Baby discomfort while feeding
20 Reasons Why Baby Fusses Or Cries While Breastfeeding
From letdown issues to teething, identifying the cause can make breastfeeding easier for you and your baby.
Research-backed
MomJunction believes in providing reliable, research-backed information to you. As per our strong editorial policy requirements, we base our health articles on references (citations) taken from authority sites, international journals, and research studies. However, if you find any incongruencies, feel free to write to us.
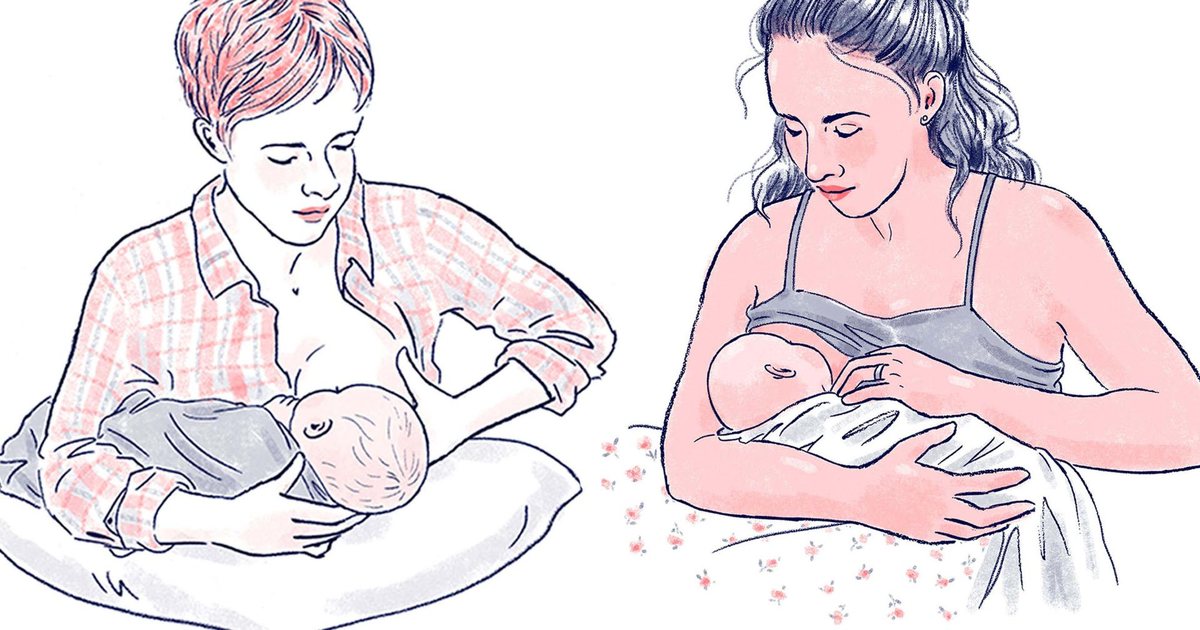
Image: iStock
You may often notice that your baby cries while breastfeeding. Babies may cry when breastfed for various reasons, ranging from simple distractions to a significant feeding problem.
While occasional weeping during nursing is normal, persistent crying and reluctance to breastfeed may necessitate medical treatment or a consultation with a lactation consultant-IBCLC (International Board of Lactation Consultant Examiners).
Read on to learn why newborns cry during breastfeeding and ways to avoid it.
Causes Of Crying In Babies While Breastfeeding
The following factors or situations may make babies fussy or cry during breastfeeding (1).
1. Overactive letdown
Sometimes, if the mother has an overactive or forceful letdown of breast milk, the baby may tend to bite the breast or cry since they cannot swallow too much milk. An overactive letdown may cause colic symptoms for the baby. Hyperactive milk ejection reflex and oversupply may cause gagging or choking while breastfeeding, making your baby cry while nursing.
Quick tip
When your baby is having a colic episode while breastfeeding, you can calm them by holding them close to your heart so they can hear your heartbeat (2).
2. Slow letdown
Slow letdown reflex could cause a slower or inadequate milk supply. Babies may become irritated or cry if they do not get enough milk while breastfeeding.
Related: 5 Helpful Ways To Increase Breastmilk Supply
3. Slow milk flow
Babies can be impatient while waiting for the milk to flow while feeding. Slow milk flow can be due to various reasons, including a slow letdown reflex. Sometimes, a fast milk flow due to overactive letdown followed by a slower flow could make your baby cry since they become frustrated by the changes in the milk flow.
4. Done with feeding
Babies should be the ones ending a feeding. If you continue to feed even when they are refusing, it is normal for babies to cry.
5. Want to burp
Image: Shutterstock
Babies may cry or pull off the breast if they want to burp while nursing, especially during the first few months. Most babies do this while changing the breast or after feeding, and a few may not burp without the assistance of the parent. Older babies can relieve gas while they move, and it is rare for them to burp while nursing.
Bottle-fed infants may burp more than breastfed infants as they are fed too fast.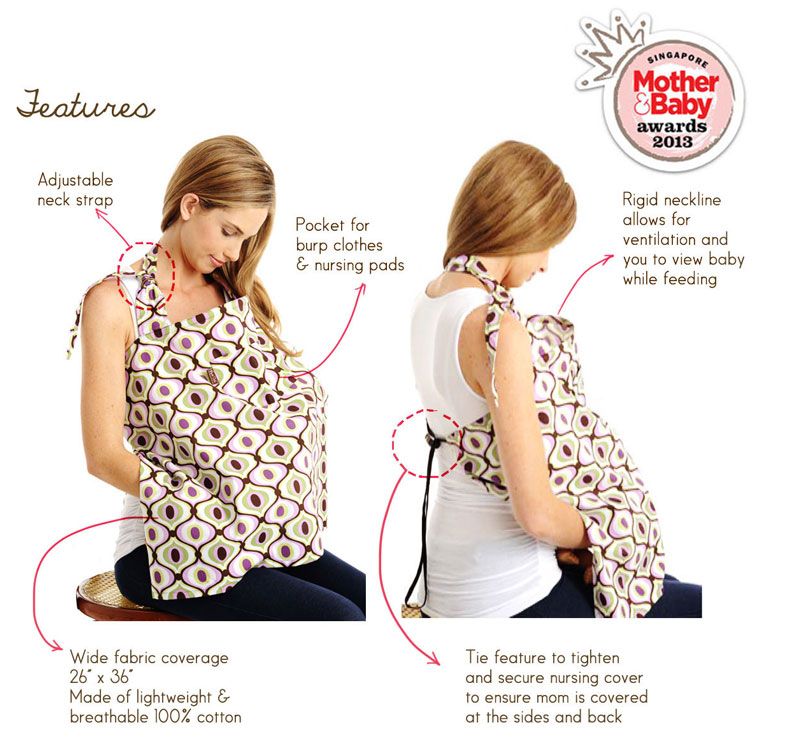 Paced bottle feeding method should be used to help the baby get what he/she needs at that feeding not more.
Paced bottle feeding method should be used to help the baby get what he/she needs at that feeding not more.
6. Not hungry
Babies who are not hungry may cry while feeding since they do not want to be fed. Crying can be a means of communication for the baby.
Related: 11 Reasons Why Baby Refuses To Eat And How To Help Them
7. GERD or acid reflux
Regurgitation of stomach acid to the food pipe could make babies gag or throw up often. Acid reflux may cause irritation or cough and often make babies cry while feeding due to the discomfort.
8. Unusual body odor
Babies may refuse feeding and often cry when they smell a new perfume, soap, or lotion on the breast while feeding since it is unusual for them.
9. Changes in the taste of breast milk
Babies may cry or refuse feeding if the taste or texture of the breast milk changes. Maternal diet, periods, high lipase levels in the milk or second pregnancy may cause changes in the milk.
10. Growth spurt
Growth spurts or frequency days are times when your baby has more intense growth. Babies can have many growth spurts during infancy, usually during two to three weeks, six weeks, three months, and six months.
The duration of growth spurts may vary in babies, and it may last for a few days. Babies may appear hungrier and feed more during this time. The baby can be fussy and may cry when feeding while experiencing a growth spurt.
11. Preference for bottle-feeding
Image: iStock
Babies who are mostly fed from a bottle may prefer bottle-feeding to breastfeeding due to the bottle’s instant and continuous milk flow. They may also find it is easy to feed from a bottle since it involves minimal effort than feeding from the breasts.
12. Preference feeding from one side
Some babies tend to prefer one-sided feeding due to various reasons, and they may cry if you offer the other breast or change the breast during nursing sessions.
Related: Breastfeeding From One Breast: Causes, Side Effects And Tips
13. Cluster feeding in the evening
Babies may feed more before sleeping in the evening hours, and they can become fussy and cry if you end feeding before they feed enough. A slow letdown of milk during cluster feeding may also irritate the baby and make them cry.
14. Teething
Teething may cause swelling and pain in the gums. It can make the baby cry while nursing due to the discomfort in the gums.
15. Thrush
Image: Shutterstock
Thrush, also known as oral candidiasis, is a fungal infection caused by the yeast Candida albicans. You may notice whitish coating of the tongue and oral cavity in this condition. Babies with oral thrush may have difficulty breastfeeding due to mouth dryness, burning, or lack of appetite.
They may cry or become fussy due to thrush while feeding, and often the candida infection can spread to the mothers’ breasts while nursing if it is left untreated.
16. Stuffy nose
Babies may cry while breastfeeding due to breathing difficulties caused by nasal congestion. Common cold or flu can be the reason for congested or stuffy noses in many babies. Blocked nose due to an inappropriate breastfeeding position may also cause feeding problems.
Expert says
According to Naser Danan, MD, Pediatrics, UH Rainbow Northeast Pediatrics, Willoughby, using saline nose drops before each feeding can help babies with nasal congestion breathe better while eating (3).
17. Food sensitivity or allergy
Babies with food sensitivities or allergies may cry during breastfeeding due to gastrointestinal discomforts. Colic, vomiting, gagging, excessive gas, diarrhea, or skin rashes can be symptoms of sensitivity to foods in mom’s diet.
18. Ankyloglossia or tongue-tie
Tongue-tie is a condition wherein a tight and thick band of tissue tethers the tip or any part of the tongue to the mouth’s floor. Lip and buccal ties can also cause feeding challenges. This condition could affect babies’ ability to suck, and they may turn fussy or cry while breastfeeding.
This condition could affect babies’ ability to suck, and they may turn fussy or cry while breastfeeding.
19. Stress
Image: Shutterstock
Babies may feel stressed for various reasons, such as teething, physical illnesses, or even psychological problems, such as fear of being away from the caregiver or parent (separation anxiety). Stress may cause the baby to be irritated and often cry more than usual, including during the nursing sessions.
20. Tiredness
Illnesses or lack of sleep could make babies cry while feeding, and you may also notice them being more irritable in such situations.
Babies may become fussy or cry while breastfeeding due to various reasons. Some babies may go into a nursing strike or breastfeeding strike due to these factors. Breastfeeding strike is a sudden refusal of breastfeeding for several days. It is essential to identify the exact reason behind crying while nursing since adequate feeding is required for your baby’s growth and development.
Related: 8 Signs Of Overtired Baby And Tips To Put Them To Sleep
How To Prevent Crying While Nursing?
Sometimes, it can be difficult for parents to find and resolve the cause of crying while nursing. If your baby frequently cries while breastfeeding or if you are unable to identify the cause, seek help from a pediatrician or a lactation consultant.
The following ways may help calm a crying baby while nursing (1).
- Nurse when the baby is relaxed. You may choose before their sleeping time since babies are less likely to be fussy during this time.
- Take the baby outdoors and feed afterward.
- If the mother is stressed or depressed, the other family member or caregiver may carry the baby until the mom relaxes since babies can often sense emotions.
- Find a calm and dark feeding room or area to reduce distraction.
- Express and bottle-feed breast milk if the baby refuses to feed from the breast.
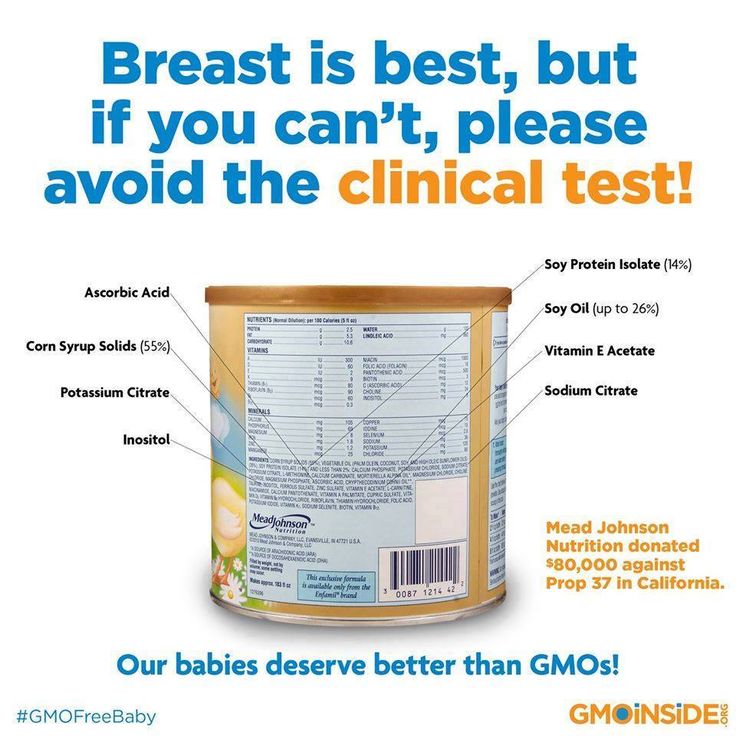
 Shift to formula milk only when there is not enough milk supply and after seeking advice from a lactation consultant or pediatrician.
Shift to formula milk only when there is not enough milk supply and after seeking advice from a lactation consultant or pediatrician.
Image: iStock
- Do not force the baby to feed if they refuse to feed.
- Feed from both breasts, and switch the breasts if they cry.
- Maintain an appropriate feeding position and change if required.
Quick tip
Make sure your baby sits as straight as possible when breast or bottle feeding to reduce the amount of air they swallow and so, to prevent them from crying (2).
- Burp the baby in between breasts and at the end of each feeding.
- Opt for surgical repair of tongue-tie after consulting a doctor.
- Treat stuffy nose, thrush, etc. to avoid feeding difficulties.
- Use comfort measures to calm and soothe the baby before continuing feeding.
- Maintain a healthy diet and drink enough water if you are a lactating mother.
 The maternal diet could be linked to food sensitivity in breastfed infants. Speak to a doctor if you suspect your baby is reacting to the maternal diet.
The maternal diet could be linked to food sensitivity in breastfed infants. Speak to a doctor if you suspect your baby is reacting to the maternal diet.
Related: Baby Crying: Types, Reasons And Tips To Cope With It
1. Is it normal if a baby cries while breastfeeding?
Babies may cry when breastfeeding if they feel uncomfortable. Improper airflow, acid reflux, satiety, and altered breast milk taste could result in a baby crying during nursing.
2. What should I not do when my baby cries while breastfeeding?
Do not stop breastfeeding immediately after the baby starts crying. Instead, offer them the other breast or try a different feeding position to see if it subsides the crying. In many cases, a change in breast or feeding position may work. If your baby continues to cry, express breast milk and offer them the bottle.
If your baby cries while breastfeeding, look for the causes such as acid reflux, overactive letdown, slow letdown, or not hungry. Some babies may also cry and fuss after they are done feeding. Teething, thrush, growth spurts, and preference for bottle-feeding or one breast can also be the reason for crying while nursing. You may feed the baby when they are hungry and relaxed. Seek suggestions from lactation consultants to manage overactive or slow letdowns with various feeding techniques. You may express and feed using bottles if the baby prefers to be bottle-fed.
Teething, thrush, growth spurts, and preference for bottle-feeding or one breast can also be the reason for crying while nursing. You may feed the baby when they are hungry and relaxed. Seek suggestions from lactation consultants to manage overactive or slow letdowns with various feeding techniques. You may express and feed using bottles if the baby prefers to be bottle-fed.
Key Pointers
- A baby can cry or become fussy while breastfeeding for various reasons such as overactive or slow letdown, not hungry, or acid reflux.
- Stuffy nose and teething can cause babies to fuss or cry while feeding due to nasal congestion or pain in the gums.
- You may feed on demand and address health issues to prevent cry or fussiness. Expressing and giving bottled breast milk can also help some babies.
References:
MomJunction's articles are written after analyzing the research works of expert authors and institutions. Our references consist of resources established by authorities in their respective fields. You can learn more about the authenticity of the information we present in our editorial policy.
You can learn more about the authenticity of the information we present in our editorial policy.
1. Crying and feeding issues; The Children and Young People Urgent Care Advisory Group
2. Breastfeeding challenges; Better Health Start for Life; NHS
3. What to Do For Your Baby’s Stuffy Nose; University Hospitals
The following two tabs change content below.
- Reviewer
- Author
10 Home Remedies For Acne During Pregnancy & Prevention Tips
10 Home Remedies For Acne During Pregnancy & Prevention Tips
When Is C Section (Cesarean Section) Done? Its Types & Risks
When Is C Section (Cesarean Section) Done? Its Types & Risks
Top 10 Baby Massage Oils: Know What's Best For Your Baby?
Top 10 Baby Massage Oils: Know What's Best For Your Baby?
Ectopic Pregnancy: Causes, Symptoms, Treatment, And Risks
Ectopic Pregnancy: Causes, Symptoms, Treatment, And Risks
HIV In Babies: Causes, Symptoms, Diagnosis And Treatment
HIV In Babies: Causes, Symptoms, Diagnosis And Treatment
Is Having A Watery Discharge During Pregnancy Normal?
Is Having A Watery Discharge During Pregnancy Normal?
Ovarian Cysts During Pregnancy: Types, Symptoms & Treatments
Ovarian Cysts During Pregnancy: Types, Symptoms & Treatments
Defiant Toddler: Causes And 11 Tips To Deal With Them
Defiant Toddler: Causes And 11 Tips To Deal With Them
Positive Coombs Test In Newborns: Causes And Tips To Follow
Positive Coombs Test In Newborns: Causes And Tips To Follow
Baby Fusses or Cries During Feeding: Causes & Solutions
Is your baby fussy every time you offer the breast? Do they cry, making it hard to breastfeed?
I’ve been there and know how it can be distressing when your baby is irritable while breastfeeding. It can make you question whether you’re doing something wrong and why the experience isn’t turning out how you imagined.
It can make you question whether you’re doing something wrong and why the experience isn’t turning out how you imagined.
To help set your mind at ease and offer you some hope, we’ll share everything we know about what makes a baby upset during breastfeeding.
We’ll help you determine the cause of your baby’s fussiness. We’ll also offer our solutions so your breastfeeding sessions can return to being a peaceful experience you both enjoy.
Causes of Baby Crying During Feeding
Half the battle is finding out why your baby is crying and fussing when they should be enjoying their time at the breast. You want to know your baby is getting enough milk and thriving. But it’s hard to be sure when they always latch on and off, crying in between.
Let’s discuss some possible causes.
1. Baby Isn’t Latching On
If your baby is fussing or crying, getting them to latch on to feed can be challenging. Whether overtired, overstimulated, or just plain hungry, a crying baby is unlikely to latch.
The Solution
Begin breastfeeding while your baby is calm and awake, before they get too hungry. Watch for early hunger cues such as rooting, smacking their lips, sucking their hands, sticking their tongue out, or waking from sleeping. Crying is a late sign of hunger.
Swaddling your baby and holding them close, dimming the lights, or moving somewhere peaceful and quiet might also help.
Another thing you can try is squeezing a few drops of milk onto your breast to entice your baby to latch on. The taste and smell of the milk might stimulate them to feed. Changing position or changing breasts can also work sometimes (1).
2. The Milk Flow Is Too Fast or Too Slow
Paying attention to when your baby starts to cry might shed some light on the reason.
If your baby is fussier in the morning, it could be that your overly full breasts release too much milk too quickly. Your breasts may have become engorged with milk during the night and your baby can’t cope with this forceful let-down.
Your breasts may have become engorged with milk during the night and your baby can’t cope with this forceful let-down.
Conversely, if they are fussier in the evenings, maybe the milk release is too slow and they get frustrated. They become impatient, waiting for the flow of milk that comes with the let-down, and start crying.
The Solution for Fast Milk Flow
A strong release of milk, or overactive let-down, can make your little one choke, gag, or cough when they’re feeding. They might unlatch from the breast because they don’t like or can’t cope with the fast flow. They could also be gulping a lot of air with the milk and getting gassy, which causes more upset.
These are some of the things you can do to counteract this:
- Express before feeding: Pumping some of your milk before feeding, or expressing by hand, can help slow down the flow. After you feel the first let-down pass and you see the flow is slowing, put your baby to your breast.

- Lie back when nursing: Adopting a laid-back feeding position with your baby lying on top of you can slow the flow. You could latch your baby on and then lie back against some cushions or pillows. Milk will flow against gravity and won’t pour down your baby’s throat.
- Burp regularly: When your milk is flowing fast, your baby may gulp lots of air while feeding. A gassy baby is a fussy baby, so burp them regularly, during and after the feed.
- Feed one side at a time: Alternate your breasts at each feed. That way, once the flow slows down on the breast your baby is feeding on, they might stop fussing.
- Take a feeding break: If your flow is too much for your little one to cope with, remove them from the breast for a few seconds. Let the excess milk leak onto a towel, and offer the breast again when it stops. This might make your baby fussier for a while, but it will pay off in the long run.
The Solution for Slow Milk Flow
Your baby is hungry, but your milk is not coming quick enough. Just as we can get “hangry” when we need food or drink and aren’t getting it, our babies can too!
Just as we can get “hangry” when we need food or drink and aren’t getting it, our babies can too!
Luckily, we have some things you can try to combat a slow flow or delayed let-down:
- Stimulate the flow: Either pumping or hand expressing a little milk before latching can kick-start your let-down reflex. Once you have a steady flow, then you can put your baby to your breast.
- Warm compress: Use a warm towel or compress for a few minutes to stimulate letdown. Place it on your breasts just before each feed.
- Massage: Massaging your breasts before and during a feed can help the milk flow faster.
- Try breast compressions: If you notice your baby is about to start fussing and might unlatch, squeeze your breast. This will give your baby a burst of milk, keeping them actively feeding.
- Get comfortable: Breastfeeding a fussy baby can be frustrating for you as well.
 Try and feed in a relaxing position, away from distractions. It’s a perfect time to just concentrate on your baby.
Try and feed in a relaxing position, away from distractions. It’s a perfect time to just concentrate on your baby. - Make sure your baby gets enough milk: All that fussing and crying might make your little one tired, and they may fall asleep at the breast before they’ve eaten enough. Try and stimulate them to continue feeding by tickling their foot or stroking their cheek. The more your baby feeds, the more milk you will produce.
- Some dos and don’ts: When breastfeeding, avoid smoking and alcohol. Also, try and steer clear of soda and coffee. All these could affect your milk production. Ensure you eat a balanced diet and stay hydrated, too (2).
3. Baby Is Going Through a Growth Spurt
There are times during a baby’s first year of life when they go through growth spurts. Their weight and length will increase, as will their head circumference.
Their weight and length will increase, as will their head circumference.
Your baby may want to feed more often during a growth spurt and can become fussy. It’s not uncommon for a baby to suddenly feed up to 18 times in 24 hours.
While one does not necessarily lead to the other, it makes sense that a growth spurt and sudden, frequent feeding go hand in hand. Your baby will need more milk to support the growth spurt, and nursing more will naturally boost your supply.
During this time, babies can also become fussier than usual. They might appear unsettled and clingy, and they may not sleep as well as usual.
Growth spurts generally happen several times during the first year. These are the ages when they are likely to occur:
- Two weeks old.
- Three weeks old.
- Six weeks old.
- Three months old.
- Six months old.
Not all babies will follow this timetable; some might have more growth spurts or they may be at different times. For some babies, there might be no change in their behavior when they have a growth spurt.
For some babies, there might be no change in their behavior when they have a growth spurt.
The Solution
During this time, follow your baby’s lead. Respond to their needs, whether it’s more feeds, extra cuddles, or just quiet time and a nap.
Your baby might get fussy if you aren’t producing as much milk as they want. It can take a day or so for your supply to catch up with the demand. The more you let your baby feed, the more milk your breasts will produce.
Your baby may seem hungry after normal feeding time, so don’t be afraid to nurse again. Keep yourself feeling good during this time by staying hydrated and eating balanced meals. Remember, you are not Superwoman; let family and friends help with chores and shopping while you spend time with your baby.
4. Baby Is Going Through a Developmental Stage
Your baby is constantly developing mentally and learning new skills as they go along. It can be a bit overwhelming and confusing for them, and there might be weeks when they are fussier than usual. Sometimes called the “Wonder Weeks,” it can explain mood changes in your baby (3).
Sometimes called the “Wonder Weeks,” it can explain mood changes in your baby (3).
You might find that during these periods, your baby becomes more curious and distracted while feeding. They might want to feed more or, conversely, not stay latched on long enough for a good feed. They can be cranky and fussy and cry a lot when you’re trying to breastfeed.
The good news is that these periods generally only last a few days before your baby returns to normal behavioral patterns.
Not all babies will fit into the pattern of wonder weeks and develop at different times.
The Solution
Feed your baby in a quiet room where there are likely to be fewer distractions. There’s nothing worse than having a situation where your little one latches on, then hears their dad or sees the dog and stops feeding (or worse yet, turns their head with your nipple still in their mouth!).
Trying to get your baby to pay attention can make them fussier and be a constant battle.
You might also find that your baby is fussier and wants to feed more often during these periods. Again, take your cue from them, and give them the extra time and attention they need.
5. Baby Needs to Burp
Babies often fuss, cry, or pull away from the breast when they need to burp. A fast flow of milk can exacerbate this. They can also swallow more air when they’re fussy or gulp down milk faster than usual if they’re over-hungry.
The Solution
Breastfed babies tend not to need burping as often as bottle-fed ones. However, there are times when gas can make them uncomfortable and they need to get it out.
If your baby is fussing, stop the feed and try and burp them. If you let them carry on feeding while they’re crying, then they can take in more air and make the problem worse. Eventually, it can end up with them spitting up.
It’s a good idea to burp your little one mid-feed, even if they don’t appear to be in too much discomfort. Try to do it when switching breasts or when your baby latches off the nipple.
Other Reasons for Crying During Breastfeeding
We’ve looked at some of the main reasons your baby might cry while breastfeeding. There are a few other things that can cause this, including:
- Baby prefers one side: Your milk supply might be better on one breast than the other. This may be apparent if your baby only fusses when fed on one side.
- Teething: This can be a painful and uncomfortable time for your baby, and they might fuss more when feeding. You might first realize it’s happening when they clamp down on your nipple and you feel the teeth through the gums. I’m all too familiar with that pain! But trust me, your baby isn’t trying to hurt you; they just want to relieve their pain (4).
- Baby has eaten enough: If your little one starts fussing toward the end of a feed, this might be a sign they’ve had enough. Try offering the breast again a few times. If they don’t want it, move on.
 If you have ruled out any other causes for their crying, their little tummy might be full.
If you have ruled out any other causes for their crying, their little tummy might be full. - Baby wants to be pacified: Your little one might be full but still wants to suckle. However, it can be frustrating for them when milk is still flowing. This could be an excellent time to offer a pacifier for them to suckle.
- Thrush: This fungal infection can affect your nipples or a baby’s mouth. If your baby has oral thrush, feeding will be uncomfortable, and they can get fussy. If you suspect this, contact your health care provider (5).
- Baby has a cold: Trying to feed and breathe through a stuffy nose simultaneously can be challenging for a little one. They will become fussy and break away from the breast a lot. Use a nasal aspirator to try to clear their nose, or ask your pediatrician for advice.
- Food sensitivity or allergy: While you might enjoy eating spicy food for dinner, your baby may not.
 The flavor of the food you eat comes through in your milk, and your little one might not always like the taste or the smell. You might notice they are fussier when you have consumed certain foods they don’t like or are allergic to (6).
The flavor of the food you eat comes through in your milk, and your little one might not always like the taste or the smell. You might notice they are fussier when you have consumed certain foods they don’t like or are allergic to (6). - Reflux: Although it’s not very common in breastfed babies, sometimes food comes back up from a baby’s stomach. This can make them cry and feel uncomfortable when feeding (7). Speak with your baby’s doctor if you suspect this is causing your baby to be fussy or cry during breastfeeding.
Feedback: Was This Article Helpful?
Thank You For Your Feedback!
Thank You For Your Feedback!
What Did You Like?
What Went Wrong?
Solutions to six breastfeeding problems in the first week
Are you having difficulty breastfeeding your newborn baby? Read on for expert advice on tackling the main challenges of the first week of breastfeeding.
Share this information
Cathy Garbin, child health nurse, midwife and lactation consultant:
Cathy, a mother of two, was a research fellow at the renowned Human Lactation Research Institute, founded by Peter Hartmann, for seven years, providing support to breastfeeding mothers in clinics and at home. Today, she still works as a family counselor, and also conducts seminars for attending physicians and speaks at international conferences. nine0003
Breastfeeding is not always easy, so if
you are having difficulty, know that you are not alone. A US study found that out of 500 new mothers surveyed, 92% experienced breastfeeding problems by the third day. 1 Fortunately, most early breastfeeding problems are easy to resolve. Below you can read recommendations for solving the main problems that mothers often face in the first week of feeding. nine0003
Problem #1. Breastfeeding hurts!
Pain during feeding is usually associated with tenderness or inflammation of the nipples, especially when milk "comes" on the second to fourth day after birth. 2 The baby will beg for a breast every couple of hours, and this can quickly aggravate the problem: some mothers' nipples crack, bleed, or blister. This is, of course, very annoying.
2 The baby will beg for a breast every couple of hours, and this can quickly aggravate the problem: some mothers' nipples crack, bleed, or blister. This is, of course, very annoying.
Solutions 3
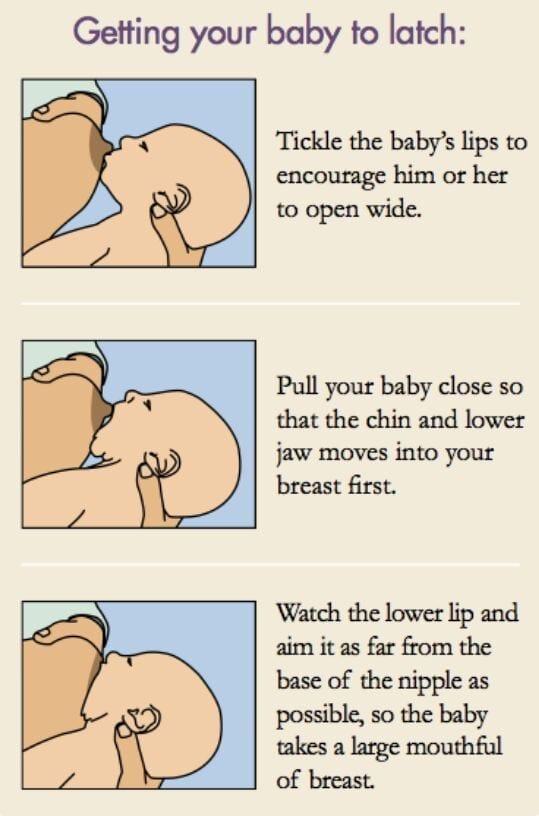
- Check how the baby latch on. An incorrect latch is one of the most common causes of pain during breastfeeding. A newborn baby should take most of the lower half of the areola (dark skin around the nipple) into his mouth, and your nipple should rest against his palate, supported from below by the tongue.
- Contact a lactation consultant or healthcare professional to make sure your baby's mouth and torso are properly positioned during feeding and there are no other latch-on problems. The doctor may also examine the baby's mouth for physical abnormalities. nine0032
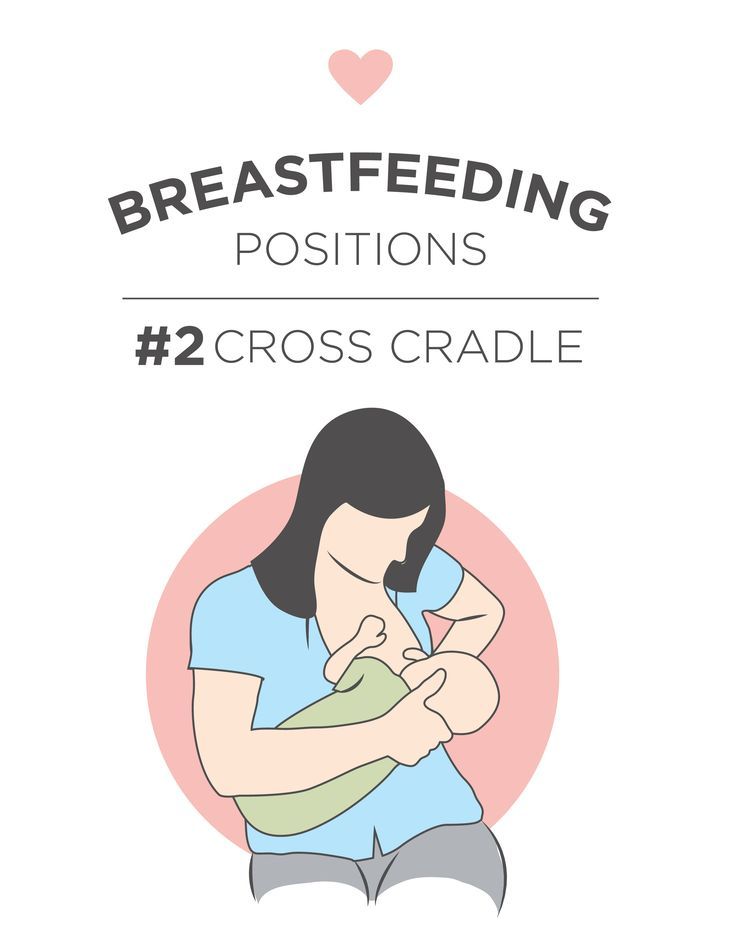
- Try other feeding positions. Reclining, cross cradle, underarm, or lying positions can relieve pressure on the most painful areas of your breasts.

- Gently wipe soaked nipples with water-soaked cotton swabs after each feed to remove milk residues that can cause infection.
- Air dry nipples or blot with a clean, soft muslin or flannel cloth to prevent bacterial growth in a humid environment. Use disposable or reusable bra pads to absorb leaking milk and remember to change them regularly. nine0032
- Soften your nipples. An ultra-pure lanolin treatment will help relieve inflammation and dry skin. You can also apply a few drops of your own breast milk to your nipples. In both cases, you do not have to wash your breasts before the next feeding. You can also apply refrigerated hydrogel pads* to your nipples. They soothe the nipples and help relieve pain during feeding, as well as speed up healing.
- Protect your nipples. nine0008 Nipple shields* protect the sore area from rubbing against clothing.
- Be patient. The inflammation usually resolves after a few days as your body adjusts to breastfeeding and your baby learns to suckle.

- Seek medical attention, if pain during feeding does not go away after a few days. Constant inflammation of the nipples may indicate an infection that requires prompt treatment.
Problem #2. Baby doesn't latch on properly
Some newborns do not latch on properly right away. Maybe both of you just need more time to learn how to breastfeed, or maybe the baby was born prematurely, feels unwell after a difficult birth, or mom has flat or inverted nipples.
Solutions
- Contact a lactation consultant or healthcare professional who can help identify the cause of the problem and suggest solutions. nine0032
- Flat or inverted nipples must be pulled out. Nipple formers* fit comfortably in the bra and apply gentle pressure to the nipples to help them come out for easier feeding.
- Try different positions and ways to support your newborn.
 The baby needs to feel supported. He must be comfortable and breathe freely in order to suckle properly. Do not hold the child by the head and do not put pressure on it. Lean back and let your child take the lead. This stimulates his natural reflexes and helps him find and latch on to his breasts. nine0013 4
The baby needs to feel supported. He must be comfortable and breathe freely in order to suckle properly. Do not hold the child by the head and do not put pressure on it. Lean back and let your child take the lead. This stimulates his natural reflexes and helps him find and latch on to his breasts. nine0013 4 - When feeding, try to find the optimal position. Instead of putting your baby on and off, stressing both of you, try to position him in a way that is easy and comfortable for him. Hold the torso and legs of the baby close to you, support him by the shoulders and hold him firmly so that he feels safe. Let the baby's head rest freely on your arm so that he can tilt it back slightly and breathe freely. The chin should be pressed against your chest. If these small adjustments don't make feeding more comfortable for your baby, seek help from a lactation consultant or healthcare professional. nine0032
- Use nursing pads. If your baby is having difficulty latch-on, a lactation consultant or healthcare professional may suggest trying nursing pads*.
 A nipple with an overlay is more convenient to take in the mouth, so it is larger and more rigid. Do not use nursing pads for a long time.
A nipple with an overlay is more convenient to take in the mouth, so it is larger and more rigid. Do not use nursing pads for a long time.
Problem #3. Not enough breast milk
You will produce little breast milk at the very beginning, as the hormonal changes that trigger milk production occur slowly and do not end until the second or fourth day after birth. nine0013 2 You may be worried that your baby is not getting enough milk, but in the early days his stomach is still too small and feedings are frequent, so don't worry. The only things to worry about these days are excessive weight loss, too few wet and soiled diapers, or signs of dehydration in the baby. For more information on how often a newborn should urinate and void, see Breastfeeding Newborns: What to Expect in the First Week. nine0003
Solutions
- Contact a Lactation Consultant or your healthcare provider who can determine if you have problems with milk production.
 The sooner you do this, the better.
The sooner you do this, the better. - Feed your baby on demand, not on a schedule. In the first week after birth, your baby will ask to breastfeed every two to three hours (or more often!), both day and night. Such frequent feeding helps to establish the production of breast milk. nine0032
- Take care of yourself. It's not always easy with a newborn, but try to rest whenever you can, eat right, and accept any help around the house or with older children that your loved ones can give you to fully focus on breastfeeding.
- Try expressing milk. If a baby is feeding frequently but not gaining any weight, a lactation consultant or doctor may recommend pumping to increase breast milk production. If milk is not coming out at all, you can try the Medela Symphony Dual Electric Clinical Breast Pump**. It features an Initiate program that mimics a baby's natural sucking rhythm for the first few days. nine0032
Problem #4.
 Breast full and heavy
Breast full and heavy Your breasts will become fuller and heavier as milk comes in.
If the baby suckles well and often, this should not cause any problems. However, in some women, the breasts become so full that they become hard and painful. This condition, called breast swelling, can cause discomfort. The swollen chest seems to be “burning”, now all the activity of your body is concentrated in it, resembling a busy traffic at rush hour. Fortunately, this condition usually resolves within 24 to 48 hours. However, due to the swelling of the mammary glands, the nipples can become flat and the baby may have difficulty latch-on. nine0013 5
Solutions
- Feed your baby often. Try to breastfeed at least 8-12 times a day. This is the main way to alleviate this condition. For more tips and tricks, see the article on Breast Swelling. 6.7
- Call your healthcare provider, if symptoms persist for more than 48 hours, you have a fever, or your baby is unable to breastfeed due to swelling.

Problem #5. Milk is leaking
Breast leakage is very common in the early days of breastfeeding when milk production begins. Milk may leak from one breast while you are feeding the other, when you sleep on your stomach, or when something accidentally triggers the milk flow reflex, such as when you hear a baby crying in a store. The leakage usually stops after about six weeks.
Solutions
- Protect clothes from stains will help disposable or reusable bra pads to be used day and night. nine0032
- Don't waste precious drops! Breast milk collection pads* fit inside the bra and allow you to collect any leaking milk. This is a very useful thing when there is too much milk and the pads are not absorbing well, or when one breast is leaking while you are feeding the other. If you want to save the collected milk, use only the milk collected at the feeding. Place it in a sterile container and refrigerate immediately if you are not supplementing with it right away.
 Collected milk must be used within 24 hours. The breast milk collection sleeves should not be worn for more than two to three hours at a time. nine0032
Collected milk must be used within 24 hours. The breast milk collection sleeves should not be worn for more than two to three hours at a time. nine0032
Problem #6. There seems to be too much milk
Sometimes when milk comes in, too much is produced! In the first few weeks there may be an overabundance of milk, but usually everything returns to normal soon. 7 Up to this point, the breasts may be heavy and sore almost all the time, even immediately after a feed, and a lot of milk may leak. A strong flush can cause a baby to cough or choke, vomit immediately after a feed, have tummy discomfort, or have hard, frothy, greenish stools. These are all signs that you are having too much milk, but the problem may resolve itself as your breasts get used to the new function. nine0003
Solutions
- Express some milk by hand at the beginning of each feed to ease the force of the flush.
- Try to feed while leaning back: this will help your baby control the flow of milk.
 The "cradle" position is also good: hold the baby obliquely by the shoulders so that the head can lean back slightly while on your arm. The torso of the baby will be located diagonally on you.
The "cradle" position is also good: hold the baby obliquely by the shoulders so that the head can lean back slightly while on your arm. The torso of the baby will be located diagonally on you. - Be kind and patient. Let your baby rest and absorb milk both during and after feeding. Don't move your baby too much or too fast, as this can make him nauseous. As the baby grows, he will learn to better cope with the rush of milk, which is likely to weaken anyway.
- Use the towel or swaddle to soak up spilled milk if the baby can't handle the flush, and place the breast milk collection pad on the other breast to catch any spilled milk. nine0032
- Contact a lactation consultant or doctor if problems persist after a few weeks . He will examine you and may suggest one-sided feedings or hourly breast changes (“breast duty”) to reduce your milk supply.
Related materials: Difficulties in breastfeeding in the next few weeks and problems with breastfeeding after the first month
Literature
1 Wagner EA et al. Breastfeeding concerns at 3 and 7 days postpartum and feeding status at 2 months. Pediatrics . 2013: peds -2013. - Wagner I.A. et al., "Breastfeeding Problems at Days 3 and 7 of a Child's Life and Type of Feeding at 2 Months". Pediatrix (Pediatrics). 2013:e865–e875.
Breastfeeding concerns at 3 and 7 days postpartum and feeding status at 2 months. Pediatrics . 2013: peds -2013. - Wagner I.A. et al., "Breastfeeding Problems at Days 3 and 7 of a Child's Life and Type of Feeding at 2 Months". Pediatrix (Pediatrics). 2013:e865–e875.
2 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
3 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women ’ s 2007;52(6):638-642. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
— Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
4 Colson SD et al. Optimal positions for the release of primitive neonatal reflexes stimulating breastfeeding. Early Hum Dev . 2008;84(7):441-449. - Colson S.D. et al., "Optimal Positions for Provoking Primitive Innate Reflexes to Induce Breastfeeding." Airlie Hume Dev. 2008;84(7):441-449.
5 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe Frauenheilkd. 2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations S -3 for the treatment of inflammatory diseases of the breast during breastfeeding. Geburtskhilfe und Frauenheilkünde. . ABM Clinical Protocol# 4: Mastitis , Revised March 2014.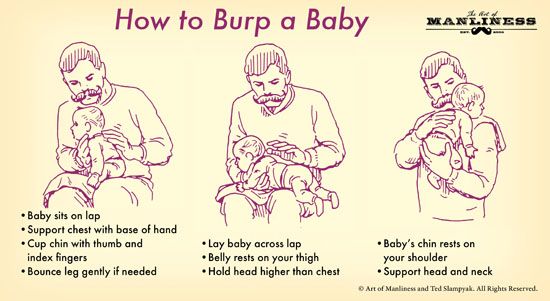 Breastfeed - 9020: 5): 5) H., Academy of Breastfeeding Protocol Committee, AVM Clinical Protocol #4: Mastitis, March 2014 edition of Brestfeed Med (Breastfeeding Medicine). 2014;9(5):239-243.
Breastfeed - 9020: 5): 5) H., Academy of Breastfeeding Protocol Committee, AVM Clinical Protocol #4: Mastitis, March 2014 edition of Brestfeed Med (Breastfeeding Medicine). 2014;9(5):239-243.
7 Academy of Breastfeeding Medicine Protocol Committee. ABM clinical protocol # 20: Engorgement. Breastfeed Med . 2009;4(2):111-113. - Protocol Committee of the Academy of Breastfeeding Medicine, "AVM Clinical Protocol No. 20: Engorgement, Revision 2016". Brestfeed Med (Breastfeeding Medicine). 2009;4(2):111-113.
Read instructions before use. Consult a specialist about possible contraindications. nine0017
* RU No. ФСЗ 2010/07352 of 07/19/10
** RU No. ФСЗ 2010/06525 of 03/17/2021 breastfeeding in the first month.
Share this information
Cathy Garbin, child health nurse, midwife and lactation consultant:
Cathy, a mother of two, was a research fellow at the renowned Human Lactation Research Institute, founded by Peter Hartmann, for seven years, providing support to breastfeeding mothers in clinics and at home.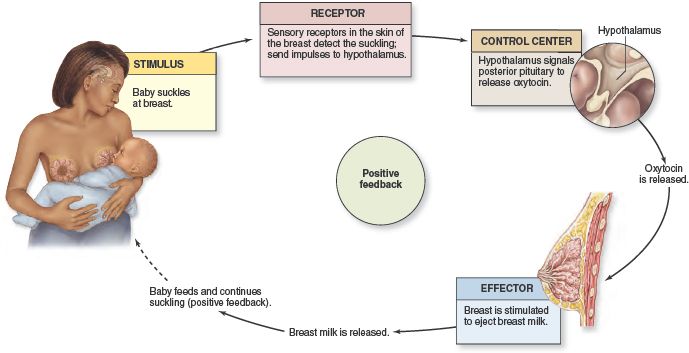 Today, she still works as a family counselor, and also conducts seminars for attending physicians and speaks at international conferences. nine0003
Today, she still works as a family counselor, and also conducts seminars for attending physicians and speaks at international conferences. nine0003
Breastfeeding is as much a skill as driving a car, and in the first month mother and baby may encounter some obstacles along the way. It takes time and experience to make it familiar to both of you. Solving breastfeeding problems in the first month helps to establish good milk production and increase the duration of breastfeeding in the future. Below you will find tips on how to overcome the main breastfeeding challenges that mothers often face from the end of the first week to the end of the first month after giving birth. nine0003
Problem #1. A painful lump appeared in the breast
Lumps and bumps in the breast of a nursing woman can appear for various reasons. One of the most common is blockage of the milk ducts, which results in a hard and painful lump that can become inflamed.
Solutions 1-3
- Massage the inflamed area, especially while breastfeeding or pumping, to clear the blockage.
 nine0032
nine0032 - Gently apply warm flannel to your breasts or take a warm shower before feeding to relieve discomfort.
- Continue breastfeeding as usual to avoid milk accumulation that can cause mastitis.
- Try to express milk from the inflamed breast after feeding to ensure that it is completely emptied. This will help to remove the blockage and restore the patency of the duct. See what breast pumps* Medela has to offer and choose the right one for you. nine0032
- Try ultrasound therapy. If you have repeated blocked ducts, your lactation consultant or healthcare professional may suggest this procedure to help restore milk flow. The procedure is performed by a physiotherapist.
- Call your healthcare provider, if you notice signs of infection (breast redness and tenderness or flu-like symptoms such as fever, aches, malaise and headache), or if you think the lump is not related to breastfeeding .
 nine0032
nine0032
Problem #2. The breast is red and sore
If one or both mammary glands are red and sore, and this is not due to blockage of the ducts, the possibility of mastitis, that is, inflammation of the breast tissue, is not excluded. Mastitis is characterized by redness, burning, and soreness of the breasts, combined with flu-like symptoms: You feel hot and cold, your joints ache, and your temperature rises above 38.5 °C (101.3 °F). Seek medical attention immediately if you experience these symptoms. Mastitis needs to be treated as soon as possible, as your condition can worsen in just a few hours. nine0013 3
Mastitis can be caused by the following causes:
- untreated blocked ducts,
- Bacteria introduced into the breast through cracked and damaged nipples,
- incorrect attachment of the child to the breast,
- long periods between feedings,
- breasts too full,
- wearing a bra that is too tight or that cuts into the skin,
- Abrupt weaning,
- excess milk.

Solutions 3
In addition to seeking medical attention:
- Continue to breastfeed or express milk frequently. Your milk is still safe for your baby. Its release will help eliminate blockage of the ducts and prevent painful accumulation of milk. Sudden cessation of feeding or pumping may exacerbate symptoms. After feeding, it is advisable to express any remaining milk. nine0029 Give the child the inflamed breast first. This way the child can empty it completely. If it hurts too much, start feeding on the healthy breast, and when milk begins to flow, go back to the first one.
- Have a good rest, drink and eat. You need to get enough fluids and good nutrition.
- Massage the sore area under a warm shower or apply a warm flannel or warm pack to clear the blockage and relieve symptoms before feeding or pumping. nine0032
- Apply a cooling pack after feeding, , to reduce inflammation.
Problem #3. My strength is running out
Breastfeeding in the first weeks can be very tiring and seem endless. The baby will ask for a breast every few hours, day and night, and you have not yet grown stronger after giving birth.
Solutions
- Take care of yourself. This may be easier said than done when you have a newborn in your arms, but still try to get as much rest as possible, eat healthy and regular meals, and drink plenty of water. Do not refuse the help of your partner, relatives and friends, or even hire an assistant if you can afford it. nine0032
- Feed lying down. This will allow you to relax and reduce stress on sore spots, stitches or c-section scars.
- Do not skip feedings. Your partner may offer to bottle feed your baby while you are resting. However, despite this temptation, it should be remembered that milk production is best established in the first four weeks through breastfeeding.
 When breastfeeding is well established, you can give your baby expressed milk, but before that, ask family or friends to help you with other things so you can fully focus on breastfeeding. nine0032
When breastfeeding is well established, you can give your baby expressed milk, but before that, ask family or friends to help you with other things so you can fully focus on breastfeeding. nine0032
Problem #4. How can I increase breast milk production?
It's easy to question whether your breastmilk supply is adequate, especially when your baby has developmental spikes between the third and fourth weeks. It may seem to you that the child asks for breasts more often because he does not have enough milk. However, if the number of wet and soiled diapers doesn't change—see Breastfeeding: What to Expect in the First Month—the baby is likely to breastfeed more often to calm down. The baby is surrounded by many new sounds and images that are easy to get tired of, and at the breast he feels safe. nine0013 4
Solutions 4.5
- Do not try to supplement your baby with formula, unless doctors are concerned about weight gain or fluid loss.
 Continue breastfeeding your baby. This will help naturally increase breast milk production.
Continue breastfeeding your baby. This will help naturally increase breast milk production. - Do not feed on a schedule. Feed your baby on demand. Thus, the production of breast milk will adapt to his needs. nine0029 Use the breast pump, , to help increase breast milk production while continuing to breastfeed.
Problem #5. I have too much milk
Hyperlactation, or too much milk, can also be difficult for you and your baby. You may experience discomfort from swollen and leaking breasts, and your baby may have difficulty latch-on, choke on the milk flowing too fast, and be unable to empty the breast properly. nine0013 6
Solutions
- Express some breast milk at the start of a feed to reduce the force of the flush. Don't pump too much as this can aggravate the situation - pump only as much as needed to ease the discomfort. Try hand pumping or use a breast pump (check out the Medela* breast pump range and choose the right one for you).

- Use the towel or pad to soak up excess milk, or place the milk collection pad** on the other breast while you breastfeed first. nine0032
- The child must feel supported. Hold him firmly (this gives a sense of security) and in a comfortable position so that he can turn his head. Talk to the baby during the first rapid flush, then he will not be frightened by surprise and will not push the breast.
- Contact a lactation consultant or health care professional who will monitor you and be able to suggest one-sided feedings or hourly breast changes (“breast duty”) to normalize your milk supply. nine0032
- Be patient . Problems with milk production usually go away after a few weeks.
Problem #6. I have different breasts!
You have noticed that the baby has a preference for one breast, or that one breast produces more milk than the other, and as a result the breasts have taken on different sizes and shapes. This happens quite often and does not pose any problems for breastfeeding. If this does not bother you or your baby, you can leave everything as it is. If this makes you uncomfortable, try the following tricks. nine0003
This happens quite often and does not pose any problems for breastfeeding. If this does not bother you or your baby, you can leave everything as it is. If this makes you uncomfortable, try the following tricks. nine0003
Solutions
- When feeding, offer your baby the less demanded breast first because babies usually suckle more vigorously at the beginning of a feed.
- Use the breast pump to increase breast milk production in the smaller breast.
- Don't give up on bigger breasts. Breastfeeding should continue with fuller breasts to avoid blocked ducts and mastitis.
- Seek medical attention. Sometimes an ear infection is the reason for a baby to latch on only one side. However, some positions may cause him discomfort, so try to keep the child more upright. In addition, a breast infection can change the taste of milk and cause milk to be rejected as well.

Issue #7. A blister has appeared on the nipple
With frequent feeding, sometimes painful friction occurs, and a blood bubble may appear on the breast,
nipple or areola. nine0013 7
Solutions
- Ask a lactation consultant or specialist to check the baby's latch on. A shallow grip can cause blistering of the nipples and areolas.
- Talk to your doctor about what medication you can take to relieve pain if needed.
- Try other feeding positions to avoid pressure on the painful area. nine0032
- Lubricate inflammation with pure lanolin.
- Use the Breast Pads** to avoid rubbing your blister with clothing and help it heal faster with air circulation, or try cooling hydrogel pads** to help relieve pain and promote healing.
- Try expressing milk. Using a breast pump can be an alternative way to get breast milk without bladder irritation.
 Choose the correct funnel size so that the nipple can move freely and the bubble does not rub against the walls of the tunnel. nine0032
Choose the correct funnel size so that the nipple can move freely and the bubble does not rub against the walls of the tunnel. nine0032 - Do not pierce the vial as this may lead to infection.
- Seek medical attention, if the problem persists and causes you pain.
Issue #8. Painful white spot on nipple
When the opening of the milk duct is blocked by milk or a thin layer of skin grows over it, a small white or yellowish spot may appear on the tip of the nipple. For some, these blocked ducts, sometimes called milk vesicles or blisters, cause pinpoint pain, especially during feeding or pumping. Others do not experience any discomfort. White blisters may persist for several days or weeks until the skin breaks and hardened milk comes out. nine0013 8
Solutions
- Follow the tips above to solve friction bubble problems.
- Remove the blockage, if you see that the milk cork is starting to bulge.
 Try to squeeze it out very gently with clean nails.
Try to squeeze it out very gently with clean nails. - Continue breastfeeding or pumping, to clear the milk duct. If the milk duct clears during feeding, it will not harm the baby in any way. nine0032
- Apply hot wet flannel to the vial just before feeding or pumping. This will help open the blocked duct. You can also try rubbing the area quickly with a clean, damp cloth.
- Hand express some milk before feeding, trying to push out hardened milk clots. If this does not help, feed the baby or express milk as usual. Repeat several times a day.
- Soak a cotton swab with olive oil and place it in the bra, pressing it against the bubble nipple. This will help soften the skin.
- Seek medical attention, if problem persists. Your doctor may remove the plug with a sterile needle. This should be done immediately after feeding, when the bubble is as inflated as possible.

Issue #9. My nipples hurt while breastfeeding
At the start of breastfeeding, my nipples may become more tender, sore, and even inflamed, but this usually goes away after a few days. If your baby's latch is checked by a specialist and the inflammation persists or the nipples hurt with every feeding, you may need medical attention to resolve this problem. nine0013 2.7
The following symptoms and signs that appear on one or both breasts during or after feeding may indicate a bacterial infection or thrush:
- burning, itching or moderate to severe pain in the nipples
- pain in nipples worse on contact with clothing,
- nipple pain persists despite attempts to attach baby differently,
- nipples hurt to touch, nine0029 stitching, shooting, burning or deep aching pain,
- chest pain during feeding and almost an hour after,
- hot pink nipples,
- discoloration and texture of the areola (hot pink, darkening, dryness or peeling),
- white rash on chest or areola.

Also check if your child has the following symptoms and signs:
- hard white patches or coating on the tongue,
- white indelible spots on the cheeks,
- bright red spotted rash on buttocks not helped by diaper rash creams.
Solutions 7
- Seek medical attention. He will most likely suggest testing for infections to make a diagnosis. Bacterial and fungal (yeast) infections are treated differently, so appropriate treatment should be started as soon as possible. There are other reasons that can cause similar nipple pain, such as eczema, psoriasis or vasospasm (narrowing of the blood vessels) in the mother and problems with latch or tongue frenulum in the child. Therefore, it is very important to make an accurate diagnosis. nine0032
- Strict hygiene. Wash hands before and after feeding and applying any medication, and after changing diapers. Change bra pads regularly, wash bras, tank tops and towels in high temperature water, thoroughly wash breast cups and anything your baby puts in her mouth, such as nipples.

- Let the nipples dry after feeding, since all infections love a warm and humid environment. nine0029 See your doctor again if there is no improvement after a few days. Do not let the problem run its course, otherwise the situation may worsen.
Related materials. Breastfeeding: what to expect in the first month
Breastfeeding: what to expect after the first month
Breastfeeding problems after the first month
Literature
1 Academy of Breastfeeding Medicine Protocol Committee. ABM clinical protocol # 20: Engorgement. Breastfeed Med. 2009;4(2):111-113.- Breastfeeding Academy Protocol Committee, "AVM Clinical Protocol #20: Breast engorgement". Brestfeed Med (Breastfeeding Medicine). 2009;4(2):111-113.
2 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe and Frauenheilkunde . 2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations S -3 for the treatment of inflammatory diseases of the breast during breastfeeding. Geburtskhilfe und Frauenheilkünde. ABM Clinical Protocol# 4: Mastitis , Revised MARCH 2014. . 23 : 50202 Med 9020 (5) H., Academy of Breastfeeding Protocol Committee, AVM Clinical Protocol #4: Mastitis, March 2014 edition of Brestfeed Med (Breastfeeding Medicine). 2014;9(5):239-243.
2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations S -3 for the treatment of inflammatory diseases of the breast during breastfeeding. Geburtskhilfe und Frauenheilkünde. ABM Clinical Protocol# 4: Mastitis , Revised MARCH 2014. . 23 : 50202 Med 9020 (5) H., Academy of Breastfeeding Protocol Committee, AVM Clinical Protocol #4: Mastitis, March 2014 edition of Brestfeed Med (Breastfeeding Medicine). 2014;9(5):239-243.
4 Kent JC et al. Principles for maintaining or increasing breast milk production. 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". F Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121. nine0203
5 Amir L. Breastfeeding managing ‘supply’ difficulties. Aust fam physician .