Baby care advice feeding aversion
Feeding Aversion - Why your baby is refusing bottles, breast or solids – Baby Care Advice
When we imagine what it should look like to feed a baby, we picture a scene of a hungry baby, gently cradled in our arms, who serenely gazes towards us as he contently feeds, peacefully stopping when satisfied. This is in stark contrast to the way in which babies who develop an aversion to feeding or eating behave. The scene is one of a screaming, hungry baby who acts like you're trying to poison him when you offer him a bottle of milk, breastfeed, or solid foods.
What is a feeding aversion?An aversion is the avoidance of a thing or situation because it is psychologically linked with an unpleasant, stressful, frightening, or painful experience. Basically, it’s fear that is displayed in anticipation of something bad happening again. A ‘feeding phobia’ and ‘feeding strike’ are other terms that may be used to describe a feeding aversion.
A feeding aversion refers to a situation where a physically well baby, repeatedly exhibits partial or full feeding refusal despite obvious hunger. A feeding-averse baby has a history that demonstrates he’s capable of feeding but for reasons yet to be identified and corrected, he refuses to feed or eats very little.
Babies as young as 7 weeks of age can develop an aversion to breastfeeding or bottle-feeding. Older babies can become averse to eating solids. Not just certain foods but the experience of eating solids. A baby could become averse to one, two, or all three feeding methods.
Feeding aversion signs and symptoms:A baby might display one or more of the following behaviors:
- Skips feedings or meals without distress.
- Appears hungry but refuses to eat.
- Fusses or cries when a bib is placed around his neck, or when placed into a feeding position, or when the bottle is offered or shown.
- Clamps his mouth shut or cries and turns his head away from the breast, bottle, spoon, or food.
- Takes a few sips or a small portion of the milk or food offered but then pulls away or arches back in a tense manner or cries.
 (NOTE: Babies back arch to distance themselves. Back arching does not provide evidence of acid reflux.)
(NOTE: Babies back arch to distance themselves. Back arching does not provide evidence of acid reflux.) - Feeds only while drowsy or asleep.
- Consumes less milk or food than expected.
- Refuses milk but eats solids.
- Displays poor or slow growth. May be diagnosed as 'failure to thrive'.
The type and intensity of behavior vary between babies. At one end of the spectrum, a baby might simply refuse to eat a particular food owing to a bad experience while eating that food. At the other end, a baby might display almost complete food refusal, eating very little, and require a feeding tube to ensure that he receives sufficient nourishment for healthy growth.
Feeding is not something that a baby can avoid entirely. A feeding-averse baby will reluctantly eat enough to survive but not voluntarily eat enough to thrive. Once averse to feeding a baby will try to ignore his hunger cues for as long as possible. Only willingly, but cautiously, eating when ravenous. Then eating quickly in fear of a repeat occurrence of whatever it is causing his fears. Eating just enough to soothe pangs of hunger, but not enough to feel completely satisfied.
Then eating quickly in fear of a repeat occurrence of whatever it is causing his fears. Eating just enough to soothe pangs of hunger, but not enough to feel completely satisfied.
A few behaviors displayed by some, but not all, feeding-averse babies require special mention due to the confusion they cause. These include:
- Conflicted feeding behavior
- Sleep-feeding
- Accepts water from a bottle
Many feeding-averse babies display conflicted feeding behavior - where the baby takes a few sucks, sharply turns away or arches back in a tense manner, possibly cries, quickly returns and wants to suck again, takes a few sucks, turns away or arches back, cries, and returns to feeding and so on. This disjointed feeding behavior is often interpreted by parents and others as an indication that the baby is experiencing pain, especially if he is intermittently crying, but it’s not necessarily due to pain. Babies who have become averse to feeding will behave in this tense or distressed manner regardless of the cause.
Feeding-averse babies often feed better or well when drowsy or during light sleep. When drowsy or asleep, a baby is not fully aware that he is being fed, and therefore he’s not on edge in anticipation of whatever it is that is causing him to fear feeding. In a drowsy or sleepy state, a hungry baby’s guard is down, instincts kick in, and he feeds well. A feeding-averse baby may refuse and fight feedings while awake but could complete a full feed without resistance when drowsy or asleep. (See other reasons for sleep-feeding.)
Accepting water from a bottleA small percentage of feeding-averse babies willingly accept water from a bottle but not milk. This causes parents to believe it’s the taste of the milk that baby objects to, which could be the case, but not necessarily so. It can be because the baby associates the taste of the milk with an unpleasant or stressful experience, for example, being pressured to feed.
Parents often pressure their baby to drink milk from a bottle but seldom pressure their baby to take water from the bottle. Babies are smarter than we give them credit for. They learn to link the taste of the milk with being pressured and therefore react as soon as they taste the milk.
Why babies become averse to feedingA baby could develop an aversion to feeding if an event occurring directly before, after, or while he is feeding triggers negative emotional responses, such as stress, pain, fear, or disgust. Several scenarios could potentially trigger such emotions. For example:
StressIf a baby is pressured or forced to feed against his will, this makes for an annoying, frustrating, or stressful experience depending on the feeding strategies parents employ, and how long they persist.
Being repeatedly pressured to feed against their will is without exception THE most common reason for babies to develop an aversion to feeding and then not want to eat. In most cases, it's the original and only cause of a baby's feeding aversion. However, in around 10 percent of cases, it's a secondary cause that develops after the baby's initial feeding refusal due to one or more of the reasons that follow.
In most cases, it's the original and only cause of a baby's feeding aversion. However, in around 10 percent of cases, it's a secondary cause that develops after the baby's initial feeding refusal due to one or more of the reasons that follow.
Sucking could be painful if a baby has mouth ulcers, and swallowing could be painful if a baby is suffering from esophagitis caused by acid reflux, or milk protein allergy. Chronic constipation or gastroparesis (delayed emptying of the stomach) could also cause a baby to associate eating with discomfort.
When a baby refuses to feed due to discomfort or pain, the parent might then pressure their baby by employing subtle or obvious forms of pressure to make him eat. This adds to the baby’s distress. The baby now has two reasons to want to avoid feeding – pain and the stress associated with being pressured to eat. It’s often the stress associated with being repeatedly pressured to feed that continues to reinforce the baby’s avoidant feeding behavior long after medications or dietary changes have removed pain from the feeding experience.
Medical procedures involving the baby's face or mouth, like nasal or oral suctioning, insertion of an NG (nasogastric) feeding tube, or intubation can be frightening, painful, and stressful.
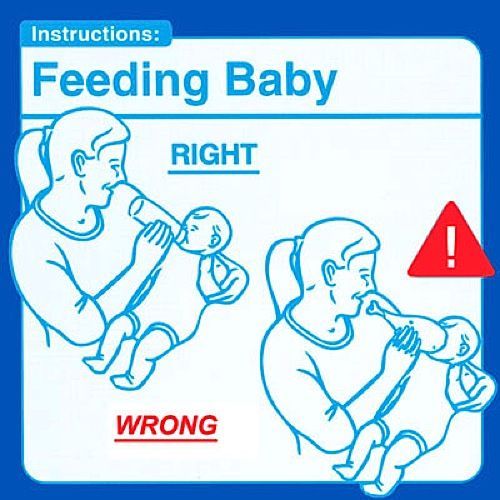
Aspirating fluids or choking on solids would make for a frightening experience. A baby could aspirate owing to dysphagia (an uncoordinated sucking-swallowing pattern) or due to moderate or severe laryngomalacia (floppy vocal cords), or because the flow rate from the nipple of a bottle or breast is too fast, or due to poor head or bottle positioning negatively impacting on the baby’s latch, suction, and sucking and swallowing coordination, or when the parent persists in trying to make their baby eat while he is crying in distress.
Disgust at taste of milk or medicinesBeing forced to take foul-tasting medicines or milk (which can be the case for hypoallergenic formula or if a mother produces high levels of lipase in her breastmilk) could cause the baby to develop an aversion to feeding. If medications are added into a baby’s milk bottle, which then changes the flavor of the milk, or if given via a nipple-like device this could cause a baby to reject bottle-feeds. Parents often resort to pressure or force to get their baby to swallow something that tastes unpleasant, adding another reason for the baby to want to avoid feeding, or anything else the parent might try to place into his mouth.
If medications are added into a baby’s milk bottle, which then changes the flavor of the milk, or if given via a nipple-like device this could cause a baby to reject bottle-feeds. Parents often resort to pressure or force to get their baby to swallow something that tastes unpleasant, adding another reason for the baby to want to avoid feeding, or anything else the parent might try to place into his mouth.
Babies affected by a sensory processing disorder may find the sensation of the nipple, or anything else in their mouth, to be abhorrent. They can display aversive behavior to lumps in food or the smell, taste, or feel of certain foods.
The cause of an infant feeding problem could be due to one or a combination of different causes. A feeding aversion can become even more complex when other feeding problems are involved. (See bottle-feeding problems.)
Other reasons for why your baby won't take a bottle, breast or solidsThere are several other possible reasons for individual babies to display aversive behavior towards breastfeeding, bottle-feeding, or eating solid foods. Any situation that results in a baby becoming frightened, stressed or experience pain while feeding has the potential to trigger partial or complete food refusal.
Any situation that results in a baby becoming frightened, stressed or experience pain while feeding has the potential to trigger partial or complete food refusal.
A single occurrence of one of these events doesn't usually trigger an aversion, but it is possible, especially if the experience is traumatic for the baby. It would generally take repeated occurrences while feeding to cause a baby to become averse to feeding. When such episodes are repeated, the baby learns to link the sequence of events and expect a similar occurrence each time he feeds. And so, he tries to avoid feeding to avoid the situation that has caused him fright, stress, or pain in the past. It's at this stage he will react before the event because he knows what's going to happen. And so, he may become distressed as soon as he recognizes he is about to be offered a feed. Or even if he thinks he is about to be fed because of the position he is held.
Is pain the cause for your baby's feeding refusal?The distress displayed by many feeding-averse babies can be so intense that it appears like they are suffering from pain. Therefore, pain is typically the first thing blamed by parents, and by health professionals during brief consultations, when other causes for a baby's feeding refusal are not obvious. However, pain is not the only reason for babies to become distressed during feeds.
Therefore, pain is typically the first thing blamed by parents, and by health professionals during brief consultations, when other causes for a baby's feeding refusal are not obvious. However, pain is not the only reason for babies to become distressed during feeds.
So how can you tell if pain is the cause of your baby’s troubled feeding behavior?Check how he behaves at times outside of feeding as this will provide clues. For example:
- If your baby is happy once you stop trying to feed him, pain is unlikely. Pain fades away. It doesn't suddenly cease because the feed has ended.
- If your baby is content between feeds, pain is unlikely. Discomfort associated with acid reflux or milk protein allergy or intolerance, constipation or gastroparesis is not restricted to feeding times only. Your baby would display signs of discomfort or distress at other times in addition to feeding times.
- If your baby predictably feeds well in certain situations, for example during the night or while drowsy or asleep, pain is unlikely to be the cause of his oppositional feeding behavior.
 Sleep does not numb a baby to the sensation of pain. If it is painful for him to feed during the day or while awake, it’s reasonable to expect it would also be painful for him to feed at night or when sleep-feeding.
Sleep does not numb a baby to the sensation of pain. If it is painful for him to feed during the day or while awake, it’s reasonable to expect it would also be painful for him to feed at night or when sleep-feeding.
NOTE: If your baby displays any unusual signs that might indicate illness or a physical problem, or if you are worried that your baby is suffering from pain, have him examined by a doctor.
Conflicted feeding behavior where baby takes a few sucks, sharply turns away or arches back, cries, quickly returns and wants to suck again, takes a few sucks, turns away or arches back, cries, returns to feeding and so on, is often interpreted by parents and others as pain, but its not necessarily due to pain. Babies who have become averse to feeding will behave in this way regardless of the cause. If your baby is quickly soothed once the feed has ended, it's probably not pain.
Is pressure the cause of your baby's feeding refusal?Some parents will pressure or force their baby to feed out of loving concern for their baby’s physical wellbeing. They hate doing this but do so because they worry that their baby will fail to gain sufficient weight or become unwell if they don’t make sure he consumes what they believe, or have been told, is an acceptable amount of milk or food.
They hate doing this but do so because they worry that their baby will fail to gain sufficient weight or become unwell if they don’t make sure he consumes what they believe, or have been told, is an acceptable amount of milk or food.
Many of the feeding strategies that we believe are ‘encouraging’ or ‘supporting’ a baby to eat involve subtle forms of pressure. For example:
- Pushing the nipple into a baby’s mouth against his wishes.
- Preventing him from pushing the nipple out of his mouth with his tongue.
- Following his head with the bottle when he turns or arches back in tense manner.
- Restraining his head to prevent him from turning away.
- Restraining his arms to prevent him from pushing the bottle away.
- Offering repeatedly at a time when he's rejecting or upset.
- Upwards pressure under his chin in a bid to trigger his sucking reflex.
- Gently compressing his cheeks to apply pressure on his buccal pads (cheek pads).

- Jiggling or twisting the bottle to try and make him continue sucking.
- Squeezing milk into his mouth.
- Trying to trick him into accepting the nipple by switching his pacifier for the nipple.
If these things don’t upset your baby - which generally appears to be the case for babies under the age of eight weeks who due to immaturity have limited ability to complain during the feed but can after the feed – such strategies might be causing no harm. However, doing these things in a bid to control how much a baby eats has the potential to make the experience of feeding unpleasant or stressful for the baby. When repeated, a baby can develop an aversion to feeding.
As a result of developing a feeding aversion the baby will fuss or refuse to feed and the parents, not knowing any better, may then feel compelled to force their baby to eat, and by doing so they may be unknowingly reinforcing their baby’s feeding aversion.
Behavior that is reinforced will continue. Once averse to feeding, the situation spirals downwards as a result of the ‘fear-avoidance-cycle’.
Once averse to feeding, the situation spirals downwards as a result of the ‘fear-avoidance-cycle’.
The more the parent pressures their baby, the less their baby is willing to eat. The less their baby eats, the more the parent pressures. And around and around it goes. The 'fear-avoidance-cycle' can spiral downwards to complete feeding refusal while awake, poor growth, and possible hospitalization where a feeding tube might be inserted.
Direct and indirect reinforcementsAny pressure, even subtle forms, has the potential to directly reinforce a feeding aversion. However, there are other strategies, for example feeding a baby while sleeping, giving solids to compensate for the loss of calories from milk, providing milk in other ways such as spoon, syringe, or feeding tube, can indirectly reinforce a behavioral feeding aversion by enabling the baby to avoid feeding while awake during the day. All reinforcements – direct and indirect – need to be removed.
Medical treatments
A feeding-averse baby is often distressed at feeding times (an exception being those who mostly sleep-feed during naps and at night). Pain is typically the first thing blamed, but the least likely cause of aversive feeding behavior displayed by physically well, thriving babies.
If you go to the doctor with a fussy baby who cries and refuses to eat, he or she may tend to explore physical causes before all others. The following treatments are often recommended by medical practitioners in a bid to remedy a baby's fussy or distressed feeding behavior.
Medications: Acid suppressing medications may be prescribed to treat suspected esophagitis - inflammation of the baby’s feeding tube caused by repeated exposure to refluxed stomach acid. And perhaps prokinetic medication (also called propulsive agents) to treat gastroparesis - delayed emptying of the stomach.
Dietary changes: A hypoallergenic infant formula may be recommended to treat suspected eosinophilic esophagitis - inflammation caused by an allergic reaction to cow’s milk based infant formula or soy infant formula.
Once the condition causing the baby's discomfort is effectively treated, his troubled feeding behavior will fade and disappear.
NOTE: A doctor cannot see into a baby’s esophagus and therefore cannot confirm if he is suffering from esophagitis during a routine medical examination. h3 antagonists and proton pump inhibitors used in the treatment of acid reflux are extremely effective in reducing the production of stomach acid. If your baby is still fussing or fighting feeds two weeks after commencing medications, there's a good chance that acid reflux is not responsible for his troubled feeding behavior. Similarly, if your baby's avoidant feeding behavior continues two weeks after switching to a specialized hypoallergenic formula, the reason may be that milk protein allergy is not the cause. This does not imply that your baby is not affected by these conditions, rather that these conditions are unlikely to be the cause of his avoidant feeding behavior.
This does not imply that your baby is not affected by these conditions, rather that these conditions are unlikely to be the cause of his avoidant feeding behavior.
Band-Aid solutions: If medications and dietary change fail to resolve a baby's aversive feeding behavior, band-aid solutions such as high-calorie feeds, food thickeners, starting solids, sleep-feeding, might be recommended in an attempt to minimize the risk of poor growth caused by an unresolved feeding aversion. However, band-aid solutions are often ineffective in the case of a feeding aversion because they do not address the cause, which is the stimulus that is causing the baby to fear feeding.
If medical treatments fail to resolve your baby's feeding issues, consider the possibility of a misdiagnosis or that there is more than one cause involved. And extend your search to cover other potential causes, in particular behavioral reasons such as being pressured to eat.
Speech therapyIf your baby often chokes or experiences problems with aspiration while feeding, his doctor might refer him to a speech therapist to assess his ability to suck and swallow effectively. This can be helpful if choking episodes are reinforcing the baby's aversive behavior.
This can be helpful if choking episodes are reinforcing the baby's aversive behavior.
However, if your baby feeds well at some feeds for example in a sleepy state or has fed well in the past before developing a feeding aversion, it's unlikely that the source of his fussy feeding behavior or food refusal is due to a sucking or swallowing problem.
Occupational therapyIf an oral aversion due to a sensory processing disorder is suspected, your doctor might refer your baby to an occupational therapist for an assessment. Encouraging a child with oral aversion occurring due to a sensory processing disorder to feed as normally as possible requires a very long process that may last months or years.
An oral aversion is wide ranging with the baby not wanting anything near his mouth. A feeding aversion is specific, related to feeding, and requires very different treatment to resolve the problem compared to an oral aversion
NOTE: Some of the feeding strategies recommended to resolve an oral aversion, such as placing rubbery implements into the baby’s mouth to ‘desensitize’ him to the feel of things in his mouth, are counterproductive in the case of a behavioral feeding aversion that developed or is currently reinforced as a result of being pressured to feed. Placing things into a baby’s mouth without his permission will not regain his trust. Hence, the diagnosis must be correct. If your baby is happy to have anything other than the nipple of a bottle or food in his mouth, it’s probably a feeding aversion rather than an oral aversion.
Placing things into a baby’s mouth without his permission will not regain his trust. Hence, the diagnosis must be correct. If your baby is happy to have anything other than the nipple of a bottle or food in his mouth, it’s probably a feeding aversion rather than an oral aversion.
A behavioral approach views challenging infant behaviors such as incessant crying, fussy feeding behavior, feeding refusal, and sleeping problems in the context of the care the baby receives. In the case of physically well babies, it’s not assumed that the baby has a physical problem, rather the parent’s childcare practices are examined.
Infant behavior, whether this is desirable or undesirable behavior, is reinforced by the actions parents take or don’t take. To resolve a behavioral problem, and thus change a healthy baby’s behavior from fussy, distressed feeding refusal to enjoying feeding to satisfaction, it’s necessary for the parent to first make appropriate changes to their childcare practices.
The parent’s infant feeding practices are the last suspected cause of a healthy baby's aversive feeding behavior when it should be one of the first. You will know how thoroughly your baby’s healthcare professionals have assessed the possibility of behavioral reasons for his feeding issues by the number of questions asked of you regarding his feeding history. For example, feeding equipment, feeding frequency and duration, milk type, and concentration, feeding pattern, total daily milk intake, his sleeping patterns (sleep has a profound effect on feeding behavior and milk intake) and most important of all, your infant feeding and sleep settling practices. Our Baby Care Advice questionnaire includes 80+ questions to pinpoint the cause.
No questions asked = minimal to no consideration given to behavioral causes.
MisdiagnosisAccurate identification of the cause is essential to finding an effective solution. This is not something that can be achieved during a brief consultation with a health professional. And it definitely cannot be achieved without asking the parents multiple questions about their infant feeding practices. An accurate, and thorough diagnosis of the cause, or causes as is often the case, requires a comprehensive understanding of infant development and behavior, and age-appropriate infant feeding practices, as well as an understanding of the reasons and solutions to infant feeding aversion. At Baby Care Advice we allocate 2 hours for feeding problems.
And it definitely cannot be achieved without asking the parents multiple questions about their infant feeding practices. An accurate, and thorough diagnosis of the cause, or causes as is often the case, requires a comprehensive understanding of infant development and behavior, and age-appropriate infant feeding practices, as well as an understanding of the reasons and solutions to infant feeding aversion. At Baby Care Advice we allocate 2 hours for feeding problems.
Misdiagnosis occurs when assumptions are made about the cause in the absence of a comprehensive feeding assessment. Failure to accurately identify the stimulus causing and reinforcing the baby's feeding aversion - which can vary for individual babies - is likely to result in an ineffective treatment plan.
Not only will a misdiagnosis fail to address the cause, but many of the strategies recommended based on a misdiagnosis, such as those described as indirect reinforcements, have the potential to reinforce a baby’s aversive feeding behavior. A baby’s feeding aversion will continue while it’s reinforced. An unresolved breast- or bottle-feeding aversion increases the risk of the baby developing an aversion to eating solids for the same reasons. Feeding issues can persist for weeks, months or years.
A baby’s feeding aversion will continue while it’s reinforced. An unresolved breast- or bottle-feeding aversion increases the risk of the baby developing an aversion to eating solids for the same reasons. Feeding issues can persist for weeks, months or years.
Few health professionals are familiar with age-appropriate infant feeding practices and/or the process involved in resolving behavioral feeding aversions experienced by normal developing babies and young children. Therefore, they are ill-equipped to guide and support parents to resolve this complex and highly stressful situation.
A baby's avoidant feeding behavior, poor milk intake, and poor growth could be due to one or a combination of the causes already mentioned. However, a feeding aversion can become even more complex if other feeding issues are involved. For example, unsuitable or faulty equipment, poor feeding position, or the parent’s providing an inappropriate response to their baby’s feeding cues. (See bottle-feeding problems for more.)
(See bottle-feeding problems for more.)
If you suspect that your baby has developed a feeding aversion, there are a couple of ways we can help.
You might choose to see if you can figure things out on your own as a result of being guided by my book 'Your Baby’s Bottle-feeding Aversion’.
You might prefer to have one of our experienced consultants undertake a comprehensive assessment of all causes and provide individualized feeding advice. You also have the option to receive daily email guidance and support as you work towards resolving your baby’s feeding aversion.
You can purchase Rowena's Online Bottle-Feeding Aversion Program - six modules with clear step by step instructions on how to overcome your baby's bottle-feeding aversion. With a 95% success rate using Rowena's Bennett's method.
‘Your Baby's Bottle-Feeding Aversion’ bookIn my book, ‘Your baby’s Bottle-feeding Aversion’, I have described physical and behavioral reasons for babies to develop an aversion to bottle-feeding. How to identify the cause and the solutions to match. Included are step-by-step instructions on how to regain your baby’s trust and resolve a feeding aversion caused or reinforced by repeated pressure to feed.
How to identify the cause and the solutions to match. Included are step-by-step instructions on how to regain your baby’s trust and resolve a feeding aversion caused or reinforced by repeated pressure to feed.
While the book was written for bottle-fed babies, many nursing mothers have found that applying the same strategies has also helped them to successfully resolve a breastfeeding aversion.
You might find that reading this book is all you need to do to understand the steps you need to take to resolve your baby’s feeding aversion and get him back to the point of enjoying eating until satisfied.
Baby Care Advice ConsultationsIf you would like an individualized assessment of all reasons for infant feeding problems, not just feeding aversion, we also provide a consultation service. Baby Care Advice consultants have extensive experience in pinpointing the cause of feeding aversion and other behavioral feeding problems such as those related to equipment and the parent’s feeding practices. (For more on what’s included in a consultation).
(For more on what’s included in a consultation).
Six time-saving modules to help your family enjoy feeding again with Rowena's step-by-step plan. Enjoy additional tools to manage anxiety, troubleshoot any issues, introduce new carers, how to manage illness/teething and much more.
Join Our Facebook Support CommunityBaby Care Advice has facebook support groups in various languages, for those who have purchased either Rowena's 'Your Baby's Bottle-Feeding Aversion' book/ Online program/ consultation. They are made possible by a volunteer group of parents, who offer empathetic, compassionate support and guidance as you work your way through resolving your baby's feeding aversion.
English
Spanish
Dutch
Romanian
By Rowena Bennett, RN, RM, CHN, MHN, IBCLC.
Written Sept 2013. Revised July 2021.
Copyright www. babycareadvice.com 2021. All rights reserved. Permission from the author must be obtained to reproduce all or any part of this article.
babycareadvice.com 2021. All rights reserved. Permission from the author must be obtained to reproduce all or any part of this article.
Bottle-Feeding – Baby Care Advice
Tongue-tie is relatively common. Many babies, children, and adults have a tongue-tie to varying degrees. For the vast majority, it causes no ill effects on feeding or speech.
Read more
Having a baby with a Bottle Aversion stripped me of everything. It stripped me of my confidence, my identify, my belief in myself as Claire and as Mum, but most devastatingly it stripped me of my relationship with you, my beautiful Sofia.
Read more
Is your baby rejecting/ refusing a bottle? When your baby squirms, appears uncomfortable during feed, fusses, cries or refuses to eat, it can be challenge to figure out the cause. The timing and type of behavior she exhibits provides vital clues. This article discusses potential reasons for why your baby won't take a bottle.
The timing and type of behavior she exhibits provides vital clues. This article discusses potential reasons for why your baby won't take a bottle.
Read more
Does your baby refuse a bottle or refuses breastfeeding? You’re wondering why your baby won't take a bottle. Feeding a baby should be an enjoyable experience for all involved, however when baby repeatedly refuses to feed despite being hungry this makes feeding a frustrating and stressful experience for all involved. Identifying the cause of why your baby is rejecting feeds is essential to the solution.
Read more
It’s obvious when a bottle-fed baby is not drinking as much milk as expected. But does this mean she’s not drinking enough? Maybe ‘yes’. Maybe ‘no’. This article explains how to tell if your baby is underfeeding and the various reasons why babies don’t drink enough milk.
But does this mean she’s not drinking enough? Maybe ‘yes’. Maybe ‘no’. This article explains how to tell if your baby is underfeeding and the various reasons why babies don’t drink enough milk.
Read more
Infant overfeeding is a common problem, particularly for newborn bottle-fed babies. It’s a problem that is frequently overlooked because of the flawed assumption that only fat babies are overfed babies and because of false claims that it’s not possible to overfeed a baby. As a result, gastro-intestinal symptoms linked to overfeeding can be mistakenly attributed to conditions such as colic, reflux, or milk allergy or intolerance.
Read more
As a parent of a bottle-fed baby, you might worry that he’s not eating enough or that he could be getting too much. This article explains how to estimate the amount your baby needs and reasons why some babies require more and some less than others.
This article explains how to estimate the amount your baby needs and reasons why some babies require more and some less than others.
Read more
We all appreciate that young babies have tiny tummies and are growing at a rate that is faster than any other time in their lives. Hence, they need to eat often. However, when parents express concern about their ‘hungry baby’ this refers to a baby that appears to be excessively hungry, who demands feeds more often than expected, or is eating well above the recommended volume of milk for a baby of his age and size.
Read more
If your formula-fed baby is irritable, wakeful or refuses to feed at times, this may cause you to wonder if her baby formula is the cause. You might be considering switching formula but are unsure which to choose. This article may help you to select the most suitable formula for your baby.
You might be considering switching formula but are unsure which to choose. This article may help you to select the most suitable formula for your baby.
Read more
How fast your baby feeds can affect how much milk he drinks, how much air he swallows, and his enjoyment of feeding. Feeding too quickly or slowly can cause problems. Discover how you can influence how long it takes for your baby to feed.
Read more
Feeding times provide a wonderful opportunity to enhance the special bond you have with your baby. Learn how to make feeding times an enjoyable and satisfying experience for your baby.
Read more
If your baby displays fussy feeding behavior, you might start to wonder if the bottle or nipple is to blame. How do you know if the equipment your baby is using is the best choice for your baby? This article explains what to look for when purchasing baby bottles and nipples.
How do you know if the equipment your baby is using is the best choice for your baby? This article explains what to look for when purchasing baby bottles and nipples.
Read more
Solving five breastfeeding problems after the first month
Expert advice on solving the top five breastfeeding problems that may arise after the first month.
Share this information
Cathy Garbin, child health nurse, midwife and lactation consultant:
Cathy, a mother of two, was a research fellow at the renowned Human Lactation Research Institute, founded by Peter Hartmann, for seven years, providing support to breastfeeding mothers in clinics and at home. Today, she still works as a family counselor, and also conducts seminars for attending physicians and speaks at international conferences.
You and your baby have already fully established the process of breastfeeding and know what and how to do. It seems that all difficulties are left behind. However, some more surprises await you. The following are suggestions for dealing with breastfeeding problems that may arise later.
It seems that all difficulties are left behind. However, some more surprises await you. The following are suggestions for dealing with breastfeeding problems that may arise later.
Problem #1. I need to be away from my baby
Whether it's social events, travel or medical treatment, at some point you may need to be away from your baby for a while.
Solutions
- Express milk so that someone else can feed the baby. Now that breastfeeding is established, you can express and store your breast milk in the refrigerator or freezer. Try different options to find the most convenient time for pumping in your daily routine. Some mothers manage to pump more breast milk in the morning when the baby wakes up after a long night's sleep. For others, it's best to express 60 minutes after feeding. Remember that everyone is different. Don't be discouraged if you don't get enough milk the first time: it's possible that you'll be able to express enough for one feeding in just two or three pumpings.
 As with feeding, it may take time for your body to adjust to pumping.
As with feeding, it may take time for your body to adjust to pumping. - Take your breast pump with you, if you plan to skip a feed. Even if you leave your baby with expressed milk, but will be absent for more than two hours, you will need to empty your breast. Pump at the same frequency as you would breastfeed your baby. This will support milk production and prevent discomfort. Express milk regularly throughout the day without waiting for your breasts to overflow. 1 Most electronic breast pumps are battery operated, so you don't have to find an outlet nearby.
Problem #2. How to continue breastfeeding after returning to work?
You will likely have to leave your baby more often and for longer when you go to work, so it's especially important to find ways to continue breastfeeding and pumping that work for both of you. As mentioned above, you can build up a supply of breastmilk before you go to work and then pump regularly to support milk production, prevent discomfort, and make sure your baby has enough pumped milk the next day.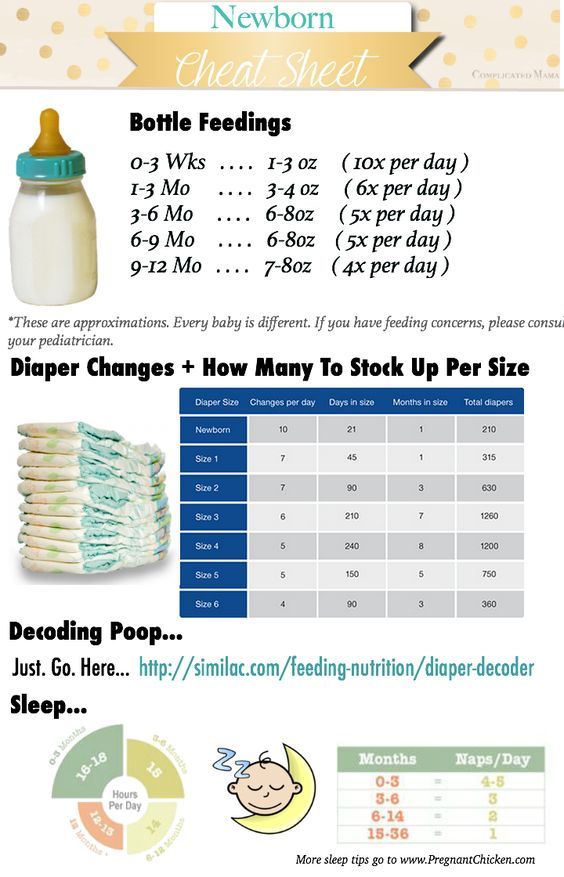 Many companies now provide dedicated pumping rooms, and modern breast pumps work efficiently and reliably. If you have a regular work schedule or work part-time, you can still breastfeed your baby before and after work and at night.
Many companies now provide dedicated pumping rooms, and modern breast pumps work efficiently and reliably. If you have a regular work schedule or work part-time, you can still breastfeed your baby before and after work and at night.
Solutions
- Express as often as you would feed your baby. This will help maintain milk production and prevent discomfort, as well as reduce the risk of clogged milk ducts, mastitis and breast swelling. 1
- Try double pumping. Double pumping not only takes half the time, but also produces an average of 18% more milk than pumping from each breast in sequence. Milk is more nutritious and has a higher fat content. 2
- Assemble and bring to work the set, which includes a breast pump, milk storage bags and, if desired, a bustier top for hands-free pumping. You will also need a cooler bag to carry your expressed milk.
- Know your rights.
 In many countries, the law allows women to express and safely store breast milk at work. Discuss these options with your employer before returning to work. This will get you both ready.
In many countries, the law allows women to express and safely store breast milk at work. Discuss these options with your employer before returning to work. This will get you both ready.
Problem #3. It seems to me that the baby suckles only for pleasure
Sometimes you may feel that the baby takes your breast in order to calm down, and not to eat. However, do not forget that breastfeeding is not only nutrition, it is also comfort for your baby. "Soothing suckling" (when the baby suckles but does not eat milk) helps the baby to calm down and relax. Remember that a sudden increase in the frequency or duration of feedings may indicate insufficient milk production. However, if the baby continues to gain weight and you use enough diapers a day, this is unlikely.
Solution
- Be patient. The baby needs your care - listen to his needs and support him. Usually, the period of soothing suckling does not last too long, but it allows the child to feel your love and protection - and this is the best thing you can give him.
Problem #4. I want to switch from mixed to exclusive breastfeeding
Breastfeeding is so good for you and your baby that it's worth trying to fight for it. However, if you have rarely fed lately, your milk production may have been reduced. If your baby has only been mixed-fed for a couple of weeks, you will most likely be able to restore enough milk. Contact a lactation consultant or medical specialist who will help you and give you the necessary advice. This is a very individual process that depends on many factors. In any case, do not despair, because every drop of your milk is important for the child.
Solutions 1.3
- Increase milk production. Try to put the baby to the breast more often, because the more milk the baby consumes, the more milk is produced. You can also express milk additionally. As mentioned earlier, double pumping in particular helps increase milk production.
- Be in physical contact with your baby as much as possible.
 As in the first days after childbirth, close physical contact with the baby promotes the production of the hormone oxytocin, which in turn triggers milk production. It will also make both of you feel more calm and relaxed.
As in the first days after childbirth, close physical contact with the baby promotes the production of the hormone oxytocin, which in turn triggers milk production. It will also make both of you feel more calm and relaxed. - Reduce the number of formula feedings gradually. Resist the urge to stop supplementing with formula right away. If you gave your baby formula after each breastfeed, start giving it every other time until milk production rises. Keep a close eye on the number of soiled diapers and weight gain during this transition period. It is likely that at first the child will ask for the breast more often, and this is absolutely normal.
- Speak with a lactation consultant or healthcare professional. He will be able to help you and strengthen your confidence that your baby gets everything he needs.
Problem #5. My child has lost interest in the breast
If your child, who always ate with appetite, suddenly began to refuse the breast for no apparent reason, this is a false refusal, the so-called "strike". You may assume that he is ready to switch to solid foods, or that he does not like your milk anymore, but this is most likely not the case. It's just that the child develops vision, and now he is more distracted by the world around him. Or maybe something frightened the child during feeding, or he reacts to a violation of the regimen, perhaps he has a stuffy nose or teething. What you take for lack of interest may actually mean that your baby has simply learned to breastfeed more effectively and therefore takes less time to suckle.
You may assume that he is ready to switch to solid foods, or that he does not like your milk anymore, but this is most likely not the case. It's just that the child develops vision, and now he is more distracted by the world around him. Or maybe something frightened the child during feeding, or he reacts to a violation of the regimen, perhaps he has a stuffy nose or teething. What you take for lack of interest may actually mean that your baby has simply learned to breastfeed more effectively and therefore takes less time to suckle.
Solutions
- Be patient. False rejection is usually temporary and goes away after a few days. To provide the baby with the necessary nutrition during this period, give him expressed milk.
- Find a quieter feeding area with as few distractions as possible. Baby is more likely to eat better if he can relax and focus on his chest.
- Check in which position you feed.
 The baby may refuse to breastfeed if he is uncomfortable or unable to move his head to breathe during feeding.
The baby may refuse to breastfeed if he is uncomfortable or unable to move his head to breathe during feeding. - Express milk to keep it flowing . You can try feeding your baby with expressed breast milk using the Medela Calma smart pacifier.
- Do not start formula or solid foods. Supplementing with formula can lead to reduced milk production and will only make matters worse. If your baby is regularly fed with expressed milk and is growing well, and the number of soiled diapers is normal, try not to worry. If the baby is less than six months old, you should not give him solid food: his digestive system is not yet strong and may not be ready for such a load.
- Do not force-feed. Try to relax and be in skin-to-skin contact with your baby as much as possible, hug him and often offer the breast so that he can take it on his own. The release of oxytocin that body contact triggers will also help you pump.
 4
4
Related content: Breastfeeding: what to expect after the first month
Literature
1 Kent JC et al. Principles for maintaining or increasing breast milk production. J Obstet , Gynecol , & Neonatal Nurs . 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Breast Milk Production". G Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
2 Prime DK et al. Simultaneous breast expression in breastfeeding women is more efficacious than sequential breast expression. Breast Med . 2012;7(6):442-447. - Prime D.K. et al., “During the breastfeeding period, pumping both breasts simultaneously is more productive than sequential pumping.” Brest Med (Breastfeeding Medicine). 2012;7(6):442-447.
3 Amir L. Breastfeeding managing ‘supply’ difficulties. Aust fam physician . 2006;35(9):686. - Amir L., "Breastfeeding: Problems of 'Supply'. Aust Fam Physical. 2006;35(9):686.
Aust fam physician . 2006;35(9):686. - Amir L., "Breastfeeding: Problems of 'Supply'. Aust Fam Physical. 2006;35(9):686.
4 Moberg KU, Prime DK. Oxytocin effects in mothers and infants during breastfeeding. Infant . 2013;9(6):201-206. - Moberg KW, Prime DK, "The effects of oxytocin on mother and child during breastfeeding." Infant. 2013;9(6):201-206.
Breast Care while Breastfeeding
Reading Time: 4 min
Breastfeeding is an unforgettable experience, full of tenderness for the baby, however, at this time, unpleasant moments can also occur, such as sensitivity and sore nipples. Such inconvenience is experienced by many nursing mothers. This guide will help you properly care for your breasts in case of discomfort.
Is it normal to have sore breasts while breastfeeding?
Breastfeeding is different for every woman, but you might want to know what feels normal in your breasts.
Remember that it is normal for a little soreness or tenderness in the nipples when your baby is first attached to the breast and during the first feedings. On the other hand, if soreness and sensitivity do not recede in the future, this is an occasion to turn, for example, to a lactation consultant for advice.
Advice
Don't put up with the pain of breastfeeding. In truth, the sooner you seek help, the more likely you are to be free of breastfeeding discomfort for months to come. Therefore, be sure to contact a specialist as soon as you feel discomfort.
Common Causes of Breast Discomfort
Before jumping straight into breast care, let's look at the main causes of sore and sore nipples.
Incorrect latch on of the nipple
At the moment of attachment to the breast, the baby may not open his mouth wide enough, and because of this, incorrect latch on of the breast occurs, the baby suckles only the nipple - this leads to painful sensations and the appearance of cracked nipples
Inverted nipples
Up to 10% of women have inverted or flat nipples, making breastfeeding a little more difficult.
Mastitis and breast thrush
Some breastfeeding mothers also experience infections such as mastitis and breast thrush.
Tongue shortening
If the tissue that connects the baby's tongue to the floor of the mouth is shorter than usual, it may cause improper nipple latch.
How to reduce soreness
If you experience discomfort and soreness in the nipples during feeding, this does not mean that you have to stop breastfeeding. Here are some ways to reduce soreness and protect your nipples so you can breastfeed comfortably.
- Check the correct attachment of the baby to the breast and correct if necessary.
- After feeding, apply a special cream to the nipples.
- Protect your nipples from chafing between feeds with breast pads.
- Keep your nipples dry with bra pads.
- To reduce soreness during breastfeeding, use silicone nipple shields.

See below ↓
Breastfeeding Basics:
- after childbirth, the mammary glands increase in size and become heavier. Therefore, it is necessary to choose a bra that will support them. The bra should be comfortable, without wires, tight cups (this can cause milk stasis), without lace and a seam in the areola area of the nipple (this can cause irritation).
- Keep your nipples dry: Use bra pads to absorb milk. Ultra-thin Philips Avent disposable earbuds are comfortable to wear both day and night. Do daily chest air baths. Leave the breast open for 10-15 minutes after feedings.
- Maintain hygiene: do not wash your breasts before and after each feeding, it is enough to shower daily or just wash your breasts no more than 2 times a day. First, the nipple is washed, then the entire mammary gland, at the end, the breast is dried with a clean towel. If you constantly wash off the secret of the mammary glands, this greatly dries out the delicate skin of the nipples and can lead to cracked nipples.

- Breast massage and compresses: Daily light breast massage and contrast shower improves blood circulation in the mammary glands. You can massage your breasts in a clockwise direction with water shower jets, or stroke both breasts at the same time in gentle circular motions, avoiding the areola of the nipples. Before feeding, you can apply a warm compress to stimulate milk flow. After feeding - cool to relieve tension and discomfort in the mammary glands. Philips Avent thermal pads are very easy to use. It is enough to hold them in hot or cold water.
Help is always at hand
As you know, breast tenderness is normal, but you don't have to put up with pain of any intensity. If pain persists, your nipples develop cracks or fluid bubbles, or you have questions, do not hesitate to contact your doctor or lactation consultant.
Discover our articles
Baby+ app
Download the app and track your baby's development and growth with trackers and keep those special moments forever.