Baby feeding milk with mother video
Maximising breastmilk - Baby Friendly Initiative
Any breastfeeding is valuable
Exclusive breastfeeding for the first six months ensures the best outcomes for babies. Right from birth, it’s important to ensure mothers and babies are supported to get breastfeeding off to the best possible start. However, there are some mothers who cannot or choose not to breastfeed exclusively. In these circumstances, any breastfeeding is valuable: babies benefit from receiving the maximum amount of breastmilk possible.
Managing supplementation rates
Evidence suggests that early supplementation is associated with an increased risk of stopping breastfeeding. This should therefore be avoided whilst feeding is being established. Ongoing sensitive support to ensure mothers can effectively attach their baby at their breast and know how to hand express if baby is reluctant to feed will reduce the need for supplementation.
Should a baby require supplementation for clinical reasons, this should be kept to a minimum, safe level and mothers should be encouraged to maintain their milk supply with a view to returning to full breastfeeding. Disruption to breastfeeding can also be minimised by choosing an alternative method of feeding which best supports the return to full breastfeeding when possible.
Local supplementation rates should be monitored and action taken if they appear to be increasing. There should be steady progress to reduce supplementation rates, especially for supplements given without medical indication or fully informed choice.
If a mother has decided to introduce formula milk for non-clinical reasons, ensure that she is aware that this may impact on her milk supply. It is important to adopt a gentle, non-judgemental approach when discussing this sensitive issue (see our guidance on conversations with mothers and our video on communication in pregnancy for tips). If she has made a fully informed decision to introduce formula milk, she can be supported to continue to provide breastmilk for her baby. You can work together on a plan to help her maximise her breastfeeding, thereby supporting her to see herself as a breastfeeding mother.
You can work together on a plan to help her maximise her breastfeeding, thereby supporting her to see herself as a breastfeeding mother.
Some mothers may want to return to full breastfeeding. Providing practical support around gradually decreasing the amount of formula she gives, whilst increasing her own milk supply, will help her make the transition as safely as possible.
This video outlines how to support women to maximise the amount of breastmilk they feed their baby and the impact this support has on mothers
To meet this standard
- In maternity services – help mothers and babies get breastfeeding off to a good start with uninterrupted skin-to-skin contact and support with positioning, attachment and hand expressing
- Where possible avoid supplementation whilst breastfeeding is being established
- If supplements are given for clinical indication or as a result of fully informed maternal decision, keep the amount of formula to a minimum (whilst ensuring safety of the baby) and support mother and baby to return to full breastfeeding as soon as possible
- Monitor supplementation rates with a view to reduce the rates for non-clinical reasons
- If a mother has decided to combine breast and formula milk, ensure that she has information and support to continue to maximise the amount of breastmilk and breastfeeding the baby receives
- Revisit the mother’s goals, as she may want to return to full breastfeeding after the initial challenges faced in the difficult early weeks; work with her to develop a plan to increase her milk production and gradually decrease the amount of formula used
- Remember to praise mothers: however much breastfeeding they are doing, they remain breastfeeding mothers.

Further resources
- Full details on achieving this standard are in the Baby Friendly Initiative Guide to the Standards
- Baby Friendly’s guide to having meaningful conversations with mothers talks through how to make the most of your time with a mother and how to provide effective, compassionate, mother-centred care
- For any persistent or complex problems, see our statement on additional and specialist support, as a requirement for the Baby Friendly standards
- The Baby Friendly maternity audit tool helps you to monitor supplementation rates in your unit. See also our dedicated supplementation form.
- The mother’s checklist for breastfeeding and breastfeeding assessment forms can be used to ensure that mothers are expressing their breastmilk effectively
- Sample infant feeding policies
- Videos on hand expression and communication with mothers
The health visitor says "Well done" and you feel so proud!
Breastfeeding mother
FIND OUT MORE
Video Blogs | Get Help
Preparing For Breastfeeding (3:48s)
Learn how to prepare for birth, including why you need to learn all you can about breastfeeding before you have your baby. Also, learn how to find health care providers who will support your decision to breastfeed.
How To Tell When Baby Is Hungry (2:29s)
Learn the feeding signs that tell you when your baby is hungry and when he is full.
How To Room-in With Baby (3:09s)
Learn how to room-in with baby. Sharing a room with baby during your hospital stay is the new normal and has health benefits for babies and moms.
Sharing a room with baby during your hospital stay is the new normal and has health benefits for babies and moms.
Colostrum to Full Milk Supply (2:00s)
In this video, Alisha and Candice, two moms from The Mom Team discuss what colostrum is, why it’s so important for your baby and helpful tips and tricks to make starting breastfeeding a little bit easier.
What To Expect On Baby's First Day (3:03s)
Learn about what to expect on baby's first day.
What To Expect On Baby's Second Day (1:51s)
Learn about what to expect on baby's second day. Your baby will probably want to eat very often on day 2, and that is normal.
Your baby will probably want to eat very often on day 2, and that is normal.
Help—Is This Normal? (1:46s)
Learn more about understanding when there are situations beyond what is normal and how you can ask for help.
When To Call Your Doctor (1:52s)
Get advice on when it's right to call your doctor. It's always okay to ask for help.
The Health Benefits of Breastfeeding (1:04s)
Learn about the health benefits of breastfeeding for mom and baby.
Breastmilk vs. Formula (3:26s)
Learn about the benefits of breastmilk compared to formula.
How Do Babies Sleep? (2:17s)
Learn about the two types of sleep that babies have.
How Do I Calm A Crying Baby? (1:44s)
All babies cry. Learn some great tips on how to help calm them.
Is Baby Getting Enough Milk? (3:04s)
Most moms make the perfect amount of milk for their babies. Learn more about milk transfer and making sure your baby is getting enough milk.
Learn more about milk transfer and making sure your baby is getting enough milk.
Am I Making Enough Milk? (2:01s)
Learn how to build a good milk supply by breastfeeding baby at the first signs of hunger.
Dads and Grandmas (2:28s)
Dads and grandmas can support moms to successfully breastfeed, even if no one else in the family has breastfed before.
Breastfeeding Myths (3:49s)
Learn about common breastfeeding myths. There is a lot of incorrect information out there about breastfeeding, and you need to have the real facts.
There is a lot of incorrect information out there about breastfeeding, and you need to have the real facts.
Preparing To Go Back To Work (2:24s)
Learn how to prepare to go back to work after having your baby. You can keep breastfeeding when you return to work, and it will keep baby healthier.
Bottle Feeding the Breastfed Baby (2:58s)
Angel and Amber from The Mom Team talk about the step you can take to bottle feed your breastfed baby.
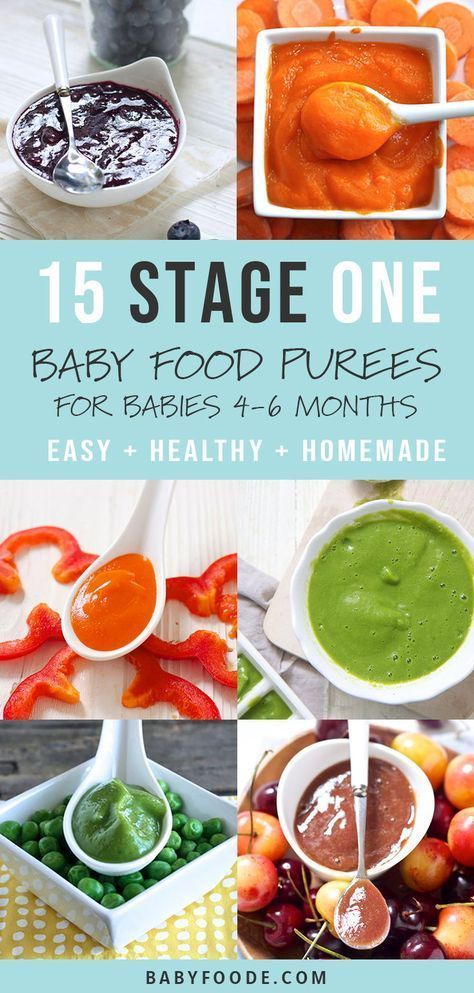
Introducing Solid Foods (5:39s)
In this VLOG two moms talk about knowing when your baby is ready to start solid foods. Also, learn how to make your own baby food at home and tips to try with your baby when beginning solid foods.
Also, learn how to make your own baby food at home and tips to try with your baby when beginning solid foods.
Introducing Solid Foods 6 to 7 Months (4:44s)
After seeing the signs that your baby is ready for solid foods, learn with real moms from the Mom Team, Nayeli and Claire, about your baby’s first few bites and the next couple months of introducing solid foods into your baby's diet.
Introducing Solid Foods 8 to 12 Months (2:20s)
Real moms, Nayeli and Claire, talk about continuing to add new foods into your baby's diet. Learn about moving from pureed foods to mashed or textured food.
Safe Formula Prep (5:17s)
Real moms, Amber and Nguyen, from The Mom Team discuss how to safely mix your baby’s formula. Learn how to safely store and mix your baby’s formula. The moms discuss sterilizing bottles with or without a dishwasher and how they should correctly be stored.
Various breastfeeding positions
Try different breastfeeding positions to find the one that works best for you and your baby. You can see the options in our selection of photos
Share this information
There is no right or wrong way to hold the baby while
feeding, and mom and baby are sure to find their favorite position.
It is important that both you and your child feel comfortable. 1.2 It's good to learn a few different breastfeeding positions and techniques because life's circumstances often require us to be flexible, especially as your baby gets older and you start to leave the house more often.
Whatever position you choose to breastfeed your baby, remember a few simple rules.
- Prepare everything you need before feeding, including drinks, food, mobile phone, TV remote control, book or magazine. And do not forget to go to the toilet - the feeding process can take a long time!
- Make sure your baby is comfortable. Whichever position you choose, it's important to keep your baby strong, level, and provide good support for their head, neck, and spine.
- You should also be comfortable. Don't stress. If necessary, use pillows of different sizes or rolls of towels to support your back or arms.
- Make sure your baby is latching on correctly. Proper grip is the key to comfort when breastfeeding.
- If your baby does not latch on well or you experience pain while feeding, contact a lactation consultant for help. The specialist will also be able to show you how to hold your baby more comfortably.
1. Relaxed feeding or reclining position
The relaxed feeding position, also known as biological feeding, 1 is often the first position for most mothers. If, immediately after birth, the baby is placed on the mother’s chest or stomach, normally, he instinctively reaches for the breast and tries to grab the nipple. This phenomenon is known as the breast seeking reflex. Skin-to-skin contact stimulates the infant's feeding instinct, and gravity helps him to latch onto the breast and maintain balance.
If, immediately after birth, the baby is placed on the mother’s chest or stomach, normally, he instinctively reaches for the breast and tries to grab the nipple. This phenomenon is known as the breast seeking reflex. Skin-to-skin contact stimulates the infant's feeding instinct, and gravity helps him to latch onto the breast and maintain balance.
But it's not just newborns that can be fed in the reclining position - this position is great for babies of all ages. It can be especially helpful if your baby does not latch well in other positions or does not like to be touched during feeding, and also if you have too much milk flow or too large breasts. Isabelle, a mother from the UK, shares her experience: “I had large breasts, and the baby was born small - 2.7 kg, so it was not easy to find a comfortable position at first. After a few weeks, it became clear that there was no “correct” posture for me. As a result, I most often fed lying down, putting the baby on my chest. ”
It is more convenient to feed not lying flat on your back, but half-sitting, leaning on pillows. So you will have a back support and you will be able to watch the baby during feeding.
So you will have a back support and you will be able to watch the baby during feeding.
2. Cradle position
This is the classic
first thought of breastfeeding. Mom sits straight
, and the baby lies on her side on her arm, pressing his stomach against her stomach. 3 Although this is a very popular position, it is not always easy to master with newborns because it gives the baby less support. Try putting a pillow under your back, and put a special breastfeeding pillow on your knees and lean on it with your hands. So you can more reliably support the child, without overstraining your back and shoulders. Just make sure that the baby does not lie too high on the pillow for feeding. The breast should remain at a natural level so that the baby can grab it without effort, otherwise sore nipples cannot be avoided.
“I breastfed in the cradle position because it suited me perfectly! It was comfortable and I loved just sitting and looking at my little one,” recalls Rachel, a mother of two from Italy.
3. Cross Cradle
This breastfeeding position looks almost the same as Cradle, but the baby is on the other arm. 3 This gives your baby support around the neck and shoulders so he can tilt his head to latch on. This position is great for breastfeeding newborns and small babies, as well as for babies who do not latch well. Since the baby lies completely on the other hand, it becomes easier to control his position and you can adjust the chest with your free hand.
Julie, a UK mother of two, finds this position very practical: “I usually breastfeed my youngest in the cross cradle position. So I have a free second hand, and I can take care of an older baby at the same time. ”
Do not hold the baby's head at first, otherwise you may inadvertently press his chin against his chest. Because of this, the child will not be able to take the breast deeply, because the nipple will rest against the base of the tongue, and not against the palate, which will lead to inflammation of the nipples. As the child grows, this position becomes more comfortable, and he can rest his head on your palm (as shown in the photo above).
As the child grows, this position becomes more comfortable, and he can rest his head on your palm (as shown in the photo above).
4. Underarm breastfeeding
In this position, also known as the “ball grip”, the mother sits with the baby lying along her arm at the side, legs towards the back of the chair (or any other seat). 3 Another comfortable position for newborn breastfeeding, you can give your baby good support, full control of his position and a good view of his face. And the baby feels safe in close contact with the mother's body. This position is especially good for those who have had a caesarean section or a premature birth, as well as mothers of twins and women with large breasts.
“When I breastfed my first daughter, I had very large K-sized breasts—twice the size of her head,” recalls Amy, an Australian mother of two. - I put rolls of towels under each breast, because they were very heavy, and fed my daughter in a pose from under the arm, but only sitting straighter so as not to crush her. This position was also convenient because I had a caesarean section and could not put the baby on my stomach.”
This position was also convenient because I had a caesarean section and could not put the baby on my stomach.”
5. Side-lying position
The side-lying position is ideal for a relaxed
nighttime feeding in bed or on the couch. If you had a
caesarean section or ruptures during childbirth, this position may be more comfortable than sitting down. 3 In this position, mother and baby lie side by side, tummy to tummy.
“It was difficult for me to sit during endless night feedings, firstly because of the caesarean section, and secondly because of lack of sleep,” recalls Francesca, a mother from the UK. “And then I discovered that you can feed your baby lying on your side and rest at the same time.”
“Because of the short tongue frenulum, Maisie could only properly latch on to her breasts while lying on her side. The lactation consultant showed me how it's done. In this position, the flow of milk was optimal for my daughter, and it was easier for her to keep the nipple in her mouth. As she got older, she became much better at grabbing her breasts in normal positions,” says Sarah, mother of two from Australia.
As she got older, she became much better at grabbing her breasts in normal positions,” says Sarah, mother of two from Australia.
6. Relaxed breastfeeding after caesarean section
If you can't find a comfortable position for breastfeeding after caesarean section, 3 try holding the baby on your shoulder in a reclining position – this does not stress the postoperative suture and allows you to breastfeed your baby comfortably. You can also try side feeding.
7. Sitting upright breastfeeding or “koala pose”
When breastfeeding in an upright position or “koala pose”, the baby sits with a straight back and a raised head on the mother's hip. 4 This position can be tried even with a newborn if it is well supported, but it is especially convenient for feeding a grown child who can already sit up by himself. The upright sitting position, or “koala pose,” is great for toddlers who suffer from reflux or ear infections and feel better sitting. In addition, this pose may be suitable for children with a shortened frenulum of the tongue or reduced muscle tone.
In addition, this pose may be suitable for children with a shortened frenulum of the tongue or reduced muscle tone.
“When my daughter got a little older, I would often feed her in an upright position, which was more comfortable for both of us, and I could still hold her close,” recalls Peggy, a mother from Switzerland. “Besides, it was possible to discreetly breastfeed her in public places.”
8. Overhanging position
In this position, the baby lies on his back, and the mother bends over him
on all fours so that the nipple falls directly into his mouth. 4 Some moms say this breastfeeding position is good to use occasionally for mastitis, when touching the breasts is especially unpleasant. Some say that this breastfeeding position helps with blockage of the milk ducts, although there is no scientific evidence for this yet. You can also feed in the “overhanging” position while sitting, kneeling over the baby on a bed or sofa, as well as reclining on your stomach with support on your elbows. Pillows of various sizes that you can lean on will help you avoid back and shoulder strain.
Pillows of various sizes that you can lean on will help you avoid back and shoulder strain.
“I have breastfed several times in the 'overhang' position for clogged milk ducts when no other means of dissolving the blockage worked. And this pose seems to have helped. I think it's because of gravity, and also because the breasts were at a completely different angle than with normal feeding, and my daughter sucked her differently, ”says Ellie, a mother of two from the UK.
Feeding in the "overhanging" position is unlikely to be practiced regularly, but in some cases this position may be useful.
“I used to breastfeed in the overhang position when my baby was having trouble latch-on,” says Lorna, mother of two in the UK. - This, of course, is not the most convenient way, but then I was ready for anything, if only he could capture the chest. We succeeded and have been breastfeeding for eight months now!”
9. Breastfeeding in a sling or in a sling
Breastfeeding in a sling takes some practice, but it can be used to go out, look after older children, or even do a little household chores.
The sling is also useful if the baby does not like to lie down or is often attached to the breast. Lindsey, a mother of two in the US, notes: “I used the carrier frequently for both of my children. When we were out, I tied the sarong around my neck and covered the carrier with it. Under such a cape, the baby can eat as much as he wants until he falls asleep.
This breastfeeding position is best when the baby is already good at breastfeeding and can hold his head up by himself. Any slings are suitable for breastfeeding, including elastic and rings, as well as carrying bags. Whatever option you choose, the main thing is that you can always see the face of the child, and his chin does not rest against his chest.
10. Double hand-held breastfeeding
Double hand-held breastfeeding (or “double-ball grab”) is great for mothers of twins—you can breastfeed both at the same time and keep your arms relatively free. 4 When feeding in this position, it is advisable to use a special pillow for breastfeeding twins, especially at first. It will provide extra support and help keep both babies in the correct position, as well as reduce the burden on the abdomen if you had a caesarean section. In addition, the hands are freer, and if necessary, you can deal with one child without interfering with the second.
It will provide extra support and help keep both babies in the correct position, as well as reduce the burden on the abdomen if you had a caesarean section. In addition, the hands are freer, and if necessary, you can deal with one child without interfering with the second.
“My twins were born very tiny and had to be fed every two hours at any time of the day or night. Very soon it became clear: if I want to do anything besides feeding, I need to feed them both at the same time, - says Emma, mother of two children from the UK. “I breastfed them two by hand using a breastfeeding pillow.”
Other good positions for breastfeeding twins are two criss-cross cradles, one baby in the cradle and the other close at hand, reclining feeding, or sitting upright (one baby on one side, the other on the other).
11. Breastfeeding in the "hand-supported" or "dancer's hand" position
muscle tone (which is typical for premature babies, children suffering from various diseases or Down syndrome), try supporting his head and your chest at the same time. 4 Grasp your chest with your palm underneath so that your thumb is on one side and all the others are on the other. Move your hand slightly forward so that your thumb and forefinger form a "U" just in front of your chest. With the other three fingers, continue to support the chest. With your thumb and forefinger, hold the baby's head while feeding so that his chin rests on the part of the palm between them, your thumb gently holds the baby on one cheek, and your index finger on the other. So the baby gets excellent support, and you can control his position and see if he is holding his breast.
4 Grasp your chest with your palm underneath so that your thumb is on one side and all the others are on the other. Move your hand slightly forward so that your thumb and forefinger form a "U" just in front of your chest. With the other three fingers, continue to support the chest. With your thumb and forefinger, hold the baby's head while feeding so that his chin rests on the part of the palm between them, your thumb gently holds the baby on one cheek, and your index finger on the other. So the baby gets excellent support, and you can control his position and see if he is holding his breast.
Literature
1 Colson SD et al. Optimal positions for the release of primitive neonatal reflexes stimulating breastfeeding. Early Hum Dev . 2008;84(7):441-449. - Colson S.D. et al., "Optimal Positions for Provoking Primitive Innate Reflexes to Induce Breastfeeding." Early Hume Dev. 2008;84(7):441-449.
2 UNICEF UK BFHI [ Internet ]. Off to the best start ; 2015 [ cited 2018 Feb ]. - UNICEF UK, Baby-Friendly Hospital Initiative, Start the Best You Can [Internet]. 2015 [cited February 2018].
Off to the best start ; 2015 [ cited 2018 Feb ]. - UNICEF UK, Baby-Friendly Hospital Initiative, Start the Best You Can [Internet]. 2015 [cited February 2018].
3 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women's Health. 2007;52(6):638-642. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
4 Wambach K, Riordan J, editors. Breastfeeding and human lactation. Jones & Bartlett Learning ; 2014. 966 p . - Wambach K., Riordan J., "Breastfeeding and female lactation". Burlington, MA: Publishing House Jones & Bartlett Learning ; 2014. Pp. 966.
Pp. 966.
Breastfeeding in case of maternal illness.
home
Articles
Nutrition
Stulova Maria Aleksandrovna Breastfeeding consultant
09.10.2013
Mom got sick! Nightmare! Grandmothers rush to the rescue, trying to protect the baby from infection and let the patient recover in peace.
However, good intentions and ignorance of physiology often lead to negative results.
Very important: if a nursing mother falls ill, it is necessary to choose medications that are compatible with breastfeeding*, and continue breastfeeding!!!
Contraindications to breastfeeding are the following diseases of the mother:
- eclampsia, severe bleeding during childbirth and in the postpartum period,
- open tuberculosis,
- state of severe decompensation in chronic diseases of the heart, lungs, kidneys, liver,
- and hyperthyroidism,
- acute mental illness,
- especially dangerous infections (typhus, cholera, etc.
 ),
), - herpetic eruptions on the nipple of the mammary gland (before their follow-up treatment),
- HIV infection.
With such diseases of a nursing mother as rubella, chicken pox, measles, mumps, cytomegalovirus infection, herpes simplex, acute intestinal and acute respiratory viral infections, if they occur without severe intoxication, breastfeeding, subject to the rules of general hygiene, is not contraindicated.
The presence of hepatitis B and C in women is currently not a contraindication to breastfeeding, however, feeding is carried out through special silicone pads. In acute hepatitis A in the mother, breastfeeding is prohibited.
And if we are dealing with banal colds, flu or mastitis, then interrupting breastfeeding for the duration of the illness is NOT good for either the mother or the child.
Why?
Because by the time the mother has symptoms of the disease, the child may already be infected. He is in a state of “pre-disease”, but has the opportunity not to get sick or to suffer the disease in a mild / latent form.
To do this, it is necessary to help the baby's immune system and save the body's resources to fight infection. What can help the immune system are breast milk immunoglobulins, as well as a huge amount of vitamins and other biologically active substances from milk.
How to preserve the resources of the body - provide the child with the most easily digestible food (this is breast milk), which will save energy, reduce stressful situations (absence of a mother nearby, inability to habitually suckle the breast, the appearance of a new person in the house to care for the baby), save heat (avoid long walks in the cold season). Conclusion: the main help for the child's body is the preservation of the usual rhythm of breastfeeding and the usual contact with the mother.
If we decide to interrupt breastfeeding for the duration of the illness, then the child has to be transferred to artificial formula. What is NOT good for the child:
- The child is deprived of mother's milk immunoglobulins and many bioactive substances
- The load on the gastrointestinal tract increases, because the mixture is an indigestible product to which the body must adapt
- The risk of allergies increases and, accordingly, the body's resistance to infections decreases
- The child is deprived of habitual sucking and nutrition, and with it the necessary contact with the mother - this is psychological stress for the baby, weakening the body's resources
- Often, when suckling the nipple, the child develops a mechanism of improper sucking, which prevents a further return to breastfeeding
What is NOT useful for a mother to interrupt breastfeeding during illness:
A change in the rhythm and quality of breast emptying, which in turn can provoke lactostasis, and then mastitis (especially if the mother has a bacterial infection).
During illness, the breast must be emptied very efficiently, sometimes giving the child to suck even more often than usual and from different positions. At the same time, many children themselves increase the rhythm of attachments during illnesses (mother's and / or their own) - they seem to “hang” on their chest for a couple of days. And grandmothers at this time can help mom around the house, take care of hygiene and the baby.
Usually safe, used in medium doses, are short courses of paracetamol, ibuprofen; most cough medicines; antibiotics - ampicillin and other penicillins, erythromycin. However, in the instructions for these drugs, you will most likely find a contraindication - breastfeeding. This is due to the fact that the manufacturer must conduct studies on the effect of the drug on the child through breast milk. Since it is very expensive and not every pharmaceutical company can conduct such studies, manufacturers are forced to write a warning. Studies by foreign companies show that the above drugs practically do not penetrate into breast milk (either due to the very large size of the molecules, or due to strong binding to blood proteins) and cannot harm the baby.