How to feed a baby with tracheomalacia
Tracheomalacia In Infants | Children's Hospital Colorado
Aerodigestive
We specialize in the big things, the small things and everything in between.
Would you like to learn more about us?
Aerodigestive Program
Ready to schedule an appointment?
Schedule online
What is tracheomalacia?
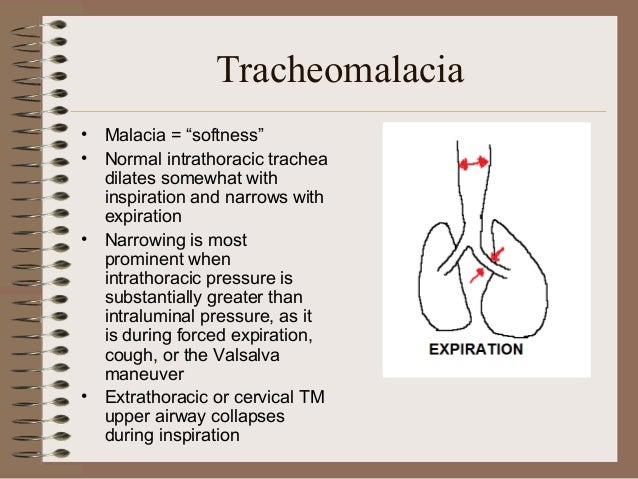
The trachea (or windpipe) is a major part of the respiratory system, carrying air in and out of the body. It is supported by several rings of cartilage that help it stay open when we exhale so air can leave the body. Tracheomalacia occurs if the cartilage cannot support the opening, which can close to half of its normal size or smaller.
Tracheomalacia is often seen between 4 and 8 weeks of age, when babies start to breathe enough air to produce a wheezing sound. Babies are typically born with the condition but usually do not have symptoms in the first month of life. Sometimes, a child can develop tracheomalacia later in infancy or childhood.
Tracheomalacia is often benign and many children will outgrow it. It often occurs with other conditions, including tracheoesophageal fistula, chronic lung disease of infancy and aspiration from gastroesophageal reflux. However, tracheomalacia can cause ongoing, sometimes severe issues with cough, recurrent wheeze, pneumonia and apnea.
What causes tracheomalacia?
Tracheomalacia has multiple causes, but most children are born with the condition. Children who have defects in the cartilage in their trachea have Type 1 tracheomalacia. If a child's tracheomalacia is due to other causes of airway compression, like abnormally formed or malfunctioning blood vessels in their trachea, it is Type 2 tracheomalacia. This is common after the repair of a tracheoesophageal fistula (TEF) or abnormal blood vessel problems (vascular ring) in the chest.
Who gets tracheomalacia?
There is no way to predict who will have tracheomalacia. It occurs evenly in males and females and in all races. Evidence suggests that it is not genetic, so there are no tests that can be run on parents to determine if their child will have it.
Evidence suggests that it is not genetic, so there are no tests that can be run on parents to determine if their child will have it.
What are the signs and symptoms of tracheomalacia?
- Noisy breathing, especially a wheezing sound
- Breathing problems that get worse with activity or colds
- High-pitched breathing
- "Happy wheezing" (children have normal oxygen levels and disposition, unlike wheezing in asthma or cystic fibrosis)
- No improvement in wheezing with bronchodilator therapy
- Normal vital signs despite respiratory symptoms
- Recurrent pneumonia
- Chronic cough
- Apnea in infancy
What tests are used to diagnose tracheomalacia?
Doctors will often use fluoroscopy, an X-ray that shows movement and allows doctors to see how your child's trachea looks while breathing in and out. It will also help doctors see what type of tracheomalacia is present and the cause.
Other tests that can be helpful when diagnosing tracheomalacia include: CT scans (a test that combines a lot of X-ray images to show an entire area of the body in detail), pulmonary function tests (tests that show how much air a child can breathe in and out), and bronchoscopy or laryngoscopy (tests in which a doctor uses a tiny camera to see the inside of a child's airways). Many times flexible bronchoscopy (.pdf) is required for diagnosis and to determine the severity of tracheomalacia and its impact on breathing.
Many times flexible bronchoscopy (.pdf) is required for diagnosis and to determine the severity of tracheomalacia and its impact on breathing.
How do providers at Children's Hospital Colorado make a diagnosis?
Providers will do a physical exam and ask about the child's symptoms and health history. They will also measure the levels of oxygen in your child's blood, which will help them decide if the symptoms are caused by tracheomalacia or a different condition. They may also use one or more of the tests above to help make the diagnosis.
How is tracheomalacia treated?
Tracheomalacia often improves on its own as babies get older and their bodies continue to develop. The condition is entirely gone by the time most children turn 3 years old. Humidified air and careful feedings are typically enough to relieve symptoms.
Severe tracheomalacia requires aggressive lung treatments to clear mucus and treat infection. These treatments should be overseen by a pediatric pulmonologist.![]() In rare cases, surgery may be needed to correct tracheomalacia.
In rare cases, surgery may be needed to correct tracheomalacia.
Why choose Children's Colorado for your child's tracheomalacia?
The Aerodigestive Program at Children's Colorado is the only one of its kind in the Western United States. The team is dedicated to the comprehensive and multidisciplinary management of children with complex airway and digestive tract disorders. We treat only children all day, everyday – making us experts when it comes to caring for kids.
Our patients' families are considered essential members of the health care team and are encouraged to participate in planning the patient’s treatment course. This family-centered care approach allows for greater efficiency in scheduling visits and procedures. In addition, family-centered care provides the opportunity for enhanced patient and family education, which can help improve our patients' overall experience and outcomes.
Get to know our pediatric experts.
Julia Boster, MD
Gastroenterology - Pediatric, Pediatrics
Steve Abman, MD
Pulmonology - Pediatric, Pediatrics
Patient ratings and reviews are not available Why?
Victoria Cohen, CPNP-PC
Pediatrics
Patient ratings and reviews are not available Why?
Jilayne Smith, CPNP-AC
Certified Pediatric Nurse Practitioner
Patient ratings and reviews are not available Why?
Meet the team
Learn about patient ratings and reviews
Tracheomalacia: Symptoms, Diagnosis and Treatment
Tracheomalacia (tray key oh mah LAY she ah) means that the walls of a child’s windpipe (trachea) collapse (fall in on themselves). This can happen because the walls of the windpipe are weak, or it can happen because something is pressing on it. The whole windpipe can be affected, or only a short piece of it. If the collapsed part of the windpipe goes past the area where the windpipe branches off into the two lungs, it is called bronchomalacia (brahn koh mah LAY she ah).
This can happen because the walls of the windpipe are weak, or it can happen because something is pressing on it. The whole windpipe can be affected, or only a short piece of it. If the collapsed part of the windpipe goes past the area where the windpipe branches off into the two lungs, it is called bronchomalacia (brahn koh mah LAY she ah).
This problem causes noisy or difficult breathing in the first 1 to 2 months after birth. This is called congenital tracheomalacia (it was present at birth). It is not very common. Babies born with tracheomalacia may have other health issues like a heart defect, reflux or developmental delay. Some children get tracheomalacia because of other health issues. Symptoms can be mild to severe.
Symptoms
- Noisy breathing that may get better when you change your baby’s position or while he or she is asleep.
- Breathing problems that get worse during coughing, crying, feeding or colds.
- High-pitched sound during breathing (stridor).

- High-pitched cough.
- Rattling noise or wheezing with breathing.
Diagnosis
If your baby’s doctor thinks your child may have this problem, he or she may order tests. Some tests that the doctor might use to learn if your baby has tracheomalacia:
- X-ray or CT scan of the chest.
- Airway Fluoroscopy (floor OSS koh pee) to look at the windpipe (trachea).
- Direct Laryngoscopy (LAYR inn GOSS koh pee) to look at the vocal cords (larynx).
- Bronchoscopy (BRAHN koh SKAH pee) to look at the airways in the lungs (bronchi).
If your child is diagnosed with tracheomalacia, the doctor may suggest other tests to find out the cause, or decide on the best treatment.
Treatment
Your baby’s noisy breathing and breathing problems will get better with time. As he or she grows, the walls of the trachea get stronger. It may take years until the problems are completely gone. Until then, your baby will breathe better if you use a humidifier. Your child’s doctor may prescribe medicine that can lower the amount of mucous or inflammation (swelling) in the windpipe.
Your child’s doctor may prescribe medicine that can lower the amount of mucous or inflammation (swelling) in the windpipe.
A cough or cold that may only cause mild problems for other children may cause severe symptoms for a child with tracheomalacia. Your child may need special treatment or medicines, or even need to go to the hospital.
If tracheomalacia is caused by something pressing in on the windpipe, your child’s doctor may recommend other therapies, or even surgery. A whole team of doctors may be part of your child’s care. These doctors have special skills in the treatment of the lungs, heart, ears, nose and throat, or in chest surgery.
Symptoms of tracheomalacia are usually gone by the time your baby is 18 to 24 months old. Surgery is rarely needed.
When to Call the Doctor
Call your child’s doctor if:
- Your baby has difficulty breathing.
- Your baby is not gaining weight.
- Your baby has other symptoms that concern you.

If you have questions, please call our Nurse Line at 614-722-6547.
Tracheomalacia (PDF)
HH-I-335 Revised 2/15 Copyright 2011 Nationwide Children’s Hospital
Tracheomalacia, its symptoms and treatments. Which clinics abroad can help?
Tracheomalacia is a softening of the supporting cartilages of the trachea, expansion of its posterior membrane wall and reduction of its anterior-posterior caliber. This condition of the trachea disrupts the breathing process, causes it to collapse (collapse) and acute airway obstruction. Tracheomalacia are congenital (malformation) and acquired due to chronic inflammatory processes (bronchitis, emphysema), intubation and endoscopic manipulations, chest trauma, compression of the trachea by tumors, cysts, abscesses, vascular formations. Tracheomalacia most commonly affects the lower (distal) part of the trachea.
In infants, tracheomalacia manifests itself during the first weeks of life with expiratory stridor (difficulty exhaling), which increases in the supine position, with crying, with a cold.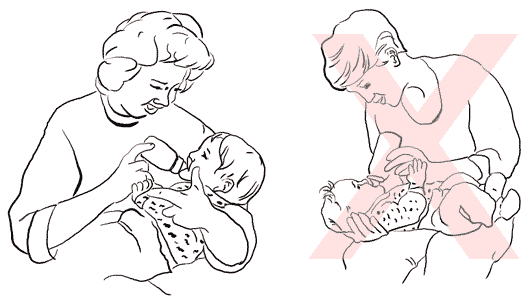 There is hoarseness, loss of voice, feeding difficulties, growth retardation. Many adults with tracheomalacia are asymptomatic and are diagnosed during testing for another condition, most commonly the lungs and bronchi. If tracheomalacia is suspected, the following examination is performed in children and adults: cinefluoroscopy (X-ray examination using filming of an X-ray image) with contrasting of the esophagus and CT (computed tomography). Fiberoptic bronchoscopy also shows loss of the normal semi-circular shape of the trachea, stretching of the posterior wall, and narrowing of the trachea.
There is hoarseness, loss of voice, feeding difficulties, growth retardation. Many adults with tracheomalacia are asymptomatic and are diagnosed during testing for another condition, most commonly the lungs and bronchi. If tracheomalacia is suspected, the following examination is performed in children and adults: cinefluoroscopy (X-ray examination using filming of an X-ray image) with contrasting of the esophagus and CT (computed tomography). Fiberoptic bronchoscopy also shows loss of the normal semi-circular shape of the trachea, stretching of the posterior wall, and narrowing of the trachea.
In most children, the condition of the trachea improves at the age of 18-24 months on the background of conservative supportive treatment (breathing with humidified air, physiotherapy, gentle feeding, prevention and treatment of respiratory diseases). For more severe respiratory disorders, a continuous positive airway pressure (CPAP) device is used.
Surgical treatment is required if other methods fail or when reflex apnea is noted.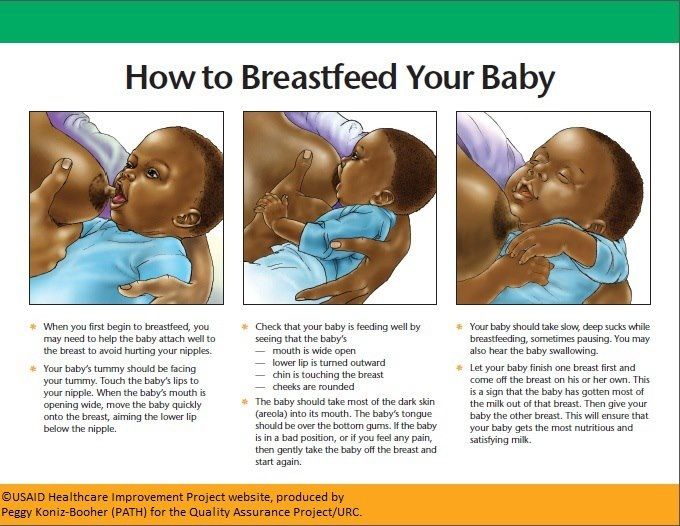 Most often, surgeons eliminate the cause of tracheomalacia, such as a tracheoesophageal fistula or vascular anomaly. An aorthopexy may also be performed. During this operation, the surgeon removes the thymus, creates a space between the aorta and the sternum, and attaches the aorta to the sternum. This relieves pressure on the trachea and it straightens out (sometimes a bronchoscopy is performed during the operation for this). With diffuse tracheomalacia and damage to the upper part of the trachea, tracheal stenting is indicated. A small tube is used as a stent, which keeps the trachea open and promotes the growth of tissues around it, that is, strengthening the trachea. This is a temporary healing technology, but may be required several times. Also, as a temporary treatment in a particularly severe case, a tracheostomy is performed (the creation of an opening in the trachea, which is connected to the external environment through a cannula and through which a person breathes). Abroad, tracheostomy in children is performed using an endoscopic technique specially designed for this.
Most often, surgeons eliminate the cause of tracheomalacia, such as a tracheoesophageal fistula or vascular anomaly. An aorthopexy may also be performed. During this operation, the surgeon removes the thymus, creates a space between the aorta and the sternum, and attaches the aorta to the sternum. This relieves pressure on the trachea and it straightens out (sometimes a bronchoscopy is performed during the operation for this). With diffuse tracheomalacia and damage to the upper part of the trachea, tracheal stenting is indicated. A small tube is used as a stent, which keeps the trachea open and promotes the growth of tissues around it, that is, strengthening the trachea. This is a temporary healing technology, but may be required several times. Also, as a temporary treatment in a particularly severe case, a tracheostomy is performed (the creation of an opening in the trachea, which is connected to the external environment through a cannula and through which a person breathes). Abroad, tracheostomy in children is performed using an endoscopic technique specially designed for this. In the future, such children undergo one of the surgical interventions, including tracheoplasty - strengthening the walls of the trachea with the help of surrounding muscles.
In the future, such children undergo one of the surgical interventions, including tracheoplasty - strengthening the walls of the trachea with the help of surrounding muscles.
Treatment of tracheomalacia in adult patients primarily involves treatment of the underlying disease (usually chronic obstructive pulmonary disease). CPAP devices help a lot. However, especially severe cases require stenting of the airways, surgical strengthening of the posterior wall of the trachea using a special mesh, and tracheostomy. Metal and silicone stents are placed during bronchoscopy. A child with a severe case of tracheomalacia will be consulted at the Cintinnati Children's Hospital Medical Center, an operation for an adult patient in one of the clinics abroad can be arranged through the company 5 Ave or VitaAgency.
Tell friends:
Tracheomalacia. Causes, symptoms and treatment of tracheomalacia!
contents
- General
- Causes
- Symptoms and diagnosis
- Treatment
1.
 General Information
General Information The term "malacia" refers to pathological changes in the composition and structure of any tissue, leading to a decrease in its density. Most often, they simply talk about “softening” of tissues (eg, osteomalacia, keratomalacia, etc.).
A similar phenomenon in the walls of the trachea (tracheomalacia) and / or bronchi (tracheobronchomalacia) refers to rare types of pulmonary pathology, usually acquired. Congenital tracheomalacia, according to most sources, is “extremely rare”, is detected already in the perinatal period and is accompanied by severe clinical manifestations. Softening mainly concerns the dense frame, the skeleton of the trachea - that is, the cartilaginous semi-rings - as well as the muscle fibers in the walls.
A must to check out!
Help with hospitalization and treatment!
2.Causes
The most common cause of tracheomalacia is a degenerative-dystrophic process caused, in turn, by prolonged mechanical compression (squeezing, pressure). This situation may be the result of, for example, thyroid hyperplasia, tumor growth, surgery, prolonged use of mechanical ventilation in premature infants, as well as a genetically determined anomaly in the anatomical structure of the respiratory system. Functional, reversible tracheomalacia, that is, weakening of the walls without gross changes in the tissues, can occur against the background of a number of pulmonary diseases (bronchitis, pneumonia, asthma, etc.). The etiopathogenetic factor in this case is chronically increased intrathoracic pressure.
This situation may be the result of, for example, thyroid hyperplasia, tumor growth, surgery, prolonged use of mechanical ventilation in premature infants, as well as a genetically determined anomaly in the anatomical structure of the respiratory system. Functional, reversible tracheomalacia, that is, weakening of the walls without gross changes in the tissues, can occur against the background of a number of pulmonary diseases (bronchitis, pneumonia, asthma, etc.). The etiopathogenetic factor in this case is chronically increased intrathoracic pressure.
Visit our page
Pulmonology
3.Symptoms and diagnosis
Any pathological process, structural or cellular anomaly, disease state or damage to the organs of the respiratory system one way or another turns into respiratory failure. Flabbiness, lethargy of the tracheal walls, loss of their natural turgor (elasticity, elasticity), a tendency to “fall off” - are manifested by turbulent stridor breathing (noise, wheezing), shortness of breath, severe fatigue, hyperhidrosis, psychomotor restlessness. With congenital tracheomalacia, newborns can refuse to breastfeed, cry almost constantly, become exhausted due to severe sleep disturbances, breathe literally “with their whole body”. In the most severe cases, cyanosis is observed (the skin becomes pale bluish), painful suffocation - and a real risk of death due to asphyxia.
With congenital tracheomalacia, newborns can refuse to breastfeed, cry almost constantly, become exhausted due to severe sleep disturbances, breathe literally “with their whole body”. In the most severe cases, cyanosis is observed (the skin becomes pale bluish), painful suffocation - and a real risk of death due to asphyxia.
The diagnosis is established clinically (with a detailed collection and study of anamnestic information), bronchoscopically and radiologically.
About our clinic
m. Chistye Prudy
Medintercom page!
4. Treatment
In some cases, treatment is either not required at all, or is palliative, aimed at facilitating respiratory activity. In children, the clinic of tracheomalacia can spontaneously decrease during the first 1-3 years of life.
As a rule, the treatment of tracheomalacia involves the obligatory elimination of its root causes.











