve the pressure, encouraging teeth to break through a little more quickly.
6. Thrush
Babies can experience an overgrowth of yeast in their mouths (7). While Candida, a parasitic fungus, is normally present in your body and in your baby’s mouth, excess yeast can be a problem. It’s extremely uncomfortable and may impact your baby’s ability to eat properly.
It’s extremely uncomfortable and may impact your baby’s ability to eat properly.
Excess amounts of yeast frequently happen after a course of antibiotics. Antibiotics will kill off the bad bacteria, but they don’t discriminate. This means they may also kill off good bacteria, leaving an imbalance that can lead to thrush.
Thrush is usually a visible condition. If you suspect your baby has thrush, look inside their mouth. If thrush is present, you’ll see filmy white patches that may look like milk. If the patch doesn’t come away with a swipe from your finger, you’re looking at thrush.
If your baby has thrush, make an appointment with your pediatrician. A simple course of prescription antifungal medication will help clean up the condition.
Yeast is quite persistent. If you’re dealing with thrush, plan on sterilizing every plastic nipple or pacifier you own to prevent recontamination. Nursing? You’ll need to be treated for thrush as well — or you will simply pass the infection back and forth between you and your baby.
Feedback: Was This Article Helpful?
Thank You For Your Feedback!
Thank You For Your Feedback!
What Did You Like?
What Went Wrong?
Why does a baby cry - an article in the newspaper of the EMS clinic "On Health"
— The simplest answer to the question about sedatives is definitely: no. Parents should not use painkillers, sedatives, herbal “bye-bye”-fees and other means to calm the baby. In any case, until it was recommended by a neurologist after a comprehensive examination. Giving a sedative to an infant is like hiding your head under a pillow when the alarm goes off: it won't stop time and you'll be late for work anyway. You need to try to understand your baby, make sure that his most basic needs are met, and only then proceed to the exclusion of more complex and rare problems.
Try to remain calm and act only in the interests of the child
Up to three weeks of age, the most common cause of constant crying of a child is banal malnutrition.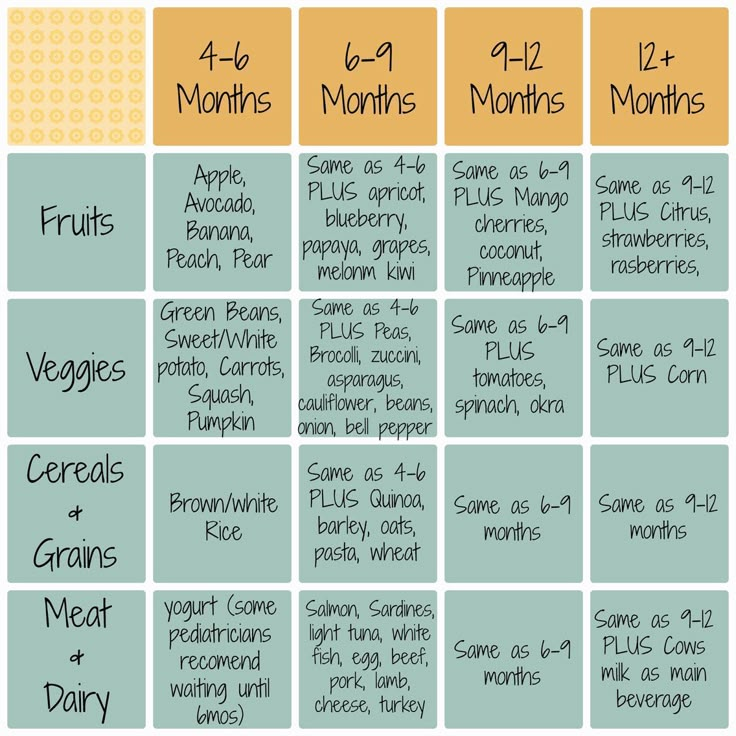 A common mistake of parents is the desire to stick to the schedule when breastfeeding in the first month of a child's life. A baby can suck out 150 ml of milk in three minutes, or maybe 20 ml in an hour, and a nursing mother is not able to understand how much has been eaten by the sensations of "emptying the breast". With free feeding in the first month, record the dynamics of the baby's weight gain. When feeding on a schedule, conduct a series of control feedings with measurement of body weight before and after feeding, so you can make sure that the amount of one feeding is sufficient. If the baby's crying stops instantly as soon as you give the breast, this is absolutely normal.
A common mistake of parents is the desire to stick to the schedule when breastfeeding in the first month of a child's life. A baby can suck out 150 ml of milk in three minutes, or maybe 20 ml in an hour, and a nursing mother is not able to understand how much has been eaten by the sensations of "emptying the breast". With free feeding in the first month, record the dynamics of the baby's weight gain. When feeding on a schedule, conduct a series of control feedings with measurement of body weight before and after feeding, so you can make sure that the amount of one feeding is sufficient. If the baby's crying stops instantly as soon as you give the breast, this is absolutely normal.
What to do if the baby cries even after you have changed the diaper, tried to feed, picked up? If this happens often and the mother does not succeed in calming the child for more than an hour, you should consult a doctor. It is not always obvious to parents, especially good ones, in what order to seek medical help: should I call an ambulance or go to see my pediatrician in a couple of days, or maybe it’s better to grab the child and the CHI policy and rush to the nearest city hospital? Try to remain calm and act only in the interests of the child. Here are some tips to help you.
Here are some tips to help you.
- If the baby cries and cannot be calmed for more than two hours, call emergency services. Pre-measure the baby's temperature, check for rashes on the baby's body, and remember if there was a stool within the last 12 hours. Also make sure you have enough breast milk for a single feed. Report this information to the emergency services
- If a child often worries , sleep is short, but there is no monotonous crying-crying for more than two hours, then this can be dealt with on your own, and then with the help of a doctor at a clinic appointment or by calling him at home. The better prepared you are for your consultation, the more productive it will be. Things to do before the consultation:
- Determine breastfeeding volume by three to four checkweighs before and after feeding
- See if there is a connection between baby crying and feeding. When does the child worry and cry - immediately after eating, during feeding, an hour later, etc.
 ?
? - Recall the circumstances in which anxiety and frequent crying appeared: vaccination, errors in the mother's diet, starting to use or changing formula?
- Note accompanying symptoms and their relationship to crying: regurgitation, constipation, frequent stools, flatulence, appearance or increase of skin rash
- Assess the change in stool frequency and consistency
- Observe whether restlessness and crying persist after passing stool or flatulence
- Find out if there is an effect when placing a gas tube or a glycerin suppository.
The task of a pediatrician when complaining of frequent and prolonged crying of a child is to determine why the child is crying, whether he has any disorders (including digestive disorders) and what kind they are - functional, that is, this is a conditionally normal condition associated with the growth and development of the body or a reaction to changes in external (primarily nutritional) factors, or it is a pathology that must be suspected, diagnosed and treated.
Three types of crying
Experts say that babies have three types of crying:
- Basic . This is, in fact, a means of communication between the child and others. This cry is intermittent, smooth, the sounds are not sharp.
- Angry . This is how babies cry when they really don't like something or they really want something. In this case, parents may notice how the child's facial expressions change. He roars loudly, confidently, mostly on the exhale. Angry crying is usually the longest.
- Painful . With his help, the baby reports that he is in pain. At the same time, he screams to a screech, with piercing notes until he exhales completely.
Colic - they pass! - articles from the specialists of the clinic "Mother and Child"
You can't confuse anything with anything
A healthy child was discharged from the maternity hospital, he grows and pleases his loved ones. Yes, the baby sometimes cries a little, but what children do not cry! Moreover, over time, mom and dad get used to their new role and gradually understand what their baby needs. Yes, and the reasons for crying are usually simple: the child wants to sleep or, conversely, to communicate, he is cold or hot, in the end, he most often just needs to eat! Later, when colic begins, that crying of the first days and weeks of life will seem to parents only a slight irritation or whims. But mom and dad don’t know this yet and just rejoice at how their son or daughter is gaining weight and gaining strength. And suddenly out of the blue it starts! Usually in the afternoon, a child who was completely calm before that first frowns, wriggles, twists his mouth, grunts, then such a cry is heard that at the first moment especially tremulous parents clutch at their hearts. The baby presses the legs to the stomach, and often beats the air with his hands, his face turns red from crying, and his stomach tenses.
Yes, the baby sometimes cries a little, but what children do not cry! Moreover, over time, mom and dad get used to their new role and gradually understand what their baby needs. Yes, and the reasons for crying are usually simple: the child wants to sleep or, conversely, to communicate, he is cold or hot, in the end, he most often just needs to eat! Later, when colic begins, that crying of the first days and weeks of life will seem to parents only a slight irritation or whims. But mom and dad don’t know this yet and just rejoice at how their son or daughter is gaining weight and gaining strength. And suddenly out of the blue it starts! Usually in the afternoon, a child who was completely calm before that first frowns, wriggles, twists his mouth, grunts, then such a cry is heard that at the first moment especially tremulous parents clutch at their hearts. The baby presses the legs to the stomach, and often beats the air with his hands, his face turns red from crying, and his stomach tenses. And suddenly the child stops. Gone? No, almost immediately everything repeats again. And so at least half an hour in a row, and as a maximum - several hours a day. In the end, the child's strength ends and he falls asleep in exhaustion. Exhausted parents, too. The next day everything starts all over again.
And suddenly the child stops. Gone? No, almost immediately everything repeats again. And so at least half an hour in a row, and as a maximum - several hours a day. In the end, the child's strength ends and he falls asleep in exhaustion. Exhausted parents, too. The next day everything starts all over again.
If you are very lucky, then such attacks will last only one or two times per evening for 30 minutes - 1 hour. On average, the attack lasts up to 3 hours. But there is a worse option: every day the strength, duration and frequency of screams will increase, until in the end the child starts screaming every two hours in the morning, and in the afternoon, and in the evening, and at night, of course. It will seem to parents that now this one is forever, but by 3 months babies are miraculously healed, only a few have colic that lasts up to 4-5 months (it’s good that they are already much less pronounced). That's what they are, infantile colic! Well, from the point of view of doctors, colic is just paroxysmal pain in the abdomen, accompanied by severe anxiety of the child.
Many years ago it was noticed that there is a certain regularity in the manifestation of colic, the so-called "rule of three" :
- Colic often begins by three weeks of life - yes, this is almost always the case.
- Lasts an average of about three hours a day - unfortunately, this is only an average.
- Usually found in children of the first three months of life - fortunately, this is true.
There is also a positive moment in colic : usually the general condition of the child does not worsen with intestinal colic: the child has a good appetite, he gains weight properly, in the intervals between bouts of colic the baby is cheerful and looks as if nothing had happened. Against the backdrop of an endless ora, parents are already happy with every little thing. And since there are no other symptoms other than crying, then colic is not considered a disease. Doctors call them a functional disorder in the work of the gastrointestinal tract (this means that there is no structural disturbance in it, it’s just that the digestive system is not yet working quite correctly).
Have you read this far and become a little scary?
The best news: not all children have colic! There are lucky ones who only shrug their shoulders in surprise when asked if their child had colic.
The reason is not established
There is another interesting feature of colic: it is difficult to determine exactly why colic occurs. There are many reasons for this, and each baby can have his own:
- Enzymatic system of the gastrointestinal tract is not yet mature. Therefore, the food is not fully digested and too much gas is formed in the intestines, the gases stretch the walls of the intestine, hence the pain.
- The intestinal microflora is not yet fully established and changes frequently, again leading to excess gas and pain.
- The neuromuscular apparatus of the intestine is also not fully mature. As a result, intestinal motility and spasms increase.
- The baby swallows too much air during feeding (it is incorrectly attached to the breast or sucks too greedily).
 Air stretches the walls of the intestines, which is also painful for many children.
Air stretches the walls of the intestines, which is also painful for many children. - Mom is breastfeeding and eating a lot of dairy products, and the baby is allergic to cow's milk protein. As a result of this allergy, the intestinal wall is damaged. Secondary lactase deficiency occurs, the child lacks the enzyme lactase, which breaks down milk sugar. Sugar ferments in the intestines, there are more and more gases and, as a result, pain occurs.
- The baby has an increased sensitivity of the intestinal wall to stretching. The child feels pain that another infant (or adult) will not pay attention to.
- If the baby is bottle-fed, then the whole thing may be in the mixture. Most likely, it is not suitable for a child.
Well, if the cause of colic is some one and not very serious. For example, a baby swallows a lot of air during feeding. Then the colic will not be too pronounced. In addition, it is not difficult to eliminate this cause, you just need to adjust the feeding.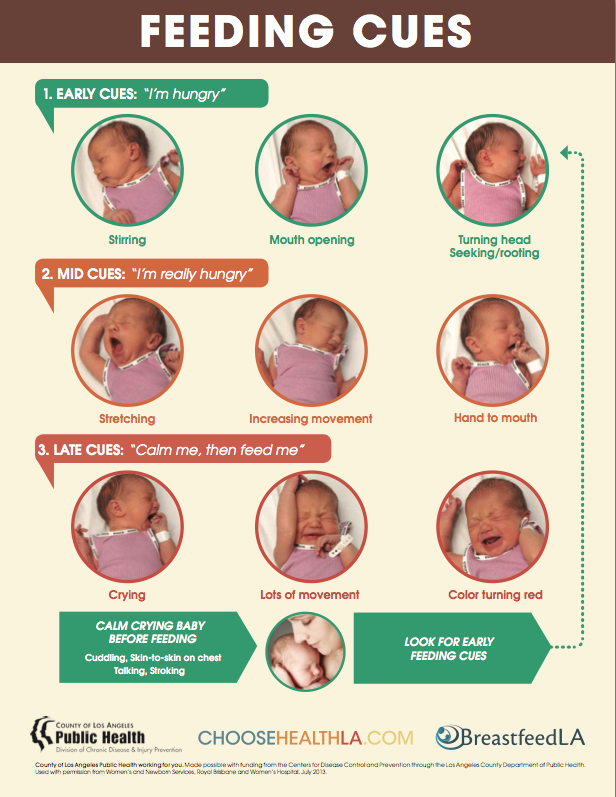 As a rule, colic is quite tolerable as long as the child has functional immaturity of the gastrointestinal tract (for example, the microflora has not been established or there are few enzymes). The baby cries in the evening, even if for three hours, but 21 hours out of 24 he is quite calm. In the end, when every evening (or three or four times a week) the same scenario is repeated, you already get used to it.
As a rule, colic is quite tolerable as long as the child has functional immaturity of the gastrointestinal tract (for example, the microflora has not been established or there are few enzymes). The baby cries in the evening, even if for three hours, but 21 hours out of 24 he is quite calm. In the end, when every evening (or three or four times a week) the same scenario is repeated, you already get used to it.
But if there are several causes of colic at once or there is an allergy to cow's milk protein with lactase deficiency, then parents will fully feel what it is like when a child throws a tantrum every two hours.
To make it easier for the pediatrician to figure out what is likely to cause colic, parents should tell them as much as possible about their child. To do this, will have to keep a diary of colic and nutrition of the baby . By the way, some mothers are so addicted to these records that they continue to keep them even when the colic has already passed (just in case). Well, then they get used to the fact that there are no more colic, and calm down.
Well, then they get used to the fact that there are no more colic, and calm down.
What should be recorded in the food diary:
- When does colic occur: before, during or after feeding, if after feeding, after what time.
- How long does colic last.
- Is there any rhythm in colic, do they occur at the same time or at different times.
- When colic is most pronounced (morning, afternoon, evening).
- How a mother feeds a child - breastfeeding or formula. If breastfeeding, then how many milliliters the baby eats in one feeding. Breastfeeding by the hour or free.
- If the child is receiving formula, what kind, dosage and how often.
- What does a mother eat if she is breastfeeding.
What to do about it
Is it necessary to somehow examine a child with colic? Even if the doctor says that the baby has the most common colic, parents will still want to take a lot of tests and ultrasound of the abdominal cavity.
And it is clear that the more a child cries, the more mom and dad want to examine him .
Ultrasound usually shows that everything is in order with the structure of the child's internal organs (immaturity and allergy are not visible on ultrasound). But parents even from this are already calmer. In coprology (fecal analysis), some changes are possible, and in the analysis of feces for carbohydrates (it confirms lactase deficiency), carbohydrates will be increased. Microbiological examination of feces (sowing) does not bring clarity to the picture of colic. The composition of the microflora, and so on, may not yet be fully established, and against the background of increased gas formation, in addition, it will be changed.
So what to do now? As already mentioned, colic disappears with age. Someone will say that you just need to be patient and wait. This, of course, is true, but when the baby cries and screams all the time, it affects the nervous system of everyone around. The situation in the house becomes nervous, the parents calm the baby with their last strength, and the mother also needs to feed the child, and walk with him, and cook food. Dad is also exhausted by endless screams and night vigils, and he is the breadwinner in the family, plus, if driving, he must concentrate on the road. In general, everyone needs rest, which means that colic needs to be dealt with somehow.
The situation in the house becomes nervous, the parents calm the baby with their last strength, and the mother also needs to feed the child, and walk with him, and cook food. Dad is also exhausted by endless screams and night vigils, and he is the breadwinner in the family, plus, if driving, he must concentrate on the road. In general, everyone needs rest, which means that colic needs to be dealt with somehow.
Let's say right away that there is no 100% effective treatment for colic: although many ways have been invented to deal with them.
Someone helps one thing, someone else - you have to try almost all methods:
Proper feeding . If the mother is breastfeeding on demand, then feeding should not become erratic, especially if colic is aggravated during meals or immediately after it. The baby should not swallow air during feeding, so you need to make sure that he completely captures the areola. If the baby is bottle-fed, then the nipple should be age-appropriate (the hole for milk in it should not be very large). You can use special anti-colic bottles - they prevent the swallowing of air during feeding. Before feeding the baby, you can put it on your stomach for 10-15 minutes, this stimulates the intestines. After feeding, the child must be held upright so that he burps the air. But for some reason, colic often occurs even if all these rules are observed.
You can use special anti-colic bottles - they prevent the swallowing of air during feeding. Before feeding the baby, you can put it on your stomach for 10-15 minutes, this stimulates the intestines. After feeding, the child must be held upright so that he burps the air. But for some reason, colic often occurs even if all these rules are observed.
Heat and massage . For some children, colic is relieved (or relieved) by putting something warm on their stomach or simply taking a warm bath. Someone helps just a diaper folded several times and ironed with an iron. But caring fathers wear someone for hours, attaching to their chest, or simply put the baby on their stomach, but, alas, there is no effect. The same thing happens if you give the baby a light massage of the abdomen in a clockwise direction: it will not help, you can only guess.
Mother's food . Pediatricians often recommend that mom exclude any dairy and sour-milk products (milk, cheese, cottage cheese, yogurt, kefir, ice cream) from her diet. Under the ban are products that, even partially, contain milk: for example, cookies, pastries. Well, women are no strangers to diets, especially since with severe colic in the crumbs, the mother will already agree to everything. Usually after 7-10 days you can see if the diet helps or not. If there are results, then it is most likely that the child is allergic to cow's milk protein and the mother will have to stay on a dairy-free diet for some more time.
Under the ban are products that, even partially, contain milk: for example, cookies, pastries. Well, women are no strangers to diets, especially since with severe colic in the crumbs, the mother will already agree to everything. Usually after 7-10 days you can see if the diet helps or not. If there are results, then it is most likely that the child is allergic to cow's milk protein and the mother will have to stay on a dairy-free diet for some more time.
Children's herbal teas and remedies with chamomile, fennel (they relieve intestinal spasm and improve flatulence) - again, the result is the opposite. But it is better not to give them yourself. Herbs can also be allergic, which will only increase colic. What remedy is better to give (or not to give anything at all), the pediatrician will decide.
Drugs that destroy the walls of the gas bubble . Here, as with other methods, the effect is often temporary and not 100%. After all, these funds only relieve the symptoms, and the cause of gas formation remains.
Enzymes for lactase deficiency . If it is confirmed, then enzymes (lactase) help well. The main thing is that the cause of colic is established correctly.
Motion sickness, wheelchairs and driving . They always rocked children, but it’s just necessary to pump, and not shake the child like a pear. Violent shaking can cause a concussion.
Unconventional products . It sounds strange, of course, but some parents claim that the sound of a vacuum cleaner or a hair dryer calms a screaming baby well.
Another way is to sleep in the fresh air. There are such amazing babies who, for some reason, calm down perfectly in the fresh air in the evening, but as soon as their mother tries to return home, they instantly wake up and raise a cry. As soon as evening colic begins, mothers grab the child, the stroller - and run into the street. And it’s not at all about riding in a stroller: the baby sleeps even if she just stands still. This is how mothers sit at the entrance until midnight.