Baby feeding chart uk
How Much and How Often Should I Bottle-Feed My Baby?
Before the birth of your little one, you, your doctor and midwife will have discussed whether or not you plan to breastfeed or bottle-feed your baby. If you have decided on the latter, you’ll not only need to get to grips with all of the sterilising equipment and learn how to make up a bottle-feed, you might also be asking yourself how much and how often you should be feeding your baby.
How often should I feed my newborn baby?
You might have decided that bottle-feeding from the start is best for you; you may be supplementing your breast milk with formula milk; or you might have decided to switch from breastmilk to formula milk. Regardless of you and your little one’s personal circumstances, it's generally recommended that you feed your baby whenever they seem hungry. As a guide - and it is just a guide, so don’t feel too wedded to this as it’s really important you get to know and understand your little one’s unique feeding pattern - most newborn babies who are bottle-feeding need to be fed every 2 to 3 hours. As they begin to grow, their little tummies can hold more milk, and they usually eat every 3 to 4 hours.
Although most little ones will eventually settle into a nice regular feeding pattern, you may find that your baby wants to feed more or less often. And just like adults, sometimes your baby will be thirsty and other times less so. Make sure you’re feeding your baby when your little one shows signs of hunger.
During the early stages, your baby will tend to want to feed little and often, so don’t worry if they don’t finish every feed. Just because there is formula milk left over in their bottle doesn’t mean there is anything wrong with your baby. By the same token, if your little one has a big feed, it doesn’t mean they won’t be hungry in a few hours time.
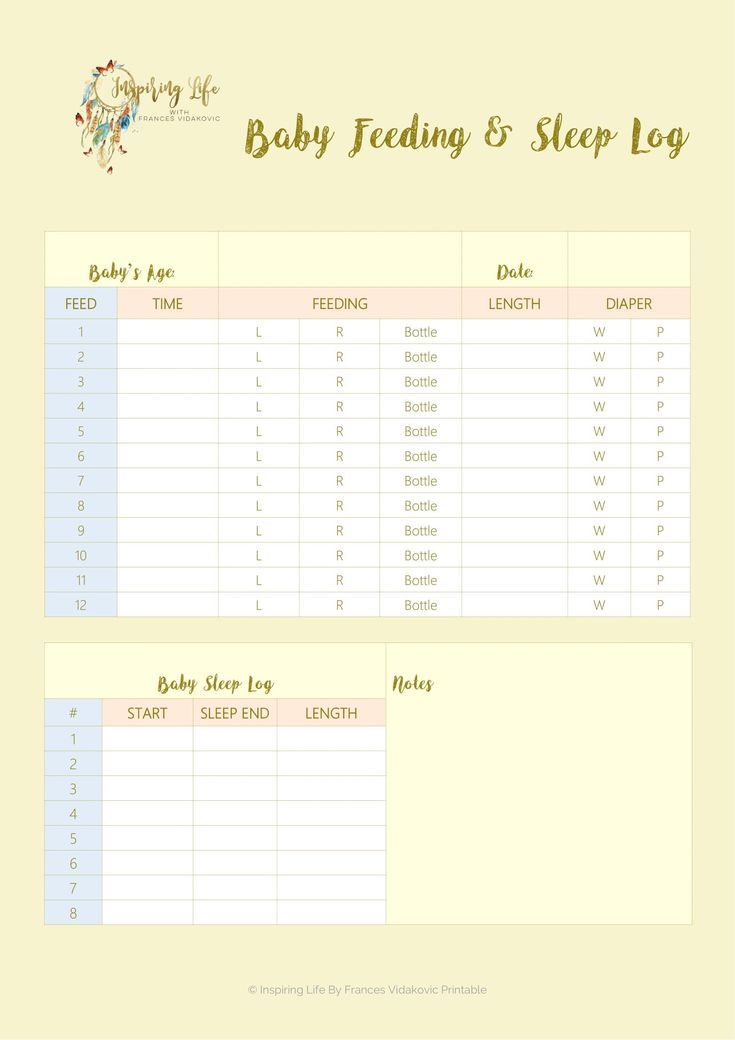
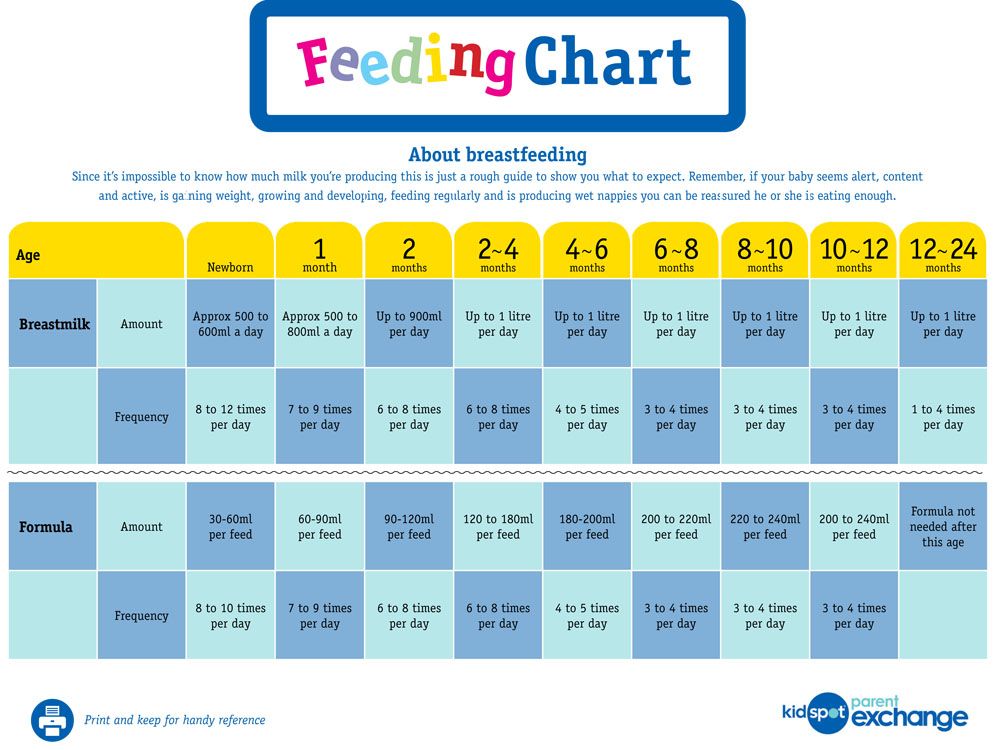
Baby milk intake chart
The table below provides a guide to how often you should be feeding your baby, dependent on their age. Of course, this is only a guide, and if your little one is premature or has a low birth weight, their feeding requirements will be different.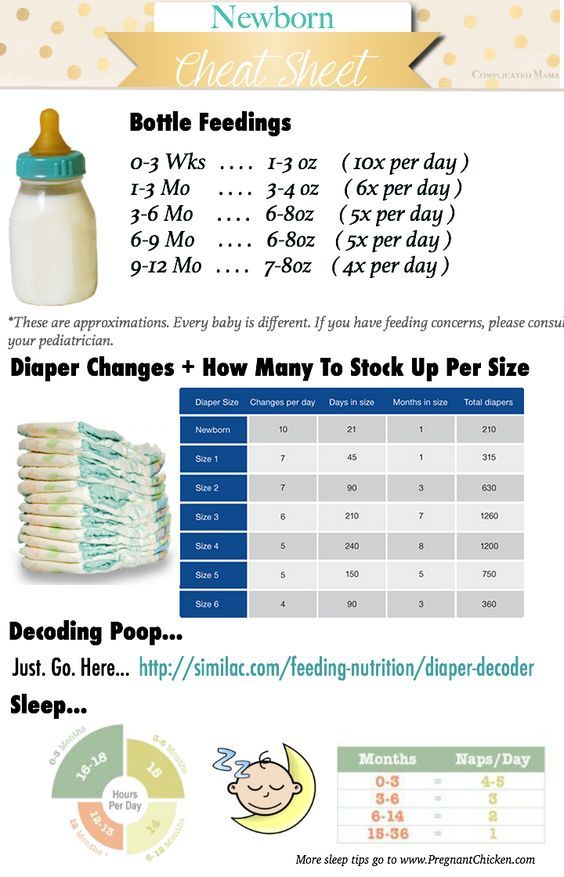 Newborn babies may take quite small amounts to start with. If you’re unsure, you can always speak to your midwife or call us to find out more.
Newborn babies may take quite small amounts to start with. If you’re unsure, you can always speak to your midwife or call us to find out more.
| Approx. age | Amount per feed - ml | Amount per feed - fluid ounces | Number of feeds per 24 hours |
| Up to 2 weeks | 90ml bottle | 3 floz | 6 |
| 2-4 weeks | 120ml bottle | 4 floz | 5 |
| 4-8 weeks | 150ml bottle | 5 floz | 5 |
| 8-12 weeks | 180ml bottle | 6 floz | 5 |
| 3-4 months | 180ml bottle | 6 floz | 5 |
| 4-5 months | 210ml bottle | 7 floz | 5 |
| 5-6 months | 210ml bottle | 7 floz | 5 |
| 7-12 months | 210ml beaker | 7 floz | 3 |
| 1 year+ | 150ml beaker | 5 floz | 2 |
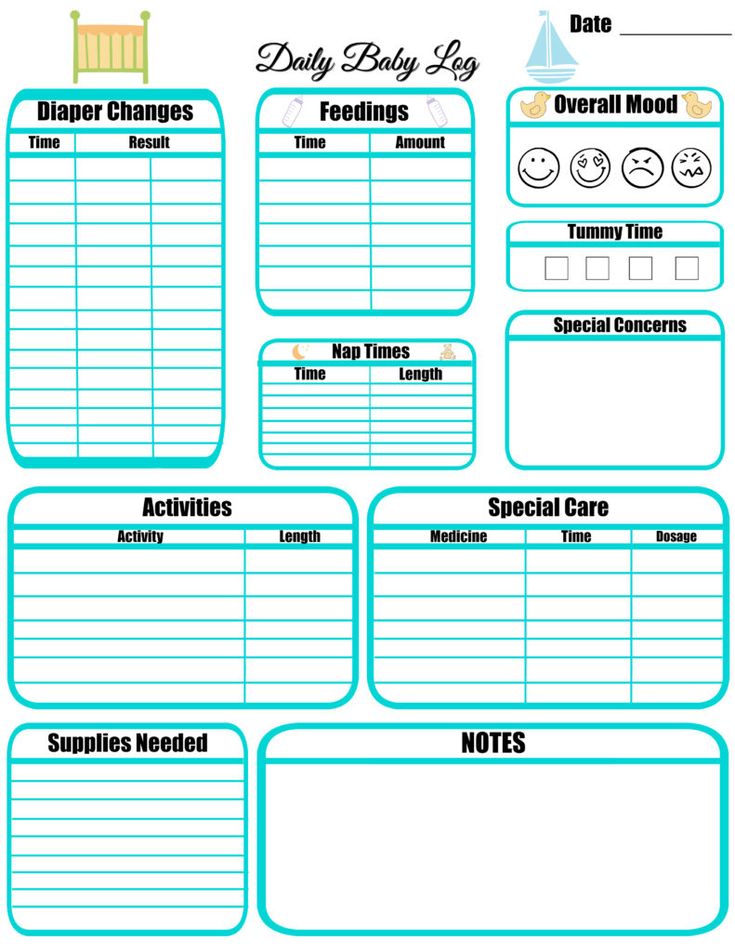
When do I start timing feeds?
Every baby is different and their appetites vary massively, so it can be normal for them to take more or fewer feeds than the guide above suggests. Your baby won't always wake at an exact time after their previous feed is finished. If you’re able to, try and time your baby’s feeds from the moment you start until the beginning of the next feed (and remember, with winding and changing, every feed may last about an hour). So if you feed your baby at 12 noon and they go back to sleep at 1pm, expect to feed them again at about 4pm. If your baby does follow a routine of feeding every three hours, you’re going to be very busy, particularly in the early months!
Your baby won't always wake at an exact time after their previous feed is finished. If you’re able to, try and time your baby’s feeds from the moment you start until the beginning of the next feed (and remember, with winding and changing, every feed may last about an hour). So if you feed your baby at 12 noon and they go back to sleep at 1pm, expect to feed them again at about 4pm. If your baby does follow a routine of feeding every three hours, you’re going to be very busy, particularly in the early months!
How do I know if my baby is getting enough milk?
If you’re worried about your baby’s appetite and whether they are getting enough milk, their nappies are quite a good (and smelly) indicator to give you a steer. You’re going to become very familiar, and potentially a little obsessed, with the contents of your baby’s nappy! (It’s really not as bad as it sounds - they are a sight to behold!)
In addition to your baby’s weight gain, the number of wet and dirty nappies will show you whether your little one is eating enough.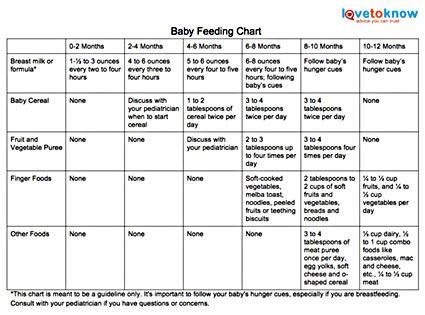 In the beginning, you'll probably be changing at least six wet and four dirty nappies every day (again, this is just a general steer). When changing your baby’s nappies, check to ensure your little one’s urine is clear or pale and it will probably feel a little weighty (all good signs!). As a newborn, your little one’s poos will probably be very dark and sticky, but after the first week they should start passing yellowish brown poos. Welcome to the joys of parenthood!
In the beginning, you'll probably be changing at least six wet and four dirty nappies every day (again, this is just a general steer). When changing your baby’s nappies, check to ensure your little one’s urine is clear or pale and it will probably feel a little weighty (all good signs!). As a newborn, your little one’s poos will probably be very dark and sticky, but after the first week they should start passing yellowish brown poos. Welcome to the joys of parenthood!
How will I know if my formula-fed baby is hungry?
It’s perfectly natural to worry about whether you’re feeding your baby enough, but once you get into a rhythm and become familiar with their feeding habits (and cute little faces during their feeds), you will get the hang of it. Here are a few common signs that your baby might be hungry:
If your little one is getting fidgety or restless, it’s probably time to give them a feed.
If they open their cute little mouth and turn their head towards you.
If they start to suck their fingers, or sometimes even their whole fist.
- If your baby starts to cry, then this could be a sign they are hungry.
How much formula milk does my weaning baby need?
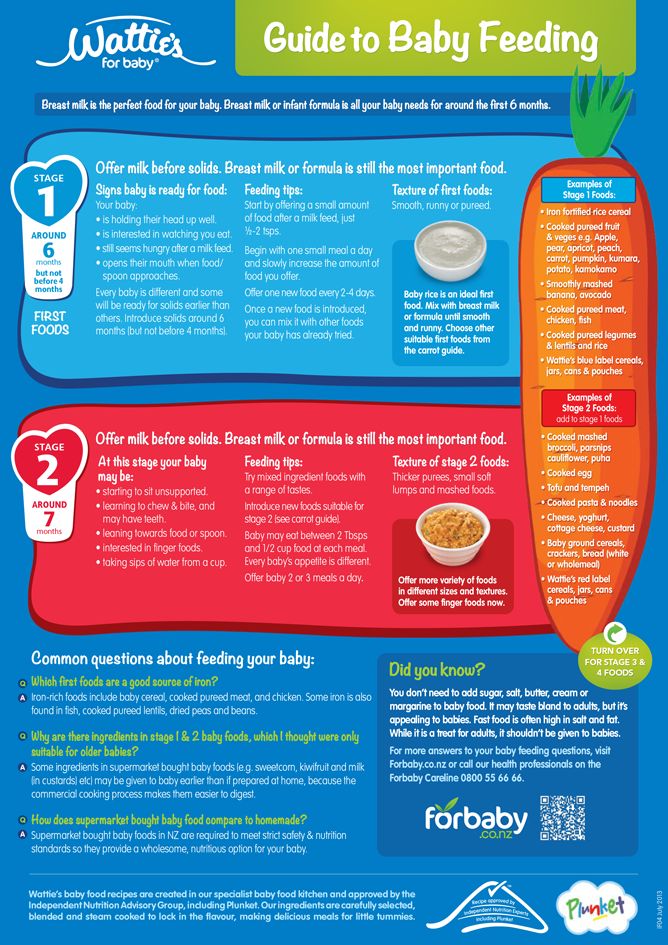
From around six months, it could be time to start introducing solids alongside your little one’s regular milk. This is called weaning, and there’s going be a lot of messy fun from here on in!
If your baby is ready to start eating a variety of purées and finger foods you still need to give your baby their regular milk. At the beginning your little one is more likely to get their solid foods all over you than in their little mouths, so it’s recommended you give them the same amount of milk feeds as before. As your little one begins to eat more solid foods, they will start to need less bottle-feeding. Babies should naturally and gradually reduce the amount of milk they want themselves, as they build on their diet of solid foods.
Join the club
Ready to stop worrying about what other people think and do what feels right to you? We’ll give you the support you need to follow your instincts and enjoy parenthood to the max:
*Weaning is recommended at around 6 months. Please speak with a healthcare professional before introducing solid foods.
Please speak with a healthcare professional before introducing solid foods.
Join the club
Ready to stop worrying about what other people think and do what feels right to you? We’ll give you the support you need to follow your instincts and enjoy parenthood to the max:
Helpful emails
Non-judgemental support
Free weaning plan*
Tips from real parents
Join now
*Weaning is recommended at around 6 months. Please speak with a healthcare professional before introducing solid foods.
More from baby
Formula Feeding Guide - Bottle Feeding
Maybe you already plan to feed your baby partly or exclusively with formula milk, or perhaps you’re still gathering the info you need to make an informed choice, or perhaps you had planned to breastfeed but now would like to switch to or supplement with formula. Either way, read on to find out more, including how much formula your baby needs, how often to feed your little one and which is the best formula milk for your newborn.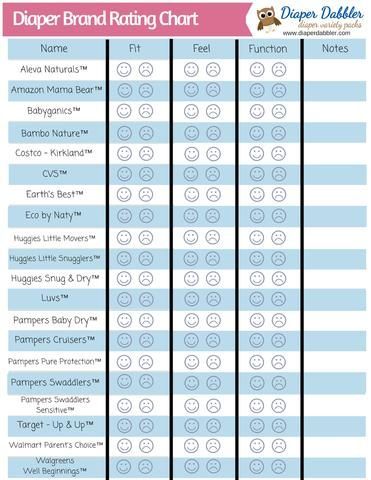
What Is Formula Milk?
Formula milk, also known as infant formula or sometimes just ‘formula’, is a substitute for breast milk that can be used either as an alternative to breastfeeding, or as a way of supplementing it.
Formula is usually (but not always) made from cow’s milk, which is specially processed to make it suitable for babies to drink. Remember: Children under 1 year old can’t digest unprocessed cow’s milk.
Formula milk contains all the nutrients your baby needs to grow and develop, but it does lack some of the additional health benefits of breast milk, such as protection from infection.
How you decide to feed your little one is a personal choice that depends on many factors unique to you. If you do plan to use formula, however, you still might want to express your first milk – known as colostrum – and feed this to your baby for the first few days before introducing the formula. Colostrum is not only packed full of nutrients; it has lots of other health benefits – such as boosting your baby’s immune system, improving digestion and helping regulate blood sugar.
Colostrum is not only packed full of nutrients; it has lots of other health benefits – such as boosting your baby’s immune system, improving digestion and helping regulate blood sugar.
Choosing the Best Formula for Your Baby
When you first walk into a shop or pharmacy that sells formula, you might find the range of boxes and packets on display a bit bewildering at first, with so many different brands and types of infant formula on offer.
Don’t let this confuse you though: Just check the label carefully and keep in mind that newborns need what is known as ‘first infant formula’ (usually marked ‘suitable for newborns’) until at least 6 months of age, unless your doctor or midwife advises otherwise.
Experts also advise sticking to this type of formula until your baby is at least around 1 year old, when you can start giving your baby (pasteurised) cow’s milk to drink.
Ready-to-Feed or Powder?
Infant formula milk comes in two forms:
Powdered.
 This is usually the most economical to buy and needs less room to store. The catch? You do have to make it up (by mixing it with water) before using it. Formula milk powder is not sterile so you need to make up each feed just before use.
This is usually the most economical to buy and needs less room to store. The catch? You do have to make it up (by mixing it with water) before using it. Formula milk powder is not sterile so you need to make up each feed just before use.
Ready-to-feed. This is formula that is already in liquid form, sold in sealed cartons or plastic bottles. It’s sterile, so it can be stored and used straight out of the bottle (although the feeding equipment must be sterilised before each use). The downside is that it can be more expensive, takes up more cupboard space and goes off quickly once you open the bottle.
Alternative Formulas
First infant formula is usually best for your baby, but in rarer cases your doctor or health visitor may suggest an alternative.
Although most of these types are available ‘off-the-shelf’ in supermarkets or pharmacies, many are only recommended for use under medical supervision. Always check with your midwife, health visitor or doctor before switching from first infant formula, especially in the first six months.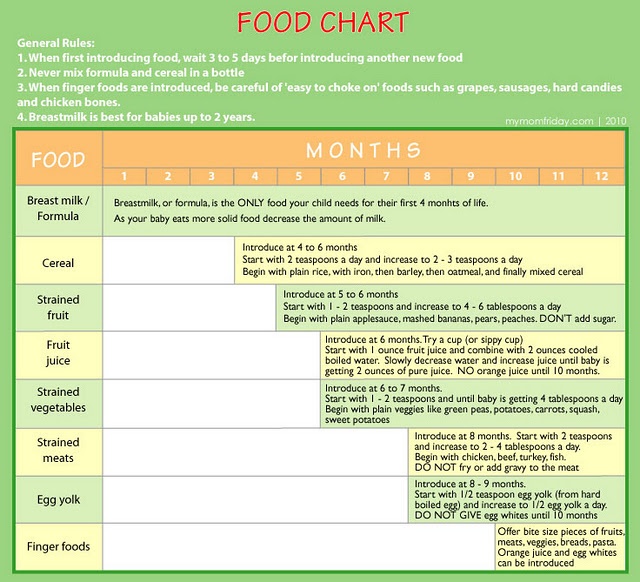
Examples of alternative formulas include:
Anti-reflux (‘staydown’) formula. This type of formula milk is thicker, to help prevent severe cases of reflux or gastro-oesophageal reflux disease (GORD) and may be recommended to you if other measures (such as frequent burping, upright feeding) don’t seem to be working. This kind of formula is only recommended for use under medical supervision.
Lactose-free formula. Some babies have difficulty digesting lactose (the natural sugar found in milk). Lactose intolerance is not an allergy, but it may cause symptoms like colicky crying, diarrhoea, tummy ache and wind. Lactose-free formula could help; but should only be used under medical supervision Tell your health visitor or doctor if you suspect your baby has a lactose intolerance.
Hypoallergenic formula. If your baby is diagnosed with an allergy to cow’s milk, your doctor can prescribe a special infant formula with fully hydrolysed (broken down) proteins.
Soya formula. Made from soya beans, this is sometimes recommended as an alternative for babies with a cow’s milk allergy. However, there are concerns about whether the phytoestrogens (similar to the hormone oestrogen) in soya beans could affect babies’ development. Only use soya formula if your doctor or health visitor has prescribed or recommended it.
Goat’s milk formula. This is produced to the same nutritional standards as cow’s milk formula, but from goat’s milk. It can’t be used as an alternative for babies with a cow’s milk allergy though, because the proteins found in goat’s milk are very similar to cow’s milk protein.
Comfort formula. Comfort formula contains partially broken-down (hydrolysed) proteins. Its claim is that this makes it easier to digest – alleviating problems like colic or constipation – although there is no medical evidence to back up this claim so it might be best to talk to your doctor or midwife first if you are concerned about your little one’s digestion and you’re considering this type of formula.
Formulas for babies older than 6 months. These include ‘follow on’ formula, ‘good night milk’ and ‘growing up’ or ‘toddler milk’ (for babies older than 1 year). Experts usually advise sticking to first infant formula until your little one is fully weaned, so it’s best to ask your health visitor or doctor for personalised advice before trying out any new type of formula marketed for older babies or toddlers.
How Much Formula Does Your Baby Need?
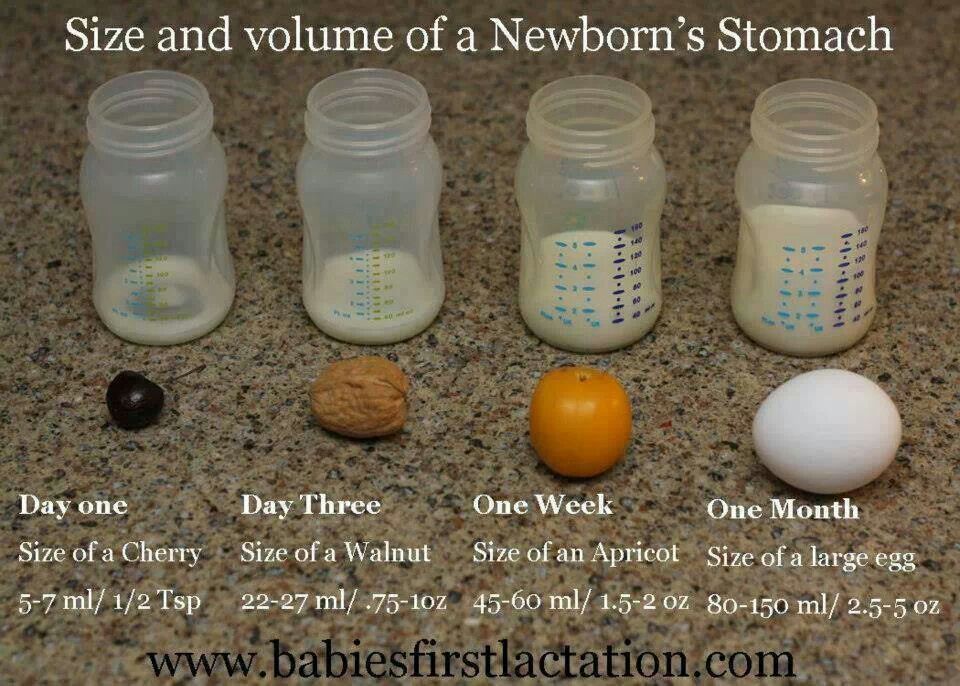
Your newborn baby only needs small amounts of formula in the first few days – after all, his or her tummy is still very small, but it’s growing all the time.
Just to give you an idea how small your newborn’s stomach is, and how fast it grows:
On day one it’s about the size of a cherry and holds around 5-7 millilitres
On day three it’s the size of a walnut, with room for 22-27 millilitres of formula or breastmilk
After one week it’s grown to the size of an apricot and can hold about 45-60 millilitres at a time
After one month your baby’s stomach is about the size of a large egg, with a capacity of 80-150 millilitres.

From after the first week until around 6 months old (when your baby starts weaning), your little one may need around 150 to 200 millilitres of formula milk a day for every kilogram of body weight.
So, for example, a 1-month-old baby weighing around 4 kilograms might need between around 600 and 800 millilitres of formula a day, spread over several feeds. Here are some more examples of how much formula your baby may need per day based on different bodyweights:
| Approximate Quantities of Formula Depending on Body Weight | |||||
|---|---|---|---|---|---|
| Baby’s weight | 3 kg | 5 kg | 7 kg | 9 kg | 10 kg |
| Daily amount of formula | 450-600 ml | 750-1,000 ml | 1,050-1,400 ml | 1,350-1,800 ml | 1,500-2,000 ml |
All babies are different, and so are their appetites! In practice, though, once your child settles into a feeding pattern and you get to know his or her feeding cues, you’ll probably find it natural to increase the quantity of formula gradually in response to demand.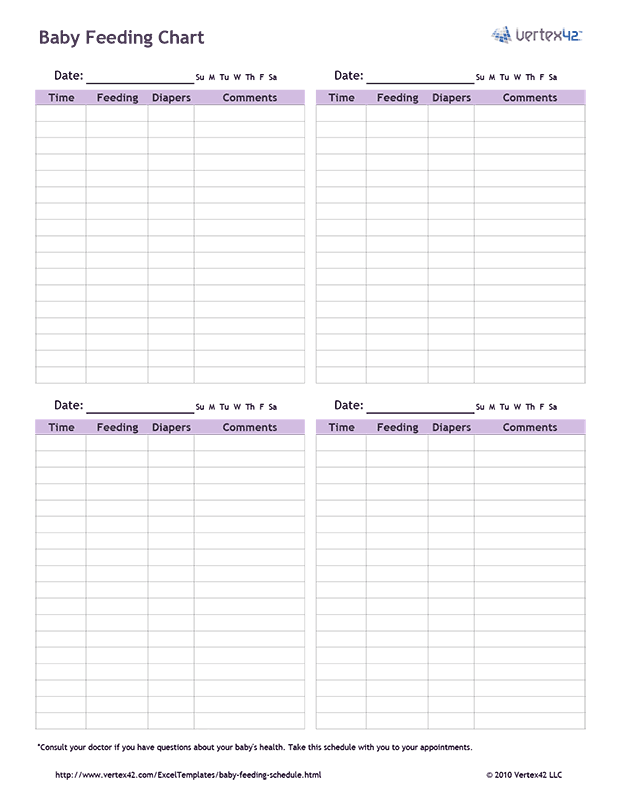
How to Tell When Your Baby Is Full
Breastfed babies usually just stop feeding when they’re full, but milk comes out of the feeding bottle’s teat more easily than out of a breast. When the formula touches the back of your baby’s throat, it triggers the swallowing reflex.
This means it is possible to overfeed your baby with a bottle, so it’s important to recognise when he or she is full. A good way of doing do this is called ‘pacing’:
Let your baby pause every few sucks – gently withdraw the bottle and see if he or she wants to stop
This could also be a good time to burp your baby, especially if he or she spits up formula, or seems windy or uncomfortable
Only start feeding again if your baby draws the teat back into his or her mouth
Don’t push the teat into your baby’s mouth or try feeding if your baby turns his or her head away.
related baby tool
Keep an eye on your baby’s height, weight, and head circumference to average growth with our simple tool.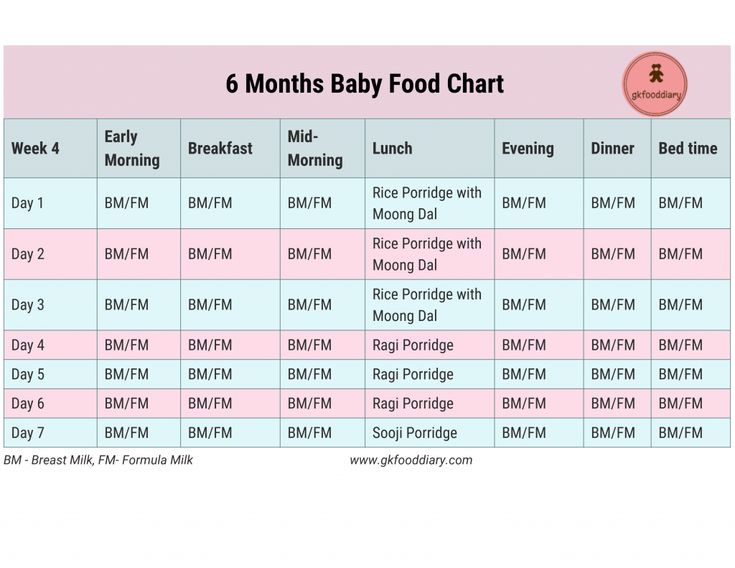
Fill out your baby's details*:
What is your child*
Boy Girl
This is a mandatory field.
Age (months)
This is a mandatory field.
Weight (kg.)
This is a mandatory field.
Height (cm.)
This is a mandatory field.
Head circumference (cm.)
This is a mandatory field.
*Input details of your baby’s last measurements **Source: World Health Organization
How Often Should Your Newborn Feed on Formula?
Feed your baby whenever he or she shows signs of being hungry. These signs are known as ‘feeding cues’, and they can include:
Moving the head from side to side (rooting)
Lifting or bobbing the head
Sucking on a finger, fist or blanket (or anything else within reach)
Drooling
Licking or smacking the lips
Crying (this is a late sign – it’s often easier to feed your baby if you can spot the earlier feeding cues in time).
How to Be Sure Your Baby Is Getting Enough Formula
Rather than strictly following a chart to decide how many ounces or millilitres a baby should eat at a given age or weight, experts advise feeding ‘on demand’ in response to the feeding cues listed above.
As long as your little one is gaining weight normally and producing enough wet nappies, you can be pretty certain he or she is getting enough formula.
From the first few days after being born it’s normal to see around six heavy nappies, soaked with pale or clear urine, every day.
Your baby will usually be weighed a few times in the first 10 days after birth, and then once a month after that – at monthly health and development reviews – until the age of 6 months.
During the health and development reviews your health visitor and/or doctor will use growth charts to keep track of your baby’s growth and weight gain.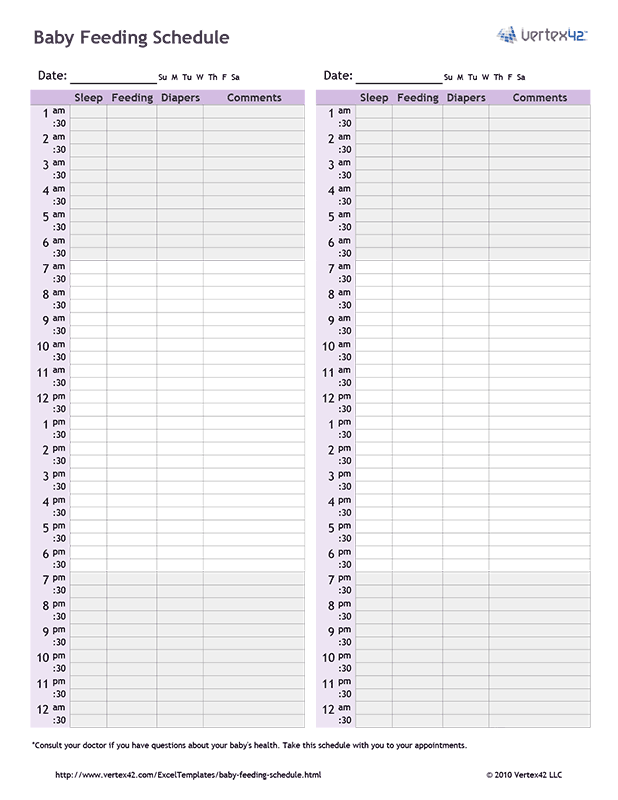
These visits are also a great opportunity for you to ask questions or discuss any concerns you might have. But if you’re ever concerned about whether your baby is eating enough, you can always turn to your midwife or doctor between the scheduled visits.
How to Make Up a Feed
If you’re using powdered milk, follow the seven steps below to make up a feed. Always read the manufacturer’s instructions carefully and ask your midwife or health visitor if there’s anything you’re not sure about.
Always make the formula just before you need to use it and don’t reuse any formula milk that’s been left over from a previous feed.
Make sure the surfaces you’re using are cleaned and disinfected, and the feeding bottle and accessories are also cleaned and sterilised.
Boil at least 1 litre of fresh tap (not bottled) water in a kettle, then leave it to cool for no more than 30 minutes (so it stays above 70 degrees Celsius – this is hot enough to kill any germs that might still be in the bottle).
Stand the bottle on the disinfected surface, and – following the manufacturer’s instructions – pour the correct amount of hot water from the kettle into the bottle. Be careful to check the water level.
Again, following the manufacturer’s instructions carefully, use the scoop supplied with the formula to add the powder to the water in the bottle. Don’t forget to level off each scoop of powder with a clean, dry knife or the provided leveller.
Insert the teat into its retaining ring (following the instructions supplied with the feeding bottle) and screw it on.
Put the cap over the teat and shake the bottle until all the powder is dissolved.
Cool the bottle under cold running water (with the cap on) or leaving it to stand in a bowl of cold water.
Test the temperature of the formula by dripping some onto the inside of your wrist – it should be warm or cool, but not hot.
Storing and Transporting Formula Milk
Powdered formula milk isn’t sterile, so only make up a feed just before using it and throw away any formula that’s left over after a feed.
If you need to feed your baby while you’re out and about, it helps to take
the amount of formula powder you need for a feed, measured out into a small, clean and dry, airtight container
a clean vacuum flask containing just-boiled tap water (the flask will keep the water at over 70 degree Celsius for several hours)
an empty, sterilised feeding bottle with the teat, retaining ring and cap.
When you need to make up a feed, follow the steps above. Don’t forget to cool the formula and check the temperature on the inside of your wrist before feeding it to your baby.
Transporting and Storing a Made-Up Feed
Sometimes, transporting a made-up feed might be the only option (for example, if you need to take a feed to nursery school). In this case, make up the formula at home, cool it in cold water and then cool it further in the back of the fridge for at least an hour before transporting it.
In this case, make up the formula at home, cool it in cold water and then cool it further in the back of the fridge for at least an hour before transporting it.
Made-up formula stored in a fridge should be used as soon as possible, but within a maximum of 24 hours.
Move the made-up formula from the fridge to a cool bag with ice packs just before leaving the house and use it within four hours (or two hours if you don’t have ice packs).
A Quick Guide to Bottle-Feeding Your Baby
Feeding isn’t just about nutrition – it’s a chance for social interaction and bonding. Sit comfortably and make eye contact. Enjoy these moments of closeness with your baby.
Just because you’re bottle-feeding, doesn’t mean you and your baby have to miss out on plenty of skin-to-skin contact. Holding your little one close against your skin is not only good for bonding, it also has a calming effect and helps regulate your baby’s breathing and body temperature.
Here’s a brief guide to bottle-feeding your baby:
Hold your baby upright in a comfortable, neutral position. Your infant shouldn’t need to tilt or turn the head to reach the bottle
Hold the bottle almost horizontal to the ground, tilted just enough to fill the teat with the formula
Brush your baby’s lips with the teat, and your child will usually open his or her mouth wide and put out his or her tongue
Help your baby to draw the teat into his or her mouth
Pace the feed by pausing occasionally to see if your baby is still hungry
Check for air bubbles rising up in the formula. If no bubbles appear, a vacuum may have formed in the teat. This can stop the formula flowing. Break the vacuum by gently moving the teat sideways in your baby’s mouth
If your infant seems restless or uncomfortable, have a ‘burping break’ before seeing if he or she wants any more more milk
Never feed your baby lying down, to avoid the risk of choking.
 Babies should never be left unattended while feeding or allowed to fall asleep with a bottle in their mouth.
Babies should never be left unattended while feeding or allowed to fall asleep with a bottle in their mouth.
FREQUENTLY ASKED QUESTIONS
‘First infant formula’ is the only type of formula milk suitable for a newborn baby, unless your doctor or midwife advises you otherwise. Experts advise sticking with this kind of formula until your infant is fully weaned.
Formula milk is usually made of cow’s milk (or sometimes goat’s milk) that has been specially processed to make it suitable for young babies. Other formulas (e.g. soya-based formula) should only be used on the advice of your doctor or health visitor.
The Bottom Line
We hope this quick guide takes some of the mystery out of formula milk and bottle feeding. And remember, the secret ingredient isn’t in the bottle: The love and care you put into feeding and caring for your baby is what makes those feeding sessions so special for you and your little one.
How we wrote this article
The information in this article is based on the expert advice found in trusted medical and government sources, such as the National Health Service (NHS). You can find a full list of sources used for this article below. The content on this page should not replace professional medical advice. Always consult medical professionals for full diagnosis and treatment.
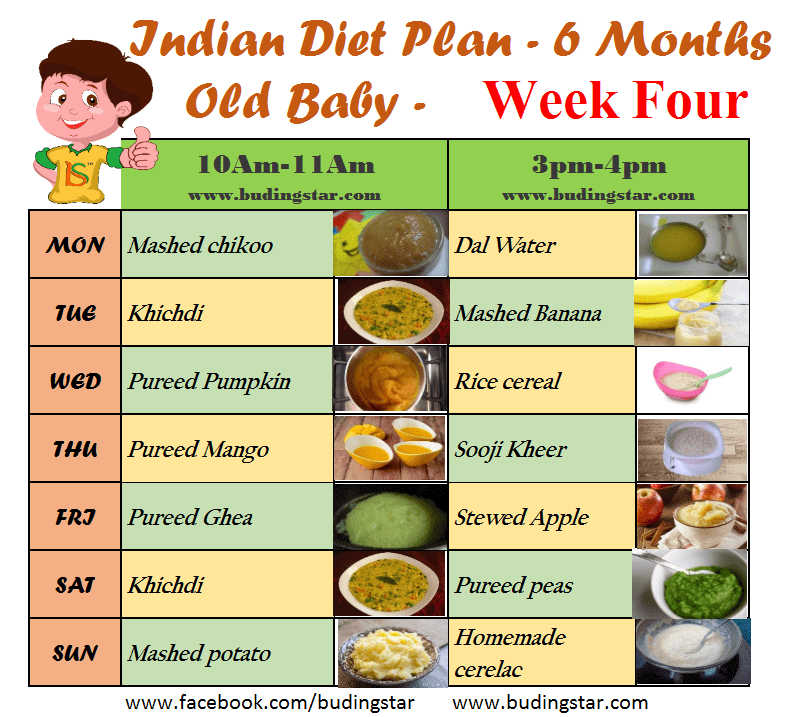
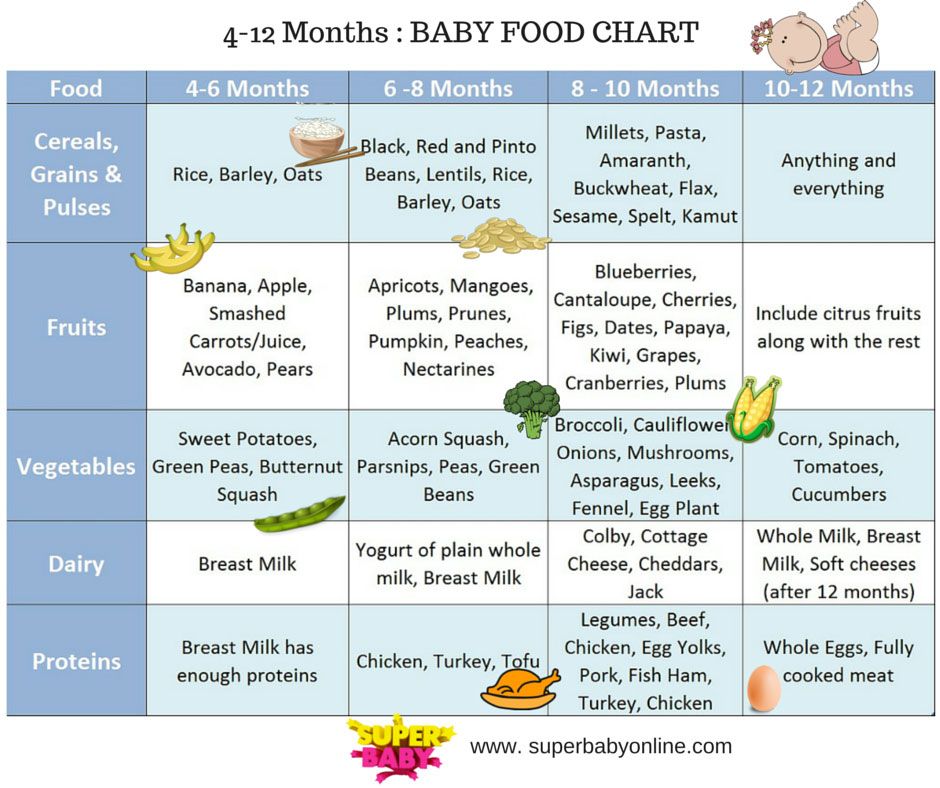
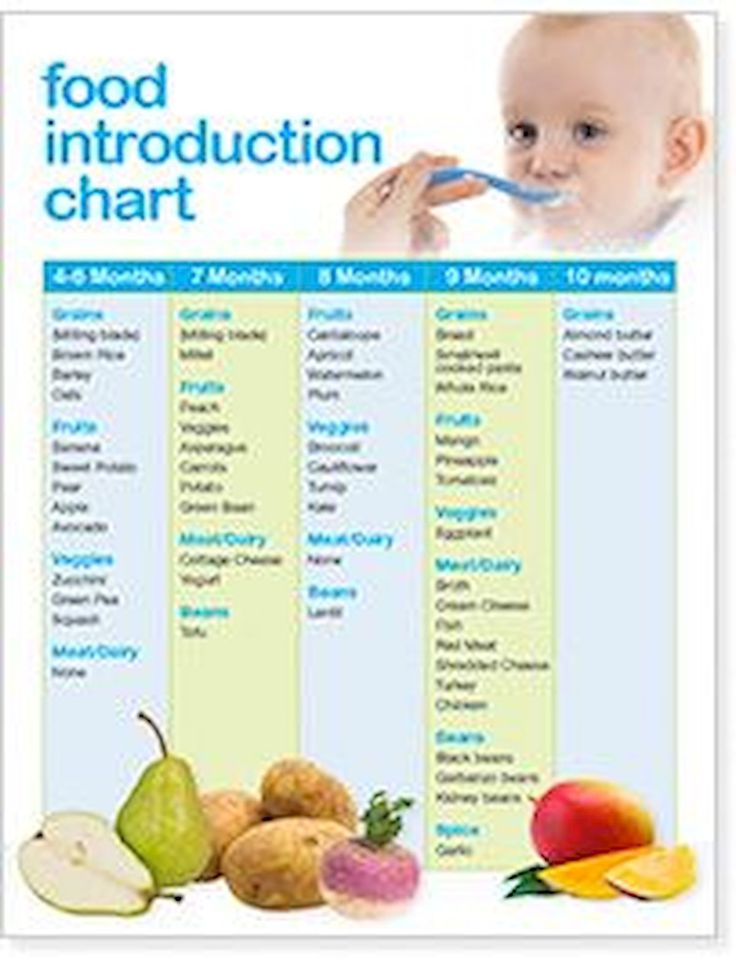
How complementary foods are introduced in other countries
Germany. Complementary foods begin at the age of 5-6 months, the first product is carrot mousse. A week later, it is replaced with mashed potatoes and carrots with the addition of vegetable oil. A week later, meat and fruit juice are added to this puree. It turns out that seven-month-old children receive mashed potatoes from meat, vegetables, juice and vegetable oil. Approximately two weeks after meeting with meat, the baby receives his first porridge. Interestingly, it is immediately recommended to cook porridge with 3. 5% whole milk. Fruit juice is added to the finished porridge. A month after the introduction of cereals (approximately about 8 months), fruit and grain purees appear in the child's diet, they are made from grains, fruits and vegetable oil. But cottage cheese, yogurt and other fermented milk products are put aside for the age of over a year: it is believed that they are harmful to children under 12 months old.
5% whole milk. Fruit juice is added to the finished porridge. A month after the introduction of cereals (approximately about 8 months), fruit and grain purees appear in the child's diet, they are made from grains, fruits and vegetable oil. But cottage cheese, yogurt and other fermented milk products are put aside for the age of over a year: it is believed that they are harmful to children under 12 months old.
Choose foods for the first feeding
Austria. The first complementary foods are introduced at the age of 5-7 months, babies receive vegetable puree with rapeseed oil. A month later, children are introduced to cereals, a month later - to fruit puree. A month later, fish, meat and even grated nuts appear in the diet of young Austrians. But about milk and dairy products, the Austrians agree with their neighbors, and babies get them strictly after a year.
France. Young Frenchmen receive vegetable purees with the addition of vegetable or butter as the first food. This happens in about six months. After a couple of weeks, the baby is offered fruit puree. At 8 months, the baby is introduced to meat, fish and boiled mushrooms, from 10 months the baby eats cheese. The French do not like porridge, children get it after a year.
This happens in about six months. After a couple of weeks, the baby is offered fruit puree. At 8 months, the baby is introduced to meat, fish and boiled mushrooms, from 10 months the baby eats cheese. The French do not like porridge, children get it after a year.
UK. At about 4.5-5 months, children are offered the first complementary foods - a bottle of liquid rice porridge on the water. This is followed by vegetables, fruits, porridge and meat. Dairy products are introduced after a year.
Argentina. Complementary foods traditionally start with yogurt and are given to babies between 5 and 6 months of age. This is followed by fruits, vegetables, cereals and meat.
Canada. The first complementary food is porridge, age 4-6 months. A month later, vegetable or fruit puree and a little oil are added to the porridge. At 8 months, meat and fish are introduced.
Cuba. The hot tropics, where there is an abundance of fruits all year round, influenced the order of introduction of complementary foods. Start at 5-6 months with fruit puree. Moreover, orange puree is among the first recommended products. Following the fruit puree, meat is introduced into the child's diet (at 6-7 months), and only then cereals.
Start at 5-6 months with fruit puree. Moreover, orange puree is among the first recommended products. Following the fruit puree, meat is introduced into the child's diet (at 6-7 months), and only then cereals.
Spain. At 5 months, babies are introduced to corn and rice porridge, then fruit puree is mixed into the porridge, and only then vegetables and meat are introduced.
Iran. From 4 months, the baby is given a few grains of rice and a couple of sips of lamb broth every day. At 6 months, the first real complementary foods appear - rice porridge with almonds. There are no fruit and vegetable purees, children immediately get pieces of fruit and try to chew them as best they can. Children are given meat from 8 months, including fatty lamb.
Indonesia. Rice porridge from 3 months, porridge with fruit additives from 4 months. Vegetables from 5 months. Meat and dairy products - after three years.
Sweden. Complementary foods start with cereals at 5-6 months, followed by vegetables, fruits, and from 8 months and meat.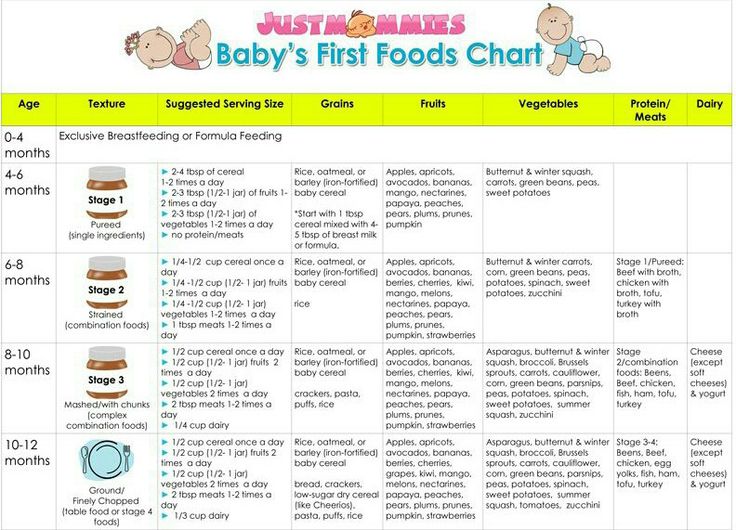 Eggs and dairy products are introduced into the child's diet after a year.
Eggs and dairy products are introduced into the child's diet after a year.
Scheme of introducing complementary foods according to the new rules: what has changed - Parents.ru
About nutrition
When the baby is five or six months old, it's time to introduce him to "adult" food. And then the difficulties begin: the pediatrician says one thing, the grandmothers say another (they also say, they say, they raised you, and everything is in order).
Until now, Russia has followed the recommendations of the World Health Organization. And last year, a document was adopted that regulates in detail all issues related to the introduction of complementary foods - this is a new version of the "National Program for Optimizing Feeding Children in the First Year of Life in the Russian Federation." She has made major changes to the scheme we are accustomed to.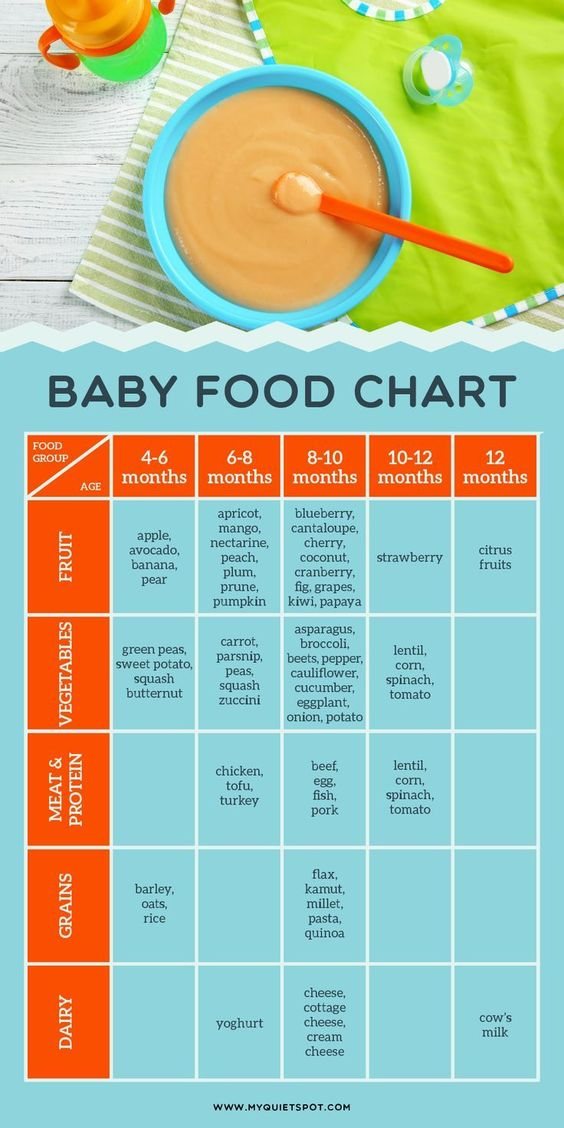
Four major innovations
- Starting complementary foods, regardless of the type of food, is recommended from 5 months, and if there are problems with weight, even earlier.
- The introduction of meat is recommended at 6 months.
- Fruit puree is recommended in case of constipation at any time. In the absence of constipation, fruit puree is introduced after meat.
- Portion size of mashed potatoes and cereals for a child of 5-7 months - 150 gr.
In addition, there are a few more important details - we will analyze them.
At what age to start complementary foods
Over the past decades, the rules for the introduction of complementary foods have changed dramatically. It is not necessary to give a baby apple juice at three months, and borscht at six months. Offering a chicken bone to scratch her gums is also not worth it.
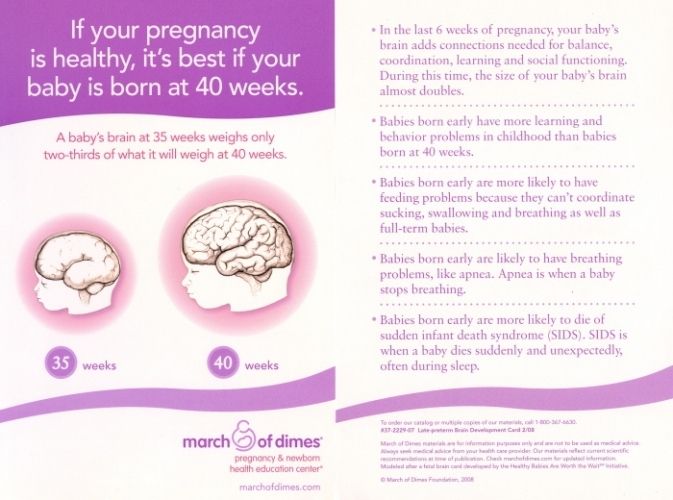
As a reminder, according to WHO recommendations, complementary feeding of breastfed babies should be started at six months. Until this moment, it is not necessary to supplement the child even with ordinary water. With artificial feeding, complementary foods are usually started a month earlier. According to an individual schedule, regular food will be introduced to babies who do not grow well on their mother's milk, do not gain weight, or they have some kind of allergy.
Until this moment, it is not necessary to supplement the child even with ordinary water. With artificial feeding, complementary foods are usually started a month earlier. According to an individual schedule, regular food will be introduced to babies who do not grow well on their mother's milk, do not gain weight, or they have some kind of allergy.
At the same time, domestic scientists, based on the opinion of ESPGHAN (European Society of Pediatric Gastroenterology, Hepatology and Nutrition), believe that exclusive breastfeeding does not always provide a sufficient level of micronutrients, especially iron, in the baby's body.
Therefore, in their opinion, the first complementary foods should be started at five months, and already at six months meat should be added to the diet as a source of this very iron.
There are additional recommendations. For example, the UK National Health Service highlights four things that indicate that a baby is ready for food other than formula and breast milk.
- He is already sitting and holding his head well.
- He can swallow food - the spoon ejection reflex has faded.
- His movements are coordinated: he can take a spoon and put it in his mouth.
- First teeth erupted.
What foods to introduce complementary foods with
The classical scheme, relatively speaking, consists of three steps: vegetables-porridge-meat.
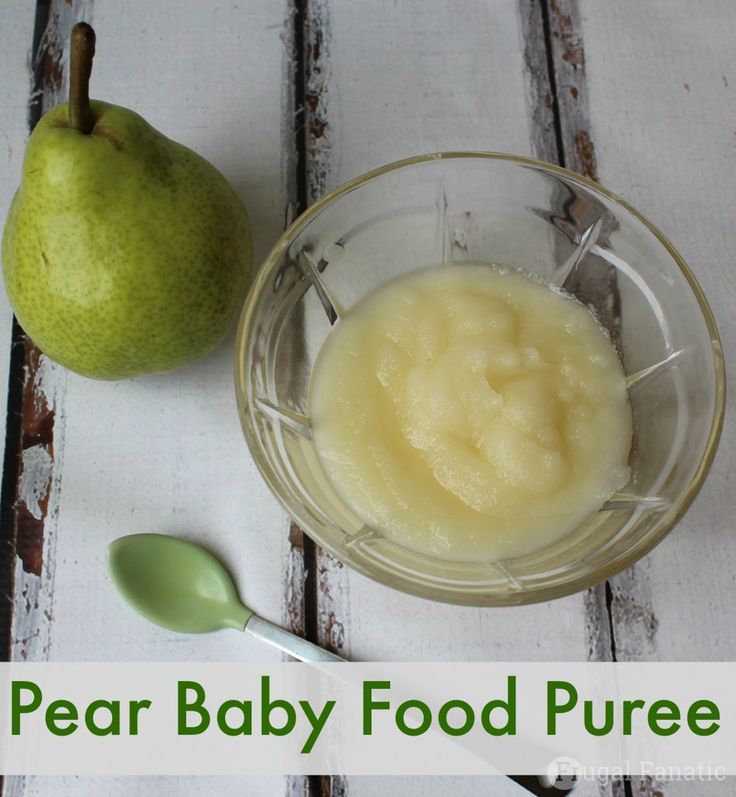
As a rule, the first vegetables of the child are white and green vegetables: zucchini, cauliflower, broccoli. Porridge is preferably buckwheat, corn or rice. Of course, on the water. Meat - turkey, beef, rabbit. The first baby fruits will be banana, apple, peach and pear.
Please note that if the child is not gaining weight well, then most likely the pediatrician will swap the first two steps, and complementary foods will start with cereals. He will tell you when it is really better to give the child meat. Any general rules can only be adjusted by a doctor who has been observing him since birth.
Cook your own or buy store-bought jars, it's up to you. Each of the options has its pros and cons. We only note that both the WHO and our doctors prefer industrial products.
“Modern industrial complementary foods are enriched with biologically active components, such as vitamins, minerals, pre- and probiotics, LCPUFA (omega 3), etc., which gives them functional properties,” the National Program says.
At 7 months, the new rules allow the addition of yolk, at 8 - fish puree, as well as cottage cheese and sour-milk drinks.
The attitude towards whole cow's milk has not changed - it is still not allowed to be used for baby food. And now, domestic experts have expressed an opinion about complementary foods with vegetarianism. In their opinion, "children on a vegan diet are at high risk for developing deficient conditions and require increased attention." And if parents are not going to give up their beliefs, then children need to be additionally given the necessary vitamins and minerals, especially B12.
9 complementary feeding rules
- One week, one new product. This is important for the adaptation of the body and in order to track signs of allergies if they appear. If you see that everything is in order, then after about a month and a half, new products can be introduced every three days.
- The first sample is literally three grams. It's less than half a teaspoon. And, of course, breastfeed or formula feed.
- It is desirable that complementary foods be in the afternoon feeding.
- The first real food should be liquid. Vegetable puree can first be slightly diluted with water or breast milk. 7-8 months is the time to introduce the baby to partially solid foods, and from 8-9 you can offer to chew small soft pieces, such as boiled carrots or potatoes. Ideally, by the age of one, the child can already safely eat solid food from the common table.
- Every day we slightly increase the portion. When we bring it to the desired volume (150 grams), we no longer give the breast or mixture in this feeding.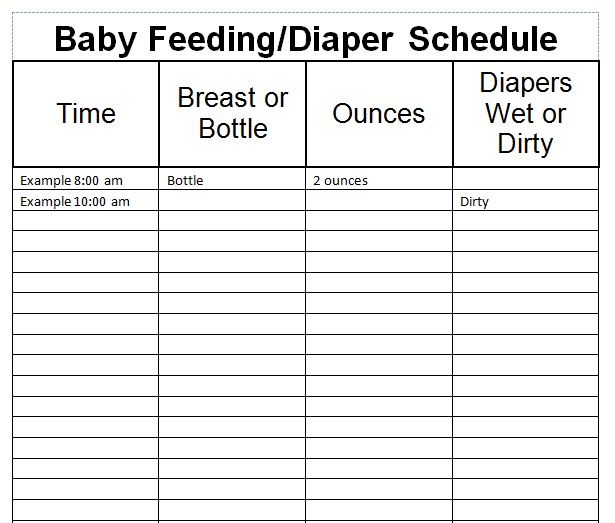 At this point, you can add half a teaspoon of vegetable oil to the puree.
At this point, you can add half a teaspoon of vegetable oil to the puree.
- When introducing new products, we always offer them first. Then we feed the already familiar ones.
- With the introduction of complementary foods, you can start offering water to your baby. And even immediately from the cup, bypassing the stage of the drinker. Juices during this period, doctors do not recommend categorically. Firstly, they have little nutritional value, and secondly, if you drink juice between meals, this increases the risk of developing caries. They can also cause weight gain if consumed in excess.
- If the child refuses complementary foods on principle, do not insist. This is common, sometimes it takes 10-15 attempts to "accept" a new product. Offer the product again after a couple of days.
- Do not introduce new foods when the baby is sick or recovering, during the period when an allergy is manifested, in preparation for or after vaccination. And how to improve digestion in case of dysbacteriosis, read the link.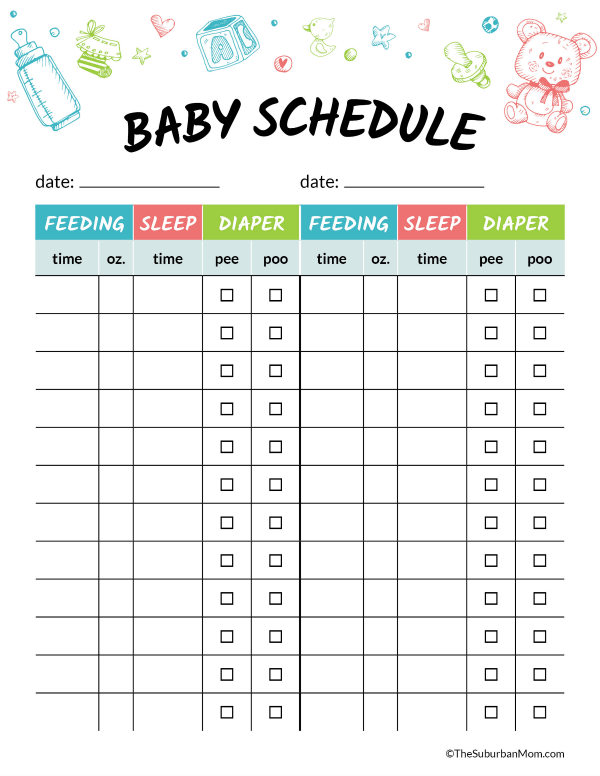
In what order to introduce foods into the diet
(for a breastfed child without any allergic manifestations)
4-5 months (vegetables for lunch, porridge for breakfast)
1 week - zucchini
2nd week - cauliflower
3rd week - broccoli
4th week - a mixture of three already familiar vegetables + vegetable oil + teaspoon of butter
8 weeks - pumpkin, fruit puree - apple, pear, prunes
6 months (new product can be introduced every three days)
Meat - rabbit, turkey, veal in the form of puree
Baby biscuits
This was the base. Now the baby has a full breakfast and lunch, and you can introduce other foods in approximately that order, gradually replacing evening feeding with dinner.
7 months
egg yolk
8-9 months
cottage cheese, kefir, potatoes, carrots, beets, white bread, fish puree (90 2 times a week instead of meat), juice
3
3
berry puree
Another approach
In the UK, by the way, there is a completely different attitude towards the first complementary foods.