Baby cramps during feeding
Breastfeeding FAQs: Pain and Discomfort (for Parents)
Breastfeeding is natural, but it takes practice to get it right. Here's how to handle pain and discomfort during nursing.
Is It Normal to Have Cramps While Breastfeeding?
Yes. During the first few days to weeks after delivery, you may feel strong, menstrual-like cramps in your uterus when your milk “lets down” (starts to flow). This is your uterus shrinking back to a smaller size.
Is It Normal for My Breasts to Get Engorged?
During the first 2–5 days after birth, it’s normal to have engorged (very full) breasts as your milk supply increases. But if your baby nurses (or you pump) every 2–3 hours, your breasts should not feel engorged.
Engorgement can lead to sore, painful breasts or a breast infection. So it’s best to try to avoid it. The longer you wait to breastfeed or pump, the more uncomfortable and engorged your breasts may get.
If you can't feed your baby right away, use warm compresses and try to pump or manually express your milk. One way to express milk is to put your thumb on top of your areola and a finger below it. Gently but firmly press your thumb and fingers back against your chest wall. Then compress your fingers together to express (push out) your milk.
Is It Normal to Feel Pain During or After Breastfeeding?
When babies latch on properly, some moms feel a few moments of discomfort at the very beginning of a nursing session. After that, discomfort should ease. You may feel a gentle tug on your breasts while your baby feeds, but it shouldn’t hurt.
If you feel discomfort during nursing, stop nursing and reposition your baby to get a better latch. Your nipple areola (the ring around the nipple) should be mostly in your baby’s mouth. When babies are latched on wrong, it can hurt or feel like a pinch each time your baby sucks. Over time, this can lead to painful, sore, cracked nipples.
If you have pain during breastfeeding, talk to your doctor or lactation consultant to make sure your baby is properly latched or that something else isn't going on.
What Else Can Cause Breast Pain?
The most common causes of breast pain include:
A plugged milk duct. Sometimes milk ducts get plugged. You may feel pain in an area of your breast or a lump may form under the skin where the duct is plugged. To help unclog the duct and ease pain:
- Take warm showers or use warm compresses on the area. Massage the area several times a day. Then, breastfeed your baby right away.
- Position your baby’s chin so that it points toward the clogged area during feeding. This will help that area of the breast empty sooner.
- Gently massage the lump while your baby feeds. It may take 2 to 3 feedings for the lump to go away. You also can use a manual (hand) or electric pump for a few minutes to help draw out the clogged milk while gently massaging the area.
- Apply cold compresses (ice wrapped in a thin towel) between feedings.
- If the lump doesn't go away within a couple of days, or if you have a fever, chills, aches, or red streaking, call your doctor.

Mastitis. This is an inflammation of the breast. If your breasts are sore; have red streaks; or have a hard, red area, you may have mastitis. Some women also get a fever and chills. If you think you have mastitis, call your doctor. In the meantime, continue to breastfeed or pump to drain the milk from your breasts. Switch between warm compresses and gentle massage right before breastfeeding and then apply cold compresses after a session. Mastitis caused by an infection may need treatment with antibiotics.
Oral thrush. Sometimes babies develop a yeast infection in the mouth called oral thrush. Babies with this have cracked skin in the corners of the mouth, and whitish or yellowish patches on the lips, tongue, or inside the cheeks. The infection can spread to your breast and cause:
- shooting or burning breast pain either during or after feedings
- pain deep within your breast
- strong pain in the breasts or nipples that doesn't get better after your baby properly latches on or you reposition your baby
- nipples that are cracked, itchy, burning, or are pink, red, shiny, flaky, or have a rash with little blisters
Call your doctor if you or your baby have any of these symptoms.
Inverted or flat nipples. Women who have inverted nipples (nipples that turn in rather than stick out) or flat nipples (that don't become as erect as they should when a baby is nursing) may have a harder time breastfeeding or have nipple pain. If either is the case, talk to your doctor or a lactation consultant about ways to make nursing easier and reduce any pain.
How Can I Ease Breast or Nipple Pain?
During Feedings
- Nurse first on the side that's less sore and vary breastfeeding positions.
- Make sure your baby latches onto your breasts correctly. If breastfeeding is too painful, it may be more comfortable to drain your breasts by pumping the milk.
- If you have sore nipples, ask a lactation consultant or your health care provider if a nipple shield is a good idea. Nipple shields go over the areola and nipple during a feeding to protect sore or cracked nipples. They should only be used when recommended by your care team as they can sometimes affect milk supply.

- Gently break the suction when removing your baby from your breast. Slip your finger in the side of your baby's mouth, between the gums, and then turn your finger a quarter turn to do so.
- At the end of a feeding, massage some breast milk onto your nipples, and then let them air dry.
Between Feedings
- Gently massage the sore area before nursing.
- Use wet or dry heat on your breasts (a warm shower, water bottle, heating pad, or warm washcloth) right before feeding. But if you have a yeast infection in your breast, you'll need to keep your nipples dry because yeast thrives on moisture. Get plenty of rest and fluids.
- Put ice packs or cool compresses on engorged breasts after feedings.
- Make the area where you feed your baby comfortable. Sit in a glider or a cozy chair with armrests. Footstools and pillows can give extra support. Some women like wraparound nursing pillows or "husband" back pillows with arms on each side for nursing in bed.
If breastfeeding is painful or uncomfortable for you, callyour doctor or lactation consultant for help.
Colic | Breastfeeding Challenges | Start for Life
There may be times when breastfeeding is challenging. Never ignore any issues you may have – talk to your health visitor, midwife, GP or breastfeeding specialist as soon as possible, they will be able to help you sort it out quickly.
Here are some common breastfeeding issues, and tips on what to do.
There are other reasons why your baby may be crying, it's a good idea to check if they:
- are hungry
- have a dirty or wet nappy
- have wind
- are too hot or too cold
- are bored or overstimulated
If your baby tends to cry during or after feeds, it's worth checking whether this could be reflux. Our guide to reflux in breastfed babies has information on the signs and symptoms.
What causes colic?
There are no known reasons why some babies get colic &ndash some doctors think it's a type of stomach cramp. But it may happen because babies find it harder to digest food when they are really young.
But it may happen because babies find it harder to digest food when they are really young.
Constant crying could also be due to food allergies, such as cow's milk allergy. If you think this is the case, talk to your GP before making any changes to your baby's diet.
Colic remedies for breastfed babies
Sadly, there is no actual cure for baby colic, only methods to provide relief and soothe them. These are some of the tried and tested techniques that other parents use to relieve colic symptoms in breastfed babies:
Burping
Burp (or wind) your baby during and after every feed – have a look at burping your baby for techniques.
Sit your baby up
When breast or bottle feeding, sit your baby up as straight as possible. This will help minimise the amount of air they swallow. If you are bottle feeding, try to make sure the milk fills the teat and there are no air pockets – you could try using an anti-colic bottle to see if that helps.
Attachment
Check that your baby is attached (latching on) properly as this may help reduce colic symptoms. If you are unsure that your baby is attaching properly while breastfeeding, have a look at our guide to latching on.
If you are unsure that your baby is attaching properly while breastfeeding, have a look at our guide to latching on.
Diet
There is no evidence that changing your diet will help &ndash however some people say that cutting down on spicy foods, caffeine and acohol has made a difference for them.
If you are mixed feeding (combining breast and bottle feeding), have a look at our guide to colic when bottle feeding.
Other ways to soothe your baby
Hold them
During bouts of crying, hold your baby to your chest so they can feel and hear your heartbeat.
Rock your baby
Sometimes the swaying motion of rocking your baby in your arms can help.
Warm bath and a massage
A warm bath can be soothing, followed by a gentle tummy massage (with gentle, circular strokes on the tummy).
Create a calming atmosphere
Babies can become overstimulated with lots of noise and activity around them. Try to quieten your surroundings, switch the TV off, dim the lights, and try to take some deep breaths yourself.
Convulsive syndrome in children - causes of convulsions, symptoms, methods of prevention
Convulsive syndrome is a non-specific reaction of the child's body to external and internal stimuli, characterized by sudden attacks of involuntary muscle contractions. The smaller the child, the more convulsive readiness he has. This is due to the immaturity of some structures of the brain and nerve fibers, the high degree of permeability of the blood-brain barrier and the tendency to generalize any processes, as well as some other reasons. nine0005
Reasons
All causes of seizures can be divided into epileptic (epilepsy) and non-epileptic.
Non-epileptic:
- Spasmophilia.
- Overheating.
- Encephalitis, meningitis, trauma and brain infections.
- Toxoplasmosis.
- Metabolic disorders, primarily potassium and calcium metabolism, for one reason or another.
- For newborns - hemolytic disease, congenital lesions of the nervous system, asphyxia.
 nine0016
nine0016 - Various hormonal disorders.
- In acute infectious diseases, especially with a rise in temperature to febrile numbers.
- Intoxication and poisoning.
- Hereditary metabolic diseases.
- Pathologies of the cardiovascular and hematopoietic systems.
Symptoms
- Tonic convulsions (spasm-muscle tension).
- Pose with the upper limbs bent at all joints, the lower limbs extended and the head thrown back. nine0016
- Respiration and pulse are slow. Contact with the outside world is lost or significantly weakened.
- Clonic convulsions (involuntary muscle twitching).
The diagnosis of convulsive syndrome in children is made on the basis of the clinic, which in most cases does not cause difficulties. After making this diagnosis, it is necessary to clarify the nature of the convulsive syndrome, for which the anamnesis of the life and illness of the child, x-ray examination of the skull, echoencephalography, electroencephalography, angiography and other methods can be used. Laboratory tests can be quite revealing. nine0005
Laboratory tests can be quite revealing. nine0005
Prevention
Febrile convulsions (at high body temperature, above 38 C) usually stop with age. To prevent their recurrence, severe hyperthermia should not be allowed if an infectious disease occurs in a child. The risk of transformation of febrile seizures into epileptic seizures is 2-10%.
In other cases, the prevention of convulsive syndrome in children includes the prevention of perinatal pathology of the fetus, the treatment of the underlying disease, and observation by children's specialists. If the convulsive syndrome in children does not disappear after the cessation of the underlying disease, it can be assumed that the child has developed epilepsy. nine0005
More about pediatric neurology at the YugMed clinic
By leaving your personal data, you give your voluntary consent to the processing of your personal data. Personal data refers to any information relating to you as a subject of personal data (name, date of birth, city of residence, address, contact phone number, email address, occupation, etc. ). Your consent extends to the implementation by the Limited Liability Company Research and Production Association "Volgograd Center for Disease Prevention "YugMed" of any actions in relation to your personal data that may be necessary for the collection, systematization, storage, clarification (updating, changing), processing (for example, sending letters or making calls), etc. subject to current legislation. Consent to the processing of personal data is given without a time limit, but can be withdrawn by you (it is enough to inform the Limited Liability Company Scientific and Production Association "Volgograd Center for Disease Prevention" YugMed "). By sending your personal data to the Limited Liability Company Research and Production Association "Volgograd Center for Disease Prevention" YugMed ", you confirm that you are familiar with the rights and obligations in accordance with the Federal Law "On Personal Data". nine0005
). Your consent extends to the implementation by the Limited Liability Company Research and Production Association "Volgograd Center for Disease Prevention "YugMed" of any actions in relation to your personal data that may be necessary for the collection, systematization, storage, clarification (updating, changing), processing (for example, sending letters or making calls), etc. subject to current legislation. Consent to the processing of personal data is given without a time limit, but can be withdrawn by you (it is enough to inform the Limited Liability Company Scientific and Production Association "Volgograd Center for Disease Prevention" YugMed "). By sending your personal data to the Limited Liability Company Research and Production Association "Volgograd Center for Disease Prevention" YugMed ", you confirm that you are familiar with the rights and obligations in accordance with the Federal Law "On Personal Data". nine0005
Convulsive syndrome, useful articles of the medical clinic Neuro-Med
Convulsive syndrome
In children of the first year of life, convulsions are observed in various diseases of the nervous system. They may appear against the background of already existing neurological disorders and delayed psychomotor development, or appear as the first symptom indicating brain damage. The clinical picture of the convulsive syndrome depends both on the nature of the disease and on the age of the child. In newborns, convulsions often begin with local twitches of facial muscles, eyes, then they spread to the arm, leg on the same side and (or) move to the opposite. Clonic twitches may follow randomly from one part of the body to another. Such roads are called generalized fragmentary, as they represent a fragment of generalized convulsions [Rose A. L., Lambroso C. T.. 1970; Lacy J. R., Penry J. K., 1976].
They may appear against the background of already existing neurological disorders and delayed psychomotor development, or appear as the first symptom indicating brain damage. The clinical picture of the convulsive syndrome depends both on the nature of the disease and on the age of the child. In newborns, convulsions often begin with local twitches of facial muscles, eyes, then they spread to the arm, leg on the same side and (or) move to the opposite. Clonic twitches may follow randomly from one part of the body to another. Such roads are called generalized fragmentary, as they represent a fragment of generalized convulsions [Rose A. L., Lambroso C. T.. 1970; Lacy J. R., Penry J. K., 1976].
Newborns may also have focal clonic seizures affecting one half of the body. Sometimes they resemble Jackson's or proceed in the form of adversive turns of the head, eyes, tonic abduction of the hands in the direction of turning the head (ASTR type), opercular paroxysms (grimaces, sucking, chewing, smacking). The motor component of the seizure is often accompanied by vasomotor disorders in the form of pallor, cyanosis, redness of the face, salivation. Less often, myoclonic-type convulsions are observed in newborns, which are characterized by single or frequent twitches of the upper or lower extremities with a tendency to bend them. They can also be manifested by general shuddering followed by a large-scale tremor of the hands. Sometimes these convulsions are accompanied by screams, vegetative-vascular disorders. In mild cases, the abnormal movements that occur with seizures can be mistaken for spontaneous neonatal movements and miss the true onset of the seizure. The cause of convulsive syndrome in the neonatal period is often metabolic disorders (hypoglycemia, hypocalcemia, hypomagnesemia, hyperbilirubinemia, pyridoxine dependence), brain development anomalies, hypoxia, intracranial birth trauma, less often neuroinfections (meningitis, encephalitis). Some early forms of hereditary metabolic disorders of amino acids (leucinosis, hypervalemia, argininemia, histidinemia, isovaleric acidemia, phenylketonuria), carbohydrates (galactosemia, glycogenosis), lipids (Norman-Wood and Norman-Landing diseases, Gaucher disease), vitamins (methylmalonic aciduria, Lee's disease, hyperglycinemia), occurring with acute development of neurological symptoms after birth, are also accompanied by a convulsive syndrome.
The motor component of the seizure is often accompanied by vasomotor disorders in the form of pallor, cyanosis, redness of the face, salivation. Less often, myoclonic-type convulsions are observed in newborns, which are characterized by single or frequent twitches of the upper or lower extremities with a tendency to bend them. They can also be manifested by general shuddering followed by a large-scale tremor of the hands. Sometimes these convulsions are accompanied by screams, vegetative-vascular disorders. In mild cases, the abnormal movements that occur with seizures can be mistaken for spontaneous neonatal movements and miss the true onset of the seizure. The cause of convulsive syndrome in the neonatal period is often metabolic disorders (hypoglycemia, hypocalcemia, hypomagnesemia, hyperbilirubinemia, pyridoxine dependence), brain development anomalies, hypoxia, intracranial birth trauma, less often neuroinfections (meningitis, encephalitis). Some early forms of hereditary metabolic disorders of amino acids (leucinosis, hypervalemia, argininemia, histidinemia, isovaleric acidemia, phenylketonuria), carbohydrates (galactosemia, glycogenosis), lipids (Norman-Wood and Norman-Landing diseases, Gaucher disease), vitamins (methylmalonic aciduria, Lee's disease, hyperglycinemia), occurring with acute development of neurological symptoms after birth, are also accompanied by a convulsive syndrome. In infants, unlike newborns, the motor component of the convulsive syndrome becomes more distinct. With generalized convulsions, a tendency to alternating tonic and clonic phases can already be noted, but it still remains mild compared to older children. The structure of the seizure is dominated by the tonic component, often convulsions (accompanied by vegetative symptoms (pain in vomiting, vomiting, fever). Involuntary urination is rarely observed. After the seizure, the child is often agitated, but may be lethargic, drowsy. clonic twitches of facial muscles, muscles of the tongue, distal limbs, turning of the head and eyes to the side.0005
In infants, unlike newborns, the motor component of the convulsive syndrome becomes more distinct. With generalized convulsions, a tendency to alternating tonic and clonic phases can already be noted, but it still remains mild compared to older children. The structure of the seizure is dominated by the tonic component, often convulsions (accompanied by vegetative symptoms (pain in vomiting, vomiting, fever). Involuntary urination is rarely observed. After the seizure, the child is often agitated, but may be lethargic, drowsy. clonic twitches of facial muscles, muscles of the tongue, distal limbs, turning of the head and eyes to the side.0005
The convulsive syndrome can also proceed according to the type of absences, which are characterized by a short stop of gaze. Sometimes at the moment of a seizure there are so-called motor automatisms in the form of sucking, chewing movements, smacking. The attack is often accompanied by vascular disorders and slight abduction towards the eyeballs. It should be noted that absences in infants are observed much less frequently than other types of seizures.
It should be noted that absences in infants are observed much less frequently than other types of seizures.
Infants are characterized by myoclonic seizures (infantile spasms) [Jeavons P. M. Bower B. D., Dimitracoudi M., 1973]. In children older than a year, seizures are rare. Due to the fact that convulsive seizures of this type have a malignant course and cause a severe delay in psychomotor development, it is necessary to dwell on them in more detail. Small propulsive seizures proceed in the form of bilateral symmetrical muscle contraction, as a result of which the trunk and limbs suddenly bend ("Salaam's seizures").
With extensor spasm, the head and trunk are sharply extended, arms and legs are abducted. Along with the classical clinical picture, there may be partial forms - general shudders, nods, head turns, flexion and extension of the arms and legs, sometimes a predominant contraction of the muscles of one side of the body is observed. A feature of small seizures is their tendency to seriality.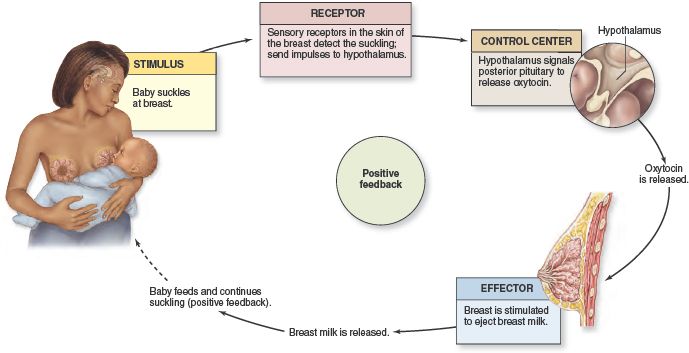 Their frequency per day ranges from single to several hundred and more. Loss of consciousness is short-lived. Convulsions may be accompanied by a scream, a grimace of a smile, dilated pupils, nystagmus, rolling the eyes, trembling of the eyelids, and vascular disorders. There are seizures more often before falling asleep or after waking up. nine0005
Their frequency per day ranges from single to several hundred and more. Loss of consciousness is short-lived. Convulsions may be accompanied by a scream, a grimace of a smile, dilated pupils, nystagmus, rolling the eyes, trembling of the eyelids, and vascular disorders. There are seizures more often before falling asleep or after waking up. nine0005
In infancy, the cause of convulsive syndroitis can be organic lesions of the nervous system due to pre- and perinatal pathology, hereditary metabolic diseases, phakomatoses, leukodystrophy, neuroinfections, post-vaccination complications. In the first year of life, febrile and affective-respiratory convulsions are also often observed.
Febrile convulsions occur in acute respiratory infections: influenza, otitis media, pneumonia. These are usually typical generalized or local tonic-clonic convulsions that occur at the height of fever. Most often, febrile convulsions are single, sometimes repeated for 1-2 days. The risk of recurrent febrile paroxysm increases with the early onset of a primary seizure, its recurrence and an unfavorable neurological background [Aicardi J. C., Chevrie J. J., 1977; Nelson K. W., Ellenberg J. H. 1978].
C., Chevrie J. J., 1977; Nelson K. W., Ellenberg J. H. 1978].
Affective-respiratory convulsions are more often observed in children with increased excitability at the age of 7-12 months. Convulsions, as a rule, come after a negative emotional reaction to a strong sudden pain, fear. The child begins to scream loudly, then the breath is held while inhaling, the child turns blue, then turns pale, throws his head back, loses consciousness for a few seconds. At the same time, muscle hypotension or, conversely, tonic muscle tension is noted. Following this, as a result of cerebral hypoxia, a generalized tonic-clonic seizure may develop. If the attention of the child is switched before the moment of loss of consciousness, the development of paroxysm can be interrupted. nine0005
The diagnosis of convulsive syndrome in children of the first year of life, especially in newborns, presents certain difficulties. This is due to the atypical course, abortion and short duration of paroxysms. Sometimes convulsions are mistaken for normal movements of the child and are diagnosed only when they become deployed and the child loses consciousness. At the same time, convulsions are sometimes referred to as pathological motor reactions of non-convulsive genesis (athetoid movements of the hands and forearms, spontaneous Moro reflex, asymmetric cervico-tonic reflex, contraction of individual facial muscles, grimacing, tremor of the tongue, sweeping hand movements such as hemibalism, hand tremor, etc. .). Sometimes "dystonic attacks" are taken for tonic convulsions, in which there is a sudden increase in muscle tone due to the influence of tonic cervical and labyrinth reflexes. Unlike convulsive syndrome in dystonic attacks, the child does not lose consciousness, and muscle tone can be reduced by giving the child a reflex-prohibiting position. In these cases, there are no EEG changes characteristic of the convulsive syndrome. nine0005
Sometimes convulsions are mistaken for normal movements of the child and are diagnosed only when they become deployed and the child loses consciousness. At the same time, convulsions are sometimes referred to as pathological motor reactions of non-convulsive genesis (athetoid movements of the hands and forearms, spontaneous Moro reflex, asymmetric cervico-tonic reflex, contraction of individual facial muscles, grimacing, tremor of the tongue, sweeping hand movements such as hemibalism, hand tremor, etc. .). Sometimes "dystonic attacks" are taken for tonic convulsions, in which there is a sudden increase in muscle tone due to the influence of tonic cervical and labyrinth reflexes. Unlike convulsive syndrome in dystonic attacks, the child does not lose consciousness, and muscle tone can be reduced by giving the child a reflex-prohibiting position. In these cases, there are no EEG changes characteristic of the convulsive syndrome. nine0005
When a convulsive syndrome occurs in a newborn, a thorough biochemical study should be carried out: blood and urine for the content of calcium, potassium, sodium, phosphorus, glucose, pyridoxine, amino acids, a lumbar puncture should be made to exclude subarachnoid hemorrhage, purulent meningitis. If convulsions first occur in infancy, then along with the above studies, an EEG is taken to detect paroxysmal brain activity. On the EEG, various changes in the bioelectrical activity of the brain can be detected, depending on the nature of the seizures and changes in the nervous system in which they arose. So, with infantile spasms on the EEG, changes are noted that are characteristic only for this type of seizure - hypsarrhythmia. Such studies as craniography, diaphanoscopy, computed tomography, REG, angiography, also in some cases allow us to clarify the cause of the convulsive syndrome. nine0005
If convulsions first occur in infancy, then along with the above studies, an EEG is taken to detect paroxysmal brain activity. On the EEG, various changes in the bioelectrical activity of the brain can be detected, depending on the nature of the seizures and changes in the nervous system in which they arose. So, with infantile spasms on the EEG, changes are noted that are characteristic only for this type of seizure - hypsarrhythmia. Such studies as craniography, diaphanoscopy, computed tomography, REG, angiography, also in some cases allow us to clarify the cause of the convulsive syndrome. nine0005
The impact of seizures on developmental delay depends on the age of the child, the level of psychomotor development before the onset of seizures, the presence of other neurological disorders, the nature of seizures, their frequency and duration. The younger the child's age at the onset of seizures, the more pronounced will be the delay in psychomotor development. If convulsions occurred in a healthy child, were episodic and short-term, then they themselves may not have a significant impact on age-related development and may not cause neurological disorders. These are, as a rule, single febrile and affective-respiratory convulsions. In all other cases, paroxysms, especially if they were long and repeated, in turn can cause irreversible changes in the central nervous system. Seizures that appeared against the background of psychomotor developmental delay and (or) other neurological disorders complicate the course of the underlying disease, exacerbating developmental delay. The child loses acquired motor, mental and speech skills. nine0005
These are, as a rule, single febrile and affective-respiratory convulsions. In all other cases, paroxysms, especially if they were long and repeated, in turn can cause irreversible changes in the central nervous system. Seizures that appeared against the background of psychomotor developmental delay and (or) other neurological disorders complicate the course of the underlying disease, exacerbating developmental delay. The child loses acquired motor, mental and speech skills. nine0005
The nature of convulsive paroxysms also affects the delay in age-related development. The most unfavorable in this regard are infantile spasms, which primarily cause a profound mental retardation. According to J. R. Lacy and J.K. Penry (1976), mental retardation is observed in 75-93% of patients with infantile spasms. The formation of motor skills is also disturbed or they are completely lost, depending on the age at which convulsions began. Regardless of whether seizures appear in the midst of apparent well-being or against the background of an already existing developmental delay, their addition and lack of effectiveness from ongoing therapy lead to a loss of points on the age development scale, and the loss is steadily increasing.