4 week old baby throwing up after every feed
Why This Happens and What to Do
It can be difficult to tell the difference between vomit and spit-up. Both might look the same since your baby is currently on a steady of diet of milk or formula. The main difference is in how they come out.
Spit-up usually happens before or after a burp and is most common in babies under the age of 1 year. Spit-up will easily flow from your baby’s mouth — almost like white, milky drool.
Vomit typically comes out forcefully (whether you’re a baby or an adult). This is because vomiting happens when the muscles around the stomach are triggered by the brain’s “vomiting center” to squeeze it. This forces whatever is in the stomach to be hurled out.
In a baby’s case, vomit may look like milky spit-up but have more clear stomach juices mixed into it. It may also look like milk that has been fermented for a little while — this is called “cheesing.” Yes, it sounds gross. But the texture probably won’t bother you when you see it — you’ll be more concerned with baby’s well-being.
Your baby may also cough or make little retching noises before they vomit. This is likely the only warning you’ll have to grab a towel, bucket, burp cloth, sweater, your shoe — hey, anything.
Additionally, spit-up is normal and can happen at any time. Your baby will only vomit if there’s a digestive issue or they have another illness.
Feeding difficulty
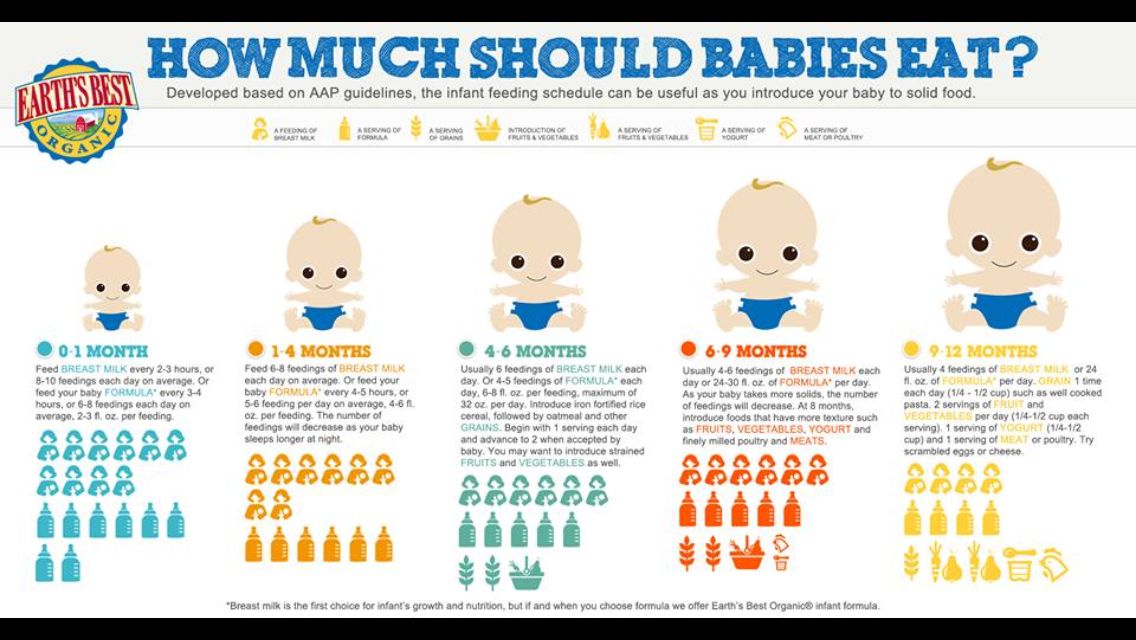
Babies have to learn everything from scratch, including how to feed and keep the milk down. Along with spit-up, your baby may vomit occasionally after being fed. This is most common in the first month of life.
It happens because your baby’s tummy is still getting used to digesting food. They also have to learn to not gulp milk down too fast or overfeed.
Post-feeding vomiting typically stops after the first month. Give your baby more frequent, smaller feeds to help stop the vomit.
But let your pediatrician know if your baby vomits often or has very forceful vomits. In some cases, it might be a sign of something other than feeding difficulty.
Stomach flu
Also known as the tummy bug or “stomach flu,” gastroenteritis is a common cause of vomiting in babies and children. Your baby may have cycles of vomiting that come and go for about 24 hours.
Other symptoms in babies may last for 4 days or longer:
- watery, runny poop or mild diarrhea
- irritability or crying
- poor appetite
- stomach cramps and pain
The tummy bug can also cause a fever, but this is actually less common in babies.
Gastroenteritis usually looks a lot worse than it is (thank goodness!). It’s typically caused by a virus that goes away by itself in about a week.
In babies, severe gastroenteritis can lead to dehydration. Call your pediatrician immediately if your baby has any signs of dehydration:
- dry skin, mouth, or eyes
- unusual sleepiness
- no wet diapers for 8 to 12 hours
- weak cry
- crying without tears
Infant reflux
In some ways, babies really are like tiny adults. Just like adults of any age can have acid reflux or GERD, some babies have infant reflux. This can lead to baby vomiting in the first weeks or months of your baby’s life.
Just like adults of any age can have acid reflux or GERD, some babies have infant reflux. This can lead to baby vomiting in the first weeks or months of your baby’s life.
Vomiting from acid reflux happens when the muscles at the top of the stomach are too relaxed. This triggers baby vomiting shortly after feeding.
In most cases, the stomach muscles strengthen, and your baby’s vomiting goes away on its own. Meanwhile, you can help slow down the vomiting by:
- avoiding overfeeding
- giving smaller, more frequent feeds
- burping your baby often
- propping your baby up in an upright position for about 30 minutes after feeding
You can also thicken milk or formula with more formula or a bit of baby cereal. Caveat: Check with your pediatrician before you try this. It might not be suitable for all babies.
Cold and flu
Babies catch colds and flus easily because they have shiny new immune systems that are still developing. It doesn’t help if they’re in day care with other sniffling kiddos, or they’re around adults that can’t resist kissing their little faces. Your baby may have up to seven colds in their first year alone.
Your baby may have up to seven colds in their first year alone.
Cold and flu can cause different symptoms in babies. Along with a runny nose, your baby may also have vomiting without a fever.
Too much mucus in the nose (congestion) can lead to a nasal drip in the throat. This can trigger bouts of forceful coughing that sometimes cause vomiting in babies and children.
As in adults, colds and flu in babies are viral and go away after about a week. In some cases, sinus congestion may turn into an infection. Your baby will need antibiotics to treat any bacterial — not viral — infection.
Ear infection
Ear infections are another common illness in babies and children. This is because their ear tubes are horizontal rather than more vertical like in adults.
If your little one has an ear infection, they might have nausea and vomiting without a fever. This happens because an ear infection can cause dizziness and loss of balance. Other symptoms of ear infections in babies include:
- pain in one or both ears
- tugging or scratching at or near the ears
- muffled hearing
- diarrhea
Most ear infections in babies and children go away without treatment. However, it’s important to see a pediatrician in case your baby needs antibiotics to clear up the infection. In rare cases, a serious ear infection can damage a baby’s tender ears.
However, it’s important to see a pediatrician in case your baby needs antibiotics to clear up the infection. In rare cases, a serious ear infection can damage a baby’s tender ears.
Overheating
Before you swaddle your baby or put them in that adorable fluffy bunny suit, check the temperature outside and in your home.
While it’s true that the womb was warm and cozy, babies can overheat quickly in hot weather or in a very warm house or car. This is because their tiny bodies are less able to sweat out heat. Overheating might cause vomiting and dehydration.
Overheating can lead to heat exhaustion or in much more serious cases, heatstroke. Look for other symptoms like:
- pale, clammy skin
- irritability and crying
- sleepiness or floppiness
Immediately remove clothing and keep your baby out of the sun and away from heat. Try to breastfeed (or give your baby water if they’re 6 months or older). Get urgent medical attention if your baby doesn’t seem their usual self.
Motion sickness
Babies below the age of 2 years don’t commonly get motion or car sickness, but some babies may get sick after a car ride or being twirled around — especially if they’ve just eaten.
Motion sickness can make your baby dizzy and nauseous, leading to vomiting. It might be more likely to happen if your baby already has an upset tummy from bloating, gas, or constipation.
Strong smells and windy or bumpy roads can also make your baby dizzy. Nausea triggers more saliva, so you might notice more dribble before your baby vomits.
You can help prevent motion sickness by traveling when your baby is ready to sleep. (Great trick if your baby loves to sleep in the car!) A sleeping baby is less likely to feel queasy.
Keep their head well supported in the car seat so it doesn’t move around too much. Also, avoid going for a drive right after giving your baby a full feed — you want your baby to digest the milk, not wear it.
Milk intolerance
A rare kind of milk intolerance is called galactosemia. It happens when babies are born without a certain enzyme needed to break down sugars in milk. Some babies with this condition are even sensitive to breast milk.
It happens when babies are born without a certain enzyme needed to break down sugars in milk. Some babies with this condition are even sensitive to breast milk.
It can cause nausea and vomiting after drinking milk or any kind of dairy products. Galactosemia can also cause a skin rash or itching in both babies and adults.
If your baby is formula fed, check the ingredients for any dairy, including milk proteins.
Most newborns are screened at birth for this rare condition and other illnesses. This is usually done with a heel prick blood test or a urine test.
In the rare event that your baby has this, you’ll know it very early on. Make sure your baby completely avoids milk to help stop vomiting and other symptoms.
Pyloric stenosis
Pyloric stenosis is a rare condition that happens when the opening between the stomach and intestines is blocked or too narrow. It can lead to forceful vomiting after feeding.
If your baby has pyloric stenosis, they may be hungry all the time. Other symptoms include:
Other symptoms include:
- dehydration
- weight loss
- wave-like stomach contractions
- constipation
- fewer bowel movements
- fewer wet diapers
This rare condition can be treated with surgery. Tell your pediatrician immediately if your baby has any of the symptoms of pyloric stenosis.
Intussusception
Intussusception is a rare intestinal condition. It affects 1 in every 1,200 babies and most commonly happens at the age of 3 months or older. Intussusception can cause vomiting without a fever.
This condition happens when the intestines are damaged by a virus or other health conditions. The damaged intestine slips — “telescopes” — into another part of the intestine.
Along with vomiting, a baby may have severe stomach cramps that last for about 15 minutes. The pain can cause some babies to curl their knees up to their chest.
Other symptoms of this intestinal condition include:
- fatigue and tiredness
- nausea
- blood or mucus in bowel movements
If your baby has intussusception, treatment can push the intestine back into place. This gets rid of vomiting, pain, and other symptoms. Treatment includes using air in the intestines to gently move the intestines. If that doesn’t work, keyhole (laparoscopic) surgery heals this condition.
This gets rid of vomiting, pain, and other symptoms. Treatment includes using air in the intestines to gently move the intestines. If that doesn’t work, keyhole (laparoscopic) surgery heals this condition.
See your baby’s pediatrician if your baby has vomiting for longer than 12 hours. Babies can get dehydrated quickly if they’re vomiting.
Get immediate medical attention if your baby is vomiting and has other symptoms and signs like:
- diarrhea
- pain or discomfort
- constant or forceful coughing
- hasn’t had a wet diaper for 3 to 6 hours
- refusing to feed
- dry lips or tongue
- few or no tears when crying
- extra tired or sleepy
- weakness or floppy
- won’t smile
- swollen or bloated stomach
- blood in diarrhea
Baby vomiting without a fever can happen because of several common illnesses. Your baby will likely have one or more of these several times in the first year. Most of these causes go away on their own, and your little one will stop vomiting without any treatment.
But too much vomiting can lead to dehydration. Check for signs of dehydration and call your pediatrician if you’re not sure.
Some causes of baby vomiting are more serious, but these are rare. Your baby will need medical care for these health conditions. Know the signs and remember to keep the doctor’s number saved in your phone — and take a deep breath. You and baby got this.
Vomiting (0-12 Months)
Is this your child's symptom?
- Vomiting (throwing up) stomach contents
- Other names for vomiting are puking, barfing and heaving
Causes of Vomiting
- Viral Gastritis. Stomach infection from a stomach virus is the most common cause. Also called stomach flu. A common cause is the Rotavirus. The illness starts with vomiting. Watery loose stools may follow within 12-24 hours.
- Food Allergy. Vomiting can be the only symptom of a food reaction. The vomiting comes on quickly after eating the food.
 Uncommon in infants, but main foods are eggs and peanut butter.
Uncommon in infants, but main foods are eggs and peanut butter. - Coughing. Hard coughing can also cause your child to throw up. This is more common in children with reflux.
- Serious Causes. Vomiting alone should stop within about 24 hours. If it lasts over 24 hours, you must think about more serious causes. An example is a kidney infection. A serious cause in young babies is pyloric stenosis. See below for more on this.
Pyloric Stenosis (Serious Cause)
- The most common cause of true vomiting in young babies.
- Onset of vomiting is age 2 weeks to 2 months
- Vomiting is forceful. It becomes projectile and shoots out.
- Right after vomiting, the baby is hungry and wants to feed. ("hungry vomiter")
- Cause: The pylorus is the channel between the stomach and the gut. In these babies, it becomes narrow and tight.
- Risk: Weight loss or dehydration
- Treatment: Cured by surgery.
Vomiting Scale
- Mild: 1 - 2 times/day
- Moderate: 3 - 7 times/day
- Severe: Vomits everything, nearly everything or 8 or more times/day
- Severity relates even more to how long the vomiting goes on for. At the start of the illness, it's common for a child to vomit everything. This can last for 3 or 4 hours. Children then often become stable and change to mild vomiting.
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much fluid.
- The younger the child, the greater the risk for dehydration.
Dehydration: How to Tell
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much water.
- Vomiting with watery diarrhea is the most common cause of dehydration.
- Dehydration is a reason to see a doctor right away.
- Your child may have dehydration if not drinking much fluid and:
- The urine is dark yellow and has not passed any in over 8 hours.

- Inside of the mouth and tongue are very dry.
- No tears if your child cries.
- Slow blood refill test: Longer than 2 seconds. First, press on the thumbnail and make it pale. Then let go. Count the seconds it takes for the nail to turn pink again. Ask your doctor to teach you how to do this test.
When to Call for Vomiting (0-12 Months)
Call 911 Now
- Can't wake up
- Not moving
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Dehydration suspected. No urine in over 8 hours, dark urine, very dry mouth and no tears.
- Stomach pain when not vomiting. Exception: stomach pain or crying just before vomiting is quite common.
- Age less than 12 weeks old with vomiting 2 or more times. Exception: normal spitting up.
- Vomited 3 or more times and also has diarrhea
- Severe vomiting (vomits everything) more than 8 hours while getting Pedialyte (or breastmilk)
- Head injury within the last 24 hours
- Weak immune system.
 Examples are sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
Examples are sickle cell disease, HIV, cancer, organ transplant, taking oral steroids. - Vomiting a prescription medicine
- Fever over 104° F (40° C)
- Fever in baby less than 12 weeks old. Caution: Do NOT give your baby any fever medicine before being seen.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- All other infants (age less than 1 year) with vomiting. See Care Advice while waiting to discuss with doctor.
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Care Advice for Vomiting
- What You Should Know About Vomiting:
- Most vomiting is caused by a viral infection of the stomach.

- Vomiting is the body's way of protecting the lower gut.
- The good news is that stomach illnesses last only a short time.
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much fluid.
- Here is some care advice that should help.
- Most vomiting is caused by a viral infection of the stomach.
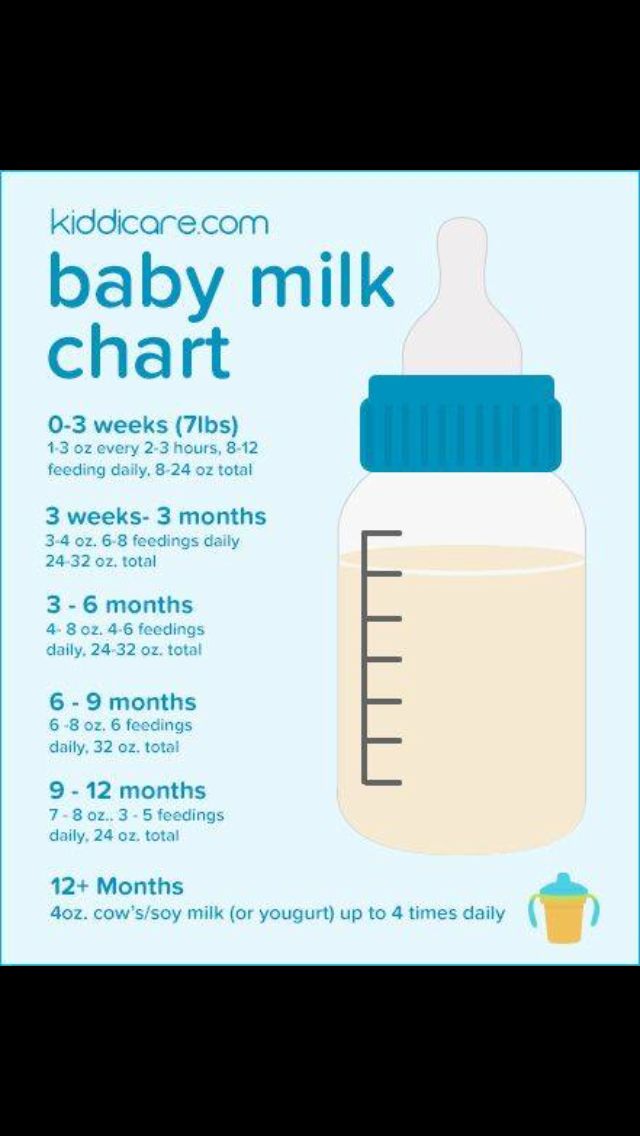
- Formula Fed Babies - May Give Oral Rehydration Solution (ORS) for 8 Hours:
- If vomits once, give half the regular amount of formula every 1 to 2 hours.
- If vomits formula more than once, offer ORS for 8 hours. If you don't have ORS, use formula until you can get some.
- ORS is a special fluid that can help your child stay hydrated. You can use Pedialyte or the store brand of ORS. It can be bought in food stores or drug stores.
- Spoon or syringe feed small amounts. Give 1-2 teaspoons (5-10 mL) every 5 minutes.
- After 4 hours without throwing up, double the amount.
- Return to Formula. After 8 hours without throwing up, go back to regular formula.

- Breastfed Babies - Reduce the Amount Per Feeding:
- If vomits once, nurse half the regular time every 1 to 2 hours.
- If vomits more than once, nurse for 5 minutes every 30 to 60 minutes. After 4 hours without throwing up, return to regular nursing.
- If continues to vomit, switch to pumped breastmilk. (ORS is rarely needed in breastfed babies. It can be used if vomiting becomes worse).
- Spoon or syringe feed small amounts of pumped milk. Give 1-2 teaspoons (5-10 mL) every 5 minutes.
- After 4 hours without throwing up, return to regular feeding at the breast. Start with small feedings of 5 minutes every 30 minutes. As your baby keeps down the smaller amounts, slowly give more.
- Pumped Breastmilk Bottle-Fed Infants - Reduce the Amount per Feeding:
- If vomits once and bottle-feeding breastmilk, give half the regular amount every 1-2 hours.
- If vomits more than once within last 2 hours, give 1 ounce (30 mL) every 30 to 60 minutes.

- If continues to vomit, give 1-2 teaspoons (5-10 mL) every 5 minutes. Only if not tolerating breastmilk, switch to ORS (e.g., Pedialyte) for every 5 minutes for a few hours.
- After 4 hours without vomiting, return to regular feedings. Start with 1 ounce (30 mL) every 30 minutes and slowly increase as tolerated.
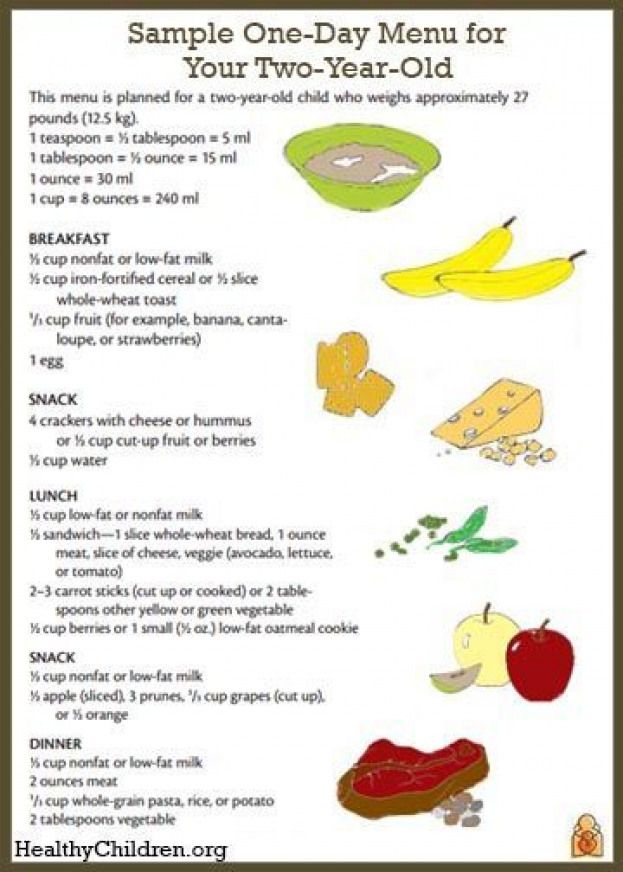
- Stop All Solid Foods:
- Avoid all solid foods and baby foods in kids who are vomiting.
- After 8 hours without throwing up, gradually add them back.
- If on solid foods, start with starchy foods that are easy to digest. Examples are cereals, crackers and bread.
- Do Not Give Medicines:
- Stop using any drug that is over-the-counter for 8 hours. Reason: Some of these can make vomiting worse.
- Fever. Mild fevers don't need to be treated with any drugs. For higher fevers, you can use an acetaminophen suppository (such as FeverAll). This is a form of the drug you put in the rectum (bottom).
 Ask a pharmacist for help finding this product. Do not use ibuprofen. It can upset the stomach.
Ask a pharmacist for help finding this product. Do not use ibuprofen. It can upset the stomach. - Call your doctor if: Your child vomits a drug ordered by your doctor.
- Try to Sleep:
- Help your child go to sleep for a few hours.
- Reason: Sleep often empties the stomach and removes the need to vomit.
- Your child doesn't have to drink anything if his stomach feels upset and he doesn't have any diarrhea.
- Return to Child Care:
- Your child can return to child care after the vomiting and fever are gone.
- What to Expect:
- For the first 3 or 4 hours, your child may vomit everything. Then the stomach settles down.
- Vomiting from a viral illness often stops in 12 to 24 hours.
- Mild vomiting and nausea may last up to 3 days.
- Call Your Doctor If:
- Vomits clear fluids for more than 8 hours
- Vomiting lasts more than 24 hours
- Blood or bile (green color) in the vomit
- Stomach ache present when not vomiting
- Dehydration suspected (no urine in over 8 hours, dark urine, very dry mouth, and no tears)
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.

Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 12/01/2022
Last Revised: 09/21/2022
Copyright 2000-2022 Schmitt Pediatric Guidelines LLC.
Spitting up and vomiting in infants
Spitting up and vomiting in babies is a common reason for visiting a doctor.
Regurgitation and vomiting is a reflex action that occurs when receptors located in various anatomical zones are irritated, incl. in the stomach, esophagus, pharynx, oral cavity. The signal is transmitted to the vomiting center, which is located in the medulla oblongata and a gag reflex occurs.
What is the difference between regurgitation and vomiting?
The difference lies in the volume and kinetics (movement) of the gastric contents expelled to the outside. When regurgitation occurs, leakage occurs without the participation of the diaphragm and abdominal muscles, i. e. passively. There is little content, up to about 10-15 ml. If the child does not swallow it, it quietly expires from the oral cavity. When vomiting, a wave-like bending of the upper half of the body occurs as a result of contraction of the muscles of the diaphragm and the anterior wall of the abdomen, the volume of vomit is greater, and they are erupted with pressure from the oral cavity with an ejection trajectory of up to 50 cm. In children of the first year of life, this is defined by the term "fountain vomiting" .
e. passively. There is little content, up to about 10-15 ml. If the child does not swallow it, it quietly expires from the oral cavity. When vomiting, a wave-like bending of the upper half of the body occurs as a result of contraction of the muscles of the diaphragm and the anterior wall of the abdomen, the volume of vomit is greater, and they are erupted with pressure from the oral cavity with an ejection trajectory of up to 50 cm. In children of the first year of life, this is defined by the term "fountain vomiting" .
Regurgitation is observed only in children of the first year of life and, mainly, up to 6 months. Contribute to this anatomical and physiological features of the esophagus and stomach of the baby. Their esophagus is short and wide, the angle of connection of the esophagus with the stomach is less pronounced, and its obturator function is weak. These regurgitations are physiological. They can be after each feeding, up to 15 ml, do not affect the well-being and weight gain of the baby. They can also be caused by excessive feeding, aerophagia (swallowing air while sucking), straining during intestinal colic. The frequency and volume of such regurgitation decreases with the growth of the child. With the introduction of complementary foods, and this is a thicker food, regurgitation stops or becomes much less frequent.
They can also be caused by excessive feeding, aerophagia (swallowing air while sucking), straining during intestinal colic. The frequency and volume of such regurgitation decreases with the growth of the child. With the introduction of complementary foods, and this is a thicker food, regurgitation stops or becomes much less frequent.
If regurgitation persists in a child older than 1 year, then this is a sign of a pathological process.
Vomiting, unlike regurgitation, is accompanied by vegetative symptoms - increased salivation, pallor of the skin, palpitations. This is due to the fact that next to the vomiting center there are additional centers of autonomic regulation, which are reflexively excited, and active biological substances such as serotonin, dopamine, histamine and others are released into the blood.
Regurgitation and vomiting, from the moment of eating, may occur during feeding, after feeding for the first 20-30 minutes or delayed, sometimes after several hours.
Regurgitation and vomiting that occurs immediately after feeding unchanged breast milk or formula may be due to narrowing of the esophagus. If they persist until the next feeding, and the milk / mixture is curdled, has a sour or musty smell, then this is the result of a long standing food in the stomach. The reason for this may be the low tone of the muscle layer of the stomach and, as a result, its peristalsis or narrowing of the output section due to an anomaly in the development or high tone of the sphincter of the lower stomach. With narrowing of the duodenum, bile is present in the regurgitated masses.
Gastroesophageal reflux is a common cause of regurgitation in infants. It is likely that there is a complex problem here, starting with the immaturity of the gastrointestinal tract and disorders of the central nervous system. Perinatal injuries of the central nervous system accompany every second child. Their manifestations are varied. Regurgitation and vomiting can be facilitated by an increase in intracranial pressure, disorders in the segment of the cervical spine, and so on. Therefore, quite often, when carrying out rehabilitation measures for neurological dysfunctions, a positive effect is manifested in the form of a decrease or cessation of regurgitation. A hernia of the esophageal opening of the diaphragm will also manifest itself in a similar way.
Therefore, quite often, when carrying out rehabilitation measures for neurological dysfunctions, a positive effect is manifested in the form of a decrease or cessation of regurgitation. A hernia of the esophageal opening of the diaphragm will also manifest itself in a similar way.
We should not forget about allergic gastrointestinal reactions in the form of regurgitation and vomiting. The most common cause of this is cow's milk protein. With intolerance to cow's milk protein, inflammation of the mucous membrane of the esophagus, stomach and intestines occurs. And, as a result of this, regurgitation and vomiting, pain and increased gas formation, diarrhea or constipation.
Rare endocrine disorders (adrenogenital syndrome) are manifested by vomiting in children from the first weeks of life. In such cases, vomiting is frequent, there may be an admixture of bile, the child loses weight due to loss of fluid and nutrients, and severe metabolic disorders develop.
Vomiting can also be caused by an intestinal infection. Viral gastroenteritis is now common. It must be remembered that the younger the child, the more severe the disease. Within a few hours, the child's condition can go from satisfactory to extremely serious.
Viral gastroenteritis is now common. It must be remembered that the younger the child, the more severe the disease. Within a few hours, the child's condition can go from satisfactory to extremely serious.
As you can see, the causes of regurgitation and vomiting in children of the first year of life are quite diverse, but most often these are transient conditions that disappear with the growth of the child.
Prevention of regurgitation in children of the first months of life is quite simple. Don't overfeed your baby. If he cries, it does not always mean that he is hungry. Excess feeding leads to increased gas formation and colic, during which the child is worried, straining, thereby increasing the likelihood of spitting up. After feeding, hold the baby more upright so that he can burp the swallowed air. This will take 15-20 minutes. If the child is bottle-fed, do not change his formula milk without the recommendation of a pediatrician.
If the child has frequent regurgitation and vomiting, it is necessary to consult a pediatrician or gastroenterologist to diagnose the cause. To make a diagnosis, it is sometimes enough to carry out simple and affordable diagnostic methods in a polyclinic. These include an ultrasound of the stomach and, if necessary, stool tests. However, the approach in each case is individual. Examination and treatment will be assigned to your baby, depending on the diagnosis. Perhaps it will be preventive measures or a certain milk formula, perhaps drug therapy. Rarely, but it happens that it is necessary to examine the child in a hospital and surgical treatment.
To make a diagnosis, it is sometimes enough to carry out simple and affordable diagnostic methods in a polyclinic. These include an ultrasound of the stomach and, if necessary, stool tests. However, the approach in each case is individual. Examination and treatment will be assigned to your baby, depending on the diagnosis. Perhaps it will be preventive measures or a certain milk formula, perhaps drug therapy. Rarely, but it happens that it is necessary to examine the child in a hospital and surgical treatment.
Why does the baby spit up after feeding?
search support iconSearch Keywords
Regurgitation is a common condition in newborns and infants and is most often a normal variant. However, it is not uncommon for parents to worry if their baby is spitting up frequently, believing that it is due to nutritional or health problems in general. Sometimes these fears are not unfounded, and regurgitation really has a pathological origin. What is its cause and when should you really consult a doctor about this?
Regurgitation — Return of a small amount of food (uncurdled or partially curdled milk) from the stomach up the digestive tract: into the esophagus and further into the oral cavity. According to statistics, at least 1 time during the day can spit up at least 50% of babies from 0 to 3 months, more than 60% of children 3-4 months, and 5% of children spit up until the year 1 .
According to statistics, at least 1 time during the day can spit up at least 50% of babies from 0 to 3 months, more than 60% of children 3-4 months, and 5% of children spit up until the year 1 .
Regurgitation in newborns is considered a physiological process. It is caused by a number of factors, including:
- Features of the structure of the upper digestive tract in babies
- In newborns and infants up to a year of age, the stomach has a spherical shape. It holds a small amount of food, besides, the release from it into the duodenum is slower in comparison with children after the year 2 .
- Weakness of the lower esophageal sphincter that separates the esophagus from the stomach
- Normally, the lower esophageal sphincter should tightly “close” the esophagus, allowing food to pass into the stomach and not allowing it to enter back into the upper digestive tract. However, in young children (up to a year), the muscles of the esophageal sphincter are poorly developed, and it does not do its job very well 2 .
- Slow movement of food through the gastrointestinal tract
- The neuromuscular apparatus of newborns is immature. It does not ensure the proper movement of food through the esophagus, causing regurgitation.
One of the important risk factors contributing to the appearance of regurgitation in newborns is aerophagia. This is the swallowing of large amounts of air during feedings. This happens when the baby is not properly attached to the breast, the mother has a lack of breast milk, or the bottle is in the wrong position in the child who receives the mixture. The size of the opening in the nipple also matters - if it is too large, the newborn swallows a lot of air 3 .
With aerophagia, the baby becomes capricious, restless immediately after feeding. Noticeable bloating. If the baby spits up immediately after a feed, the milk (or formula) remains practically fresh, uncurdled 3 .
Promotes post-feeding regurgitation and predominantly horizontal position of the baby during the day, combined with relatively high intra-abdominal pressure 4 . Therefore, the correct position of the baby after feeding is so important. To avoid regurgitation of an excessive amount of stomach contents, after feeding, it is necessary to hold the baby in an upright “column” position for some time (10-20 minutes), lightly patting on the back and allowing excess air to “exit”.
Therefore, the correct position of the baby after feeding is so important. To avoid regurgitation of an excessive amount of stomach contents, after feeding, it is necessary to hold the baby in an upright “column” position for some time (10-20 minutes), lightly patting on the back and allowing excess air to “exit”.
Regurgitation in many newborns can be triggered by other situations in which pressure in the abdominal cavity increases and stomach contents are thrown into the esophagus, in particular 3 :
- tight swaddling;
- stool disorders, in particular constipation;
- long, forced cry and some others.
Want to avoid common feeding problems?
Start with a baby bottle with an anti-colic system that helps you avoid common feeding problems such as colic, gas and spitting up*
How can you tell the difference between normal spitting up and vomiting?
Sometimes regurgitation is considered a manifestation of disorders in the digestive tract of children. Due to the constant reflux of acidic stomach contents into the upper sections, inflammation and other complications may develop, including growth retardation, a decrease in hemoglobin levels, and others. Therefore, it is important for parents to understand where the line is between physiological and pathological regurgitation 1 .
Due to the constant reflux of acidic stomach contents into the upper sections, inflammation and other complications may develop, including growth retardation, a decrease in hemoglobin levels, and others. Therefore, it is important for parents to understand where the line is between physiological and pathological regurgitation 1 .
If the mother is worried that her baby is spitting up, keep track of when this happens and count the total number of spit ups per day. Normally, regurgitation usually occurs after eating (the child burps after each feeding), lasts no more than 20 seconds and repeats no more than 20-30 times a day. With pathology, the problem manifests itself at any time of the day, regardless of when the baby was fed. Their number can reach 50 per day, and sometimes more 1 .
The amount of discharge during regurgitation also matters. With normal, physiological regurgitation, it is approximately 5 - 30 ml. If this volume fluctuates between 50 and 100 ml, it is already defined as profuse vomiting. When the range of the jet of vomit is up to 50 cm, doctors talk about "vomiting a fountain." A variant of atonic vomiting is possible, when the contents of the stomach flow "sluggishly". It occurs with atony of the stomach (decrease in muscle tone of the stomach wall) and disruption of the esophagus 1 .
When the range of the jet of vomit is up to 50 cm, doctors talk about "vomiting a fountain." A variant of atonic vomiting is possible, when the contents of the stomach flow "sluggishly". It occurs with atony of the stomach (decrease in muscle tone of the stomach wall) and disruption of the esophagus 1 .
Vomiting in babies is a warning sign. Doctors are especially alarmed by repeated vomiting, a fountain, with an admixture of bile, in combination with constipation. Vomiting can lead to the development of dehydration, acid-base imbalance and other consequences, therefore, if it occurs, you should urgently contact a pediatrician to find out the cause and begin treatment. A doctor's consultation is necessary if the child is spitting up a lot (more than 15-30 ml at a time), with a frequency of more than 50 episodes per day 1.3 .
Physiological regurgitation: symptoms
Regurgitation in newborns, which is considered normal and not of concern to pediatricians 3 :
- usually continues for a certain period of time;
- is characterized by slow, "passive" leakage; if the baby spits up a fountain, it is better to consult a doctor;
- has a sour smell of curdled milk;
- occurs without the participation of muscles - the baby does not strain during regurgitation;
- does not affect the general well-being of the baby.

How to help a newborn who spit up often?
If the baby is healthy, no medication is prescribed for spitting up. To help the child allow simple measures based on lifestyle changes and feeding.
. To improve the situation, it is recommended to feed the baby more often, avoiding oversaturation, best of all - on demand 5 . The AirFree valve prevents air from entering the baby's stomach. To allow air that has entered the digestive tract during meals to escape, it is important to keep the newborn upright for 10-20 minutes after feeding 4 . To reduce the negative impact of the acidic contents of the stomach on the esophagus, it is necessary to put the baby to sleep in the supine position. The side or prone position, which many pediatricians used to recommend, is no longer recommended. It was found to be associated with an increased risk of sudden infant death syndrome 5 . If parents notice alarming symptoms, such as spitting up too often or large volume, etc., it is important to consult a pediatrician without delay. This will allow you to identify the real problem in time and help the baby grow up healthy and happy. 1 Zakharova I. Nagornaya 2904 V., Limarenko M. P., Logvinenko N. G. Experience with the use of domperidone in suspension in young children with regurgitation syndrome // Child Health, 2013. No. 5 (48). 3 Zakharova IN Regurgitation and vomiting in children: what to do? //Pediatrics. Supplement to Consilium Medicum, 2009. No. 3. S. 58-67. 4 Zakharova I. N., Sugyan N. G., Pykov M. I. Regurgitation syndrome in young children: diagnosis and correction // Effective pharmacotherapy, 2014. No. 3. P. 18-28. 5 Vandenplas Y. et al. Pediatric gastroesophageal reflux clinical practice guidelines: joint recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) //Journal of pediatric gastroenterology and nutrition.
Every feeding, the mother must ensure that the baby does not swallow too much air during suckling. When sucking, there should be no loud, smacking, clicking sounds. You also need to control that the baby captures the nipple along with the areola.
If a newborn is bottle-fed and receiving formula, it is important to choose the right bottle and nipple. The hole in it should be such that the milk flows out in drops, and not in a stream. The nipple must not be filled with air New Anti-colic bottle with AirFree valve

References  N., Andryukhina E. N. Regurgitation and vomiting syndrome in young children // Pediatric pharmacology, 2010. V. 7. No. 4.
N., Andryukhina E. N. Regurgitation and vomiting syndrome in young children // Pediatric pharmacology, 2010. V. 7. No. 4.