Baby eczema food allergies
Why Eczema Increases Your Baby's Risk of Developing Food Allergies – Lil Mixins
Now reading: Why Eczema Increases Your Baby's Risk of Developing Food Allergies
PrevNextEczema and food allergies are linked together. Eczema is a sign that your baby’s immune system is over-reactive. The more severe the eczema is, and the earlier it starts, the more the immune system is going crazy, and the more likely a baby is to develop food allergies. An immune system that is overactive is more likely to mistake harmless food as a danger.
Eczema also makes a bad situation worse. Eczema leaves cracks in your baby’s skin for food protein to sneak through. Eczema skin also gets infected easily, and infected eczema skin makes the immune system rev-up even more. Finally, the act of scratching itself can also activate the immune system.
What is Eczema?
Eczema is the “itch that rashes.” Eczema always begins with itching. Your baby’s skin itches either because it is very dry or because of a hidden immune reaction to a trigger like pollen, mold, or milk.
The hallmark of eczema is persistent red, dry skin on the face, especially the cheeks and forehead, in the arms near the elbows and wrists, and behind the knees as a baby starts to crawl. If a baby has enough hand control to scratch, the itchy skin can become thickened and scaly.
How Eczema Cracks in the Skin Can Cause Food Allergies
Many doctors are convinced cracks in eczema skin are the number one way that eczema causes food allergies and they have called it the Dual Exposure Hypothesis.
Eczema causes itching and dry skin. Very dry skin, or skin that has been scratched enough, will develop cracks. Some of these cracks are too small to see, others bleed or have scabs. When babies get food all over themselves, or even just crawl around, bits of food or dust get into those cracks.
A baby’s immune system will get scared by protein that it thinks broke through the skin. Once the immune system learns to be scared, it thinks harmless food is dangerous. This is what a food allergy is.
How Eczema Infections Can Cause Food Allergies
Every person’s skin is covered in bacteria, viruses, and fungi. One bacteria that is found on everyone is staph A. This bacteria is usually harmless, but when skin gets dry or cracked, like on babies with eczema, staph A jumps at the chance to spread out.
Staph A is very dangerous if it gets into your blood, and your body knows that. If staph A infects dry skin, your baby’s immune system will go into attack mode, flooding the body with immune cells.
In the LEAP study on peanut allergy prevention, doctors saw that almost all of the children with eczema who developed peanut allergy had a staph A infection. The kids with eczema but no infection had far fewer peanut allergies.
When the immune system is on high alert, it does a bad job of telling friend from foe, and makes the mistake of a food allergy.
How Eczema Scratching Can Cause Food Allergies
The weirdest way in which eczema itching causes food allergies is the act of scratching.
New research, so far only done in mice, at Boston Children’s Hospital showed that scratching the skin increases the chance of allergic reactions to foods, including anaphylaxis. The study showed that when you injure your skin by scratching, the immune system releases certain immune cells in the small intestine. Putting so many unnecessary immune cells in the small intestine can cause them to overreact to any food proteins that are undigested, leading to a food allergy.
What Can You Do to Stop Eczema from Causing Food Allergy?
Because eczema usually develops way before a baby starts eating solid food, your first priority should be to prevent or control eczema flares so that your baby’s skin doesn't have cracks, doesn’t get infected, and so that they don’t scratch.
The second most important way to stop eczema from causing food allergies is to train your baby’s body to recognize foods as safe and harmless. Early, regular feedings of nuts, eggs, peanut, dairy, and wheat can train your baby’s immune system not to have allergic reactions to food.
Eczema and Food Allergies in Infants
A breakdown of the skin barrier and inflammation in the skin that occurs in eczema could play a key role in triggering food sensitivity in babies, a new study reveals. Scientists say this finding indicates that food allergies may develop via immune cells in the skin rather than the gut, highlighting eczema as a potential target for preventing food allergy in children.
A link between eczema and food allergy has been known for some time, but researchers from King’s College London and the University of Dundee say this study, published in the Journal of Investigative Dermatology, adds to growing evidence of the skin barrier’s role in this process.
Almost 1 in 12 children in the UK have a food allergy and 1 in 5 suffer from eczema. Both diseases have a significant impact on patients and their families, often requiring treatment and in severe cases hospitalization.
Previous studies show that people with a skin barrier defect such as eczema do not have adequate protection against environmental allergens. In this study, funded by the Food Standards Agency, Medical Research Council, and the National Institute for Health Research (NIHR), researchers found that infants with an impaired skin barrier, especially if they also have eczema, are over six times more likely than healthy infants to be sensitized to a variety of foods such as egg, cow’s milk and peanut.
In this study, funded by the Food Standards Agency, Medical Research Council, and the National Institute for Health Research (NIHR), researchers found that infants with an impaired skin barrier, especially if they also have eczema, are over six times more likely than healthy infants to be sensitized to a variety of foods such as egg, cow’s milk and peanut.
The researchers at King’s and Dundee analyzed over 600 three-month-old babies from the EAT (Enquiring About Tolerance) Study who were exclusively breastfed from birth. They examined the infants for eczema, tested how much water the skin was able to retain, and screened for gene mutations associated with eczema. They then carried out skin prick tests to see whether the infants were also sensitized to the six commonest allergenic foods. They found that egg white was the most common allergen, followed by cow’s milk, and peanut. They observed that the more severe the eczema, the stronger the correlation to food sensitivity, independent of genetic factors.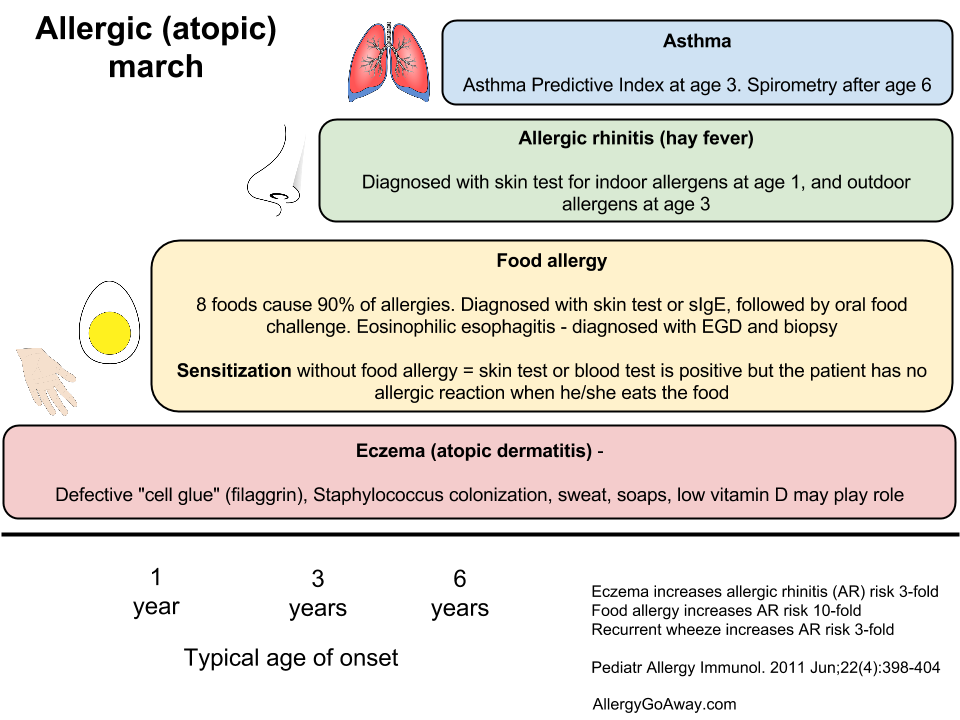 The researchers cautioned, however, that food sensitivity does not always lead to clinical allergy and further follow up of the EAT Study children is currently underway.
The researchers cautioned, however, that food sensitivity does not always lead to clinical allergy and further follow up of the EAT Study children is currently underway.
As the infants involved in the study were exclusively breast-fed, and therefore had not ingested any solid foods yet, this suggests that active immune cells in the skin, rather than the gut, may play a crucial role in food sensitization. It is thought that the breakdown of the skin barrier in eczema leaves active immune cells found in skin exposed to environmental allergens – in this case food proteins – which then triggers an allergic immune response.
Dr Carsten Flohr, NIHR Clinician Scientist and Senior Lecturer at King’s College London and Consultant at St John’s Institute of Dermatology at St Thomas’ Hospital, said: ‘This is a very exciting study, providing further evidence that an impaired skin barrier and eczema could play a key role in triggering food sensitivity in babies, which could ultimately lead to the development of food allergies.
‘This work takes what we thought we knew about eczema and food allergy and flips it on its head – we thought that food allergies are triggered from the inside out, but our work shows that in some children it could be from the outside in, via the skin. The skin barrier plays a crucial role in protecting us from allergens in our environment, and we can see here that when that barrier is compromised, especially in eczema, it seems to leave the skin’s immune cells exposed to these allergens.
‘It opens up the possibility that if we can repair the skin barrier and prevent eczema effectively then we might also be able to reduce the risk of food allergies.
eczema | Nestlé Health Science
- Nestlé Health Science
- health care
- Eczema
Eczema - a typical inflammatory skin disease accompanied by intense itching, which is characterized by red or brownish, dry, cracked and scaly skin, which is especially itchy at night. In children, eczema usually appears on the face, scalp, and outer surfaces of the limbs.
In children, eczema usually appears on the face, scalp, and outer surfaces of the limbs.
Why does my child have eczema?
The exact causes of eczema are not well known, but in many cases your child may have eczema due to a food allergy, eg Cow's Milk Protein Allergy (CMP) . Many children who develop eczema are allergic to one or more allergy-causing substances during infancy. If there is a family history of allergic reactions, such as asthma or a pollen allergy, your child may be more likely to develop eczema.
Baby eczema is one of the most common symptoms of CMPA
Symptom analysis
Could this be a manifestation of CMPA?
Children with CMPA usually have more than one symptom, and these symptoms can be very different from each other.
If you think baby has eczema it could be CMPA.
You may have noticed other symptoms (other than eczema) that may affect other parts of your child's body.
As a simple and easy way to check for typical symptoms associated with CMPA, you can use our Symptom Checker.
It will allow you to select all cow's milk symptoms your baby may have. You can then discuss this with your doctor.
In any case, if you have any doubts or concerns about your child's health, you should consult with a healthcare professional as soon as possible.
Other symptoms of cow's milk protein allergy
ANAPHILACTIC SHOCK
View product
CRYING AND COLIC
View product
CONSTIPATION
View product
COUGH
View product
DIARRHEA
View product
GROWTH DISTURBANCE
View product
urticaria
View product
REFUSAL TO FOOD
View product
RASH
View product
REFLUX AND BUCK
View product
Runny nose and sneezing
View product
EDITEC
View product
VOMITING
View product
HRIP
View product
IMPORTANT NOTE: : It is possible to continue breastfeeding if the infant is allergic to cow's milk protein. To do this, the mother needs a special diet with the exclusion of all sources of cow's milk protein. Only if these measures do not bring the desired effect, the doctor recommends the use of a special therapeutic mixture intended for children from 0 to 1 year old. It is important to follow the correct methods of preparing the mixture: using boiled water, sterilized bottles and following the rules for diluting the mixture. Medicinal mixtures intended for diet therapy of CMPA should be used under the supervision of a physician.
To do this, the mother needs a special diet with the exclusion of all sources of cow's milk protein. Only if these measures do not bring the desired effect, the doctor recommends the use of a special therapeutic mixture intended for children from 0 to 1 year old. It is important to follow the correct methods of preparing the mixture: using boiled water, sterilized bottles and following the rules for diluting the mixture. Medicinal mixtures intended for diet therapy of CMPA should be used under the supervision of a physician.
It is useful to know about eczema ( EKSEM)
Useful information about the Eczema - the information sheet of the Norwegian Astmatics and Allergies
9
Eczema is the general term for various itchy skin conditions. The most common forms of eczema are atopic, occupational (contact), seborrheic, and childhood. Atopy means "difference". In this case, it refers to differences in skin properties and describes hereditary allergic eczema.
In this case, it refers to differences in skin properties and describes hereditary allergic eczema.
Eczema may be chronic ie. with a long, or acute form of the course of the disease and in most cases is characterized by improvement in the summer and deterioration in winter. The chronic form is characterized by the appearance of a rash with itching. The result of scratching is often the formation of thickened areas of the skin that crack easily. Acute eczema is characterized by itching, redness and swelling of the skin with the possible formation of watery blisters.
In eczema, there is a deterioration in the body's defense against infections, which easily leads to infectious inflammation, which can lead to a worsening of eczema.
Symptoms of eczema
Atopic eczema results in itchy, dry skin.
New or recurrent contact eczema is characterized by itching, redness and swelling of the skin with the formation of small and large blisters, as well as wet sores in places of direct exposure to the allergen. With prolonged contact eczema, the skin becomes increasingly dry and cracked. Severe itching is common. In the initial stage, eczema is observed only on the area of \u200b\u200bthe skin that was exposed to the allergen, but then the rash can spread to other areas.
With prolonged contact eczema, the skin becomes increasingly dry and cracked. Severe itching is common. In the initial stage, eczema is observed only on the area of \u200b\u200bthe skin that was exposed to the allergen, but then the rash can spread to other areas.
With seborrheic eczema in infants, there is the formation of oily, red skin covered with greasy crusts on the forehead, head, face, as well as in skin folds on the neck and in the perineum. In adults, it appears as scaly, red, oily skin on the central areas of the face, on the head, behind the ears, and on the chest.
Baby eczema is accompanied by the formation of red, smooth, sometimes wet areas of the skin in diaper wear areas.
Who can get eczema?
Atopic eczema primarily affects young children. It is estimated that about 15% of Norwegian children suffer from eczema. Often the disease occurs in children in the first months of life, in 60% of them it disappears by the age of four. However, recurrence of the disease may occur in adolescence or adulthood.
However, recurrence of the disease may occur in adolescence or adulthood.
Contact eczema is uncommon in young children, but it has become more common since school age. Ear piercings, body piercings and base metal contact with the skin are responsible for a significant increase in nickel contact allergies. Getting a tattoo can lead to allergic contact eczema, which can occur weeks or even months after getting a tattoo. Hair coloring is also an increasingly common cause of eczema, especially as more and more young people dye their hair.
Seborrheic eczema is relatively common. Eczema can appear as early as the first months of life, but usually occurs in adults.
Causes of eczema
The cause of atopic eczema is unknown. Allergies can play a role, but only in conjunction with other factors. The disease has a connection with heredity and the environment. The presence of atopic diseases in other family members (asthma, eczema or allergic rhinitis) is common.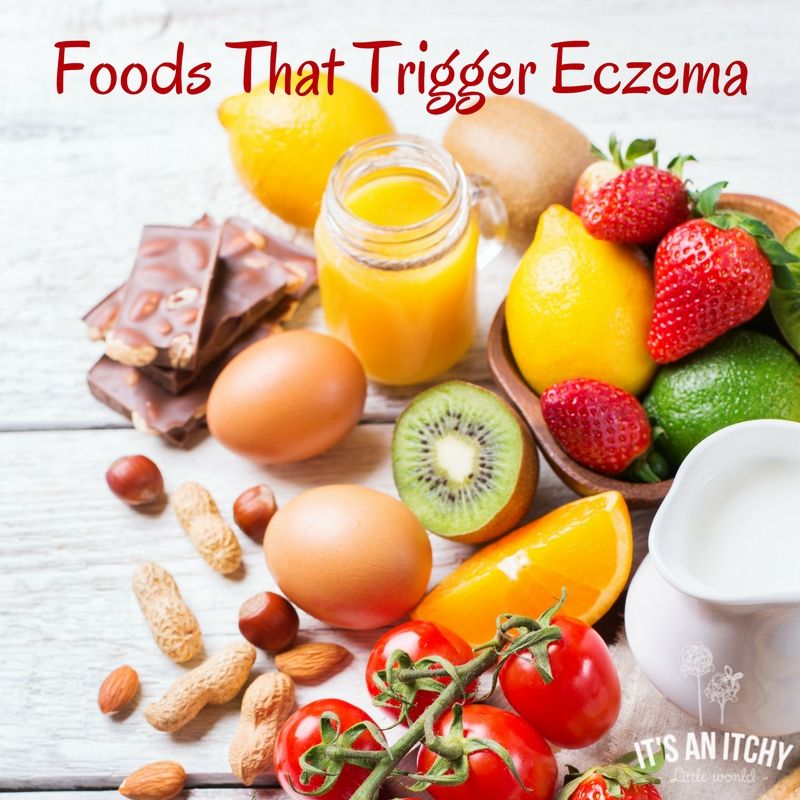 In 20-30% of patients, allergies can be detected, which for some of them may be the cause of eczema. Food allergies are never the only cause of eczema.
In 20-30% of patients, allergies can be detected, which for some of them may be the cause of eczema. Food allergies are never the only cause of eczema.
Seborrheic eczema is not caused by hypersensitivity, but by a painful reaction in the sebaceous glands, possibly caused by a specific yeast usually found on the surface of the skin. This form of eczema is especially prone to people with oily skin and increased productivity of the sebaceous glands.
Contact eczema occurs when the skin reacts to contact with certain substances. The reaction may be allergic or non-allergic. A non-allergic reaction occurs in direct contact with skin irritating substances such as detergents or disinfectants. An allergic reaction is caused by allergenic substances such as nickel, chromium, rubber, formaldehyde and perfumes. Paraphenylenediamine (PPD) is one of the substances frequently associated with allergic contact eczema. PPD is found in many types of hair dye.
Childhood eczema is caused by irritants found in urine and feces.
Treatment of eczema
In the treatment of eczema, the most important thing is hygiene, the systematic use of creams and ointments to prevent drying of the skin, refraining from scratching, reducing exposure to irritants and refraining from eating foods known to be allergic. Sunlight and salt baths work well for mild to moderate eczema. Regular bathing with calcium permanganates gives a good preventive effect.
However, in most cases a cortisone ointment is necessary. The indicated treatment will give the desired result, provided that the correct drug is applied to the appropriate area of \u200b\u200bthe body at the prescribed frequency. Once control of eczema is established, it is important to reduce the concentration of cortisone ointment, and, if necessary, increase the intervals between applications of the ointment. Proper use of cortisone ointment does not lead to negative effects. The attending physician will give you the necessary recommendations for the use and reduction of the concentration of the drug.
In general terms, we can say that it is necessary to use strong drugs for a sufficiently long period of time. By opting for weaker drugs, you will not be able to get eczema under control. In this case, the whole process of cortisone treatment may be in vain. Often this leads to increased eczema. It is important to remember that the poor effect of cortisone ointment is due to infection in the eczema itself, which should be treated with antibiotics, both locally and in general.
In the event of a new flare-up of eczema in a child with a previous history of the condition, treatment may be initiated with cortisone group 2 or 3. Once the condition has stabilized, application may be made less frequently (at intervals of 2-3 days). With further improvement in the condition, you can switch to a weaker ointment in order to eventually switch to applying the drug with an interval of 2-3 days.
After healing of eczema, it is recommended to continue applying the drug 1-2 times a week for at least 2-4 weeks in order to achieve the best result. It is also recommended to use a moisturizer in the morning and evening, as well as every time after taking a bath or shower, even during periods without eczema.
It is also recommended to use a moisturizer in the morning and evening, as well as every time after taking a bath or shower, even during periods without eczema.
Children suffering from eczema that regularly flares up and worsens benefit from calcium permanganate baths even during good times. During periods of active eczema, baths with calcium permanganate can be done every day or every other day.
Cortisone-free anti-eczema ointments (Elidel®, Protopic®) are good alternatives to try for chronic eczema. These ointments are applied daily, twice a day. The advantage of these ointments is that they do not affect the thickness of the skin even with prolonged use, and also that they can be used in cases where treatment with cortisone ointments does not lead to the desired result and control of eczema is not established by treatment with cortisone ointments without risk. side effects.
For skin infections, the infection itself must be treated first, and then the above remedies should be applied.
Medical light or climate treatments for eczema may work. However, some patients may experience a temporary increase in eczema, which is probably due to sweat irritation. In addition, such treatment requires a lot of money and time, which makes it unacceptable for school-age children. This treatment is carried out exclusively by doctors specializing in skin diseases.
Achieving positive results depends on how well the patient is informed about the treatment. Eczema can be a very debilitating disease, but early treatment can in most cases bring it under control. Fortunately, the disease eventually subsides on its own, and 80% of patients recover by the age of 18. There is evidence to suggest that quality treatment of eczema leads to an improved prognosis.
Aggravating factors
Rough, tight clothing, rough wools, polyester, heavily dyed fabrics, moisture, stress, infections, food, chlorinated water, tobacco smoke, perfumes, allergies, alkaloid soaps, degreasing chemicals and exposure to heat.
The child knows what clothes cause itching!
Prevention of eczema
Prevention of eczema by monitoring the mother's diet during pregnancy, or after the birth of the child, has no effect on the development of atopic eczema in the child. Research shows that symptoms of atopic eczema may be delayed in some cases in children who are breastfed for the first four to six months of life.
Where to get help
For mild sporadic eczema in children, getting advice from a nurse may be enough. In more complex cases, you should contact your doctor, who, if necessary, will write a referral to a specialist. The hospital free choice system in Norway allows for informed choice. On the Internet site www.frittsykehusvalg.no and free of charge on 800 41 004, you can find out about available eczema treatment sites and your rights in choosing a hospital.
People suffering from eczema and other skin diseases, as well as people who work with this group of patients, can communicate with specialists at the skin disease clinic, Villa Derma, Oslo University Hospital, by contacting the “skin phone” 23075803 , open for calls three hours a week according to the following schedule: Tuesday and Friday from 8 am to 9 am, Thursday from 12 am to 1 pm (check that this schedule is correct!).











