Baby food protease
Protein digestion of baby foods: study approaches and implications for infant health
[1] Michaelsen KF, Greer FR, Protein needs early in life and long-term health. Am. J. Clin. Nutr. 2014, 99, 718S–722S. [PubMed] [Google Scholar]
[2] Nelson WE, Kliegman R, Nelson textbook of pediatrics, Saunders, Philadelphia, PA: 2011. [Google Scholar]
[3] Lonnerdal B, Nutritional and physiologic significance of human milk proteins. Am. J. Clin. Nutr. 2003, 77, 1537S–1543S. [PubMed] [Google Scholar]
[4] Galli SJ, Tsai M, Piliponsky AM, The development of allergic inflammation. Nature 2008, 454, 445–454. [PMC free article] [PubMed] [Google Scholar]
[5] Grimshaw KEC, Maskell J, Oliver EM, Morris RCG, et al., Introduction of complementary foods and the relationship to food allergy. Pediatrics 2013, 132, e1529–e1538. [PubMed] [Google Scholar]
[6] Complementary feeding: report of the global consultation, and summary of guiding principles for complementary feeding of the breastfed child, World Health Organization; 2003. [Google Scholar]
[7] Eidelman AI, Schanler RJ, Johnston M, Landers S, et al., Breastfeeding and the use of human milk. Pediatrics 2012, 129, e827–e841. [PubMed] [Google Scholar]
[8] Agostoni C, Decsi T, Fewtrell M, Goulet O, et al., Complementary feeding: a commentary by the ESPGHAN committee on nutrition. J. Pediatr. Gastroenterol. Nutr. 2008, 46, 99–110. [PubMed] [Google Scholar]
[9] Victora CG, Bahl R, Barros AJD, França GVA, et al., Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. The Lancet 2016, 387, 475–490. [PubMed] [Google Scholar]
[10] Brown K, Dewey K, Allen L, Complementary feeding of young children in developing countries: a review of current scientific knowledge, World Health Organization, Geneva: 1998. [Google Scholar]
[11] Neville MC, Anderson SM, McManaman JL, Badger TM, et al., Lactation and neonatal nutrition: defining and refining the critical questions. J. Mammary Gland Biol. Neoplasia 2012, 17, 167–188. [PMC free article] [PubMed] [Google Scholar]
[PMC free article] [PubMed] [Google Scholar]
[12] Bourlieu C, Menard O, Bouzerzour K, Mandalari G, et al., Specificity of infant digestive conditions: some clues for developing relevant in vitro models. Crit. Rev. Food Sci. Nutr. 2014, 54, 1427–1457. [PubMed] [Google Scholar]
[13] Poquet L, Wooster TJ, Infant digestion physiology and the relevance of in vitro biochemical models to test infant formula lipid digestion. Mol. Nutr. Food Res. 2016, 60, 1876–1895. [PubMed] [Google Scholar]
[14] Wal JM, Cow’s milk proteins/allergens. Ann. Allergy, Asthma Immunol. 2002, 89, 3–10. [PubMed] [Google Scholar]
[15] Shan L, Molberg O, Parrot I, Hausch F, et al., Structural basis for gluten intolerance in Celiac Sprue. Science 2002, 297, 2275–2279. [PubMed] [Google Scholar]
[16] Duodu KG, Taylor JRN, Belton PS, Hamaker BR, Factors affecting sorghum protein digestibility. Journal of Cereal Science 2003, 38, 117–131. [Google Scholar]
[17] Liu DS, Wang YY, Yu Y, Hu JH, et al. , Effects of enzymatic dephosphorylation on infant in vitro gastrointestinal digestibility of milk protein concentrate. Food Chem. 2016, 197, 891–899. [PubMed] [Google Scholar]
, Effects of enzymatic dephosphorylation on infant in vitro gastrointestinal digestibility of milk protein concentrate. Food Chem. 2016, 197, 891–899. [PubMed] [Google Scholar]
[18] de Jongh HHJ, Robles CL, Timmerman E, Nordlee JA, et al., Digestibility and IgE-binding of glycosylated codfish parvalbumin. Biomed Res. Int. 2013, 2013. [PMC free article] [PubMed] [Google Scholar]
[19] Boonvisut S, Whitaker JR, Effect of heat, amylase, and disulfide bond cleavage on the in vitro digestibility of soybean proteins. J. Agric. Food Chem. 1976, 24, 1130–1135. [PubMed] [Google Scholar]
[20] Hamaker BR, Kirleis AW, Butler LG, Axtell JD, Mertz ET, Improving the in vitro protein digestibility of sorghum with reducing agents. Proc. Natl. Acad. Sci. U. S. A. 1987, 84, 626–628. [PMC free article] [PubMed] [Google Scholar]
[21] Breiteneder H, Mills ENC, Molecular properties of food allergens. J. Allergy Clin. Immunol. 2005, 115, 14–23. [PubMed] [Google Scholar]
[22] Sicherer SH, Sampson HA, Food allergy. J. Allergy Clin. Immunol. 2010, 125, S116–S125. [PubMed] [Google Scholar]
J. Allergy Clin. Immunol. 2010, 125, S116–S125. [PubMed] [Google Scholar]
[23] Host A, Frequency of cow’s milk allergy in childhood. Annals of Allergy Asthma & Immunology 2002, 89, 33–37. [PubMed] [Google Scholar]
[24] Hays T, Wood RA, A systematic review of the role of hydrolyzed infant formulas in allergy prevention. Arch. Pediatr. Adolesc. Med. 2005, 159, 810–816. [PubMed] [Google Scholar]
[25] Alexander DD, Cabana MD, Partially hydrolyzed 100% whey protein infant formula and reduced risk of atopic dermatitis: a meta-analysis. J. Pediatr. Gastroenterol. Nutr. 2010, 50, 422–430. [PubMed] [Google Scholar]
[26] Szajewska H, Horvath A, Meta-analysis of the evidence for a partially hydrolyzed 100% whey formula for the prevention of allergic diseases. Curr. Med. Res. Opin. 2010, 26, 423–437. [PubMed] [Google Scholar]
[27] Greer FR, Sicherer SH, Burks AW, Comm N, Effects of early nutritional interventions on the development of atopic disease in infants and children: the role of maternal dietary restriction, breastfeeding, timing of introduction of complementary foods, and hydrolyzed formulas. Pediatrics 2008, 121, 183–191. [PubMed] [Google Scholar]
Pediatrics 2008, 121, 183–191. [PubMed] [Google Scholar]
[28] Boyle RJ, Ierodiakonou D, Khan T, Chivinge J, et al., Hydrolysed formula and risk of allergic or autoimmune disease: systematic review and meta-analysis. BMJ-British Medical Journal 2016, 352, i974. [PMC free article] [PubMed] [Google Scholar]
[29] Moscovici AM, Joubran Y, Briard-Bion V, Mackie A, et al., The impact of the Maillard reaction on the in vitro proteolytic breakdown of bovine lactoferrin in adults and infants. Food Funct. 2014, 5, 1898–1908. [PubMed] [Google Scholar]
[30] Mehta BM, Deeth HC, Blocked lysine in dairy products: formation, occurrence, analysis, and nutritional implications. Comprehensive Reviews in Food Science and Food Safety 2016, 15, 206–218. [Google Scholar]
[31] Feeney RE, Means GE, Bigler JC, Inhibition of human trypsin, plasmin, and thrombin by naturally occurring inhibitors of proteolytic enzymes. J. Biol. Chem. 1969, 244, 1957–1960. [PubMed] [Google Scholar]
[32] Rehman ZU, Shah WH, Thermal heat processing effects on antinutrients, protein and starch digestibility of food legumes. Food Chem. 2005, 91, 327–331. [Google Scholar]
Food Chem. 2005, 91, 327–331. [Google Scholar]
[33] Finot PA, Aeschbacher HU, Hurrell RF, Liardon R, The Maillard reaction in food processing, human nutrition and physiology, Birkhauser Verlag, Basel: 1990. [Google Scholar]
[34] Finot PA, Historical perspective of the Maillard reaction in food science. Ann. N. Y. Acad. Sci. 2005, 1043, 1–8. [PubMed] [Google Scholar]
[35] Restani P, Fiocchi A, Restelli R, Velona T, et al., Effect of technological treatments on digestibility and allergenicity of meat-based baby foods. J. Am. Coll. Nutr. 1997, 16, 376–382. [PubMed] [Google Scholar]
[36] Ahmed J, Ramaswamy HS, Viscoelastic properties of sweet potato puree infant food. J. Food Eng. 2006, 74, 376–382. [Google Scholar]
[37] Ahmed J, Ramaswamy HS, Viscoelastic and thermal characteristics of vegetable puree-based baby foods. J. Food Process Eng. 2006, 29, 219–233. [Google Scholar]
[38] Ahmed J, Ramaswamy HS, Dynamic rheology and thermal transitions in meat-based strained baby foods. J. Food Eng. 2007, 78, 1274–1284. [Google Scholar]
J. Food Eng. 2007, 78, 1274–1284. [Google Scholar]
[39] Ramamoorthi L, Lee Y, Brewer S, Effect of food matrix and heat treatment on the rheological properties of salmon-based baby food. J. Food Eng. 2009, 95, 432–437. [Google Scholar]
[40] Bourlieu C, Menard O, De La Chevasnerie A, Sams L, et al., The structure of infant formulas impacts their lipolysis, proteolysis and disintegration during in vitro gastric digestion. Food Chem. 2015, 182, 224–235. [PubMed] [Google Scholar]
[41] Mackie A, Macierzanka A, Colloidal aspects of protein digestion. Current Opinion in Colloid & Interface Science 2010, 15, 102–108. [Google Scholar]
[42] Oria MP, Hamaker BR, Axtell JD, Huang CP, A highly digestible sorghum mutant cultivar exhibits a unique folded structure of endosperm protein bodies. Proc. Natl. Acad. Sci. U. S. A. 2000, 97, 5065–5070. [PMC free article] [PubMed] [Google Scholar]
[43] Duodu KG, Nunes A, Delgadillo I, Parker ML, et al., Effect of grain structure and cooking on sorghum and maize in vitro protein digestibility. Journal of Cereal Science 2002, 35, 161–174. [Google Scholar]
Journal of Cereal Science 2002, 35, 161–174. [Google Scholar]
[44] Johnson LR, Gastrointestinal physiology, Elsevier Health Sciences; 2013. [Google Scholar]
[45] Chen JS, Food oral processing - a review. Food Hydrocolloids 2009, 23, 1–25. [Google Scholar]
[46] Hamosh M, Digestion in the newborn. Clin. Perinatol. 1996, 23, 191–209. [PubMed] [Google Scholar]
[47] Stolovitz P, Gisel EG, Circumoral movements in response to three different food textures in children 6 months to 2 years of age. Dysphagia 1991, 6, 17–25. [PubMed] [Google Scholar]
[48] Blossfeld I, Collins A, Kiely M, Delahunty C, Texture preferences of 12-month-old infants and the role of early experiences. Food Qual. Prefer. 2007, 18, 396–404. [Google Scholar]
[49] Carruth BR, Skinner JD, Feeding behaviors and other motor development in healthy children (2–24 months). J. Am. Coll. Nutr. 2002, 21, 88–96. [PubMed] [Google Scholar]
[50] Bailey KV, Dental development in new guinean infants. J. Pediatr. 1964, 64, 97–100. [PubMed] [Google Scholar]
J. Pediatr. 1964, 64, 97–100. [PubMed] [Google Scholar]
[51] Archambault M, Millen K, Gisel EG, Effect of bite size on eating development in normal children 6 months to 2 years of age. Phys. Occup. Ther. Pediatr. 1991, 10, 29–47. [Google Scholar]
[52] Kamegai T, Tatsuki T, Nagano H, Mitsuhashi H, et al., A determination of bite force in northern Japanese children. Eur. J. Orthod. 2005, 27, 53–57. [PubMed] [Google Scholar]
[53] Le Reverend BJD, Edelson LR, Loret C, Anatomical, functional, physiological and behavioural aspects of the development of mastication in early childhood. Br. J. Nutr. 2014, 111, 403–414. [PMC free article] [PubMed] [Google Scholar]
[54] Benaryeh H, Lapid S, Szargel R, Benderly A, Gutman D, Composition of whole unstimulated saliva of human infants. Arch. Oral Biol. 1984, 29, 357–362. [PubMed] [Google Scholar]
[55] Agunod M, Yamaguch N, Lopez R, Luhby AL, Glass GBJ, Correlative study of hydrochloric acid, pepsin, and intrinsic factor secretion in newborns and infants. Am. J. Dig. Dis. 1969, 14, 400–414. [PubMed] [Google Scholar]
Am. J. Dig. Dis. 1969, 14, 400–414. [PubMed] [Google Scholar]
[56] Rødbro P, Krasilnikoff PA, Christiansen PM, Parietal cell secretory function in early childhood. Scand. J. Gastroenterol. 1967, 2, 209–213. [PubMed] [Google Scholar]
[57] Mason S, Some aspects of gastric function in the newborn. Arch. Dis. Child. 1962, 37, 387–391. [PMC free article] [PubMed] [Google Scholar]
[58] Harries JT, Fraser AJ, The acidity of the gastric contents of premature babies during the first fourteen days of life. Biol. Neonat. 1968, 12, 186–193. [PubMed] [Google Scholar]
[59] Cavell B, Postprandial gastric acid secretion in infants. Acta Paediatr. Scand. 1983, 72, 857–860. [PubMed] [Google Scholar]
[60] Dressman JB, Berardi RR, Dermentzoglou LC, Russell TL, et al., Upper gastrointestinal (GI) pH in young, healthy men and women. Pharm. Res. 1990, 7, 756–761. [PubMed] [Google Scholar]
[61] Roman C, Carriere F, Villeneuve P, Pina M, et al., Quantitative and qualitative study of gastric lipolysis in premature infants: Do MCT-enriched infant formulas improve fat digestion? Pediatr. Res. 2007, 61, 83–88. [PubMed] [Google Scholar]
Res. 2007, 61, 83–88. [PubMed] [Google Scholar]
[62] Russell TL, Berardi RR, Barnett JL, Dermentzoglou LC, et al., Upper gastrointestinal pH in seventy-nine healthy, elderly, North American men and women. Pharm. Res. 1993, 10, 187–196. [PubMed] [Google Scholar]
[63] Calbet JAL, Holst JJ, Gastric emptying, gastric secretion and enterogastrone response after administration of milk proteins or their peptide hydrolysates in humans. Eur. J. Nutr. 2004, 43, 127–139. [PubMed] [Google Scholar]
[64] Rødbro P, Krasilnikoff P, Bitsch V, Gastric secretion of pepsin in early childhood. Scand. J. Gastroenterol. 1967, 2, 257–260. [PubMed] [Google Scholar]
[65] Sondheimer JM, Clark DA, Gervaise EP, Continuous gastric pH measurement in young and older healthy preterm infants receiving formula and clear liquid feedings. J. Pediatr. Gastroenterol. Nutr. 1985, 4, 352–355. [PubMed] [Google Scholar]
[66] Van Den Driessche M, Peeters K, Marien P, Ghoos Y, et al., Gastric emptying in formula-fed and breast-fed infants measured with the C-13-octanoic acid breath test. J. Pediatr. Gastroenterol. Nutr. 1999, 29, 46–51. [PubMed] [Google Scholar]
J. Pediatr. Gastroenterol. Nutr. 1999, 29, 46–51. [PubMed] [Google Scholar]
[67] Maes BD, Ghoos YF, Geypens BJ, Hiele MI, Rutgeerts PJ, Relation between gastric emptying rate and energy intake in children compared with adults. Gut 1995, 36, 183–188. [PMC free article] [PubMed] [Google Scholar]
[68] Bonner JJ, Vajjah P, Abduljalil K, Jamei M, et al., Does age affect gastric emptying time? A model-based meta-analysis of data from premature neonates through to adults. Biopharm. Drug Disposition 2015, 36, 245–257. [PMC free article] [PubMed] [Google Scholar]
[69] Boirie Y, Dangin M, Gachon P, Vasson MP, et al., Slow and fast dietary proteins differently modulate postprandial protein accretion. Proc. Natl. Acad. Sci. U. S. A. 1997, 94, 14930–14935. [PMC free article] [PubMed] [Google Scholar]
[70] Jarvenpaa AL, Rassin DK, Raiha NCR, Gaull GE, Milk protein quantity and quality in the term infant II. Effects on acidic and neutral amino acids. Pediatrics 1982, 70, 221–230. [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
[71] Tolia V, Lin CH, Kuhns LR, Gastric emptying using three different formulas in infants with gastroesophageal reflux. J. Pediatr. Gastroenterol. Nutr. 1992, 15, 297–301. [PubMed] [Google Scholar]
[72] Whitcomb DC, Lowe ME, Human pancreatic digestive enzymes. Dig. Dis. Sci. 2007, 52, 1–17. [PubMed] [Google Scholar]
[73] Zoppi G, Andreotti G, Pajnofer F, Njai DM, Gaburro D, Exocrine pancreas function in premature and full term neonates. Pediatr. Res. 1972, 6, 880–886. [PubMed] [Google Scholar]
[74] Lebenthal E, Lee PC, Development of functional response in human exocrine pancreas. Pediatrics 1980, 66, 556–560. [PubMed] [Google Scholar]
[75] Borulf S, Lindberg T, Cathodal elastase in duodenal Juice from children with gastrointestinal disorders. Pediatr. Res. 1981, 15, 1051–1054. [PubMed] [Google Scholar]
[76] Norman A, Ojamae O, Strandvi. B, Bile acids and pancreatic enzymes during absorption in the newborn. Acta Paediatr. Scand.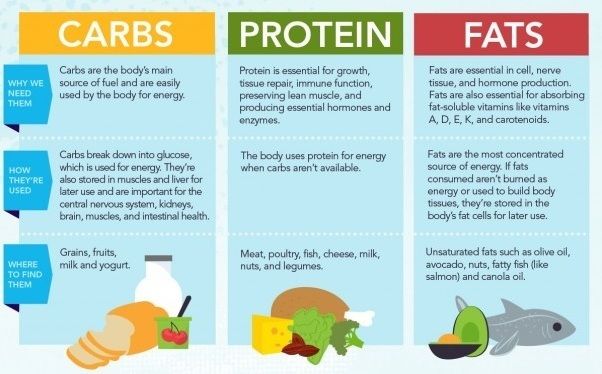 1972, 61, 571–576. [PubMed] [Google Scholar]
1972, 61, 571–576. [PubMed] [Google Scholar]
[77] McCloy R, Greenberg G, Baron J, Duodenal pH in health and duodenal ulcer disease: effect of a meal, Coca-Cola, smoking, and cimetidine. Gut 1984, 25, 386–392. [PMC free article] [PubMed] [Google Scholar]
[78] Klumpp TG, Neale AV, The gastric and duodenal contents of normal infants and children: the duodenal enzyme activity and the gastric and duodenal reactions (H-ion). Am. J. Dis. Child. 1930, 40, 1215–1229. [Google Scholar]
[79] Dumont RC, Rudolph CD, Development of gastrointestinal motility in the infant and child. Gastroenterol. Clin. North Am. 1994, 23, 655–671. [PubMed] [Google Scholar]
[80] Bode S, Dreyer T, Greisen G, Gastric emptying and small intestinal transit time in preterm infants: a scintigraphic method. J. Pediatr. Gastroenterol. Nutr. 2004, 39, 378–382. [PubMed] [Google Scholar]
[81] Myo K, Bolin TD, Oo T, Nyunt TW, et al., Investigation of small-intestinal transit time in normal and malnourished children. J. Gastroenterol. 1999, 34, 675–679. [PubMed] [Google Scholar]
J. Gastroenterol. 1999, 34, 675–679. [PubMed] [Google Scholar]
[82] Van den Driessche M, Van Malderen N, Geypens B, Ghoos Y, Veereman-Wauters G, Lactose- C-13 ureide breath test: a new, noninvasive technique to determine orocecal transit time in children. J. Pediatr. Gastroenterol. Nutr. 2000, 31, 433–438. [PubMed] [Google Scholar]
[83] Evenepoel P, Claus D, Geypens B, Hiele M, et al., Amount and fate of egg protein escaping assimilation in the small intestine of humans. American Journal of Physiology-Gastrointestinal and Liver Physiology 1999, 277, G935–G943. [PubMed] [Google Scholar]
[84] Windey K, De Preter V, Verbeke K, Relevance of protein fermentation to gut health. Mol. Nutr. Food Res. 2012, 56, 184–196. [PubMed] [Google Scholar]
[85] Fan PX, Li LS, Rezaei A, Eslamfam S, et al., Metabolites of dietary protein and peptides by intestinal microbes and their impacts on gut. Curr. Protein Peptide Sci. 2015, 16, 646–654. [PubMed] [Google Scholar]
[86] Pieper R, Boudry C, Bindelle J, Vahjen W, Zentek J, Interaction between dietary protein content and the source of carbohydrates along the gastrointestinal tract of weaned piglets. Arch. Anim. Nutr. 2014, 68, 263–280. [PubMed] [Google Scholar]
Arch. Anim. Nutr. 2014, 68, 263–280. [PubMed] [Google Scholar]
[87] Lucassen P, Assendelft WJJ, Gubbels JW, van Eijk JTM, et al., Effectiveness of treatments for infantile colic: systematic review. Br. Med. J. 1998, 316, 1563–1569. [PMC free article] [PubMed] [Google Scholar]
[88] Camilleri M, Park SY, Scarpato E, Staiano A, Exploring hypotheses and rationale for causes of infantile colic. Neurogastroenterol. Motil. 2017, 29, 11. [PMC free article] [PubMed] [Google Scholar]
[89] de Weerth C, Fuentes S, Puylaert P, de Vos WM, Intestinal microbiota of infants with colic: development and specific signatures. Pediatrics 2013, 131, E550–E558. [PubMed] [Google Scholar]
[90] Chatterton DEW, Rasmussen JT, Heegaard CW, Sorensen ES, Petersen TE, In vitro digestion of novel milk protein ingredients for use in infant formulas: research on biological functions. Trends Food Sci. Technol. 2004, 15, 373–383. [Google Scholar]
[91] Hernandez-Ledesma B, Quiros A, Amigo L, Recio I, Identification of bioactive peptides after digestion of human milk and infant formula with pepsin and pancreatin.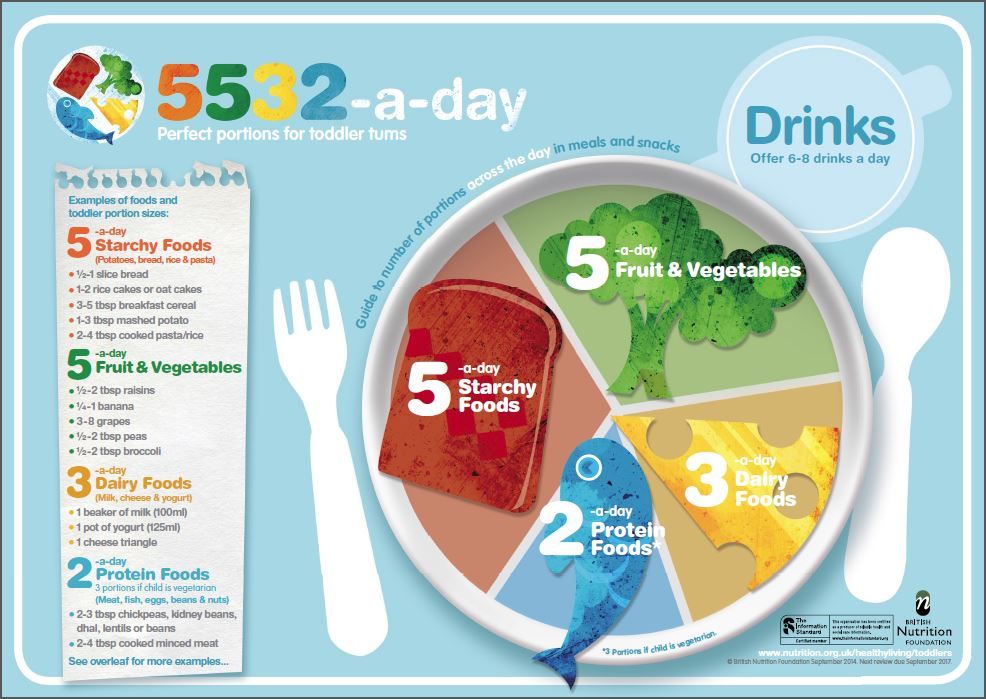 Int. Dairy J. 2007, 17, 42–49. [Google Scholar]
Int. Dairy J. 2007, 17, 42–49. [Google Scholar]
[92] Dupont D, Mandalari G, Molle D, Jardin J, et al., Comparative resistance of food proteins to adult and infant in vitro digestion models. Mol. Nutr. Food Res. 2010, 54, 767–780. [PubMed] [Google Scholar]
[93] Dupont D, Mandalari G, Molle D, Jardin J, et al., Food processing increases casein resistance to simulated infant digestion. Mol. Nutr. Food Res. 2010, 54, 1677–1689. [PubMed] [Google Scholar]
[94] Shani-Levi C, Levi-Tal S, Lesmes U, Comparative performance of milk proteins and their emulsions under dynamic in vitro adult and infant gastric digestion. Food Hydrocolloids 2013, 32, 349–357. [Google Scholar]
[95] Zhang Q, Cundiff JK, Maria SD, McMahon RJ, et al., Differential digestion of human milk proteins in a simulated stomach model. J. Proteome Res. 2014, 13, 1055–1064. [PubMed] [Google Scholar]
[96] Wada Y, Lonnerdal B, Bioactive peptides released from in vitro digestion of human milk with or without pasteurization. Pediatr. Res. 2015, 77, 546–553. [PubMed] [Google Scholar]
Pediatr. Res. 2015, 77, 546–553. [PubMed] [Google Scholar]
[97] Menard O, Cattenoz T, Guillemin H, Souchon I, et al., Validation of a new in vitro dynamic system to simulate infant digestion. Food Chem. 2014, 145, 1039–1045. [PubMed] [Google Scholar]
[98] Darragh AJ, Moughan PJ, The three-week-old piglet as a model animal for studying protein digestion in human infants. J. Pediatr. Gastroenterol. Nutr. 1995, 21, 387–393. [PubMed] [Google Scholar]
[99] Moughan P, Birtles M, Cranwell P, Smith W, Pedraza M, The piglet as a model animal for studying aspects of digestion and absorption in milk-fed human infants. Nutritional triggers for health and in disease 1992, 67, 40–113. [PubMed] [Google Scholar]
[100] Aguilera A, de Souza TCR, Mariscal-Landin G, Escobar K, et al., Standardized ileal digestibility of proteins and amino acids in sesame expeller and soya bean meal in weaning piglets. J. Anim. Physiol. Anim. Nutr. 2015, 99, 728–736. [PubMed] [Google Scholar]
[101] Morise A, Seve B, Mace K, Magliola C, et al. , Impact of intrauterine growth retardation and early protein intake on growth, adipose tissue, and the insulin-like growth factor system in piglets. Pediatr. Res. 2009, 65, 45–50. [PubMed] [Google Scholar]
[102] Bouzerzour K, Morgan F, Cuinet I, Bonhomme C, et al., In vivo digestion of infant formula in piglets: protein digestion kinetics and release of bioactive peptides. Br. J. Nutr. 2012, 108, 2105–2114. [PubMed] [Google Scholar]
[103] Catzeflis C, Schutz Y, Micheli JL, Welsch C, et al., Whole body protein synthesis and energy expenditure in very low birth weight infants. Pediatr. Res. 1985, 19, 679–687. [PubMed] [Google Scholar]
[104] Decsi T, Veitl V, Szasz M, Pinter Z, Mehes K, Plasma amino acid concentrations in healthy, full-term infants fed hydrolysate infant formula. J. Pediatr. Gastroenterol. Nutr. 1996, 22, 62–67. [PubMed] [Google Scholar]
[105] Hirata Y, Matsuo T, Kokubu H, Digestion and absorption of milk protein in infants’ intestine. Kobe J. Med. Sci. 1965, 11, 103–109. [Google Scholar]
Sci. 1965, 11, 103–109. [Google Scholar]
[106] Dallas DC, Guerrero A, Khaldi N, Borghese R, et al., A peptidomic analysis of human milk digestion in the infant stomach reveals protein-specific degradation patterns. J. Nutr. 2014, 815–820. [PMC free article] [PubMed] [Google Scholar]
[107] Holton TA, Vijayakumar V, Dallas DC, Guerrero A, et al., Following the digestion of milk proteins from mother to baby. J. Proteome Res. 2014, 13, 5777–5783. [PMC free article] [PubMed] [Google Scholar]
[108] Amidon GL, Lennernas H, Shah VP, Crison JR, A theoretical basis for a biopharmaceutic drug classification: the correlation of in vitro drug product dissolution and in vivo bioavailability. Pharm. Res. 1995, 12, 413–420. [PubMed] [Google Scholar]
[109] Emami J, In vitro-in vivo correlation: from theory to applications. Journal of Pharmacy and Pharmaceutical Sciences 2006, 9, 169–189. [PubMed] [Google Scholar]
[110] Su MY, Broadhurst M, Liu CP, Gathercole J, et al., Comparative analysis of human milk and infant formula derived peptides following in vitro digestion. Food Chem. 2017, 221, 1895–1903. [PubMed] [Google Scholar]
Food Chem. 2017, 221, 1895–1903. [PubMed] [Google Scholar]
[111] Kannan S, Nielsen SS, Mason AC, Protein digestibility-corrected amino acid scores for bean and bean-rice infant weaning food products. J. Agric. Food Chem. 2001, 49, 5070–5074. [PubMed] [Google Scholar]
[112] Yoneda M, Shiraishi J, Kuraishi T, Aoki F, et al., Gastric proteinase digestion of caseins in newborn pups of the mouse. J. Dairy Sci. 2001, 84, 1851–1855. [PubMed] [Google Scholar]
[113] Olsen IE, Harris CL, Lawson ML, Berseth CL, Higher protein intake improves length, not weight, z scores in preterm infants. J. Pediatr. Gastroenterol. Nutr. 2014, 58, 409–416. [PubMed] [Google Scholar]
[114] Inostroza J, Haschke F, Steenhout P, Grathwohl D, et al., Low-protein formula slows weight gain in infants of overweight mothers. J. Pediatr. Gastroenterol. Nutr. 2014, 59, 70–77. [PMC free article] [PubMed] [Google Scholar]
[115] Maas C, Mathes M, Bleeker C, Vek J, et al., Effect of increased enteral protein intake on growth in human milk-fed preterm infants: a randomized clinical trial. JAMA Pediatrics 2017, 171, 16–22. [PubMed] [Google Scholar]
JAMA Pediatrics 2017, 171, 16–22. [PubMed] [Google Scholar]
Protease Enzymes in Human Milk
Author(s):
J. Bruce German
Download full article
- Full Article
Author: J. Bruce German
Key Messages
Human milk evolved not as simple proteins but rather as a combination of proteins and protease enzymes.
Young infants are developmentally naïve, produce little gastric acid, and express low protease activity.
The selective proteolysis of milk proteins begins within the mammary gland.
Introduction
The emergence of lactation as the system of nourishing infants has been a core asset to the success of mammalia. The traits of lactation selected within the mother infant dyad has been a Darwinian engine of nourishment for over 200 million years [1]. The proteins of milk are proving to be an even more complex nutrition and protection system than previously considered. Scientists are now using modern tools of biological research to understand milk proteins and their digestion into peptides within infants [2, 3]. Mapping these peptides to the proteins that contained them and the sites that were cleaved revealed a surprising result: the protease enzymes defined by their cleavage specificity correspond to enzymes not in babies but in the milk [4]. A total of five protease enzymes (plasmin, cathepsin, elatase, kalikrein, and amino and carboxypeptidase) were identified to be either translocated to or synthesized in the mammary gland, present in milk, and active within the infant stomach. These results suggest that milk evolved not as simple proteins but rather as a combination of proteins and protease enzymes.
Scientists are now using modern tools of biological research to understand milk proteins and their digestion into peptides within infants [2, 3]. Mapping these peptides to the proteins that contained them and the sites that were cleaved revealed a surprising result: the protease enzymes defined by their cleavage specificity correspond to enzymes not in babies but in the milk [4]. A total of five protease enzymes (plasmin, cathepsin, elatase, kalikrein, and amino and carboxypeptidase) were identified to be either translocated to or synthesized in the mammary gland, present in milk, and active within the infant stomach. These results suggest that milk evolved not as simple proteins but rather as a combination of proteins and protease enzymes.
Implications
First: the infant. The current paradigm for protein nourishment is that intact proteins denatured by stomach acid and attacked by endogenous proteases in the stomach begin a digestive process that continues with hydrolysis by neutral proteases in the small intestine, and ultimately leads to the release and complete absorption of amino acids by the intestinal epithelia. Young infants, however, are developmentally naïve, produce little gastric acid, and express low protease activity. Nonetheless, infants digest and absorb milk proteins effectively with an array of proteases activated within the infant and contributing to catalytic activity. Specificity to protein digestion within the infant has some important implications to infant nourishment.
Young infants, however, are developmentally naïve, produce little gastric acid, and express low protease activity. Nonetheless, infants digest and absorb milk proteins effectively with an array of proteases activated within the infant and contributing to catalytic activity. Specificity to protein digestion within the infant has some important implications to infant nourishment.
Second: the milk. There are no means at hand to measure – and much less to deliver – this aspect of human milk to all infants. Sharing of breast milk, storing, processing, all will affect the net ability of milk’s enzymes to selectively digest the proteins. Formula does not currently contain these activities. Scientific discovery must now identify all peptides released, where and when, annotate their functions, and understand their value to infants.
Third: the mother. The selective proteolysis of milk proteins begins within the mammary gland. Are these activities of benefit to the mother, to lactation? How diverse are these activities across mothers, across lactation, across varying maternal health and nutritional status? Answers to these questions will guide future policies and practices of lactation.
Understanding this magnificent system of nourishment is likely to provide insights for nourishing humans of all ages and all health conditions.
Fig. 1. Schematic of production and transfer of enzymes into milk within the lactating mammary gland. Enzymes can reach milk by direct protein synthesis by the epithelial cell, by translocation from blood, and by secretion from immune cells within the mammary gland and milk itself
References
1. Oftedal OT: The mammary gland and its origin during synapsid evolution. J Mammary Gland Biol Neoplasia 2002;7:225–252.
2. Dallas DC, Guerrero A, Khaldi N, Castillo PA, Martin WF, Smilowitz JT, Bevins CL, Barile D, German JB, Lebrilla CB: Extensive in vivo human milk peptidomics reveals specific proteolysis yielding protective antimicrobial peptides. J Proteome Res 2013;12:2295–2304
3. Dallas DC, Guerrero A, Khaldi N, Borghese R, Bhandari A, Underwood MA, Lebrilla CB, German JB, Barile D: A peptidomic analysis of human milk digestion in the infant stomach reveals protein-specific degradation patterns. J Nutr 2014;144:815–820.
J Nutr 2014;144:815–820.
4. Khaldi N, Vijayakumar V, Dallas DC, Guerrero A, Wickramasinghe S, Smilowitz JT, Medrano JF, Lebrilla CB, Shields DC, German JB: Predicting the important enzyme players in human breast milk digestion. J Agric Food Chem 2014;62:7225–7232.
Soy: a potential hazard for therapeutic baby food | partners
| Studies of the properties of soy and its effect on the adult and children's organisms are not completed. But soy products are strictly not recommended for children with congenital hypothyroidism, premature infants, underweight and disorders of the gastrointestinal tract |
Key words / keywords: Nestle meals for kids, Nutrition science, pediatric
Soy and products from it imperceptibly, but are firmly included in our daily diet. Today it is already becoming problematic to find a food product, meat or dairy, which would not include soy protein. nine0011
Today it is already becoming problematic to find a food product, meat or dairy, which would not include soy protein. nine0011
A few years ago, the world was swept by "soy fever": the benefits of the product were described everywhere and in the brightest colors. Japan was cited as an example, where the average resident eats 27 kg of soybeans annually, while in Europe this figure was only 3 kg. The high life expectancy of the Japanese was put in direct dependence on soybeans. Recent studies have shown that there were much fewer reasons for such enthusiasm than it seemed.
Research on the positive and negative properties of soybeans continues today, and the debate between advocates and opponents continues to flare up. nine0011
In defense of soy
To date, it can be considered proven that soy protein can fully replace animal protein. In addition, unlike meat, soy does not increase the level of "bad" cholesterol and, accordingly, the risk of cardiovascular disease. As a plant product, soy is a source of useful vitamins and minerals that have a positive effect on metabolism, and can serve as a prevention of cancer and some other diseases.
As a plant product, soy is a source of useful vitamins and minerals that have a positive effect on metabolism, and can serve as a prevention of cancer and some other diseases.
Big "But"
Scientists around the world who are closely involved in the study of soy warn that the use of soy products, along with the benefits, is fraught with certain dangers, which should not be forgotten when compiling your diet, and especially when planning the diet of children. The threat posed by soy may not manifest itself in healthy people, but with certain pathologies of the endocrine and digestive systems, such a diet can aggravate the condition of patients. In children, the active use of soy products can lead to disruption of the formation and normal functioning of some body systems. nine0011
Why is soy dangerous?
Soy as a plant over the centuries of its existence has developed protective properties that prevent pests - insects and animals from actively eating it. The same anti-nutritional factors cause the negative effects of soy intake on the human body.
The same anti-nutritional factors cause the negative effects of soy intake on the human body.
So, most of the protease inhibitors contained in soy products are not cleaved in gastric juice and, passing on, block the work of pancreatic enzymes, forcing it to work much more actively, causing its hypertrophy. nine0011
Lectins, which are part of soy, make it difficult to absorb in the intestines. Under-digested and remaining in the intestinal lumen, polypeptides are an excellent breeding ground for bacteria and cause the formation of toxins. Studies also show that the same substances cause growth retardation in children.
Plant hormones (phytoestrogens) of soy negatively affect the maturation of the reproductive system. In girls, this is expressed in the early onset of menstruation, while in boys, sexual development slows down, and a decrease in testosterone levels is observed. Even in adults, in some cases, on the background of a soy diet, problems with conception in women and impotence in men were noted. nine0011
nine0011
The strumagenic substances of soybeans cause thyroid dysfunction, up to the formation of a goiter. This problem most often occurs against the background of iodine deficiency in the daily diet. As early as half a century ago, it was proved that a diet based on soy flour led to serious endocrine disorders in infants.
Thus, soy products are strictly not recommended for babies with congenital hypothyroidism and other endocrine problems. The risk category also includes premature infants, children with underweight and disorders of the gastrointestinal tract. nine0011
Soy and GMOs
Soy is one of the most beloved plants by geneticists, so it is really difficult to find a soy product that has not undergone genetic modification today. According to domestic experts, genetically modified soybeans are not used in the food industry in our country. But, even if this information is to be believed, the soy products that we see on store shelves are rarely of Russian origin.
We reduce risks to a minimum!
Research on the various properties of soybeans and their effect on adults and children is far from over. Often such works give contradictory results, and scientists often explain the discrepancies in data in different countries by the peculiarities of genetic memory and the tradition of using this product. In Russia, where the history of soy use, to put it mildly, does not go back to the Middle Ages, the population is more at risk of encountering unforeseen results of fashionable adherence to this product. nine0011
The already proven dangers of soy-based diets in young children are leading responsible manufacturers to move away from soy supplements in infant formulas, and especially in formulas.
Resource Clinutren Junior: Soy-Free Special Nutrition for Children
Ready-to-eat nutritional formula from Nestle was created specifically for children from one to 11 years old, taking into account the needs of a rapidly growing body. When preparing a unique recipe, scientists took into account the latest recommendations from the pediatric community. Therefore, the product contains high-quality milk protein - a source of essential amino acids, as well as fats, carbohydrates, a rich set of 29vitamins and minerals.
When preparing a unique recipe, scientists took into account the latest recommendations from the pediatric community. Therefore, the product contains high-quality milk protein - a source of essential amino acids, as well as fats, carbohydrates, a rich set of 29vitamins and minerals.
The mixture is suitable as an additional food - a 200 ml bottle is convenient to take to a kindergarten or school. In case of illness and serious condition of the baby, Resource Clinutren Junior can replace the entire daily diet.
Children will no doubt appreciate the delicious chocolate, strawberry or vanilla drink, while parents will love its carefully balanced composition and the absence of potentially harmful products.
Enzyme preparations for delicious pastries | FNW
Various enzyme preparations have been widely used in the food industry for a long time. Their use in baking for the production of crackers, biscuits and waffles allows you to get high-quality and tasty products.
The presence of a large amount of fat and sugar in the recipe often has a depressing effect on the maturation of yeast dough. Sometimes the quality of modern types of flour also does not allow to produce a product that meets certain standards and characteristics. And even high-quality raw materials do not always, for one reason or another, make it possible to follow the standards of baking. The use of enzymes from Kerry Bioscience (Netherlands) will help optimize flour properties. nine0011
Enzymes can affect both the quality of the flour used and the technology, and in the finished product, the taste, texture, maturation speed of the dough and appearance. The composition of flour includes proteins, carbohydrates and fats in small quantities. Complex food enzymes affect precisely the protein and carbohydrate components of flour.
One preparation may contain several enzymes at the same time, for example, protease + amylase or protease + hemicellulase, etc.
Also, enzymes can affect the softening of the gluten texture, the cohesion of the dough, and improve the color of the crust of an already baked product. Some types of enzymes make it possible to replace sodium metabisulphite in crackers by introducing bacterial proteases. In specialty products such as ice cream cones and wafer sheets, enzymes can change the viscosity of the dough and reduce the hygroscopicity of the finished product.
Some types of enzymes make it possible to replace sodium metabisulphite in crackers by introducing bacterial proteases. In specialty products such as ice cream cones and wafer sheets, enzymes can change the viscosity of the dough and reduce the hygroscopicity of the finished product.
Kerry Bioscience (Netherlands) markets its products under the brand name Biobake®. In the production of biscuits, crackers and wafers, enzyme preparations make it possible to control the rheology of the dough, reduce the amount of fat in the recipe, affect the color of the crust and the structure of the finished product, help increase productivity and improve the flavor yield. nine0011
Biobake ® BPN is a concentrated proteolytic product available in powder form. Due to the action of the protease, gluten is stretched and destroyed by endohydrolysis. This, in turn,
has the effect of reducing the shrinkage of the dough and improves the control over the size of the product.
Biobake ® BSC is a powdered blend of bacterial protease and amylase. Protease destroys gluten by endohydrolysis and affects its stretching, amylase crushes starch into simple sugars and reduces water absorption. Such a product is used for the production of crackers. This enzyme improves the extensibility and the ability to control the size of the finished cracker. nine0011
Biobake ® CDI is a powdered bacterial protease supplemented with yeast extract. Yeast extract is used as a functional carrier. Like the enzyme preparations described above, this product works in a similar way. Biobake ® CDI also reduces the number of breakages, the finished product is more crunchy. Despite a number of advantages of adding conventional baking powder, it also has negative aspects, such as the destruction of vitamin B2, the effect on the taste of the finished product and possible allergenicity. Enzyme Biobake ® CDI is also used in the production of crackers and biscuits as an alternative replacement for sodium metabisulphite.