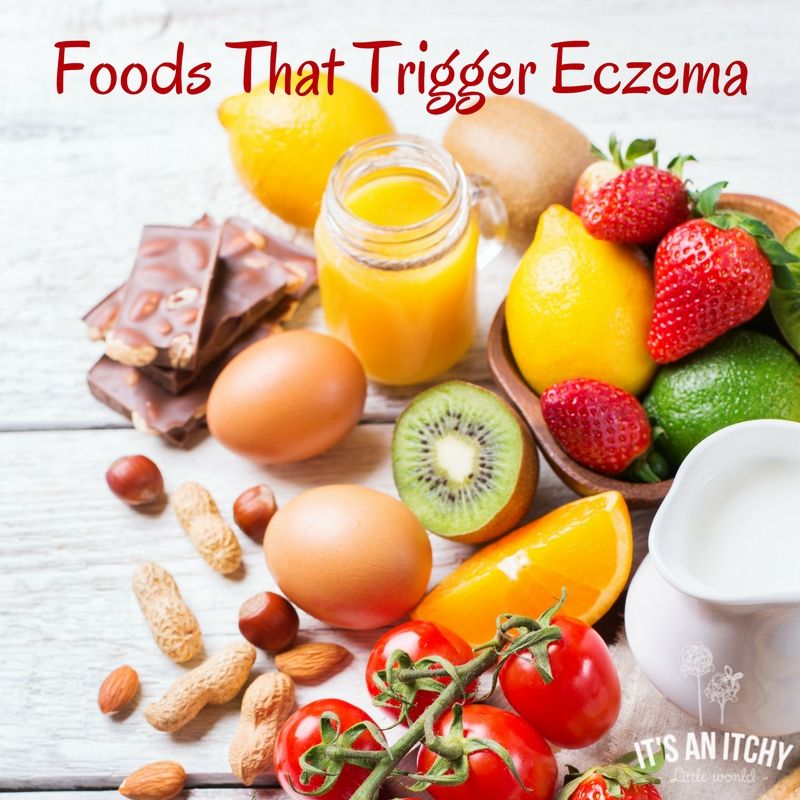
Baby eczema food triggers
7 Foods to Avoid in Babies and Toddlers with Eczema
Also known as atopic dermatitis, eczema is a common condition characterized by red, itchy, and inflamed skin.
Although eczema can affect anyone, it’s especially common among children. In fact, about 60% of cases develop within the first year of life (1).
Many factors can worsen eczema flare-ups, including foods.
Research shows that certain foods may trigger eczema in 20–30% of cases of moderate to severe eczema. Additionally, foods are more likely to worsen symptoms in children and infants under age 5 (2).
While foods do not directly cause eczema, making dietary changes could help reduce symptoms, especially for those who have a sensitivity or allergy to specific foods (3).
In children with a confirmed food allergy, eliminating trigger foods from the diet may significantly improve symptoms of eczema within just 1–2 months (4).
However, keep in mind that it’s not necessary to avoid all the foods listed below to help manage your child’s eczema.
SummaryCertain foods may worsen symptoms of eczema, especially in children and infants. However, it depends on the child’s particular allergies or sensitivities, so speak with a healthcare professional to determine which foods might be best to eliminate.
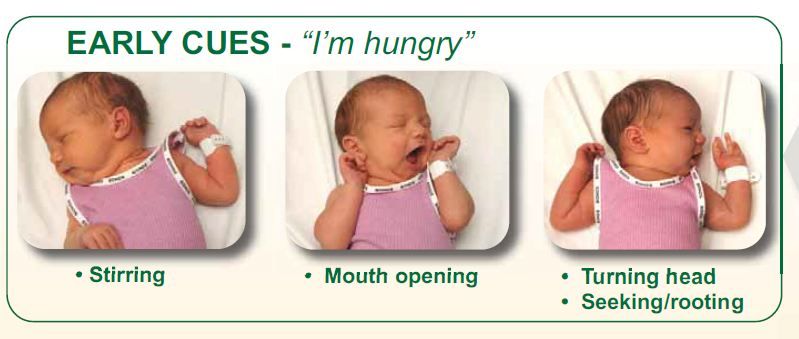
Preventing food allergies
Introducing common allergen foods to an infant early in life may actually help prevent them from developing food allergies, including to eggs and peanuts (5).
If you’re considering eliminating certain foods from your child’s diet or you’re concerned about your child developing food allergies, speak with a healthcare professional. They can help you develop a diet plan based on your child’s needs.
Research has shown that eliminating one or more of these foods from the diet may significantly improve symptoms of eczema in some children.
1. Dairy
Not only is a cow’s-milk allergy the most common food allergy in young children, but dairy products like milk, yogurt, and cheese are also common triggers for eczema (6).
One study in 132 children with food-triggered eczema found that 39% of children developed an immediate reaction after consuming cow’s milk (2).
A 2019 review reported that infants with eczema were six times more likely to have an allergy to cow’s milk, eggs, or peanuts at 12 months of age compared with infants without eczema (7).
Fortunately, there are several simple plant-based milks available as an alternative to cow’s milk, including soy milk, almond milk, and cashew milk.
However, be sure to check the ingredients lists carefully, as some of these products are high in calories and added sugar.
2. Fish and shellfish
The term “shellfish” refers to any aquatic animal that has a shell-like exterior, including crabs, lobsters, oysters, mussels, and shrimp. Meanwhile, most types of fish, including salmon, trout, tuna, and tilapia, have fins and scales.
Although both fish and shellfish are highly nutritious and can be great sources of protein and omega-3 fatty acids, they can also worsen symptoms of eczema for many children.
This is because fish and shellfish allergies are common and can cause a wide range of side effects, including hives, itching, and eczema (8, 9).
While some children may be sensitive to finned fish or shellfish, others may experience reactions only to certain types, such as crustaceans (like shrimp and crab) or mollusks (like oysters and clams) (8).
A pediatrician or registered dietitian can help determine which specific types of seafood may trigger symptoms for your baby or toddler.
3. Soy products
For those with a soy allergy, consuming soy products like soy milk, tofu, or edamame can cause an immune response, which could trigger skin reactions such as eczema (10).
Compared with allergies to other major food allergens, soy allergies are not nearly as common (11, 12).
For example, one 2013 study in 175 people with eczema found that around 30% had an immune reaction to soy. However, only about 3% of people experienced symptoms, such as hives and itching, after consuming soy (13).
If your baby or toddler has a sensitivity to soy products, keep in mind that many processed foods contain soy-based ingredients, all of which could worsen symptoms of eczema. Examples include (14):
- soy sauce
- tamari
- soy protein
- textured vegetable protein
4. Eggs
Share on PinterestElena Botta/Getty Images
Some babies or toddlers may have an allergy to the proteins found in egg whites or yolks, which could trigger symptoms of eczema (15).
Egg allergy is one of the most common food allergies, affecting an estimated 1.3% of children under 5 in the United States (16).
Furthermore, one study reported that infants with eczema are nearly 6 times as likely to develop an egg allergy by 12 months of age compared with those without eczema (7).
However, most egg allergies in children resolve by around age 5 (17).
Additionally, some babies and toddlers who are sensitive to eggs may be able to tolerate them in some forms, such as baked eggs (16).
5. Tree nuts
Tree nuts could worsen eczema for many young children with a tree nut allergy. Examples of tree nuts include:
- almonds
- cashews
- walnuts
- pecans
Tree nut allergies are very common and may affect up to 4.9% of children and adults (18).
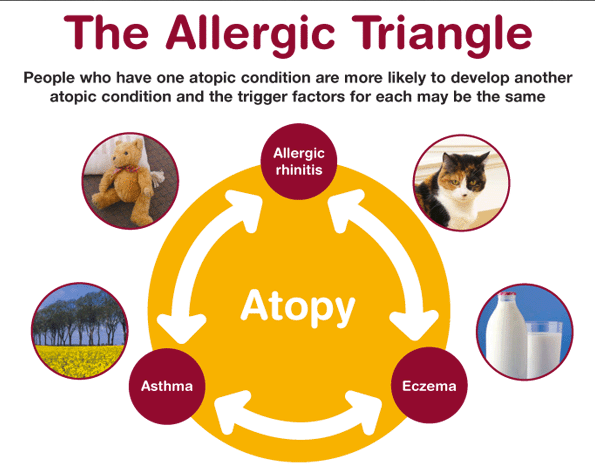
Unfortunately, tree nut allergies can be very serious, and some research suggests that more severe reactions to tree nuts are often associated with severe cases of eczema, asthma, and seasonal allergies (19).
In addition to avoiding tree nuts specifically, your child may need to avoid foods that contain tree nuts, including pesto, nut butters, coconut products, and certain types of cereals, cookies, crackers, or candies.
6. Wheat or gluten
Wheat is a type of cereal grain and a staple ingredient in many foods, such as bread, pasta, and baked goods.
Gluten is a specific protein found in wheat, barley, and rye that gives dough its structure and elasticity.
For those with a wheat allergy, consuming products that contain wheat may worsen eczema and could also cause other symptoms, including hives, asthma, and digestive issues (20, 21).
Eczema and skin rashes can also be caused by a sensitivity to gluten, as well as by celiac disease, an autoimmune condition that triggers an immune reaction when gluten-containing foods are consumed (22, 23, 24).
While there is no test available to diagnose non-celiac gluten sensitivity, your child’s pediatrician can use a skin or blood test to help determine if your child has celiac disease or an allergy to wheat.
7. Peanuts
Peanuts are a common allergen and are associated with several skin reactions, including rashes, hives, itching, and eczema (25).
Peanut allergies are especially common among babies and toddlers, as most peanut allergies appear within the first 2 years of life (25).
Additionally, some research shows that peanut allergies are more common among infants with moderate to severe eczema (26).
If peanuts cause flare-ups of eczema for your baby or toddler, try swapping other ingredients into your favorite recipes instead, such as seeds or seed butters.
SummarySome of the most common foods that cause allergies in infants and toddlers are dairy, fish, shellfish, soy products, wheat, peanuts, tree nuts, and eggs.
Several foods can be beneficial for eczema and may help reduce symptoms such as itching and inflammation.
For example, fruits and vegetables are rich in antioxidants, which are compounds that can protect against oxidative stress, cell damage, and inflammation (27).
Although studies in humans are still limited, some research suggests that reducing oxidative stress could play a role in managing eczema (28).
Increasing your intake of probiotics through fermented foods or supplements may also be helpful.
According to one review of 13 studies, certain strains of probiotics were effective at reducing eczema severity in children. These strains included Lactobacillus fermentum and Lactobacillus salivarius (29).
However, more research is needed because other studies have found that probiotics do not have a significant effect on symptom severity or quality of life for those with eczema (30).
SummaryIncluding more foods rich in antioxidants and probiotics in your child’s diet could be beneficial for eczema, but more research is needed.
For many babies and toddlers, diet can play a key role in managing symptoms of eczema.
While certain foods can make eczema symptoms worse, others may decrease inflammation and oxidative stress, which could reduce symptoms.
However, it’s best to talk with a pediatrician or dietitian before making any changes to your child’s diet, especially because eliminating certain foods from their diet could make it harder for them to meet their nutritional needs.
Additionally, keep in mind that many other factors can contribute to eczema and some children may also need other types of treatment to help relieve symptoms.
Just one thing
Try this today: Consider experimenting with some at-home remedies for your child’s eczema. Check out this article for a few ideas to help provide relief for your baby or toddler.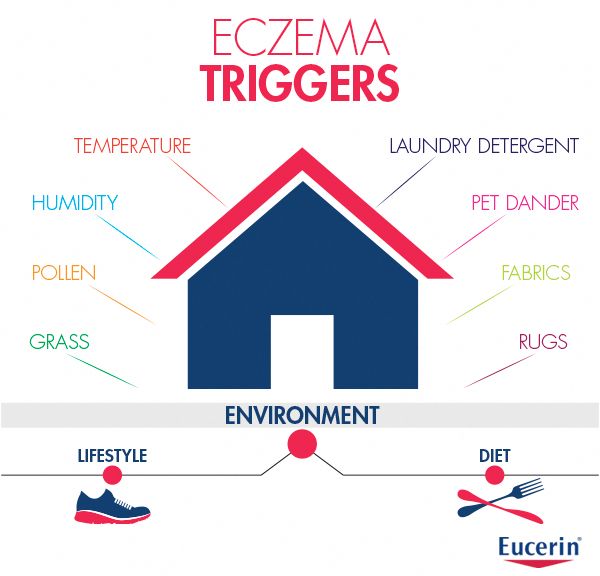
7 Foods to Avoid in Babies and Toddlers with Eczema
Also known as atopic dermatitis, eczema is a common condition characterized by red, itchy, and inflamed skin.
Although eczema can affect anyone, it’s especially common among children. In fact, about 60% of cases develop within the first year of life (1).
Many factors can worsen eczema flare-ups, including foods.
Research shows that certain foods may trigger eczema in 20–30% of cases of moderate to severe eczema. Additionally, foods are more likely to worsen symptoms in children and infants under age 5 (2).
While foods do not directly cause eczema, making dietary changes could help reduce symptoms, especially for those who have a sensitivity or allergy to specific foods (3).
In children with a confirmed food allergy, eliminating trigger foods from the diet may significantly improve symptoms of eczema within just 1–2 months (4).
However, keep in mind that it’s not necessary to avoid all the foods listed below to help manage your child’s eczema.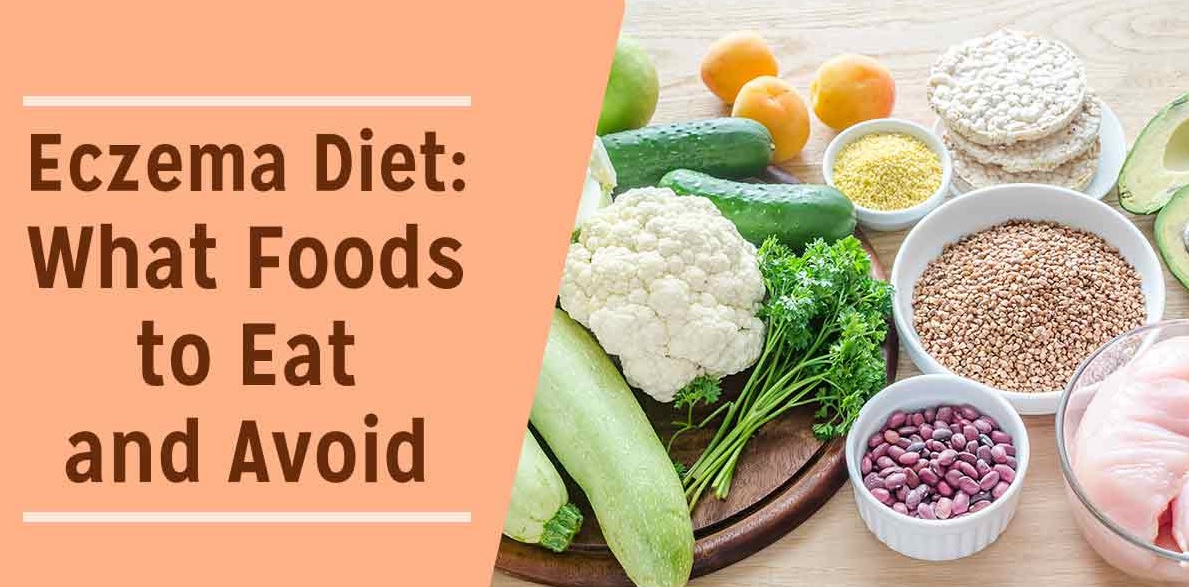
SummaryCertain foods may worsen symptoms of eczema, especially in children and infants. However, it depends on the child’s particular allergies or sensitivities, so speak with a healthcare professional to determine which foods might be best to eliminate.
Preventing food allergies
Introducing common allergen foods to an infant early in life may actually help prevent them from developing food allergies, including to eggs and peanuts (5).
If you’re considering eliminating certain foods from your child’s diet or you’re concerned about your child developing food allergies, speak with a healthcare professional. They can help you develop a diet plan based on your child’s needs.
Research has shown that eliminating one or more of these foods from the diet may significantly improve symptoms of eczema in some children.
1. Dairy
Not only is a cow’s-milk allergy the most common food allergy in young children, but dairy products like milk, yogurt, and cheese are also common triggers for eczema (6).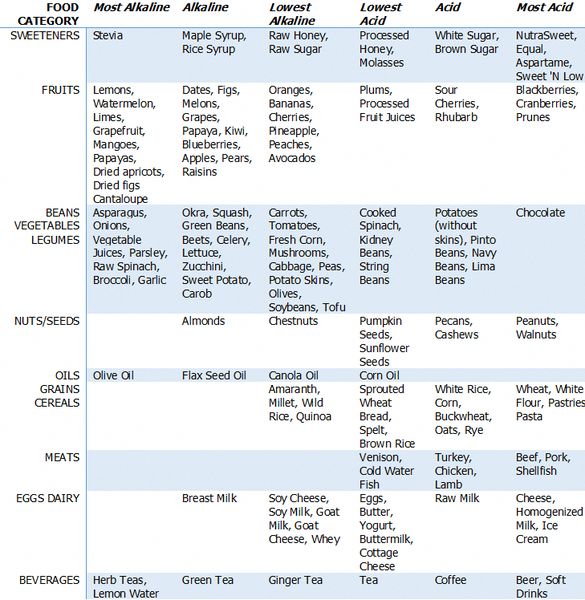
One study in 132 children with food-triggered eczema found that 39% of children developed an immediate reaction after consuming cow’s milk (2).
A 2019 review reported that infants with eczema were six times more likely to have an allergy to cow’s milk, eggs, or peanuts at 12 months of age compared with infants without eczema (7).
Fortunately, there are several simple plant-based milks available as an alternative to cow’s milk, including soy milk, almond milk, and cashew milk.
However, be sure to check the ingredients lists carefully, as some of these products are high in calories and added sugar.
2. Fish and shellfish
The term “shellfish” refers to any aquatic animal that has a shell-like exterior, including crabs, lobsters, oysters, mussels, and shrimp. Meanwhile, most types of fish, including salmon, trout, tuna, and tilapia, have fins and scales.
Although both fish and shellfish are highly nutritious and can be great sources of protein and omega-3 fatty acids, they can also worsen symptoms of eczema for many children.
This is because fish and shellfish allergies are common and can cause a wide range of side effects, including hives, itching, and eczema (8, 9).
While some children may be sensitive to finned fish or shellfish, others may experience reactions only to certain types, such as crustaceans (like shrimp and crab) or mollusks (like oysters and clams) (8).
A pediatrician or registered dietitian can help determine which specific types of seafood may trigger symptoms for your baby or toddler.
3. Soy products
For those with a soy allergy, consuming soy products like soy milk, tofu, or edamame can cause an immune response, which could trigger skin reactions such as eczema (10).
Compared with allergies to other major food allergens, soy allergies are not nearly as common (11, 12).
For example, one 2013 study in 175 people with eczema found that around 30% had an immune reaction to soy. However, only about 3% of people experienced symptoms, such as hives and itching, after consuming soy (13).
If your baby or toddler has a sensitivity to soy products, keep in mind that many processed foods contain soy-based ingredients, all of which could worsen symptoms of eczema. Examples include (14):
- soy sauce
- tamari
- soy protein
- textured vegetable protein
4. Eggs
Share on PinterestElena Botta/Getty Images
Some babies or toddlers may have an allergy to the proteins found in egg whites or yolks, which could trigger symptoms of eczema (15).
Egg allergy is one of the most common food allergies, affecting an estimated 1.3% of children under 5 in the United States (16).
Furthermore, one study reported that infants with eczema are nearly 6 times as likely to develop an egg allergy by 12 months of age compared with those without eczema (7).
However, most egg allergies in children resolve by around age 5 (17).
Additionally, some babies and toddlers who are sensitive to eggs may be able to tolerate them in some forms, such as baked eggs (16).
5. Tree nuts
Tree nuts could worsen eczema for many young children with a tree nut allergy. Examples of tree nuts include:
- almonds
- cashews
- walnuts
- pecans
Tree nut allergies are very common and may affect up to 4.9% of children and adults (18).
Unfortunately, tree nut allergies can be very serious, and some research suggests that more severe reactions to tree nuts are often associated with severe cases of eczema, asthma, and seasonal allergies (19).
In addition to avoiding tree nuts specifically, your child may need to avoid foods that contain tree nuts, including pesto, nut butters, coconut products, and certain types of cereals, cookies, crackers, or candies.
6. Wheat or gluten
Wheat is a type of cereal grain and a staple ingredient in many foods, such as bread, pasta, and baked goods.
Gluten is a specific protein found in wheat, barley, and rye that gives dough its structure and elasticity.
For those with a wheat allergy, consuming products that contain wheat may worsen eczema and could also cause other symptoms, including hives, asthma, and digestive issues (20, 21).
Eczema and skin rashes can also be caused by a sensitivity to gluten, as well as by celiac disease, an autoimmune condition that triggers an immune reaction when gluten-containing foods are consumed (22, 23, 24).
While there is no test available to diagnose non-celiac gluten sensitivity, your child’s pediatrician can use a skin or blood test to help determine if your child has celiac disease or an allergy to wheat.
7. Peanuts
Peanuts are a common allergen and are associated with several skin reactions, including rashes, hives, itching, and eczema (25).
Peanut allergies are especially common among babies and toddlers, as most peanut allergies appear within the first 2 years of life (25).
Additionally, some research shows that peanut allergies are more common among infants with moderate to severe eczema (26).
If peanuts cause flare-ups of eczema for your baby or toddler, try swapping other ingredients into your favorite recipes instead, such as seeds or seed butters.
SummarySome of the most common foods that cause allergies in infants and toddlers are dairy, fish, shellfish, soy products, wheat, peanuts, tree nuts, and eggs.
Several foods can be beneficial for eczema and may help reduce symptoms such as itching and inflammation.
For example, fruits and vegetables are rich in antioxidants, which are compounds that can protect against oxidative stress, cell damage, and inflammation (27).
Although studies in humans are still limited, some research suggests that reducing oxidative stress could play a role in managing eczema (28).
Increasing your intake of probiotics through fermented foods or supplements may also be helpful.
According to one review of 13 studies, certain strains of probiotics were effective at reducing eczema severity in children. These strains included Lactobacillus fermentum and Lactobacillus salivarius (29).
However, more research is needed because other studies have found that probiotics do not have a significant effect on symptom severity or quality of life for those with eczema (30).
SummaryIncluding more foods rich in antioxidants and probiotics in your child’s diet could be beneficial for eczema, but more research is needed.
For many babies and toddlers, diet can play a key role in managing symptoms of eczema.
While certain foods can make eczema symptoms worse, others may decrease inflammation and oxidative stress, which could reduce symptoms.
However, it’s best to talk with a pediatrician or dietitian before making any changes to your child’s diet, especially because eliminating certain foods from their diet could make it harder for them to meet their nutritional needs.
Additionally, keep in mind that many other factors can contribute to eczema and some children may also need other types of treatment to help relieve symptoms.
Just one thing
Try this today: Consider experimenting with some at-home remedies for your child’s eczema. Check out this article for a few ideas to help provide relief for your baby or toddler.
symptoms and treatments at EMC
-
Diagnosis and treatment of eczema according to international protocols
-
Dermatologists with experience and long-term internships in leading clinics in Israel and Western Europe
-
Opportunity to obtain a second opinion from the world's leading experts in the treatment of eczema
-
We help even in the most difficult cases
Treatment of eczema
In each case, for the correct selection of therapy, preliminary diagnosis is necessary, which may include immunological, allergological, biochemical methods and microbiological examination. If necessary, consultations of narrow specialists (therapist, endocrinologist, gastroenterologist, psychotherapist, etc.) are held.
Comprehensive personalized treatment is prescribed taking into account the characteristics and degree of skin lesions and always includes the use of antihistamines..jpg)
When prescribing therapy, the doctor also takes into account the gender and age of the patient, medical history, the results of previous treatment, and individual intolerance to drugs. The key factors are the stage and prevalence of the disease.
What is eczema?
Eczema is a chronic inflammatory skin disease characterized by itching, redness and rashes in the form of small fluid-filled vesicles. Rashes resemble air bubbles that form when water boils. Hence the name of the disease (from the Greek eczeo - boil).
Eczema is not transmitted from person to person. This is a genetically determined disease. Eczema is quite common, it is diagnosed in about 30-40% of patients who visit a dermatologist.
What does eczema look like and on what parts of the body does it appear
Weeping and itchy skin on the face and hands
Rashes on the skin in the form of vesicles and bumps, accompanied by redness, may be manifestations of true eczema. Subsequently, the bubbles open with the release of serous fluid, in their place shallow point erosions (ulcers) form. The released liquid dries up with the formation of a soft crust.
Subsequently, the bubbles open with the release of serous fluid, in their place shallow point erosions (ulcers) form. The released liquid dries up with the formation of a soft crust.
The appearance of repeated rashes in the area of the pathological focus leads to the simultaneous localization of vesicles, sores, and crusts on the skin. All rashes are accompanied by severe itching, which causes significant discomfort to the patient and reduces the quality of life. Sometimes nighttime itching causes insomnia.
Eruptions are characterized by symmetry, the absence of clear boundaries near the affected area.
The rash tends to spread to the chest, trunk, abdomen and back.
Scaly layer at the border of the scalp
Seborrheic eczema often develops on the scalp. In the initial stages, it manifests itself as single yellowish nodules, the number of which increases rapidly. The nodules turn into spots with the formation of whitish scales on the surface.
Due to the fusion of foci of rashes on the border of the hair, a “seborrheic crown” is often formed - a scaly ring, along the edges of which there are areas of hyperemic skin. Without treatment, this form of scalp eczema spreads to the behind the ear and neck.
Some doctors consider seborrheic eczema to be just a variation of true seborrhea with minor differences in the course of the pathological process.
Round rashes on the skin of the hands
Itchy rashes on the hands can indicate many different diseases. Eczema is one of them, in 80% of cases true eczema is localized on the hands.
Rashes at the initial stage have rounded outlines, with the development of the disease, the contours lose their correctness. A similar nature of rashes on the hands is also characteristic of mycotic eczema.
Microbial eczema on the hands is rare and is characterized by the formation of purulent crusts on the surface.
Rashes with clear edges on the legs
Due to the increased frequency of skin injuries and chronic venous insufficiency, post-traumatic and microbial eczema most often appear on the legs. In 75% of cases, they occur in women. Rashes are often located next to varicose veins, have a rounded shape and clear boundaries.
In 75% of cases, they occur in women. Rashes are often located next to varicose veins, have a rounded shape and clear boundaries.
Often, microbial eczema is manifested by many separate rounded foci up to 3 cm in size. Due to the similarity with a scattering of coins, this form of eczema is called coin-like.
Symmetrical scaly rashes on the body
Symmetrical rashes are characteristic of true eczema. In most cases, it primarily appears on the limbs, but sometimes the foci initially form on the trunk.
In the early stages, lesions are typical and consist of fluid-filled vesicles. With a long course, in place of weeping foci, areas of compacted skin appear with increased skin pattern. In chronic eczema, the lesions become covered with flaky skin during healing, eczema becomes dry.
Fine-grained eruptions on the palms and soles
Eczema may affect the skin of the hands and feet. In these cases, due to the structural features of the skin, foci of eczema appear as small whitish bumps. The bumps come together to form blisters that can open. After opening, large sores remain on the palms and feet, releasing serous fluid.
The bumps come together to form blisters that can open. After opening, large sores remain on the palms and feet, releasing serous fluid.
Callus-like rashes on the palms
Callus-like rashes on the palms, appearing in areas not characteristic of corns, may indicate tylotic eczema. Bubbles form, but may not open due to the structure of the skin.
Tylotic eczema usually accompanies true eczema, therefore, when corn-like rashes appear, it is recommended to pay attention to other parts of the body.
Multiple vesicles in the axillary region with a hair in the center
A rash with a hair in the center is a sign of sycosis - a special lesion of the hair follicles. Eruptions of this kind, located outside the scalp, are called sycosiform eczema. Eczema is also indicated by the itching that accompanies the rash. In addition to the axillary region, this type of eczema can be localized on the chin, upper lip and pubic area.
Lumps on the skin of the hands and on the body
Thickening of the skin may be evidence of the transition of eczema into a chronic form. Additionally, a decrease in weeping and the appearance of large areas of thickened, scaly skin indicate the chronicity of the disease.
Areas of depigmentation after peeling on the skin
Usually appear during the recovery phase. At the site of the rash, the skin is lighter. Most often, such light spots disappear on their own within a month.
Areas of depigmentation appear after most types of eczema, but more often after true and microbial.
Multiple bumps on the face and hands without weeping and crusts
Sometimes with true eczema, the vesicles do not open, but appear only as multiple bumps and papules. This is how pruriginous eczema manifests itself - one of the varieties of true eczema. Pruriginous eczema is localized on the extensor surfaces of the hands and on the face.
Itchy areas of redness on the skin of the legs and arms
A hyperemic and itchy area of the skin with many rashes indicates true or microbial eczema. The most pronounced pruritus in eczema is manifested at the stages of active formation of fresh papules and vesicles. Itching is aggravated by the addition of bacterial flora.
With varicose and post-traumatic eczema, these symptoms are observed in most cases on the legs. In occupational eczema, itching and flushing are typical signs. The severity of symptoms increases after repeated contact with the provoking agent. After the provoking factor is eliminated, the symptoms disappear.
Suppuration and itching around the wounds on the legs and arms
Hyperemia of the skin and the formation of purulent crusts indicate microbial eczema. Most often they appear on areas of the skin that are most susceptible to injury.
When the pus dries out, rough crusts form, which fall off, exposing the skin that continues to become wet.
Types of eczema
Understanding the types of eczema is essential for proper treatment.
True or idiopathic eczema.
Characterized by a classic course, rashes go through all six stages.
Stages of true eczema:
First stage . It is characterized by wide foci of hyperemia with a red-blue tint and blurred edges without clear boundaries.
Second stage - papules. Soft nodular connections appear, merging into small foci. In places, swelling and plaques appear.
The third stage is vasculotic. The nodules gradually turn into bubbles.
Fourth stage . The accumulation of subcutaneous exudate causes the opening of papules and the release of serous fluid. Point foci of maceration with depressions (wells) appear on the skin. At this stage, the development of the disease reaches its peak.
Fifth stage - crusty. The secreted serous fluid begins to dry out, the forming crusts are layered on top of each other.
Sixth stage - squamous. Dried whitish scales separate on their own, the skin is restored. In places of the rash, pink or whitish spots may remain.
It is serous wells that are the main distinguishing feature of true eczema. Foci of inflammation are often located in a symmetrical order. The first symptoms appear on the face and hands, then the disease spreads to other parts of the body. Severe itching and soreness joins in places where ulcers form.
Without treatment, the process quickly flows into the chronic stage, when even during the period of remission, the foci of rashes are excessively compacted, a pronounced linear pattern appears on the skin.
Chronic eczema
The acute stage of true eczema can quickly turn into a chronic one. It is characterized by compaction and coarsening of endogenous foci. New rashes actively appear, followed by infiltration and the formation of serous wells. Itching increases many times and does not stop even at night, so patients with chronic eczema often suffer from insomnia. After getting rid of the symptoms in the affected areas, pigmentation is disturbed, dry skin appears.
New rashes actively appear, followed by infiltration and the formation of serous wells. Itching increases many times and does not stop even at night, so patients with chronic eczema often suffer from insomnia. After getting rid of the symptoms in the affected areas, pigmentation is disturbed, dry skin appears.
Exacerbations are more common in winter.
Microbial eczema
Caused by infectious or fungal agents. It occurs at the stage of opening papules with true eczema or with chronic ulcerative-vegetative pyoderma, in places of fistulas, wounds, etc.
Pathogenic foci have clear pink borders. In addition to papules and weeping erosions, from which fluid is released, there is a layering of purulent crusts. The size of the affected areas increases rapidly. Often, separate pustules with scaly areas form near the foci.
Depending on the source of the disease, microbial eczema is divided into nummular and varicose.
Coin-shaped eczema
The name is due to the appearance of red spots that resemble coins in shape.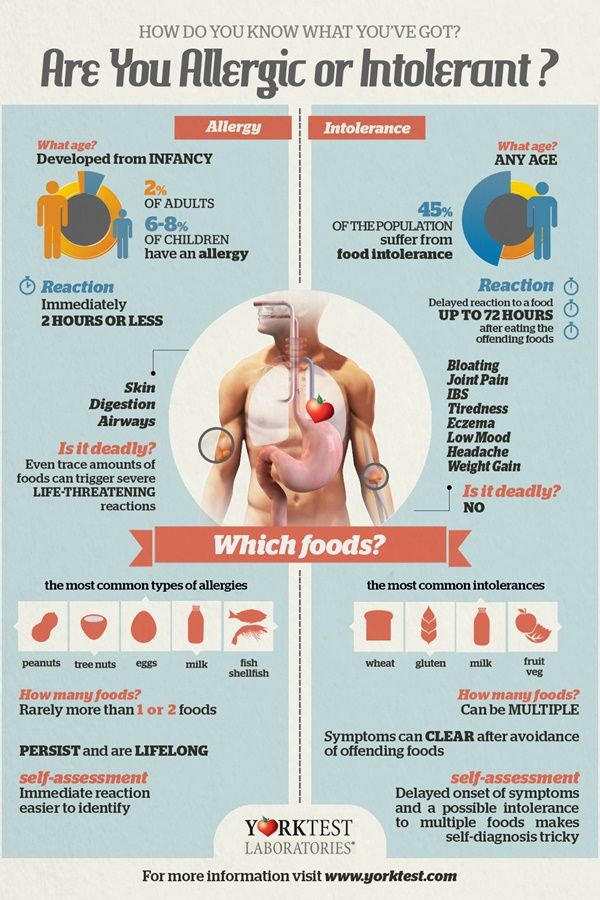 Education may not take place for a long time (from a month to several years). In most cases, symptoms begin to appear on the inner thigh and outer side of the hands.
Education may not take place for a long time (from a month to several years). In most cases, symptoms begin to appear on the inner thigh and outer side of the hands.
In addition to blisters of a red-pink, sometimes bluish hue, there is severe itching and burning, weeping is noted after the opening of the rash.
Varicose eczema
Primarily develops on the legs. Accompanied by moderate itching, increased dryness of the skin, scaly formations in the localization of dilated venous vessels. The disease greatly affects the condition of the skin - edematous, hyperemic foci with a burgundy-violet tint appear. Specific dark spots appear on the skin.
Small blisters also form on the skin, which open with the release of fluid and the formation of ulcers. The weeping stage passes into the drying stage after about two weeks. Outgrowths are formed by the type of crusts. Pathological foci thicken and darken, up to brown. There is pain when pressed.
The inflammatory process is accompanied by severe itching. The patient combs the foci of inflammation, as a result of which abrasions and cracks form on the skin, there is a risk of secondary infection.
Seborrheic eczema
The trigger of this type of eczema is the weakening of local immunity, dysfunction of the sebaceous glands, malnutrition of the scalp. Most patients have a history of congenital allergic reactions.
Each person has the fungus Pityrosporum ovale as part of the hairy epithelial layer. In case of failures in the protective function, it can penetrate deeper, in response, local immunity reacts in the form of an allergic reaction. The inflammatory process begins in the form of local edema. Normally, it stops after the treatment of the fungus, but with seborrheic eczema, the inflammatory process is more pronounced and lasts a long time.
A feature of seborrheic eczema is excessive activity of the sebaceous glands in the lesions. There is a gluing of thinned skin scales and the formation of yellow fatty flakes.
There is a gluing of thinned skin scales and the formation of yellow fatty flakes.
Lesions:
-
trunk: umbilical region, chest, around the halo of the mammary glands, in the folds of the axillary and inguinal zones;
-
head: nasolabial fold, ears and behind the ears, eyebrows, chin, eyelashes, scalp.
Dry eczema
In the initial stages, patches with blurred pink edges form, later the contours turn red. Sharp papules appear, merging into large plaques.
No blistering but skin breakage occurs. The upper thin and dry layer peels off, forming small and deep cracks. Without treatment, the disease progresses and becomes acute with weeping, the formation of dense crusts and severe redness. In this case, the patient may not experience pain.
The disease worsens in dry and cold seasons.
Allergic eczema
Is the result of the body's hypersensitivity to external or internal stimuli. More often develops in patients with a weak immune response.
More often develops in patients with a weak immune response.
The main factor is contact with foreign compounds that cause excessive production of histamine.
Any manifestation of the disease causes excitation of the nervous system, so the patient experiences irritation, may suffer from insomnia and severe headaches.
Symptoms:
-
rash accompanied by itching,
-
dryness and flaking of the skin,
-
Crusts form at the site of opening blisters,
-
reddening of the skin, burning sensation,
-
thickening of the skin in the eyes of the lesion.
Allergic eczema is divided into dry and weeping. The first type is characterized by dry, flaky skin. The trigger may be direct contact with the allergen or the presence of internal diseases.
The second type is more often localized on the hands and occurs due to direct contact with the chemical. At the same time, the skin swells strongly, red foci appear with small papules, which, after opening, turn into painful ulcers.
Eruptions in this type of eczema can appear on any part of the body.
Dyshidrotic eczema
Dyshidrosis affects the sweat glands of the feet (in 20% of cases) and hands (80%), has a chronic course with seasonal exacerbations. Serous vesicles form on the affected areas.
The hallmark of dyshidrosis is the development of vesicles. The rashes are covered with a dense membrane. Purulent discharge appears only when a secondary infection is attached. Under normal conditions, the formations contain a clear liquid.
All stages are accompanied by gradually increasing itching. The lesions are swollen and flaky. Vesicles open themselves, or in the process of combing or damage, small wounds and cracks appear in their place. The skin pattern becomes more distinct.
The skin pattern becomes more distinct.
In this type of eczema, itching appears before skin symptoms, rashes form later, first on the lateral areas of the fingers, then on the palms and feet.
Weeping eczema
This species is characterized by several phases. The first phase: pink spots of various shapes and sizes appear on the skin, swelling, as well as papules or vesicles. Due to the constant release of subcutaneous exudate, weeping zones are formed.
Opening, formations are covered with crusts with active exfoliation. A feature of this type is that the rash is at different stages of development. In one zone, new and already opened rashes can be located, and rejection of dead cells is also observed. Severe itching causes insomnia and neuroses.
When the process is chronic, the skin in the affected areas thickens and scars, a blue-red tint appears. During the period of remission, the skin in the lesions constantly peels off.
Symptoms
Symptoms of eczema may vary depending on the type of disease, but there are common symptoms:
-
regular fever in occupational eczema;
-
the appearance of a focus of inflammation and redness, thickening of the skin;
-
the appearance of a rash;
-
increased sensitivity of the skin, the appearance of itching, which reduces the quality of life of the patient;
-
the appearance of painful cracks, wounds, erosion at the site of the rash, the formation of serous or hemorrhagic crusts;
-
increased dryness of the skin, loss of elasticity during remission.
Eczema has very specific manifestations even with a small area of rash. In adults, it usually affects large areas of the body, most commonly on the arms, shoulders, face, feet, and lower legs. Eczema can also occur against the background of swelling and redness of the skin.
Eczema can also occur against the background of swelling and redness of the skin.
Eczema is difficult to treat, and frequent relapses are possible, but thanks to modern protocols, doctors are increasingly able to achieve stable remissions. It is important to consult a doctor in a timely manner.
Eczema on the face
City air, climate, improper care can have a negative effect on the skin. If you notice itchy, swollen reddish spots on your face with rashes in the form of bubbles that burst, forming crusts, and the crusts then merge into a large weeping spot, urgently make an appointment with a dermatologist. This is especially true, given that eczema is accompanied by severe burning and itching.
The disease is characterized by symmetry, if the rash appears on one side of the face, they will appear on the other. Eczema can affect the mouth and eyes. The skin on the eyelids thickens and coarsens, itching and peeling appear. Lamellar scales form on the lips, which then turn into bleeding painful cracks.
True, seborrheic and occupational eczema appears on the face. The symptoms are largely similar. Separate areas on the face swell and turn red, then small itchy vesicles appear, filled with a clear or cloudy liquid. Cracks form on the skin, it begins to peel off.
True eczema is distinguished by symmetrical rashes, seborrheic eczema appears on the scalp, and professional eczema occurs in places of direct contact with the irritant.
Eczema on the legs
Often, eczema on the legs appears as a result of an allergic reaction and the presence of vascular pathology of the lower extremities (varicose eczema). Psycho-emotional state and reduced immunity can also be triggers.
Most often, microbial eczema appears on the legs. It is localized in places of burns, postoperative sutures, fungal infection, varicose veins. Eczema occurs against the background of an already existing inflammatory process.
Main symptoms of eczema on the legs:
-
swelling of the legs;
-
the appearance of a characteristic crust;
-
sore and dry skin;
-
the appearance of bubbles, cracks and pigmentation in places of localization.

Possible sleep disturbances and headache.
Self-treatment of eczema is unacceptable. It can lead to the development of complications and complicate the treatment process.
Eczema on the hands
According to the intensity of the development of the disease on the hands, acute and chronic eczema can be distinguished.
Depending on triggers:
-
microbial (affects areas around wounds, abrasions, boils),
-
professional,
-
dyshidrotic (affects palms, nails), horny (may appear in the form of calluses).
There is a childhood eczema that appears as a severe rash on the hands and may go away with age.
There are 4 stages of the disease:
-
Erythematous - swelling and redness of the focus.
-
Papulovesicular - the appearance of rashes.

-
Moist - opening of the bubbles.
-
Cortical - formation of crusts.
When the disease passes into the chronic stage, the skin becomes rough, pigmentation, peeling, dryness appear.
Causes of the disease
Hereditary factor is the main cause of eczema . If there are cases of eczema in close relatives, the patient is at times more likely to develop this disease.
One of the provoking factors is immune disorders. The immune system begins to produce immunoglobulins to its own skin cells, which leads to the appearance of areas of inflammation. Violation of intercellular immunity is confirmed by an imbalance of glycoproteins: laboratory values of IgG and IgE are above normal, IgM is in short supply.
There is a connection between exacerbations of eczema and stress.
It has been scientifically proven that dietary habits and disorders of the gastrointestinal tract can also influence the development of eczema.
How to treat eczema
Weeping eczema
Weeping eczema character for all types of eczema. After the diagnosis, the dermatologist will create a personalized treatment plan, including:
- Drug treatment:
a) general;
b) local.
-
Physiotherapy.
-
Dieting.
The goal of treatment is to diagnose and eliminate the cause of the disease.
Dry eczema
Dry eczema is manifested by excessive dryness of the skin. Features are:
-
chronic;
-
seasonal exacerbations;
-
localization on any part of the skin, but most often on the limbs.
Dry eczema on the hands is often a sign of liver or gastrointestinal disease. It can also appear due to frequent stress.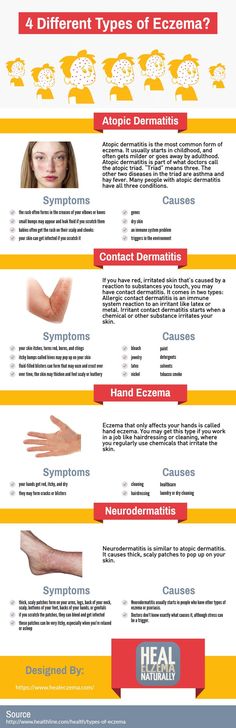 But the main factor is genetic predisposition.
But the main factor is genetic predisposition.
In treatment, adherence to therapy is extremely important, all activities prescribed as part of the treatment plan must be completed in full. Treatment should not be interrupted at the first sign of improvement.
Corticosteroids in the form of an ointment show a good effect in the early stages of the development of eczema. But they are not recommended for long-term use. To eliminate the symptoms in the future, emollients are used.
The attending dermatologist can recommend consultations of specialized specialists: endocrinologist, gastroenterologist, etc. A multidisciplinary approach improves the results of therapy.
Treatment of eczema with medicines
The development of eczema is associated with increased sensitivity of the body to a number of irritants. Therefore, treatment should be systemic with the appointment of hormonal ointments, antihistamines, antibiotics. The doctor's task is to select the most effective drugs in each case.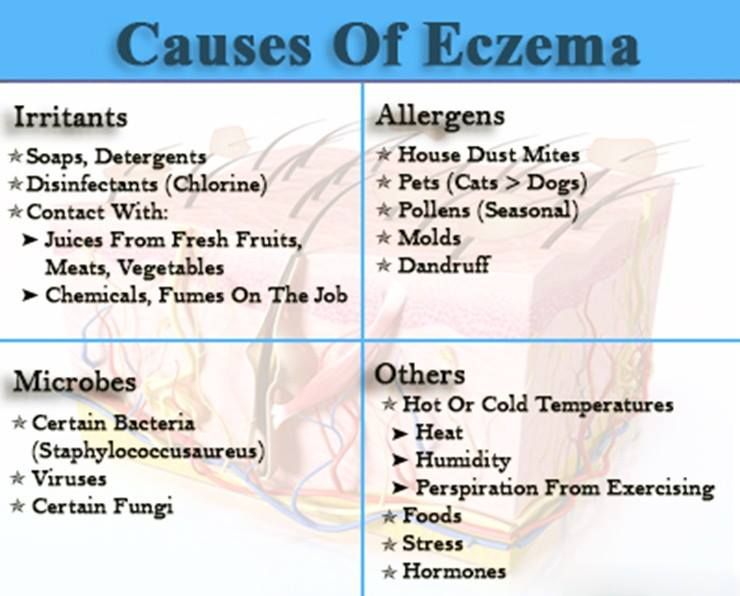
Sorbents and antihistamines
Antihistamines help to get rid of itching and inflammation.
Antibacterial therapy
Antibiotics with tetracycline should be used with caution in children under 10 years of age. Laboratory diagnostics helps the doctor determine the safest drug.
Anti-itching and sedative preparations
-
moisturizers;
-
oral substances;
-
intravenous corticosteroids.
Among sedatives, Novopassit, Persen, Valemidin are more commonly prescribed.
Hormonal drugs
Therapeutic regimens include hydrocortisone. Hormonal preparations are recommended in the form of ointments, tablets, lotions. These drugs are not recommended for use for more than 2 weeks due to possible complications.
Corticosteroid-based creams are effective for weeping eczema because they dry out the skin. Ointments have a healing effect and eliminate rough crusts. When localized in the scalp, emulsions and lotions with a light texture are used.
Ointments have a healing effect and eliminate rough crusts. When localized in the scalp, emulsions and lotions with a light texture are used.
Antiseptic and anti-inflammatory drugs
Antiseptic preparations are used to exclude additional complications and disorders:
Features of the treatment of eczema on the hands
For local treatment of eczema, ointments (pastes and creams) with corticosteroids, hormones with a pronounced anti-inflammatory effect, are used. They can reduce the inflammatory response and accelerate the process of skin regeneration.
Corticosteroid ointments have side effects: thinning of the skin, increased risk of bacterial and fungal infections, etc. Therefore, they should only be prescribed by the attending physician.
There are non-hormonal preparations that are also effective in treating eczema. These are topical calcineurin inhibitors - tacrolimus ointment (Protopic) and pimecrolimus cream. They reduce inflammation and itching. The dosage and duration of administration should also be determined only by the attending physician.
They reduce inflammation and itching. The dosage and duration of administration should also be determined only by the attending physician.
In severe eczema, extensive foci of inflammation and the absence of the effect of local therapy, systemic treatment is prescribed in the form of immunosuppressors - medicines that suppress the immune system.
In case of severe course of the disease, as well as in case of erythroderma, cytostatics are prescribed.
Antibiotics and antifungals are used to treat microbial and fungal eczema.
Features of the treatment of eczema on the legs
Eczema on the legs often develops as a result of an allergic reaction or severe vascular pathology (varicose eczema). Additional provoking factors may be weakened immunity and prolonged psycho-emotional stress.
Most often, microbial eczema develops on the legs. The main localization in places of burns, postoperative sutures, fungal infection, varicose veins. Eczema develops against the background of an already existing inflammatory process.
Main symptoms of eczema on the legs:
Sleep disturbances and headache may occur.
If you see a doctor in time, the prognosis for the treatment of eczema on the legs is favorable.
What is the treatment for eczema
The essence of the treatment of eczema is:
-
exclusion of contact with irritants,
-
proper nutrition,
-
itching,
-
local treatment with ointments and creams,
-
general treatment with tablets and injections.
The treatment of eczema in children is no different from that in adults. Often, the treatment plan includes physiotherapeutic methods that allow you to act directly on the damaged areas.
Dermatologists, through a combination of different methods, develop the best treatment for each patient.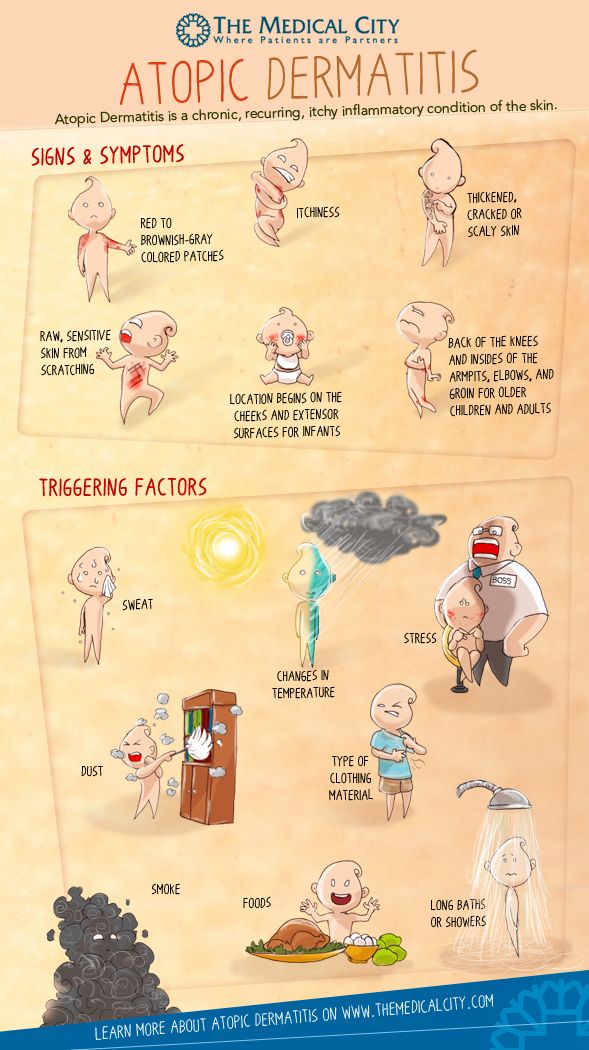
Treatment of eczema in children
To determine the tactics of treatment, it is necessary to establish the type of eczema, the cause of its occurrence and differentiate it from other dermatological diseases (herpes rash, diathesis, allergic reactions, urticaria, lichen, etc.).
Diagnosis includes:
-
complete blood count;
-
skin scraping for examination under a microscope;
-
allergy tests for atopic eczema to identify the source of the allergy;
-
histological examination - for the diagnosis of autoimmune diseases.
Treatment is selected taking into account the results of examinations, the age and characteristics of the health status of a small patient.
Comprehensive therapeutic treatment includes:
-
Individual diet
-
Sedatives (for sleep regulation)
-
Antihistamines (for itching and burning)
-
Anti-inflammatory drugs (to relieve swelling of the skin and improve general condition)
-
Multivitamins
-
Antibiotics or antivirals
To speed up recovery processes, and as an alternative to certain drugs, may be prescribed physiotherapy .
Mandatory antiseptic treatment of wounds and abrasions to exclude secondary infections.
It is especially important to properly care for the child's skin and follow all the recommendations of a dermatologist who will select individual care products.
Prevention of eczema
Personal hygiene is important, frequent overheating, accompanied by increased sweating, is unacceptable. A balanced diet should include a dairy-vegetarian diet with a low amount of carbohydrates and spices.
Prevention of eczema in adults
Overwork and stress can be triggers for the development of eczema, so it is important to maintain a balance between work and personal life, take time for good sleep and rest, play sports.
Use gloves when working around the house to prevent harsh detergents from coming into contact with your skin. Clean your hands thoroughly and use protective moisturizers.
For oily skin and genetic predisposition to eczema:
-
it is recommended to exclude fatty, sweet, fried and spicy foods from the diet.

-
It is not recommended to visit the bath and sauna.
-
it is not advisable to visit countries with high humidity or too hot climate.
For occupational eczema, it is recommended to change jobs to avoid complications.
Prevention of eczema in children
-
Personal hygiene
-
No diaper rash
-
Healthy and balanced nutrition
-
Regular cleaning
-
Footwear and clothing made from natural materials
-
Seaside recreation
If you experience symptoms, do not delay your visit to the doctor.
To make an appointment with EMC dermatologists, call +7 (495) 933 66 55.
Exacerbation of eczema in adults: causes, symptoms, recommendations for care - Body Care - Dry and atopic skin - Blog
The term eczema combines several types of dermatitis characterized by itching, redness and flaking of the skin. The mechanism of the occurrence of this disease is not fully understood, but doctors agree that the key factors are the genetic predisposition and the body's response to external and / or internal factors. It is impossible to get infected with eczema, but there is a high probability of its transmission “by inheritance”.
The mechanism of the occurrence of this disease is not fully understood, but doctors agree that the key factors are the genetic predisposition and the body's response to external and / or internal factors. It is impossible to get infected with eczema, but there is a high probability of its transmission “by inheritance”.
A common cause of eczema is an overactive immune system. The body reacts sharply to external and internal triggers with the development of inflammation, the symptoms of which are just itching, redness of the skin and pain.
Research shows that some people with eczema also have a mutation in the FLG gene responsible for producing filaggrin. Filaggrin is a structural protein of the skin involved in creating its protective barrier. With its deficiency, the stratum corneum of the skin cannot retain sufficient moisture, and also becomes more permeable to viruses and bacteria. Therefore, patients with eczema often have very dry skin that is prone to infection and inflammation.
Factors that provoke exacerbation of eczema
Dry/dehydrated skin. If the water-lipid balance is disturbed, the skin becomes fragile, easily injured, peeling and cracks appear on it. These conditions contribute to the development or aggravation of eczema.
External stimuli. Catalysts of irritation may well be the means and objects with which we come into contact on a daily basis: household chemicals, cosmetics, and even natural substances (for example, juice of fresh vegetables / fruits).
Some of the common triggers are:
- metals (especially nickel)
- cigarette smoke
- soaps and cleansers
- perfumery
- certain fabrics such as polyester and wool
- antibacterial creams and ointments
- formaldehyde (found in disinfectants, some adhesives)
- isothiazolinone - an antibacterial compound found in hygiene products such as baby wipes
- cocamidopropyl betaine - an ingredient used as a thickener in shampoos and lotions
- paraphenylenediamine - an ingredient used in various dyes, such as hair and eyebrow dyes or temporary tattoo inks
External irritants also include the adverse effects of temperatures and ultraviolet radiation, and injuries.
Internal factors. Malfunctions of the kidneys, gastrointestinal tract, neuroendocrine diseases, heredity, neuroses.
Stress. Overwork and stressful situations are also often triggers for exacerbation of eczema.
Types of eczema
According to the nature of the rash, eczema can be divided into two types:
Dry. It manifests itself in the form of excessive dryness of some areas of the skin. It resembles a dry crust and is accompanied by itching, redness, peeling and the appearance of painful cracks. Most often localized on the arms and legs.
Wet. A scattering of small bubbles or a wet spot, accompanied by intense redness of the skin, as well as severe itching and burning. Most often occurs on the head (under the hair), on the inner surfaces of the elbows and knees, on the chest.
In domestic medicine, they are divided into the following types:
| View | Causes | Symptoms | Localization |
| Eczema vera | It is not possible to find out the exact cause of the development of the disease. Exacerbation can be caused by stress, skin trauma, contact with allergens, endocrine disorders, etc. | During periods of exacerbation, reddening of the skin occurs (while the red spots do not have clear boundaries), a rash appears in the form of small bubbles. Over time, they burst, while the damaged surface begins to release a light, transparent liquid. With a decrease in the inflammatory process, the weeping surface dries up and becomes covered with crusts. | "Islands" of inflammation (often multiple) on the skin of the face, hands and feet. |
| Eczema dyhydrotic | Is a form of true eczema. Approximately half of patients have a hereditary predisposition to allergic diseases, and such eczema appears most often between the ages of 20 and 40 years. | Vesicles with a clear liquid, shaped like grains of rice and located deep in the skin. Their appearance is accompanied by itching, and when they break, painful, slowly healing cracks are formed, which are characterized by other signs of true eczema: redness, peeling, itching. | On the lateral surfaces of the fingers (in 80% of cases), less often on the legs. |
| Microbial eczema | Occurs as a complication against the background of a weakening of local and / or general immunity in skin diseases caused by microorganisms (streptoderma, fungal infection, scabies, etc. | Red, crusty lesions with well-defined margins. Surrounded by small itchy vesicles filled with a light clear liquid. | Near injured or infected skin. |
| Seborrheic eczema | It is believed that the causative agent is a yeast-like fungus of the species Malassezia. They are a normal component of the normal microflora of the skin, however, under the influence of genetic, hormonal, immune and other factors, their balance may be disturbed. | Reddish rash covered with yellow or white scales, with larger nodules and crusts. Accompanied by itching of varying severity. The foci of inflammation are characterized by swelling, swelling of the skin, the areas look elevated above the rest of the skin. | On areas of the skin with a large number of sebaceous glands, hairy areas. It usually starts on the head and can spread to behind the ears, eyebrows, nasolabial folds, neck, upper chest, and back. |
| Childhood eczema | Occurs due to insufficient immunity and / or failure of the gastrointestinal tract. Typically develops between 3-6 months of age. | May have clinical features of true, microbial and seborrheic eczema. Characterized by "milky" crusts. Accompanied by itching, insomnia. | Cheeks, forehead, ears, scalp, folds of extremities, buttocks. |
| Occupational eczema | Develops under the influence of "industrial" allergens: alloys of various metals, mercury and its compounds, antibiotics, epoxy resins, synthetic adhesives, pesticides, etc. | Develops gradually as a result of prolonged exposure. Symptoms repeat the picture of true eczema, but cause much more discomfort. The disease has a long course, since the cessation of contact with the allergen does not lead to a rapid disappearance of symptoms. | On exposed skin, in contact with an irritant. |
Atopic dermatitis and eczema
In the Russian medical classification, eczema and atopic dermatitis are not identified, unlike in many other countries. However, comparing the symptoms and course of atopic dermatitis with the above characteristics of the types of eczema, you can see many similarities.
Atopic dermatitis is a chronic skin disease, in the acute stage characterized by bouts of itching of varying intensity, redness of the skin, the appearance of a rash in the form of vesicles or nodules, fluid separation.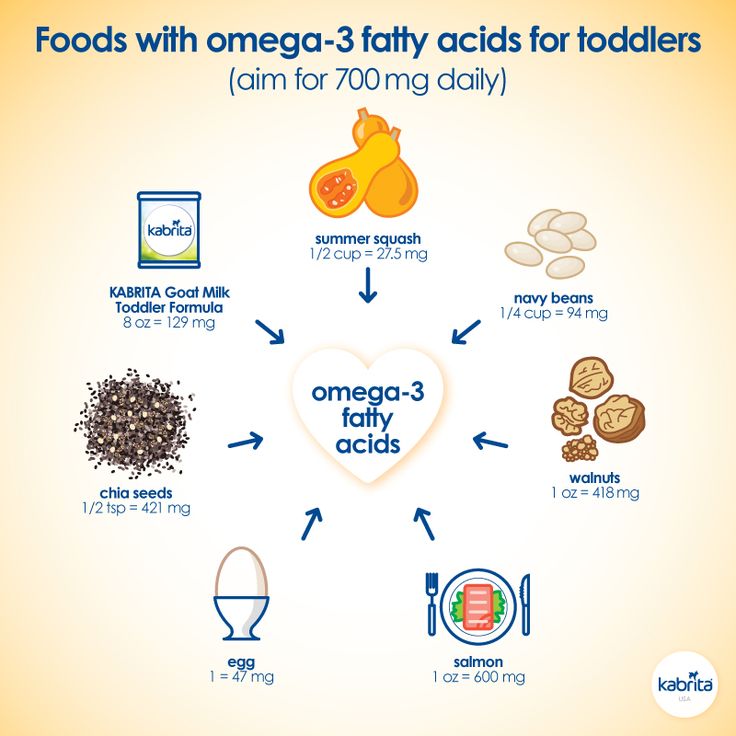 During periods of "calm" the disease manifests itself as increased dryness of the skin, and in places that are often prone to irritation, compaction and coarsening may persist.
During periods of "calm" the disease manifests itself as increased dryness of the skin, and in places that are often prone to irritation, compaction and coarsening may persist.
Dermatologists define three age periods for atopic dermatitis:
- infant - from two months to two years. In some cases, the symptoms of infantile atopic dermatitis disappear by the age of two;
- children - from 2 to 13 years;
- adolescent and adult (over 13 years old).
As in the case of true eczema, the likelihood of developing atopic dermatitis is closely related to hereditary factors: if both parents are healthy, the probability of its occurrence is only 20, rising to 50% if one of the parents is ill with atopic dermatitis or was ill in childhood , and up to 80% - if both parents are or were affected by the disease.
Due to the similar nature of the two conditions, the basic guidelines for skin care for eczema (which we list below) also apply to cases of atopic dermatitis.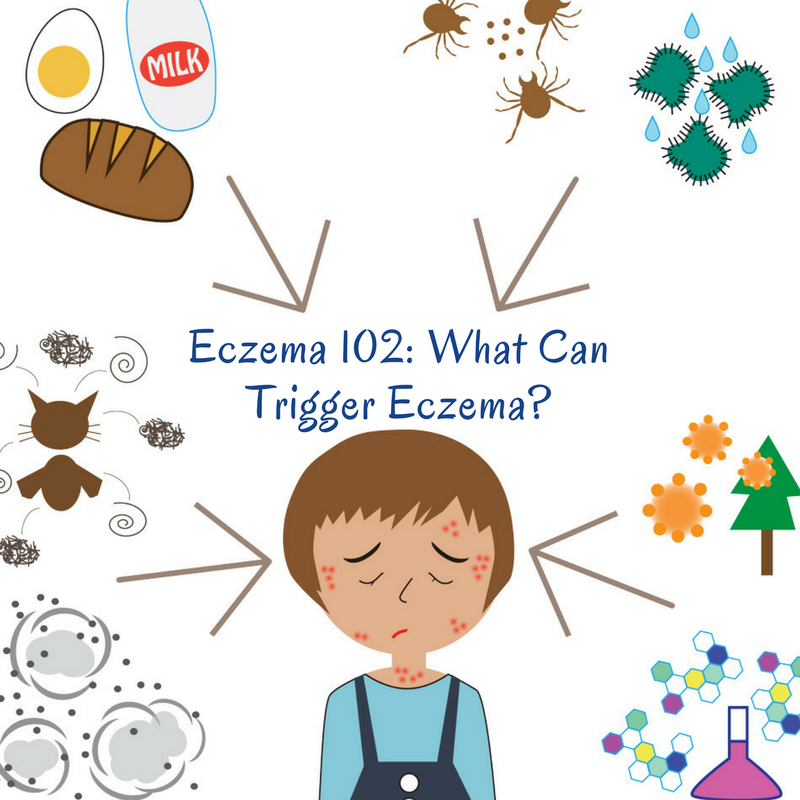
Read more about atopic dermatitis in our articles:
Atopic dermatitis in children
Adult atopic dermatitis
Treatment and care
Eczema is not only a cosmetic problem. During periods of exacerbation, it can negatively affect the overall quality of life, causing significant physical discomfort and emotional stress. Unfortunately, modern medicine does not provide an opportunity to cure this disease once and for all, however, with the help of properly selected medications and constant skin care, it is quite possible to minimize its symptoms.
In the case of eczema, it is important to first consult a dermatologist in order to find out the cause of the disease and select the appropriate medication and physiotherapy. To identify the triggers of eczema in case of its allergic nature, consultation with an allergist will help. With the sudden development of eczema in adulthood without the intervention of external factors, a general examination of the body is also recommended in order to identify internal pathologies that could provoke a skin disease.
Both in the acute phase and in the "calm" periods, skin prone to eczema requires special care.
Regular cleaning
For eczema, a daily shower is indicated, however, it is advisable to reduce the time of its use to 10 minutes, and use special delicate, hypoallergenic products for cleansing. When taking a bath, do not use hot water (it can dry out the skin).
Shower gel Atoderm, Bioderma
Lipikar AP+ Cleansing Oil, La Roche-Posay
Cleansing Foaming Cream with Pump, Uriage
In case the eczema foci are located in the scalp, it is also important to choose a mild shampoo with a neutral pH.
Mild Shampoo pH5, Topicrem
Shampoo pH-Balance, Librederm
Moisturizing Shampoo, Emolium
Moisturizing and protecting the skin
Because eczema-prone skin is often dry and flaky, skin care should focus on restoring the protective barrier and fluid-lipid balance. Be sure to use a moisturizer, balm, or lotion immediately after your shower to prevent moisture loss.
Be sure to use a moisturizer, balm, or lotion immediately after your shower to prevent moisture loss.
Exomega Control Softening Lotion, A-Derma
Lipid-restoring balm, Topicrem
,
Lipid replenishing balm Xeracalm A.D., Avene
In the acute phase, it is desirable to exclude products with AHA / BHA acids, retinol and other potent components from the care system, even if they are not applied to disease-prone areas of the face and body. pH-neutral emollients will help keep your skin in a stable, healthy condition.
Exomega Control Emollient Cream, A-Derma
Hyalu B5 Hydrating Serum, La Roche-Posay
Face cream Xemose, Uriage
Solar protection
Sunbathing is thought to improve the skin in seborrheic and microbial eczema, but in true eczema it can aggravate the reaction.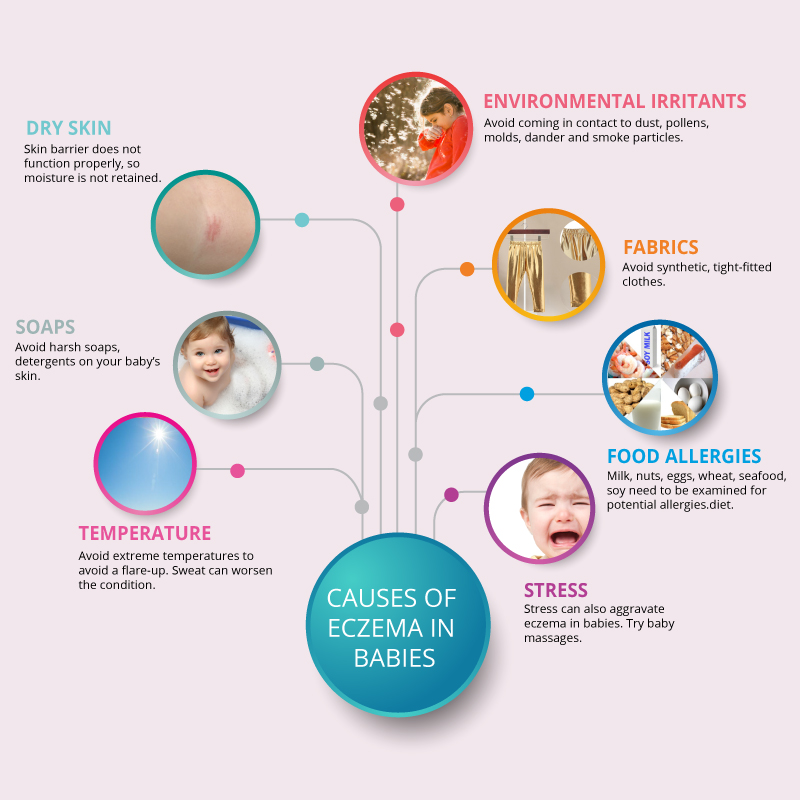

 As a rule, it occurs in childhood and passes into the chronic stage, where periodic outbreaks are replaced by periods of remission, persisting throughout life.
As a rule, it occurs in childhood and passes into the chronic stage, where periodic outbreaks are replaced by periods of remission, persisting throughout life.  Often occurs as a reaction to household chemicals or as a result of regular prolonged contact with water.
Often occurs as a reaction to household chemicals or as a result of regular prolonged contact with water.  ) and injuries.
) and injuries.