Baby cluster feeding nhs
Breastfeeding: the first few days
In the first few days, you and your baby will be getting to know each other. It may take time for both of you to get the hang of breastfeeding.
This happens faster for some women than others. But nearly all women produce enough milk for their baby.
Preparing to breastfeed before the birth
It's good to find out as much as you can about breastfeeding before you have your baby. It may help you feel more confident when you start breastfeeding your baby.
Antenatal classes usually cover the most important aspects of breastfeeding, such as positioning and attachment, expressing, and how to tackle common breastfeeding problems.
Find antenatal classes near you.
You can find out about breastfeeding from your midwife, family and friends, and useful helplines and websites.
Find breastfeeding help and support.
There are lots of groups and drop-ins, some specially designed for pregnant women who want to know more about breastfeeding. You can find out more by asking your midwife, health visitor, local peer supporter or GP. Or visit your local Children's Centre.
Find a Sure Start Children's Centre on GOV.UK.
Skin-to-skin contact
Having skin-to-skin contact with your baby straight after giving birth will help to keep them warm and calm and steady their breathing.
Skin-to-skin means holding your baby naked or dressed only in a nappy against your skin, usually under your top or under a blanket.
Skin-to-skin time can be a bonding experience for you and your baby. It's also a great time to have your first breastfeed. If you need any help, your midwife will support you with positioning and attachment.
Skin-to-skin contact is good at any time. It will help to comfort you and your baby over the first few days and weeks as you get to know each other. It also helps your baby attach to your breast using their natural crawling and latching-on reflexes.
You'll still be able to bond with and breastfeed your baby if skin-to-skin contact is delayed for some reason, for example if your baby needs to spend some time in special care.
If necessary, your midwife will show you how to express your breast milk until your baby is ready to breastfeed. They can also help you have skin-to-skin contact with your baby as soon as it's possible.
Skin-to-skin after a caesarean
If your baby is delivered by caesarean, you should still be able to have skin-to-skin contact with your baby straight after delivery.
Colostrum: your first milk
The fluid your breasts produce in the first few days after birth is called colostrum. It's thick and usually a golden yellow colour. It's a very concentrated food, so your baby will only need a small amount, about a teaspoonful, at each feed.
It's thick and usually a golden yellow colour. It's a very concentrated food, so your baby will only need a small amount, about a teaspoonful, at each feed.
Your baby may want to feed quite often, perhaps every hour to begin with. They'll begin to have fewer, but longer feeds once your breasts start to produce more "mature" milk after a few days.
The more you breastfeed, the more your baby's sucking will stimulate your supply and the more milk you'll make.
Your let-down reflex
Your baby's sucking causes muscles in your breasts to squeeze milk towards your nipples. This is called the let-down reflex.
Some women get a tingling feeling, which can be quite strong. Others feel nothing at all.
You'll see your baby respond when your milk lets down. Their quick sucks will change to deep rhythmic swallows as the milk begins to flow.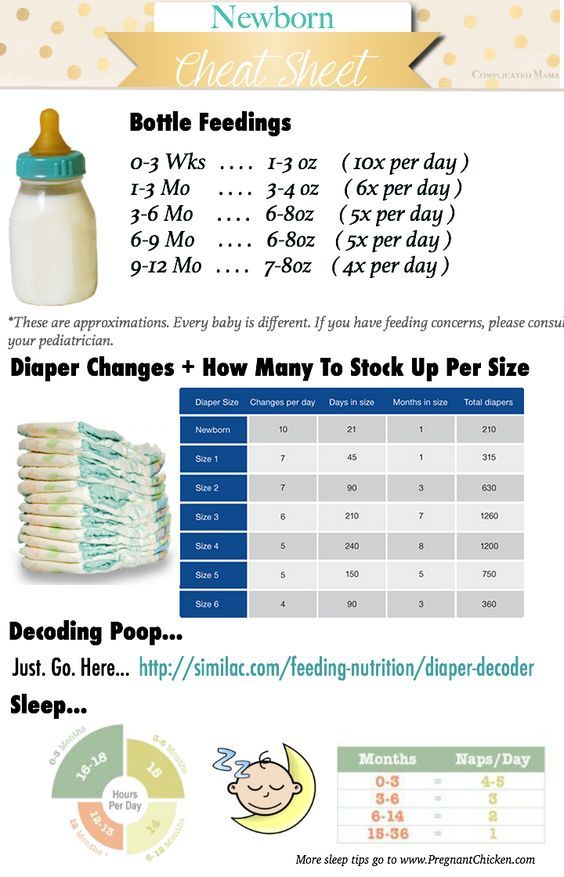 Babies often pause after the initial quick sucks while they wait for more milk to be delivered.
Babies often pause after the initial quick sucks while they wait for more milk to be delivered.
Occasionally this let-down reflex can be so strong that your baby coughs and splutters. Your midwife, health visitor or breastfeeding supporter can help with this.
If your baby seems to be falling asleep before the deep swallowing stage of feeds, they may not be properly attached to the breast. Ask your midwife, health visitor or breastfeeding supporter to check your baby's positioning and attachment.
Sometimes you'll notice your milk letting down in response to your baby crying or when you have a warm bath or shower. This is normal.
How often should I feed my baby?
In the first week, your baby may want to feed very often. It could be every hour in the first few days.
Feed your baby as often as they want and for as long as they want.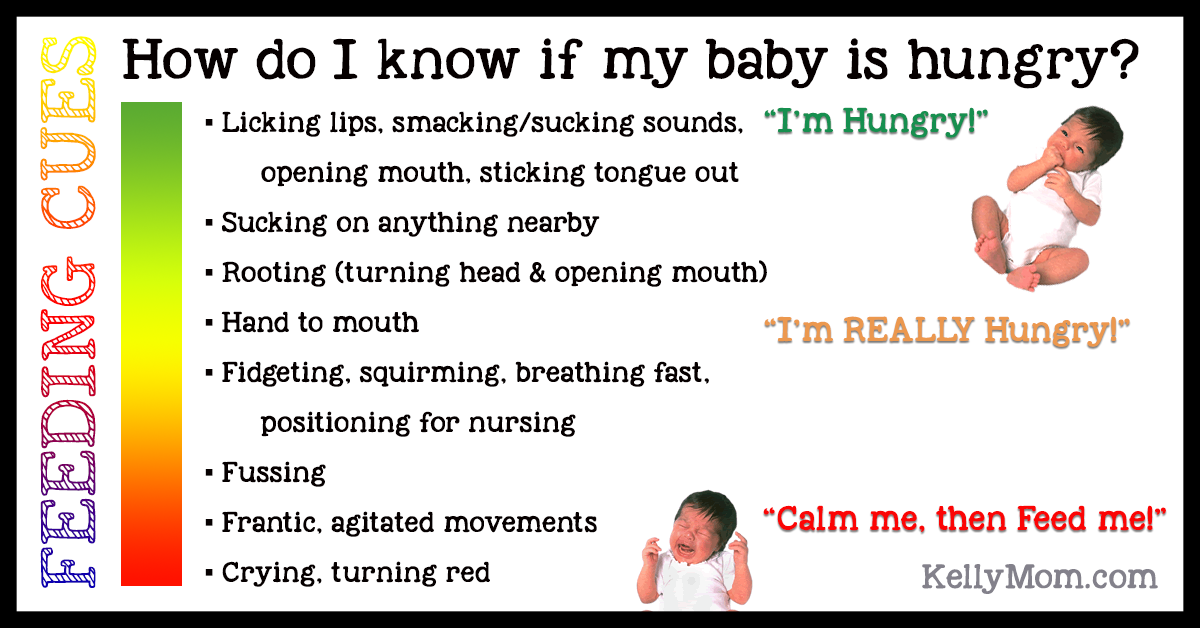 They'll begin to have fewer, but longer feeds after a few days.
They'll begin to have fewer, but longer feeds after a few days.
As a very rough guide, your baby should feed at least 8 to 12 times, or more, every 24 hours during the first few weeks.
It's fine to feed your baby whenever they are hungry, when your breasts feel full or if you just want to have a cuddle.
It's not possible to overfeed a breastfed baby.
When your baby is hungry they may:
- get restless
- suck their fist or fingers
- make murmuring sounds
- turn their head and open their mouth (rooting)
It's best to try and feed your baby during these early feeding cues as a crying baby is difficult to feed.
Building up your milk supply
Around 2 to 4 days after birth you may notice that your breasts become fuller.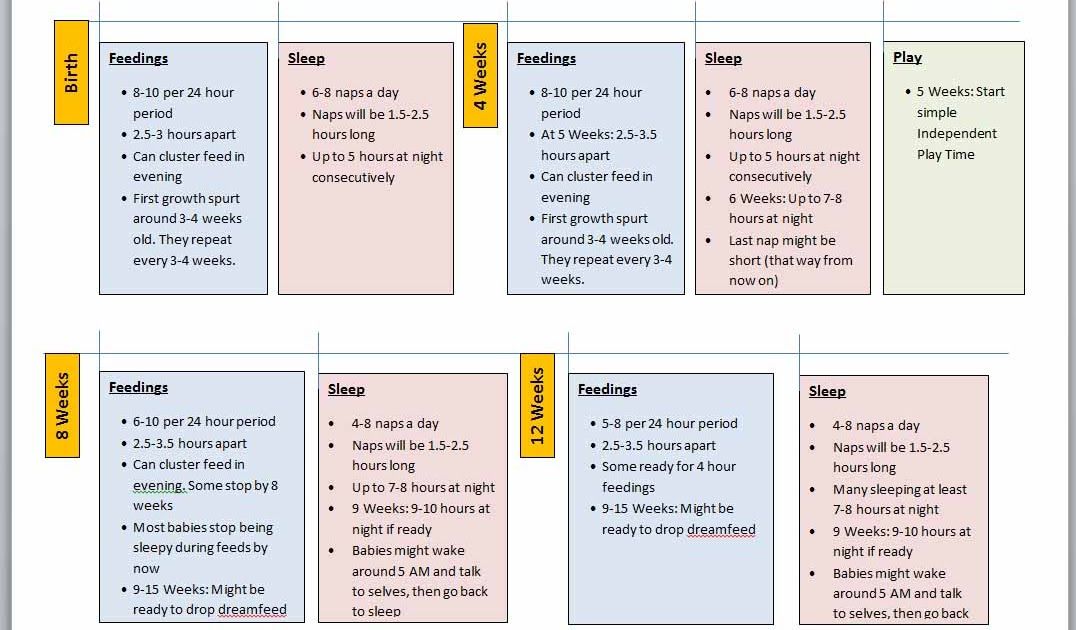 This is often referred to as your milk "coming in".
This is often referred to as your milk "coming in".
Your milk will vary according to your baby's needs. Each time your baby feeds, your body knows to make more milk for the next feed. The amount of milk you make will increase or decrease depending on how often your baby feeds.
Feed your baby as often as they want and for as long as they want. This is called responsive feeding. In other words, responding to your baby's needs. It's also known as on-demand or baby-led feeding.
In the beginning, it can feel like you're doing nothing but feeding. But gradually you and your baby will get into a pattern and the amount of milk you produce will settle down.
It's important to breastfeed at night because this is when you produce more hormones (prolactin) to build up your milk supply.
In the early weeks, before you and your baby have become comfortable with breastfeeding, "topping up" with formula milk or giving your baby a dummy can lower your milk supply.
Speak to a midwife or health visitor if you are worried about breastfeeding or you think your baby is not getting enough milk.
They might suggest giving your baby some expressed breast milk along with breastfeeding.
Find out more about how to tell if your baby is getting enough breast milk.
Dealing with leaking breasts
Sometimes, breast milk may leak unexpectedly from your nipples.
Wearing breast pads will stop your clothes becoming wet with breast milk. Remember to change them frequently to prevent an infection.
Expressing some milk may also help. Only express enough to feel comfortable as you do not want to overstimulate your supply.
Find out about expressing and storing breast milk.
If your baby has not fed recently, you could offer them a feed as breastfeeding is also about you being comfortable.
Help and support for breastfeeding
- Find out more about positioning and attachment, including how to get comfortable and make sure your baby is properly attached.
- If you are having difficulties with breastfeeding, take a look at common breastfeeding problems.
- Ask a midwife or health visitor for help. They can also tell you about other breastfeeding support available near you.
- Search online for breastfeeding support in your area.
- Call the National Breastfeeding Helpline on 0300 100 0212 (9.30am to 9.30pm daily).
Get Better Health: Start for Life pregnancy and baby emails
Sign up for Start for Life emails for expert advice, videos and tips on pregnancy, birth and beyond.
Community content from HealthUnlockedCluster Feeding Your Newborn: Helpful Tips
If you’re breastfeeding, you might find that your little one sometimes keeps you busier than usual from time to time. Occasional sudden increases in the frequency of feeds, usually caused by growth spurts, are sometimes known as cluster feeding.
Occasional sudden increases in the frequency of feeds, usually caused by growth spurts, are sometimes known as cluster feeding.
Cluster feeding affects breastfeeding moms in particular; however, formula-fed babies can also feed more frequently at certain stages of development.
Why do babies cluster feed? When does cluster feeding start? When might it end? What’s the best way to cope with a cluster-feeding baby? Keep reading for the answers to these questions and more.
What Is Cluster Feeding?
Cluster feeding is a term used to describe when a breastfed baby wants to be fed more often than usual at certain times of the day.
Every baby is different, so it’s difficult to define precisely when normal feeding crosses the line to become cluster feeding. As a breastfeeding mom, what you’ll notice is a marked increase in the number of feeds compared to what’s been normal so far.
But what does normal even mean, given that the frequency of your little one’s feeds tends to change anyway as your little one grows?
Well, right after birth, your newborn baby’s stomach is still very small, so in the first few days it’s normal for your little one to eat very often — perhaps every one to three hours — to get all the nutrients she needs.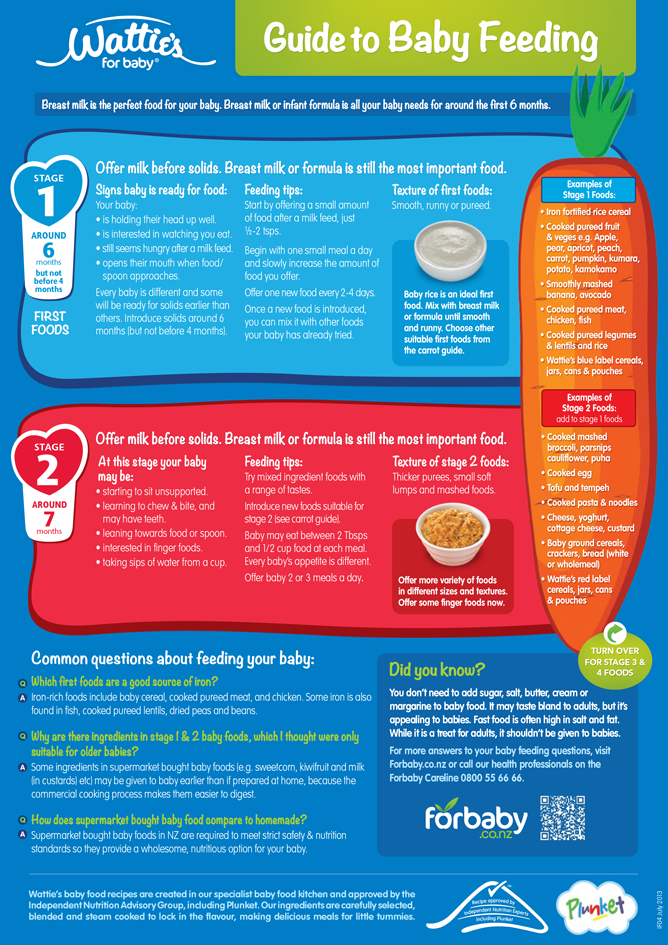
Then, during your baby’s first few weeks and later when your baby is about 1 month old and 2 months old, her stomach gets bigger and she gradually starts taking more milk at each feed. The gaps between feeds also usually get longer.
If your baby starts cluster feeding, this trend is suddenly reversed. When this happens, it might seem as if you’re back to square one, and that your little one has reverted to the constant feeding you experienced in those first few days or weeks.
But don’t worry: Cluster feeding is a common and normal stage in your baby’s development. While it may be a little more tiring for you, it’s actually helping her grow and develop.
Why Does a Newborn Baby Start Cluster Feeding?
Bouts of cluster feeding can occur if your little one is having a growth spurt and needs more food to fuel this rapid development.
Despite their name, growth spurts aren’t always related to an increase in your baby’s size and weight; you could also see a spike in your little one’s appetite when she’s working on developing new mental or motor skills.
In the first year, babies tend to experience the most rapid growth in the first two months after birth, so there may be a higher chance of cluster feeding during this period.
A growth spurt often occurs at around the beginning of the second week, and another one is common between three and six weeks, but every baby is different. There’s no knowing precisely when your little one’s hunger pangs will strike, or how long the cluster feeding phase will last.
Do Formula-Fed Babies Cluster Feed?
The short answer is yes, they can. Although formula-fed babies usually feed less often than breastfed ones because breast milk is digested faster than formula, formula-fed babies, of course, also experience growth spurts — and the associated munchies — as well.
If you’re formula feeding your little one, there’s a chance that she may eat more frequently — and even cluster feed — during these periods, too; but it’s also possible that the interval between feeds will stay more or less the same and she’ll just want to take a little more at each feed. Paced bottle feeding is a good method to use if you prefer your baby having more control over the pace of feeding.
Paced bottle feeding is a good method to use if you prefer your baby having more control over the pace of feeding.
How Long Does Cluster Feeding Last?
Feeding patterns can vary continuously for as long as your baby is breastfed or formula-fed, but bouts of cluster feeding generally occur during the first few weeks and months after your little one is born.
How to Deal With Cluster Feeding
Bouts of cluster feeding can make those first few months — already a tiring time — seem more challenging, but it’s important to go with the flow and ride out those periods of more intensive feeding. Remember, the growth spurts won’t last forever.
In the meantime, try and get as much rest as you can in the “calmer” periods, and take steps to avoid getting sore nipples, such as making sure your baby’s mouth is deeply latched, and using different breastfeeding positions from time to time.
Rather than setting a rigid timetable for feeding your baby, keep an eye out for feeding cues — the signs that he’s hungry — and let him feed “on demand” as much as possible.
Signs that your baby is hungry include turning towards your breast (rooting) if he’s breastfeeding, as well as smacking his lips or putting a fist in his mouth and sucking on it.
Reach out to your healthcare provider or enlist the help of a lactation consultant if you need help with cluster feeding or any other aspect of breastfeeding.
Our downloadable go-to breastfeeding guide is also a great source of tips and advice.
How to Tell if Your Baby Is Still Eating the Right Amount
All the changes in feeding patterns that can occur during those first few months of your little one’s life can be confusing. If you’re at all unsure, check in with your baby’s healthcare provider.
In the meantime, here are some ways to check your baby is getting enough milk:
Pay attention to your baby’s feeding cues.
 If you’re breastfeeding, it’s hard to be sure exactly how much milk your little one’s had. Keep in mind that your baby’s feeding sessions can vary in length, and he’ll usually stop eating when he’s feeling full. If you’re bottle-feeding, you might be unsure whether your little one has gotten all the breast milk or formula he needs from the bottle. Signs that he’s still hungry might include putting his hand in his mouth or smacking his lips after draining the feeding bottle dry. Fidgeting or looking distracted mid-feed could mean he’s no longer hungry. As your little one’s feeding patterns become established, you’ll soon get to know his unique signals and cues.
If you’re breastfeeding, it’s hard to be sure exactly how much milk your little one’s had. Keep in mind that your baby’s feeding sessions can vary in length, and he’ll usually stop eating when he’s feeling full. If you’re bottle-feeding, you might be unsure whether your little one has gotten all the breast milk or formula he needs from the bottle. Signs that he’s still hungry might include putting his hand in his mouth or smacking his lips after draining the feeding bottle dry. Fidgeting or looking distracted mid-feed could mean he’s no longer hungry. As your little one’s feeding patterns become established, you’ll soon get to know his unique signals and cues.Keep an eye on your baby’s growth. As long as your little one’s size and weight gain are on track, he’s probably eating the right amount. Your baby’s healthcare provider will be keeping track of all this for you.
Count those dirty diapers. What goes in must come out, so counting wet and poopy diapers is another way of keeping tabs on your baby’s intake of fluid and nutrients.
 After the first 5 days, around 6 or more heavy wet diapers and about 3 or 4 poopy ones every 24 hours is a good sign that your little one is getting enough milk. Incidentally, all those diapers — whether they end up filled with meconium, regular poop, or pee — could be earning you great gifts, discounts, and coupons. Download the Pampers Rewards app to get started.
After the first 5 days, around 6 or more heavy wet diapers and about 3 or 4 poopy ones every 24 hours is a good sign that your little one is getting enough milk. Incidentally, all those diapers — whether they end up filled with meconium, regular poop, or pee — could be earning you great gifts, discounts, and coupons. Download the Pampers Rewards app to get started.
Will Cluster Feeding Make My Breast Milk Run Out?
Your little one’s feeding actually stimulates milk production, so in most cases your body will ramp up the supply to meet demand during periods of cluster feeding.
Stress or illness may decrease your milk supply temporarily. Ways of overcoming these temporary glitches include staying hydrated, eating healthily, and getting a little more rest (if you can).
Some medications can also affect your milk supply. If you think a medicine that you’re taking could be reducing the amount of breast milk you make, talk to your healthcare provider. Your provider might be able to suggest an alternative medication for you while you’re breastfeeding.![]()
If you think you might not be producing enough milk, you can always ask your provider or a lactation consultant for personalized advice on how to increase your breast milk supply.
Caring for a newborn baby is a full-time job and, just like any other rewarding occupation, it can have its more relaxed and its busier periods. For most moms, times of cluster feeding fall into the latter category!
But there’s a big upside to all of this: As you watch your little one growing and changing from day to day, simply knowing that each bout of cluster feeding is fueling the next stage of your baby’s development will make the extra effort seem worth it in the end.
Feeding for cow's milk protein allergy
- Nestlé Health Science
- health care
- Feeding with CMPA
Feeding and treatment of CMPA
The appearance of allergy symptoms in an infant always causes fear in parents. The first step is to consult a doctor who will conduct an examination, make the correct diagnosis and prescribe competent treatment. With the right approach, most symptoms will disappear within 2-4 weeks.
The first step is to consult a doctor who will conduct an examination, make the correct diagnosis and prescribe competent treatment. With the right approach, most symptoms will disappear within 2-4 weeks.
Important! Do not experiment with a diet that excludes cow's milk protein without the advice and direction of a doctor.
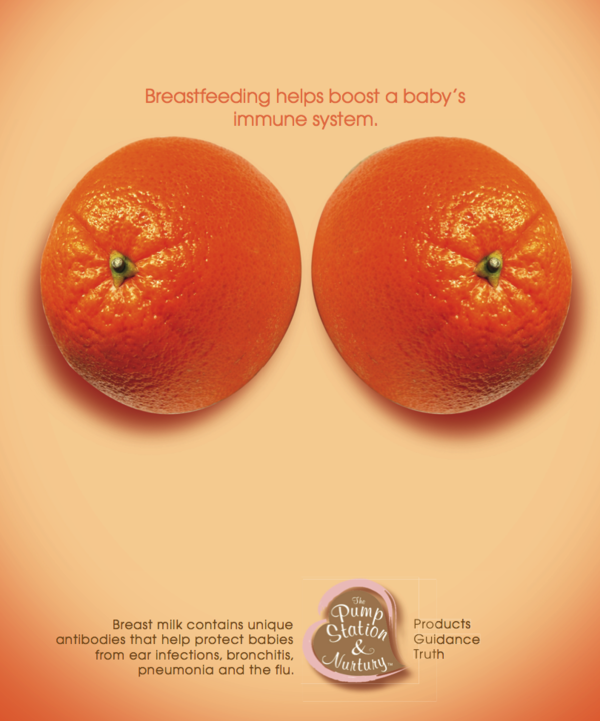
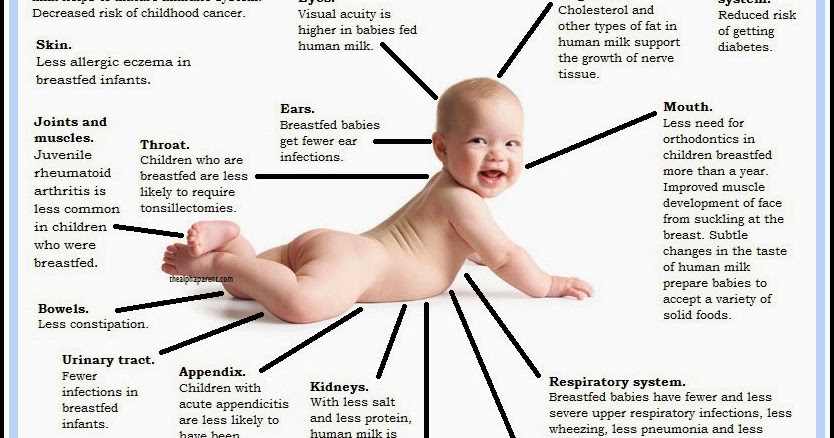
Breastfeeding is the best nutritional option for you and your baby. Even if your baby has been diagnosed with CMPA, breastfeeding should continue. Based on the severity of the symptoms and the presence of other types of food allergies in the child, the doctor will help determine the most appropriate diet for your child to quickly resolve the symptoms of the allergy.
Continue breastfeeding
A diagnosis of CMPA should not affect breastfeeding. Breastfeeding is the best nutritional option for your baby. Breast milk contains all the nutrients your baby especially needs during the first 6 months and continues to be beneficial for a long time to come.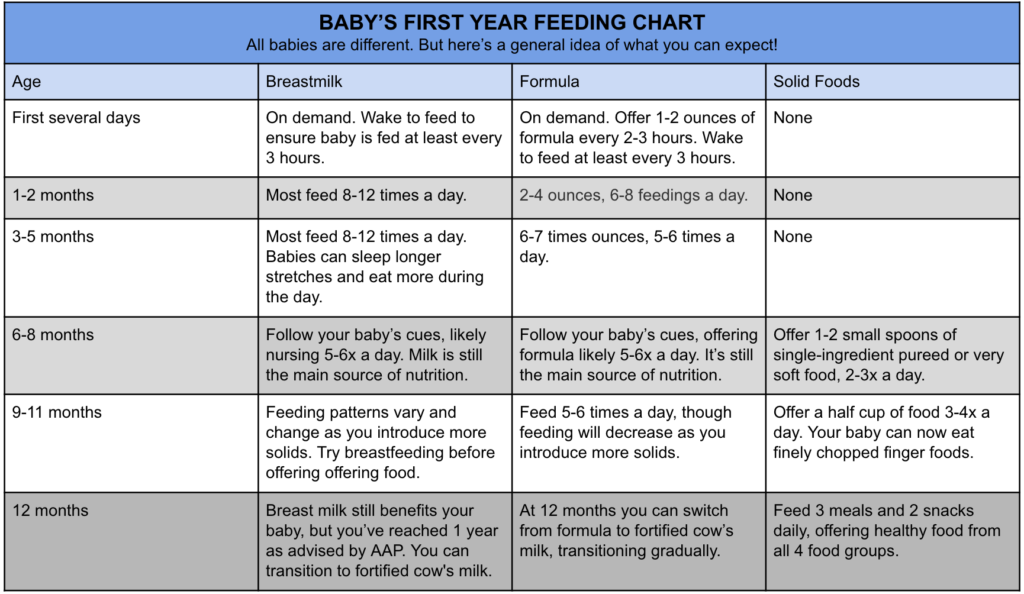 In addition to nutritional properties, breast milk contains antibodies, leukocytes and immune complexes, which together form the baby's immunity. In rare cases where the baby's immune system reacts to cow's milk proteins in breast milk, your doctor may recommend that you start a diet eliminating cow's milk proteins entirely (remember that a dairy-free diet may not be sufficient, as all traces of cow's milk must be eliminated) .
In addition to nutritional properties, breast milk contains antibodies, leukocytes and immune complexes, which together form the baby's immunity. In rare cases where the baby's immune system reacts to cow's milk proteins in breast milk, your doctor may recommend that you start a diet eliminating cow's milk proteins entirely (remember that a dairy-free diet may not be sufficient, as all traces of cow's milk must be eliminated) .
Early start: The sooner you start breastfeeding, the better. According to doctors, starting breastfeeding within 1 hour of birth ensures that your baby receives first milk (colostrum) and the protective factors it contains as soon as possible.
Emotional Benefit: Breastfeeding is an important factor in establishing and maintaining a strong emotional bond with your baby.
Long-term health benefits: Breastfeeding will also help develop your baby's immune system and thus protect your baby's health in the long term.
Protection for you and your baby: Studies have shown that breastfeeding reduces the risk of further infections in children, digestive tract diseases, diabetes, obesity and even leukemia. Breastfeeding is also good for you! Mothers who breastfeed have a reduced risk of developing diabetes, as well as breast and ovarian cancer.
Importance and benefits of breastfeeding
The sooner the better
- Breastfeeding during the first hour of birth ensures that the baby receives its first milk called colostrum
- Exclusive breastfeeding recommended for the first 6 months
Protective role for you and your child
- Breast milk is rich in protective factors that promote healthy growth and development in babies and reduce the risk of developing diseases later on.
- Mothers who breastfeed have a lower risk of developing diabetes and developing breast and ovarian cancer
Emotional Benefits
- You and your child develop and maintain a strong emotional bond.
What type of food is best for my child?
The only way to eliminate symptoms is to eliminate cow's milk proteins from the child's diet.
Important! Do not experiment with a diet that excludes cow's milk protein without the advice and direction of a doctor.
If breastfeeding is not possible, or supplemented with infant formula, your doctor will help you select an appropriate infant formula that does not contain cow's milk proteins. These infant formulas are formulated with children in mind and contain all the necessary nutrients to support growth and development.
These specialized infant formulas can be based on:
- cow's milk processed in a certain way so that the proteins are no longer recognized by the baby's immune system and therefore do not cause an allergic reaction
- amino acids
The table below describes the differences between the two types of infant formula.
| SOGSB | SOA | |
| What is it? | WGHB stands for "Whey Protein Hydrolysate Blend". The proteins in cow's milk that cause allergic reactions in a baby are severely broken down (hydrolyzed). | COA stands for "amino acid blend". This mixture does not contain any cow's milk proteins. |
| What does it consist of? | Cow's milk proteins have been broken down into smaller particles, which means they can no longer be recognized by the baby's immune system. Mixtures contain the macro- and micronutrients necessary for the child. | In severe forms of allergies, an amino acid mixture is used. This mixture does not contain any cow's milk proteins. The mixture is also enriched with all the necessary elements to support healthy growth and development. |
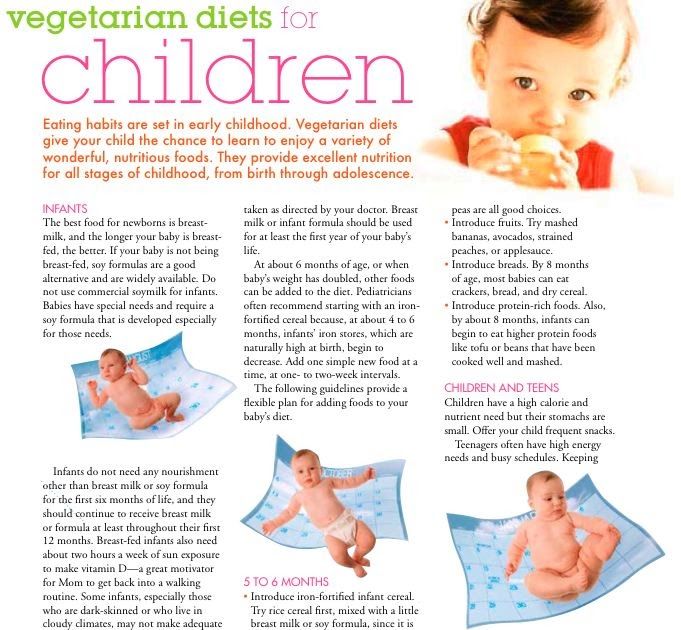
When and how to introduce complementary foods
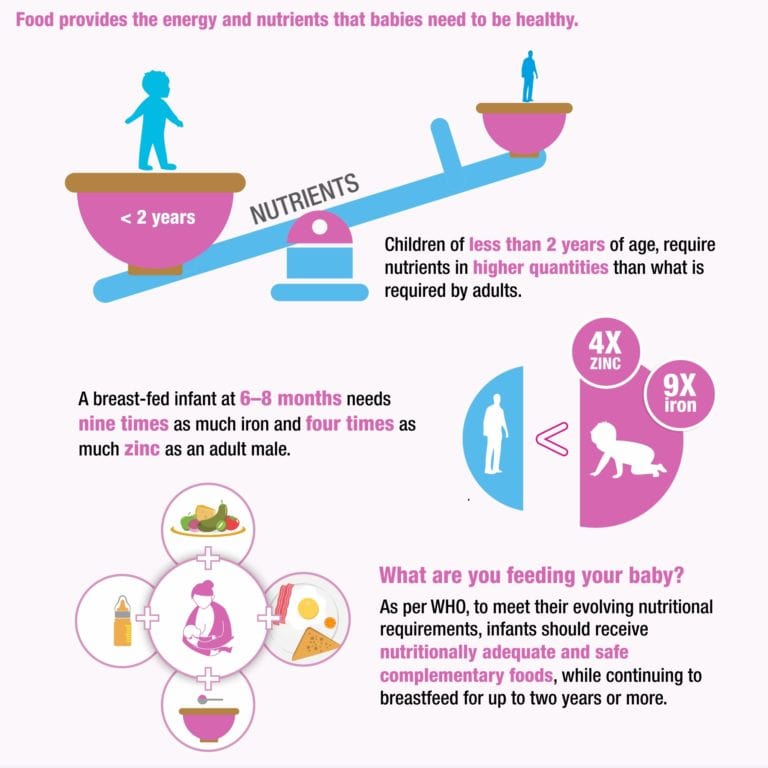
At 6 months of age, breastfeeding (or special infant formula) is no longer sufficient to fully support a child's growth and development and supplementary foods must be introduced into the diet.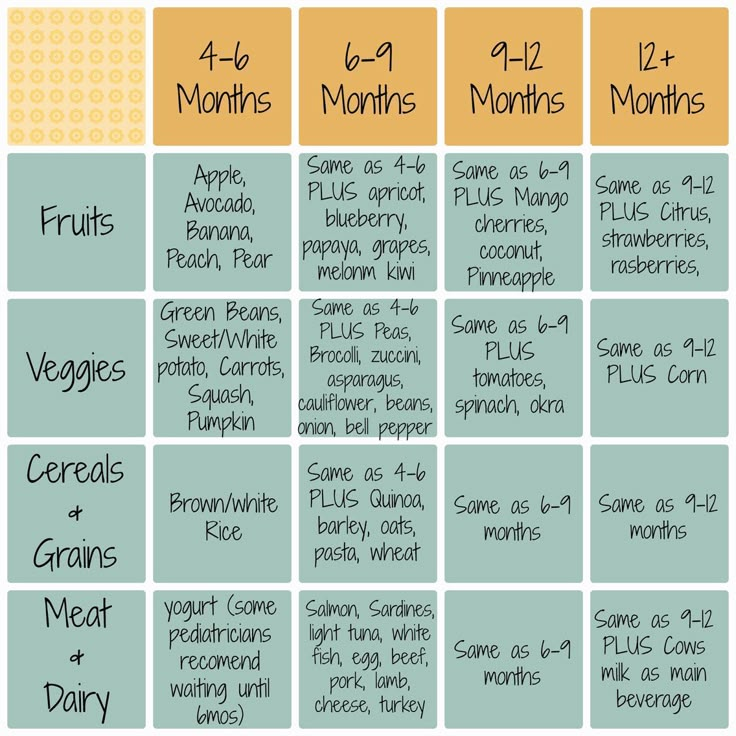 But throughout this time, breastfeeding (or special infant formula) is still the main source of nutrition for the baby.
But throughout this time, breastfeeding (or special infant formula) is still the main source of nutrition for the baby.
It is important to introduce complementary foods on time. The reflex responsible for moving solid foods in the mouth and swallowing them usually develops between 4 and 7 months of age. If you start solid foods too early, the baby will not be ready for it. Similarly, if you start too late, your child may not get all the nutritional support he or she needs, which increases the child's risk of developing essential vitamin and mineral deficiencies and stunting. Along with the nutritional benefits, introducing complementary foods will also provide sensory stimulation and improve your baby's motor skills.
IMPORTANT NOTE: : It is possible to continue breastfeeding if the infant is allergic to cow's milk protein. To do this, the mother needs a special diet with the exclusion of all sources of cow's milk protein. Only if these measures do not bring the desired effect, the doctor recommends the use of a special therapeutic mixture intended for children from 0 to 1 year old.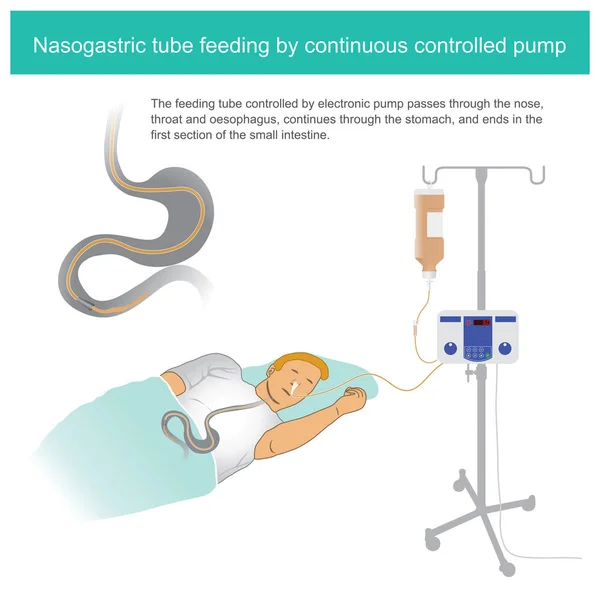 It is important to follow the correct methods of preparing the mixture: using boiled water, sterilized bottles and following the rules for diluting the mixture. Medicinal mixtures intended for diet therapy of CMPA should be used under the supervision of a physician.
It is important to follow the correct methods of preparing the mixture: using boiled water, sterilized bottles and following the rules for diluting the mixture. Medicinal mixtures intended for diet therapy of CMPA should be used under the supervision of a physician.
Lack of sleep while breastfeeding | Philips Avent
4 min.
Sept. 2021
This material is intended for healthcare professionals
In the first months of a newborn's life, lack of sleep in parents can be of great importance for its further development. The newborn's feeding and sleeping schedule means that parents can only rely on short sleep, which is contrary to the adult's need for uninterrupted 7–9-hour sleep. 1
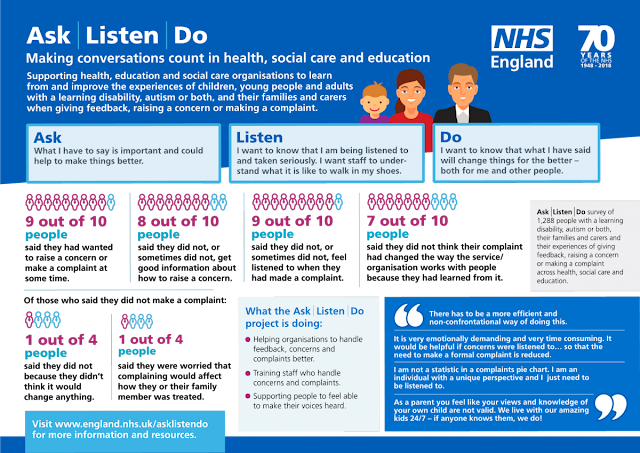
When parents try to find ways to cope with night feedings, strong emotions and deep insecurities often arise. This happens even among parents who already have experience with newborns. Health professionals can help and support parents by providing them with complete information and advice on caring for newborns.
Health professionals can help and support parents by providing them with complete information and advice on caring for newborns.
Feeling unwell due to exhaustion
Educating mothers about sleep physiology is a good starting point. Since they are unable to sleep for longer periods of time, they often skip REM sleep, which begins around 90 minutes of uninterrupted sleep is critical to restoring vitality. Lack of sleep during REM sleep reduces stress tolerance and the ability to think clearly. So it is only natural that they are exhausted and irritated.
Mothers would like to have a nightly feeding schedule and still want to get a good night's sleep. Moms often feel guilty about switching to bottle feeding, even if it's just to share the worries of nighttime feeding with their partner. They may worry that bottle feeding will interfere with bonding and may also negatively impact a child's development if they don't always respond to a newborn's diet.
Advice from health professionals
Parents value the support of health professionals and advice tailored to the mother's specific situation. Your experience and knowledge helps them by increasing their confidence in parenthood. The health worker's advice is as follows:
- Look at the sleep conditions of the parents and the child, perhaps some changes can be made. For example, if the bedroom is too hot or too cold, it can disturb a child's sleep 2 so he may wake up and need more attention at night.
- Explain the advantages and disadvantages of night feeding bottles so parents can make an informed decision and possibly share responsibility.
- Advise preventing baby from falling asleep on the breast at night and replacing this with close physical contact.
- Reassure mothers that they are great mothers, even if they (or their partner) bottle feed their baby.
And if mothers are worried about losing contact with their baby, reassure them that feeding is not their only connection. As partners help with bottle feeding and night feedings decrease, physical contact with the baby should become the primary focus for each. Together they will find their common biological rhythm so that all family members are happy.
As partners help with bottle feeding and night feedings decrease, physical contact with the baby should become the primary focus for each. Together they will find their common biological rhythm so that all family members are happy.
Share this article:
Similar articles
Are you not a healthcare professional?
Resources
1. Nemours Foundation. A Guide for First-Time Parents: Sleeping Basics. www.kidshealth.org/parent/pregnancy_newborn/pregnancy/guide_parents_p4.html
2. www.nhs.uk/conditions/baby/caring-for-a-newborn/helping-your-baby-to-sleep .html
You are leaving the Philips Healthcare (“Philips”) official website. Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain.