Baby face goes red when feeding
Why Does My Baby’s Face Turn Red When Breastfeeding?
Being a new mom is quite challenging, especially if you start facing problems you weren’t prepared for.
One of the most confusing questions you might end up asking is: why does my baby’s face turn red when breastfeeding?
Because many mothers have faced this issue, we’ve decided to discuss the reasons behind it and what you can do to fix it.
Let’s dive in!
Why Does My Baby’s Face Turn Red When Breastfeeding?
The answer isn’t as straightforward as you might assume. This is because there are numerous reasons why a newborn face turns red when breastfeeding.
In some cases, the cause can be purely natural. While sometimes, red blotches appearing on your baby’s face can be a result of other things you could treat.
In this section, we’ll address every possible reason behind this issue.
Why does my baby’s face turn red when breastfeeding?
Blood Sugar Spike
Let’s start with the most basic reason why many babies turn a bit redder in the face after eating.
When a baby consumes breast milk, the blood sugar levels get higher because of the carbohydrates in milk.
Also, some studies have found that secondhand sugars can pass through breast milk to the baby.
As a result, the blood vessels dilate, causing the baby’s face to flush for a little while.
Of course, this isn’t problematic at all. Just wait for a few minutes after the feeding session, and the redness should fade.
Natural Reaction to the Food You’ve Eaten
Ever noticed that your face might get a bit flushed after having an exceptionally good meal? Oftentimes, this meal tends to be spicy.
Well, it could be just the same when a newborn face turns red when breastfeeding.
Usually, your baby might develop red cheeks as a reaction to some types of food that you’ve consumed.
If you’ve eaten something with spices, nuts, or cow milk, you might get this response from your baby’s skin.
In this case, the red skin should disappear shortly after your baby is done feeding.
How to Fix This Issue
You can prevent this from happening by eliminating possible allergens from your diet.
If you must, you can have a spicy meal about two hours before you start breastfeeding. Therefore, its traces shouldn’t find their way to your breast milk.
Cow’s Milk Protein Intolerance
While CMPI is rare in babies, it’s still a possibility if your newborn face turns red when breastfeeding.
Cow’s milk can reach your baby’s system from both your breast milk and the baby formula.
If your diet includes dairy, then the cow’s milk protein will surely find its way to your little one.
As a result, your baby might develop an allergic reaction to it, including having red splotches on his or her cheeks.
But how can you be sure it’s CMPI that’s causing this issue?
The only way to know is to start following a dairy-free diet for 6-8 weeks, then see if the symptoms go away.
I know it can be hard since the majority of food includes dairy, i. e. butter, cheese, milk, etc.
e. butter, cheese, milk, etc.
This could be a viable answer to the question: why does my baby’s face turn red when breastfeeding?
How to Fix This Issue
Once you’re certain that it’s CMPI you’re facing, you’ll have to cut out on your dairy intake.
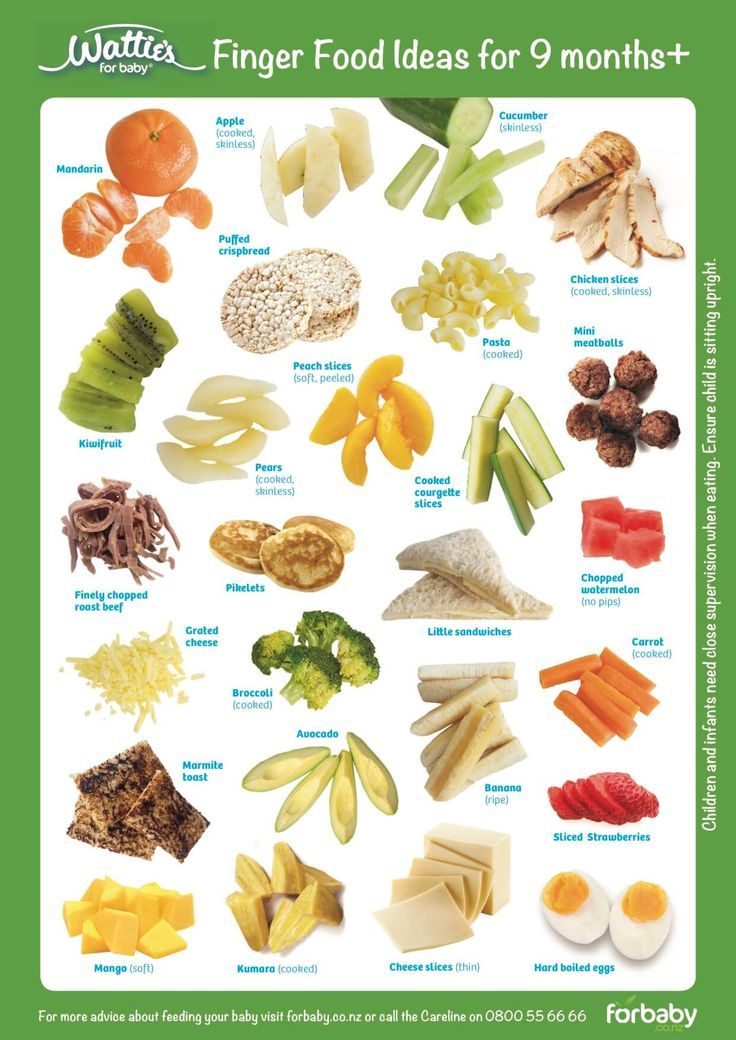
You can reintroduce foods that contain dairy gradually when the baby reaches six months of age. Remember to go slow and watch for any worrisome signs.
Some mothers might consider switching to bottle feeding if they don’t want to give up on dairy products.
However, it still may not be the best option because most types of baby formula also contain traces of cow’s milk.
If this is the case, you could switch to a soy-based formula. Just make sure that your baby isn’t allergic to soy milk.
Sensitive Skin
Again, you might ask yourself: why does my baby’s face turn red when breastfeeding? And the answer could be really simple.
The face of an infant tends to be sensitive, especially during the weeks after birth. In some areas of his or her body, the skin might even seem translucent.
In some areas of his or her body, the skin might even seem translucent.
So, the mere act of being pressed against your body can cause him or her to flush slightly.
Therefore, having this extra temperature besides being fed a generous amount of breast milk could cause this redness. Yet, this isn’t limited to breastfeeding only.
In fact, several moms have noticed that their babies’ faces turn red when drinking from the bottle. As a result, you can assume that the act of feeding itself causes a healthy flush on your baby’s face.
Consuming food increases energy, and more energy in your baby’s body could cause him or her to move while being fed. Then, more blood will rush to his face, which isn’t problematic as you may have presumed.
Overheating
Sometimes, red blotches on your baby’s cheeks could be an indicator of an underlying health condition you might not notice right away. One of these conditions could be overheating.
See, a baby may already have this problem before a feeding session due to multiple reasons. Overheating in infants can occur due to:
Overheating in infants can occur due to:
- High room temperature
- Co-sleeping with parents
- Too many blankets
- Too many layers of clothing
Of course, you can easily tell if a baby is too warm to be comfortable. However, a sleep-deprived mom can be too tired to notice the signs of overheating.
So, she’ll start breastfeeding her baby and then will begin to see that his face has turned red.
Why does my baby’s face turn red when breastfeeding, she’ll wonder. In this case, an already warm baby will get even hotter because of his proximity to his mother’s body.
How to Fix This Issue
Now, if this scenario ever happens, the mom should stop the feeding session to cool down her overheated baby.
- Dress your baby in lighter clothing
- Take your baby to another room with a cooler temperature
- Dip a soft cloth in lukewarm water, then wipe your baby’s body
If the high temperature remains, then the mom has to contact her pediatrician at once.
Eczema
Eczema is quite common in infants, especially during their first few months. This condition appears as red, crusty patches on the baby’s skin.
These red areas can show anywhere on the body, but mostly on the cheeks and the joints of the arms and legs.
Of course, eczema is easily treatable, and most babies quickly overcome it. You can’t be exactly sure if the red spots on your baby’s face are a result of eczema or some other type of rash.
In this case, always consult your doctor before starting treatment.
Therefore, ‘why does my baby’s face turn red when breastfeeding?’ may not be the right question to ask here.
This is because eczema has nothing to do with breastfeeding. However, the red patches on a baby’s face could become more irritated because of friction and extra body heat.
Still, you might be curious about what causes eczema.
Sometimes, it just runs in the family. So, if you or your partner have eczema, then your baby will have a bigger chance of having it, too.
On another note, eczema can affect babies with problems in the skin barrier. In this case, their skin tends to let germs in while keeping the moisture out. So, that’s another possibility.
How to Fix This Issue?
You don’t need to trouble yourself if your baby has eczema. Most of the time, it just disappears as your baby grows older. Such a relief!
Yet, some children grow into adults without getting rid of eczema. In these rare cases, children can go years without developing any symptoms, but their skin tends to be too dry.
Luckily, you can do many things to treat eczema to get rid of the irritated patches on a baby’s face. For instance, you could:
- Apply moisturizer after each bath (go for an ointment with ceramides)
- Bathe your baby often in lukewarm water to keep his skin moist
- Baths could also relieve itching
- Keep the baths short (only 10 minutes)
- Clean your baby’s skin gently not to irritate it
- Gently pat the skin dry after each bath
- Use unscented laundry detergent to wash baby clothes
Also, make sure that you steer clear of the following eczema triggers.
- Dry skin and low humidity
- Allergens such as nuts, eggs, or cow’s milk
- Irritants including scented products, perfumes, polyester clothes, etc.
- Heat
- Sweat
- Stress
Once a baby recovers from eczema, the red blotches on his or her skin should disappear. So, you should no longer have to ask, ‘why does my baby’s face turn red when breastfeeding?’
Milk Rash
At a first glance, you might think that breast milk can cause rashes. But milk rash isn’t exactly caused by breast milk. Rather, it might be a result of the breastfeeding process itself.
Milk rash, or Atopic Dermatitis, is a skin condition that can affect babies, leaving red spots on their cheeks. So, how can breastfeeding cause milk rash?
Breastfeeding can pass different allergens to the baby’s system, which can cause these red blotches. The food that the mother consumes, especially chicken and eggs, can lead to this condition.
Yet, other things could trigger milk rash, too. These include:
These include:
- Air pollution
- Heat
- Dust mites
- Germs in the air
How to Fix This Issue?
You’ll have to act based on the cause of milk rash. If you suspect that the culprit is your dietary choices, then you might have to make several changes to the food you consume.
Besides that, you should work to eliminate any of the triggers that we’ve listed above. Then, it may be a good idea to do the following to soothe the rash.
- Avoid bathing your baby in warm water to prevent dryness
- Apply moisturizer to the affected skin
- Try to prevent your baby from scratching these red spots
In some cases, the rash might spread and develop a fever. If things get this far, the mother should take her baby to the doctor at once.
Frequently Asked Questions
If you’ve ever wondered, ‘why does my baby’s face turn red when breastfeeding’, you might have the following questions as well.
Why is my baby drooling while breastfeeding?
It’s completely normal for a baby to drool while breastfeeding.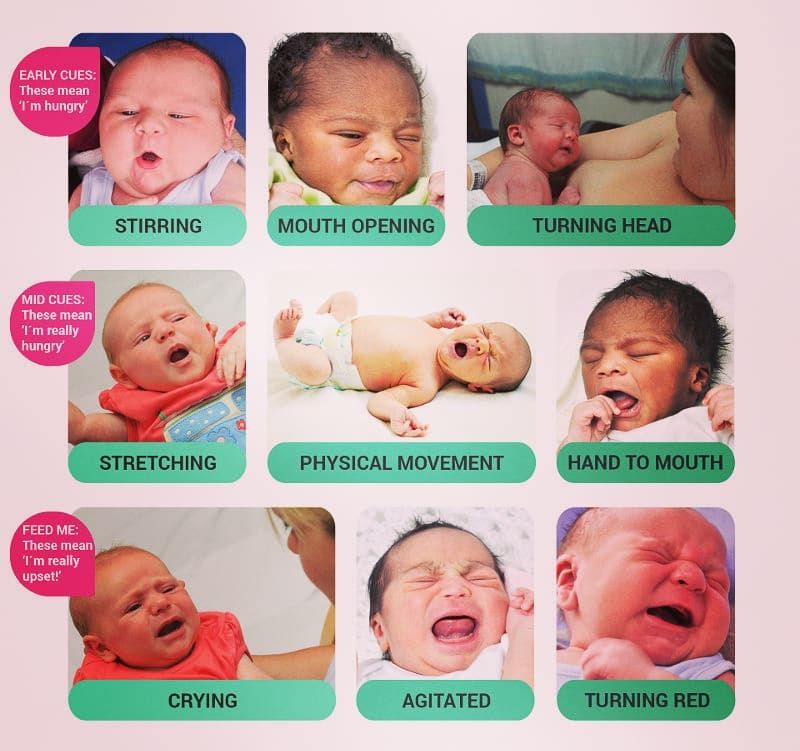 When the baby is still an infant, he or she doesn’t have full control of their swallowing function.
When the baby is still an infant, he or she doesn’t have full control of their swallowing function.
Also, babies learn to use their mouth muscles during this stage of their lives.
Drooling can last up to 18-24 months.
Does breast milk irritate babies?
Not at all. In fact, you can use breast milk to ease several types of rashes, including eczema.
This is because breast milk includes elements that offer protection against infections. Also, it can be a natural moisturizer for your baby’s skin.
Therefore, you could pour a few drops of breast milk on a cotton pad. Then, use this pad to wipe down the red spots on your baby’s cheeks. After a while, you should begin to notice improvements.
Can milk rash only affect breastfed babies?
Not exclusively. Milk rash can also happen to bottle-fed babies because many baby formulas include cow’s milk protein.
Some people confuse milk allergies with lactose intolerance because they share some symptoms. However, these two conditions have varying causes, not to mention that they affect the human body in different ways.
However, these two conditions have varying causes, not to mention that they affect the human body in different ways.
What does it mean when a baby’s face turns red?
Most of the time, the red coloring on a baby’s face can be the aftermath of the blood vessels expanding.
On the other hand, it can be a skin rash with blotchy or flaky spots. Usually, these spots tend to be dry.
Both conditions can be caused by many things, which we’ve already discussed in this article.
To Wrap It Up
Why does my baby’s face turn red when breastfeeding?
The answer could be as simple as having the baby pressed against your body heat. In other cases, knowing the causes might require you to notice other symptoms.
‘But now I’m confused’, you might say, ‘I can’t tell which thing is the reason why my newborn face turns red when breastfeeding.’
We understand that some moms may not find the right conclusion quickly. Therefore, you must consult your pediatrician to let you know what caused this condition. With an accurate diagnosis, you could begin treating your baby without missing a beat.
With an accurate diagnosis, you could begin treating your baby without missing a beat.
Red Blotches On Baby's Face When Breastfeeding
-- Discover a safe space for women to meet, listen and share valuable advice!
The Mothers Community is a safe online community sharing advice on fertility, pregnancy and motherhood through to menopause. Join Community Here --
Are you concerned about red blotches on baby’s face when breastfeeding?
New moms often face challenges, especially physical body-changing to post-partum issues, which they weren’t expecting.
It becomes mentally difficult for a new mom to concentrate on their baby’s health wholeheartedly during these times.
Breastfeeding is one of the most effective methods to ensure a child’s health.
Antibodies in the vaccine protect against many common childhood illnesses and are safe, clean, and effective.
Nearly two out of three infants do not receive breastmilk exclusively during their first six months, a report which hasn’t changed since the early 1990s.
Infants thrive on breast milk. Breastmilk supplies all the energy and nutrients babies require for the first few months.
During the second half of the first year, breastmilk usually provides half of a child’s nutritional needs and one-third during the second year.
Red Blotches On Baby’s Face When BreastfeedingInfants whose parents suffer from allergies are often affected by milk rash.
Babies can develop the rash after their mothers consume food allergens such as chicken or eggs.
Individuals can be affected in different ways. Further, air pollution, heat, dust mites, or tiny germs present in the air or on household items, like pillows and blankets, triggers milk rash.
These are all causes of irritated skin. Since it locates on the cheeks, your baby can easily scratch milk rash with their hands.
This will lead to an open skin wound and develop a rash. The sores can allow infections to spread to other parts of the body.
Breastfed children score higher on intelligence tests and are less likely to become overweight or obese.
They also have a lower probability of developing diabetes later in life.
Moreover, breastfeeding women have a lower risk of developing breast and ovarian cancer.
A lack of understanding of breast-milk substitutes undermines global efforts to improve breastfeeding rates and duration.
1. Does Breastfeeding Cause Rashes On Babies’ Face?Before birth, a woman experiences fluctuating hormone levels due to the womb and postpartum environment.
These hormone fluctuations can also affect the skin of her newborn.
If mothers have clogged pores during pregnancy due to their hormone levels, their newborns may also have acne bumps.
Milk allergy can result in fussy, gassy, snorting, barfy, and rashy skin in the newborn.
This is due to the immune system resisting and revolting against the proteins of the cow’s milk.
Mother’s breastmilk proteins are mild; they won’t harm the baby’s skin.
2. When Is A Baby Allergic To Breastmilk The Best Time To Find Out?The symptoms of a food allergy may appear in babies who have never been breastfed or exposed to formulae, such as abdominal pain, bloody stools, diarrhea, vomiting, eczema, bloating, nausea, and constipation.
A mother eating allergic food can develop allergies in their babies through breast milk.
3. A Rash On My Baby’s Face: Do I Need To Worry?If the rash on your newborn’s skin suggests a severe concern about their health, you should think twice before bringing them home.
If a child has a fever, cold or cough, congestion, swollen neck glands, or other symptoms, the parent should insist that the child see a doctor.
4. My Baby Has A Rash On His Face. What Is The Best Way To Treat It Naturally?Regular application of olive oil on the skin can heal and regenerate damaged skin tissue.
Coconut oil may soothe and hydrate a rash. Also, petrolatum might help to prevent rashes. Baby oil can also benefit the skin.
5. Why Do Babies Get Milk Spots?You can use biodegradable, vegan, cruelty-free, and sensitive wet wipes to remove leftover milk spots from your newborn and boiled cool water.
A variety of factors can lead to milk spots. One of them is that the child’s skin is still developing.
One of them is that the child’s skin is still developing.
It might be due to hormonal or nutritional reasons, such as passing hormones from the mother or the child or something else blocking the pores. You should also make sure that they are eating on schedule.
- Prevent and treat
Avoiding the triggers of milk rash is the first step to avoiding it.
If the rash is caused by breastmilk, you should avoid foods that might cause an allergic reaction.
Avoid bathing your baby with warm water when they have milk rash because it will make their skin drier and itchier.
Keep the cheeks dry by applying a gentle baby moisturizer.
No matter how itchy your baby’s cheeks seem, don’t scratch them. If you observe them having fever, then consult with your doctor.
6. What Can Be Done To Fix This Problem?Depending on the cause of the milk rash, you will have to take action.
There could be several dietary changes you need to make if your diet is causing the problem.
In addition to eliminating any triggers above, you should also work to minimize triggers that you cannot control.
You may want to do the following to soothe the rash:
- To prevent dryness, do not bathe your baby in warm water
- To moisturize affected skin, apply moisturizer
- Try not to scratch these red spots on your baby
- A fever might develop if the rash spreads. The mother should seek medical attention immediately if things get to this point.
If you press the baby against your body heat, you might be able to fix the problem.
You might have to notice other symptoms to figure out the cause.
Some mothers might not reach the correct conclusion right away, which is understandable.
It’s imperative to consult your pediatrician about this condition to determine its origination.
As soon as your baby’s diagnosis is accurate, you can begin treatment immediately.
Baby’s aren’t fully developed during their infancy years. Babies tend to drool between 18 and 24 months.
Additionally, babies learn to use their mouth muscles during this development phase.
Learn more about drooling: How Many Bibs Do I Need?
When Breastfeeding, Why Does My Baby Drool?A Baby’s swallowing function is when their mouth muscles are developing.
They excessively drool during this stage while they’re breastfed.
Do Breastfed Babies Only Suffer From Milk Rash?Certainly not exclusively. Cow’s milk protein found in baby formulas can also trigger milk rash.
There are similarities between milk allergies and lactose intolerance, which leads to confusion among people.
However, the two conditions are caused by different things and affect the body differently.
Iesha Mulla
Iesha is a loving mother of 2 beautiful children. She’s an active parent who enjoys indoor and outdoor adventures with her family. Her mission is to share practical and realistic parenting advice to help the parenting community becoming stronger.
A safe space for women to meet and find support!
The Mothers Community is a place to connect with women who are at a similar stages in life–from fertility, pregnancy and motherhood through to menopause.
Join a community who are there to listen, share information and offer valuable advice. Join Community
Take matters into your own hands! Expert advice for Fertility, Pregnancy and Motherhood! Discover More Here
Diathesis, red cheeks - atopic dermatitis?
When children come to an appointment with red cheeks, red spots with peeling on the arms and legs, manifestations of atopic dermatitis, then parents often do not know why their child has such problems.
Most often, mothers in such cases associate the manifestations of dermatitis with "Moscow water", which "does not suit" them.
However, it must be admitted that food allergies are most often manifested in infants and, in the vast majority of cases, the culprit is cow's milk, or rather, cow's milk proteins (proteins).
If the child receives artificial nutrition, then the basis of such mixtures is cow's milk proteins (whey and casein fractions of proteins). Thus, when receiving milk formula, the child receives the corresponding allergen in large volume.
If the baby is breastfed, cow's milk proteins enter the baby's body through breast milk.
Studies have shown that 95% of women have beta-lactoglobulin in breast milk, one of the most allergenic proteins in cow's milk.
However, it should be emphasized that children who are breastfed (naturally) suffer from food allergies much less often, which is due, among other things, to a lower content of such components in breast milk.
The basis for the treatment of manifestations of food allergies, intolerance to cow's milk proteins, is the selection of proper nutrition.
When a child is breastfed and symptoms of intolerance to cow's milk proteins are noted, the mother is often advised to follow a strict dairy-free diet, when all dairy products are excluded from the diet, including cheese, kefir, cottage cheese, etc., and not just whole milk, as sometimes think. Since such dietary recommendations are quite difficult to maintain, especially for us, the inhabitants of the middle lane, where the culture of dairy nutrition is widespread, it is very important that these prescriptions have a real basis.
However, it is impossible not to admit that there is an improvement in the condition of the child's skin, the work of his digestive tract with the correct correction of nutrition. Hence even such a term as "diet diagnostics" appeared, i.e., when, after the exclusion of certain products, we see a positive result, which confirms the diagnosis, and "diet therapy", when continuing to follow the recommendations on proper nutrition, it is possible to achieve a good therapeutic effect.
One of the frequently asked questions of parents is: "Is it possible to transfer a child with intolerance to cow's milk proteins to goat's milk?"
The answer is not entirely reassuring. In the vast majority of children, when trying to replace a formula based on cow's milk with a "goat" formula, it is not possible to achieve remission and subsidence of the symptoms of the disease.
For the rational nutrition of formula-fed children with manifestations of allergy to cow's milk proteins, therapeutic specialized nutrition based on hydrolyzed (split) components is used. In such mixtures, the protein is divided into smaller components, down to the smallest particles - amino acids. Such therapeutic nutrition should be selected by a pediatrician in close cooperation with an allergist-immunologist.
Another important aspect of the treatment of atopic dermatitis is topical therapy. And it is necessary to start in this case with a basic, long-term moisturizing of the skin with specialized means - emollients.
Atopic dermatitis is treated in stages, i.e. according to the severity of the disease, the "severity" of the drug effect is selected. In other words, we move from the simple to the complex, from moisturizers for the skin to preparations containing anti-inflammatory agents, hormones, antibiotics, if necessary, etc.
Fortunately, usually by the age of 2-3 years, allergy to cow's milk proteins fades into the background, and in 80% of cases, children develop tolerance (immunity) to this product by the age of 5.
However, the calmer the child's early age passes, the higher the chances of not moving to a new stage of allergic processes, and maintaining health for many years.
Therefore, it is very important, if allergic pathology is suspected, to look for the correct cause of such a condition, and to adhere to a healthy lifestyle, the principles of rational nutrition.
Pediatrician, allergist-immunologist, chief physician of the clinic "Sanare" Marinina Yulia Mikhailovna
Alarming symptom: pathologies in newborns
depends on the timely detection of certain pathologies in the baby.
Pediatrician of clinic “9months" Avdeeva Natalya Nikolaevna.
- Natalya Nikolaevna, what pathologies are most common in newborns?
- Almost 99% of newborns have neurological abnormalities, which are minimal at first and, with adequate management of the child, in most cases level out by the year.
— What does "adequate management of the child" mean?
- I mean a massage performed on time, gymnastics started on time ... Moreover, I want to note that even for an absolutely healthy child under one year old, it is desirable to conduct at least three courses of gymnastics and massage, with the involvement of a good specialist. This is necessary so that the child learns to turn, sit down, get up, walk in time. Such courses are aimed at the development of the nervous and, as a result, the musculoskeletal systems.
— What symptoms can “tell” the mother that the baby has this or that neurological disorder?
- Parents should definitely pay attention to such a symptom as twitching of the chin. This may indicate that there is an underdevelopment of the nervous system and individual structures of the brain. It should also cause concern when the child stands on tiptoe. As a rule, no attention is paid to such a phenomenon. But if the baby stands on tiptoe and at the same time crosses his legs, leans poorly - this may be a mild symptom of flaccid lower paraparesis, and later, by the age of one, it may result in cerebral palsy.
This may indicate that there is an underdevelopment of the nervous system and individual structures of the brain. It should also cause concern when the child stands on tiptoe. As a rule, no attention is paid to such a phenomenon. But if the baby stands on tiptoe and at the same time crosses his legs, leans poorly - this may be a mild symptom of flaccid lower paraparesis, and later, by the age of one, it may result in cerebral palsy.
The fact is that usually cerebral palsy is not diagnosed until a year old, since this period of time is a long rehabilitation period, when the crumbs have a good potential for recovery. The first year of life in general, in terms of its restorative capacity, is incommensurable with any other interval in a person's life. Here, a very large work of the mother herself must take place, in combination with the work of a neuropathologist, a manual therapy doctor, a massage therapist, and an exercise therapy doctor. The treatment includes water therapy, drug therapy, massage, gymnastics, etc.
Hand tremor should be another alarming symptom for the mother. Pay attention to the situations in which this occurs. The norm is if it is a reaction to a bright light, a strong sound. If a baby older than a month often throws up his hands in an absolutely calm environment, this may indicate convulsions. Here, too, a full examination is necessary. You will need to measure the intracranial pressure in a child, make an electroencephalogram, check the reaction to light and sound stimuli at rest, in sleep, etc.
If, in combination with shudders and fears, the baby also has a protrusion of the tongue, this may indicate such an endocrinological pathology as congenital hypothyroidism. Initially, screening is carried out in the maternity hospital, when blood is taken for 5 infections, and geneticists look at it. But further consultation with an endocrinologist is necessary. Early initiation of treatment prevents the disability of the child. In connection with the foregoing, I want to note that an early discharge from the hospital is highly undesirable - for 3-4 days. After all, many such moments are revealed just on the 4th-5th day - that is, when the mother, who was discharged earlier, is already alone with the child and with the problem that has arisen.
After all, many such moments are revealed just on the 4th-5th day - that is, when the mother, who was discharged earlier, is already alone with the child and with the problem that has arisen.
— In addition to neurological, what other pathologies can parents independently suspect in a child?
— The baby's reaction to external stimuli says a lot. So, if a child in 2-3 months does not respond to sounds (rattles, voice), you need to urgently contact an otolaryngologist. The first hearing test is carried out at the maternity hospital, but at the age of three months, the ENT doctor must definitely examine the baby. In Kazan, for example, quite often children are identified who initially respond well to checks, but in the end, conductive hearing loss is found in them. The fact is that before that, the child could react purely intuitively, say, not to his mother's voice, but to facial expressions. It happens that as early as 3 years old, such children begin to be treated as autistic, although in reality it's all about hearing loss.
There should also be concerns if the child does not follow objects (at a distance of 30 cm - the brightest vision in newborns - the baby should "catch" his mother's face and reach for it, try to keep it in his field of vision), by 3 months reacts to light, to colors. Of course, the baby does not yet identify the colors themselves, but the change of colors should cause him some emotions (joy or, conversely, irritation). The mother can also track the reaction of the pupil to light on her own. To do this, you need to take the baby to bright light from a dark room. If at the same time the pupils of the crumbs did not narrow, they remained as wide as in the dark, it means that the child does not see light, which indicates a pathology of the retina. At the same time, the same constriction of the pupil is already a neurological pathology. In any case, you need to urgently contact the specialists.
At a scheduled examination by a surgeon at the age of one month, you should definitely pay attention to the doctor if the baby burps frequently and profusely. In fact, the child should spit up. For the first three months, the baby burps after almost every feeding. But he should not give out all the food outside with a "fountain". If this happens, and the child gains weight poorly in the first month or two, it is necessary to exclude pylorospasm, a serious surgical pathology that requires hospitalization.
In fact, the child should spit up. For the first three months, the baby burps after almost every feeding. But he should not give out all the food outside with a "fountain". If this happens, and the child gains weight poorly in the first month or two, it is necessary to exclude pylorospasm, a serious surgical pathology that requires hospitalization.
Also, the mother should carefully monitor the frequency and volume of urination in the child. It is believed that until the age of three months, the child should urinate little by little, but every hour. If urinary retention occurs, the baby rarely gives out, but a lot of urine is a very alarming symptom that may indicate such a serious disease of the urinary system as ureterohydronephrosis, which, unfortunately, has been quite common lately. It can be detected already in late pregnancy with an ultrasound examination. To exclude the same pathology, ultrasound is performed at the age of one month. It is important not to lose time here, since by 3 months, in the absence of treatment, the kidney tissue dies.
Another disturbing "bell" for the mother may be the pallor and cyanosis of the nasolabial triangle in the baby, when the child turns blue when feeding, crying. All this can be caused by low hemoglobin, and in this case it is enough to prescribe treatment to a nursing mother. However, it is important not to miss cardiological pathology. Again, in the last stages of pregnancy during an ultrasound examination, gross heart defects are determined, but there may also be small anomalies that are detected only after the birth of the baby. Often, by the age of three, minor anomalies level out by themselves, but it is quite possible that intervention will be required. Therefore, if the mother noticed that the child regularly turns blue, he has shortness of breath, he is sweating (normally, babies do not sweat!), there is pallor and blueness of the nail phalanges - this may indicate a hidden heart defect. You need to draw the attention of the pediatrician to this, make a cardiogram, an ultrasound of the heart and make an appointment with a cardiologist.
In conclusion, I would like to appeal to all young mothers: be attentive to your babies, trust your intuition and do not hesitate to ask questions to the doctor, tell about all your suspicions.
A well-timed alarm is the key to timely and successful treatment, and hence the health of your baby!
Table of alarm symptoms
| Pathologies | Symptoms | Actions |
| Neurological abnormalities | Twitching of the chin. Rising of the child on tiptoe, while the baby crosses the legs, leans poorly. This may be a symptom of flaccid lower paraparesis, in the future (by a year) it may result in cerebral palsy. Hand tremor, you need to pay attention to the situations in which it occurs. The norm is if this is a reaction to a bright light, a strong sound, etc. If a baby older than a month often throws up his hands in an absolutely calm environment, this may indicate convulsions. Protrusion of tongue. In combination with tremors, it can speak of endocrinological pathology - congenital hypothyroidism. Protrusion of tongue. In combination with tremors, it can speak of endocrinological pathology - congenital hypothyroidism. | You need to contact a neurologist. In many children, neurological abnormalities are minimal and, with adequate management of the child, level out by the year. Massage, gymnastics, water therapy, drug therapy, etc. are used. Additional examinations may be required. |
| hearing loss | The child does not respond to sound stimuli (rattles, voice). | Contact an otolaryngologist. The first screening is carried out in the maternity hospital, but the ENT doctor must definitely examine the baby at 3 months. |
| Pathology of the retina | 1. The child does not follow objects, by 3 months does not react to light, to colors (the change of colors does not cause any emotions). 2. After the child was taken out of a dark room into a bright light, his pupils did not narrow, they remained wide. | Contact an oculist. Pay close attention to the child's reaction. A newborn 30 cm has the brightest vision. The baby should "catch" at a distance of 30 cm mother's face and reach for him, try to keep him in his field of vision. |
| Surgical pathology | The child often spits up a "fountain", does not gain weight well with adequate feeding. All this may indicate pylorospasm. | At a scheduled examination by a surgeon, it is necessary to focus on the existing problem. |
| Urinary pathology | It is believed that normally a child under 3 months of age should urinate a little, but every hour. If urinary retention occurs, the baby rarely gives out, but a lot of urine - this may indicate a serious disease - ureterohydronephrosis, which, in the absence of timely treatment, leads to the death of kidney tissues. | Ureterohydronephrosis is often detected late in pregnancy by ultrasound. To exclude the same pathology, ultrasound is performed at the age of one month. |
| Heart defects | Paleness and cyanosis of the nasolabial triangle. The child turns blue when feeding, crying. All this may indicate low hemoglobin, and in this case it is often enough to prescribe treatment to a nursing mother. However, if at the same time the baby has shortness of breath, he is sweating, there are pallor and blue nail phalanges - this may indicate a hidden heart disease. | It is necessary to contact a pediatrician who will prescribe an electrocardiogram and ultrasound of the heart for the child. Contact a cardiologist with the results. |
Even in an absolutely healthy child up to a year old, it is desirable to conduct at least three courses of gymnastics and massage, with the involvement of a good specialist.
The first year of life in general, in terms of its restorative capacity, is incommensurable with any other interval in a person's life.
Early discharge from the maternity hospital is highly undesirable - for 3-4 days.