Babies with eczema and food allergies
Why Eczema Increases Your Baby's Risk of Developing Food Allergies – Lil Mixins
Now reading: Why Eczema Increases Your Baby's Risk of Developing Food Allergies
PrevNextEczema and food allergies are linked together. Eczema is a sign that your baby’s immune system is over-reactive. The more severe the eczema is, and the earlier it starts, the more the immune system is going crazy, and the more likely a baby is to develop food allergies. An immune system that is overactive is more likely to mistake harmless food as a danger.
Eczema also makes a bad situation worse. Eczema leaves cracks in your baby’s skin for food protein to sneak through. Eczema skin also gets infected easily, and infected eczema skin makes the immune system rev-up even more. Finally, the act of scratching itself can also activate the immune system.
What is Eczema?
Eczema is the “itch that rashes.” Eczema always begins with itching. Your baby’s skin itches either because it is very dry or because of a hidden immune reaction to a trigger like pollen, mold, or milk.
The hallmark of eczema is persistent red, dry skin on the face, especially the cheeks and forehead, in the arms near the elbows and wrists, and behind the knees as a baby starts to crawl. If a baby has enough hand control to scratch, the itchy skin can become thickened and scaly.
How Eczema Cracks in the Skin Can Cause Food Allergies
Many doctors are convinced cracks in eczema skin are the number one way that eczema causes food allergies and they have called it the Dual Exposure Hypothesis.
Eczema causes itching and dry skin. Very dry skin, or skin that has been scratched enough, will develop cracks. Some of these cracks are too small to see, others bleed or have scabs. When babies get food all over themselves, or even just crawl around, bits of food or dust get into those cracks.
A baby’s immune system will get scared by protein that it thinks broke through the skin. Once the immune system learns to be scared, it thinks harmless food is dangerous. This is what a food allergy is.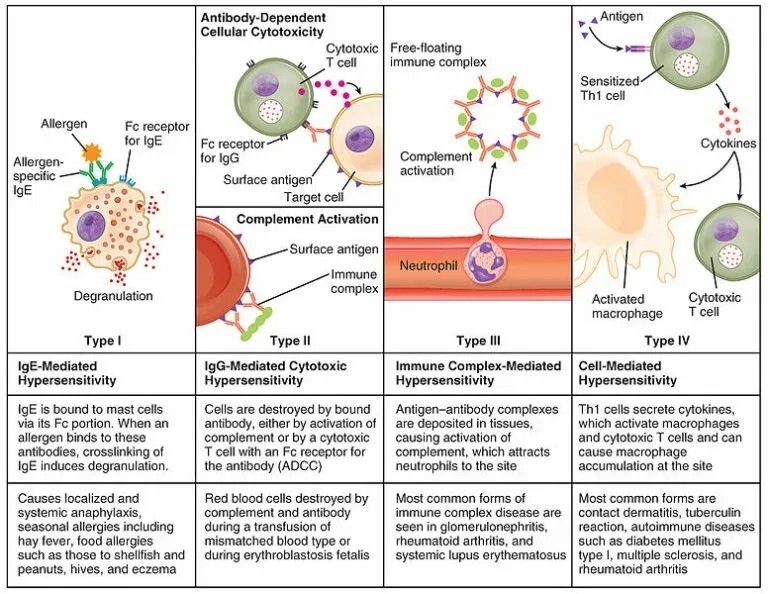
How Eczema Infections Can Cause Food Allergies
Every person’s skin is covered in bacteria, viruses, and fungi. One bacteria that is found on everyone is staph A. This bacteria is usually harmless, but when skin gets dry or cracked, like on babies with eczema, staph A jumps at the chance to spread out.
Staph A is very dangerous if it gets into your blood, and your body knows that. If staph A infects dry skin, your baby’s immune system will go into attack mode, flooding the body with immune cells.
In the LEAP study on peanut allergy prevention, doctors saw that almost all of the children with eczema who developed peanut allergy had a staph A infection. The kids with eczema but no infection had far fewer peanut allergies.
When the immune system is on high alert, it does a bad job of telling friend from foe, and makes the mistake of a food allergy.
How Eczema Scratching Can Cause Food Allergies
The weirdest way in which eczema itching causes food allergies is the act of scratching.
New research, so far only done in mice, at Boston Children’s Hospital showed that scratching the skin increases the chance of allergic reactions to foods, including anaphylaxis. The study showed that when you injure your skin by scratching, the immune system releases certain immune cells in the small intestine. Putting so many unnecessary immune cells in the small intestine can cause them to overreact to any food proteins that are undigested, leading to a food allergy.
What Can You Do to Stop Eczema from Causing Food Allergy?
Because eczema usually develops way before a baby starts eating solid food, your first priority should be to prevent or control eczema flares so that your baby’s skin doesn't have cracks, doesn’t get infected, and so that they don’t scratch.
The second most important way to stop eczema from causing food allergies is to train your baby’s body to recognize foods as safe and harmless. Early, regular feedings of nuts, eggs, peanut, dairy, and wheat can train your baby’s immune system not to have allergic reactions to food.
7 Foods to Avoid in Babies and Toddlers with Eczema
Also known as atopic dermatitis, eczema is a common condition characterized by red, itchy, and inflamed skin.
Although eczema can affect anyone, it’s especially common among children. In fact, about 60% of cases develop within the first year of life (1).
Many factors can worsen eczema flare-ups, including foods.
Research shows that certain foods may trigger eczema in 20–30% of cases of moderate to severe eczema. Additionally, foods are more likely to worsen symptoms in children and infants under age 5 (2).
While foods do not directly cause eczema, making dietary changes could help reduce symptoms, especially for those who have a sensitivity or allergy to specific foods (3).
In children with a confirmed food allergy, eliminating trigger foods from the diet may significantly improve symptoms of eczema within just 1–2 months (4).
However, keep in mind that it’s not necessary to avoid all the foods listed below to help manage your child’s eczema.
SummaryCertain foods may worsen symptoms of eczema, especially in children and infants. However, it depends on the child’s particular allergies or sensitivities, so speak with a healthcare professional to determine which foods might be best to eliminate.
Preventing food allergies
Introducing common allergen foods to an infant early in life may actually help prevent them from developing food allergies, including to eggs and peanuts (5).
If you’re considering eliminating certain foods from your child’s diet or you’re concerned about your child developing food allergies, speak with a healthcare professional. They can help you develop a diet plan based on your child’s needs.
Research has shown that eliminating one or more of these foods from the diet may significantly improve symptoms of eczema in some children.
1. Dairy
Not only is a cow’s-milk allergy the most common food allergy in young children, but dairy products like milk, yogurt, and cheese are also common triggers for eczema (6).
One study in 132 children with food-triggered eczema found that 39% of children developed an immediate reaction after consuming cow’s milk (2).
A 2019 review reported that infants with eczema were six times more likely to have an allergy to cow’s milk, eggs, or peanuts at 12 months of age compared with infants without eczema (7).
Fortunately, there are several simple plant-based milks available as an alternative to cow’s milk, including soy milk, almond milk, and cashew milk.
However, be sure to check the ingredients lists carefully, as some of these products are high in calories and added sugar.
2. Fish and shellfish
The term “shellfish” refers to any aquatic animal that has a shell-like exterior, including crabs, lobsters, oysters, mussels, and shrimp. Meanwhile, most types of fish, including salmon, trout, tuna, and tilapia, have fins and scales.
Although both fish and shellfish are highly nutritious and can be great sources of protein and omega-3 fatty acids, they can also worsen symptoms of eczema for many children.
This is because fish and shellfish allergies are common and can cause a wide range of side effects, including hives, itching, and eczema (8, 9).
While some children may be sensitive to finned fish or shellfish, others may experience reactions only to certain types, such as crustaceans (like shrimp and crab) or mollusks (like oysters and clams) (8).
A pediatrician or registered dietitian can help determine which specific types of seafood may trigger symptoms for your baby or toddler.
3. Soy products
For those with a soy allergy, consuming soy products like soy milk, tofu, or edamame can cause an immune response, which could trigger skin reactions such as eczema (10).
Compared with allergies to other major food allergens, soy allergies are not nearly as common (11, 12).
For example, one 2013 study in 175 people with eczema found that around 30% had an immune reaction to soy. However, only about 3% of people experienced symptoms, such as hives and itching, after consuming soy (13).
If your baby or toddler has a sensitivity to soy products, keep in mind that many processed foods contain soy-based ingredients, all of which could worsen symptoms of eczema. Examples include (14):
- soy sauce
- tamari
- soy protein
- textured vegetable protein
4. Eggs
Share on PinterestElena Botta/Getty Images
Some babies or toddlers may have an allergy to the proteins found in egg whites or yolks, which could trigger symptoms of eczema (15).
Egg allergy is one of the most common food allergies, affecting an estimated 1.3% of children under 5 in the United States (16).
Furthermore, one study reported that infants with eczema are nearly 6 times as likely to develop an egg allergy by 12 months of age compared with those without eczema (7).
However, most egg allergies in children resolve by around age 5 (17).
Additionally, some babies and toddlers who are sensitive to eggs may be able to tolerate them in some forms, such as baked eggs (16).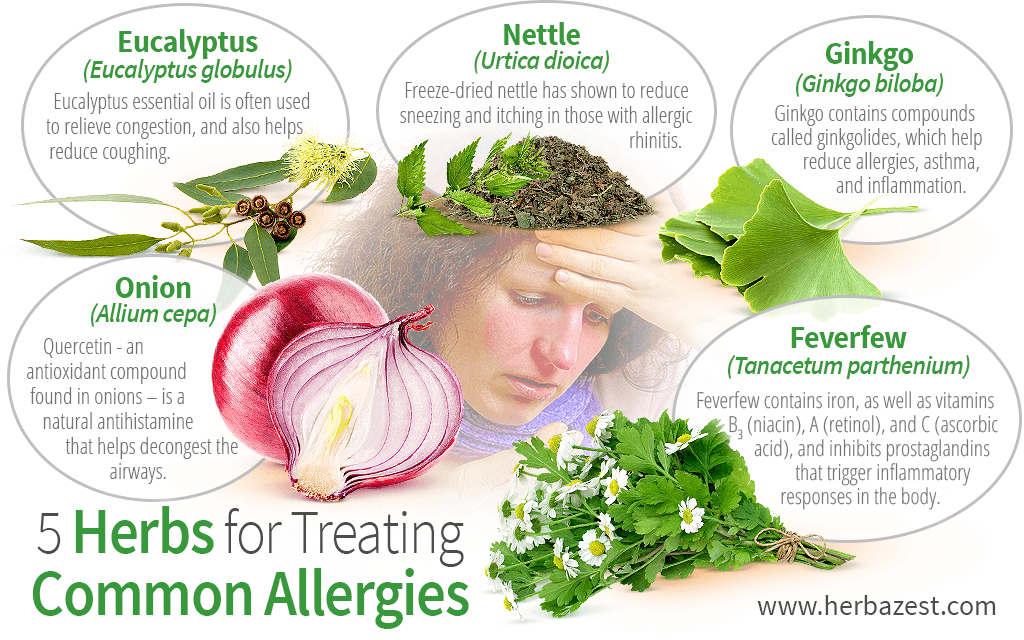
5. Tree nuts
Tree nuts could worsen eczema for many young children with a tree nut allergy. Examples of tree nuts include:
- almonds
- cashews
- walnuts
- pecans
Tree nut allergies are very common and may affect up to 4.9% of children and adults (18).
Unfortunately, tree nut allergies can be very serious, and some research suggests that more severe reactions to tree nuts are often associated with severe cases of eczema, asthma, and seasonal allergies (19).
In addition to avoiding tree nuts specifically, your child may need to avoid foods that contain tree nuts, including pesto, nut butters, coconut products, and certain types of cereals, cookies, crackers, or candies.
6. Wheat or gluten
Wheat is a type of cereal grain and a staple ingredient in many foods, such as bread, pasta, and baked goods.
Gluten is a specific protein found in wheat, barley, and rye that gives dough its structure and elasticity.
For those with a wheat allergy, consuming products that contain wheat may worsen eczema and could also cause other symptoms, including hives, asthma, and digestive issues (20, 21).
Eczema and skin rashes can also be caused by a sensitivity to gluten, as well as by celiac disease, an autoimmune condition that triggers an immune reaction when gluten-containing foods are consumed (22, 23, 24).
While there is no test available to diagnose non-celiac gluten sensitivity, your child’s pediatrician can use a skin or blood test to help determine if your child has celiac disease or an allergy to wheat.
7. Peanuts
Peanuts are a common allergen and are associated with several skin reactions, including rashes, hives, itching, and eczema (25).
Peanut allergies are especially common among babies and toddlers, as most peanut allergies appear within the first 2 years of life (25).
Additionally, some research shows that peanut allergies are more common among infants with moderate to severe eczema (26).
If peanuts cause flare-ups of eczema for your baby or toddler, try swapping other ingredients into your favorite recipes instead, such as seeds or seed butters.
SummarySome of the most common foods that cause allergies in infants and toddlers are dairy, fish, shellfish, soy products, wheat, peanuts, tree nuts, and eggs.
Several foods can be beneficial for eczema and may help reduce symptoms such as itching and inflammation.
For example, fruits and vegetables are rich in antioxidants, which are compounds that can protect against oxidative stress, cell damage, and inflammation (27).
Although studies in humans are still limited, some research suggests that reducing oxidative stress could play a role in managing eczema (28).
Increasing your intake of probiotics through fermented foods or supplements may also be helpful.
According to one review of 13 studies, certain strains of probiotics were effective at reducing eczema severity in children. These strains included Lactobacillus fermentum and Lactobacillus salivarius (29).
However, more research is needed because other studies have found that probiotics do not have a significant effect on symptom severity or quality of life for those with eczema (30).
SummaryIncluding more foods rich in antioxidants and probiotics in your child’s diet could be beneficial for eczema, but more research is needed.
For many babies and toddlers, diet can play a key role in managing symptoms of eczema.
While certain foods can make eczema symptoms worse, others may decrease inflammation and oxidative stress, which could reduce symptoms.
However, it’s best to talk with a pediatrician or dietitian before making any changes to your child’s diet, especially because eliminating certain foods from their diet could make it harder for them to meet their nutritional needs.
Additionally, keep in mind that many other factors can contribute to eczema and some children may also need other types of treatment to help relieve symptoms.
Just one thing
Try this today: Consider experimenting with some at-home remedies for your child’s eczema. Check out this article for a few ideas to help provide relief for your baby or toddler.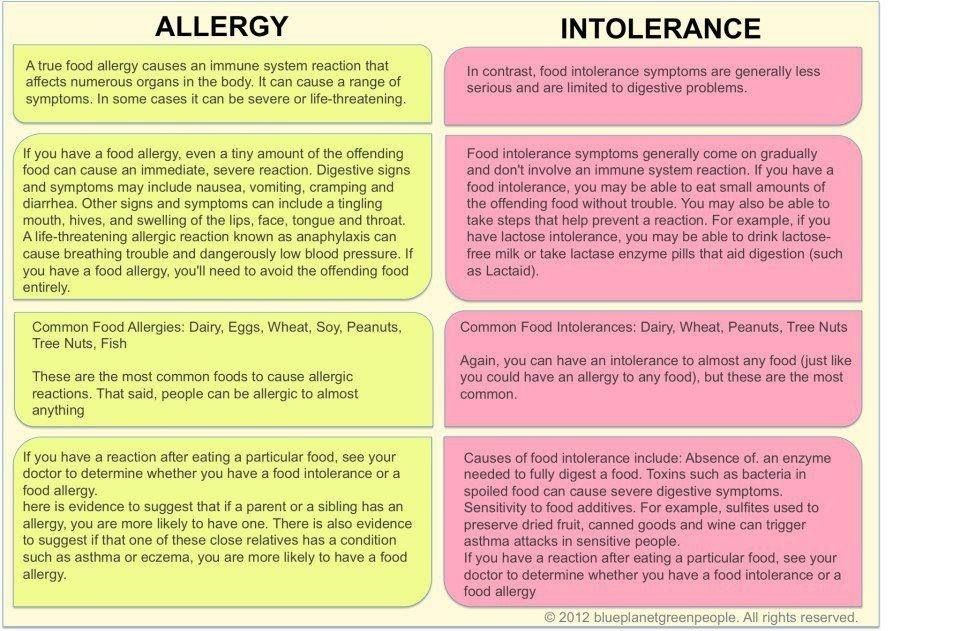
eczema | Nestlé Health Science
- Nestlé Health Science
- health care
- Eczema
Eczema - a typical inflammatory skin disease accompanied by intense itching, which is characterized by red or brownish, dry, cracked and scaly skin, which is especially itchy at night. In children, eczema usually appears on the face, scalp, and outer surfaces of the limbs.
Why does my child have eczema?
The exact causes of eczema are not well known, but in many cases your child may have eczema due to a food allergy, eg Cow's Milk Protein Allergy (CMP) . Many children who develop eczema are allergic to one or more allergy-causing substances during infancy. If there is a family history of allergic reactions, such as asthma or a pollen allergy, your child may be more likely to develop eczema.
Baby eczema is one of the most common symptoms of CMPA
Symptom analysis
Could this be a manifestation of CMPA?
Children with CMPA usually have more than one symptom, and these symptoms can be very different from each other.
If you think baby has eczema it could be CMPA.
You may have noticed other symptoms (other than eczema) that may affect other parts of your child's body.
As a simple and easy way to check for typical symptoms associated with CMPA, you can use our Symptom Checker.
It will allow you to select all cow's milk symptoms your baby may have. You can then discuss this with your doctor.
In any case, if you have any doubts or concerns about your child's health, you should consult with a healthcare professional as soon as possible.
Other symptoms of cow's milk protein allergy
ANAPHILACTIC SHOCK
View product
CRYING AND COLIC
View product
CONSTIPATION
View product
COUGH
View product
DIARRHEA
View product
GROWTH DISTURBANCE
View product
urticaria
View product
REFUSAL TO FOOD
View product
RASH
View product
REFLUX AND BUCK
View product
Runny nose and sneezing
View product
EDITEC
View product
VOMITING
View product
HRIP
View product
IMPORTANT NOTE: : It is possible to continue breastfeeding if the infant is allergic to cow's milk protein. To do this, the mother needs a special diet with the exclusion of all sources of cow's milk protein. Only if these measures do not bring the desired effect, the doctor recommends the use of a special therapeutic mixture intended for children from 0 to 1 year old. It is important to follow the correct methods of preparing the mixture: using boiled water, sterilized bottles and following the rules for diluting the mixture. Medicinal mixtures intended for diet therapy of CMPA should be used under the supervision of a physician.
To do this, the mother needs a special diet with the exclusion of all sources of cow's milk protein. Only if these measures do not bring the desired effect, the doctor recommends the use of a special therapeutic mixture intended for children from 0 to 1 year old. It is important to follow the correct methods of preparing the mixture: using boiled water, sterilized bottles and following the rules for diluting the mixture. Medicinal mixtures intended for diet therapy of CMPA should be used under the supervision of a physician.
Allergic skin diseases in children
External treatment of allergic diseases in children
Allergic diseases in childhood are not uncommon. Eczema, food allergies, allergic dermatitis, diathesis, urticaria, pruritus, atopic dermatitis - this is not a complete list of what a child of even a very young age can suffer from. Among these diseases, the most persistent and difficult to treat is atopic dermatitis. Its mandatory treatment is the guarantee of skin health for life.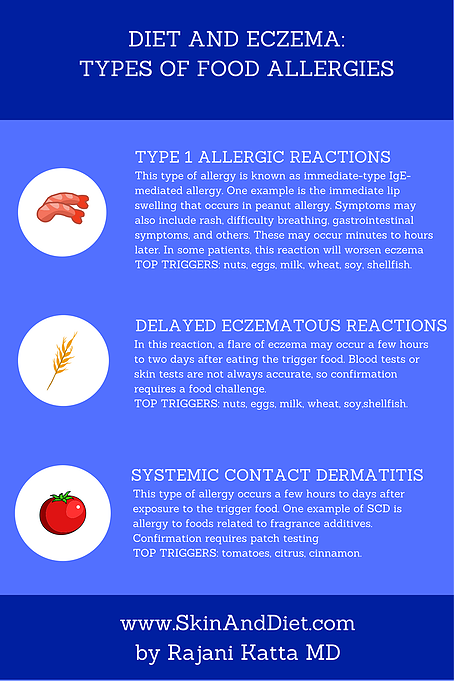 Well and competently treated at an early age, it can disappear by 3 years forever. But even older children should not give up.
Well and competently treated at an early age, it can disappear by 3 years forever. But even older children should not give up.
In treatment, internal remedies are always combined with external ones. In this publication, I will focus on the features of external treatment.
In recent years, corticosteroid (hormonal) ointments have taken the leading place among the external therapy of atopic dermatitis, pushing other drugs aside. Every doctor knows the names of corticosteroid ointments, and the question is no longer whether to use them or not to use them. Rather, the choice of the most effective of them is carried out, with fewer side effects and the possibility of more or less long-term use. It often does not coincide with the financial capabilities of parents who, not seeing the difference between the drugs, choose a cheaper ointment. Without denying the undeniable benefits of corticosteroid ointments during an exacerbation, I want to note that none of them is suitable for long-term use, and an exacerbation can last for many months. In addition, there is no drug specifically designed for the treatment of children. In this regard, each dermatologist and pediatrician, in an effort to reduce the concentration of the medicinal substance applied to the skin of a sick child, uses his “home-made preparations”, which generally come down to mixing the finished drug with various creams, oils, solutions or other ointments. In this case, the dosage form of the drug is violated, which is highly undesirable, since its physicochemical and pharmacological properties change in this case.
In addition, there is no drug specifically designed for the treatment of children. In this regard, each dermatologist and pediatrician, in an effort to reduce the concentration of the medicinal substance applied to the skin of a sick child, uses his “home-made preparations”, which generally come down to mixing the finished drug with various creams, oils, solutions or other ointments. In this case, the dosage form of the drug is violated, which is highly undesirable, since its physicochemical and pharmacological properties change in this case.
We agree that it is difficult to do without glucocorticosteroid (hormonal) external preparations. But here are some quite typical situations that both the doctor and the parents of patients have to face during the treatment of atopic dermatitis in children:
- A short (usually 2 weeks) course of treatment with corticosteroid ointments has been completed - what to lubricate the skin further?
- Long-term treatment with corticosteroid ointments has led to addiction - which external agents should I switch to?
- Parents strongly refuse treatment with corticosteroid ointments (corticophobia is now a common phenomenon, and there are good reasons for it, because the permeability of the child's skin is much higher than in adults, and corticosteroid ointments applied to it cannot but have a systemic effect - than their replace?
- The long-awaited remission has come, but the skin remains dry and easily irritated - how to eliminate these phenomena?
To answer these questions, let's consider what dermatologists have in the arsenal of external non-steroidal treatments for atopic dermatitis, and what tasks can be solved using the means of various groups. In the following, we present only finished medicinal products. The success of numerous medicinal prescriptions used in pediatric practice depends on the experience of the dermatologist and has not been proven by clinical trials.
In the following, we present only finished medicinal products. The success of numerous medicinal prescriptions used in pediatric practice depends on the experience of the dermatologist and has not been proven by clinical trials.
Antimicrobial and antiseptic agents
Fukaseptol and Fukortsin (solutions for external use, 10 and 25 ml in vials) are similar in composition to a red liquid with a characteristic odor of aniline dye (magenta). Fukaseptol is manufactured using a new technology that allows you to keep the composition of the drug stable throughout the entire shelf life. The components of fucorcin during long-term storage may precipitate. Both drugs have an excellent antimicrobial and antifungal effect, without interfering with healing. They are used for application to crusts, places of combing, pustules. It is not recommended to lubricate fresh wounds, because. the alcohol in the composition causes a burning sensation. Large areas of skin should not be treated. After the solution has dried, pastes, ointments and creams can be applied to the skin.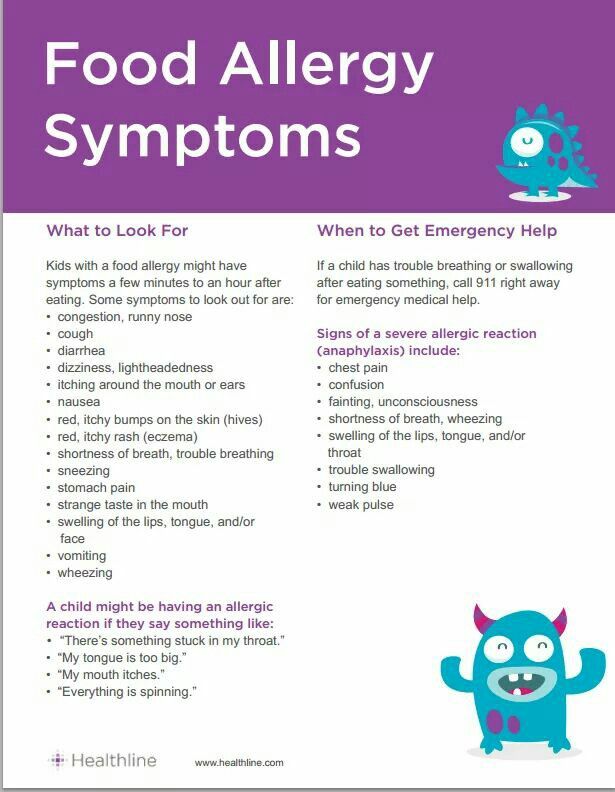
Alcohol solution of methylene blue 1% has similar indications and application features. When applied to large areas of the skin, the urine of the child turns blue.
Hydrogen peroxide 3% causes stinging when applied to the skin but is always well tolerated. She treats fresh wounds and scratches.
Furacilin solution 0.02%, made from powder and 0.2 g tablets, belongs to another group of antiseptics - nitrofurans. Due to the weak effect and frequent cases of increased inflammation, nitrofurans in the treatment of allergic diseases have given way to stronger antiseptics - halogen-containing (chlorhexidine - 0.05% solution of 100 ml per vial) and miramistin (0.01% solution of 100 ml per vial). .). Both solutions are aqueous, they can treat fresh wounds and scratches without risking causing pain in the child, however, aqueous solutions dry out for a long time, and the skin treatment process, which is always unpleasant for babies, is delayed.
Antibiotic ointments are used with caution in atopic dermatitis, as they are often allergenic.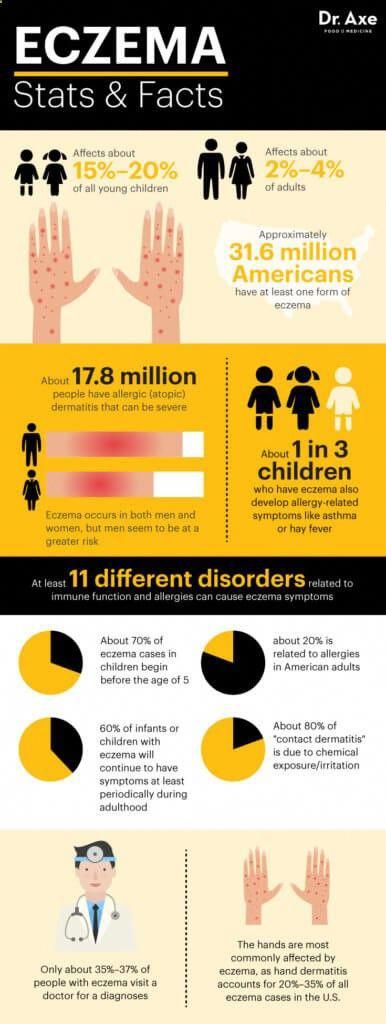 This group is dominated by domestic preparations, with the exception of Bactroban ointments (contains 2% mupirocin), Baneocin, Fucidin. Combined ointments Baneocin (contains bacitracin and neomycin), Levomekol ointment (contains chloramphenicol and methyluracil), Levosin ointment (contains chloramphenicol, methyluracil, sulfadimethoxin), in our experience, do not have any significant advantages. Unfortunately, the fatty base of domestic antibiotic ointments does not contribute to the drying and falling off of the crusts, rather softening them, so dermatologists prefer to use pastes with antibiotics (1% erythromycin, 2-5% lincomycin), manufactured by prescription in a pharmacy. Fusidin gel and Fucidin cream (contains 2% fusidic acid) has some advantage since there are still few resistant strains of microorganisms to the fusidic acid contained in the preparation.
This group is dominated by domestic preparations, with the exception of Bactroban ointments (contains 2% mupirocin), Baneocin, Fucidin. Combined ointments Baneocin (contains bacitracin and neomycin), Levomekol ointment (contains chloramphenicol and methyluracil), Levosin ointment (contains chloramphenicol, methyluracil, sulfadimethoxin), in our experience, do not have any significant advantages. Unfortunately, the fatty base of domestic antibiotic ointments does not contribute to the drying and falling off of the crusts, rather softening them, so dermatologists prefer to use pastes with antibiotics (1% erythromycin, 2-5% lincomycin), manufactured by prescription in a pharmacy. Fusidin gel and Fucidin cream (contains 2% fusidic acid) has some advantage since there are still few resistant strains of microorganisms to the fusidic acid contained in the preparation.
Significantly better tolerated, although less frequently used, silver sulfathiazole preparations - Argosulfan cream and ointment containing 2% silver sulfathiazole in tubes of 40 g, Dermazin cream, 1%, 50 g each, Sulfargin ointment in tubes of 50 g. should not be used in case of allergy to sulfanilamide and sulfur-containing drugs.
should not be used in case of allergy to sulfanilamide and sulfur-containing drugs.
Bismuth preparations (dermatol ointment 10%, xeroform ointment 10%) are inexpensive domestic preparations that have an excellent effect (antiseptic, drying and anti-inflammatory), however, they have a sharp unpleasant odor and are rarely found in pharmacies.
Skin-cap preparations (70 and 100 ml aerosol, 50 g cream) also combine antiseptic and anti-inflammatory properties, high cost limits their wide application.
Anti-inflammatory and antipruritic drugs
ASD paste 5% is an excellent drug that successfully competes with corticosteroid ointments in terms of its strength. It used to be possible to make it in a pharmacy with a prescription, but due to the strong unpleasant smell and the reduction in the number of manufacturing pharmacies, this is now very difficult to do.
Elidel (contains pimecrolimus, 1% cream at 15.30 and 100 g) is a relatively new anti-inflammatory drug that prevents the production and release of biologically active substances from lymphocytes and mast cells (involved in cell inflammation). Can be used in children from 3 months of age. Use is contraindicated in case of infection of rashes (the appearance of pustules, crusts, weeping), it is not recommended to combine with other external agents. The use of the drug is limited by its high cost.
Preparations containing zinc oxide (suspension Zindol zinc paste and ointment) have a moderate anti-inflammatory and drying effect, but are widely used in pediatric practice, since they almost never cause side effects, are cheap and available.
Ichthyol ointment 10 and 20% - a drug with a moderate anti-inflammatory and resolving effect, is used in a period when acute inflammation is behind, and skin density is maintained. The action of the ointment is enhanced by the application of occlusive dressings (compress paper or a piece of cellophane is placed on top of the ointment and covered with a bandage), they also prevent soiling of linen in the dark brown color characteristic of this ointment.
Naftaderm (10% Naftalan oil liniment in tubes of 35 g) is an anti-inflammatory, antipruritic, analgesic, wound healing drug that also has the ability to enhance the effect of other externally applied agents, therefore it is usually used in combination with other external preparations. Its disadvantage is a specific oil smell.
Ointments related to non-steroidal anti-inflammatory drugs (indomethacin ointment 10% and gel 5% and 10%, Butadion 5%, etc.) are rarely used for treatment, as they are not effective enough and sometimes cause allergic skin reactions.
Lead water or lotion (0.5% lead acetate solution - 100 ml per vial) is one of the old ways to relieve acute inflammation. Other preparations for lotions in finished form are not currently available.
Topical antihistamines such as Fenistil (gel 1% in tubes of 20 and 30 g) are unfortunately not often effective in atopic dermatitis. They are useful in the first hours of an exacerbation, as well as with concomitant urticaria or a hyperergic reaction to insect bites in the summer.
Healing agents that improve trophism and tissue regeneration
The group primarily includes preparations containing vitamin A (ointments Videstim, Radevit, Redecyl). Videstim ointment (containing 0. 5% emulsion-based retinol palmitate, in tubes of 35 g) is specially designed for a low concentration of vitamin A, which makes it suitable for use in the youngest children. Ointment Radevit contains 3 fat-soluble vitamins - A, D and E (in tubes of 35 g), which act as synergists, that is, they enhance each other's action. They are used in the subacute and chronic phases of atopic dermatitis, as they do not have a pronounced anti-inflammatory activity.
Methyluracil ointment 10% - includes methyluracil as an immunomodulator and healing stimulator. This is a remedy with a moderate healing effect, which is partly due to its vaseline base, which prevents the active principle of the ointment from penetrating into the dermis. A new modern analogue, Stizamet ointment (contains 3% methyluracil on an emulsion basis in tubes of 35 g), is easily absorbed into the skin, while softening and moisturizing it, has a pronounced healing and immunomodulatory effect (improves skin immunity). Ointment Redecyl (combined preparation containing 1% retinol palmitate and 3% methyluracil on an emulsion basis in tubes of 35 g) combines the healing and immunomodulatory properties of both active substances included in it. It is specially designed for the treatment of allergic skin diseases. In addition, it turned out to be useful in restoring the skin after suffering an exacerbation and prolonged use of hormonal ointments.
Drugs containing dexpanthenol are often and successfully used in therapy. Aerosol Panthenol (130 ml each) and Bepanten (5% cream, 5% ointment in tubes of 30 g and 2.5% lotion of 200 ml) have a good and fast effect on combed skin areas.
Calf blood preparations are increasingly used by dermatologists and pediatricians (Actovegin cream 5% and ointment 5% in tubes of 20 g, Solcoseryl - gel 5% and ointment 5% in tubes of 20 g). Their therapeutic spectrum is rather narrow, in addition, dosage forms are changed as they heal, so the use is limited to the healing of cracks and scratches.
The range of softening and moisturizing products is not that wide, however, these are very necessary products that eliminate dry skin. They can be used in any phase of inflammation.