Baby feeding guidelines australia
Bottle feeding - nutrition and safety
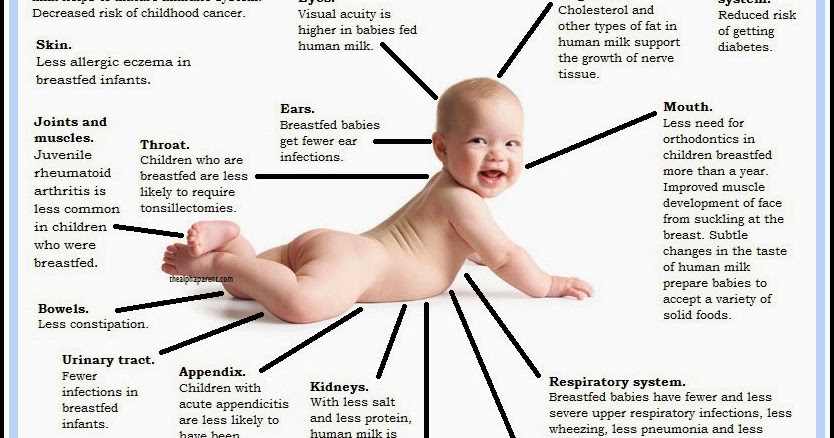
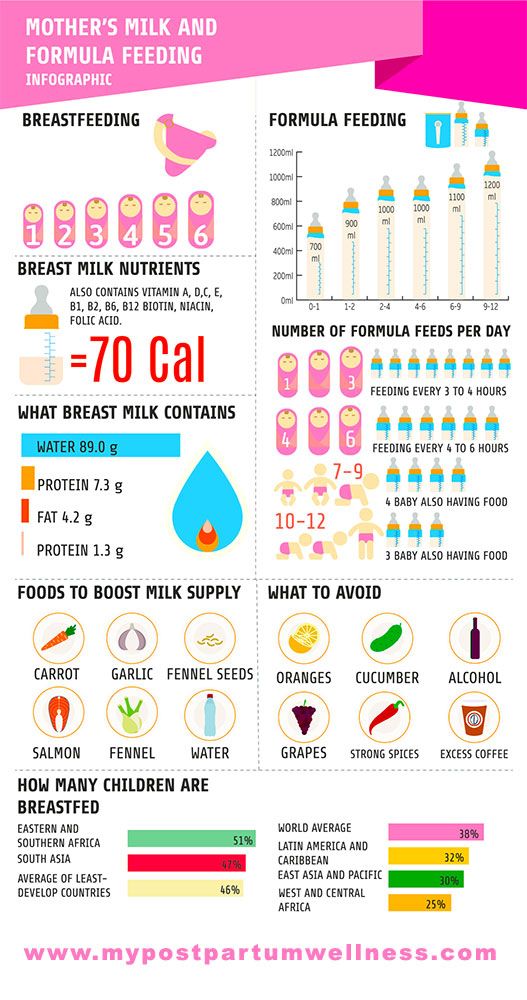
Breastmilk or a suitable infant formula is recommended as the main source of nutrition for all babies less than 12 months of age. Breastmilk is the feeding option of choice, but commercial infant formula is the only suitable alternative when breastmilk is not available.
Babies under 12 months of age should not be fed:
- regular, low-fat or skim cow’s milk
- evaporated or powdered milk, sweetened condensed milk
- cereal and legume-based beverages (such as rice, oat or soy)
- nut and seed-based beverages (such as almond or pumpkin seed)
- any do-it-yourself preparations using homemade recipes.
Commercial infant formulas have been developed to contain similar nutrition to breastmilk. They provide all the nutrition your baby needs until you introduce solids at around 6 months. All formulas sold in Australia conform to the Australia New Zealand Food Standard Code (Standard 2. 9.1 – Infant Formula Products). There is little difference between differently priced brands.
The composition of infant formula continues to change as research provides a greater understanding of the role of the unique ingredients contained in breastmilk. A variety of new ingredients have been added to infant formulas in recent years.
Starter or first formula
There is a variety of starter formulas based on cow’s milk protein (whey or casein). Formula based on soy or goat's milk is also available. These formulas are suitable for babies from birth to 12 months.
Read the label carefully because:
- Formulas developed for toddlers as well as pregnant women can look very similar, so check the label carefully to ensure your baby gets a formula that is safe and appropriate for their age.
- The label may list a number of additions such as LCPUFAs (long chain polyunsaturated fatty acids or omega-3 fatty acids), probiotics or prebiotics. These ingredients are added because they are found naturally in breastmilk.
Caution on changing formula
If your child sleeps or feeds badly, or is unsettled or ‘colicky’, you may think you need to change the formula you are using. There is little evidence that this is helpful for the majority of babies. Seek the advice of your maternal and child health nurse or doctor before switching formulas.
Soy formula
Infant soy formula is suitable for babies with a medical reason to use them, such as an allergy to cow’s milk. This formula must not be confused with regular soy milk, which does not provide suitable nutrition for babies.
‘Follow on’ formula
‘Follow on’ formula is suitable for babies 6 months of age and over. It is your choice whether you use one. ‘Follow on’ formula is available based on cow’s milk, soy or goat’s milk. They are made for babies over 6 months of age and contain higher protein and mineral content than starter formula.
Specialised infant formula
Infant formula can be modified in a variety of ways, including changes to the fat, carbohydrate or protein content. Specialised infant formula is sometimes necessary for babies with certain medical conditions and may be prescribed by paediatricians through the Pharmaceutical Benefits Scheme (PBS).
Specialised infant formula is sometimes necessary for babies with certain medical conditions and may be prescribed by paediatricians through the Pharmaceutical Benefits Scheme (PBS).
Reasons for using one of these formulas might include:
- severe allergy or intolerance
- fat or carbohydrate malabsorption
- severe digestive disorders.
Some examples of specialised infant formula and when they are used include:
- Low lactose – is used for lactose (milk sugar) intolerance.
- Modified protein content – in some formula, the cow’s milk protein is broken down into smaller units. In other formula, the whole protein is replaced by amino acids, the individual building blocks of protein. These preparations are used for severe allergy, malabsorption and digestive disorders or metabolic conditions.
- Modified fat content – this includes formula with a high concentration of triglycerides and lower levels of fatty acids, which may be used for babies with liver or gastrointestinal conditions.
- Thickened formula – sometimes recommended for babies who frequently regurgitate (vomit or cough up) large amounts after feeding, although a thickened formula may not solve this problem. Only use under medical advice.
- Premature infant formula– designed for preterm (born premature) babies while they are preterm. Premature babies need a formula with additional energy and mineral content. This is not suitable for full-term babies or for preterm babies who are now full term, unless under medical advice.
Seek medical advice before using specialised formula.
Amount of formula required
From 5 days to 3 months, a full-term, healthy baby will need about 150 ml of prepared formula per kilogram of body weight, every day. For example, a baby who weighs 3 kg will need 450 ml of prepared infant formula each day.
From 3 to 6 months, this falls to 120 ml of infant formula per kilogram of body weight each day. From 6 to 12 months, it falls again to between 90 and 120 ml of infant formula per kilogram of body weight each day.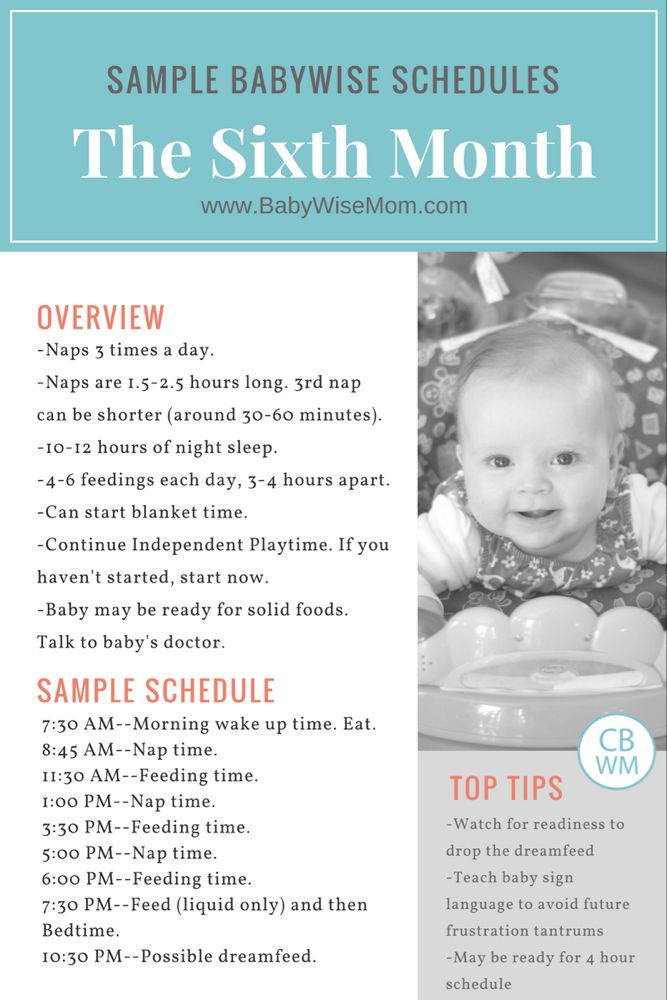
Premature babies need more formula. At first, they usually need about 160–180 ml of formula per kilogram of body weight per day. Your neonatal doctor or maternal and child health nurse will advise you.
See your doctor or maternal and child health nurse if you are worried about your baby’s appetite or growth.
Preparing formula
Always remember to:
- Wash your hands thoroughly and make sure your preparation area is clean.
- Check the date on the bottom of the tin or on the sachet to ensure the formula has not passed its expiry (use-by) date.
- Use the powder within one month of opening the tin.
- Follow the manufacturer’s instructions strictly. Accuracy is important to make sure your baby receives the right nutrition.
- Boil fresh, clean water in a kettle or saucepan.
- Do not let the water cool for longer than 30 minutes before making up infant formula. Hot water helps kill any bacteria (germs) in the powder.
- Pour the recommended amount of boiled water into the bottle.
- Use the scoop that came with the formula to measure the exact amount of powder. A scoop from another brand of powder might be larger or smaller. Never use a half-scoop as it may not be accurate. Make up the full volume (later throw out any leftover mixture).
- Level the powder with a sterilised knife or spatula (do not pack it down). Add this powder to the bottle of boiled water.
- Place the disc and cap on the bottle, and shake until thoroughly mixed.
- Make up only one bottle at a time. Germs can easily grow in prepared formula, and can make your baby ill.
- Never warm a bottle in a microwave oven. This is unsafe as it does not heat evenly and there may be ‘hot spots’ in the bottle that can burn your baby’s mouth.
- You can warm a bottle by standing it in a container of hot (not boiling) water for 10 minutes.
- Test the temperature by dripping some milk onto the inside of your wrist. It should feel the same temperature as your skin.
 If it is too warm, then cool the bottle under running water or in a container of cool water. Re-test on your wrist before giving to your baby.
If it is too warm, then cool the bottle under running water or in a container of cool water. Re-test on your wrist before giving to your baby. - If you are going out for the day, carry hot water in a hot water flask and the formula separately, then prepare it just before it is needed.
- When the tin of formula is empty, discard the scoop that was provided with the tin of infant formula.
- Read the instructions carefully if you change formula brands to ensure you use the correct amount of water and powder.
Do not use leftover formula
Use a fresh bottle for every feed. Throw away any leftover formula or expressed breastmilk following the feed. Never give your baby leftovers. They can grow bacteria (germs) that may make your baby ill.
Do not add other food, such as baby rice cereal, to the milk. If you think your baby needs more food than recommended, talk to your maternal and child health nurse.
Enjoy mealtimes with your baby
Mealtimes are a time to be together and communicate. Just as adults and children enjoy talking with each other at mealtimes, so do babies. Hold your baby close to your body, facing you, when feeding. This should be an enjoyable and social experience for you both.
Just as adults and children enjoy talking with each other at mealtimes, so do babies. Hold your baby close to your body, facing you, when feeding. This should be an enjoyable and social experience for you both.
Take the bottle away as soon as your baby has had enough.
Do not put your baby to bed with a bottle, to feed alone. This is dangerous because your baby may choke. Also, older children who are regularly fed this way are more likely to get middle-ear infections and tooth decay.
Equipment for bottle-feeding
Whether you are using a bottle for expressed breastmilk or infant formula, the equipment you will need includes:
- infant formula or expressed breastmilk
- clean water
- bottles
- teats
- sterilising equipment (and possibly sterilising chemicals).
Bottles for expressed breastmilk or infant formula
When buying bottles, remember that:
- You will need at least 3 large bottles with leak-proof caps, discs and teats.
- Plastic bottles are better, because glass breaks more easily.
- Bottles should be smooth on the inside surface (no ribbing or indentation), so they are easy to clean properly.
- Bottles should have clearly marked measurement guides that will not wear off over time.
Teats for bottle-feeding
When choosing teats, consider:
- Flow rate – check the label to make sure the teat has the right flow rate for your baby’s age. For example, a teat designed for an older baby can flood a newborn’s mouth with too much milk and may lead to choking.
- Testing the flow – hold the bottle upside down and milk should drip out at a constant, steady rate. If it drips too slowly, your baby will get tired before finishing their feed. If milk pours out in a stream, your baby may dribble and splutter and will not enjoy the feed. A baby should take 15 to 30 minutes to drink a bottle.
- Teat shape – many manufacturers claim that their teats are an exact copy of a mother’s nipple in her baby’s mouth, but there is no proof that any teat design is the best.
 ‘Orthodontic’ teats are no better than regular-shaped teats and they may, in fact, not be good for later tooth development. Over time, you will discover which teat works best for your baby.
‘Orthodontic’ teats are no better than regular-shaped teats and they may, in fact, not be good for later tooth development. Over time, you will discover which teat works best for your baby. - Air – air bubbles should rise through the milk as the baby drinks. If the teat flattens during feeding, loosen the cap a little.
Sterilise all equipment for bottle-feeding
You must sterilise (thoroughly clean and kill all germs) all bottle-feeding equipment until your baby is 12 months old. This is very important.
Always remember:
- Steam can cause severe skin burns, so be careful when boiling or steaming equipment.
- Place all equipment out of reach of children.
- Avoid unnecessary handling of sterilised equipment and do not touch the inner surfaces of bottles or teats.
First, wash all the equipment in warm, soapy water. Use a clean bottlebrush to thoroughly remove all traces of milk, then rinse, then sterilise. You can use different sterilising methods, such as boiling, chemicals, steam or microwave steam.
Boiling bottle-feeding equipment
Put all equipment in a large pot and cover with tap water (make sure your water meets the Australian Drinking Water Guidelines if you are not using town water).
Remember to:
- Make sure there are no air bubbles trapped inside the bottles.
- Put the saucepan lid on and bring to the boil.
- Allow 5 minutes of rapid boiling.
- Turn off heat and allow to cool.
- Always wash your hands thoroughly with soap and water before handling the equipment.
- Store the sterilised equipment in a clean container in the fridge and re-boil after 24 hours if it has not been used before then.
Chemical sterilising bottle-feeding equipment
Sterilising chemicals usually come in liquid or tablet form. When you sterilise the equipment:
- Follow the manufacturer’s instructions to get the correct strength.
- Mix the chemicals with water in a large plastic or glass bowl.
- Place all equipment in the solution.
 Cover every surface – for example, squirt solution through the teats and get rid of any air bubbles.
Cover every surface – for example, squirt solution through the teats and get rid of any air bubbles. - Soak for at least one hour.
- Remove the equipment and shake off excess solution, but do not rinse.
- Use only glass or plastic equipment, as metal will rust in the solution.
- Change the solution every 24 hours.
- Scrub the container with warm soapy water and rinse thoroughly before refilling with new solution.
Steam sterilising bottle-feeding equipment
A steam steriliser plugs into a power point. It works automatically once you have switched it on. You must follow the manufacturer’s directions. Most will tell you to:
- Place the equipment in the steriliser and add the correct amount of water.
- Put the lid on and steam the equipment for the recommended time.
- Leave the lid on the steriliser until the bottles are needed.
- Wipe and dry the inside of the container once a day to keep it clean.

Microwave steam sterilising bottle-feeding equipment
This is used in a microwave oven. You should:
- Follow the instructions carefully.
- Check the microwave power needed – not all microwave ovens are the same.
- Do not put any metal inside these sterilisers.
Where to get help
- Your maternal and child health nurse
- Your paediatrician
- Dietitians Australia Tel. 1800 812 942
- Royal Children’s Hospital Tel. (03) 9345 5522
- Advisory Panel on the Marketing in Australia of Infant Formula (APMAIF) Tel. (02) 6289 7358
Infant formula feeding
Category: Child Health
Topics: Babies and Toddlers, Diet and Eating
If you are not able to breastfeed your baby, infant formula is the only safe way of feeding your baby to around 6 months of age. Formula-fed babies are kept on formula until 12 months of age in addition to complementary food. Talk to your doctor or child health nurse before you start feeding your baby infant formula.
When preparing and giving your baby infant formula:
- Follow the instructions on the can to make sure your baby is getting the right nourishment
- Sterilise bottles by boiling for 5 minutes
- Wash your hands before you prepare a bottle
- Keep feeding your baby on demand
- Hold your baby while he or she is drinking.
Combining breastfeeding and infant formula feeding
Feeding your baby any amount of breastmilk has benefits for you and your baby. You might be able to combine breastfeeding with formula feeding if you are unable to give your baby only breastmilk. Here are some tips to help you:
- Try to breastfeed first before giving formula.
- Any breastmilk has benefits to mother and baby, even if it is only a few drops.
- The more you can express or breastfeed, the more milk you will make.
Choosing an infant formula
There are many types of infant formula in grocery stores and chemists. Your doctor, child health nurse or dietitian will advise you on a suitable type of infant formula.
Your doctor, child health nurse or dietitian will advise you on a suitable type of infant formula.
Remember…
- Cow’s milk-based formulas are right for most babies. They are recommended over infant formulas made from soy or goat’s milk.
- Special or soy-based formulas only need to be used for medical reasons. They should only be used with advice from a health professional.
- All infant formulas in Australia have enough nutrients to meet the growing needs of babies.
- Babies’ stomachs cannot break down regular milk. Avoid giving milk to babies younger than 12 months of age.
Getting started
Infant formulas can be a little bit different from one another. Always use the instructions on the can to make sure you are making it right for your baby. It is safest to feed your baby as soon as you make the formula. Only make 1 bottle at a time. Here is a list of steps for you to follow:
- Clean all preparation areas.
 Wash your hands using soap and water.
Wash your hands using soap and water. - Wash and sterilise bottles, teats and caps.
- Boil fresh water. If using an automatic kettle, let it switch off.
- Leave water to sit for at least 30 minutes to cool. Pour the right amount of water into the bottle.
- Add the amount of formula listed on the can. Too much and it can hurt your baby’s kidneys; too little and your baby won’t grow well. Measure the formula with the scoop from the can and level with a knife. Take care not to mix up scoops from other containers.
- Shake the bottle until the powder is dissolved.
- Check the temperature by putting a few drops on your wrist. It should feel just warm.
- You can now feed your baby. Hold your baby while he or she is drinking.
- Any formula left at the end of the feed must be discarded.
- Only keep made-up formula in the fridge for 24 hours.
Preparing feeds in advance
It is best to make 1 bottle of infant formula at a time, just before feeding. Sometimes you may need to make feeds in advance (e.g. for a babysitter). Here are some tips:
Sometimes you may need to make feeds in advance (e.g. for a babysitter). Here are some tips:
- Keep made-up feed in the fridge (temperature no higher than 5°C).
- Feeds can be stored in the fridge for up to 24 hours. Only remove when ready to be used.
Warming infant formula
- Stand the bottle of formula in a container of hot water for a few minutes (no more than 10 minutes). Using a microwave to rewarm feeds is not recommended, as it does not heat evenly and can burn your baby’s mouth. You can use a bottle warmer if you have one.
- Check the temperature by putting a few drops onto the inside of your wrist. It should feel warm or even a little bit cool.
- Any formula left at the end of the feed must be discarded.
Transporting infant formula
The best way to transport formula is to carry individual portions of the powdered formula and cooled boiled water in sterilised containers. Formula can also be made before transporting. Here are some tips:
Here are some tips:
- Feeds that need to be transported should be put in the fridge until they are cold before transporting.
- Keep the feed in the fridge until it needs to be transported.
- Transport feeds in a cool bag with ice bricks and use within 2 hours. Place the formula in the fridge if you arrive before then. Use the formula within 24 hours from the time it was made.
Cleaning feeding equipment
Equipment needs to be cleaned and sterilised. Clean bottles and teats by hand or in a dishwasher. Bottles and teats can be sterilised by boiling or with a steaming machine. (Use steamers according to the manufacturers’ instructions).
Boiling method
- Wash hands.
- Wash teats and bottles in hot, soapy water using a bottle brush and rinse well.
- Place equipment in a saucepan of cold water on a stove.
- Bring to the boil and boil for 5 minutes. Turn off and allow to cool.
- Store equipment in a clean container in the fridge if not being used immediately.
- Sterilised equipment can be stored in the fridge for up to 24 hours.
How much formula?
Feed your baby on demand. Each baby is different and needs vary from day to day. Refer to the Is my baby getting enough milk? sheet if you are concerned about how much your baby is drinking.
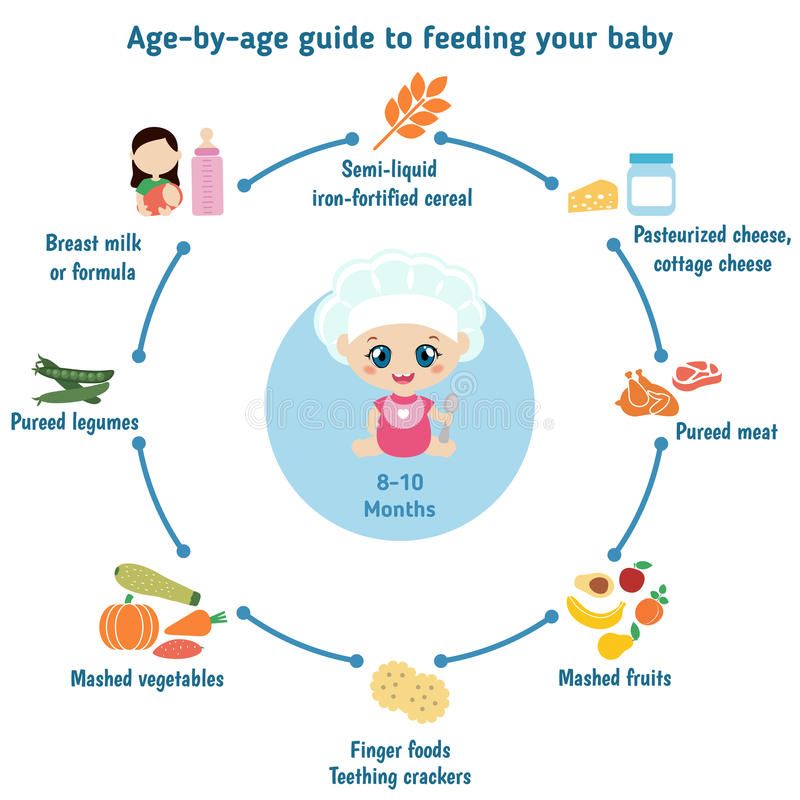
This is a general guide of how much infant formula your baby might need:
- 5 days to 3 months old: 150mL per kilogram of body weight each day.
- 3 to 6 months old: 120mL per kilogram of body weight each day.
- 6 to 12 months old: 100mL per kilogram of body weight each day. Babies at this age also eat complementary foods.
How to feed
- Sit comfortably with your baby in your arms while giving the bottle. Try holding your baby a different way each feed. This is because a baby’s skull is soft and changes in shape can occur if the baby always places their head in the same position.
- Hold the bottle tilted upside down.
 You can gently press under your baby’s chin to encourage your baby to firmly grip the teat. This will help the baby to not swallow air.
You can gently press under your baby’s chin to encourage your baby to firmly grip the teat. This will help the baby to not swallow air. - Check the bottle flow. The milk should drop at a steady flow from the teat. Sometimes the teat gets clogged when a powdered infant formula is used.
- It is common for babies to swallow some air. You can help your baby to burp by holding them upright over your shoulder or on your lap. Pat or rub the middle of their back gently until they burp.
- If the baby is feeding happily, don’t stop until they are finished.
- Avoid leaving your baby to feed on their own or while going to sleep. The milk may flow too fast and cause your baby to choke.
- Your baby is feeding well if they have 6 or more wet nappies per day, consistent weight gain (following a curve on their growth chart), and are alert and content after a feed.
Resources for parents, families and carers
Booklet: Child health information (PDF, 1. 34MB), Queensland Government (given to parents of every baby born in Queensland with the Personal Health record)
34MB), Queensland Government (given to parents of every baby born in Queensland with the Personal Health record)
Growing Strong—Formula feeding (PDF, 799kB), Queensland Government
Raising Children Network—Newborns nutrition, Australian Government
Raising Children Network—Breastfeeding videos, Australian Government
Booklet: Breastfeeding and postnatal care, New South Wales Government—available in English, Arabic, Chinese (Simplified), Chinese (Traditional), Farsi, Hindi, Korean, Punjabi and Tamil languages
Related content
The importance of breastfeeding
Managing common breast concerns
Is my baby getting enough milk?
Drinks for babies and toddlers
Acknowledgements
This fact sheet is consistent with the National breastfeeding strategy 2010–2015.
Information is drawn from:
- Children’s Health Queensland Hospital and Health Service 2015, Child health information: Your guide to the first 12 months.
- National Health and Medical Research Council 2012, Australian dietary guidelines.
- National Health and Medical Research Council 2012, Infant feeding guidelines.
- Preventative Health, Queensland Health 2008, Growing Strong: Feeding you and your baby.
- Preventative Health, Queensland Health 2010, Breastfeeding and your baby.
- Queensland Maternity and Neonatal Clinical Guidelines Program 2010, Breastfeeding initiation.
This fact sheet is also the result of input and effort from many health professionals in Queensland. Their assistance with the content is greatly appreciated.
This information is provided as general information only and should not be relied upon as professional or medical advice. Professional and medical advice should be sought for particular health concerns or events. Best efforts have been used to develop this information, which is considered correct and current in accordance with accepted best practice in Queensland as at the date of production. The State of Queensland (Queensland Health) does not accept liability to any person for the information provided in this fact sheet nor does it warrant that the information will remain correct and current. The State of Queensland (Queensland Health) does not promote, endorse or create any association with any third party by publication or use of any references or terminology in this fact sheet.
The State of Queensland (Queensland Health) does not accept liability to any person for the information provided in this fact sheet nor does it warrant that the information will remain correct and current. The State of Queensland (Queensland Health) does not promote, endorse or create any association with any third party by publication or use of any references or terminology in this fact sheet.
Back to top ( http://conditions.health.qld.gov.au/healthcondition/condition/8/31/325/infant-formula-feeding#top )
- Last updated:
- 20/09/2017 2:59:36 PM
Breastfeeding in the first month: what to expect
Not sure how to establish lactation and increase milk production? If you need help, support, or just want to know what to expect, read our first month breastfeeding advice
Share this information
The first weeks of breastfeeding are a very stressful period. If at times you feel like you can't handle it, know that you are not alone. Feeding your baby all day long is completely natural and helps produce breast milk, but can be quite tiring at times. Be patient, think about yourself and remember: after the first month, when milk production stabilizes, it will become easier.
If at times you feel like you can't handle it, know that you are not alone. Feeding your baby all day long is completely natural and helps produce breast milk, but can be quite tiring at times. Be patient, think about yourself and remember: after the first month, when milk production stabilizes, it will become easier.
How often should a baby be breastfed?
Babies are born with a small stomach that grows rapidly with increasing milk production: in the first week it is no larger than an apricot, and after two weeks it is already the size of a large chicken egg. 1.2 Let the child eat as much as he wants and when he wants. This will help him quickly regain the weight lost after birth and grow and develop further.
“Be prepared to feed every two to three hours throughout the day. At night, the intervals between feedings can be longer: three to four or even five hours, says Cathy Garbin, a recognized international expert on breastfeeding. Some eat quickly and are satiated in 15 minutes, while others take an entire hour to feed. Do not compare your breastfeeding regimen with that of other mothers - it is very likely that there will be nothing in common between them.
Do not compare your breastfeeding regimen with that of other mothers - it is very likely that there will be nothing in common between them.
At each feed, give your baby a full meal from one breast and then offer a second one, but don't worry if the baby doesn't take it. When the baby is full, he lets go of his chest and at the same time looks relaxed and satisfied - so much so that he can immediately fall asleep. The next time you feed, start on the other breast. You can monitor the order of the mammary glands during feeding using a special application.
Why does the child always ask for a breast?
The first month is usually the hardest time to breastfeed. But do not think that because the baby is constantly hungry and asks for a breast almost every 45 minutes, then you do not have enough milk.
In the first month, the baby needs to eat frequently to start and stimulate the mother's milk production. It lays the foundation for a stable milk supply in the future.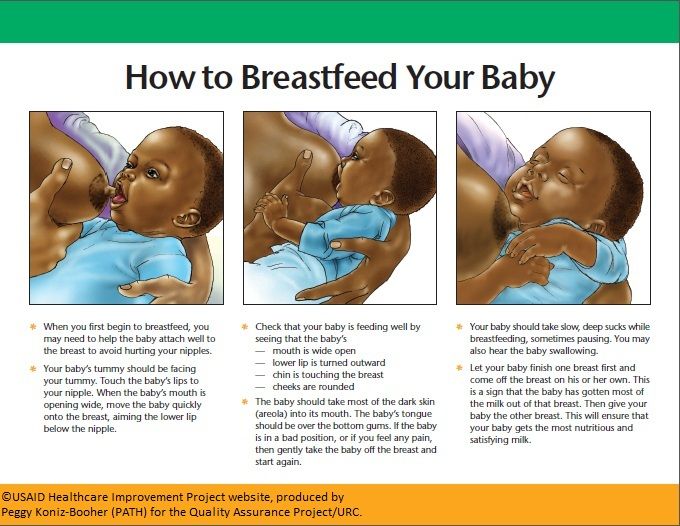 3
3
In addition, we must not forget that the child needs almost constant contact with the mother. The bright light and noise of the surrounding world at first frighten the baby, and only by clinging to his mother, he can calm down.
Sarah, mother of three from the UK, confirms: “Crying is not always a sign of hunger. Sometimes my kids just wanted me to be around and begged for breasts to calm them down. Use a sling. Place the cradle next to the bed. Don't look at the clock. Take advantage of every opportunity to relax. Forget about cleaning. Let those around you take care of you. And not three days, but six weeks at least! Hug your baby, enjoy the comfort - and trust your body."
Do I need to feed my baby on a schedule?
Your baby is still too young for a strict daily routine, so
forget about breastfeeding schedules and focus on his needs.
“Volumes have been written about how to feed a baby on a schedule, but babies don't read or understand books,” Cathy says. - All children are different. Some people can eat on a schedule, but most can't. Most often, over time, the child develops his own schedule.
- All children are different. Some people can eat on a schedule, but most can't. Most often, over time, the child develops his own schedule.
Some mothers report that their babies are fine with scheduled feedings, but they are probably just the few babies who would eat every four hours anyway. Adults rarely eat and drink the same foods at the same time of day - so why do we expect this from toddlers?
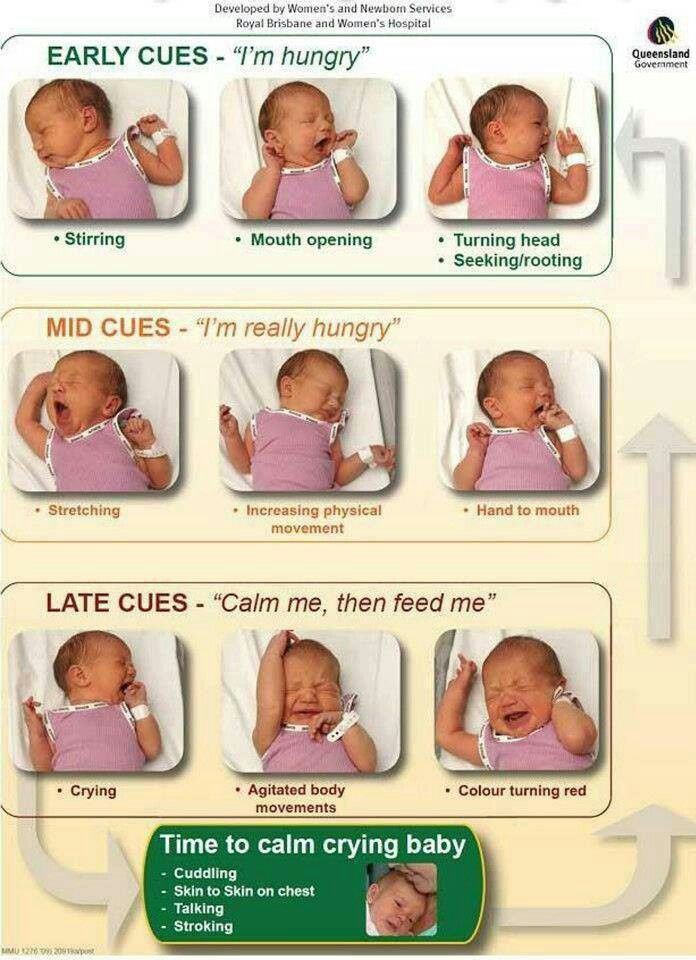
Offer your baby the breast at the first sign of hunger. Crying is already the last stage, so be attentive to early signs: the baby licks his lips, opens his mouth, sucks his fist, turns his head with his mouth open - looking for the breast. 4
What is a "milk flush"?
At the beginning of each feed, a hungry baby actively sucks on the nipple,
thereby stimulating the milk flow reflex - the movement of milk through the milk ducts. 5
“Nipple stimulation triggers the release of the hormone oxytocin,” explains Cathy. “Oxytocin is distributed throughout the body and causes the muscles around the milk-producing glands to contract and the milk ducts to dilate. This stimulates the flow of milk.
This stimulates the flow of milk.
If the flushing reflex fails, milk will not come out. This is a hormonal response, and under stress it may not work at all or work poorly. Therefore, it is so important that you feel comfortable and calm when feeding.
“Studies show that each mother has a different rhythm of hot flashes during one feed,” Kathy continues, “Oxytocin is a short-acting hormone, it breaks down in just 30-40 seconds after formation. Milk begins to flow, the baby eats, the effect of oxytocin ends, but then a new rush of milk occurs, the baby continues to suckle the breast, and this process is repeated cyclically. That is why, during feeding, the child periodically stops and rests - this is how nature intended.
The flow of milk may be accompanied by a strong sensation of movement or tingling in the chest, although 21% of mothers, according to surveys, do not feel anything at all. 5 Cathy explains: “Many women only feel the first rush of milk. If you do not feel hot flashes, do not worry: since the child eats normally, most likely, you simply do not understand that they are.
If you do not feel hot flashes, do not worry: since the child eats normally, most likely, you simply do not understand that they are.
How do you know if a baby is getting enough milk?
Since it is impossible to track how much milk a baby eats while breastfeeding, mothers sometimes worry that the baby is malnourished. Trust your child and your body.
After a rush of milk, the baby usually begins to suckle more slowly. Some mothers clearly hear how the baby swallows, others do not notice it. But one way or another, the child himself will show when he is full - just watch carefully. Many babies make two or three approaches to the breast at one feeding. 6
“When a child has had enough, it is noticeable almost immediately: a kind of “milk intoxication” sets in. The baby is relaxed and makes it clear with his whole body that he is completely full, says Katie, “Diapers are another great way to assess whether the baby is getting enough milk. During this period, a breastfed baby should have at least five wet diapers a day and at least two portions of soft yellow stool, and often more. ”
”
From one month until weaning at six months of age, a baby's stool (if exclusively breastfed) should look the same every day: yellow, grainy, loose, and watery.
When is the child's birth weight restored?
Most newborns lose weight in the first few days of life. This is normal and should not be cause for concern. As a rule, weight is reduced by 5-7%, although some may lose up to 10%. One way or another, by 10–14 days, almost all newborns regain their birth weight. In the first three to four months, the minimum expected weight gain is an average of 150 grams per week. But one week the child may gain weight faster, and the next slower, so it is necessary that the attending physician monitor the health and growth of the baby constantly. 7.8
At the slightest doubt or signs of dehydration, such as
dark urine, no stool for more than 24 hours, retraction of the fontanel (soft spot on the head), yellowing of the skin, drowsiness, lethargy, lack of appetite (ability to four to six hours without feeding), you should immediately consult a doctor.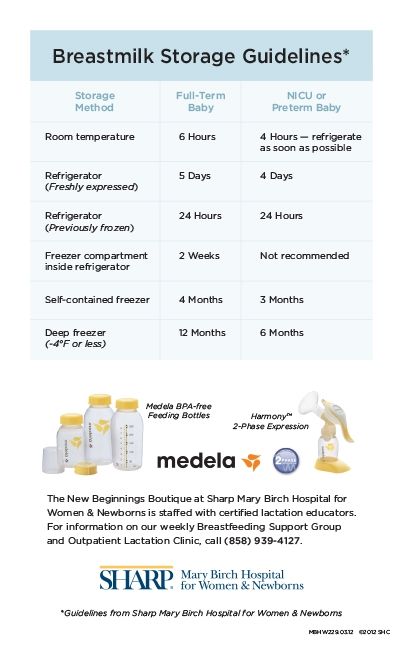 7
7
What is "cluster feeding"?
When a baby asks to breastfeed very often for several hours, this is called cluster feeding. 6 The peak often occurs in the evening between 18:00 and 22:00, just when many babies are especially restless and need close contact with their mother. Most often, mothers complain about this in the period from two to nine weeks after childbirth. This is perfectly normal and common behavior as long as the baby is otherwise healthy, eating well, gaining weight normally, and appears content throughout the day. 9
Cluster feeding can be caused by a sharp jump in the development of the body - during this period the baby especially needs love, comfort and a sense of security. The growing brain of a child is so excited that it can be difficult for him to turn off, or it just scares the baby. 9 If a child is overworked, it is often difficult for him or her to calm down on his own, and adult help is needed. And breastfeeding is the best way to calm the baby, because breast milk is not only food, but also pain reliever and a source of happiness hormones. 10
And breastfeeding is the best way to calm the baby, because breast milk is not only food, but also pain reliever and a source of happiness hormones. 10
“Nobody told me about cluster feeding, so for the first 10 days I just went crazy with worry - I was sure that my milk was not enough for the baby,” recalls Camille, a mother from Australia, “It was a very difficult period . I was advised to pump and supplement until I finally contacted the Australian Breastfeeding Association. There they explained to me what was happening: it turned out that it was not about milk at all.
Remember, this is temporary. Try to prepare dinner for yourself in the afternoon, when the baby is fast asleep, so that in the evening, when he begins to often breastfeed, you have the opportunity to quickly warm up the food and have a snack. If you are not alone, arrange to carry and rock the baby in turns so that you have the opportunity to rest. If you have no one to turn to for help and you feel that your strength is leaving you, put the baby in the crib and rest for a few minutes, and then pick it up again.
Ask your partner, family and friends to help you with household chores, cooking and caring for older children if you have any. If possible, hire an au pair. Get as much rest as possible, eat well and drink plenty of water.
“My daughter slept a lot during the day, but from 23:00 to 5:00 the cluster feeding period began, which was very tiring,” recalls Jenal, a mother from the USA, “My husband tried his best to make life easier for me - washed, cleaned, cooked, changed diapers, let me sleep at every opportunity and never tired of assuring me that we were doing well.
If you are concerned about the frequency of breastfeeding, it is worth contacting a specialist. “Check with a lactation consultant or doctor to see if this is indicative of any problems,” recommends Cathy. “Resist the temptation to supplement your baby with formula (unless recommended by your doctor) until you find the cause. It may not be a matter of limited milk production at all - it may be that the child is inefficiently sucking it.
When will breastfeeding become easier?
This early stage is very special and does not last long. Although sometimes it seems that there will be no end to it, rest assured: it will get easier soon! By the end of the first month, breast milk production will stabilize, and the baby will become stronger and learn to suckle better. 2.3 Any problems with latch on by this time will most likely be resolved and the body will be able to produce milk more efficiently so inflammation and leakage of milk will begin to subside.
“The first four to six weeks are the hardest, but then things start to get better,” Cathy assures. It just needs to be experienced!”
The longer breastfeeding continues, the more benefits it brings, from saving on formula and improving sleep quality 11–13 to boosting your baby's immune system 14 and reducing your risk of certain cancers. 15
“When you feel like you're pushing yourself, try to go from feed to feed and day to day,” says Hannah, a UK mom.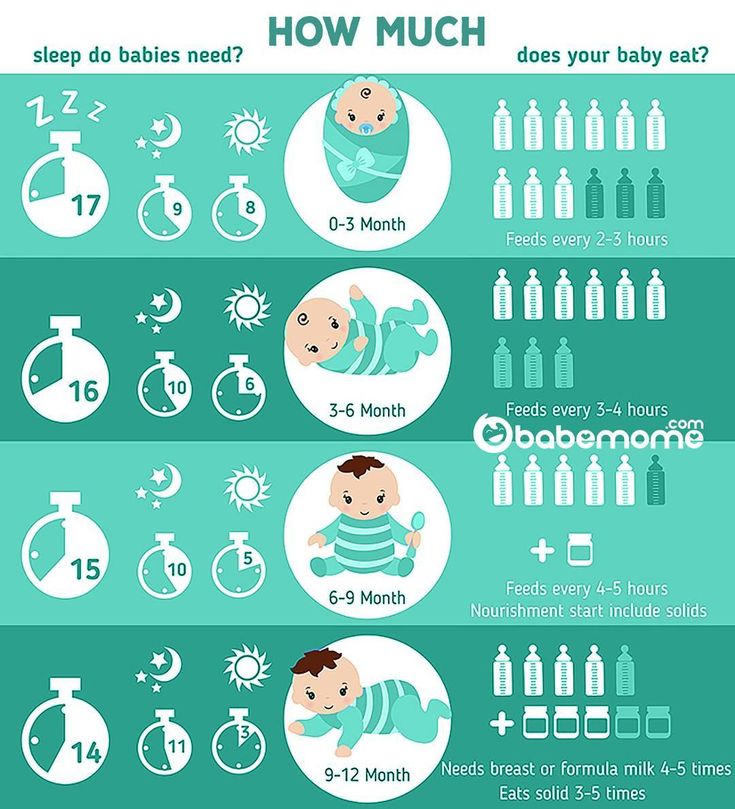 “I was sure I wouldn’t make it to eight weeks. And now I have been breastfeeding for almost 17 weeks, and I dare say it is very easy.”
“I was sure I wouldn’t make it to eight weeks. And now I have been breastfeeding for almost 17 weeks, and I dare say it is very easy.”
Read the resource Breastfeeding Beyond the First Month: What to Expect
Literature
1 Naveed M et al. An autopsy study of relationship between perinatal stomach capacity and birth weight. Indian J Gastroenterol .1992;11(4):156-158. - Navid M. et al., Association between prenatal gastric volume and birth weight. Autopsy. Indian J Gastroenterol. 1992;11(4):156-158.
2 Neville MC et al. Studies in human lactation: milk volumes in lactating women during the onset of lactation and full lactation .Am J Clinl Nutr . 1988;48(6):1375-1386. at the beginning and at the peak of lactation." Am F Clean Nutr. 1988;48(6):1375-1386.
3 Kent JC et al. Principles for maintaining or increasing breast milk production. J Obstet , Gynecol , & Neonatal Nurs . 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
Principles for maintaining or increasing breast milk production. J Obstet , Gynecol , & Neonatal Nurs . 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
4 Australian Breastfeeding Feeding cues ; 2017 Sep [ cited 2018 Feb ]. - Australian Breastfeeding Association [Internet], Feed Ready Signals; September 2017 [cited February 2018]
5 Kent JC et al. Response of breasts to different stimulation patterns of an electric breast pump. J Human Lact . 2003;19(2):179-186. - Kent J.S. et al., Breast Response to Different Types of Electric Breast Pump Stimulation.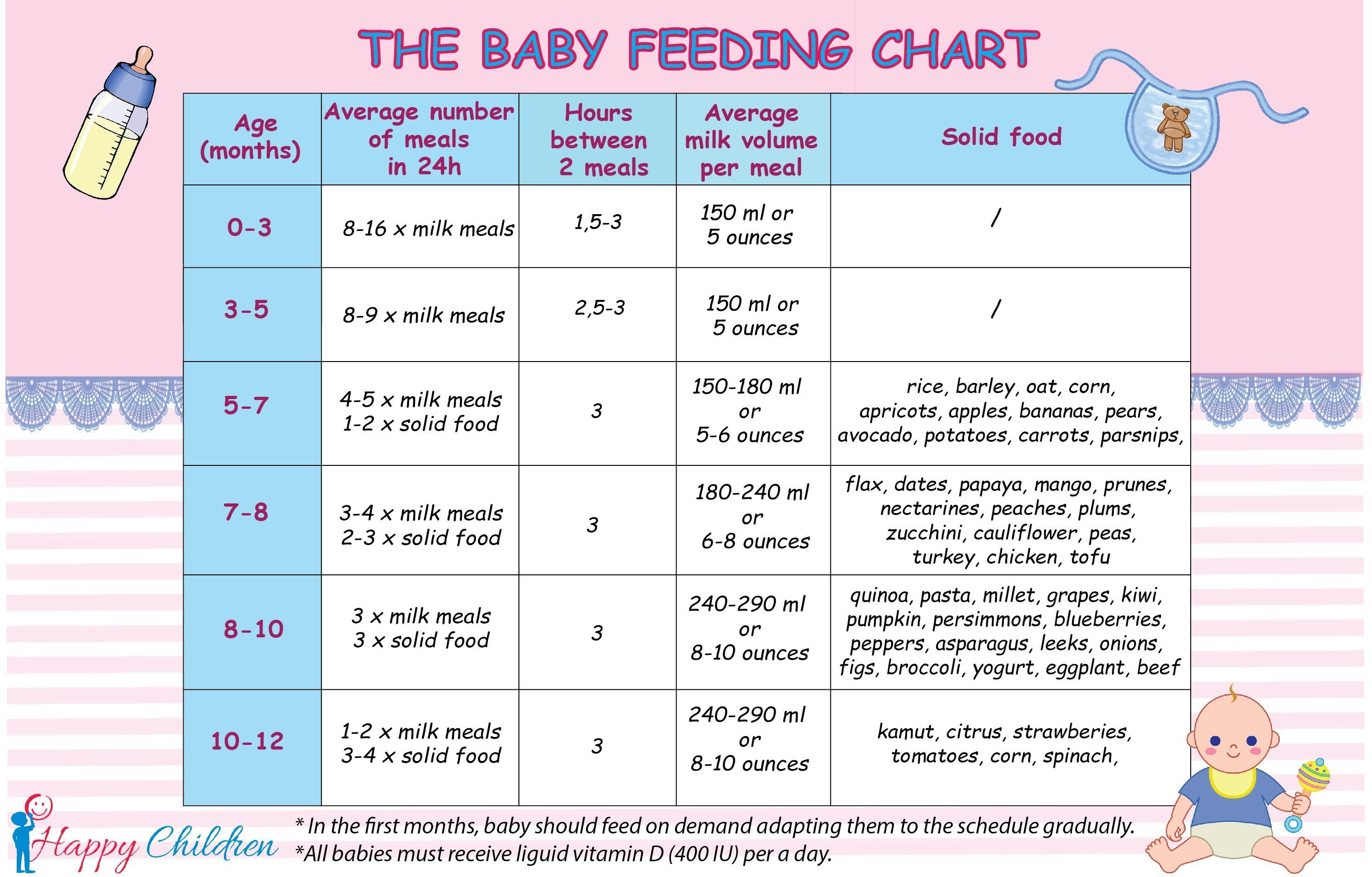 J Human Lact (Journal of the International Association of Lactation Consultants). 2003;19(2):179-186.
J Human Lact (Journal of the International Association of Lactation Consultants). 2003;19(2):179-186.
6) Kent JC et al . Volume and frequency of breastfeedings and fat content of breast milk throughout the day. Pediatrics. 2006;117(3): e 387-395. - Kent J.S. et al., "Amount and frequency of breastfeeding and fat content of breast milk during the day." Pediatrix (Pediatrics). 2006;117(3):e387-95.
7 Lawrence RA, Lawrence RM. Breastfeeding: A guide for the medical profession. 7th ed. Maryland Heights MO, USA: Elsevier Mosby; 2010. 1128 p . - Lawrence R.A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." Seventh edition. Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2010. P. 1128.
8 World Health Organization. [Internet]. Child growth standards; 2018 [cited 2018 Feb] - World Health Organization. [Internet]. Child Growth Standards 2018 [cited February 2018].
[Internet]. Child growth standards; 2018 [cited 2018 Feb] - World Health Organization. [Internet]. Child Growth Standards 2018 [cited February 2018].
9 Australian Breastfeeding Association . [ Internet ]. Cluster feeding and fussing babies ; Dec 2017 [ cited 2018 Feb ] - Australian Breastfeeding Association [Internet], Cluster Feeding and Screaming Babies; December 2017 [cited February 2018].
10 Moberg KU, Prime DK. Oxytocin effects in mothers and infants during breastfeeding. Infant . 2013;9(6):201-206.- Moberg K, Prime DK, "Oxytocin effects on mother and child during breastfeeding". Infant. 2013;9(6):201-206.
11 U.S. Department of Health & Human Services [Internet]. Surgeon General Breastfeeding factsheet; 2011 Jan 20 [cited 2017 Feb] - Department of Health and Human Services [Internet], "Breastfeeding Facts from the Chief Medical Officer", Jan 20, 2011 [cited Feb 2017]
12 Kendall-Tackett K et al.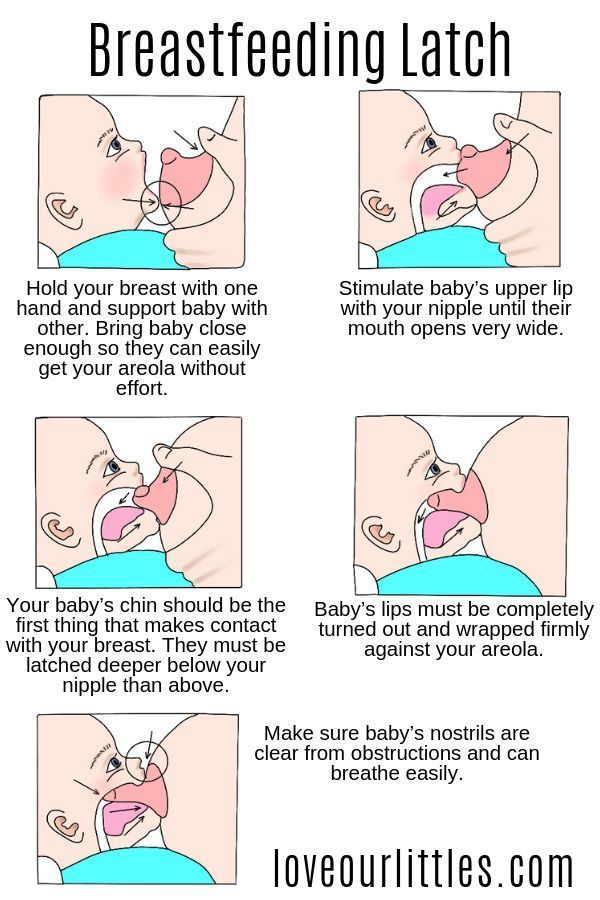 The effect of feeding method on sleep duration, maternal well-being, and postpartum depression. clinical lactation. 2011;1;2(2):22-26. - Kendall-Tuckett, K. et al., "Influence of feeding pattern on sleep duration, maternal well-being and the development of postpartum depression." Clinical Lactation. 2011;2(2):22-26.
The effect of feeding method on sleep duration, maternal well-being, and postpartum depression. clinical lactation. 2011;1;2(2):22-26. - Kendall-Tuckett, K. et al., "Influence of feeding pattern on sleep duration, maternal well-being and the development of postpartum depression." Clinical Lactation. 2011;2(2):22-26.
13 Brown A, Harries V. Infant sleep and night feeding patterns during later infancy: Association with breastfeeding frequency, daytime complementary food intake, and infant weight. Breast Med . 2015;10(5):246-252. - Brown A., Harris W., "Night feedings and infant sleep in the first year of life and their association with feeding frequency, daytime supplementation, and infant weight." Brest Med (Breastfeeding Medicine). 2015;10(5):246-252.
14 Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk.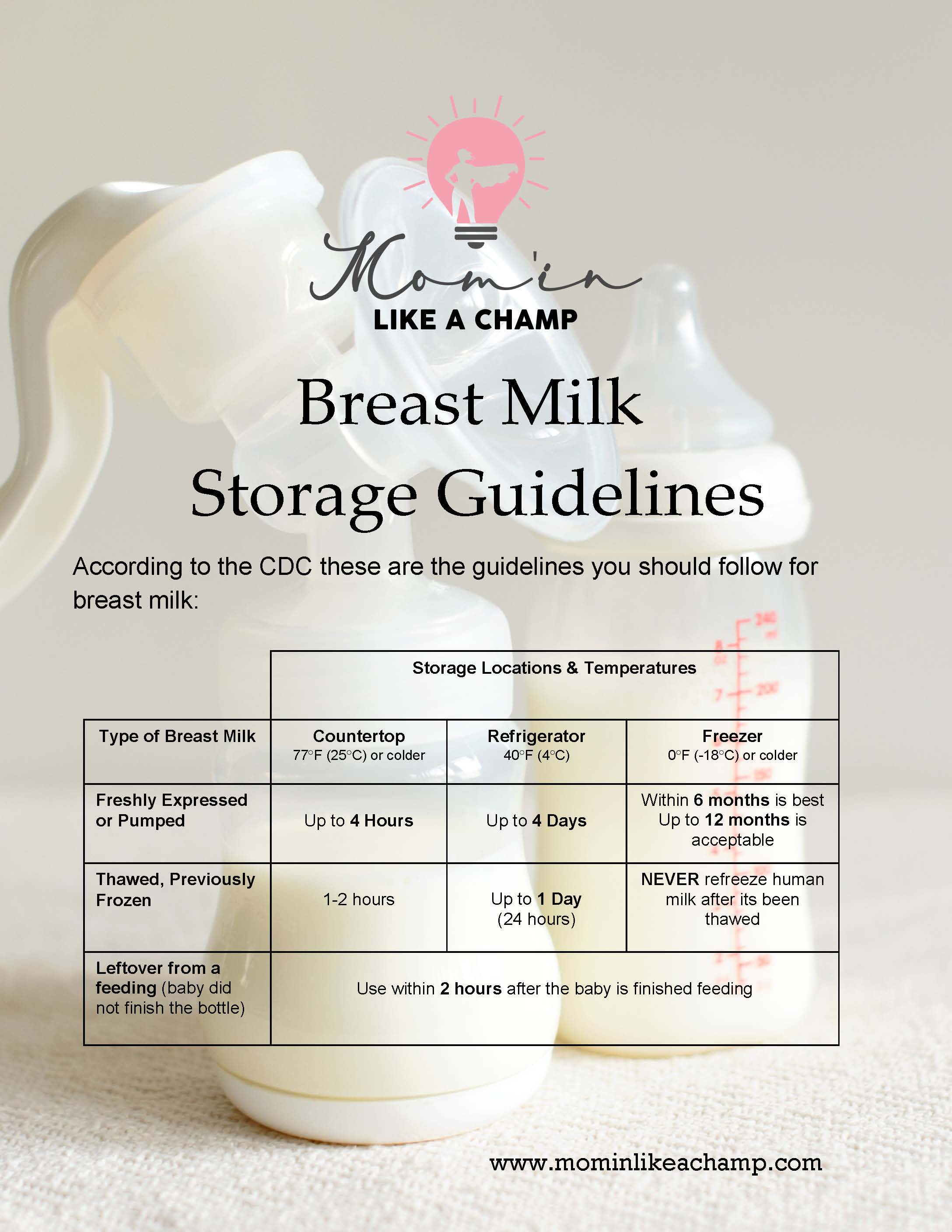 Clin Transl immunology. 2013;2(4). - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
Clin Transl immunology. 2013;2(4). - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
15 Li DP et al. Breastfeeding and ovarian cancer risk: a systematic review and meta-analysis of 40 epidemiological studies. Asian Pac J Cancer Prev . 2014;15(12):4829-4837. - Lee D.P. et al., "Breastfeeding and the risk of ovarian cancer: a systematic review and meta-analysis of 40 epidemiological studies." Asia Pas J Cancer Prev. 2014;15(12):4829-4837.
Breastfeeding a newborn | What to Expect in the First Week
The first week of a baby's life is a wonderful but hectic time, especially if you haven't breastfed before. Our breastfeeding tips will help you settle in as quickly as possible
Share this information
The first time after childbirth, mothers are often confused. The body is still recovering, and you are already starting to get to know your newborn baby. The emotional state during this period can be unstable, especially between the second and fifth day, when many women have milk 1 and at the same time postpartum depression begins 2 . In addition, people around often expect (and demand) that a woman come to her senses as soon as possible and become a “super mom”. But the best thing to do this first week is just to be with your baby and get breastfeeding going.
The body is still recovering, and you are already starting to get to know your newborn baby. The emotional state during this period can be unstable, especially between the second and fifth day, when many women have milk 1 and at the same time postpartum depression begins 2 . In addition, people around often expect (and demand) that a woman come to her senses as soon as possible and become a “super mom”. But the best thing to do this first week is just to be with your baby and get breastfeeding going.
When should I start breastfeeding my newborn?
Try to breastfeed your baby within the first hour after birth. When the baby latch onto the breast and begins sucking rhythmically, it stimulates the mammary gland cells and starts milk production. 1 It is not for nothing that this time is called the “magic hour”!
“Ideally, the baby should be placed on the mother's stomach immediately after birth so that it can immediately attach to the breast.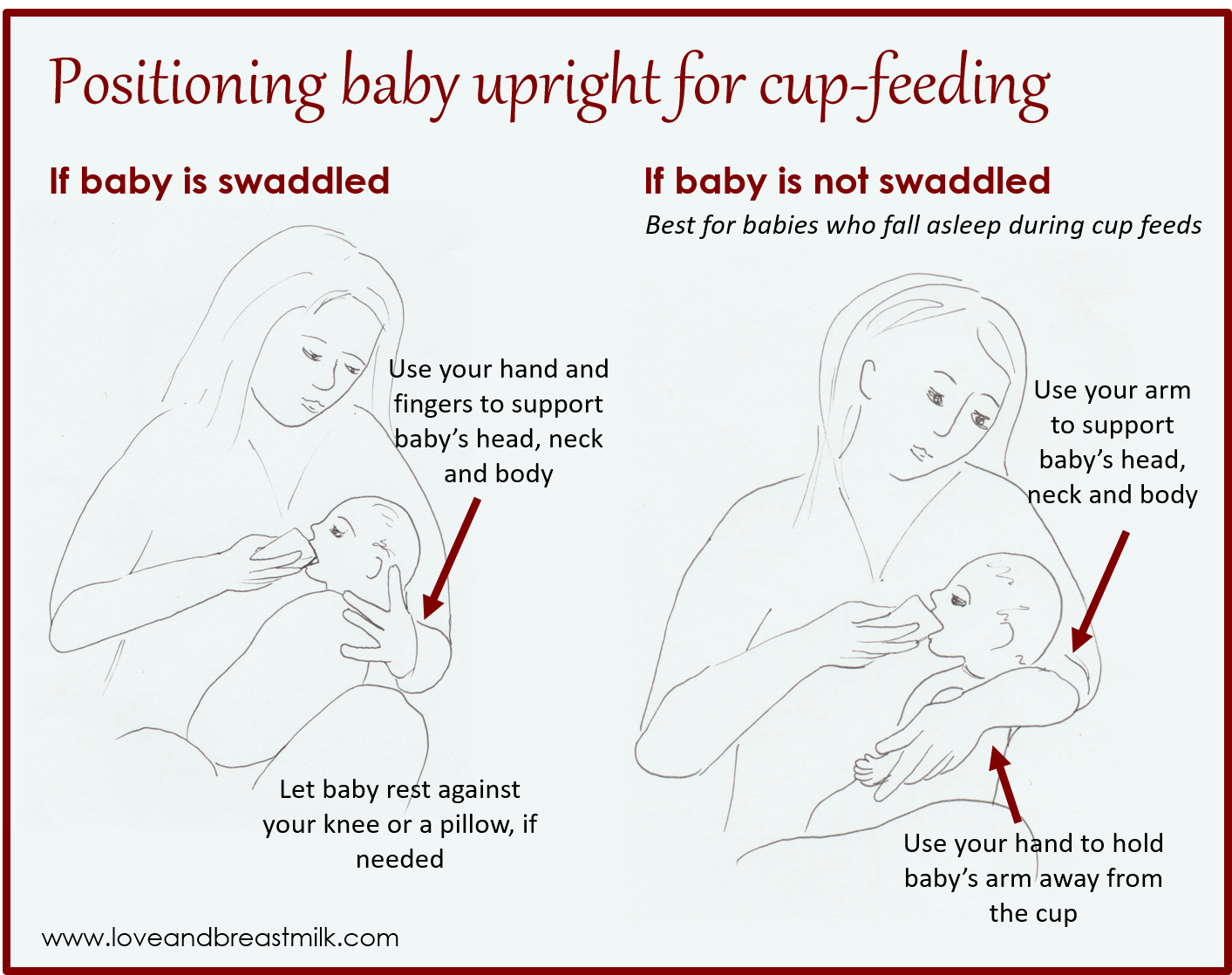 He won't necessarily eat, but he should be able to,” explains Cathy Garbin, an internationally recognized expert on breastfeeding.
He won't necessarily eat, but he should be able to,” explains Cathy Garbin, an internationally recognized expert on breastfeeding.
“Hold your baby and let him find the breast on his own and put the nipple in his mouth. This is called the breast-seeking reflex. On the Internet you can watch videos that show what this process looks like. If the baby does not latch onto the nipple on its own, the midwife will help to properly attach it to the breast. But for starters, it’s good to give the baby the opportunity to do it on their own. In this case, the optimal position for the mother is reclining. ”
Don't spend that special first hour of your baby's life weighing and swaddling—or at least wait until he's suckling for the first time. Enjoy hugs and close skin-to-skin contact. This promotes the production of oxytocin, the hormone of love, in you and your baby, and oxytocin plays a key role in the supply of the first breast milk - colostrum. 3
“As soon as the obstetricians were convinced that our son was healthy, the three of us — me, my husband and our baby — were left to give us the opportunity to get to know each other.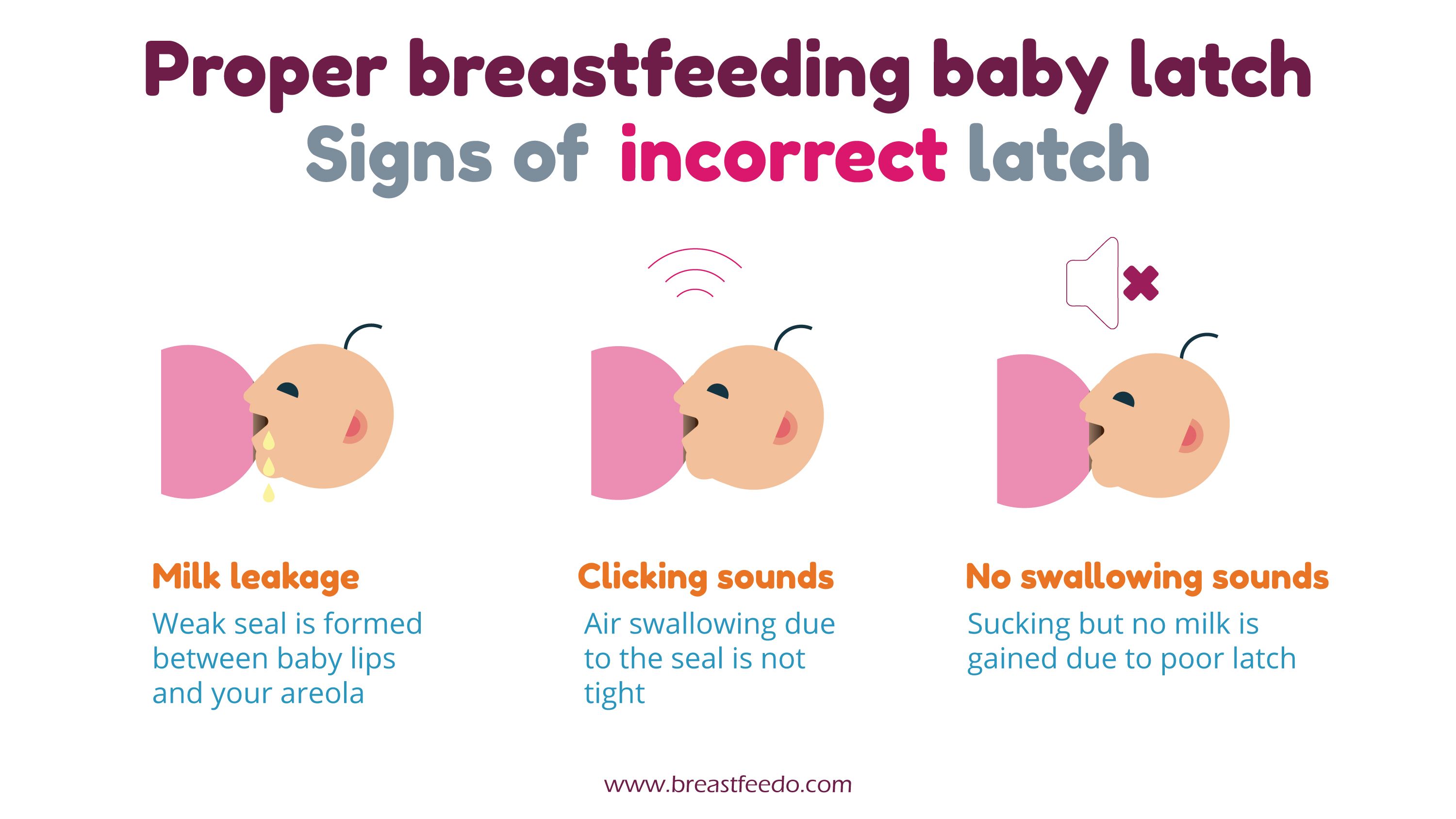 It was a very special hour - an hour of awkwardness, turbulent emotions and bliss. During this time, I breastfed my son twice, ”recalls Ellie, a mother of two from the UK.
It was a very special hour - an hour of awkwardness, turbulent emotions and bliss. During this time, I breastfed my son twice, ”recalls Ellie, a mother of two from the UK.
Did you know that breastfeeding helps to recover after childbirth? This is because oxytocin stimulates uterine contractions. In the first hours after childbirth, this contributes to the natural release of the placenta and reduces blood loss. 4
What if the birth did not go according to plan?
If you had a caesarean section or other complications during childbirth,
You can still establish skin-to-skin contact with your baby and breastfeed him in the first hours after birth.
“If you can't hold your baby, have your partner do it for you and make skin-to-skin contact with the baby. This will give the baby a sense of security, care and warmth so that he can hold on until you recover, ”Katie advises.
If the baby is unable to breastfeed, it is advisable to start expressing milk as early as possible and do so as often as possible until the baby is able to feed on its own. “While breastfeeding in the first hours after birth lays an excellent foundation for the future, it is not so important,” Cathy reassures. “It is much more important to start lactation so that in the future, if necessary, you can start breastfeeding.”
“While breastfeeding in the first hours after birth lays an excellent foundation for the future, it is not so important,” Cathy reassures. “It is much more important to start lactation so that in the future, if necessary, you can start breastfeeding.”
To start milk production, you can express milk manually or use a breast pump that can be given to you at the hospital. 5 And with expressed precious colostrum, it will be possible to feed the child. This is especially important if the baby was born premature or weak, since breast milk is extremely healthy.
If a baby was born prematurely or has a medical condition and cannot be breastfed immediately, this is no reason not to continue breastfeeding. “I have worked with many new mothers who were unable to breastfeed their baby for the first six weeks due to preterm labor or other reasons. Nevertheless, all of them later successfully switched to breastfeeding,” says Kathy.
Does the baby latch on correctly?
Correct breastfeeding is essential for successful breastfeeding 6 , as it determines how effectively the baby will suckle milk and hence grow and develop. Latching on the breast incorrectly can cause sore or damaged nipples, so don't hesitate to ask your doctor to check that your baby is properly attached to the breast, even if you are told that everything is fine and you do not see obvious problems - especially while you are in the hospital.
Latching on the breast incorrectly can cause sore or damaged nipples, so don't hesitate to ask your doctor to check that your baby is properly attached to the breast, even if you are told that everything is fine and you do not see obvious problems - especially while you are in the hospital.
“While I was in the hospital, I called the doctor at every feed and asked me to check if I was breastfeeding correctly,” says Emma, mother of two from Australia. - There were several cases when it seemed to me that everything seemed to be right, but it was painful to feed, and the doctor helped me take the baby off the breast and attach it correctly. By the time I was discharged, I had already learned to do it confidently.”
When applying to the breast, point the nipple towards the palate. This will allow the baby to take the nipple and part of the areola under it into their mouth. It will be easier for him to suck if he has both the nipple and part of the areola around in his mouth.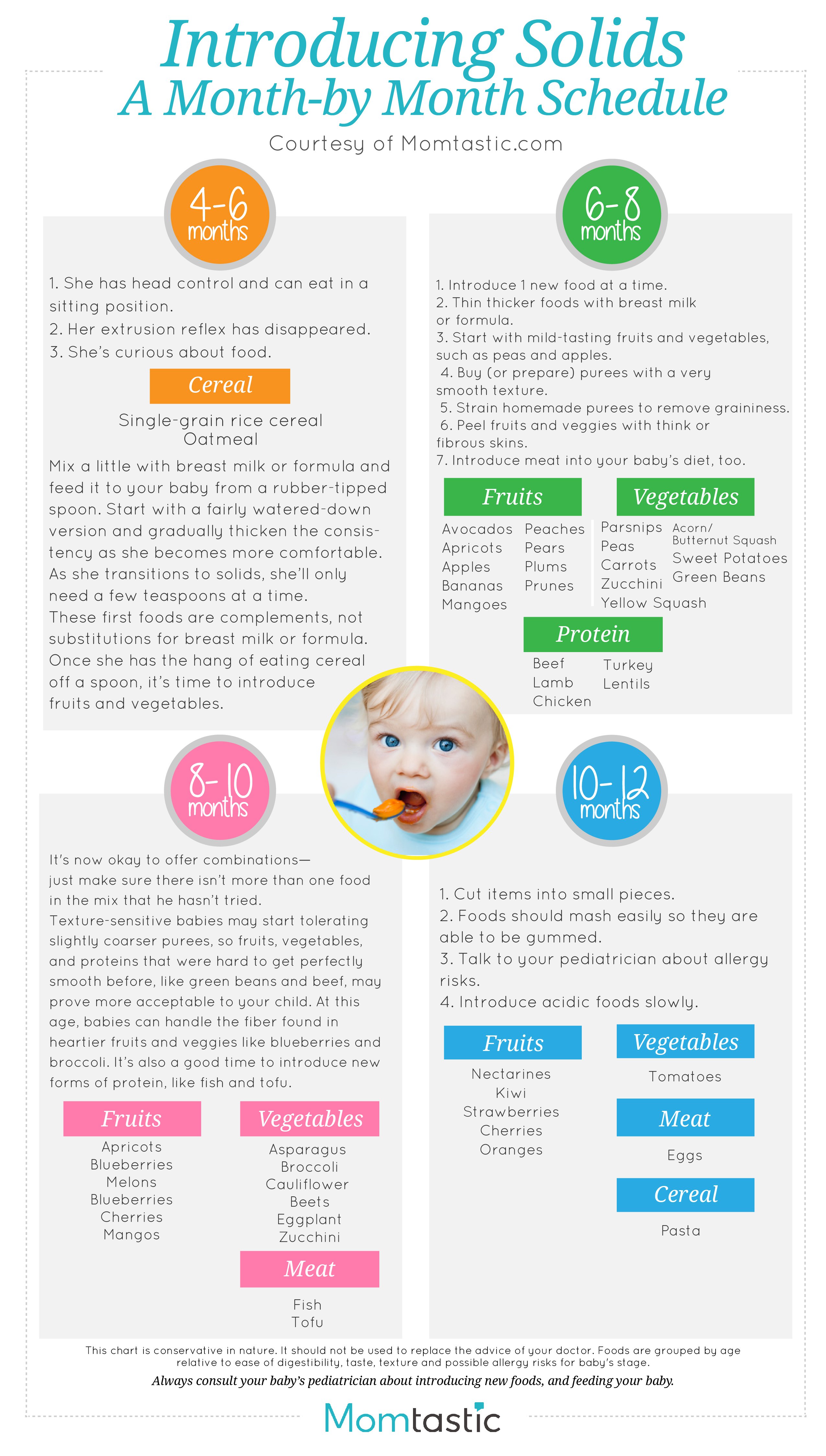 6
6
“When a baby latch on properly, it doesn't cause discomfort and it causes a pulling sensation, not pain,” Cathy explains. - The baby's mouth is wide open, the lower lip may be slightly turned outward, and the upper one lies comfortably on the chest. The body language of the child indicates that he is comfortable. There isn't much milk at this early stage, so you probably won't notice your baby swallowing, but he will suckle a lot and nurse frequently."
How often should a newborn be fed?
The frequency and duration of breastfeeding in the first week can vary greatly. “The first 24 hours of life are completely different for different children. Someone sleeps a lot (after all, childbirth is tiring!), And someone often eats, says Katie. - Such a variety greatly confuses young mothers. Everyone gives different advice, so it's important to remember that every mother and child is different."
“Colostrum is thicker than mature breast milk and is produced in smaller amounts, but has many benefits. When the baby eats colostrum, he learns to suck, swallow and breathe until milk begins to flow in more volume, ”explains Cathy.
When the baby eats colostrum, he learns to suck, swallow and breathe until milk begins to flow in more volume, ”explains Cathy.
Milk usually arrives on the second or fourth day after delivery. Until this time, the baby is applied to the breast 8-12 times a day (and sometimes more often!), including at night. 7 Feeding may take 10-15 minutes at this stage, or 45 minutes or even an hour, as the baby is just beginning to develop the muscles and coordination needed to suckle effectively.
“At first, the intensity of feeding is very high, often higher than many people realize, and this is shocking to most new mothers,” says Cathy. - Sometimes mom has no time to go to the toilet, take a shower and have a snack. It usually comes as a surprise."
Camille, a mother from Australia, experienced this. “The first week, Frankie ate every two hours, day and night, and each time it took half an hour to an hour to feed,” she recalls. “My husband and I were completely exhausted!”
Do I need to feed my newborn on a schedule?
The good news is that frequent feeding promotes lactation and stimulates milk production. 7 The more your baby eats, the more milk you will have. Therefore, forget about feeding your newborn on a schedule - this way he will have less chance of feeding. Try to feed your baby when he signals that he is hungry 8 :
7 The more your baby eats, the more milk you will have. Therefore, forget about feeding your newborn on a schedule - this way he will have less chance of feeding. Try to feed your baby when he signals that he is hungry 8 :
- toss and turn in her sleep;
- opens eyes;
- turns his head if he feels a touch on his cheek;
- sticks out tongue;
- groans;
- licks lips;
- sucks fingers;
- is naughty;
- whimpers;
- is crying.
Crying is the last sign of hunger, so if in doubt, just offer your baby the breast. If he bursts into tears, it will be more difficult to feed him, especially at first, when both of you are just learning how to do it. As your baby grows, he will likely eat less frequently and take less time to feed, so breastfeeding will seem more predictable.
Does breastfeeding hurt?
You may have heard that breastfeeding is not painful at all, but in fact, in the early days, many new mothers experience discomfort. And this is not at all surprising, given that the nipples are not used to such frequent and strong sucking.
And this is not at all surprising, given that the nipples are not used to such frequent and strong sucking.
“Breastfeeding can be uncomfortable for the first couple of days – your body and your baby are just getting used to it. If a baby eats for too long and does not latch well, the sensations are almost the same as from unworn new shoes, Cathy compares. Just as tight shoes can rub your feet, improper suckling can damage your nipples. Prevention is always better than cure, so if the pain persists after a few days of feeding, contact a lactation consultant or healthcare professional.”
Maria, a mother from Canada, agrees: “Although my son seemed to latch onto the breast well, he damaged his nipples while feeding, and I was in pain. As it turned out, the reason was a shortened frenulum of the tongue. The breastfeeding specialists at our city clinic have been of great help in diagnosis and treatment.”
In addition, you may experience period cramps during the first few days after breastfeeding, especially if this is not your first baby. This is the so-called postpartum pain. The fact is that oxytocin, which is released during breastfeeding, contributes to further contraction of the uterus to restore its normal size. 4
This is the so-called postpartum pain. The fact is that oxytocin, which is released during breastfeeding, contributes to further contraction of the uterus to restore its normal size. 4
When milk arrives, the breasts usually become fuller, firmer and larger than before delivery. In some women, the breasts swell, harden and become very sensitive - swelling of the mammary glands occurs. 10 Frequent breastfeeding relieves these symptoms. For more breast care tips, read our article What is Breast Swelling?
How often does a newborn urinate and defecate?
What goes into the body must go back out. Colostrum
has a laxative effect, helping to eliminate meconium - the original feces. It looks a little scary - black and sticky, like tar. 11 But don't worry, it won't always be like this. Breastfed babies usually have a slightly sweet smell of stool.
How many times a day you will need to change diapers and how the contents should look like, see below.
Day one
- Frequency: once or more.
- Colour: greenish black.
- Texture: sticky like tar.
Day two
- Frequency: twice or more.
- Colour: dark greenish brown.
- Texture: less sticky.
Day three
- Frequency: twice or more.
- Colour: greenish brown to brownish yellow.
- Texture: non-sticky.
Fourth day and then the entire first month
- Frequency: twice or more.
- Color: yellow (feces should turn yellow no later than the end of the fourth day).
- Texture: grainy (like mustard with grains interspersed). Leaky and watery.
The baby's urine should be light yellow. On average, babies urinate once a day for the first two days. Starting around the third day, the number of wet diapers increases to three, and from the fifth day onwards, diapers have to be changed five times a day or more often.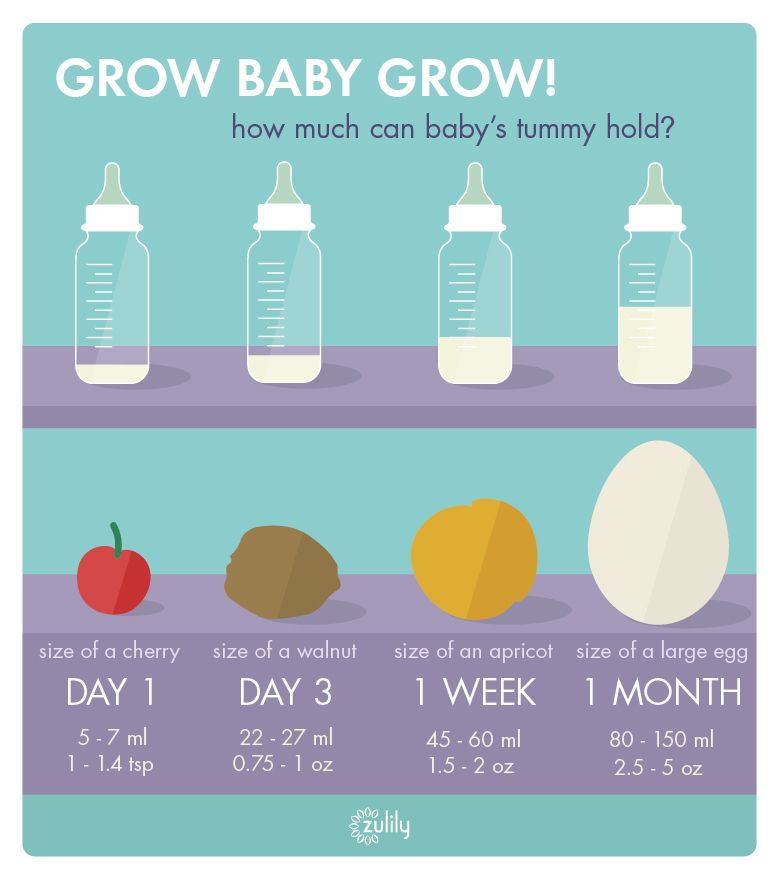 In addition, during the first few days, the weight of wet diapers increases. 11
In addition, during the first few days, the weight of wet diapers increases. 11
Is the baby getting enough breast milk?
Since very little milk is produced at first,
You may feel that your baby is not getting enough milk. But if you feed your baby on demand, you will produce exactly as much milk as he needs. If you want to keep the process under control, be guided by the frequency of diaper changes above. If your baby soils less diapers, check with your doctor.
“For the first three or four weeks, most babies just eat and sleep. If the child is worried and constantly asks for a breast, you should consult with your doctor, ”recommends Katie.
Sometimes the baby may vomit after feeding. If the vomit is the color of milk, this is not a cause for concern. But if there are orange, red, green, brown or black blotches in it, or the child vomits with a "fountain", consult a doctor. You should also consult a doctor if the baby has a high temperature, the fontanel (soft spot on the head) has sunk, blood is found in the stool, and also if the weight recorded at birth has not recovered within two weeks. 11
11
But if there are no frightening symptoms and the baby is growing at a normal pace, then he has enough milk. Soon you will both get used to breastfeeding and establish a more stable routine.
For the next step in breastfeeding, see Breastfeeding in the First Month: What to Expect.
Literature
1 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J9 Mammary Gland Biol Neoplasia . 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
2 Shashi R et al. Postpartum psychiatric disorders: Early diagnosis and management. Indian J Psychiatry . 2015; 57( Suppl 2): S 216– S 221. - Shashi R. et al., Postnatal mental disorders: early diagnosis and treatment. Indian J Saikiatri. 2015; 57(App 2):S216-S221.
- Shashi R. et al., Postnatal mental disorders: early diagnosis and treatment. Indian J Saikiatri. 2015; 57(App 2):S216-S221.
3 Moberg KU, Prime DK. Oxytocin effects in mothers and infants during breastfeeding. Infant . 2013;9(6):201-206. - Moberg K, Prime DK, "The effects of oxytocin on mother and child during breastfeeding." Infant. 2013;9(6):201-206.
4 Sobhy SI, Mohame NA. The effect of early initiation of breast feeding on the amount of vaginal blood loss during the fourth stage of labor. J Egypt Public Health Assoc . 2004;79(1-2):1-12. - Sobhi SI, Moham NA, "Early initiation of breastfeeding and its effect on vaginal bleeding in the fourth stage of labor." G Egypt Public Health Assoc. 2004;79(1-2):1-2.
5 Meier PP et al. Which breast pump for which mother: an evidence-based approach to individualizing breast pump technology. J Perinatol . 2016;36(7):493. - Meyer P.P. et al., Breastpump Selection: A Scientific Approach to Customizing Pumping Technology. J Perinatol (Journal of Perinatology). 2016;36(7):493-499.
J Perinatol . 2016;36(7):493. - Meyer P.P. et al., Breastpump Selection: A Scientific Approach to Customizing Pumping Technology. J Perinatol (Journal of Perinatology). 2016;36(7):493-499.
6 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women s Health . 2007;52(6):638-642. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
7 Kent JC et al. Principles for maintaining or increasing breast milk production. J Obstet , Gynecol , & Neonatal Nurs . 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production".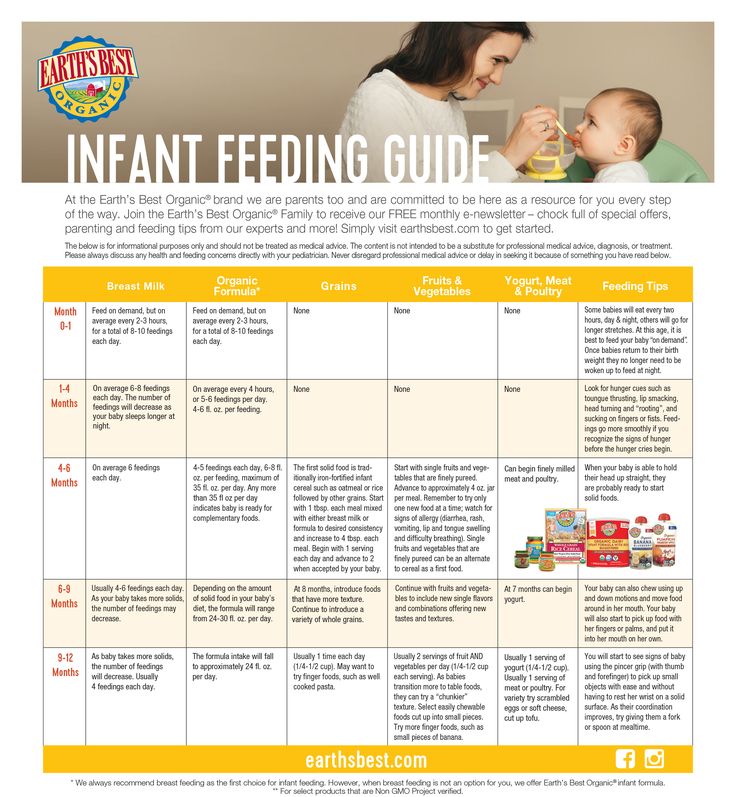 J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
8 Australian Breastfeeding Association [ Internet ]. Feeding cues ; 2017 Sep [ cited 2018 Feb ]. - Australian Breastfeeding Association [Internet], Feed Ready Signals; September 2017 [cited February 2018]
9 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe Frauenheilkd . 2013;73(12):1202-1208. - Jacobs A. et al., "Guidelines S -3 for the management of inflammatory breast disease during breastfeeding." Geburtskhilfe und Frauenheilkünde. 2013;73(12):1202-1208.
10 Lawrence RA, Lawrence RM. Breastfeeding: A guide for the medical profession.